Abstract
Multi-Modality Aphasia Treatment (M-MAT) is an effective group intervention for post-stroke aphasia. M-MAT employs interactive card games and the modalities of gesture, drawing, reading, and writing to improve spoken language. However, there are challenges to implementation of group interventions such as M-MAT, particularly for those who cannot travel or live in rural areas. To maximise access to this effective treatment, we aimed to adapt M-MAT to telehealth format (M-MAT Tele). The Human-Centred Design Framework was utilized to guide the adaptation approach. We identified the intended context of use (outpatient/community rehabilitation) and the stakeholders (clinicians, people with aphasia, health service funders). People with aphasia and practising speech pathologists were invited to co-design M-MAT Tele in a series of iterative workshops, to ensure the end product was user-friendly and clinically feasible. The use of co-design allowed us to understand the hardware, software and other constraints and preferences of end users. In particular, clinicians (n = 3) required software compatible with a range of telehealth platforms and people with aphasia (n = 3) valued solutions with minimal technical demands and costs for participants. Co-design within the Human-Centred Design Framework led to a telehealth solution compatible with all major telehealth platforms, with minimal hardware or software requirements. Pilot testing is underway to confirm acceptability of M-MAT Tele to clinicians and people with aphasia, aiming to provide an effective, accessible tool for aphasia therapy in telehealth settings.
IMPLICATIONS FOR REHABILITATION
We applied the Human-Centred Design Framework to ensure that the adaptation of Multi-Modality Aphasia Therapy (M-MAT) for telehealth was suited to the end users and context of use
Compatibility and accessibility were valued by stakeholders over technological sophistication, an important consideration for similar design projects in rehabilitation
If shown to have similar clinical effectiveness as the in person M-MAT protocol, M-MAT Tele will offer a highly feasible group treatment option for people with aphasia in remote locations or who are unable to travel
Approximately one third of strokes result in aphasia, an impairment of language processing that affects speaking, comprehension, reading and writing [Citation1]. People with aphasia experience profound impacts on quality of life and mood [Citation2,Citation3], low rates of return to work [Citation4], and higher levels of relationship breakdown [Citation5]. Therefore, effective rehabilitative interventions for people with aphasia are crucial.
Multi-Modality Aphasia Treatment (M-MAT) is an aphasia intervention provided by a speech pathologist to groups of two to three people with the aim of improving language and communication [Citation6]. In M-MAT, participants practise production of verbal phrases and sentences through interactive card games. These games progress through specific verbal requests from participants, a concept known as language action games [Citation7]. The clinician guides participants in the use of non-speech modalities—namely gesture, drawing, reading and writing—to facilitate successful verbal production of target words, phrases and sentences (For detailed descriptions of M-MAT procedures, see Pierce et al. [Citation8]; Rose et al. [Citation9]). As a group-based intervention, M-MAT is vastly more efficient than traditional 1:1 service models. Recently, a large, Phase III randomised controlled trial showed that M-MAT is effective in improving communication-related quality of life, word retrieval, and everyday communication in people with aphasia when provided at a high intensity of 30 h in 2 weeks (3 h × 10 days), compared to usual care [Citation9]. However, there are multiple barriers to conducting high intensity interventions such as M-MAT for people with aphasia. Frequent transport to therapy sessions places a high burden on family and carers [Citation10], while for stroke survivors without family or friends to transport them, cognitive, language and motor symptoms can make both public transport and driving challenging, if not impossible [Citation11]. In addition, it can be challenging for speech pathologists to find two to three people with the same aphasia severity within driving distance of each other to form a group for M-MAT. This is particularly the case in rural, regional or remote areas within geographically large countries such as Australia, meaning that people with aphasia who live outside of cities are considerably less likely to benefit from this effective treatment.
Amongst the range of recent technological advances for people with aphasia [Citation12], telehealth is an option that can improve accessibility of treatment. Telehealth expands the availability of services to people living rurally and to those who have difficulty travelling [Citation13]. For caregivers, telehealth can alleviate the considerable burden of transporting their family member to treatment. Service provision costs are also lowered [Citation14] and demand for physical treatment space at health services may be reduced. Currently, there are very few evidence-based telehealth treatments for aphasia. In a recent systematic review of telerehabilitation in aphasia, just five studies with an experimental or quasi-experimental design (that is, with a control group) were reported [Citation15]. Following the unprecedented expansion of telehealth during the COVID-19 pandemic, telehealth is likely to remain a standard component of care delivery and more evidence-based aphasia telehealth options are therefore needed [Citation13]. There are also very few group-based telehealth treatments for aphasia – only five of 23 studies in a recent scoping review involved group treatments [Citation16]. Yet, group interventions offer comparable outcomes [Citation17] at a significant cost saving [Citation18]. Thus, a successful adaptation of M-MAT for telehealth administration could provide an evidence-based, group treatment option.
In this project we aimed to adapt the evidence-based, in-person, group intervention M-MAT to an online format (M-MAT Tele). The objective was an adaptation that is accessible for and acceptable to patients and speech pathologists and therefore able to be readily implemented in clinical settings, while also retaining the key components of the original in-person treatment.
Method
The adaptation of M-MAT for telehealth delivery was conducted through application of the Human Centred Design Framework [Citation19]. Human Centred Design focuses on the user’s needs and requirements in the design process in order to promote a usable, accessible and effective end result. A user-centric approach is especially valuable when users have unique needs and is therefore highly relevant to people with aphasia, whose communication disability often necessitates special adaptations to ensure technology is fully accessible [Citation20,Citation21]. The Human Centred Design approach was also valuable in ensuring that M-MAT Tele would meet the requirements of the second key user group, speech pathologists, which would in turn, promote implementation in clinical settings.
A central component of the original, in-person M-MAT is the use of multiple communication modalities to facilitate verbal language rehabilitation (i.e., use of a cueing that includes gesture, drawing, reading and writing). Treatment also requires specifically designed picture cards of the target words and written examples of the sentences in which the words are used. Both the multimodal aspect and the group language action games () required careful translation into telehealth form to preserve treatment fidelity of the in-person treatment and maintain participant motivation. Therefore, prior to initiation of the design process, a task analysis was conducted to outline the key activities and elements involved in M-MAT [Citation11]. The M-MAT protocol was carefully evaluated, considering the materials used and therapist and participant requirements at each step. Potential technical functions that might fulfil each requirement were also listed. As an example, for the game Go Fish, each participant is dealt five cards at random, and participants should not be able to see one another’s cards, yet the therapist needs to be able to view all participants’ cards. Clear audio is required for participants to request cards from one another, a method of changing player scores is needed, and new cards are assigned at random from the remaining stack. For the multimodal cues, the therapist needs to model and view participants’ gestures, drawings and writing. This might be achieved through pre-prepared photographs or videos, through a whiteboard function, or by holding paper up to a web camera. The M-MAT task analysis is attached as Supplemental Appendix A.
Table 1. Brief description of games found in M-MAT (original, in person protocol).
The Human Centred Design Framework does not rigidly specify a process but describes four activities that should be iteratively undertaken [Citation19,p.5):
Understanding and specifying the context of use
Specifying the user requirements
Producing design solutions
Evaluating the design.
These four stages are described in this paper within the method (1–2) and results (3–4) sections, though as design was a cyclical process, the steps occurred non-linearly.
Understand and specify context of use
The context of use outlines the users and stakeholders, their characteristics, the goals of the system being designed, and the environment in which it is expected to be used [Citation19]. The intended goal of M-MAT Tele is rehabilitation of people with post-stroke aphasia, delivered remotely by qualified speech pathologists. More specifically, M-MAT Tele is likely to be used with outpatients in the subacute and chronic stages of stroke recovery (2–6 and >6 months post stroke respectively). Speech pathologists are therefore most likely to be working in outpatient or community services. They are likely to be familiar with technology and telehealth service delivery but not necessarily with group treatment or group telehealth treatment. People with aphasia who will participate in M-MAT Tele are likely to do so from home. We were cognisant that, as with all telehealth, M-MAT Tele would not be acceptable or desirable to all people with aphasia, as some prefer exclusively in-person treatment. Target users were therefore thought to be those who used tablets or computers in some form prior to their stroke. Other key stakeholders included health service managers, funding bodies, and caregivers/family of people with aphasia, though these stakeholders will not directly use M-MAT Tele and were not considered target users.
Understanding user requirements
With the planned context of use established, we sought co-designers representative of the key users to participate in the development process: people with aphasia and speech pathologists. Three co-designers from each user group were sought, a pragmatic decision based on (a) project resources and (b) the ability to meaningfully involve co-designers throughout the project. There is minimal research on the ideal number of co-designers for a project [Citation22]. However, some qualitative feedback suggests that many with acquired brain injury prefer smaller groups for this purpose [Citation23,Citation24].
Inclusion criteria were developed according to the target users outlined above. For people with aphasia, the criteria were:
Willing to use videoconference
Diagnosed with aphasia from a stroke
Aged 18 years or over
Sufficient communication ability to provide informed consent and express views/opinions.Footnote1
Co-designers were purposively sampled to include at least one participant from a rural, regional, or remote area and at least one participant who had previously received rehabilitation over telehealth.
For speech pathologists, inclusion criteria were (1) practicing speech pathologist with experience working with aphasia; (2) experience in providing telehealth. We also sought at least one co-designer who had previously provided M-MAT in-person.
Ethical approval for the study was received from La Trobe University Human Research Ethics Committee (#HEC22031). All participants gave informed consent, with appropriate modifications made to the written materials to make them accessible to people with aphasia.
Co-designers participated in initial workshops of two hours, with speech pathologists and people with aphasia in separate workshops. These workshops were held online over videoconference, which allowed a spread of geographical location and also primed co-designers’ views on the use of this medium. People with aphasia were enabled to access and participate in the online workshops through additional communication supports such as the use of images, visual rating scales, multiple choice responses and written key words.
During the initial workshops, co-designers were asked to describe the existing context of their telehealth use; that is, when and where they conduct/receive rehabilitation over telehealth, or where they would prefer to do so, what hardware and software they use and would be willing/unwilling to use, and how often. In addition, an example video of in-person M-MAT was shown to participants to prompt their views on a telehealth adaptation, including potential challenges, necessary and desirable features, cost constraints, and other comments. The workshops were semi-structured, with both specific and open-ended questions and time for general comments and thoughts. Topic guides from the workshops are available in Supplemental Appendices B and C.
Results
Six co-designers were successfully recruited to the project. Relevant demographic details are shown in and . All participants were white, native English speakers. People with aphasia were distributed across age, location, and experience with telehealth, though all were male. Speech pathologists were experienced in providing telehealth and in working with aphasia. They were located in three different states – an important characteristic given each Australian state has its own health system requirements. All speech pathologists were female, which is grossly representative of the Australian speech pathology workforce (97%). One had previously conducted in-person M-MAT ().
Table 2. Key demographic data for co-designers with aphasia.
Table 3. Key demographic data for clinician co-designers.
Clinician user requirements
The use of telehealth at clinicians’ workplaces varied considerably; one was a specialised telehealth service prior to COVID, which provided training and loan devices to patients; others were rapidly required to switch to telehealth during the COVID-19 pandemic, with mixed continuation of telehealth vs in-person services since. For telehealth delivery, clinicians used desktop computers with single or dual screens, inbuilt and external web cameras, and headphones with microphone. Two clinicians did not have access to a document camera, limiting this as an option for demonstrating drawing and writing examples for M-MAT Tele. They reported that their clients commonly used tablets, sometimes smartphones, and rarely computers. Except at the specialised telehealth service, clients were expected to provide their own device. The importance of helping clients position their device for telehealth was emphasised, as many hold it on their lap which would limit the clinician’s view of gesture and facial expression.
Telehealth platforms varied by state and each included different features. contains a summary of supported features for relevant platforms, adapted from Vuong et al. [Citation21]) and based on clinician and researcher exploration of platforms in June 2022. Screensharing was the only feature common across all platforms, meaning that relying on options such as chat, virtual whiteboard and cursor control would limit the suitability of M-MAT Tele. Clinicians expressed a preference for software being contained within a single window, as switching between multiple windows could become complex and confusing.
Table 4. Support for features on commonly used telehealth platforms as of June 2022.
Additional important points raised by clinicians were:
Text should be large enough to be viewed on client tablets.
The difficulty of typing on touchscreens for many clients.
The challenge in clients holding up paper to the camera, as they often misjudged the position of the camera.
Significant time required to get some clients logged on and with other troubleshooting.
Clinicians reported that their workplace would consider funding software or hardware of up to “several hundred dollars,” but more than that would need justification. Importantly, clinicians worked in IT environments that often restricted the use of executable files or installation of software. They were open to using a group approach to rehabilitation, though concerned that if one participant required extensive technical support, it would waste the therapy time of the remaining two. Overall, they recommended simplicity wherever possible; specifically, fewer logins, installations, pieces of equipment and technical demands on clients were preferred wherever feasible.
User requirements of people with aphasia
The co-designers with aphasia attended the initial workshop with a caregiver for support. One co-designer rated in-person and telehealth treatment as equal, and the others preferred in-person if forced to choose, but all reported positive perspectives of telehealth for aphasia. Positives included not having to travel and clinicians not wearing masks on telehealth, as opposed to in-person appointments during COVID-19 restrictions, which aided their comprehension. In past experiences of telehealth, co-designers had used Apple iPads and/or laptops, therefore the built in camera and microphone had been used. They preferred not to use headphones. Co-designers described the telehealth platforms they had used in the past and it was determined they had used Zoom, QHealth telehealth portal and Microsoft Teams.
The co-designers reported sitting in various places in their house during telehealth, including at tables and desks, on the couch or even in bed. All felt that if a desk was needed for handwriting and drawing, this would be acceptable. Finding a quiet place in the house was not problematic for these co-designers. With regards to group therapy, they expressed concern that more reticent participants might miss out on therapy but were satisfied that this might not be an issue within M-MAT as it is turn-based. In terms of the help required to use videoconferencing, they reported needing someone on site with them to provide troubleshooting support for technical or communication issues.
The co-designers were asked about their experiences and preferences with specific features that had potential for use in M-MAT Tele:
Typing (e.g., into chat or other software) – No issues were raised with typing itself. However, in some videoconference software, the chat window is difficult to open and then gets in the way of the videoconference image and can be difficult to close.
Handwriting and showing the paper to the camera – participants were happy to do this, including one participant with upper limb hemiparesis, but discussed that individuals would find typing or handwriting preferable depending on age and profession.
Sharing their screen – with support from a family member or caregiver, co-designers had shared their screen with the clinician in the past or were happy to attempt this.
Controlling the clinician’s screen/cursor control – All were happy to try or had used with some success.
Drawing on a digital whiteboard – All were happy to try or had used with some success.
Despite a willingness to try many videoconferencing features such as using cursor control or chat boxes, co-designers recommended minimising the technical demands on the participants with aphasia where possible. Co-designers expressed a willingness to pay for hardware and/or software for M-MAT Tele if it was beneficial to their communication but felt strongly that those with aphasia who could not afford to pay should not be disadvantaged; overall, avoiding specialised equipment or software where possible was recommended.
Producing design solutions
Following the initial workshops and task analysis, the authors synthesised the findings to a list of required and desirable features. Based on the required and desired features, and considering the user requirements and context, a draft of software and process was developed, avoiding designs that would limit broad usability. The suggested solution was envisaged to run in an internet browser, thus not requiring installation. Rather than having participants log in to a game hosted on a server, which would require passwords/logins and hosting, the games would be controlled by the clinician who would share their screen. While this clinician-control approach would limit the games that could be integrated, it would simplify use by putting the burden of technology on the clinician and also create an imperative for participants with aphasia to communicate – in order to participate in the games, they would need to request a card or turn. It would also eliminate hosting costs and password database management and reduce integration of videoconferencing. With this approach, the software could be kept low cost or free.
Not all games from the previous in-person intervention [Citation9] were suitable for the clinician-controlled approach. Go Fish requires participant to have cards that the other players cannot see, which is not possible with a single shared screen. Four games from the in-person intervention were included in the software draft – Snap, Bingo, Memory, and Who am I – and an additional game was proposed called Guess the Card. In Guess the Card, participants would select cards within a grid and place tokens on them. A random card would be chosen as the winner and any player with a token on the card would receive points. This proposed game includes an imperative to make verbal requests that is the key element of language action games [Citation7]. Cues were to be pre-recorded, to minimise starting and stopping of screensharing and to improve standardisation of the cues provided to participants.
A mock-up of possible software was developed to present to the co-designers, first on paper and then using Microsoft PowerPoint. This allowed a visual representation of the software and some simulation of the software through animations. During a second workshop, co-designers with aphasia were shown the mock-up and assisted to rate the five games on enjoyability and complexity. Open ended feedback on improvements was also sought. Three of the games were unanimously endorsed (Bingo, Memory and Guess the Card) while two received mixed feedback. In the clinician workshop, co-designers were positive about the games but gave detailed advice on the cues, example sentences and visual layout. Ultimately, three games were chosen for development, based on direct feedback, observations of use during workshops, and additional consideration of statistics from the in-person COMPARE trial: Analysis of data from over 2000 h of M-MAT conducted during the COMPARE trial showed that Bingo and Memory were chosen by participants for 19% and 22% of sessions respectively, while Who Am I and I Went Shopping were chosen for only 13% of sessions combined [Citation9].
Evaluating the design
When all co-designer input had been considered, a design brief was sent to software developers. Throughout the development process, six additional meetings were held with co-designer groups to review each iteration: 3 h total for clinicians and 3 h total for people with aphasia. As the navigation, cues, and games became more functional, the experience became a more concrete and accurate simulation of the final product. This meant that input by the co-designers became more targeted, particularly for those with aphasia who could experience details of treatment process rather than imagine it. A large proportion of the feedback was related to the user interface and visual elements. Flaws in the visual design became apparent, such as elements moving too quickly to be seen during screensharing, items being too small, and highlights of active elements being too subtle. Clinician co-designers also suggested that word classes be coloured differently on the sentence frames, e.g., spaces for nouns to be red, verbs blue, etc.
One challenge with the workshops was the limited time to experience the games – meetings were typically 1 h, leaving only about 15 min for trialling each game, whereas in treatment, participants have at least an hour to play each game. The games Bingo and Memory were visually similar as they both have a central grid of cards. This led to difficulties for the co-designers with aphasia understanding that a new game was being played with different rules, particularly given the short game duration in these meetings. To aid with visual signalling of a new game, a unique colour theme was suggested for each game and matched to the game icon on the main menu. This was helpful, although further testing will confirm whether new users can distinguish these games.
Co-designers also requested changes to the game functionality. Rather than a simple “[player 1] won!”, they suggested a popup screen that included an image of a trophy or medal. They also wanted to be able to view the final board and scores prior to starting a new game. Initially, the two cards flipped over in Memory automatically turned back over after several seconds, but clinicians felt this would not give enough time for users to attempt to memorise the shapes beneath them. A manual button to turn cards back over was therefore added.
Further evaluation is required through pilot testing of the intervention.
In total, the development process took six months to complete, producing software with a treatment protocol that meets key user requirements (see for screenshots); most significantly, compatible with the majority of telehealth platforms, minimal hardware and software requirements, maximal ease of use for participants, and inclusion of key elements of in-person M-MAT including multimodal cueing, language action games, multiple card sets and example sentence frames. Pilot testing is underway to further refine M-MAT Tele in preparation for clinical trials of efficacy and effectiveness. shows the key intervention elements from the task analysis and a summary of the way in which they were adapted.
Figure 1. M-MAT tele software screenshots.
(a) Screenshot of the homepage for M-MAT Tele. (b) Screenshot of the memory game within M-MAT Tele.
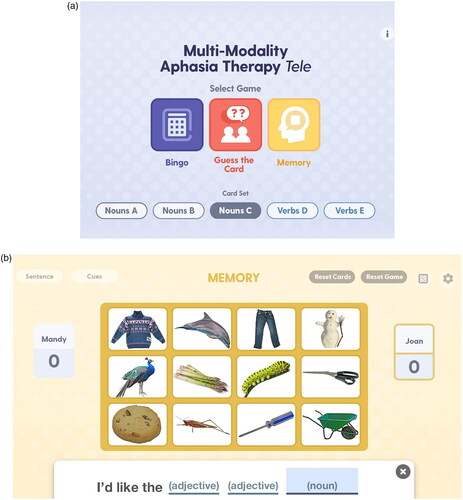
Table 5. Key elements of M-MAT and how they were adapted.
Discussion
The Human Centred Design framework was extremely valuable in designing M-MAT Tele for users with aphasia, who have highly specialised needs, and speech pathologists, who would ultimately make decisions on using M-MAT Tele or not. Thoroughly describing the context of use allowed us to consider the end environment in which M-MAT Tele would be used, which subsequently allowed us to select appropriate co-designers to provide user input. Understanding user requirements, including software limitations, cost, hardware, and preferences, was crucial to guiding the design process. It meant that we avoided inclusion of features that might have been innovative and useful but also excluded a portion of intended users, such as software requiring installation or the use of a graphics tablet for drawing and writing.
Our solution meets requirements for the project, according to (1) the intended context of use, based on the overall project aims, (2) key intervention ingredients of the original in-person intervention protocol, gathered through the task analysis, and (3) the user requirements, which were either explicitly reported by co-designers or observed by the researchers during testing of prototypes. However, in fulfilling the specifications for broad compatibility and ease of use, there was a trade-off in that M-MAT Tele did not include some sophisticated potential features. For instance, M-MAT Tele might have considered incorporating advanced technology such as computer gesture therapy (e.g., Marshall et al. [Citation25]) but such a feature would require shipping hardware to participants and/or installation of additional software, both of which could create barriers to implementation.
During the design process, valuable suggestions were raised by co-designers that could not be included in the final product. For example, customisable targets were suggested by clinicians, where the group would choose the words and sentences to practise during M-MAT Tele, but this required creation of an additional portal for clinicians to upload images, gesture videos and drawings, which was not feasible within the timeline and budget of the project. However, it was valuable to hear these suggestions from users as it allowed us to consider implementing them in future versions should funding allow. Past investigation of speech pathologists’ preferences for digital aphasia resources has shown that clinicians typically suggest a large number of ideal features [Citation26,Citation27]. Discussion of whether suggested items are “essential” versus “desirable” [Citation28] and ranking in order of priority could be useful approaches to manage suggestions in future developments.
As experienced by Spelter et al. [Citation20], our co-designers outlined the need for a visually simple, uncluttered interface, yet there were a high number of features that need to be available and reached within as few clicks as possible. Conflicts between simplicity of the user interface and the features are often present during technology design. For users with acquired brain injury, a “narrow-deep” interface (simpler layout with more screens to progress through) may result in fewer errors than a “broad-shallow” interface (more features available with fewer screens) [Citation29]. However, individual preferences for each interface differ, potentially based on experience with technology and cognitive profile. By putting the burden of navigation and use on the clinician, we were able to add some complexity compared to a system for direct use by people with aphasia.
Many policy frameworks do not require ethical approval for inclusion of consumers in co-design activities, as the role is not one of a passive research subject and should not involve vulnerability or risk. However, this is not universally agreed [Citation30,Citation31]. Given the personal experiences of telehealth that we discussed, along with the linguistic disability present in aphasia, the research team erred on the conservative side and gained ethical approval and informed consent from all co-designers. On reflection, this may not have been necessary and may even have implied reduced power on the user representatives’ side.
A larger sample size would have been beneficial in ensuring maximum feasibility and usability of M-MAT Tele. Using a maximal sampling approach did ensure representation across several important categories such as location, experience, and aphasia severity. However, all participants were white, native English speakers, limiting the diversity of the input for this project. People with aphasia who are also from a non-dominant ethnosocial background or language community can face additional disadvantages on top of the language disability [Citation32,Citation33]; thus, such voices are an important missing element. The project also lacked the input of women with aphasia.
In summary, involvement of end users from the beginning of the project, which is regarded as essential for technology development in aphasia [Citation34], has produce an acceptable, widely compatible tool. Next, we plan to test M-MAT Tele in a Phase I proof of concept study with a small cohort, collect user experience of both therapists and participants, and measure preliminary therapy outcomes. If found to be effective in treating aphasia, M-MAT Tele will be offered to clinicians free of charge and this collaborative, user-centred process will maximise the chances of implementation in clinical practice.
Supplemental Material
Download MS Word (25.4 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes
1 Note that by “communication ability,” we refer to communication using any modality; people with more severe aphasia who could communicate with gesture, drawing or writing were not excluded.
References
- Dickey L, Kagan A, Lindsay MP, et al. Incidence and profile of inpatient stroke-induced aphasia in Ontario, Canada. Arch Phys Med Rehabil. 2010;91(2):196–202. doi: 10.1016/j.apmr.2009.09.020.
- Hilari K. The impact of stroke: are people with aphasia different to those without? Disabil Rehabil. 2011;33(3):211–218. doi: 10.3109/09638288.2010.508829.
- Hilari K, Wiggins R, Roy P, et al. Predictors of health-related quality of life (HRQL) in people with chronic aphasia. Aphasiology. 2003;17(4):365–381. doi: 10.1080/02687030244000725.
- Flowers HL, Skoretz SA, Silver FL, et al. Poststroke aphasia frequency, recovery, and outcomes: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2016;97(12):2188–2201.e8. doi: 10.1016/j.apmr.2016.03.006.
- Dalemans RJP, De Witte L, Wade DT, et al. A description of social participation in working-age persons with aphasia: a review of the literature. Aphasiology. 2010;22(10):1071–1091. doi: 10.1080/02687030701632179.
- Rose ML, Attard MC. M-MAT Procedure Manual [Manual]. 2011.
- Pulvermüller F, Berthier ML. Aphasia therapy on a neuroscience basis. Aphasiology. 2008;22(6):563–599. doi: 10.1080/02687030701612213.
- Pierce JE, OHalloran R, Togher L, et al. Acceptability, feasibility and preliminary efficacy of low-moderate intensity Constraint Induced Aphasia Therapy and Multi-Modality Aphasia Therapy in chronic aphasia after stroke. Top Stroke Rehabil. 2023;31(1):44–56. doi: 10/gr559q.
- Rose ML, Nickels L, Copland D, et al. Results of the COMPARE randomised controlled trial of Constraint Induced or Multi-modality Aphasia Therapy compared with usual care in chronic post-stroke aphasia. J Neurosurg Psychiatry. 2022;93(6):573–581. doi: 10.1136/jnnp-2021-328422.
- Page SJ, Wallace SE. Speech language pathologists’ opinions of constraint-induced language therapy. Top Stroke Rehabil. 2014;21(4):332–338. doi: 10.1310/tsr2104-332.
- Pitt R, Theodoros D, Hill AJ, et al. The development and feasibility of an online aphasia group intervention and networking program – TeleGAIN. Int J Speech Lang Pathol. 2019;21(1):23–36. doi: 10.1080/17549507.2017.1369567.
- Pisano F, Marangolo P. Editorial: new perspectives and methodologies in the diagnosis and rehabilitation of aphasia. Brain Sci. 2021;11(11):1508. doi: 10.3390/brainsci11111508.
- Øra HP, Kirmess M, Brady MC, et al. The effect of augmented speech-language therapy delivered by telerehabilitation on poststroke aphasia—a pilot randomized controlled trial. Clin Rehabil. 2020;34(3):369–381. doi: 10.1177/0269215519896616.
- Knepley KD, Mao JZ, Wieczorek P, et al. Impact of telerehabilitation for stroke-related deficits. Telemed J E Health. 2021;27(3):239–246. doi: 10.1089/tmj.2020.0019.
- Cacciante L, Kiper P, Garzon M, et al. Telerehabilitation for people with aphasia: a systematic review and meta-analysis. J Commun Disord. 2021;92:106111. doi: 10.1016/j.jcomdis.2021.106111.
- Teti S, Murray LL, Orange JB, et al. Telehealth assessments and interventions for individuals with poststroke aphasia: a scoping review. Am J Speech Lang Pathol. 2023;32(3):1360–1375. doi: 10.1044/2023_AJSLP-22-00324.
- Brady MC, Kelly H, Godwin J, et al. Speech and language therapy for aphasia following stroke. Cochrane Database Syst Rev. 2016;2016(6):CD000425. doi: 10.1002/14651858.cd000425.pub4.
- Wenke R, Lawrie M, Hobson T, et al. Feasibility and cost analysis of implementing high intensity aphasia clinics within a sub-acute setting. Int J Speech Lang Pathol. 2014;16(3):250–259. doi: 10.3109/17549507.2014.887777.
- BSI. Ergonomics of human-system interaction. Part 210. Human-centred design for interactive systems (ISO 9241-210:2010). London (UK): British Standards Institution; 2010.
- Spelter B, Corsten S, Diehlmann L, et al. The user-centred design in the development of a platform for teletherapy for people with aphasia. In: Antona M, Stephanidis C, editor. Universal access in human-computer interaction. Novel design approaches and technologies. Vol. 13308. Springer International Publishing; 2022. p. 342–359. doi: 10.1007/978-3-031-05028-2_23.
- Vuong G, Burns CL, Dignam J, et al. Configuration of a telerehabilitation system to deliver a comprehensive aphasia therapy program via telerehabilitation (TeleCHAT): a human-centred design approach. Aphasiology. 2024;0(0):1–32. doi: 10.1080/02687038.2024.2314328.
- Slattery P, Saeri AK, Bragge P. Research co-design in health: a rapid overview of reviews. Health Res Policy Syst. 2020;18(1):17. doi: 10.1186/s12961-020-0528-9.
- Anemaat L. Using experience-based co-design to understand unmet needs and priorities across the continuum of care: a blueprint for aphasia service development [PhD thesis]. Brisbane: The University of Queensland; 2023. doi: 10.14264/795687c.
- Carminati J-YJ, Holth K, Ponsford JL, et al. Co-designing positive behaviour support (PBS + PLUS) training resources: a qualitative study of people with ABI, close-others, and clinicians’ experiences. Brain Impair. 2024;25(2):IB23060. doi: 10.1071/IB23060.
- Marshall J, Roper A, Galliers J, et al. Computer delivery of gesture therapy for people with severe aphasia. Aphasiology. 2013;27(9):1128–1146. doi: 10.1080/02687038.2013.786803.
- Cuperus P, de Kok D, de Aguiar V, et al. Understanding user needs for digital aphasia therapy: experiences and preferences of speech and language therapists. Aphasiology. 2022;37(7):1016–1038. doi: 10.1080/02687038.2022.2066622.
- Swales MA, Hill AJ, Finch E. Feature rich, but user-friendly: speech pathologists’ preferences for computer-based aphasia therapy. Int J Speech Lang Pathol. 2016;18(4):315–328. doi: 10.3109/17549507.2015.1081283.
- World Health Organization. Preferred profile for hearing-aid technology suitable for low- and middle-income countries. Geneva: World Health Organization; 2017. https://iris.who.int/handle/10665/258721.
- Jamieson M, Lennon M, Cullen B, et al. Supporting people with acquired brain injury to use a reminding app; narrow-deep vs. broad-shallow user interfaces. ACM Trans Access Comput. 2022;15(1):1–23. doi: 10.1145/3501275.
- Goodyear-Smith F, Jackson C, Greenhalgh T. Co-design and implementation research: challenges and solutions for ethics committees. BMC Med Ethics. 2015;16(1):78. doi: 10.1186/s12910-015-0072-2.
- Louise L, Annette B. Drawing straight lines along blurred boundaries: qualitative research, patient and public involvement in medical research, co-production and co-design. Evid Policy. 2019;15(3):409–421. doi: 10.1332/174426419X15552999451313.
- Centeno JG, Laures-Gore JS. Intersectionality in aphasia services for ethnosocially diverse adult populations. Semin Speech Lang. 2024;45(1):1–4. doi: 10.1055/s-0043-1778016.
- Mellahn K, Kilkenny M, Siyambalapitiya S, et al. Comparing acute hospital outcomes for people with post-stroke aphasia who do and do not require an interpreter. Top Stroke Rehabil. 2023;31(5):527–536. doi: 10.1080/10749357.2023.2295128.
- Hill AJ, Breslin HM. Refining an asynchronous telerehabilitation platform for speech-language pathology: engaging end-users in the process. Front Hum Neurosci. 2016;10:640. doi: 10.3389/fnhum.2016.00640.
