Abstract
Purpose
There is growing interest in intelligent assistive technologies (IATs) in the rehabilitation and support of older adults, however, the factors contributing to or preventing their use in practice are not well understood. This study aimed to develop an overview of current knowledge on barriers and facilitators to the use of smart technologies in rehabilitative practice with older adults.
Materials and Methods
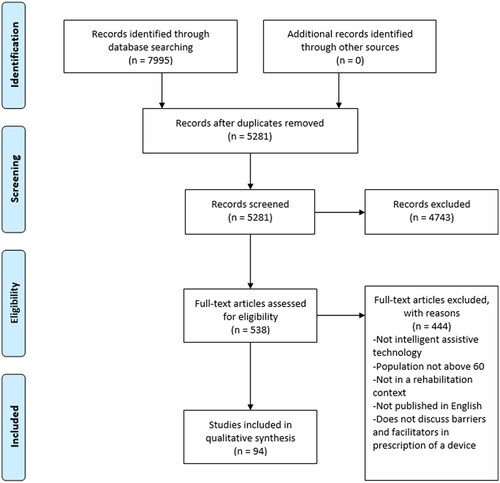
We undertook a scoping review following guidelines proposed by Arksey and O’Malley (2005) and Levac et al. (2010). A computerised literature search was conducted using the Scopus and Ovid databases, yielding 7995 citations. Of these, 94 studies met inclusion criteria. Analysis of extracted data identified themes which were explored in semi-structured interviews with a purposefully selected sample of seven clinical rehabilitation practitioners (three physical therapists, two occupational therapists, and two speech-language pathologists).
Results
Barriers and facilitators to using these technologies were associated with accessibility, reported effectiveness, usability, patient-centred considerations, and staff considerations.
Conclusions
Collaborative efforts of policy-makers, researchers, manufacturers, rehabilitation professionals, and older persons are needed to improve the design of technologies, develop appropriate funding and reimbursement strategies, and minimise barriers to their appropriate use to support independence and quality of life. Any strategies to improve upon barriers to prescribing smart technologies for older people should leverage the expertise of rehabilitation professionals operating at the interface between older people; their health/mobility; their families; and technology-based solutions.
IMPLICATIONS FOR REHABILITATION
There is growing interest in intelligent assistive technologies (IATs) in the rehabilitation of older adults, as well as barriers to their use in practice.
Rehabilitation professionals can play a key role in enabling access to IATs by recommending or prescribing their use to their older clients. Strategies to address barriers to the use of IATs for older people should leverage the expertise of rehabilitation professionals operating at the interface between older people, their families, and technology-based solutions.
Older people and their families require technical support to initiate and continue to use IATs for rehabilitation. While rehabilitation providers may be well-placed to offer this support, they may require time and organizational support to build and maintain expertise in the fast-advancing field of smart technologies for rehabilitation.
Cost and usability are universal challenges across the types of smart technologies considered in this review. Participatory approaches to involving older people in the design and development of smart assistive technologies contribute to better usability of these technologies. Devices and interventions that leverage more readily available devices and lower-cost components may overcome cost barriers to accessibility.
Introduction
Worldwide, more than 250 million older people are estimated to live with a moderate to severe disability [Citation1]. Over the past 30 years, demand for rehabilitation grew by 63% [Citation2], contributing to staff shortages and wait lists to receive rehabilitation services [Citation3,Citation4].
In Canada, nearly 90% of older people living with a disability report using an assistive technology (AT), which are devices designed to “maintain or improve an individual’s functioning and independence to facilitate participation and to enhance overall well-being” [Citation5,Citation6]. Assistive technologies have tremendous potential to support meaningful daily activities of individuals who experience functional limitations, to increase independence, and to enable aging-in-place for a growing older adult population [Citation7–9]. AT devices can range from relatively low-tech options, such as a conventional walking cane [Citation10], to sophisticated high-tech devices, such as robotic exoskeletons [Citation11]. By 2050, more than two billion people worldwide will require an assistive technology [Citation12], and though there is evidence of the barriers and facilitators for older adults [Citation13], little is known about the barriers to prescribing these devices to older adults [Citation14].
In many cases, rehabilitation providers enable access to assistive technologies by recommending or prescribing their use to clients. There are challenges, though, in accessing these devices, such as a lack of awareness of AT devices, and differences in power and priorities between providers and consumers of AT devices [Citation15]. These challenges may be felt acutely by older people, who are most likely to need rehabilitation services [Citation2]. Given expected increases in demand for rehabilitative services and assistive technologies, combined with staff shortages, a better understanding of the extreme variability (between 35–86%) of abandonment of AT is warranted [Citation16].
Intelligent assistive technologies (IATs) are a type of AT which harness innovations in communications, robotics, sensors and voice-activated systems into assistive technologies [Citation17]. Ienca and colleagues, in a recent review characterised the rapidly expanding field of IATs into six categories: 1) wearables (smart-watches, GPS necklaces, fall monitoring); 2) handheld devices (tablets, GPS trackers, fitness trackers, smartphones); 3) mobility aids (smart canes, smart wheelchairs with built-in sensors); 4) voice-activated assistants (Siri, Alexa, Google Home); 5) distributed systems (including smart-homes with integrated sensors for light and heat); and 6) situation-specific robots (floor cleaning, soothing, emotional response) [Citation17,Citation18]. Both AT and IAT have showed promising results as a cost-effective health care investment to improve the quality of life for older people [Citation19,Citation20]. Although work has been done on AT adoption and service delivery processes in certain age groups [Citation21,Citation22], to our knowledge, no previous studies have examined the barriers and facilitators to IAT prescription and use among older adults in a rehabilitation context. Though similar barriers, such as cost, access, and privacy, have been shown to affect the use of both AT and IAT by older people [Citation13,Citation17], we feel that given the rate at which smart assistive technology has advanced, a separate discussion of facilitators and barriers to IAT use is warranted. Furthermore, access to assistive technology is legislatively protected as an international human right and allocated government funding in more than 80% of WHO member states [Citation23]. Smart-enabled AT does not enjoy this protection or widespread government support, yet the market for these devices is expected to grow to $5 billion USD by 2031 [Citation24]. As the spectrum of IAT doubles every 5 years [Citation17], in the future, all AT may be technology-enabled, and the distinction between AT and IAT will be redundant. At present, IAT are a unique subset of AT, with potentially different sets of facilitators and barriers to their use. Specifically, an independent discussion of IAT facilitators and barriers is warranted, if governments are to broaden their coverage of IAT, as suggested by Ienca [Citation17], to avoid recreating the expensive, fragmented, inaccessible, and inequitable features of the current global AT market [Citation23,Citation25–28].
Reviews which have focused on older adults have been narrow, investigating the use of IAT devices among older adults with specific diseases, such as dementia and alzheimers [Citation29–31], or specific devices, such as exoskeletons [Citation32–34]. As the first review of factors affecting IAT prescription and use, this paper will provide professionals practicing in the field of rehabilitation with an overview of the barriers and facilitators that may be experienced by older people using these devices. We aimed to identify the barriers and facilitators that influence use -prescription, acquisition, implementation, and adoption- of intelligent assistive technologies (IATs) among older adults for the purpose of rehabilitation.
Materials and methods
Rehabilitation research is heterogeneous, with a wide range of study types (qualitative, quantitative), clinicians involved, health care settings (inpatient, outpatient, acute, long-term care) and publication sites. This diversity makes scoping reviews especially appropriate for rehabilitation research [Citation35]. Scoping reviews are designed to provide information about the breadth and depth of a field of literature and identify priorities for future research [Citation36].
We conducted a scoping review guided by the framework developed by Arksey and O’Malley [Citation37] and refined by Levac and colleagues [Citation36] using the following six steps: defining the research question; identifying relevant studies; study selection; charting the data; collating, summarising and reporting the results; and consultation. Each step is described below:
Step 1: Identify the research question
We asked: What are the facilitators and barriers that exist in rehabilitation settings which influence the prescription, acquisition, implementation, or adoption of intelligent assistive technologies for older adults?
Step 2: Identify relevant studies
The search strategy was developed in consultation with a university health sciences librarian. Search terms included: self-help devices; assistive technology; remote sensing technology; innovation; robotics; medical device; invention; handheld computer; microcomputer; minicomputer; sensory aids; rehabilitation; exercise therapy; physical therapy; physiotherapy; occupational therapy; geriatrics; older adults; elderly; and aged.
The Scopus and Ovid databases were searched for English language studies from 1998 to August 2021, a time frame chosen as reflective of modern AT use in rehabilitative settings.
Step 3: Study selection
Citations and abstracts identified in the search were amalgamated into RefWorks, a web-based reference management software. Four reviewers (MM, LN, KL, LR) screened out studies with irrelevant titles and abstracts. Studies were included if they: addressed assistive technology in a rehabilitative context between 1998-2021; described information-enabled or “smart” assistive technologies and described barriers and facilitators to their use in rehabilitation; the average age of participants was 60 or older, or else persons aged 60 or older and older were the majority of participants; or selected papers which look at older adults, or in the case of articles where no age range is provided, explicitly commented on older adults. Any study type was permitted, and any rehabilitative setting, such as inpatient and outpatient hospital settings, community settings, outpatient therapist practice settings [Citation38], and research instiutions were included. Articles in which the average age was below 60, or did not explicitly investigate older adults were excluded. The age 60 years old was used as a cut off for inclusion to match the United Nations definition of an older person [Citation39]. For the purpose of this review, use of IAT devices will be considered across a continuum of prescription, acquisition, implementation, and adoption. The study selection process is summarised in , which is adapted from the PRISMA diagram produced by Moher et al. [Citation40]. Any discrepancies were resolved by discussion between the reviewers, or by referring to a third reviewer.
Step 4: Charting the data
Reviewers recorded the author(s), country, year, study population, study type, description of the technology, barriers, and facilitators in a data extraction table shown in .
Table 1. Extracted data.
Step 5: Collating summarising, and reporting the results
Reviewers used an inductive thematic approach to identify, analyse and report on themes related to facilitators and barriers to prescription, acquisition, implementation, and adoption of assistive technologies [Citation41]. Reviewers familiarised themselves with the data by making notes about the extraction table and debriefing with one another during the extraction process. Reviewers individually coded the data in the extraction table, and then met as a group to collate codes into themes [Citation41]. After collating the themes, the reviewers agreed to names, and definitions for each theme [Citation41].
Step 6: Consultation
The final stage of the review included consulting with rehabilitation professionals to obtain their perspectives on the facilitators and barriers to IAT use in rehabilitation settings with older adults. Key informants included occupational therapists, physiotherapists, and speech-language pathologists whose scope of practice included the prescription and acquisition of both assistive technologies and intelligent assistive technologies. Purposeful sampling was used to obtain two or more professionals from each of the three specialties. To be included in the consultation, professions must have had clinical experience related to prescription and recommendation of assistive technologies, possess knowledge of assistive devices, be fluent in English, and be able to provide informed consent. Semi-structured interviews were used to collect data from participants, with an interview guide including questions related to how much experience professionals had with assistive technologies, how well informed they are regarding intelligent assistive technologies, what works well in practice for intelligent and traditional assistive technologies, and what are the most prominent barriers to their use and implementation. Participants were not provided the results of the scoping review prior to their interviews to ensure that responses were that of the respondent alone, and not impacted by the initial research findings. Rather, findings were reflected in the interview prompts, where data and details surrounding the barriers and facilitators to IAT use, as identified in the scoping review, were translated to questions which were then posed to participants. This was done to collect unbiased opinions from the consulting clinicians. Interviews were conducted over the phone and were audio-taped for transcription. Thematic analysis was used to analyse interview data [Citation41]. Interview results were then integrated with the results of the scoping review, using excerpts and quotes from interviews to support and reinforce findings identified in the review. Ethics clearance was provided by the University of Waterloo Office of Research Ethics (ORE# 30529).
Results
Two databases, Scopus (5485) and Ovid (2510), were searched for articles published between January 1998 and August 2021, generating 7995 articles, of which 5281 were screened for title and abstract, 538 were screened for full-text, and 94 were included in the qualitative synthesis. See for the combined study selection process. A sample of 40 articles with a Cohen’s Kappa of 0.61, demonstrated substantial agreement between reviewers (MM, LR).
Ienca’s typology was instructive in categorising the types of IATs found in this review [Citation17]. This review included 33 studies on handheld devices, 27 on situation-specific robots, 9 on distributed systems, 7 studies on wearables, one study about intelligent mobility aids, and no studies on voice-activated assistants. In 17 of the included studies, multiple categories of IATs were discussed.
Included studies were published in 27 different countries, predominantly the United States (n = 21), Canada (n = 15), and the Netherlands (n = 10), and used 20 different study designs, predominantly qualitative interviews (n = 23), reviews (n = 18), and surveys (n = 11). The IAT users represented by the included studies experienced a variety of conditions including: Alzheimer’s/dementia (n = 17), stroke (n = 15), and heart failure (n = 4). Other IAT users included people living with: diabetes, sarcopenia, hearing loss, low vision, and people living with disabilities. The average age of participants within included studies ranged from 60.1 years [Citation25], to 85.8 years [Citation42].
Key informants included seven clinical rehabilitation practitioners [three physical therapists (PTs), two occupational therapists (OTs), and two speech-language pathologists (SLPs)] working in the Canadian province of Ontario. Experience amongst the professionals consulted ranged from five to 30 years; two participants taught in universities. All participants were female, with the exception of one physical therapist.
We identified five main themes in the data that help categorise facilitators and barriers to prescribing IAT: accessibility, effectiveness, usability, patient-centred considerations, and staff considerations. These are presented below, in , along with related sub-themes.
Table 2. Themes and sub-themes.
Accessibility
Many of the articles discussed prescribing IATs in rehabilitation as enabled or constrained by issues of access. This theme contained findings about awareness of what IATs are available, as well as costs of IATs and how to pay for and acquire them. The theme of accessibility is summarized in .
Table 3. Accessibility summary.
Awareness and access
Many articles contained findings about the problems of accessing technologies that are in the research and development stage and are not yet commercially available [Citation43–47]. Some articles indicated that low and middle-income countries may not have implemented policy frameworks related to assistive technology in general, may have low supplies of IATs, and/or difficulties evaluating available technologies [Citation25–27]. Additionally, some people with limited mobility may struggle to access IAT devices located in hospitals or rehabilitation centres [Citation48]. Internet-based services and treatments offered by computers, tablets, or smartphones were reported to be currently accessible, or as a way to improve future accessibility [Citation49–51], though they may be lacking in healthcare institutions [Citation51]. Rehabilitation mediated through commonly available handheld devices may be able to improve access to those who are geographically more isolated [Citation49]. Some studies found that users’ awareness of available IAT devices was limited, making it more difficult to access devices [Citation52,Citation53]. In places with a wide variety of IATs available, patients may be overwhelmed by the choice among many options [Citation52]. Some studies discussed strategies to enhance access to IATs, such as leveraging the widespread availability of smartphones or tablets as platforms to deliver rehabilitation services, as well as remote access to tele-operated devices [Citation48,Citation54]. Another study cited the low-cost and widespread availability of single-factor sensors to enable IAT prescription and use [Citation45]. One study indicated that health institutions owning, leasing or renting IAT, especially for high-tech, high-cost IATs such as robotics or exoskeletons, would improve access [Citation55].
The interviewed practitioners discussed trialling technology as a way to improve patients’ access to technology: “they get the trial with whatever the equipment is, and they realise how great it is - they feel safer, they just feel better, and then they end up buying the equipment” - [OT1].
Cost
High cost to individuals was listed as a barrier to accessibility of IAT in a considerable proportion of the studies in this review [Citation25,Citation27,Citation43,Citation47,Citation48,Citation53,Citation55–69]. Cost of IATs was the barrier most frequently cited in a focus group study of older powered chair users [Citation70]. Conversely, the affordability of a wearable robotic orthosis glove was considered a facilitator by participants [Citation71]. Designing technologies to be low-cost [Citation26] and making them more affordable through discounts for certain groups were seen as enablers of IAT use [Citation70].
Study informants also emphasised the importance of cost as a barrier to discussing or prescribing IAT with clients: “it’s almost unethical to say ‘oh yes, this is really good for you’ but then it costs you $10,000 and it’s not under insurance so people cannot buy it; you’re not going to set someone up with something that you know is ultimately out of reach” – [PT1]; “we have to be good resource allocators with the funding available” – [SLP1]. Available funding is often constrained by the time required to acquire it: “even if they do qualify for funding it is a lengthy process to get that funding – it will take up to six months to a year or sometimes longer” - [OT1].
Costs of IATs were reportedly exacerbated when coverage was unclear, or not available through government or private insurance [Citation27,Citation72]. Examples of high-cost technologies include robots and exoskeletons, the latter costing between $30,000 and $100,000) [Citation55,Citation73]. Wearable low-vision assistive devices, in one study, were regarded by patients as prohibitively expensive to use [Citation64]. Transitioning robots quickly out of controlled labs into real-world settings was suggested to mitigate costs [Citation74].
Accessibility by tech type
In terms of accessibility, the included studies showed that, across all technology types, device cost was a barrier to their prescription and use [Citation43,Citation47,Citation48,Citation58,Citation62,Citation63]. This was more pronounced with situation-specific robots [Citation55,Citation73], and less so with wearable and handheld devices, which are more ubiquitous and accessible [Citation48,Citation49,Citation71]. Devices and interventions that leverage more readily available devices and lower-cost components may overcome barriers to accessibility [Citation45,Citation54].
Effectiveness
The following topics related to effectiveness were discussed within articles and by key informants: cost-effectiveness, how well IATs work for the health care system, and how well IATs work for older individuals. The theme of effectiveness is summarized in .
Table 4. Effectiveness summary.
Cost-effectiveness
Reports of the cost-effectiveness of IAT were mixed. Some studies found that IATs contribute to lower care costs [Citation73,Citation75], whereas other studies reported IATs as not cost-effective [Citation76]. Other studies brought up the consideration that IATs that delay or prevent 24-hour care or placement into institutional care should be considered cost-effective [Citation44,Citation46,Citation60,Citation77]. Ambiguous reports of cost-effectiveness data could be problematic for health systems with high evidence thresholds, as described in the following quote by PT3: “our organisation wants to see something that’s evidence-based. They are not interested in starting something that’s novel or undeveloped” - [PT3].
Effectiveness for health systems
System-level cost-considerations affect the prescription and use of IATs. Some studies reported that IAT use impacted health systems by: reducing hospitalisation [Citation78]; decreasing emergency department and rehabilitation visits [Citation78], reducing healthcare utilisation [Citation79], and contributing to shorter lengths of hospital stay [Citation78]. IATs were reported as beneficial to track important clinical outcomes including gait, balance and fall risk [Citation56], physical activity [Citation80], sleeping and eating [Citation81]. One review reported that, across five different studies, robotic devices in stroke rehabilitation should be favoured over conventional delivery [Citation75]. This same review reported cost and health benefits of the robotic intervention, for all but mild or moderate stroke patients [Citation75]. Data produced by some types of IATs were reported to quantify recovery [Citation82,Citation83] and contribute to earlier or preventive treatment through their ability to detect frailty or functional decline, or to manage symptom changes in chronic disease [Citation45,Citation46,Citation73,Citation78,Citation84].
Informants preferred technology with evidence of benefits, or which are accepted as best practice, as illustrated by PT1: “If there was a new device that was deemed to be best practice in stroke rehab, we would try to arrange education, if we can, implement it locally and regionally.” - [PT1]. One author reported a lack of evidence for the effectiveness and efficacy of mobile and connected health technologies for older adults aging in place [Citation68].
Effectiveness for older individuals
A variety of different types of smart assistive technologies were reported to improve older people’s ability to complete their activities of daily living, including a wrist robot [Citation85], a distributed system [Citation86], a mobility aid [Citation47], a social robot [Citation76], a virtual reality system [Citation43], and upper-limb rehabilitation robots [Citation87]. Other studies reported that IAT could improve medication adherence among older adults through custom reminders [Citation46] and could lead to more precise prescription by health care providers [Citation46,Citation56]. The timing with which IAT devices are introduced impacts their successful incorporation and use [Citation52,Citation87,Citation88].
Uncertain outcomes for older people were reported in some of the included studies. For example, a systematic review reported that, though robotic exoskeleton rehabilitation should be favored in the majority of stroke patients, conventional therapy is preferred for mild and moderate stroke patients [Citation75]. Other studies reported weak evidence for using IATs such as social robots for persons living with dementia in long-term care, and virtual reality technologies or older adults with neurological disorders [Citation43,Citation89]. In some studies, outcomes of IAT use were reportedly not more beneficial than usual forms of therapy, such as one study which measured the task-performance of people with cognitive impairment using virtual reality, a study of stroke patients using robot-assisted gait therapy, and another study where stroke survivors completed smartphone-based caregiver-mediated rehabilitation [Citation43,Citation90,Citation91]. Some included studies reported mixed findings on IAT use and safety. A road robot, a social alarm, an assistive robot, a wearable fall detector, a home integration system, a wearable virtual reality system and an ICT system were reported to contribute to greater feelings of safety [Citation43,Citation47,Citation60,Citation63,Citation92,Citation93], while one study that covered multiple types of IATs reported concerns for safety among participants due to privacy concerns and functionality limitations [Citation59].
Effectiveness by tech type
The reported effectiveness of IAT devices varied greatly. Studies reported that all device types, besides voice-activated systems and handheld devices, improved activities of daily living for those who used them [Citation43,Citation47,Citation85,Citation86]. Wearable devices were reported to improve safety for older individuals but were also cost prohibitive [Citation43]. Of all tech types, situation-specific robots were the most common type of tech within the theme of effectiveness, though that data was conflicting. Robotic-assisted rehabilitation was purported to have superior effectiveness in stroke rehabilitation for severely afflicted patients [Citation75], however some studies reported a weak evidence base for upper-limb rehabilitation robots [Citation89].
Usability
Studies found many factors when designing and developing IATs that can facilitate their prescription and use by older adults. These features include participatory approaches to IAT design; design features; individualised, adaptable IATs; and training/support for IAT use. The theme of usability is summarized in .
Table 5. Usability summary.
Participatory approaches to designing IAT
Many of the included studies referenced a participatory approach between engineers and manufacturers with end-users, older adults and caregivers as a way to improve implementation [Citation45,Citation46,Citation60,Citation61,Citation71,Citation72,Citation76,Citation85,Citation86,Citation89,Citation94–96]. For example, participatory approaches were noted in robot implementation [Citation85] and in designing a handheld sensor-enabled medication injector [Citation97]. Studies found participatory approaches should be iterative, with continued engagement throughout development, design and delivery of the IAT as was completed in the development of several self-management applications [Citation68,Citation80,Citation98,Citation99].
Design features
Some studies identified specific design approaches, which could contribute to more useful IATs. Universal design creates usable AT for all ages; values-based design (an extension of this approach) focuses on values identified by users [Citation45]. Universal design features would ensure the technology was ambient, discreet and unobtrusive, which were seen as important for IATs in the home of a patient [Citation45,Citation46,Citation81].
IAT that was not aesthetically pleasing [Citation63,Citation64,Citation69,Citation94,Citation97,Citation100,Citation101], bulky [Citation53,Citation55,Citation63,Citation102,Citation103], or cumbersome [Citation87] could increase resistance to use, potentially leading to abandonment. Simple, intuitive design and instruction was reported as enabling continued use of IAT devices [Citation53,Citation64,Citation69,Citation98]. For a sensor-enabled wearable fall detector, the small size and light weight of the device contributed to usability [Citation104]. A key informant confirmed size was a limiting factor to IAT use, in their experience: “the device was so cumbersome, they had no room to store it” - [PT1]. The findings of one study, though, suggested that aesthetic properties may be more important to younger populations than older adults [Citation74]. The desire for portable IAT was expressed by some studies in this review [Citation64,Citation67,Citation71,Citation97,Citation105]. For IAT to be portable for an older adult, it may need to be lightweight or require minimal strength to operate [Citation71]. Tensions exist between the desire for a lightweight, portable IAT and one with a long battery life, which may make the device heavier [Citation55]. One review found that portable low-vision aids may not be as cost-effective as their non-portable comparators, though they were easier to use [Citation67]. A short battery life [Citation72,Citation104,Citation106–108] and limited storage capacity [Citation72,Citation106] of an IAT were seen as barriers to use. One study found that older adults may be opposed to smaller devices, such as tablets [Citation105]. Regarding robotic IATs, older adults were reported to desire small, slightly anthropomorphised devices, that possess the ability to communicate similarly to human caregivers while maintaining safety standards [Citation79,Citation109]. However, robots that were large and too anthropomorphic were found to cause uneasiness [Citation79,Citation109].
Studies emphasised the desire for IAT with the capability to send patients reminders about the timing of medication delivery, diet choices, and their health goals, and able to function as a panic button to enhance safety [Citation72,Citation79,Citation97,Citation110,Citation111]. Individualised prompts, based on health history, to help manage chronic diseases were seen as desirable features [Citation46,Citation110]. The ability to cancel false alarms, which are common, was also identified as a desired feature [Citation46,Citation81,Citation107].
IAT that enabled communication with the health care system was seen as useful [Citation85]. Studies discussed the relevance of IAT that is interoperable with the wider healthcare system as a facilitator to use [Citation68]. The desire for interoperable IAT, though, was reported among concerns about privacy issues of having health information stored and shared confidentially [Citation45,Citation46,Citation60,Citation68,Citation110,Citation112].
Healthcare providers were reported as preferring IAT which was developed and reviewed by clinicians; and had the ability to: access patient data remotely; print graphs of patient data [Citation46,Citation51,Citation68,Citation95,Citation96,Citation113,Citation114]; and perform real-time assessments of gait-speed and balance [Citation56]. Patients, similarly, preferred IAT devices which allowed them to access their own health records [Citation95] and share their own health data [Citation110]
Easy to use IAT interfaces were an important consideration, in terms of graphics, color and text size [Citation47,Citation64,Citation81,Citation87,Citation93,Citation97,Citation98,Citation103,Citation104,Citation111]. There were examples among included studies where IAT was not usable by older people. For example: patients who had trouble using their hands could not use a touch screen [Citation47,Citation103]; voice-recognition was unable to understand accented speech or speech affected by disability [Citation83,Citation103,Citation112]; some IAT could not be used by people with visual impairments [Citation71,Citation115]; or hearing impairments [Citation115]. For people with rheumatic diseases, the ergonomics of IAT devices were considered essential due to limitations in hand mobility [Citation97].
Individualised, adjustable at
Many studies identified the necessity of an adjustable IAT that could be individualized to each patient through smartphones, app interfaces, provided information, behaviour and delivery, or motorized devices [Citation25,Citation49,Citation50,Citation53,Citation63,Citation67,Citation69,Citation72,Citation74,Citation79,Citation87,Citation93,Citation95,Citation96,Citation101,Citation104,Citation108,Citation111,Citation113,Citation116,Citation117]. This may be particularly relevant for older people with changing health statuses [Citation55,Citation118]. Some studies identified problems when an IAT was designed for a younger population, finding it did not adapt well for use by older adults [Citation45,Citation68]. Adaptability was also shown to be a priority for family caregivers, and helpful to physiotherapists in managing different capabilities of stroke patients [Citation76,Citation82].
Patient training & support
Older adults may require training to install and use IAT; one of the key informants felt that older persons would likely require greater training than younger persons because “the comfort level of the older population is very different” - [PT3], and they were seen as “not as tech savvy” – [SLP2]. Training can increase familiarity and alleviate uncertainty about IAT use [Citation70]. Many studies reported training older people on IAT as a facilitator to use [Citation25,Citation26,Citation67,Citation70,Citation81,Citation84,Citation102,Citation105,Citation106,Citation110,Citation119–121] though the number of studies where patients did not receive training on IAT [Citation25,Citation26,Citation42,Citation64,Citation122] suggests it may not be widespread or adequate. In one study, ease of installation and ease of training was noted as a facilitator to use [Citation69]. Some studies found that information overload during IAT device selection and training may be a barrier to the acquisition and acceptance of smart devices [Citation52,Citation62]. To this end, it was reported that concise language [Citation104], without medical jargon, was desired or beneficial to patients using IAT [Citation98]. Providing technical support and training to caregivers may also aid in the uptake and continued use of IAT [Citation25,Citation123]. Additionally, support from family and caregivers was reported as an important component of patient confidence in using IAT [Citation96]. Easy-to-use technologies that would not require training or would be simple enough for those with less technology experience could readily adopt them, were also discussed in some studies [Citation43,Citation124].
Role-playing, strategising how to fit IAT into the daily environment, group workshops about IAT use, and practising task success were mentioned as positive, even enjoyable, components of in-person training [Citation47,Citation54,Citation70,Citation125]. Take-home resources including leaflets, detailed written instructions; a checklist outlining device features; and accessible tips in case someone forgets how to operate the IAT, facilitated older adults’ training [Citation116,Citation126].
Ongoing technical support and managing patients’ expectations about the duration of support were important features of training people for IAT use [Citation81]. Participants in one study found that support following the cessation of the trial (while participants transitioned to independent use) would have been beneficial [Citation108]. Key informants echoed the importance of training and support for older people as a facilitator for their older patients to use IAT in the following quotes from SLP2: “there are some companies that offer technologies with all of the necessary training, and then they will continue and support it, so for me I look for that for my elderly clients” – [SLP2] “I don’t tend to prescribe devices that come from agencies that don’t have this support in place” – [SLP2]. OT1 described the importance of clients having an opportunity for a hands-on trial of the equipment: “What happens is they get the trial with whatever the equipment is, and they realise how great it is – they feel safer, they just feel better, and then they end up buying the equipment. Otherwise, they chase me out of the house saying get out of here – I’m not paying money for this!” - [OT1]. Informants also emphasised the importance of having follow-up or resources available if problems are encountered later on: “People get training initially but then they forget, because if you don’t use it all the time, when you come to use it again then you may forget how to use it. So that ongoing follow up or opportunity to go back and remember how to use things is important.” - [OT2].
Usability, ease of use, and reliability were essential to the adoption of IAT devices [Citation61,Citation64,Citation67–69,Citation79,Citation108,Citation127], and were also emphasised by the key informants. For example, OT1 talked about the time required to learn the technology and to teach the client to use it: “Ease of use is important, you don’t want it to be more work” - [OT1]. OT2 discussed how the complexity of the technology could be a challenge for implementation: “I’m always in awe at what engineers and computer scientists and such can do but if devices are too complex then the client may not use them to their full function…There’s a lot of stuff around usability that determines whether the technology will be used or not, reliability is one of them; is it easy to use, is it easy to learn how to use, are there a few steps or many?” – [OT2]. Complex features of a technology may be an aid to its adaptability and versatility, but might also be a barrier to its use in practice.
For some people, certain limitations (visual; cognitive; pain; comorbidities; injuries; fine motor control; hearing; anxiety) made IAT use difficult or impossible [Citation4,Citation63,Citation87,Citation96,Citation103,Citation119,Citation121]. In one study, worsening limitations made older people more willing to try a range of IAT, which may present an opportunity for IAT uptake [Citation128].
Usability by tech type
Device usability was a facilitator for the majority of device types. The ease of use of device interfaces was described as a facilitator to use by all five included technology types: situation specific robots [Citation87,Citation93], distributed systems [Citation81], wearable devices [Citation104,Citation111], handheld devices [Citation64,Citation97,Citation98,Citation103], and mobility aids [Citation47]. The benefits of a participatory design process on implementing distributed systems [Citation46,Citation86], handhelds [Citation94], and wearables were marked [Citation72]; support for a participatory design was most pronounced within the category of situation-specific robots [Citation71,Citation85,Citation89,Citation95]. Aesthetics and bulkiness of devices were considerations for handheld [Citation94,Citation102] and wearable devices [Citation55,Citation63], and unobtrusiveness was considered a facilitator to distributed systems [Citation46]. The adjustability of prescribed devices was identified as a facilitator for use of situation-specific robots [Citation101,Citation117], and for wearable [Citation72] and handheld devices [Citation53]. Training of older adults was important for handheld devices [Citation102], wearables [Citation106], distributed systems [Citation81], and situation-specific robots [Citation121].
Staff considerations
Staff-related considerations included their role in prescribing IAT, training requirements, and staff knowledge and awareness of IAT. The theme of staff considerations is summarized in .
Table 6. Staff considerations.
Role in prescription
Rehabilitation professionals mediate the relationship between older adults and their use of IAT, as they often prescribe or recommend IAT. Clinician recommendations can initiate and reassure patients about IAT use and reduce abandonment of IAT [Citation84,Citation124]. One study found that a provider’s attitude and perception of IAT can mediate prescription and use, where, perceiving a robotic IAT device unfavourably, caused some providers to withdraw from using it [Citation115]. Follow-up with older patients about IAT use increases their adherence, with abandonment dropping from 37% to 10% [Citation59]. Some providers may lack experience in providing rehabilitation through smartphone and technology-enabled medias [Citation49,Citation96]. One study found, concerning a social and exercise robot, that although providers were eager to incorporate robotic IATs into practice, there were still concerns held by the general population regarding safety, the replacement of human care providers by robots, and an overall prevailing fear of robotic devices [Citation66]. The use of ICT-based IAT may also increase provider burden due to increased demand for follow-up [Citation49,Citation51], and large amounts of data produced by such technologies [Citation68]. However, care robot IATs were reported to have the potential to reduce care provider burden, by providing opportunities to outsource some tasks and responsibilities, such as providing exercise instructions to patients [Citation115].
Staff training
One of the informants felt that the amount of training and support available could vary significantly depending on the size of the centre: “We are very blessed here having a ton of support in the background but I can imagine that if you were at a smaller centre that would be a huge problem.” - [PT3]. Key informant OT1 reinforced the importance of staff training on the technology: “We would need training on it so we become experts on it and can teach our clients how to use it best” – [OT1].
Educating and training personnel was identified as critical to ensuring best outcomes for older adults, though training programs may not sufficiently incorporate the requirements of older adults [Citation26]. Despite their proximity to and influence on older people, some studies outlined challenges associated with training rehabilitation professionals on IAT. For example, studies found that it is challenging for therapists to allocate time to research and familiarise themselves with current IAT [Citation66,Citation115], which was echoed by our study informants: “we just don’t have the time, not that everything needs to be spoon fed, but the reality is that we don’t have time to just sit and look at articles, it just doesn’t happen” – [PT2]; “I mean the time it takes to just try and to keep updated on this stuff, there’s such a demand to see more people, to get them in quicker, to do things more efficiently” - [OT1].
Staff knowledge and awareness
In some studies, therapists felt they had limited awareness of IAT products to recommend, while other studies mentioned a shortage of staff knowledgeable in set-up and training of older people [Citation4,Citation27,Citation61]. Key informants indicated that previous experience and associated comfort levels with IATs had a significant effect on the level of acceptance and training required: “some therapists are a lot more comfortable with technology and others are not, and it goes with age usually, some of the older therapists are like ‘I’m not touching that!’ which I think is quite common” - [PT2]. The lack of legal frameworks for the use of robotic healthcare IAT, and the speed at which these frameworks can be developed in comparison to the development of IATs, has also raised concerns [Citation109].
Staff considerations by tech type
There were several staff considerations for the prescription of different IAT types. Handheld devices were found to have barriers for staff involved in prescribing IAT devices, as they may lack experience in using handheld devices [Citation49,Citation96], and the increased demand for follow-up through the use of such devices may increase care provider burden [Citation49,Citation51]. Similarly, rehabilitation professionals had difficulty researching situation-specific robots [Citation66,Citation115], and lacked awareness of situation-specific robots and mobility aids [Citation61].
Patient-centred considerations
This theme includes results related to patients or users of IATS, such as their home environment, their motivation, beliefs and attitudes, and the stigma associated with IAT use as an older person. The theme of patient-centred considerations is summarized in .
Table 7. Patient-centered considerations summary.
Patient’s environment
Many studies discussed how aspects of the patient’s environment can prevent them from using IAT. In some studies, the patient’s home environment would require modifications or renovations to integrate IAT [Citation47,Citation113]. One study recommended developing and tailoring IAT devices to the environment of the users [Citation25]. Examples of specific aspects of homes which impede IAT use include: inability of a motorised IAT to navigate different terrains such as carpet or stairs [Citation74] and weak or no wireless internet and Bluetooth [Citation63,Citation104,Citation107,Citation108,Citation122]. Key informants’ shared concern about lack of wireless internet as potentially problematic for their patients: “how many of the clients will actually have internet at home?” - [PT2]. “It’s always tricky because some of these technologies are connected to Wi-Fi but sometimes it’s hard to have those things in place, these technologies can be great but not everyone has access to that” - [OT1].
Two studies, one investigating patients who had experienced spinal cord injuries and another reviewing the use of smart homes for older adults and people with disabilities, found that distributed systems provide independence [Citation122] and improved quality of life through their use [Citation46]. Another study found that interactive robot pets may bypass the environmental barriers experienced with owning conventional pets [Citation127].
Motivation
Studies discussed patients’ motivations for using IAT as well as motivation as a by-product of IAT use [Citation50,Citation79,Citation123]. Studies discussed the desire for increased or preserved independence as a source of motivation for IAT use [Citation27,Citation71,Citation72,Citation122,Citation128]. Other studies mentioned IAT use as motivating to complete activities of daily living [Citation71,Citation106] and to age in place in one’s own home [Citation76,Citation129]. Feedback provided through app-based IAT was seen as a way to improve motivation for continued use [Citation98,Citation111].
Some studies mentioned family caregivers as influential in a patient’s motivation. Patients are motivated to use IAT to improve their caregivers’ experience. For example, in some studies social and assistive robots reduced conflict and burden [Citation76,Citation93], while distributed systems enhanced caregivers’ quality of sleep [Citation81] and reduced burden [Citation47,Citation51,Citation65]. Similarly, a multi-functional system was reported to reduce caregiver burden and improve perceptions of safety and trust [Citation86]. Study subjects were motivated to use IAT to offer peace of mind to caregivers not living with the patient, and to demonstrate to family that they were progressing in their rehabilitation [Citation85,Citation123].
Family or friend caregivers can act as a source of motivation for IAT use in rehabilitation by supporting older adults to adopt or operate the IAT [Citation59,Citation62,Citation65,Citation83,Citation88]. IAT use was also reported as beneficial to caregivers by reducing injuries and burden incurred in the process of caring for IAT users [Citation47]. Key informants we interviewed described care partners as a resource to motivate and troubleshoot for older adult clients. For example, OT2 said: “you have to think about who can help the person problem-solve or help them learn how to do it and set it up if they need assistance” - [OT2].
Some study subjects were motivated to use IAT for social purposes, to connect with friends and family, to reduce loneliness, or as a means to engage in leisure activities [Citation108,Citation129]. Some studies discussed how rehabilitation involving exercise games helped to motivate older adults to exercise, as they enjoyed competing with friends and family [Citation59,Citation116]. Other studies showed that human-like robots or robotic animals could provide comfort, entertainment or relieve agitation for some older adults [Citation43,Citation46,Citation76,Citation93].
Included studies outlined the ways that IAT used in rehabilitation can be motivating for older adults to develop abilities, change behaviour, complete more rehabilitation activities, join new programs or stimulate learning to use new types of IAT [Citation89,Citation102,Citation110]. Stroke patients in particular, may be motivated by IAT use in rehabilitation to regain previous capacities [Citation85]. One study indicated that there is a need for frameworks to evaluate IAT devices, particularly ones which account for the intended users [Citation130].
Beliefs and attitudes
Some papers discussed how different beliefs or attitudes of patients mediated their IAT use or non-use. For older adults in many of the included studies, IAT was intimidating or fear-inducing to try [Citation47,Citation54,Citation62,Citation79,Citation88,Citation92,Citation96,Citation105,Citation115,Citation117,Citation126]. For some older people, IAT use can cause stress [Citation26,Citation100], or anxiety [Citation123]. For example, in some studies, older adults were worried about breaking something by clicking around on a tablet [Citation62,Citation100,Citation105]. These beliefs are echoed in other studies where patients believed an IAT was too difficult to use or learn [Citation52,Citation81,Citation123] or they lacked the confidence to try to learn [Citation59]. Other studies showed that some older adults believed IAT was for young people [Citation53,Citation62,Citation70], that they were unable to manage IAT [Citation117] or that it would be distracting, or burdensome to have to manage IAT [Citation57,Citation112]. Some included studies reported, older adults minimised their need for rehabilitative devices [Citation25,Citation45,Citation63,Citation93], or outright had little interest in using IAT devices [Citation25].
As might be expected, more experience using technology before the onset of conditions requiring IAT use [Citation53,Citation62,Citation65,Citation105,Citation119], was reported as a facilitator to using IAT for rehabilitation [Citation61,Citation85]. Those with lower digital literacy were more likely to be sceptical towards technology, influencing their AT use [Citation27,Citation100]. Robotic IAT generated scepticism as older adults felt their skills and social lives might deteriorate [Citation69,Citation77].
Key informants we interviewed mentioned the importance of reassurance and persuasion to influence older patients’ beliefs about IATs: “There’s certainly a lot to do though with educating this population to help them understand that it’s not a bigger headache than it is worth”- [SLP2].
Some studies reported that older adults and researchers felt sceptical about the surveillance and privacy aspect of IAT [Citation57,Citation61,Citation64,Citation65,Citation68,Citation72,Citation79,Citation92,Citation97,Citation109,Citation131], for example, the sensitivity of sharing personal health data [Citation59]. One study reported that older people were willing to look past the sensitivity of sharing health information if it meant they could communicate with their health care providers outside appointments [Citation84]. Other studies found that caregivers and people with dementia were not concerned about privacy or surveillance by IAT [Citation65,Citation70,Citation81]. In fact, one study found that, amongst caregivers of people with dementia, safety was more important than the privacy or autonomy of the person they care for, and that safety IATs, such as trackers, were most appreciated [Citation65].
Older adults’ beliefs about IAT were influenced by family caregivers. In three studies, older adults reported they did not want IAT use to replace the help they received from their family [Citation76,Citation93,Citation123]. Some studies found that caregivers may fear that the use of assistive robots could contribute to reduced social connnection for older adults [Citation79,Citation93], or replace the personal component of caring for someone with dementia [Citation65].
Stigma
Included studies listed social stigma surrounding the visibility of IAT as a deterrent to IAT use [Citation27,Citation53,Citation63,Citation76,Citation79,Citation87,Citation93,Citation127]. Using IAT publicly made older adults feel self-conscious [Citation112], led to negative attention, and unwanted pity [Citation77]. Smartphone-connected hearing aids and robots are examples of stigmatised IAT reported in included studies [Citation53,Citation77]. Ageist ideas about older adults were also mentioned; some study participants felt that IAT use would signal they were old and frail, while others reported self-stigmatising ideas (e.g., “I’m too old for that”) as a deterrent to IAT use [Citation58,Citation100]. One study mentioned that media portrayals of older people and technology, as well as advocacy campaigns, could increase public knowledge about disability, and reduce the stigma around IAT use as a signal of dependence [Citation81]. Additionally, for home-based cognitively assistive robots, interactions with people already using similar devices promoted interest and a desire to use those IAT devices [Citation79]. Smartphone-mediated hearing devices may also provide a means to reduce the stigma of IAT use due to the ubiquity of smartphones [Citation53].
Patient-centred considerations by tech type
Use of all tech types was affected by factors relating to the patients who used IAT devices. Both mobility aids [Citation47] and situation-specific robots [Citation113] were negatively impacted by the physical environment in which they were used, and wearables [Citation63,Citation104], handhelds [Citation108], and distributed systems [Citation122] were impacted by wireless infrastructure. Conversely, one situation-specific robot, a robotic pet, was found to be better suited to patient environments than its living analogue [Citation127]. Some IAT types, such as handheld devices [Citation123], aided in motivating older adults, however, the visibility of some handheld-mediated devices also stigmatised older adults who used them [Citation53]. The use of handheld [Citation54,Citation62,Citation88,Citation96,Citation105,Citation126] and situation-specific [Citation79,Citation115,Citation117] robotic IAT devices was described as inducing fear in older adults, due to concerns of breaking the device [Citation62] and the potential of device use increasing social isolation [Citation77].
Discussion
This paper sought to identify facilitators and barriers influencing the prescription, acquisition, implementation, and adoption of smart assistive technologies among older adults for rehabilitation and found that IAT use was mediated by external forces such as cost, accessibility and usability of IAT, as well as intrinsic factors such as motivation, beliefs, attitudes, and stigma. This review found many studies that made recommendations to future technology developers, including the importance of individualised, adjustable technology which fits a patient’s home environment. To take advantage of the important role rehabilitation professionals play in influencing IAT use by older adults, they should be supported to understand available, effective IATs to recommend to their patients. Additionally, older people require support from rehabilitation professionals and/or through IAT-producing companies to continue to use these technologies on their own.
The Unified Theory of Acceptance and Use of Technology (UTAUT) is a synthesis of leading technology acceptance theory, that identifies factors that facilitate or constrain someone’s intention and use of technology in workplace contexts and has been widely applied and replicated [Citation132]. The UTAUT2 provides a similar framework for technology acceptance in a consumer setting and can be used to situate the findings of this review. The UTAUT2 proposes seven constructs that weigh on the behavioural intention to use a technology: performance expectancy, effort expectancy, social influence, facilitating conditions, hedonic motivation (fun), price value, and habit [Citation132]. These constructs are moderated by age, gender and experience [Citation132].
Our theme about the patient-centredness of IATs aligned with the performance expectancy construct. Older adults are motivated by their desire for independence [Citation71,Citation72,Citation100,Citation122,Citation128], thus, IAT should be presented as a tool that helps to preserve this. Studies referenced many domains (physical, psychological and health system) where IAT use can be impactful, countering the idea some older people had that IAT use signals dependence. Rehabilitation professionals we interviewed emphasised the role they play in motivating older people to consider IATs. By persuading them that the technology will provide benefits, clinicians increase older people’s performance expectancy, assuring them that using smart technology for rehabilitation will not be a “bigger headache than it’s worth” – [SLP2].
The UTAUT2 proposes that intention to use technology is driven by experience, or the perception about the previous passage of time. This aligns with our findings about patient beliefs and attitudes suggesting that older adults with previous experience using technology were more likely to engage in IAT use. Our findings show that many studies recognize the benefits to training older people on IAT use [Citation25,Citation67,Citation70,Citation83,Citation84,Citation102,Citation105,Citation106,Citation119–121], but some studies [Citation26,Citation42,Citation122] reported that older adults did not receive training on IAT. We recommend creating opportunities for older adults to gain digital literacy skills (build experience using technology) to enable IAT adoption.
In the eyes of technology developers, older adults represent an untapped market who are expected to spend $645 billion dollars by 2050 on technology [Citation133]. It may be important for device companies to know that support and training play a role in clinicians’ decisions about which IATs to prescribe to which older people. To better market IATs to older people, ongoing training, support, and troubleshooting could be important considerations.
The UTAUT2 proposes that fun, pleasure or enjoyment mediate consumers’ use of IAT, which corresponded with our results about patient beliefs, attitudes and stigma. These themes contained information about unenjoyable aspects of IAT use, specifically, that it could be fear-inducing, difficult or time consuming to learn [Citation47,Citation54,Citation62,Citation79,Citation81,Citation88,Citation92,Citation93,Citation96,Citation105,Citation115,Citation117,Citation126]. Ageist attitudes that IAT use may signal dependence or frailty, or internalised ideas about technology being for young people were found in this review [Citation58,Citation100]. Stigma and lack of self-efficacy around technology use may contribute to a lack of hedonic motivation for older people, creating barriers to IAT use. Awareness to increase public knowledge about disability, and to reduce the stigma around IAT use as a signal of dependence, would contribute to increased IAT use [Citation81].
Our findings around the patients’ environment corresponded closely with UTAUT2’s facilitating conditions, literally, the physical support to use IAT. These findings covered how physical aspects of a patient’s home such as narrow passageways, stairs, or a weak internet signal [Citation74,Citation122] may impede IAT use. As older adults overwhelmingly prefer to age in place in their own homes [Citation134] and the alternative (institutional care) is costly to publicly funded health care systems [Citation135], supporting their IAT-enabled independence through tax credits or home modification grants could help governments avoid costs.
Our theme containing results about staff training corresponds with the social influence construct of the UTAUT2. Rehabilitation professionals can represent what the UTAUT2 calls, an ‘important other’ and can play a critical role in influencing older adults’ technology use. To play this role, rehabilitation professionals need knowledge regarding current best practices and the ability to translate them into their own clinical practice. Multi-component knowledge translation interventions have been used to support this, wherein self-perceived knowledge and self-perceived practice behaviours of rehabilitation professionals are observed [Citation136]. This knowledge will become even more important as assistive technology is increasingly developed to support older adults.
The findings from the clinicians emphasise the role that care partners have as a social influence in older people’s use of smart assistive technology. It is evident (across themes of patient attitudes and beliefs, motivation, outcomes, usability and patient training) that family caregivers may also represent an important other influencing older adults’ technology use. Family-centred AT decision-making is commonplace when providing AT to children [Citation22] but our research suggests this practise is important to facilitate older adults’ adoption of IAT as well. Older people may be motivated by family caregivers to use IAT for rehabilitation and to engage with others socially. Our findings suggest that IAT use is perceived by some older people as a form of reciprocity to family caregivers: a way to enable independence, reduce burden of family caregivers, and demonstrate commitment to their rehabilitation [Citation47,Citation65,Citation76,Citation83,Citation85].
Our theme around usability aligns with the idea of effort expectancy (or ease of use): including patient training; design considerations, and individualised/adjustable technology. Results from these sections of the review emphasise the importance of participatory approaches to developing technologies that are easy to use and easy to change, as the functional ability of older patients is variable [Citation45,Citation46,Citation60,Citation72,Citation76,Citation85,Citation124]. Our findings emphasise that older adults may require in-person support and/or practice to learn technology before using it on their own [Citation70,Citation83,Citation84,Citation106,Citation110], and those older people who have more practice or experience using technology (for example, through previous employment) may be more comfortable and more likely to use IATs for rehabilitation activities [Citation85,Citation108]. Key informants emphasised the role that usability and training have played in their experience working with older people.
The UTAUT2 discusses the trade-off between monetary cost and quality of products or services as price value, which overlaps with our findings about the accessibility of IAT. The UTAUT2 seems to presume access to technology, which our review showed was complex. Access to technology is complicated by awareness of what IAT are available, what government supports are available for IAT, and understanding how to select suitable IAT from many commercial options [Citation26,Citation27,Citation53,Citation54]. Furthermore, costs of IAT can be prohibitive, aligning with previous author’s findings which cite cost as the reason for nearly 20% of unmet needs in disability supports for older Canadians [Citation5,Citation28]. Our findings suggest a central access point for IAT purchasing, which could include clear information about which IAT may be reimbursable, and for whom, could increase IAT use [Citation27,Citation72]. Additionally, health systems leasing or renting IATs could make their use more affordable [Citation55].
Our categorisation of the findings did not overlap with UTAUT2 constructs entirely. Gender did not play prominently in our theming of results, which the UTAUT2 shows as moderating the relationship between consumers and their intention to use AT. Our results did not demonstrate culture or ethnicity as a moderating factor in older people’s IAT use for rehabilitation as [Citation137] have suggested. Future research is warranted in this area as the digital divide may be more pronounced in certain groups, precluding access to smart technology for use in rehabilitation.
Our results may be of specific relevance in the context of the COVID-19 pandemic that has spread rapidly through long-term care homes, killing thousands of older people [Citation138]. As older people and their families navigate care decisions, they may pay special attention to delay or avoid placement into institutional care, enhancing the relevance of recommendations to support IAT adoption. IAT use can contribute to reduced pain, increased cognition, and better participation in rehabilitation activities [Citation100,Citation114]. Gamifying rehabilitation could increase enjoyment and preserve functional mobility in older people who may be encouraged by their governments to stay at home to minimise COVID-19 exposure. In Canada, telerehabilitation options are being explored to support people in their rehabilitation from COVID-19 [Citation139].
Our research showed that patients were motivated to use IAT to connect with friends and family, to reduce loneliness, or to participate in social settings [Citation26,Citation70,Citation74,Citation102]. Stay-at-home orders designed to minimise COVID-19 exposure could represent an opportunity to engage in IAT use for rehabilitation purposes, and reduce the social isolation associated with limited in-person connection [Citation140].
Limitations
Although our search strategy was focused on returning articles about older people, this review did not explicitly seek to capture information regarding the impact of gender or ethnicty on the prescription of IAT devices. Gender, as well as age and experience, are recognized as key constructs in the acceptance of technology and play a pivotal role in modifying a patient’s use of an IAT device [Citation132]. Future research should investigate the intersection of age, ethnicity, and gender on the prescription, acquisition, implementation, and adoption of intelligent assistive technologies in older adults undergoing rehabilitation.
This review did not place any geographic restrictions on the search strategy. It is important to acknowledge that the countries covered operate with very different health care systems and correspondingly different frameworks, policies and regulations regarding developing, assessing, implementing and reimbursing IAT, which could limit the applicability of the findings. In low and middle-income countries, IAT prescription may be crowded out by other health-priorities. Additionally, this review did not attempt to assess or evaluate the quality of the evidence include within the review. As such, results should be considered emblematic of the state of research conducted regarding the use of IAT devices with older adults in rehabilitation. This should be especially noted for the effectiveness results of the review, where no aggregation was conducted to identify whether individual IAT types were statistically effective.
Conclusions
This study outlines the breadth and depth of the literature surrounding IAT prescription, acquisition, implementation, and adoption for older people undergoing rehabilitation, detailing how cost, access, home environment, attitude, stigma, technology development, adaptability of technology, motivation, training (staff and patient) and usability interact to influence IAT adoption. This scoping review is strengthened by consultation with clinical rehabilitation providers, who provided context on how facilitators and barriers appear in and resonate with their practice. Any strategies to improve upon barriers to prescribing smart technologies for older people should leverage the expertise of rehabilitation professionals operating at the interface between older people; their health/mobility; their families; and technology-based solutions. We offer practical insight on the ways rehabilitation practitioners and health systems can enable older adults’ IAT use, to promote their good health and independent living for as long as possible.
Acknowledgements
We are grateful to University of Waterloo Health Sciences Librarian Jackie Stapleton for advice on our search strategy. Larissa Nagora, Kassandra Lemmon and Melissa Koch were of great assistance during data analysis.
Disclosure statement
The authors report there are no competing interests to declare.
Additional information
Funding
References
- United Nations. Ageing and disability [internet]. Department of Economic and Social Affairs - Disability. [cited 2022 Dec 6]. Available from: https://www.un.org/development/desa/disabilities/disability-and-ageing.html.
- Cieza A, Causey K, Kamenov K, et al. Global estimates of the need for rehabilitation based on the global burden of disease study 2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2021;396(10267):2006–2017 [cited 2022 Dec 6]; Available from: http://www.thelancet.com/article/S0140673620323400/fulltext. doi:10.1016/S0140-6736(20)32340-0.
- Sheehy L, Taillon-Hobson A, Sveistrup H, et al. Home-based virtual reality training after discharge from hospital-based stroke rehabilitation: a parallel randomized feasibility trial. Trials [Internet]. 2019;20(1):333. [cited 2022 Dec 6]; Available from: https://pubmed.ncbi.nlm.nih.gov/31174579/. doi:10.1186/s13063-019-3438-9.
- Krishnaswami A, Beavers C, Dorsch MP, et al. Gerotechnology for older adults with cardiovascular diseases: JACC state-of-the-art review. J Am Coll Cardiol. 2020;76(22):2650–2670. doi:10.1016/j.jacc.2020.09.606.
- Arim R. Canadian survey on disability, 2012: a profile of persons with disabilities among Canadians aged 15 years or older. [Internet]. Statistics Canada. 2015. Available from: https://www150.statcan.gc.ca/n1/en/pub/89-654-x/89-654-x2015001-eng.pdf?st=PZ3et3Qxhttps://www150.statcan.gc.ca/n1/en/pub/89-654-x/89-654-x2015001-eng.pdf?st=PZ3et3Qx.
- Assistive Devices and Technologies. 2021 [Internet]. World Health Organization. 2021. Available from: https://www.who.int/disabilities/technology/en/
- Agree E. The potential for technology to enhance independence for those aging with a disability. Disabil Health J. 2014;7(1 Suppl): s 33–9. doi:10.1016/j.dhjo.2013.09.004.
- Chabot M, Delaware L, McCarley S, et al. Living in place: the impact of smart technology. Curr Geri Rep. 2019;8(3):232–238. [cited 2023 Apr 18]; Available from: https://link.springer.com/article/10<?sch-permit JATS-0034-007?>.1007/s13670-019-00296-4. doi:10.1007/s13670-019-00296-4.
- Gore PG, Kingston A, Johnson GR, et al. New horizons in the compression of functional decline. Age Ageing. 2018;47(6):764–768. [cited 2023 Apr 18]. Available from: https://academic.oup.com/ageing/article/47/6/764/5079486.
- Sehgal M, Jacobs J, Biggs WS. Mobility assistive device use in older adults. Am Fam Physician. 2021;103(12):737–744. [cited 2023 Feb 27]. Available from: https://pubmed.ncbi.nlm.nih.gov/34128609/.
- Molteni F, Gasperini G, Cannaviello G, et al. Exoskeleton and End-Effector robots for upper and lower limbs rehabilitation: narrative review. PM R. 2018;10(9 Suppl 2):S174–S188. [cited 2023 Feb 27]. Available from: https://pubmed.ncbi.nlm.nih.gov/30269804/ doi:10.1016/j.pmrj.2018.06.005.
- World report on disability. [Internet]. Geneva; 2011 [cited 2022 Dec 6]. Available from: https://www.who.int/publications/i/item/9789241564182.
- Yusif S, Soar J, Hafeez-Baig A. Older people, assistive technologies, and the barriers to adoption: a systematic review. Int J Med Inform. 2016;94:112–116. doi:10.1016/j.ijmedinf.2016.07.004.
- Adolfsson P, Lindstedt H, Pettersson I, et al. Perception of the influence of environmental factors in the use of electronic planning devices in adults with cognitive disabilities. Disabil Rehabil Assist Technol. 2016;11(6)::493–500. [cited 2023 Apr 18] Available from: https://pubmed.ncbi.nlm.nih.gov/25434402/.
- Steel EJ, Layton NA, Foster MM, et al. Challenges of user-centred assistive technology provision in Australia: shopping without a prescription. Disabil Rehabil Assist Technol. 2016;11(3):235–240. doi:10.3109/17483107.2014.941953.[Internet]. [cited 2023 Feb 27]; Available from: https://www.tandfonline.com/doi/abs/10<?sch-permit JATS-0034-007?>.3109/17483107.2014.941953.
- Steel D, Gray M. Baby boomers’ use and perception of recommended assistive technology: a systematic review. Disabil Rehabil Assist Technol. 2009;4(3):129–136. doi:10.1080/17483100902767175.
- Ienca M, Fabrice J, Elger B, et al. Intelligent assistive technology for Alzheimer’s disease and other dementias: a systematic review. J Alzheimers Dis. 2017;56(4):1301–1340. doi:10.3233/JAD-161037.
- Vollmer DD, Ory M. Emerging issues of intelligent assistive technology use among people with dementia and their caregivers: a U.S. Perspective. Front Public Health. 2020;8:191. doi:10.3389/fpubh.2020.00191.
- ATscale. The Case for Investing in Assistive Technology [Internet]. 2020 [cited 2022 Dec 6]. Available from: https://static1.squarespace.com/static/5b3f6ff1710699a7ebb64495/t/5fbf5c44eaf37e3b64932e6c/1606376534765/Case_for_Investing_in_AT_a11y.pdf.
- Maresova P, Režný L, Bauer P, et al. An effectiveness and cost-estimation model for deploying assistive technology solutions in elderly care. Int J Healthcare Manag. 2022; 1–16 [cited 2023 Feb 20]; Available from : [Internet]. https://www.tandfonline.com/doi/abs/10<?sch-permit JATS-0034-007?>.1080/20479700.2022.2134635. doi:10.1080/20479700.2022.2134635.
- Brandt Å, Hansen E, Christensen J. The effects of assistive technology service delivery processes and factors associated with positive outcomes–a systematic review. Disabil Rehabil Assist Technol. 2020;15(5):590–603. doi:10.1080/17483107.2019.1682067.
- Van Niekerk K, Dada S, Tönsing K, et al. Factors perceived by rehabilitation professionals to influence the provision of assistive technology to children: a systematic review. Phys Occup Ther Pediatr. 2018;38(2):168–189. doi:10.1080/01942638.2017.1337661.
- World Health Organization. The United Nations Children’s Fund (UNICEF). Global report on assistive technology [Internet]. Geneva; 2022 [cited 2023 May 7]. Available from: https://www.unicef.org/media/120836/file/%20Global%20Report%20on%20Assistive%20Technology%20.pdf.
- Technavio. Assistive Technology Market Size, Share & Trends to 2027 [Internet]. 2022; [cited 2023 May 7]. Available from: https://www.technavio.com/report/assistive-technology-market-report-analysis?utm_source=prnewswire&utm_medium=pressrelease&utm_campaign=Auto-V7_VSG_wk26_2022_004_report&utm_content=IRTNTR40244
- Okonji PE, Ogwezzy DC. Awareness and barriers to adoption of assistive technologies among visually impaired people in Nigeria. Assist Technol. 2019;31(4):209–219. doi:10.1080/10400435.2017.1421594.
- Garçon L, Khasnabis C, Walker L, et al. Medical and assistive health technology: meeting the needs of aging populations. Gerontologist. 2016;56 Suppl 2: S293–S302. doi:10.1093/geront/gnw005.
- Tangcharoensathien V, Witthayapipopsakul W, Viriyathorn S, et al. Improving access to assistive technologies: challenges and solutions in low- and Middle-income countries. WHO South East Asia J Public Health. 2018;7(2):84–89. doi:10.4103/2224-3151.239419.
- Mattison CA, Wilson MG, Wang RH, et al. Enhancing equitable access to assistive technologies in Canada: insights from citizens and stakeholders. Can J Aging. 2020;39(1):69–88. doi:10.1017/S0714980819000187.
- Löbe C, AboJabel H. Empowering people with dementia via using intelligent assistive technology: a scoping review. Arch Gerontol Geriatr. 2022;101:104699. doi:10.1016/j.archger.2022.104699.
- Ienca M, Wangmo T, Jotterand F, et al. Ethical design of intelligent assistive technologies for dementia: a descriptive review. Sci Eng Ethics. 2018;24(4):1035–1055. [cited 2023 Apr 10]. Available from: https://link.springer.com/article/10<?sch-permit JATS-0034-007?>.1007/s11948-017-9976-1.
- Dada S, van der Walt C, May AA, et al. Intelligent assistive technology devices for persons with dementia: a scoping review. Assist Technol. 2022; 1–14. [cited 2023 Apr 10]. Available from: doi:10.1080/10400435.2021.1992540.[Internet]. https://www.tandfonline.com/doi/abs/10<?sch-permit JATS-0034-007?>.1080/10400435.2021.1992540.
- Chen B, Ma H, Qin LY, et al. Recent developments and challenges of lower extremity exoskeletons. J Orthop Translat. 2016;5:26–37. doi:10.1016/j.jot.2015.09.007.
- Kalita B, Narayan J, Dwivedy SK. Development of active lower limb robotic-based orthosis and exoskeleton devices: a systematic review. Int J of Soc Robotics. 2021;13(4):775–793. [cited 2023 Apr 10Available fromhttps://link.springer.com/article/10<?sch-permit JATS-0034-007?>.1007/s12369-020-00662-9. doi:10.1007/s12369-020-00662-9.
- Chen B, Zi B, Qin L, et al. State-of-the-art research in robotic hip exoskeletons: a general review. J Orthop Translat. 2020;20:4–13. doi:10.1016/j.jot.2019.09.006.
- Colquhoun HL, Jesus TS, O’Brien KK, et al. Study protocol for a scoping review on rehabilitation scoping reviews. Clin Rehabil. 2017;31(9):1249–1256. doi:10.1177/0269215516688514.
- Levac D, Colquhoun H, O’Brien K. Scoping studies: advancing the methodology. Implement Sci. 2010;5:1–9.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi:10.1080/1364557032000119616.
- World Health Organization. Rehabilitation [Internet]. 2023; [cited 2023 Apr 11]. Available from: https://www.who.int/news-room/fact-sheets/detail/rehabilitation.
- The UN Refugee Agency. UNHCR Emergency Handbook: Older persons [Internet]. 2023; [cited 2023 Feb 27]. Available from: https://emergency.unhcr.org/entry/43935/older-persons.
- Moher D, Liberati A, Tetzlaff J, PRISMA Group., et al. Preferred reporting items for systematic reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi:10.1371/journal.pmed.1000097.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi:10.1191/1478088706qp063oa.
- Smallfield S, Berger S, Hillman B, et al. Living with low vision: strategies supporting daily activity. Occup Ther Health Care. 2017;31(4):312–328. doi:10.1080/07380577.2017.1384969.
- Cherniack E. Not just fun and games: applications of virtual reality in the identification and rehabilitation of cognitive disorders of the elderly. Disabil Rehabil Assist Technol. 2011;6(4):283–289. doi:10.3109/17483107.2010.542570.
- Bedaf S, Gelderblom G, De Witte L. Overview and categorization of robots supporting independent living of elderly people: what activities do they support and how far have they developed. Assist Technol. 2015;27(2):88–100. doi:10.1080/10400435.2014.978916.
- Bharucha AJ, Anand V, Forlizzi J, et al. Intelligent assistive technology applications to dementia care: current capabilities, limitations, and future challenges. Am J Geriatr Psychiatry. 2009;17(2):88–104. doi:10.1097/JGP.0b013e318187dde5.
- Chan M, Estève D, Escriba C, et al. A review of smart homes-present state and future challenges. Comput Methods Programs Biomed. 2008;91(1):55–81. doi:10.1016/j.cmpb.2008.02.001.
- Krishnan R, Pugazhenthi S. Mobility assistive devices and self-transfer robotic systems for elderly, a review. Intel Serv Robotics. 2014;7(1):37–49. doi:10.1007/s11370-013-0142-6.
- Pradhan B, Bharti D, Chakravarty S, et al. Internet of things and robotics in transforming current-day healthcare services. J Healthc Eng. 2021;2021:9999504. doi:10.1155/2021/9999504.
- Inskip JA, Lauscher HN, Li LC, et al. Patient and health care professional perspectives on using telehealth to deliver pulmonary rehabilitation. Chron Respir Dis. 2018;15(1):71–80. doi:10.1177/1479972317709643.
- Philips B, Smits C, Govaerts PJ, et al. Empowering senior cochlear implant users at home via a tablet computer application. Am J Audiol. 2018;27(3S):417–430. doi:10.1044/2018_AJA-IMIA3-18-0014.
- Gélinas-Bronsard D, Mortenson WB, Ahmed S, et al. Co-construction of an internet-based intervention for older assistive technology users and their family caregivers: stakeholders’ perceptions. Disabil Rehabil Assist Technol. 2019;14(6):602–611. doi:10.1080/17483107.2018.1499138.
- Holthe T, Jentoft R, Arntzen C, et al. Benefits and burdens: family caregivers’ experiences of assistive technology (at) in everyday life with persons with young-onset dementia (YOD). Disabil Rehabil Assist Technol. 2018;13(8):754–762. doi:10.1080/17483107.2017.1373151.
- Maidment DW, Ali YHK, Ferguson MA. Applying the COM-B model to assess the usability of smartphone-connected listening devices in adults with hearing loss. J Am Acad Audiol. 2019;30(5):417–430. doi:10.3766/jaaa.18061.
- Imbeault H, Langlois F, Bocti C, et al. Can people with Alzheimer’s disease improve their day-to-day functioning with a tablet computer? Neuropsychol Rehabil. 2018;28(5):779–796. doi:10.1080/09602011.2015.1133431.
- Rupal BS, Rafique S, Singla A, et al. Lower-limb exoskeletons: research trends and regulatory guidelines in medical and non-medical applications. Int J Adv Robot Syst. 2017;14:1–27.
- Khanuja K, Joki J, Bachmann G, et al. Gait and balance in the aging population: fall prevention using innovation and technology. Maturitas. 2018;110:51–56. doi:10.1016/j.maturitas.2018.01.021.
- Ng SL, Phelan S, Leonard M, et al. A qualitative case study of smartphone-connected hearing aids: influences on patients, clinicians, and patient-clinician interactions. J Am Acad Audiol. 2017;28(6):506–521. doi:10.3766/jaaa.15153.
- Peek STM, Luijkx KG, Vrijhoef HJM, et al. Origins and consequences of technology acquirement by independent-living seniors: towards an integrative model. BMC Geriatr. 2017;17(1):189. doi:10.1186/s12877-017-0582-5.
- Scott RA, Callisaya ML, Duque G, et al. Assistive technologies to overcome sarcopenia in ageing. Maturitas. 2018;112:78–84. doi:10.1016/j.maturitas.2018.04.003.
- Robinson L, Gibson G, Kingston A, et al. Assistive technologies in caring for the oldest old: a review of current practice and future directions. Aging Health. 2013;9(4):365–375. doi:10.2217/ahe.13.35.
- Alqahtani S, Joseph J, Dicianno B, et al. Stakeholder perspectives on research and development priorities for mobility assistive-technology: a literature review. Disabil Rehabil Assist Technol. 2021;16(4):362–376. doi:10.1080/17483107.2019.1650300.
- Arthanat S, Vroman KG, Lysack C, et al. Multi-stakeholder perspectives on information communication technology training for older adults: implications for teaching and learning. Disabil Rehabil Assist Technol. 2019;14(5):453–461. doi:10.1080/17483107.2018.1493752.
- Hall A, Boulton E, Stanmore E. Older adults’ perceptions of wearable technology hip protectors: implications for further research and development strategies. Disabil Rehabil Assist Technol. 2019;14(7):663–668. doi:10.1080/17483107.2018.1491647.
- McGrath C, Corrado AM. The environmental factors that influence technology adoption for older adults with age-related vision loss. Br J Occup Ther. 2019;82(8):493–501. doi:10.1177/0308022618813247.
- Sriram V, Jenkinson C, Peters M. Informal carers’ experience of assistive technology use in dementia care at home: a systematic review. BMC Geriatr. 2019;19(1):160. doi:10.1186/s12877-019-1169-0.
- Tuisku O, Pekkarinen S, Hennala L, et al. “Robots do not replace a nurse with a beating heart”: the publicity around a robotic innovation in elderly care. ITP. 2019;32(1):47–67. doi:10.1108/ITP-06-2018-0277.
- Virgili G, Acosta R, Grover LL, et al. Reading aids for adults with low vision. Cochrane Database Syst Rev. 2018;10.
- Wang J. Mobile and connected health technology needs for older adults aging in place. J Gerontol Nurs. 2018;44(6):3–5. doi:10.3928/00989134-20180509-01.
- Xiong C, Astell A, Mihailidis A, et al. Needs and preferences for technology among Chinese family caregivers of persons with dementia: a pilot study. J Rehabil Assist Technol Eng. 2018;5:2055668318775315. doi:10.1177/2055668318775315.
- Seaborn K, Pennefather P, Fels D. “Learn what we’re going through”: attitudes of older powered chair users towards mixed reality games that involve power mobility. Univ Access Inf Soc. 2016;15(4):699–711. doi:10.1007/s10209-015-0450-z.
- Yurkewich A, Hebert D, Wang RH, et al. Hand extension robot orthosis (HERO) glove: development and testing with stroke survivors with severe hand impairment. IEEE Trans Neural Syst Rehabil Eng. 2019;27(5):916–926. doi:10.1109/TNSRE.2019.2910011.
- Olsson A, Skovdahl K, Engstrom M. Using diffusion of innovation theory to describe perceptions of a passive positioning alarm among persons with mild dementia: a repeated interview study. BMC Geriatr. 2016;16:3. doi:10.1186/s12877-016-0183-8.
- Stefanov D, Bien Z, Bang W-C. The smart house for older persons and persons with physical disabilities: structure, technology arrangements, and perspectives. IEEE Trans Neural Syst Rehabil Eng. 2004;12(2):228–250. doi:10.1109/TNSRE.2004.828423.
- Eftring H, Frennert S. Designing a social and assistive robot for seniors. Z Gerontol Geriatr. 2016;49(4):274–281. doi:10.1007/s00391-016-1064-7.
- Lo K, Stephenson M, Lockwood C. The economic cost of robotic rehabilitation for adult stroke patients: a systematic review. JBI Database System Rev Implement Rep. 2019;17(4):520–547. doi:10.11124/JBISRIR-2017-003896.
- Wang RH, Sudhama A, Begum M, et al. Robots to assist daily activities: views of older adults with Alzheimer’s disease and their caregivers. Int Psychogeriatr. 2017;29(1):67–79. doi:10.1017/S1041610216001435.
- Wu YH, Cristancho-Lacroix V, Fassert C, et al. The attitudes and perceptions of older adults with mild cognitive impairment toward an assistive robot. J Appl Gerontol. 2016;35(1):3–17. doi:10.1177/0733464813515092.
- Martín-Lesende I, Orruño E, Mateos M, et al. Telemonitoring in-home complex chronic patients from primary care in routine clinical practice: impact on healthcare resources use. Eur J Gen Pract. 2017;23:135–142.
- Van Patten R, Keller AV, Maye JE, et al. Home-Based cognitively assistive robots: maximizing cognitive functioning and maintaining independence in older adults without dementia. Clin Interv Aging. 2020;15:1129–1139. doi:10.2147/CIA.S253236.
- van den Houten MML, Spruijt S, Fokkenrood HJP, et al. User preferences for mobile health interventions: a survey among intermittent claudication patients and their physical therapists. Ann Vasc Surg. 2018;46:249–256. doi:10.1016/j.avsg.2017.08.020.
- Hattink BJJ, Meiland FJM, Overmars-Marx T, et al. The electronic, personalizable rosetta system for dementia care: exploring the user-friendliness, usefulness and impact. Disabil Rehabil Assist Technol. 2016;11(1):61–71. doi:10.3109/17483107.2014.932022.
- Crea S, Cempini M, Mazzoleni S, et al. Phase-II clinical validation of a powered exoskeleton for the treatment of elbow spasticity. Front Neurosci. 2017;11:261. doi:10.3389/fnins.2017.00261.
- Fan J, Bian D, Zheng Z, et al. A robotic coach architecture for elder care (ROCARE) based on multi-user engagement models. IEEE Trans Neural Syst Rehabil Eng. 2017;25(8):1153–1163. doi:10.1109/TNSRE.2016.2608791.
- Evans J, Papadopoulos A, Silvers CT, et al. Remote health monitoring for older adults and those with heart failure: adherence and system usability. Telemed J E Health. 2016;22(6):480–488. doi:10.1089/tmj.2015.0140.
- Nasr N, Leon B, Mountain G, et al. The experience of living with stroke and using technology: opportunities to engage and co-design with end users. Disabil Rehabil Assist Technol. 2016;11(8):653–660. doi:10.3109/17483107.2015.1036469.
- Maia JC, Coutinho JFV, De Sousa CR, et al. Assistive technologies for demented elderly: a systematic review. Acta Paul. enferm. 2018;31(6):651–658. doi:10.1590/1982-0194201800089.
- Tedesco Triccas L, Burridge JH, Hughes AM, et al. A qualitative study exploring views and experiences of people with stroke undergoing transcranial direct current stimulation and upper limb robot therapy. Top Stroke Rehabil. 2018;25:1–9. doi:10.1080/10749357.2018.1493072.
- Øksnebjerg L, Woods B, Ruth K, et al. A tablet app supporting self-management for people with dementia: explorative study of adoption and use patterns. JMIR Mhealth Uhealth. 2020;8(1):e14694. doi:10.2196/14694.
- Mordoch E, Osterreicher A, Guse L, et al. Use of social commitment robots in the care of elderly people with dementia: a literature review. Maturitas. 2013;74(1):14–20. doi:10.1016/j.maturitas.2012.10.015.
- Swinnen E, Lefeber N, Willaert W, et al. Motivation, expectations, and usability of a driven gait orthosis in stroke patients and their therapists. Top Stroke Rehabil. 2017;24(4):299–308. doi:10.1080/10749357.2016.1266750.
- Zhou B, Zhang J, Zhao Y, et al. Caregiver-delivered stroke rehabilitation in rural China. Stroke. 2019;50(7):1825–1830. doi:10.1161/STROKEAHA.118.021558.
- Halvorsrud L, Holthe T, Karterud D, et al. Perspectives on assistive technology among older norwegian adults receiving community health services. Disabil Rehabil Assist Technol. 2023;18(5):685–692. doi:10.1080/17483107.2021.1906962.
- Fiorini L, De Mul M, Fabbricotti I, et al. Assistive robots to improve the independent living of older persons: results from a needs study. Disabil Rehabil Assist Technol. 2021;16(1):92–102. doi:10.1080/17483107.2019.1642392.
- Cinini A, Cutugno P, Ferraris C, et al. Final results of the NINFA project: impact of new technologies in the daily life of elderly people. Aging Clin Exp Res. 2021;33(5):1213–1222. doi:10.1007/s40520-019-01357-6.
- García-Soler Á, Facal D, Díaz-Orueta U, et al. Inclusion of service robots in the daily lives of frail older users: a step-by-step definition procedure on users’ requirements. Arch Gerontol Geriatr. 2018;74:191–196. doi:10.1016/j.archger.2017.10.024.
- Hawley-Hague H, Tacconi C, Mellone S, et al. Smartphone apps to support falls rehabilitation exercise: app development and usability and acceptability study. JMIR Mhealth Uhealth. 2020;8(9):e15460. doi:10.2196/15460.
- Jørgensen TS, Skougaard M, Taylor PC, et al. The parker model: applying a qualitative three-step approach to optimally utilize input from stakeholders when introducing new device technologies in the management of chronic rheumatic diseases. Patient. 2018;11(5):515–526. doi:10.1007/s40271-018-0306-8.
- Raghunath N, Dahmen J, Brown K, et al. Creating a digital memory notebook application for individuals with mild cognitive impairment to support everyday functioning. Disabil Rehabil Assist Technol. 2020;15(4):421–431. doi:10.1080/17483107.2019.1587017.
- van der Cammen TJM, Albayrak A, Voûte E, et al. New horizons in design for autonomous ageing. Age Ageing. 2017;46:11–17.
- Tomšič M, Domajnko B, Zajc M. The use of assistive technologies after stroke is debunking the myths about the elderly. Top Stroke Rehabil. 2018;25(1):28–36. doi:10.1080/10749357.2017.1376845.
- Bedaf S, Marti P, Amirabdollahian F, et al. A multi-perspective evaluation of a service robot for seniors: the voice of different stakeholders. Disabil Rehabil Assist Technol. 2018;13(6):592–599. doi:10.1080/17483107.2017.1358300.
- Amlani AM, Smaldino J, Hayes D, et al. Feasibility of using a Smartphone-Based hearing aid application to improve attitudes toward amplification and hearing impairment. Am J Audiol. 2019;28(1):125–136. doi:10.1044/2018_AJA-17-0068.
- Lemke M, Rodríguez Ramírez E, Robinson B, et al. Motivators and barriers to using information and communication technology in everyday life following stroke: a qualitative and video observation study. Disabil Rehabil. 2020;42(14):1954–1962. doi:10.1080/09638288.2018.1543460.
- Thilo FJS, Hahn S, Halfens RJG, et al. Usability of a wearable fall detection prototype from the perspective of older people-A real field testing approach. J Clin Nurs. 2019;28(1-2):310–320. doi:10.1111/jocn.14599.
- Quintana M, Anderberg P, Berglund JS, et al. Feasibility-usability study of a tablet app adapted specifically for persons with cognitive impairment-SMART4MD (support monitoring and reminder technology for mild dementia). Int J Environ Res Public Health. 2020;17:1–21.
- Sejunaite K, Lanza C, Ganders S, et al. Augmented reality: sustaining autonomous way-finding in the community for older persons with cognitive impairment. J Frailty Aging. 2017;6(4):206–211. doi:10.14283/jfa.2017.25.
- Nauha L, Keränen NS, Kangas M, et al. Assistive technologies at home for people with a memory disorder. Dementia (London). 2018;17(7):909–923. doi:10.1177/1471301216674816.
- Rawstorn JC, Gant N, Rolleston A, et al. End users want alternative intervention delivery models: usability and acceptability of the REMOTE-CR exercise-based cardiac telerehabilitation program. Arch Phys Med Rehabil. 2018;99(11):2373–2377. doi:10.1016/j.apmr.2018.06.027.
- Yasuhara Y, Tanioka T, Kai Y, et al. Potential legal issues when caring healthcare robot with communication in caring functions are used for older adult care. Enferm Clin. 2020;30:54–59. doi:10.1016/j.enfcli.2019.09.024.
- Pludwinski S, Ahmad F, Wayne N, et al. Participant experiences in a smartphone-based health coaching intervention for type 2 diabetes: a qualitative inquiry. J Telemed Telecare. 2016;22(3):172–178. doi:10.1177/1357633X15595178.
- Jie LJ, Jamin G, Smit K, et al. Design of the user interface for “Stappy”, a sensor-feedback system to facilitate walking in people after stroke: a user-centred approach. Disabil Rehabil Assist Technol. 2020;15(8):959–967. doi:10.1080/17483107.2019.1629654.
- Gerling K, Hebesberger D, Dondrup C, et al. Robot deployment in long-term care: case study on using a mobile robot to support physiotherapy. Z Gerontol Geriatr. 2016;49(4):288–297. doi:10.1007/s00391-016-1065-6.
- Bedaf S, Marti P, De Witte L. What are the preferred characteristics of a service robot for the elderly? A multi-country focus group study with older adults and caregivers. Assist Technol. 2019;31(3):147–157. doi:10.1080/10400435.2017.1402390.
- Searcy RP, Summapund J, Estrin D, et al. Mobile health technologies for older adults with cardiovascular disease: current evidence and future directions. Curr Geri Rep. 2019;8(1):31–42. doi:10.1007/s13670-019-0270-8.
- Melkas H, Hennala L, Pekkarinen S, et al. Impacts of robot implementation on care personnel and clients in elderly-care institutions. Int J Med Inform. 2020;134:104041. doi:10.1016/j.ijmedinf.2019.104041.
- Reyes A, Qin P, Brown CA. Standardized review of smartphone applications to promote balance for older adults. Disabil Rehabil. 2018;40(6):690–696. doi:10.1080/09638288.2016.1250124.
- D’Onofrio G, Fiorini L, Hoshino H, et al. Assistive robots for socialization in elderly people: results pertaining to the needs of the users. Aging Clin Exp Res. 2019;31(9):1313–1329. doi:10.1007/s40520-018-1073-z.
- Braley R, Fritz R, Van Son CR, et al. Prompting technology and persons with dementia: the significance of context and communication. Gerontologist. 2019;59(1):101–111. doi:10.1093/geront/gny071.
- Kringle EA, Setiawan IMA, Golias K, et al. Feasibility of an iterative rehabilitation intervention for stroke delivered remotely using mobile health technology. Disabil Rehabil Assist Technol. 2020;15(8):908–916. doi:10.1080/17483107.2019.1629113.
- Mallet K, Shamloul R, Pugliese M, et al. RecoverNow: a patient perspective on the delivery of mobile tablet-based stroke rehabilitation in the acute care setting. Int J Stroke. 2019;14(2):174–179. doi:10.1177/1747493018790031.
- Werner C, Kardaris N, Koutras P, et al. Improving gesture-based interaction between an assistive bathing robot and older adults via user training on the gestural commands. Arch Gerontol Geriatr. 2020;87:103996. doi:10.1016/j.archger.2019.103996.
- Etingen B, Martinez RN, Vallette MA, et al. Patient perceptions of environmental control units: experiences of veterans with spinal cord injuries and disorders receiving inpatient VA healthcare. Disabil Rehabil Assist Technol. 2018;13(4):325–332. doi:10.1080/17483107.2017.1312574.
- Emmerson KB, Harding KE, Lockwood KJ, et al. Home exercise programs supported by video and automated reminders for patients with stroke: a qualitative analysis. Aust Occup Ther J. 2018;65(3):187–197. doi:10.1111/1440-1630.12461.
- Cajita MI, Hodgson NA, Budhathoki C, et al. Intention to use mHealth in older adults with heart failure. J Cardiovasc Nurs. 2017;32(6):E1–E7. doi:10.1097/JCN.0000000000000401.
- Span M, Hettinga M, Groen-van de Ven L, et al. Involving people with dementia in developing an interactive web tool for shared decision-making: experiences with a participatory design approach. Disabil Rehabil. 2018;40(12):1410–1420. doi:10.1080/09638288.2017.1298162.
- Isaković M, Sedlar U, Volk M, et al. Usability pitfalls of diabetes mHealth apps for the elderly. J Diabetes Res. 2016;2016:1604609. doi:10.1155/2016/1604609.
- Hudson J, Ungar R, Albright L, et al. Robotic pet use among community-dwelling older adults. J Gerontol B Psychol Sci Soc Sci. 2020;75(9):2018–2028. doi:10.1093/geronb/gbaa119.
- Franceschini M, Goffredo M, Pournajaf S, et al. Predictors of activities of daily living outcomes after upper limb robot-assisted therapy in subacute stroke patients. PLoS One. 2018;13(2):e0193235. doi:10.1371/journal.pone.0193235.
- Huang T, Huang C. Attitudes of the elderly living independently towards the use of robots to assist with activities of daily living. Work. 2021;69(1):55–65. doi:10.3233/WOR-205166.
- Choukou MA, Shortly T, Leclerc N, et al. Evaluating the acceptance of ambient assisted living technology (AALT) in rehabilitation: a scoping review. Int J Med Inform. 2021;150.
- Berridge C, Wetle TF. Why older adults and their children disagree about in-home surveillance technology, sensors, and tracking. Gerontologist. 2020;60(5):926–934. doi:10.1093/geront/gnz068.
- Venkatesh V, Thong J, Xu X. Consumer acceptance and use of information technology: extending the unified theory of acceptance and use of technology. MIS Quarterly 2012;36:157–178. doi:10.2307/41410412.
- Accius J, Suh J. The longevity economy outlook: how people ages 50 and older are fueling economic growth, stimulating jobs, and creating opportunities for all. DC; 2019.
- Housing for older Canadians. The definitive guide to the over-55 market [Internet]. Ottawa; 2015. Available from: http://publications.gc.ca/site/eng/9.696164/publication.html.
- Grignon M, Spencer B. The funding of long-term care in Canada: what do we know, what should we know? Can J Aging. 2018;37(2):110–120. doi:10.1017/S0714980818000028.
- Menon A, Korner-Bitensky N, Kastner M, et al. Strategies for rehabilitation professionals to move evidence-based knowledge into practice: a systematic review. J Rehabil Med. 2009;41(13):1024–1032. doi:10.2340/16501977-0451.
- Baptista G, Oliveira T. Understanding mobile banking: the unified theory of acceptance and use of technology combined with cultural moderators. Comput Hum Behav. 2015;50:418–430. doi:10.1016/j.chb.2015.04.024.
- Fisman D, Bogoch I, Lapointe-Shaw L, et al. Risk factors associated with mortality among residents with coronavirus disease 2019 (COVID-19) in long-term care facilities in Ontario, Canada. JAMA Netw Open. 2020;3(7):e2015957. doi:10.1001/jamanetworkopen.2020.15957.
- Daniel A. Rehab facilities preparing for COVID-19 crunch as more patients recover. CMAJ News [Internet]; [2020 Jun 12]. Available from: http://cmajnews.com/2020/06/12/covid-rehab-1095878/
- Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5(5):e256. doi:10.1016/S2468-2667(20)30061-X.