ABSTRACT
Feeding problems are common in autistic children. They include eating a limited repertoire of foods and often impact on health and quality of life. To examine the experiences of parents of autistic children who have feeding problems, and their service needs. A pragmatic, qualitative research approach was adopted. Six participants were recruited using purposive and snowball sampling. Data was collected via semi-structured interviews. Participants also submitted photographs with captions. These illustrated their child’s feeding problems and the effect on them and their family. Interviews were transcribed. They were analyzed alongside the photos and captions using inductive thematic analysis. Rigor was ensured via member checking, peer review of themes, and reflexive journaling. Five themes emerged. Parents and children found ‘mealtimes difficult.’ Parents were ‘unsure when or whether to pursue help.’ They felt ‘let down by a lack of support.’ ‘Lowered expectations of parents and professionals’ prevailed about their child’s feeding problems. Parents desired ‘services that are easily accessible and supportive.’ This is the first qualitative study of parents’ experiences of feeding problems in autistic children in the UK. It has been the first study to incorporate participatory photography. These problems have a negative impact on the child’s learning and the child’s, and family’s wellbeing. Support needs are largely unmet. This study has provided rich insight into autistic children’s feeding problems. The findings will inform the design of better support for autistic children and their families.
Introduction
AutismFootnote1 is a common neurodevelopmental condition characterized by differences in social interaction, communication, interests, and behavior (American Psychiatric Association, Citation2013). Feeding problems can be defined as “eating-related behaviours and/or symptoms of feeding disorders that are unrelated to weight, shape, and/or body image concerns, yet impair functioning” (Baraskewich, Ranson, McCrimmon, & McMorris, Citation2021). They affect up to 90% of autistic children irrespective of intellectual ability, and often persist into adulthood (Emond, Emmett, Steer, & Golding, Citation2010; Mayes & Zickgraf, Citation2019). Feeding problems are far more pervasive than typical toddler ‘picky eating’ and include disruptive mealtime behaviors, narrow food repertoires, aversion to new foods, and overeating (Ledford & Gast, Citation2006).
Although the reasons for high rates of feeding problems in autistic children are not fully understood (Baraskewich et al., Citation2021), the complexities of the experience of eating likely make it challenging. Eating is an unpredictable sensory-rich experience intertwined with complex social rituals; an autistic child’s social difficulties, preference for sameness, and potential sensory processing difficulties likely make mealtimes less enjoyable and more stressful for them than for non-autistic people (Dovey, Kumari, & Blissett, Citation2019).
Feeding problems impact on health and wellbeing, and participation in family mealtimes and learning activities. Shared family mealtimes are culturally important, and promote healthy eating, social skills, and daily and independent living skills (Backman, Granlund, & Karlsson, Citation2021; Fulkerson, Story, Neumark-Sztainer, & Rydell, Citation2008). The importance of healthy eating is well established: low-quality diets are linked to a lower capacity to learn, poorer mental health (Francis et al., Citation2019; O’Neil et al., Citation2014; Opie, O’Neil, Itsiopoulos, & Jacka, Citation2015), disability and premature death (Afshin et al., Citation2019). Feeding problems often lead to low vitamin and mineral intakes (Ranjan & Nasser, Citation2015); there are case reports of micronutrient deficiencies in feeding problems which have led to vision loss and life-threatening illness (Sharp, Berry, Burrell, Scahill, & McElhanon, Citation2020; Yule et al., Citation2020). Low quality diets established in childhood likely contribute to autistic adults having high rates of diet-related diseases such as diabetes, cardiovascular disease, and mental health disorders, and dying on average 18 years younger than the general population (Autistica, Citation2016; Croen et al., Citation2015; Lai et al., Citation2019).
The NICE clinical guideline CG128: Autism spectrum disorder in under 19s: recognition, referral and diagnosis recognizes feeding problems as common in autistic children and recommends routine assessment for them but makes no recommendations for management (NICE: National Institute for Health and Care Excellence, Citation2011). There is limited evidence on which to base the management of feeding problems. However a recent UK survey of over 800 parents and professionals identified that various interventions tailored by health professionals (including occupational therapists, speech and language therapists and dietitians) were found to be helpful for feeding problems in autistic children and children with neurodisabilities, such as graded exposure, modifying meals or equipment and visual supports (Parr et al., Citation2021).
Qualitative research allows for in-depth exploration of a family’s experience. Previous qualitative studies from Australia, Brazil, Canada, India, South Africa, and the USA have provided rich analysis of nearly 100 parental experiences of their autistic child’s feeding problems. Mealtimes are typically the most stressful and unpleasant time of the day, often with family members eating separately (Adams, Dadabhay, & Neille, Citation2021; Adams, Verachia, & Coutts, Citation2020; Ausderau & Juarez, Citation2013; Marquenie, Rodger, Mangohig, & Cronin, Citation2011; Naik & Vajaratkar, Citation2019; Suarez, Atchison, & Lagerwey, Citation2014). Reactions to being offered new foods include aggressive and self-injurious behavior (Lázaro & Pondé, Citation2017; Marquenie et al., Citation2011; Suarez et al., Citation2014). Parents found that even when they could access professional support, they felt let down and dismissed, with feeding problems not being perceived as an important problem (Burkett, Haggard, van Rafelghem, & Harpster, Citation2021; Rogers, Magill-Evans, & Rempel, Citation2012; Suarez et al., Citation2014).
Incorporation of participant-provided photography is popular in health and social-care related research. It lends itself well to research into issues that are difficult to articulate, in particular parental approaches to food choice and diet-related problems in their families (Burles & Thomas, Citation2014; Johnson, Sharkey, Dean, McIntosh, & Kubena, Citation2011; Martin, Garcia, & Leipert, Citation2010; Power, Citation2003). For participants it can be enjoyable and empowering to share images, for the researcher they can enrich discussion, and they can enhance research impact by generating a richer understanding and empathy in the viewer (Catalani & Minkler, Citation2010).
Understanding the experiences of parents of autistic children is key to designing the best support to reducing the negative impacts on the child and their family, improving the quality of life of all. This research aimed to examine the experiences and service needs of parents of autistic children who have feeding problems. It is the first qualitative study in the UK, and the first internationally to incorporate participatory photography relating to feeding problems in autistic children.
Materials and Methods
Study Design
This was a pragmatic, qualitative, interview and participatory photography study involving parents of autistic children.
Sample
Participants were recruited via adverts in local support groups, specialist schools, clinics, and social media from September to December 2016. Inclusion criteria were 1) primary carer of a child (aged 0–18 years inclusive) who has a diagnosis of autism spectrum disorder or a former diagnosis that this now encompasses such as childhood autism, pervasive developmental disorder not otherwise specified (PDD-NOS) or Asperger syndrome; 2) carers identify their child as having eating or feeding problems; 3) resident in the Lewisham NHS services catchment area in south London, UK. Exclusion criteria were 1) carers of children awaiting an autism spectrum disorder diagnosis; 2) child has a diagnosis of anorexia nervosa or bulimia nervosa (due to the differences in service provision needs of these eating disorders). A purposive and snowball sampling approach was used, with interested participants encouraged to tell eligible friends about the study.
Ethical Considerations
The study was approved by the Coventry University Research Ethics Committee (ref: P38615) and the Clinical Effectiveness department at Lewisham and Greenwich Hospitals NHS Trust (ref: 4278). NHS Health Research Authority Research Ethics Committee review was not needed (Health Research Authority, Citationn.d.). Eligible participants were sent information about the study after responding to adverts. All had the chance to talk to the principle investigator prior to consenting. Participants signed photo release forms to authorize the use of the photos in the study and its dissemination. Signposting to relevant support services was provided to all participants as a debriefing sheet.
Data Collection
Participants were invited to attend either a focus group or semi-structured interview. Six were interested in a focus group. One focus group was arranged but ran as a semi-structured interview after two of the three participants pulled out at the last minute, one due to work commitments, and one due to a medical emergency. After being unable to secure a mutually convenient time for a further focus group the remaining three potential participants plus twelve other respondents were invited to interviews. Five responded to these invitations and were interviewed via telephone. Interviews lasted 45 to 74 minutes and were recorded using a digital recorder and transcribed verbatim. The interview guide is in the supplementary information (box S1).
Participants were invited to provide approximately five captioned photographs illustrating their child’s feeding problems and the effect on them and their family. Instructions on taking photographs were modified from a participatory photography guide, and provided to participants via e-mail (Sutton-Brown, Citation2015). Participants provided 37 photos in total. The photos were then discussed in their interviews.
Demographic data, a 24-hour dietary recall, and autism and eating behavior screening tool scores were collected via parent-administered questionnaires prior to the interviews. These served to confirm eligibility, and to describe type and severity of eating problems.
The tests were selected pragmatically due to being short and easy to self-administer. The 39-item Cambridge University-developed Childhood Autism Spectrum Test (CAST) (Allison et al., Citation2007) aims to identify children aged 4–11 years who are ‘at risk of autism’ (Scott, Baron-Cohen, Bolton, & Brayne, Citation2002). The maximum score is 31 with a cut off for suspicion of autism of 15 (Allison et al., Citation2007). Both eating behavior screening tools have been validated using autistic children. The 10-item Brief Assessment of Mealtime Behavior in Children (BAMBIC) results in scorings across three domains: food refusal, limited variety, and disruptive behavior (Seiverling et al., Citation2016). The 15-item Screening Tool of Feeding Problems in Children (STEP-CHILD) results in scores on six subscales: chewing problems, rapid eating, food refusal, food selectivity, vomiting and stealing food (Seiverling, Hendy, & Williams, Citation2011).
The 24-hour recalls were used pragmatically to calculate Healthy Eating Index-2010 (HEI-2010) scores – a validated measure of diet quality, based on the 2010 Dietary Guidelines for Americans (Guenther et al., Citation2014). US and UK typical intakes and dietary guidelines were considered similar enough for this score to be applied in this study. HEI-2010 consists of twelve scored components that are summed to yield a total score of up to 100. Normative data based on US-wide national food surveys are publicly available and were used as a comparator (Guenther et al., Citation2013, Citation2014; Guenther, Reedy, Krebs-Smith, & Reeve, Citation2008; Guenther, Reedy, Krebs-Smith, Reeve, & Basiotis, Citation2007).
Thematic Analysis
Inductive thematic analysis was carried out as per the methodology of Braun and Clarke (Braun & Clarke, Citation2006). Coding of the verbatim transcripts of the participant interviews, the content of the submitted photographs and the captions of the photographs, was carried out using NVivo Pro 11 software (Qualitative Solutions and Research International, Doncaster, Victoria, Australia) and resulted in 137 identified codes. The supplementary materials contain the initial coding map, and the refined and final themes (figures S1 and S2, table S1).
Rigor
Triangulation of data was incorporated by the inclusion of both interviews and participatory photography; peer checking of themes by the final author, and member checking of themes. Participants were emailed the final themes, and all responded in agreement with them. Throughout the research, the primary investigator kept a reflexive journal and critically examined her influence and positionality, in particular as a clinical pediatric dietitian who had been involved in the management of one of the children.
Results
Sample Characteristics
The six participants were all mothers in their forties. Between them, they have seven autistic children aged 6–13 years old, two girls and five boys (one participant had two autistic children). Their detailed demographics are in below.
Table 1. Demographic characteristics of participants. All names are pseudonyms to protect anonymity.
The autism and eating behavior screening tool scores showed varied autistic and eating behavior profiles for each child. Healthy Eating Index scores ranged from 32 to 48 (out of 100) – all falling below the mean score (55) for children aged 2–17 years in the US National Health and Nutrition Examination Survey (Guenther et al., Citation2013, Citation2013, Citation2014). Full scores are available in the supplementary material in tables S2 and S3.
Thematic Analysis
Five themes were identified from this research:
Difficult mealtimes
Unsure when or whether to pursue help
Lowered expectations of parents and professionals
Feeling let down by a lack of support
Services must be easily accessible and supportive
Theme 1: Difficult Mealtimes
All participants gave rich examples of their children’s feeding problems and the impact they had on them and their families. This theme incorporates four subthemes:
Subtheme 1a: Unusual Eating Habits
All participants described unusual eating routines and habits, including rigidity around the range of foods they would eat, as these photos and their caption exemplifies:
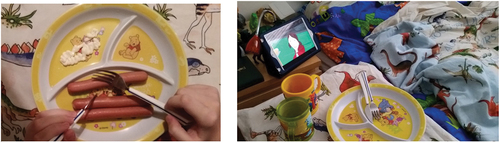
“This first picture shows the main foods that Ben eats. The second is a picture of some toast. […] On a typical day, at the moment in the mornings normally it’s always toast with Nutella, it has to be almost … at the moment it has to be almost cremated … it’s really really burnt […] he’ll like examine it. I have to make sure the burnt side is on the side that hasn’t got the Nutella, because he inspects it basically, underneath, and if it isn’t as burnt he’ll put that bit in the - in the bin. […].” (Becky, caption accompanies )
Others had rigid preferences for where they ate as well as what they ate:
“Frankfurters for breakfast every day. Mayo and fork and knife. No bread. On the table has to be two cups. One animal one with water and dinosaur one with mint tea. On the side table is story played on tablet. It is every day the same set of Fairy Tales volume 2 and 1. Breakfast is always eaten at the small table sitting at her bed.” (Kay, caption accompanies )
The use of separated plates was apparent in three of the six participants’ photos. Participants’ descriptions of mealtimes ranged from boring to chaotic, but none as enjoyable:
“Extremely disruptive, very chaotic, […] he’s very volatile, very unpredictable so sometimes he’ll be, um, you know, screaming. […] he’s very messy […] he’s just you know always got this sort of agitation about him” (Dee about David)
Subtheme 1b: Trying New Food Is Challenging
All participants’ children found new food a challenge. Their responses to new foods ranged from ignoring it to getting really upset.
This photo and caption was of the first time Christopher tried a new dish:
“I can’t count how many times we have tried this. Christopher will get extremely upset, screaming and protesting, pushing everything away. Made me feel like I’m force feeding him. It was very tense for a while and the food was pretty cold in the end but with lots of praise and encouragement, he tried it … .” (Clare, caption accompanies )
Dee explained how particular David is:
“He’ll go through phases of wanting the same meal over and over and over again, then he’ll go back to another sort of common meal that he used to eat but it’s very difficult to introduce new foods to him”
Subtheme 1c: Feeding Problems Affect Children’s Health, Behavior, Learning and Mood
All participants felt that the feeding problems had negative impacts on their children.
Children got very hungry or thirsty due to food refusal and the effects of this varied from struggling to concentrate at school to more challenging behaviors. These quotes are from three different participants:
“He’ll get extremely, um, start having a panic attack and screaming […] he won’t be able to say sometimes that he’s thirsty, he just needs to drink you know and he’ll have extremely violent, angry, aggressive behaviour.” (Dee)
“When she was hungry, she didn’t like to eat anything else and then, when she was hungry she was unbearable. Her behaviour was unbearable. Was frustrated, throwing things, she wasn’t happy with anything. Obviously, because she was hungry. But she refused to eat anything else.” (Kay)
“He was often sort of hungry at school so not being able to work properly and getting quite agitated.” (Jenny)
Two children suffer from chronic severe constipation that their parents attribute to their poor diet and cause their children distress.
Four parents reported that their children became distressed and exhibited challenging behavior when encountering certain foods:
“a smell can kind of completely throw him you know and sort of make him panic almost you know, […] he’d run off generally […] Just escape, escape.” (Jenny)
“he has strong and angry reactions to butter. If he feels– if he thinks– he detects or smells his food and he’ll get quite a bit paranoid actually that there’s butter in there.” (Dee)
Subtheme 1d: Feeding Problems Impact on Parents and Families
All participants reported negative impacts on their and their family’s wellbeing; feeling guilty, exhausted, and worried:
“It’s exhausting. I am so drained and so exhausted. […] it’s almost like having a baby that never grows, […] it’s a constant worry, you know, it’s a constant anxiety to me.” (Dee)
Two participants expressed concerns that their younger children copied their older siblings’ diet and as a result had a poorer dietary variety.
Three participants highlighted that their child’s eating habits affect their entire family in limiting social food related activities. The photograph below and caption
illustrates this:
“This is from a recent holiday. He is resistant to sitting in a big group. The people behind him are his cousins and uncle and aunt, but he would find it hard to sit at the same table as them. Mealtimes are always a stress point on holiday - I get upset because it should be enjoyable but it is never relaxed.” (Jenny, caption accompanies )
Two parents shared a sense of guilt and self-blame for their child’s eating problems:
“The first thing you do is sort of assume that you are making mistakes somehow, or you’re doing something wrong. Um, and I think that did burden us quite a lot for many years really.” (Jenny)
Five of the parents expressed worries about the adequacy of their child’s dietary intake:
“I think he’s physically not getting everything that he should get because he doesn’t eat any fruit or veg, he has no dairy […], it does worry me.” (Becky)
Another participant highlighted the extensive time spent catering for her child’s preferences:
“That could take me about an hour to prepare, cooking the sausages and then you know - and then peeling them, takes about an hour really, and you know, I try to peel them as carefully as I can but obviously some of the sausage gets taken away because there’s peel in them, but yeah, it can take about an hour to do and as soon as I give it to him, he’s like, ‘Mummy I’m finished.’” (Becky, discussion accompanied )
Theme 2: Unsure When or whether to Pursue Help
One parent (Fiona) expressed high satisfaction for the service received and had received help almost uninterrupted since birth due to her child needing tube feeding in infancy.
All the other participants had been unsure when to or whether to seek help from professional services regarding their child’s eating. They were unsure whether their child’s feeding problems were severe enough to seek help, because their weight was not faltering:
“I could never been to the doctor and said, ‘I am worried about Jack’s eating.’ Um, because of, you know he’s never been worryingly underweight or anything like that. […] when you talk about these things, sometimes I feel like I’m still talking about things that are a bit trivial because they’re not, you know, Jack’s not, he’s not malnourished.” (Jenny)
Two participants reported they had considered getting help but had given up, as they did not know how to access help:
“Perhaps I should have tried harder, um, but life was hard enough it was one of the things that probably fell through the net, d’you know what I mean?” (Clare)
“I didn’t ever think, um, I think I was too busy blaming ourselves so I didn’t ever think […] anyone else could help [laughs].” (Jenny)
Theme 3: Lowered Expectations from Parents and Professionals
An underlying reason for being unsure whether to seek help (theme 2) was a lowered expectation for eating habits and dietary quality in autistic children, from parents and sometimes from professionals too:
“Everyone just takes it for granted that your children will eat whatever and, um, you know and you just sort of, I think, ‘oh well, we’ve got a child who doesn’t really and has got a really restrictive [diet].’” (Becky)
“Everybody said, ‘Oh, you know, it’s not too bad because other children, they will eat only, you know, one type of crackers only.’” (Kay)
Parents doubted whether professionals would take their concerns seriously and seemed resigned to dealing with their children’s eating problems without professional help:
“We did seem to sort of muddle through on our own, […] but then it got to a stage where, you know, it’s not good at all, really.” (Becky)
“I thought, ‘well what are they going to say? They’ll say he does eat this and he does eat that.’ […] I just got on with it.” (Clare)
One parent recalled a time when she had sought help during her child’s annual check by the pediatrician in her school:
“She was in a period that she has eaten like ten eggs a day and she didn’t like to eat anything else. And one of the doctors in, uh, one, um, one of the consultations, um, I said, you know, she’s eating all the time the-the eggs and he said, ‘You know, it’s fine. You don’t have to worry about it.’” (Kay)
Theme 4: Feeling Let down by a Lack of Support
Other than the one parent who felt she had had excellent support all through her child’s life, all parents felt there was a lack of available support, and had a feeling of being let down:
“I haven’t seen anybody about him, I’ve just done everything indoors, just pulled my hair out now and again to my husband.” (Clare)
“I would like it if I went to the doctor with any concerns that they would take that seriously.” (Jenny)
One parent expressed frustration with the dietetic service (the primary investigator’s clinic). She was referred but was put on a long waiting list and was never offered an appointment. Another felt let down by the same service:
“I had one appointment and because he didn’t really have any problems, they discharged him from the [dietetic] service. […] because their service was so stretched” (Clare)
Another parent was disappointed that her child’s school hadn’t let her know that her child had not been eating well for many years:
“He didn’t have packed lunch until he was about, I think it was when he was about eight. I suddenly sort of realised that he wasn’t, he hadn’t been eating school dinners at all.” (Jenny)
Theme 5: Services Must Be Easily Accessible and Supportive
When asking parents about which services they desired, many struggled, partly because many were not sure if their child’s eating warranted help. Others doubted how helpful any support could be:
“I’m not prepared to stand here and cook four dinners, either. Do you know what I’m saying? For each one of them to go in the bin? So, um– I don’t know if that sounds really harsh, but I suppose that’s what I-I-I-I- I don’t want, um– When someone tells me ‘do this,’ or ‘do that,’ I might not have took to that. Does that make sense?” (Clare)
The data is arranged into the different services discussed by parents below:
Subtheme 5a: The Role of School
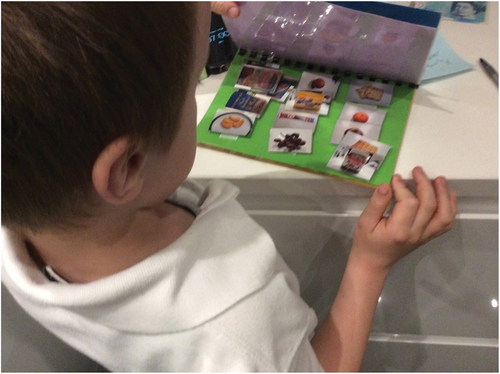
Four parents talked about potential and previous support from schools. One parent highlighted that her child’s mainstream school could have helped with his eating: better monitoring of intake at mealtimes; modification to his mealtime environments; and improved food quality provision. Three parents felt their child’s schools had helped to find ways to manage underlying issues related to eating, for example introducing pictorial choice resources around food (see photo below ()), and help in writing social stories:
Figure 6. One of Clare’s photos, with the caption “Carl is hungry and choosing food from his picture book.”
Two parents reported that food technology sessions were successful in helping their children try new food in their respective schools:
“Food tech is certainly helping, because she’s cooking different meals and she’s done a stir fry this week with green peppers. They did that on Monday, and she’s eaten some of it! I can’t believe it, wonderful! Onions and green peppers in this stir fry, and she’s eating it, it’s fantastic! So, if she’s cooking it, she’ll eat it.” (Fiona)
Subtheme 5b: A ‘Super-nanny’ Service
Two parents discussed how helpful a one-to-one home visit service would be:
“In any of it, not just food, when they’re having a meltdown, when you can’t get them to bed, you just want someone to come in and help you.” (Clare)
Subtheme 5c: Group Sessions
The option of group sessions to help with their children’s eating problems was discussed by a few parents, and there was mixed feelings about this. One felt these would be very useful and she would be keen to attend, to share experiences with others that understood. Two felt groups were great in theory but would be unable to attend due to work and childcare:
“Just meeting other, sort of, parents new to the area or whatever who’s going through the same, same thing as what we are really would be, would be useful, yeah.” (Becky)
“I found it very difficult to access courses, um, you know, without, you know, childcare, you know, that’s always been the problem because it’s, you know, they’re extremely needy– they have extreme needs, you know. So it’s very difficult.” (Clare)
Subtheme 5d: Online Help
Access to online help was explored with some parents. One would not use this due to not liking being online, however two were interested, particularly as access would be flexible alongside work commitments:
“Groups and yeah, exactly, as I say, I mean I would attend but obviously would be in, you know, I’d have to, you know, be d-dependant on whether my work, working and that so it might be that I’ll be out all day - Yeah, videos and things that’s easy accessible would be, um, would be useful as well.” (Becky)
Another felt that curated content would be great, as she often sought help online but:
“I feel very overwhelmed when I look online. I find it very, a very, exhausting process - it’s like information overload.” (Dee)
Discussion
This study aimed to explore the experiences and service needs of parents of autistic children who have feeding problems. Six participants provided rich and detailed accounts and photographs depicting varied problems associated with their children’s eating. Consistent with previous quantitative and qualitative studies the participants’ children had rigid food preferences, and found trying new foods challenging (Adams et al., Citation2021, Citation2020; Ausderau & Juarez, Citation2013; Burkett et al., Citation2021; Emond et al., Citation2010; Lázaro & Pondé, Citation2017; Ledford & Gast, Citation2006; Marquenie et al., Citation2011; Mayes & Zickgraf, Citation2019; Naik & Vajaratkar, Citation2019; Rogers et al., Citation2012; Suarez et al., Citation2014). The impacts on the participants’ children included stress, constipation, reduced participation in family mealtimes, and struggling to concentrate at school. Furthermore, all of the children had Healthy Eating Index scores below the population average for children, indicating a low dietary quality, with some scores so low, due to a lack of variety and lack of inclusion of foods from specific food groups, as to pose a risk to health (Guenther et al., Citation2013, Citation2014, Citation2008, Citation2007).
Families are an interactive unit, what affects one member affects them all (Beckett, Citation1973; Goldenberg, Goldenberg, & Stanton, Citation2016). In our study parents experienced worry, guilt, and increased time spent on food preparation; siblings copied problematic eating behaviors; and enjoyment of family mealtimes was reduced or absent. Our findings resonate with the findings of previous researchers of ‘unfilled hopes for mealtimes being quality family time’ (Suarez et al., Citation2014); and the absence of enjoyment in mealtimes (Adams et al., Citation2020; Ausderau & Juarez, Citation2013; Burkett et al., Citation2021; Lázaro & Pondé, Citation2017; Marquenie et al., Citation2011; Naik & Vajaratkar, Citation2019; Suarez et al., Citation2014).
Parents of children with disabilities are observed to adapt to their challenges in four modes – normalization, crusadership, altruism, or resignation to a problematic existence (Darling, Citation1979). Resignation is most common in parents who feel isolated from support from peers and professionals (Seligman & Darling, Citation2007). In our study, many participants had been unsure whether to seek help for their children and were in resignation mode in accepting problematic mealtimes.
Our study has uncovered insight into not just the micro level of the functioning and occupation of the child and their family, but also the meso level of relationships with professionals and their child’s schools. When some participants had sought help, they felt dismissed by health professionals. The difficulties in finding any help and indeed the right help (themes 2,3 and 4) echo findings in previous studies of parents searching for answers, giving up on family mealtimes, and seeking support but being dismissed (Lázaro & Pondé, Citation2017; Rogers et al., Citation2012; Suarez et al., Citation2014). Parents of disabled children often feel anomie, powerlessness, exacerbated by poor professional support (Seligman & Darling, Citation2007). At the root of this may be professionals’ lack of role-taking ability – the ability to see a situation from the parent’s perspective – which can often lead to professionals appearing insensitive, even to the point of causing parents to be reluctant to seek help again in the future (Seligman & Darling, Citation2007).
Our study has touched on the potential of schools in helping with the identification of and management of feeding problems. According to systems theory, boundaries exist around a family unit, and that boundary can be more or less permeable to outside help and influence (Beckett, Citation1973). Effective families develop a balance between the closed self-containment that can be needed to effectively manage a disability, and enough openness to take advantage of useful outside help (Darling, Citation1979; Seligman & Darling, Citation2007). Schools and school-based therapists such as occupational therapists are ideally placed to work at the micro level, permeating these boundaries; the meso level, linking families to health professionals and other sources of support; and the macro level in raising awareness of the impact of feeding problems and the need for better support.
It is widely accepted that feeding problems are common in autistic children (NICE: National Institute for Health and Care Excellence, Citation2011). Our study adds to the rich understanding that qualitative studies proffer on how this affects children and their families, and starkly illustrates this via the participants’ photographs.
Strengths and Limitations of the Study
This study provides rich insight into the experiences of parents of seven autistic children with feeding problems; however, the study sample was homogeneous – all participants were mothers in their forties and most mothers and children were White British, therefore their experiences may not represent those of the diverse population of families caring for autistic children. These limitations were largely mitigated against: an experienced team supervised the study, and various strategies of triangulation and reflexivity were incorporated into the study to optimize its rigor (Guba & Lincoln, Citation1989). In qualitative research, the aim is not for large sample sizes but instead for data saturation (Fusch & Ness, Citation2015; Kerr, Nixon, & Wild, Citation2010) Several factors suggest data saturation was reached in this study: The data collected was rich, including both in-depth interviews and participatory photography; the sample was relatively homogenous; and the findings were aligned with previously published research.
Clinical Implication of Results and Future Steps
This study suggests that:
1.Parents with autistic children and feeding problems may be unsure when or whether to seek help
2.Both parents and professionals can be dismissive of feeding problems
3.When parents do seek help, accessible services aren’t always available
Clear guidance on when feeding problems warrant professional help is needed, education of professionals on the far-reaching impact of feeding problems, and accessible and sympathetic support provided.
Conclusions
In summary, this research examined the experiences and service needs of parents of autistic children who have feeding problems. In rich data from a sample of six mothers of seven autistic children, it was found that mealtimes are difficult, and affect both the children’s and parent’s health and wellbeing, and can affect the child’s ability to concentrate at school. Parents are often unsure when or whether to pursue help and feel let down by a lack of support; both parents and professionals may have lowered expectations of autistic children’s eating habits and dietary intake; and desired services must be easily accessible and supportive. These findings are the first of their kind in the UK and concur with other published findings.
The findings of this study add to the evidence-base that feeding problems have a significant impact on autistic children and their families. Professionals and parents need to examine and challenge any low expectations of feeding and diet quality in autistic children. Accessible, high quality services and raised expectations are needed in order for children to thrive and for parents to feel supported rather than let down.
Authorship
This work was carried out for ZLC’s MRes for which DL was her main supervisor and KHP and RK additional supervisors. ZLC, KHP, RK, and DL were involved in the initial conceptualisation of the study. ZLC conducted the interviews and analysed interviews, analysed, and interpreted the data. DL provided peer review of the data analysis and interpretation. ZLC wrote the paper. DL reviewed the paper. All authors read and approved the final manuscript submitted for publication.
Acknowledgments
We thank the parents who took part in this study and Health Education England (HEE) and the National Institute of Health Research (NIHR) for funding the principal investigator and supervisors’ time via an Integrated Clinical Academic MRes studentship. Thank you to Sarah Cooke and Sally Brothers, Dietetic Department, Lewisham Hospital for their support as clinical supervisor and department head respectively. Thank you to Professor Jacqueline Blissett, Aston University, for her help in revising this paper.
Disclosure Statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes
1 This article uses identity-first language throughout i.e. autistic children to respect the preference of many autistic people (Kenny et al., Citation2016; National Autistic Society, Citationn.d.).
References
- Adams, S., Dadabhay, A., & Neille, J. (2021). An exploration into mothers’ experiences of feeding children with autism spectrum disorder in South Africa. Folia Phoniatrica Et Logopaedica, 73(3), 164–173. doi:10.1159/000507928
- Adams, S., Verachia, R., & Coutts, K. (2020). ‘A blender without the lid on’: Mealtime experiences of caregivers with a child with autism spectrum disorder in South Africa. South African Journal of Communication Disorders, 67(1), 1–9. doi:10.4102/sajcd.v67i1.708
- Afshin, A., Sur, P. J., Fay, K. A., Cornaby, L., Ferrara, G., Salama, J. S., … Murray, C. J. L. (2019). Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the global burden of disease study 2017. The Lancet, 393(10184), 1958–1972. doi:10.1016/S0140-6736(19)30041-8
- Allison, C., Williams, J., Scott, F., Stott, C., Bolton, P., Baron-Cohen, S., & Brayne, C. (2007). The childhood asperger syndrome test (CAST): Test-retest reliability in a high scoring sample. Autism : The International Journal of Research and Practice, 11(2), 173–185. doi:10.1177/1362361307075710
- American Psychiatric Association. 2013. Diagnostic and statistical manual of mental disorders: DSM-5 5th. Arlington, VA: Author. doi:10.1176/appi.books.9780890425596.744053
- Ausderau, K., & Juarez, M. (2013). The impact of autism spectrum disorders and eating challenges on family mealtimes. Infant, Child, and Adolescent Nutrition, 5(5), 315–323. doi:10.1177/1941406413502808
- Autistica. (2016). Personal tragedies, public crisis The urgent need for a national response to early death in autism. https://www.autistica.org.uk/wp-content/uploads/2016/03/Personal-tragedies-public-crisis.pdf
- Backman, E., Granlund, M., & Karlsson, A.-K. (2021). Parental perspectives on family mealtimes related to gastrostomy tube feeding in children. Journal of Paediatric Nursing, 58, 53–59. doi:10.1177/1049732321997133
- Baraskewich, J., Ranson, K. M. V., McCrimmon, A., & McMorris, C. A. (2021). Feeding and eating problems in children and adolescents with autism: A scoping review. Autism, 25(6), 1505. doi:10.1177/1362361321995631
- Beckett, J. A. (1973). General systems theory, psychiatry and psychotherapy. International Journal of Group Psychotherapy, 23(3), 292–305. doi:10.1080/00207284.1973.11492234
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. May 2015. 10.1191/1478088706qp063oa
- Burkett, K., Haggard, M., van Rafelghem, D., & Harpster, K. (2021). Restricted eating in preschoolers with autism: Mother stressors and solutions. Journal of Autism and Developmental Disorders. doi:10.1007/S10803-021-05078-6
- Burles, M., & Thomas, R. (2014). “I just don’t think there’s any other image that tells the story like [this] picture does”: Researcher and participant reflections on the use of participant-employed photography in social research. International Journal of Qualitative Methods, 13(1), 185–205. doi:10.1177/160940691401300107
- Catalani, C., & Minkler, M. (2010). Photovoice: A Review of the literature in health and public health. Health Education & Behavior, 37(3), 424–451. doi:10.1177/1090198109342084
- Croen, L. A., Zerbo, O., Qian, Y., Massolo, M. L., Rich, S., Sidney, S., & Kripke, C. (2015). The health status of adults on the autism spectrum. Autism, 19(7), 814–823. doi:10.1177/1362361315577517
- Darling, R. B. (1979). Families against society: A study of reactions to children with birth defects. Beverley Hills & London: Sage.
- Dovey, T. M., Kumari, V., & Blissett, J. (2019). Eating behaviour, behavioural problems and sensory profiles of children with avoidant/restrictive food intake disorder (ARFID), autistic spectrum disorders or picky eating: Same or different? European Psychiatry, 61, 56–62. doi:10.1016/j.eurpsy.2019.06.008
- Emond, A., Emmett, P., Steer, C., & Golding, J. (2010). Feeding symptoms, dietary patterns, and growth in young children with autism spectrum disorders. Pediatrics, 126(2), e337–e342. doi:10.1542/peds.2009-2391
- Francis, H. M., Stevenson, R. J., Chambers, J. R., Gupta, D., Newey, B., Lim, C. K., & Matsuoka, Y. J. (2019). A brief diet intervention can reduce symptoms of depression in young adults – A randomised controlled trial. PLOS ONE, 14(10), e0222768. doi:10.1371/journal.pone.0222768
- Fulkerson, J. A., Story, M., Neumark-Sztainer, D., & Rydell, S. (2008). Family meals: Perceptions of benefits and challenges among parents of 8- to 10-year-old children. Journal of the American Dietetic Association, 108(4), 706–709. doi:10.1016/j.jada.2008.01.005
- Fusch, P. I., & Ness, L. R. (2015). Are we there yet? Data saturation in qualitative research. The Qualitative Report, 20(9), 1408–1416. h t tps://d o i.o rg/1,1408-1416
- Goldenberg, H., Goldenberg, I., & Stanton, M. (2016). Family therapy: An overview (9th ed.). Pacific Grove, CA: Brooks Cole.
- Guba, E. G., & Lincoln, Y. S. (1989). Fourth generation evaluation. Thousand Oaks, CA: SAGE Publications. http://opac.rero.ch/get_bib_record.cgi?db=ne&rero_id=1643937
- Guenther, P. M., Casavale, K. O., Reedy, J., Kirkpatrick, S. I., Hiza, H. A. B., Kuczynski, K. J., Krebs-Smith, S. M. (2013). Update of the healthy eating index: HEI-2010. Journal of the Academy of Nutrition and Dietetics, 113(4), 569–580. doi:10.1016/j.jand.2012.12.016
- Guenther, P. M., Kirkpatrick, S. I., Krebs‐Smith, S. M., Reedy, J., Buckman, D. W., Dodd, K. W., & Carroll, R. J. (2013). Evaluation of the Healthy Eating Index‐2010 (HEI‐2010). The FASEB Journal, 27(S1), 230.5–230.5. doi:10.1096/FASEBJ.27.1_SUPPLEMENT.230.5
- Guenther, P. M., Kirkpatrick, S. I., Reedy, J., Krebs-Smith, S. M., Buckman, D. W., Dodd, K. W., Carroll, R. J. (2014). The healthy eating index-2010 is a valid and reliable measure of diet quality according to the 2010 dietary guidelines for Americans. The Journal of Nutrition, 144(3), 399–407. doi:10.3945/jn.113.183079
- Guenther, P. M., Reedy, J., Krebs-Smith, S. M., & Reeve, B. B. (2008). Evaluation of the healthy eating index-2005. Journal of the American Dietetic Association, 108(11), 1854–1864. doi:10.1016/j.jada.2008.08.016
- Guenther, P. M., Reedy, J., Krebs-Smith, S. M., Reeve, B. B., & Basiotis, P. P. (2007). Development and evaluation of the healthy eating index-2005: Technical report. http://www.cnpp.usda.gov/HealthyEatingIndex.htm
- Health Research Authority. (n.d.). Do I need NHS Ethics approval? Retrieved September 20, 2021, from http://www.hra-decisiontools.org.uk/ethics/
- Johnson, C. M., Sharkey, J. R., Dean, W. R., McIntosh, W. A., & Kubena, K. S. (2011). It’s who I am and what we eat: Mothers’ food-related identities in family food choice. Appetite, 57(1), 220. doi:10.1016/J.APPET.2011.04.025
- Kenny, L., Hattersley, C., Molins, B., Buckley, C., Povey, C., & Pellicano, E. (2016). Which terms should be used to describe autism? Perspectives from the UK autism community. Autism, 20(4), 442–462. doi:10.1177/1362361315588200
- Kerr, C., Nixon, A., & Wild, D. (2010). Assessing and demonstrating data saturation in qualitative inquiry supporting patient-reported outcomes research. Expert Review of Pharmacoeconomics & Outcomes Research, 10(3), 269–281. doi:10.1586/erp.10.30
- Lai, M. C., Kassee, C., Besney, R., Bonato, S., Hull, L., Mandy, W., Ameis, S. H. (2019). Prevalence of co-occurring mental health diagnoses in the autism population: A systematic review and meta-analysis. The Lancet Psychiatry, 6(10), 819–829. doi:10.1016/S2215-0366(19)30289-5
- Lázaro, C. P., & Pondé, M. P. (2017). Narratives of mothers of children with autism spectrum disorders: Focus on eating behavior. Trends in Psychiatry and Psychotherapy, 39(3), 4–11. doi:10.1590/2237-6089-2017-0004
- Ledford, J. R., & Gast, D. L. (2006). Feeding problems in children with autism spectrum disorders: A review. Focus on Autism and Other Developmental Disabilities, 21(3), 153–166. doi:10.1177/10883576060210030401
- Marquenie, K., Rodger, S., Mangohig, K., & Cronin, A. (2011). Dinnertime and bedtime routines and rituals in families with a young child with an autism spectrum disorder. Australian Occupational Therapy Journal, 58(3), 145–154. doi:10.1111/j.1440-1630.2010.00896.x
- Martin, N., Garcia, A. C., & Leipert, B. (2010). Photovoice and its potential use in nutrition and dietetic research. Canadian Journal of Dietetic Practice and Research, 71(2), 93–97. doi:10.3148/71.2.2010.93
- Mayes, S. D., & Zickgraf, H. (2019). Atypical eating behaviors in children and adolescents with autism, ADHD, other disorders, and typical development. Research in Autism Spectrum Disorders, 64, 76–83. doi:10.1016/j.rasd.2019.04.002
- Naik, S., & Vajaratkar, P. (2019). Understanding parents’ difficulties in executing activities of daily living of children with autism spectrum disorder: A qualitative descriptive study. The Indian Journal of Occupational Therapy, 51(3), 107. doi:10.4103/ijoth.ijoth_22_19
- National Autistic Society. (n.d.). How to talk about autism. Retrieved March 19, 2021, from https://www.autism.org.uk/what-we-do/help-and-support/how-to-talk-about-autism
- NICE: National Institute for Health and Care Excellence. (2011). Guideline CG128: Autism in under 19s: Recognition, referral and diagnosis. London, UK: NICE. https://www.nice.org.uk/Guidance/CG128
- O’Neil, A., Quirk, S. E., Housden, S., Brennan, S. L., Williams, L. J., Pasco, J. A., Jacka, F. N. (2014). Relationship between diet and mental health in children and adolescents: A systematic review. American Journal of Public Health, 104(10), e31–e42. doi:10.2105/AJPH.2014.302110
- Opie, R. S., O’Neil, A., Itsiopoulos, C., & Jacka, F. N. (2015). The impact of whole-of-diet interventions on depression and anxiety: A systematic review of randomised controlled trials. Public Health Nutrition, 18(11), 2074–2093. doi:10.1017/S1368980014002614
- Parr, J., Pennington, L., Taylor, H., Craig, D., Morris, C., McConachie, H., Colver, A. (2021). Parent-delivered interventions used at home to improve eating, drinking and swallowing in children with neurodisability: The feeds mixed-methods study. Health Technology Assessment, 25(22), 1–208. doi:10.3310/HTA25220
- Power, E. M. (2003). De-Centering the text: Exploring the potential for visual methods in the sociology of food. Journal for the Study of Food and Society, 6(2), 9–20. doi:10.2752/152897903786769670
- Ranjan, S., & Nasser, J. A. (2015). Nutritional status of individuals with autism spectrum disorders: Do we know enough? Advances in Nutrition, 6(4), 397. doi:10.3945/AN.114.007914
- Rogers, L. G., Magill-Evans, J., & Rempel, G. R. (2012). Mothers’ challenges in feeding their children with autism spectrum disorder-managing more than just picky eating. Journal of Developmental and Physical Disabilities, 24(1), 19–33. doi:10.1007/s10882-011-9252-2
- Scott, F. J., Baron-Cohen, S., Bolton, P., & Brayne, C. (2002). The CAST (childhood asperger syndrome test): preliminary development of a UK screen for mainstream primary-school-age children. Autism, 6(1), 9–31. doi:10.1177/1362361302006001003
- Seiverling, L., Hendy, H. M., & Williams, K. (2011). The screening tool of feeding problems applied to children (STEP-CHILD): Psychometric characteristics and associations with child and parent variables. Research in Developmental Disabilities, 32(3), 1122–1129. doi:10.1016/j.ridd.2011.01.012
- Seiverling, L. J., Williams, K. E., Hendy, H. M., Adams, K., Fernandez, A., Alaimo, C., Hart, S. (2016). Validation of the brief assessment of mealtime behavior in children (BAMBIC) for children in a non-clinical sample. Children’s Health Care, 45(2), 165–176. doi:10.1080/02739615.2014.979925
- Seligman, M., & Darling, R. B. (2007). Ordinary families, special children: A systems approach to childhood disability (3rd ed.). New York: Guilford Press.
- Sharp, W. G., Berry, R. C., Burrell, L., Scahill, L., & McElhanon, B. O. (2020). Scurvy as a sequela of avoidant-restrictive food intake disorder in autism: A systematic review. Journal of Developmental and Behavioral Pediatrics JDBP, 41(5), 397–405. doi:10.1097/DBP.0000000000000782
- Suarez, M. A., Atchison, B. J., & Lagerwey, M. (2014). Phenomenological examination of the mealtime experience for mothers of children with autism and food selectivity. American Journal of Occupational Therapy, 68(1), 102–107. doi:10.5014/ajot.2014.008748
- Sutton-Brown, C. A. (2015). Photovoice: A methodological guide. Photography and Culture, 7(2), 169–185. 10.2752/175145214X13999922103165
- Yule, S., Wanik, J., Holm, E. M., Bruder, M. B., Shanley, E., Sherman, C. Q., Ziff, M. (2020). Nutritional deficiency disease secondary to ARFID symptoms associated with autism and the broad autism phenotype: a qualitative systematic review of case reports and case series. Journal of the Academy of Nutrition and Dietetics, 121(3), 467–492. doi:10.1016/j.jand.2020.10.017