ABSTRACT
Inflammatory bowel disease (IBD) is characterized by chronic intestinal inflammation that includes Crohn´s disease (CD) and ulcerative colitis (UC). Although the etiology is still unknown, some specific factors have been directly related to IBD, including genetic factors, abnormal intestinal immunity, and/or gut microbiota modifications. Recent findings highlight the primary role of the gut microbiota closely associated with a persistent inappropriate inflammatory response. This gut environment of dysbiosis in a susceptible IBD host can increasingly worsen and lead to colonization and infection with some opportunistic pathogens, especially Clostridium difficile. C. difficile is an intestinal pathogen considered the main cause of antibiotic-associated diarrhea and colitis and an important complication of IBD, which can trigger or worsen an IBD flare. Recent findings have highlighted the loss of bacterial cooperation in the gut ecosystem, as well as the pronounced intestinal dysbiosis, in patients suffering from IBD and concomitant C. difficile infection (CDI). The results of intestinal microbiota studies are still limited and often difficult to compare because of the variety of disease conditions. However, these data provide important clues regarding the main modifications and interrelations in the complicated gut ecosystem to better understand both diseases and to take advantage of the development of new therapeutic strategies. In this review, we analyze in depth the gut microbiota changes associated with both forms of IBD and CDI and their similarity with the dysbiosis that occurs in CDI. We also discuss the metabolic pathways that favor the proliferation or decrease in several important taxa directly related to the disease.
Introduction
Clostridium (Clostridioides) difficile is a worldwide public health concern and is considered the major cause of antibiotic-associated infections in healthcare settings. It is responsible for serious outbreaks of hospital-acquired infections and for several sporadic diarrheas in the community. The pathogen is a sporulating, strictly anaerobic bacterium, and transmission occurs mainly by the fecal-oral route. Intestinal colonization and toxin production are necessary to trigger the infection; therefore, the disease is strongly related to the disruption of the gut microbiomeCitation1.
Inflammatory bowel disease (IBD) is a chronic disease of mainly the intestinal tract that includes ulcerative colitis (UC) and Crohn´s disease (CD). UC is a diffuse, continuous, and nonspecific inflammation of the colonic mucosa proximal to the rectum. Crohn´s disease is a chronic granulomatous inflammation that affects the entire digestive tract, especially the ileocaecum and perianal regions. While the cause of both disease forms is still unknown, some specific factors have been directly related to IBD, including genetic factors, abnormal intestinal immunity, and gut microbiota modifications directly caused by diet or infections.Citation2
Patients suffering from IBD are particularly susceptible to C. difficile infection (CDI), with an increase in morbidity and mortality.Citation3 Even if it is not clear if IBD itself or disease activity is an independent risk factor for CDI,Citation3,Citation4 further predisposing and specific conditions have been suggested in these patients,Citation3 including colectomy and ileal-anal pouch anastomosis,Citation5 nonsteroidal anti-inflammatory drugs,Citation6 proton pump inhibitors, and other immunosuppressant treatments.Citation7 Recurrence of CDI is common in IBD,Citation8 and in the most complicated cases, only gut ecosystem restoration by fecal microbiota transplantation can help to break the cycle of recurrence.Citation9 In the last decade, the availability of new omic technologies has allowed the investigation of gut microbial communities to identify whether any change in the bacterial composition is involved in CDI or an IBD flare.
This review analyses all the latest findings about the specific role of the gut microbiota composition in intestinal inflammation and infection. We will also focus on the decrease in gut diversity and its causative role in the development of CDI in patients suffering from IBD. Finally, we will link all these modifications in the gut with the production of microbial metabolites and their role in the worsening of CDI and IBD.
A brief history of concomitant CDI and IBD
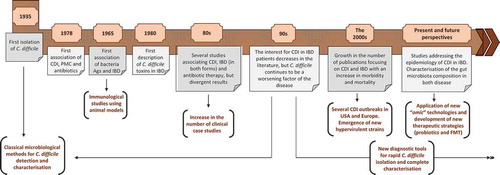
The history of C. difficile dates back to 1935 (), when the bacterium was isolated for the first time from the feces of breastfed infants.Citation10 Despite the interest that the bacterium aroused in the following years, it was not until 1978 that it was first associated with pseudomembranous colitis and previous antibiotic therapy.Citation11,Citation12 First, immunological studies of ulcerative colitis observed the increase in anti-colon antibody titers due not only to chronic colon alteration, but also to unrelated gastrointestinal diseases, such as those caused by C. difficile, Staphylococcus aureus, Forsman antigen or Escherichia coli (E. coli) 014. These early findings showed that some antigens, especially those from E. coli 014, may contribute to colon autoimmunity in ulcerative colitis through disruption of tolerance.Citation13 In 1980, two studies that were published in the literature almost simultaneously described for the first time the presence of C. difficile toxins in patients with IBD during a symptomatic relapse and suggested the association of these toxins with further complications in chronic disease or even with an IBD flare.Citation14,Citation15 In the following years, several other reports documented the possible association between CDI and IBD, and different studies began to investigate more specifically the role of C. difficile and its toxins, differentiating patients with UC and CD, although the results were not always the same or conclusive.Citation16–Citation18 Some studies directly associated the bacterium with toxic megacolon, acute relapses of IBD and/or hospital admissions.Citation19,Citation20 However, other further studies began to question the role of C. difficile in both forms of IBD, suggesting that the bacterium could be a part of the bowel gut, without specific cytopathic effects in the intestinal tissues of these patients, and that it would be relevant in only specific cases with previous antimicrobial therapies.Citation21,Citation22 The diversity in C. difficile detection methods used at the time varied greatly among the different studies, and they were not always as sensitive as needed.Citation23 Furthermore, clinical evidence of the role of C. difficile in IBD patients was scarce.Citation24
During the 1990s, a few studies were published reporting the presence of toxigenic C. difficile in the feces of IBD patients, with a prevalence that varied strongly up to 32%, and they described an exacerbation of the disease with the presence of the bacterium.Citation25,Citation26 However, it was not until the 2000s when there is an important growth in the number of publications that focused repeatedly on the impact of CDI in patients with IBD.Citation27–Citation29 This growing interest concurred with several outbreaks of CDI in hospitals in Europe and in the United States, and it is at this moment when C. difficile went from being an intestinal pathogen associated with antibiotic therapy to being the most important cause of nosocomial diarrhea in humans.Citation30 Therefore, it seems logical that the IBD population was also increasingly affected by this pathogen, as reflected in the literature, with significant morbidity and mortality.Citation31 Other additional but not mutually exclusive possibilities to explain the increase in the incidence of CDI in IBD patients in the last two decades are the evolution of the detection methods for the bacterium, the rapid diagnosis of the infection and a change in the epidemiology, with the emergence of new, best adapted, hypervirulent, and multidrug-resistant strains.Citation32,Citation33
In addition to epidemiological and clinical studies addressing the impact of CDI in IBD patients, in the last decade, several studies have investigated the interplay between the gut microbiota and disease. Advances in culture-independent molecular methods have allowed the identification of these bacterial populations present in the gut at each phase of the disease, which is followed by the use of new promising therapies, such as fecal microbiota transplantation or diet strategies (including prebiotics and probiotics), to successfully treat both of the diseases.
Gut microbial community imbalances in human IBD
In IBD patients, intestinal tissue alteration by bacteria and/or inflammation results in a favorable environment with readily available nutrient sources leading to important perturbations in the normal composition of gut bacteria, in their functions, and finally in their metabolism. These alterations are potential precursors of other concomitant infections, including not only CDI but also other bacterial enteric pathogens, e.g., cytomegalovirus, enteroviruses, Mycoplasma pneumoniae, and upper respiratory viruses, and Entamoeba histolytica, among others. This perturbation finally triggers an important relapse or exacerbation of IBD symptoms.Citation34
The results of intestinal microbiota studies are often difficult to compare due to different factors, including patient´s variability or the analysis methods and techniques used. Different sequencing technologies, annotation tools, and statistical analysis have been developed to study the microbial diversity and changes in the gut ecosystem. Several recent reviews on metagenomics (from sampling to data analysis) are already available in the literatureCitation35 and they show the need for a standardization of analysis techniques and workflows, in order to avoid variability in the results related to the methodology of the study.
Regarding patients, the variety of disease treatments (such as surgical interventions, anti-inflammatory drugs, biologics, immunosuppressant treatments, corticosteroids, proton pump inhibitors or antibiotics) and the demographical characteristics of the study population (gender, age, other overlapping syndromes, diet, smoking history, etc.) could have a direct impact on the results obtained.Citation36–Citation39 For example, it was reported that liver diseases could be the primary factors associated with disease-specific dysbiotic influences of IBD patients.Citation36 Disease phenotypes (including IBD extent or activity) have also been associated with important changes in the gut mucosa, especially in CD,Citation39 while other study observed no significant changes in the gut microbiota of UC patients after the use of biologic treatment (infliximab, adalimumab, or golimumab).Citation36 Other described factors that influence the intestinal bacterial structure are the sample origin (stool or biopsy), as well as the biopsy location, which can induce other changes.Citation37,Citation38 In this context, it has been observed that the microbial imbalance due to intestinal inflammation is not always reflected in the lumen or in the stool. Therefore, a complementary analysis of tissue biopsies would be necessary to identify disease biomarker signals.Citation40
Despite all these interindividual, sample, or methodological factors, the recovery of consistent changes in the bacterial composition, which are repeatedly reported in different studies investigating IBD patients, can highlight disease-specific bacterial signatures. It has also been suggested that changes in gut bacterial communities are not only a consequence of inflammation but also possible primary factors in disease.Citation37 These changes could be interpreted as promising biomarkers, noninvasive diagnostic tools or new therapeutic approaches.
Ulcerative colitis
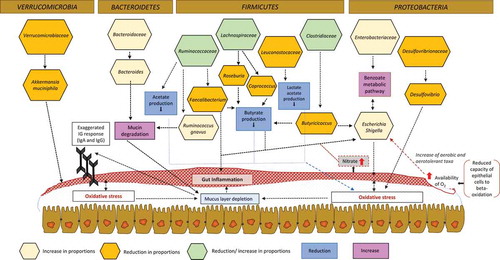
General disruption of gut homeostasis in patients with UC is characterized by a depleted mucous layer (loss of mucus-containing goblet cells), a decrease in microbial alpha diversity,Citation36,Citation41 an increase in bacterial penetration, and an exaggerated Ig response, especially for IgA and IgG.Citation37 Recently, all these changes were observed in both inflamed and non-inflamed intestinal sections of pediatric UC patients, suggesting that they are not a result of inflammation but rather precede (and probably promote) the disease.Citation37 However, it remains unclear if the decrease in bacterial diversity is the cause or the result of the depleted mucus layer.Citation37 Differences in bacterial diversity have been found when UC groups are compared with control individuals.Citation36,Citation41,Citation42 The global microbiota composition was shifted by the presence of UC, with a reduced number of species and diminished richness and evenness, with an alteration in the community composition and structure.Citation41 However, these findings can also be observed in both forms of IBD.Citation40,Citation41.
Specific gut microbiota signatures have been detected in patients suffering from UC. These changes include a decrease in the abundance of the phylum VerrucomicrobiaCitation36 or a decrease in the family Leuconostocaceae, the latter being known as acetate and lactate producersCitation38. There is not a clear consensus proportion of the genus Bacteroides within the phylum Bacteroidetes. While some studies in the literature reported significant reduction in Bacteroides,Citation42 further studies found that this group is increased in UC patientsCitation43 and directly associated with the degradation of acid mucin as a carbon source in the colon, with an exaggerated inflammatory response and with colitis.Citation37 Regarding the Clostridia class (phylum Firmicutes), we found some differences between families and genera, especially for the Clostridiaceae, Ruminococcaceae, and Lachnospiraceae families.Citation36–Citation39,Citation44 In UC, studies have reported a reduction in the proportions of the genus Coprococcus and some species of genus Roseburia, along with other genera and species belonging to the family Lachnospiraceae.Citation36,Citation39 In contrast, for the Clostridiaceae family, some species seem to be in increased proportions in these patients,Citation37 like Clostridium symbiosum, while a reduction in the abundance of other groups, such as Clostridium colinum and Clostridium subcluster XIVab, has also been described.Citation36,Citation42 Additionally, in the order Clostridiales, a decrease in the genus Phascolarctobacterium was linked to the presence of colonic inflammation regardless of the UC phenotypeCitation36,Citation38 ( and ).
Table 1. Main changes detected in the gut microbiota of patients suffering from ulcerative colitis and Crohn´s disease. Bacteria for which a reduction in relative proportions has been detected.
Table 2. Main changes detected in the gut microbiota of patients suffering from ulcerative colitis and Crohn´s disease. Bacteria for which an increase in relative proportions has been detected.
Crohn's disease
Most of the microbiota changes previously described in the gut microbiota of patients with UC are also observed in patients suffering from CD. For example, an increase in the proportion of the Enterobacteriaceae family is found in UC patients, which is also present in the gut of patients suffering from CD,Citation43,Citation47,Citation68 especially regarding Escherichia and Shigella relative proportions, which are directly implicated in intestinal inflammation.Citation38,Citation39,Citation61
In CD patients with ileal involvement, an important reduction in the proportions of Ruminococcaceae and Faecalibacterium has been reported in several studies (). They are recognized as acetate and butyrate producers, respectively, and therefore they contribute to creating an environment of oxidative stress in the intestineCitation38 (). In this context, while some bacteria seem to be associated with a specific disease phenotype, a decrease in Clostridiales is most likely present in all forms of CDCitation39,Citation47,Citation48,Citation51,Citation54,Citation59,Citation63 with only a few exceptions.Citation61 In contrast, there is no unanimity regarding the increase or decrease in Lachnospiraceae abundance in CD. While some studies reported an increase in the proportions of this family in the intestinal mucosa of patients with moderate activity,Citation37 further studies reported a decrease in their proportionsCitation38,Citation40,Citation52,Citation61 or an increase at the family level but a depletion in lower taxonomical levels.Citation46 These findings may indicate an important correlation between intestinal dysbiosis and CD phenotypeCitation39 ( and ).
Dysbiosis implications
At this point, we can observe that the available studies in the literature have described more similarities than dissimilarities in the gut environment of IBD patients, regardless of whether they suffer from CD or UC. Furthermore, the proportions of some phylum seem to vary in function of the compartments of the intestinal tract, notably in ileal, colonic tissue, and rectal tissue.Citation69
The decrease in the alpha-diversity index and the increase or decrease in the different taxa in the gut have important functional implications for epithelium repair and inflammation regulation, playing a fundamental role in the course and worsening of the disease. The crosstalk of the bacterial groups in the gut ecosystem is a competitive, bidirectional, and dynamic process, which evolves in the function of the local environment. In turn, this environment directly depends on the available nutrients and the bacterial metabolites, which finally promotes differential bacterial growth. In IBD individuals, a decrease in basic biosynthesis has been observed, along with changes in several other metabolic processes (the biosynthesis of essential amino acids, cobalamin synthesis, purine and pyrimidine biosynthesis, acetogenesis to replace biomethanation, lipid catabolism, and phospholipid metabolism).Citation38–Citation40 Under these conditions, the levels of hydrogen are strongly reduced, promoting an increase in aerobic and aerotolerant taxa and exacerbating disease severity.Citation40
Proteobacteria phylum in IBD patient: enterobacteriaceae, pasteurellaceae, and desulfovibrionaceae families
Several studies have reported an increase in the Pasteurellaceae and/or Enterobacteriaceae families in patients with CD.Citation37–Citation40,Citation45-Citation47,Citation49,Citation68 Gut inflammation and chronic colitis have been further associated with an important increase of Enterobacteriaceae familyCitation68 and an oxidative stress in the gut. A recent study goes beyond and suggests Enterobacteriaceae as stool biomarkers in IBD.Citation45 There are several metabolic changes that promote oxidative stress at the mucosal surface of IBD patients and favor an increased level or depletion of different taxa that use mucin as a primary energy source.Citation37,Citation38 Specifically, the increase in components of the benzoate metabolic pathway (aminobenzoate and fluorobenzoate degradation) seems to be directly associated with Enterobacteriaceae growth, virulence, and stress response.Citation40 Bacteria such as Salmonella or enterohemorrhagic E. coli would take advantage of these redox stresses and therefore proliferate to a large extent. Indeed, in the ileum mucosa of CD patients and in the fecal samples of UC patients,Citation60 high numbers of adherent and invasive E. coli have been found, as well as a high prevalence of antibodies directed against E. coli outer membrane porin C (OmpC) and flagellin. It seems that E. coli acts as an opportunistic pathogen and is directly implicated in the disease, with the induction of the production of cytokines, such as tumor necrosis factor α (TNFα) and IL8,Citation39 and an increase in mucin degradation.
In contrast, the Desulfovibrionaceae family is reported in reduced proportions,Citation37 with a negative correlation between physiological distress and its abundance.Citation70 The genus Desulfovibrio degrades acidic mucin normally found in the colon. However, in CD patients, the mucus is mostly neutral, which can explain the reductions observed in these subjects.Citation37
Bacteroidetes pylum in IBD patients: prevotellaceae and bacteroidaceae families
In IBD patients, inflammation and colitis have been also associated with an increase of PrevotellaceaeCitation43,Citation51 and BacteroidaceaeCitation46 family. Within the latter, Bacteroides genus has been suggested as an IBD biopsy biomarker.Citation45
There is an important increase in other bacterial-mediated processes, which in turns favor the proliferation of members of Bacteroidetes phylum. These processes include an increase in the metabolism of the sulfur amino acid cysteine, riboflavin metabolism, lipopolysaccharide production, glutathione biosynthesis, N-acetylgalactosamine phosphotransferase transporters, and virulence factor production. A decrease in proportions of Bacteroides genus has been reported in inflamed mucosa when compared with non-inflamed mucosa of patients suffering IBD,Citation49 and have been identified as a predictor of relapse.Citation54
Firmicutes phylum in IBD patients: clostridiaceae, lachnospiraceae ruminococcaceae and veillonellaceae families
The oxidative stress previously described has also a direct impact in the phylum Firmicutes, with an increase in some mucolytic bacteria, especially Ruminococcus torques and Ruminococcus gnavus.Citation67 A previous study showed differences in their abundance in the dysbiotic gut of CD and CU patients.Citation62 Furthermore, R. gnavus along with Clostridium hathewayi and Clostridium bolteae have increased expression during dysbiosis, suggesting that they could have a role in the disease.Citation62
On the other hand, a decrease in the abundance of butyrate-producing, hydrogen-utilizing bacteria and other taxa with anti-inflammatory activity, including Faecalibacterium, Phascolarctobacterium (Veillonellaceae family), and Clostridia clades IV and XIVa, especially the genera Roseburia (Lachnospiraceae family) and Butyricicoccus (Clostridiaceae family) have been observed (). Species of Roseburia are butyrate producers and acetate consumers and are associated with anti-inflammatory regulatory T cell production, while Phascolarctobacterium species are only succinate consumers. Both of these genera have been associated with a decrease in butyrate and propionate production in both forms of IBD.Citation36,Citation38 In relation to the genus Faecalibacterium, a low rate of Faecalibacterium prausnitzii have been identified as predictors of relapse.Citation54 IBD inflamed mucosa presents a decrease in F. prausnitzii compared to non-inflamed mucosa.Citation49 Furthermore, low abundance of Faecalibacterium in postoperative ileal mucosa has been associated with a higher risk of recurrence,Citation64 and also associated with a massive increase of leukocytes in UC.Citation66 This bacterium can metabolize host-derived polysaccharides (pectin, uronic acids) and other substrates (such as N-acetyl glucosamine) from the intestinal mucus for growth, and it is also described as an important anti-inflammatory commensal bacterium.Citation38 The anti-inflammatory properties of F. prausnitzii have been associated with inhibition of the NF-κB pathway via protein production in intestinal epithelial cells, while a decrease in proportions of Butyricicoccus pullicaecorum seems to attenuate trinitrobenzene sulfonic acid (TNBS)-induced colitis in rats and to increased transepithelial resistance.Citation36 This depletion of Faecalibacterium and Butyricicoccus, but also of Ruminococcus hominis, combined with alterations in bacterial products, especially butyrate,Citation53,Citation57,Citation62 provides the appropriate conditions to allow E. coli to proliferate.Citation39
Verrucomicrobia phylum, akkermansia abundance, and its impact on IBD
Unlike for other mucolytic bacteria, some studies reported a reduction in the levels of Akkermansia muciniphila in both CD and UC patients and in the early onset of CD.Citation67,Citation71 It has been proposed that A. muciniphila could be responsible for exacerbated gut inflammation in IBD patients. However, a recent study using animal models did not find any correlation between short-term intestinal inflammation and the presence of the bacterium in the gut.Citation72 A. muciniphila use mucus as a carbon, nitrogen, and energy source, and therefore, as a consequence of its metabolism, it produces short-chain fatty acids (acetate, propionate, 1,2-propanediol, and succinate).Citation73 It is worth mentioning that short-chain fatty acids seem to be depleted in IBD patients.Citation74 Furthermore, as specifically described for UC patients, the decrease in the abundance of the genus Akkermansia and the low abundance of A. muciniphila could affect the use of mucins as a carbon source by other symbiotic commensal bacteria,Citation36 and it was proposed as a possible marker of dysbiosis.Citation75 Reductions in Akkermansia genus were also described in the gut microbiota of patients with CD.Citation56
CDI and IBD: gut microbiota relationships and implications for disease treatment with fecal microbiota transplantation
Only a few studies have investigated the specific impact of CDI on the IBD microbiota. A previous studyCitation76 directly compared the gut microbiota of IBD patients with and without CDI disease. The authors found that in patients with both IBD and CDI, there was a loss of bacterial cooperation in the gut ecosystem as well as a more pronounced intestinal dysbiosis than in patients suffering from only IBD. Metabolite production is also altered in the inflamed gut, which is essential for several metabolic processes, as energy production and host immunity.Citation77 Among these metabolites, butyrate has a fundamental role in maintaining the balance of the intestinal microbiota, with the preservation of the epithelial barrier and regulation of the immunity.Citation53,Citation74 Butyric acid, along with acetic acid and propionic acid are the end products of indigested carbohydrates in the intestine after bacterial fermentation. It was demonstrated that butyrate enhances the intestinal barrier function by facilitating the assembly of tight junctions.Citation78 Butyrate producers supply energy to gut epithelial cells and therefore they protect against inflammation and infection.Citation79 In the last decade, several studies have focused on the modification of the gut microbiota to successfully treat several intestinal diseases, including IBD and CDI. Among the various taxa investigated, it seems that positive results are obtained when the feces include the following taxa: Clostridium clusters IV and XIVa, which include the Ruminococcaceae and Lachnospiraceae families, respectively, and the genera Roseburia, Oscillibacter, Blautia, and Dorea. This selection of microbes has important underlying metabolic mechanisms, specially the production of butyrate in the gut.Citation80
Blautia and Dorea genera: role in maintenance and recovery of gut homeostasis
In concomitant IBD and CDI diseases, there is a specific reduction in two groups of bacteria, Blautia and Dorea. Members of Blautia (butyrate-producing bacterial species) are already significantly reduced in patients with only IBD, but it seems that the decrease in the relative proportions in the gut is more marked when the disease is aggravated with CDI.Citation76 The Blautia genus (especially Blautia obeum) is selected among the bacterial species enriched in the fecal microbiota of healthy donors for fecal microbiota transplant (FMT) and was also found after successful restoration of the gut in patients with recurrent CDI.Citation81–Citation85 Furthermore, in vitro analysis has shown a negative correlation between the production of a bile metabolism enzyme (bile salt hydrolase, of which Blautia is one of the representative producers) and C. difficile germination.Citation86,Citation87 It was recently described that the bacterial strain B. obeum A2-162 produces a lantibiotic, nisin O, in the human gastrointestinal tract, which presents antimicrobial activity against both Clostridium perfringens and C. difficile.Citation88 Therefore, its depletion would favor C. difficile colonization and infection in the IBD gut.
Regarding the Dorea genus, its depletion has been previously reported in studies investigating patients suffering from CDI and IBD separately.Citation40,Citation79 Blautia and Dorea have been described as major acetate producers in the normal gut, but it is hypothesized that they are replaced when CDI occurs.Citation79 Recently, a study proposed a cocktail of bacteria to treat recurrent CDI, which includes Blautia producta (Peptostreptococcus productus), E. coli and Clostridium bifermentans. The authors demonstrate in their work that this bacteriotherapy could antagonize chronic relapse of CDI, which in turn inhibited the growth of Bacteroides species.Citation89
Undesirable increase of some taxa: proliferation of other pathogens and aggravating factors of disease
There are some taxa that seem to increase in abundance in patients suffering from IBD and CDI, including some species of Clostridium, Enterococcus, and R. gnavus,Citation76 which have also been described to increase in patients with IBD (). High abundances of Proteobacteria and Enterobacteriaceae are often found in patients with recurrent CDICitation82 but also in those suffering from IBD.Citation37–Citation40,Citation46 Within these two bacterial groups, some species are classified as important pathogens, such as Salmonella and enterohemorrhagic E. coli, which may take advantage of the intestinal conditions under dysbiosis to proliferate and worsen the disease.Citation39 These intestinal conditions include altered oxygen availability and nitrate production. Under inflammatory conditions, epithelial cells reduce their capacity to undergo beta-oxidation, resulting in an increase in available oxygen and a reduction in hydrogen levels.Citation40 Furthermore, the depletion of butyrate-producing bacteria favors the expression of Nos2 (an important gene encoding nitrite oxidase synthase), resulting in elevated levels of available nitrate and proliferation of the Enterobacteriaceae family, especially E. coli.Citation90
After fecal microbiota transplantation for CDI treatment, an increase in Bacteroidetes to the detriment of Protobacteria was found.Citation91 The important role of Proteobacteria in IBD and CDI diseases is associated with its direct role as a disruptor of intestinal homeostasis and its direct implication in the inflammation of the intestine. The absence of differentiated B-cells and deficiency in the production of specific IgA (specifically targeting Proteobacteria) is correlated with the persistence of Proteobacteria in the inflamed gut.Citation92 Other taxonomical alterations related to CDI and IBD are increased levels of Fusobacterium and Mycobacterium taxa.Citation93 The Fusobacteriaceae family has also been found in high proportions in the gut microbiota of patients with CD and UC.Citation40,Citation75 Mycobacterium avium subs. Paratuberculosis and Fusobacterium nucleatum have been recently investigated as potential aggravating factors for IBD.Citation94
Altered intestinal barrier function and C. difficile colonization
The impairment of intestinal barrier function or disruption of mucosal T cells by inflammatory mediators favor C. difficile colonization and toxin production. Some phospholipids, such as phosphatidylcholine and phosphatidylethanolamine, are released during this disruption. Phosphatidylcholine is converted into ethanolamine and glycerol by bacterial phosphodiesterases. C. difficile benefits from the breakdown of ethanolamine and utilizes it as a source of nitrogen and carbon.Citation95,Citation96 On the other hand, a higher glycosidase activity has been reported in IBD patients than in healthy subjects. Indeed, disruption of intestinal barrier function and the intestinal microbiota also entails the liberation of monosaccharides, which promote the multiplication and colonization of C. difficile.Citation96 A previous study described in depth how C. difficile catabolises microbiota-liberated mucosal carbohydrates and how pathogen expansion is even aided by microbiota-induced elevation of sialic acid levels in vivo.Citation97
C. difficile is able to produce para-cresol (p-cresol) through the fermentation of tyrosine in the gut. A recent study demonstrated that this ability provides a competitive advantage over other gut bacteria, including E. coli, Klebsiella oxytoca, and Bacteroides thetaiotaomicron.Citation98 Further studies have proposed that bacterial metabolites, such as p-cresol, ammonium, and hydrogen sulfide, notably affect intestinal barrier function and participate in the IBD course.Citation99
Other microbiota signatures and metabolic pathways associated with specific conditions and populations of CDI and IBD
In pediatric population, it has been described that IBD patients with CDI and with a previous history of surgery presented a reduction of Ruminococcus, Alistipes, and Bifidobacterium.Citation100 Even if there are significant differences in the gut microbiota between pediatric patients and adults due to the gut microbiota is not yet fully developed, throughout this review we have observed several discrepancies among the different studies in relation to the presence of some species of Bifidobacterium and Ruminococcus and their role in the inflamed mucosa ( and ). It has been demonstrated that some strains of R. gnavus are able to assimilate mucin monosaccharides, to use sialic acid and to produce propanol and propionate.Citation101 As previously described, mucin users are implicated in gut inflammation.Citation37 But the finding that not all of R. gnavus strains are able to grow on mucin as the sole carbon sourceCitation101 may explain the differences about its depletion or increase in IBD and CDI disease. Further explanations for an overexpression of Bifidobacterium,Citation61,Citation68,Citation102 Ruminococcus,Citation49,Citation61,Citation67 or even AkkermansiaCitation102 in the inflamed gut include the important role of the modifications in the intestinal micro-environment, as, for example, an increase of mucus production,Citation102 and also microbiota modifications and interactions with aging.
Other three studies have confirmed the reduction of Alistipes in pediatric patients with IBD,Citation37,Citation52,Citation56 but also in patients with CDI.Citation102 Alistipes has been associated with protection against CDI and positive modulate the immune response against experimental colitis in mouse models.Citation103 Furthermore, it has been proposed as biomarker of CDI,Citation102 and used as one of the dominant genera in the fecal bacterial composition of donors for fecal microbiota transplantation to treat CDI, resulting in the successful integration of this bacterial group in the gut ecosystem of the patient.Citation104
Finally, and in relation with metabolic pathways, a further analysis showed a reduction in methionine biosynthesis in IBD patients with C. difficile after surgery.Citation100 Alterations of sulfur and cysteine/methionine metabolism in IBD patients have been previously related to changes in proportions of some bacteria with specific functions involving these pathways,Citation105 including F. prausnitzii and Roseburia among others.Citation100 Furthermore, it has been observed that a commercial form of methionine (available as dietary supplement) enhances the viability of Saccharomyces boulardii in the gut, especially in acidic environments. This nonpathogenic yeast is classified as a probiotic and it has been used to prevent CDICitation106 and suggested as a treatment of IBD. Furthermore, serological antibodies Anti-Saccharomyces have been used as a marker for prediction of CD disease course, within other variables and patient characteristics.Citation107
Microbiota and treatments for IBD and CDI: situation and perspective
As already described in this review, one of the most proposed options in recent years have been fecal microbiota transplantation to restore the altered gut ecosystem. We can find in the literature several studies describing its use in CDI patients with underlying IBD.Citation108 In a previous study treating patients with CDI and concurrent IBD, the effectiveness of FMT was between 79% and 88%, after one and two interventions, respectively.Citation109 A further study also reported the efficacy of FMT to treat recurrent CDI in IBD, but authors found that more than half of patients required IBD treatment escalation shortly after FMT.Citation110 Similarly, in the study of Khoruts et al.Citation111 results showed that FMT was less effective in IBD patients suffering recurrent CDI than in those without IBD, as more than 25% of the studied IBD patients have a disease flare following FMT, especially in those cases with extensive colon involvement, and they required a treatment with prednisone. Hypothesis about the problems with FMT in these patients include implantation of the major taxa in the gut and deficiency in host immune defenses.Citation111 Meighani et al.Citation112 found a good response to FMT in patients with CDI and IBD. In their study, three patients who failed therapy had newly diagnosis of IBD and one presented severe active disease. Therefore, authors conclude that FMT is a good alternative treatment for well-controlled IBD patients with recurrent CDI.
Consistent with the microbiota changes observed in IBD and CDI patients, a specific microbiota signature for fecal microbiota donors has been describedCitation80,Citation113 (). The selection of microbes has important underlying metabolic mechanisms, such as the production of butyrate in the gut, as largely described in the section above.
Table 3. Group of bacteria modifications associated with CDI and IBD. Main characteristics and role in disease and fecal microbiota transplant treatment.
A previous study selected a total of 37 bacteria to treat dysbiosis during CDI, which could be administrated orally in a noninvasive way.Citation85 In this contest, some problems derived from FMT are related to the actual method of the feces delivery, which may require colonoscopy and sedation.Citation116 In addition, other problems could include the degree of engraftment and immune response to the transplanted microbiota (donor-recipient incompatibilities), stemming from an underlying genetic factor.Citation80 A previous study suggested only a marginal risk of worsening in FMT-treated IBD patients, and hypothesized the role of donors to induce remission or to induce worsening in IBD activity.Citation117 Other described complications include the transmission of parasites from donors to patients by FMT, but without gastrointestinal symptomatology.Citation118 A recent study used washed microbiota transplantation in mice and concluded that the technique avoids the virus transmission among other complications and is safer than crude FMT.Citation119
In addition to FMT, probiotic nutrition with multiple strains for gastrointestinal health modulation has been proposed as an effective and safe treatment.Citation120 One recent study proposed the strain Bacillus licheniformis to treat colitis, which seems to modulate the gut microbiota composition and has been associated with a decrease in Bacteroidetes.Citation121 Other probiotics classically used in different trials to reduce intestinal inflammation are Lactobacillus rhamnosus, Lactobacillus plantarum, Lactobacillus acidophilus, and Enterococcus faecium. However, the available results on their effectiveness in both CD and UC are still not concise.Citation122 To prevent the likelihood of incurring CDI, a combination of various probiotics, including Streptococcus faecalis, Bacillus mesentericus, and Clostridium butyricum,Citation123 has been proposed (once again, we can find among “protective” strains those associated with butyric acid production). Competition for the niche with non-toxigenic C. difficile strains has also been suggested for CDI prevention. Bacillus clausii and Lactobacillus reuteri also act as probiotics for this infection because they secrete compounds that directly inhibit C. difficile.Citation124 Those probiotics proposed for CDI and IBD separately could be used jointly to treat both diseases. However, a recent study underlines the important role of mutual interaction of probiotics, which can inhibit other probiotics or protective taxa in the gut.Citation125 Therefore, further studies addressing these metabolic interactions are necessary to better understand the role of these probiotics in both diseases.
Conclusions and future directions
In this review, we have summarized the gut microbiota changes associated with both forms of IBD and CDI and their similarity with the dysbiosis that occurs in the CDI. IBD is itself a complicated and poorly understood disease. The alteration of the microbiota and the metabolic environment of the gut have direct consequences in chronic inflammation and in the colonization and multiplication of opportunistic pathogens, with C. difficile being one of the most important causes of infection in this group. Our analysis reveals important modifications in specific taxa that recur in both diseases despite the intrinsic differences of each study (variable environment, genetic diversity, medication usage, smoking history, and variable diet). Furthermore, the investigation of the metabolic pathways of these groups of bacteria reveals the specific mechanism of action in the epithelial cells and lumen in the gut. Elucidating the impact of bacterial metabolites in other microbial communities, it is possible to better discern between protective bacteria and those that cause harm. All the advances in new sequencing technologies have provided a large number of publications that apply these methods to better understand intestinal inflammation. However, in this review, we highlight that there is an insufficient number of studies addressing the microbiota composition and its changes in the gut of patients suffering from both CDI and IBD. Furthermore, the only available data are focused either on the epidemiology and treatment of the infection in IBD patients or on the microbiota composition of adult patients, but there are no results on other patient groups, such as the elderly, pediatric, or pregnant IBD populations. In addition, the results regarding adults are scarce and supported by only a few studies. Therefore, there is an urgent need to develop new research lines addressing the changes in the gut microbiota in IBD patients suffering from CDI. These studies will provide results that are now necessary to develop new therapeutic strategies to prevent and treat C. difficile and its infection in IBD.
Disclosure of Potential Conflicts of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Additional information
Funding
References
- Rodriguez C, Van Broeck J, Taminiau B, Delmée M, Daube G. Clostridium difficile infection: early history, diagnosis and molecular strain typing methods. Microb Pathog. 2017;97:59–25. doi:10.1016/j.micpath.2016.05.018. PMID: 27238460.
- Matsuoka K, Kobayashi T, Ueno F, Matsui T, Hirai F, Inoue N, Kato J, Kobayashi K, Koganei K, Kunisaki R, et al. Evidence-based clinical practice guidelines for inflammatory bowel disease. J Gastroenterol. 2018;53:305–353. doi:10.1007/s00535-018-1439-1. PMID: 29429045.
- D´Aoust J, Battat R, Bessissow T. Management of inflammatory bowel disease with clostridium difficile infection. World J Gastroenterol. 2017;23:4986–5003. doi:10.3748/wjg.v23.i27.4986. PMID: 28785153.
- Hourigan SK, Sears CL, Oliva-Hemker M. Clostridium difficile infection in pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2016;22:1020–1025. doi:10.1097/MIB.0000000000000666. PMID: 26689599.
- Li Y, Qian J, Queener E, Shen B. Risk factors and outcome of PCR-detected Clostridium difficile infection in ileal pouch patients. Inflamm Bowel Dis. 2013;19:397–403. doi:10.1097/MIB.0b013e318280fcb9. PMID: 23328770.
- Regnault H, Bourrier A, Lalande V, Nion-Larmurier I, Sokol H, Seksik P, Barbut F, Cosnes J, Beaugerie L. Prevalence and risk factors of Clostridium difficile infection in patients hospitalized for flare of inflammatory bowel disease: a retrospective assessment. Dig Liver Dis. 2014;46:1086–1092. doi:10.1016/j.dld.2014.09.003. PMID: 25294795.
- Vitikainen K, Haapamäki J, Färkklä M, Anttila VJ, Arkkila P. Clostridium difficile infection in patients with inflammatory bowel disease: a case control study. Scand J Gastroenterol. 2018;53:947–951. doi:10.1080/00365521.2018.1492012. PMID: 30041549.
- Razik R, Rumman A, Bahreini Z, McGeer A, Nguyen GC. Recurrence of Clostridium difficile infection in patients with inflammatory bowel disease: the RECIDIVISM Study. Am J Gastroenterol. 2016;111:1141–1146. doi:10.1038/ajg.2016.187. PMID: 27215924.
- Rao K, Higgins P. Epidemiology, diagnosis and management of Clostridium difficile infection in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22:1744–1754. doi:10.1097/MIB.0000000000000793. PMID: 27120571.
- Hall IC, O´Toole E. Intestinal flora in new-born infants with a description of a new pathogenic anaerobe, Bacillus difficilis. Am J Dis Child. 1935;49:309–402. doi:10.1001/archpedi.1935.01970020105010.
- George RH, Symonds JM, Dimock F, Brown JD, Arabi Y, Shinagawa N, Keighley MR, Alexander-Willians J, Burdon DW. Identification of Clostridium difficile as a cause of pseudomembranous colitis. Br Med J. 1978;1:695. doi:10.1136/bmj.1.6114.695. PMID: 630301.
- George WL, Sutter VL, Goldstein EJ, Ludwig SL, Finegold SM. Aetiology of antimicrobial-agent-associated colitis. Lancet. 1978;1:802–803. doi:10.1016/s0140-6736(78)93001-5. PMID: 85818.
- Perlmann P, Hammarström S, Lagercrantz R, Campbell D. Auto-antibodies to colon in rats and human ulcerative colitis: cross-reactivity with E. coli 014 antigen. Proc Soc Exptl Biol Med. 1967;125:975. doi:10.3181/00379727-125-32253. PMID: 15938314.
- LaMont JT, Trnka YM. Therapeutic implications of Clostridium difficile toxin during relapse of chronic inflammatory bowel disease. Lancet. 1980;1(8165):381–383. doi:10.1016/s0140-6736(80)90939-3. PMID: 6101841.
- Bolton RP, Sherriff RJ, Read AE. Clostridium difficile associated diarrhoea: a role in inflammatory bowel disease? Lancet. 1980;1(8165):383–384. doi:10.1016/s0140-6736(80)90940-x. PMID: 6101842.
- Barlett JG. Clostridium difficile and inflammatory bowel disease. Gastroenterology. 1981;80(4):863–865. doi:10.1016/0016-5085(81)90154-2.
- Keighley MR, Youngs D, Johnson M, Allan RN, Burdon DW. Clostridium difficile toxin in acute diarrhoea complicating inflammatory bowel disease. Gut. 1982;23:410–414. doi:10.1136/gut.23.5.410. PMID: 7076018.
- Tvede M, Willumsen L. Clostridium difficile in patients with irritable bowel syndrome and ulcerative colitis. Lancet. 1982;1(8281):1124. doi:10.1016/s0140-6736(82)92305-4. PMID: 6122916.
- Bolton RP, Read AE. Clostridium difficile in toxin megacolon complicating acute inflammatory bowel disease. Br Med J (Clin Res Ed). 1982;285(6340):475–476. doi:10.1136/BMJ.285.6340.475-a. PMID: 6809132.
- Greenfield C, Aguilar-Ramirez JR, Pounder RE, Williams T, Danvers M, Marper SR. Clostridium difficile and inflammatory bowel disease. Gut. 1983;24(8):713–717. doi:10.1136/gut.24.8.713.
- Gurian L, Klein K, Ward TT. Role of Clostridium difficile and Campylobacter jejuni in relapses of inflammatory bowel diseases. West J Med. 1983;138(3):359–360. PMID:6858121.
- Pokorney BH, Nichols TW Jr. Pseudomembranous colitis. A complication of sulfasalazine therapy in a patient with Crohn´s colitis. Am J Gastroenterol. 1981;76(4):374–376. PMID: 6119900.
- Browman RA, Riley TV. Routine culturing for Clostridium difficile? Pathology. 1984;16:240–242. doi:10.3109/00313028409068530. PMID: 6514390.
- Hyams JS, McLaughlin JC. Lack of relationship between Clostridium difficile toxin and inflammatory bowel disease in children. J Clin Gastroenterol. 1985;7(5):387–390. doi:10.1097/00004836-198510000-00003. PMID: 4067226.
- Gryboski JD. Clostridium difficile in inflammatory bowel disease relapse. J Pediatr Gastroenterol Nutr. 1991;13:39–41. doi:10.1097/00005176-199107000-00007. PMID: 1919950.
- Kochhar R, Ayygari A, Goenka MK, Dhali GK, Aggarwai R, Mehta SK. Role of infectious agents in exacerbations of ulcerative colitis in India. A study of Clostridium difficile. J Clin Gastroenterol. 1993;16:26–30. doi:10.1097/00004836-199301000-00008. PMID: 8421140.
- Tremaine WJ. Inflammatory bowel disease and Clostridium difficile-associated diarrhoea: a growing problem. Clin Gastroenterol Hepatol. 2007;5:310–311. doi:10.1016/j.cgh.2006.12.030.3. PMID: 17368229.
- Issa M, Vijayapal A, Graham MB, Beaulieu DB, Otterson MF, Lundeen S, Skaros S, Weber LR, Komorowski RA, Knox JF, et al. Impact of Clostridium difficile on inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007;5(3):345–351. doi:10.1016/j.cgh.2006.12.028. PMID: 17368234.
- Ananthakrishnan AN, McGinley EL, Bionion DG. Excess hospitalisation burden associated with Clostridium difficile in patients with inflammatory bowel disease. Gut. 2008;57(2):205–210. doi:10.1136/gut.2007.128231. PMID: 17905821.
- Zilberbeg MD, Shorr AF, Kollef MH. Increase in Clostridium difficile-related hospitalizations among infants in the United States, 2000-2005. Pediatr Infect Dis J. 2008;27(12):1111–1113. doi:10.1097/inf.0b013e31817eef13. PMID: 19068517.
- Issa M, Ananthakrishnan AN, Binion DG. Clostridium difficile and inflammatory bowel disease. Inflamm Bowel Dis. 2008;14(10):1432–1442. doi:10.1002/ibd.20500. PMID: 18484669.
- DuPont HL, Garey K, Caeiro JP, Jiang ZD. New advances on Clostridium difficile infection: changing epidemiology, diagnosis, treatment and control. Curr Opin Infect Dis. 2008;21:500–507. doi:10.1097/qco.0b013e32830f9397. PMID: 18725800.
- Ali S, Tamboli CP. Advances in epidemiology and diagnosis of inflammatory bowel diseases. Curr Gastr Rep. 2008;10(6):576–584. doi:10.1007/s11894-008-0105-9. PMID: 19006614.
- Hermens DJ, Miner PB Jr. Exacerbation of ulcerative colitis. Gastroenterology. 1991;101(1):254–262. doi:10.1016/0016-5085(91)90487-6.
- Torsten T, Gilbert J, Meyer F. Metagenomics -a guide from sampling to data analysis. Microb Inform Exp. 2012;2:3. doi:10.1186/2042-5783-2-3. PMID: 22587947.
- Bajer L, Kuerka M, Kostovcik M, Macinga P, Dvorak J, Stehlikova Z, Brezina J, Wohl P, Spicak J, Drastich P. Distinct gut microbiota profiles in patients with primary sclerosing cholangitis and ulcerative colitis. World J Gastroenterol. 2017;23(25):4548–4558. doi:10.3748/wjg.v23.i25.4548. PMID: 28740343.
- Alipour M, Zaidi D, Valcheva R, Jovel J, Martinez I, Sergi C, Walter J, Mason AL, Wong GK, Dieleman LA, et al. Mucosal barrier depletion and loss of bacterial diversity are primary abnormalities in paediatric ulcerative colitis. J Crohns Colitis. 2016;10(4):462–471. doi:10.1093/ecco-jcc/jiv223. PMID: 26660940.
- Morgan XC, Tickle TL, Sokol H, Gevers D, Devaney KL, Ward DV, Reyes JA, Shah SA, LeLeiko N, Snapper SB, et al. Dysfunction of the intestinal microbiome in inflammatory bowel disease and treatment. Genome Biol. 2012;13(9):R79. doi:10.1186/gb-2012-13-9-r79. PMID: 23013615.
- Baumgart M, Dogan B, Rishniw M, Weitzman G, Bosworth B, Yantiss R, Orsi RH, Wiedmann M, McDonough P, Kim SG, et al. Culture independent analysis of ileal mucosa reveals a selective increase in invasive Escherichia coli of novel phylogeny relative to depletion of Clostridiales in Crohn´s disease involving the ileum. Isme J. 2007;1(5):403–418. doi:10.1038/ismej.2007.52. PMID: 18043660.
- Gevers D, Kugathasan S, Denson LA, Vázquez-Baeza Y, Van Treuren W, Ren B, Schwager E, Knights D, Song SJ, Yassour M, et al. The treatment-naïve microbioma in new-onset Crohn´s disease. Cell Host Microbe. 2014;15(3):382–392. doi:10.1016/j.chom.2014.02.005. PMID: 24629344.
- Aden K, Rehman A, Waschina S, Pan WH, Walker A, Lucio M, Nunez AM, Bharti R, Zimmerman J, Bethge J, et al. Metabolic functions of gut microbes associate with efficacy of tumor necrosis factor antagonists in patients with inflammatory bowel disease. Gastroenterology. 2019;157(5):1279–1292. doi:10.1053/j.gastro.2019.07.025. PMID: 31326413.
- Nemoto H, Kataoka K, Ishikawa H, Ikata K, Arimochi H, Iwasaki T, Ohnishi Y, Kuwchara T, Yasutomo K. Reduced diversity and imbalanced fecal microbiota in patients with ulcerative colitis. Dig Dis Sci. 2012;57(11):2955–2964. doi:10.1007/s10620-012-2236-y. PMID:22623042.
- Kabeerdoss J, Jayakanthan P, Pugazhendhi S, Ramakrishna SB. Alterations of mucosal microbiota in the colon of patients with inflammatory bowel disease revealed by real time polymerase chain reaction amplification of 16S ribosomal ribonucleic acid. Indian J Med Res. 2015;142(1):23–32. doi:10.4103/0971-5916.162091. PMID: 26261163.
- Danilova NA, Abdulkhakov SR, Grigoryeva TV, Markelova MI, Vailyev IY, Boulygina EA, Ardatskaya MD, Pavlenko AV, Tyakht AV, Odintsova AK, et al. Markers of dysbiosis in patients with ulcerative colitis and Crohn´s disease. Ter Arkh. 2019;91(4):17–24. doi:10.26442/00403660.2019.04.000211. PMID: 31094471.
- Altomare A, Putignani L, Del Chierico F, Cocca S, Angeletti S, Ciccozzi M, Tripiciano C, Dalla Piccola B, Cicala M, Guarino MPL, et al. Gut mucosal-associated microbiota better discloses inflammatory bowel disease differential patterns than faecal microbiota. Dig Liver Dis. 2019;51(5):648–656. doi:10.1016/j.dld.2018.11.021. PMID: 30573380.
- Imhann F, Vich Vila A, Bonder MJ, Fu J, Gevers D, Visschedijk MC, Spekhorst LM, Alberts R, Franke L, van Dullemen HM, et al. Interplay of host genetics and gut microbiota underlaying the onset and clinical presentation of inflammatory bowel disease. Gut. 2018;67(1):108–119. doi:10.1136/gutjnl-2016-312135. PMID: 27802154.
- Shaw KA, Bertha M, Hofmekler T, Chopra P, Vatanen T, Srivatsa A, Prince J, Kumar A, Sauer C, Zwick ME. Dysbiosis, inflammation, and response to treatment: a longitudinal study of pediatric subjects with newly diagnosed inflammatory bowel disease. Genome Med. 2016;8(1):75. doi:10.1186/s13073-016-0331-y. PMID: 27412252.
- Andoh A, Kuzuoka H, Tsujikawa T, Nakamura S, Hirai F, Suzuki Y, Matsui T, Fujiyama Y, Matsumoto T. Multicenter analysis of fecal microbiota profiles in Japanese patients with Crohn´s disease. J Gastroenterol. 2012;47(12):1298–1307. doi:10.007/s00535-012-0605-0. PMID:22576027.
- Lo Presti A, Zorzi F, Del Chierico F, Altomare A, Cocca S, Avola A, De Biasio F, Russo A, Cella E, Reddel S, et al. Fecal and mucosa microbiota profiling in irritable bowel syndrome and inflammatory bowel disease. Front Microbiol. 2019;10:1655. doi:10.3389/fmicb.2019.01655. PMID: 31379797.
- Nishino K, Nishida A, Inoue R, Kawada Y, Ohno M, Skai S, Inatomi O, Bamba S, Sugimoto M, Kawahara M, et al. Analysis of endoscopic brush samples identified mucosa-associated dysbiosis in inflammatory bowel disease. J Gastroenterol. 2018;53(1):95–106. doi:10.1007/s00535-017-1384-4. PMID: 28852861.
- Manichanh C, Rigottier-Gois L, Bonnaud E, Gloux K, Pelletier L, Frangeul L, Nalin R, Jarrin C, Chardon P, Marteau P, et al. Reduced diversity of faecal microbiota in Crohn´s disease revealed by a metagenomic approach. Gut. 2006;55(2):205–211. doi:10.1136/gut.2005.073817. PMID: 16188921.
- Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel disease. Proc Natl Acad Sci USA. 2007;104(34):13780–13785. doi:10.1073/pnas.0706625104. PMID: 17699621.
- Pryde SE, Duncan SH, Hold GL, Stewart CS, Flint HJ. The microbiology of butyrate formation in the human colon. FEMS Microbiol Lett. 2002;217(2):133–139. doi:10.1111/J.1574-6968.2002.tb11467.x. PMID: 12480096.
- Rajca S, Grondin V, Louis E, Venier-Massoville G, Grimaud JC, Bouhnik Y, Laharie D, Dupas JL, Pillant H, Picon L, et al. Alterations in the intestinal microbiome (dysbiosis) as a predictor of relapse after infliximab withdrawal in Crohn´s disease. Inflamm Bowel Dis. 2014;20(6):978–986. doi:10.1097/MIB.0000000000000036. PMID: 24788220.
- Ott SJ, Musfeldt M, Wenderoth DF, Hampe J, Brant O, Fölsch UR, Timmis KN, Schreiber S. Reduction in diversity of the colonic mucosa associated bacterial microflora in patients with active inflammatory bowel disease. Gut. 2004;53(5):685–693. doi:10.101136/gut2003.025403. PMID: 15082587.
- Lewis DJ, Chen EZ, Baldassson RN, Otley AR, Griffiths AN, Lee D, Bithinger K, Bailey A, Friedman ES, Hoffmann C, et al. Inflammation, antibiotics, and diet as environmental stressors of the gut microbiome in pediatric Crohn´s disease. Cell Host Microbe. 2015;18(4):489–500. doi:10.1016/j.chom.2015.09.008. PMID:26468751.
- Halfvarson J, Brislawn CJ, Lamendella R, Vazquez-Baeza Y, Walters WA, Bramer LM, D´Amato M, Bonfiglio F, McDonald D, Gonzalez A, et al. Dynamics of the human gut microbiome in inflammatory bowel disease. Nat Microbiol. 2017;2:17004. doi:10.1038/nmicrobiol.2017.4. PMID: 28191884.
- Rojas-Feria M, Romero-García T, Fernández Caballero-Rico JA, Pastor Ramírez H, Avilés-Recio M, Castro-Fernández M, Chueca Porcuna N, Romero-Gómez M, García F, Grande L, et al. Modulation of faecal metagenome in Crohn´s disease: role of microRNAs as biomarkers. World J Gastroenterol. 2018;24(46):5223–5233. doi:10.3748/wjg.v24.i46.5223. PMID: 30581271.
- Andoh A, Imaeda H, Aomatsu T, Inatomi O, Bamba S, Sasaki M, Saito Y, Tsujikama T, Fujiyama Y. Comparison of the fecal microbiota profiles between ulcerative colitis and Crohn´s disease using terminal restriction fragment length polymorphism analysis. J Gastroenterol. 2011;46(4):479–486. doi:10.1007/s00535-010-0368-4. PMID: 21253779.
- Knoll RL, Forslund K, Kultima JR, Meyer CU, Kullmer U, Sunagawa S, Bork P, Gehring S. Gut microbiota differs between children with inflammatory bowel disease and healthy siblings in taxonomic and functional composition: a metagenomic analysis. Am J Physiol Gastrointest Liver Physiol. 2017;312(4):G327–G339. doi:10.1152/ajpgi.00293.2016. PMID: 28039159.
- Franzosa EA, Sirota-Madi A, Avila-Pacheco J, Fornelos N, Haiser HJ, Reinker S, Vatanen T, Hall AB, Mallick H, Mclver LJ, et al. Gut microbiome structure and metabolic activity in inflammatory bowel disease. Natural Microbiol. 2019;4(2):293–305. doi:10.1038/s41564-018-0306-5. PMID: 30531976.
- Lloyd-Price J, Arze C, Ananthakrishnan AN, Schirmer M, Avila-Pacheco J, Poon TW, Andrews E, Ajami NJ, Bonham KS, Brisawn CJ, et al. Multi-omics of the gut microbial ecosystem in inflammatory bowel disease. Nature. 2019;569(7758):655–662. doi:10.1038/s41586-019-1237-9. PMID: 31142855.
- Fujimoto T, Imaeda H, Takahashi K, Kasumi E, Bamba S, Fujiyama Y, Amdoh A. Decrease abundance of Faecalibacterium prausnitzii in the gut microbiota of Crohn´s disease. J Gastroenterol Hepatol. 2013;28(4):613–619. doi:10.1111/jgh.12073. PMID: 23216550.
- Wright EK, Kamm MA, Wagner J, Teo SM, Cruz P, Hamilton AL, Ritchie KJ, Inouye M, Kirkwood CD. Microbial factors associated with postoperative Crohn´s disease recurrence. J Crohns Colitis. 2017;11(2):191–203. doi:10.1093/ecco-jcc/jjw136. PMID: 27466174.
- Vaster-Andersen MK, Mirsepasi-Lauridsen HC, Prosberg MV, Mortensen CO, Träger C, Skovsen K, Thorkilgaard T, Nojgaard C, Vind I, Krogfelt KA, et al. Increased abundance of proteobacteria in aggressive Crohn´s disease seven years after diagnosis. Sci Rep. 2019;9(1):13473. doi:10.1038/s41598-019-49833-3. PMID: 31530835.
- Swidsinski A, Loening-Baucke V, Vaneechoutte M, Doerffel Y. Active Crohn´s disease and ulcerative colitis can be specifically diagnosis and monitored based on the biostructure of fecal flora. Inflamm Bowel Dis. 2008;14(2):147–161. doi:10.101002/ibd.20330. PMID: 18050295.
- Png CW, Lindén SK, Gilshenan KS, Zoetendal EG, McSweeney CS, Sly LI, McGuckin MA, Florin TH. Mucolytic bacteria wit increased prevalence in IBD mucosa augment in vitro utilization of mucin by other bacteria. Am J Gastroenterol. 2010;105(11):2420–2428. doi:10.1038/ajg.2010.281. PMID: 20648002.
- Jacobs JP, Goudarzi M, Singh N, Tong M, McHardy IH, Rvegger P, Asadourian M, Moon B, Ayson A, Borneman Y, et al. A disease-associated microbial and metabolomics state in relatives of pediatric inflammatory bowel disease patients. Cell Mol Gastroenterol Hepatol. 2016;2(6):750–766. doi:10.1016/j.jcmgh.2016.06.004. PMID: 281747747.
- Forbes JD, Van Domselaar G, Bernstein CN. Microbiome survey of the inflamed and non-inflamed gut at different compartments within the gastrointestinal tract of inflammatory bowel disease patients. Inflamm Bowel Dis. 2016;22(4):817–825. doi:10.1097/MIB.0000000000000684. PMID: 26937623.
- Humbel F, Rieder JH, Franc Y, Juillerat P, Scharl M, Misselwitz B, Schreiner P, Begré S, Rogler G, von Känel R, et al. Association of alterations in intestinal microbiota with impaired psychological function in patients with inflammatory bowel disease in remission. Clin Gastroenterol Hepatol. 2019;20. PMID: 31546058. doi:10.1016/j.cgh.2019.09.022.
- Lopez-Siles M, Enrich-Capó N, Aldeguer X, Sabat-Mir M, Duncan SH, Garcia-Gil LJ, Martinez-Medina M. Alterations in the abundance and co-occurrence of Akkermansia muciniphila and Faecalibacterium prausnitzii in the colonic mucosa of inflammatory bowel disease subjects. Front Cell Infect Microbiol. 2018;8:281. doi:10.3389/fcimb.2018.00281. PMID: 30245977.
- Ring C, Klopfleisch R, Dahlke K, Basic M, Bleich A, Blaut M. Akkermansia nuciniphila strain ATCC BAA-835 does not promote short-term intestinal inflammation in gnotobiotic interleukin-10-deficient mice. Gut Microbes. 2019;10(2):180–203. doi:10.1080/19490976.2018.1511663. PMID: 30252588.
- Geerlings SY, Kostopoulos I, de Vos WM, Belzer C. Akkermansia. muciniphila in the human gastrointestinal tract: when, where, and how? Microorganisms. 2018;6(3):75. doi:10.3390/microorganisms6030075. PMID: 30041463.
- Machiels K, Joossens M, Sabino J, De Preter V, Arijs I, Eeckhaut V, Ballet V, Claes K, Van Immerseel F, K V, et al. A decrease of the butyrate-producing species Roseburia hominis and Faecalibacterium prausnitzii defines dysbiosis in patients with ulcerative colitis. Gut. 2014;63(8):1275–1283. doi:10.1136/gutjnl-2013-304833. PMID: 24021287.
- Rajilic-Stojanovic M, Shanahan F, Guarner F, de Vos WM. Phylogenetic analysis of dysbiosis in ulcerative colitis during remission. Inflamm Bowel Dis. 2013;19(3):481–488. doi:10.1097/MIB.0b013E31827fec6d. PMID: 23385241.
- Sokol H, Jegou S, McQuitty C, Straub M, Leducq V, Landman C, Kirchgesner J, Le Gall G, Bourrier A, Nion-Larmurier I, et al. Specificities in the intestinal microbiota in patients with inflammatory bowel disease and Clostridium difficile infection. Gut Microbes. 2018;9(1):55–60. doi:10.1080/19490976.2017.1361092. PMID: 28786749.
- Parada Venegas D, De la Fuente MK, Landskron G, González MJ, Quera R, Dijkstra G, Harmsen HJM, Faber KN, Hermoso MA. Short chain fatty acids (SCFAs)- mediated gut epithelial and immune regulation and its relevance for inflammatory bowel diseases. Front Immunol. 2019;10:277. doi:10.3389/fimmu.2019.00227. PMID: 30915065.
- Peng L, Li ZR, Green RS, Holzman IR, Lin J. Butyrate enhances the intestinal barrier by facilitating tight junction assembly via activation of AMP-activated protein kinase in Caco-2 cell monolayers. J Nutr. 2009;139(9):1619–1625. doi:10.3945/jn.109.104638. PMID:19625695.
- Antharam VC, Li EC, Ishmael A, Sharma A, Mai V, Rand KH, Wang GP. Intestinal dysbiosis and depletion of butyrogenic bacteria in Clostridium difficile infection and nosocomial diarrhea. J Clin Microbial. 2013;51(9):2884–2892. doi:10.1128/JCM.00845-13. PMID: 23804381.
- Wilson BC, Vatanen T, Cutfield WS, O´Sullivan JM. The Super-Donor Phenomenon in fecal microbiota transplantation. Front Cell Infect Microbiol. 2019;9:2. doi:10.3389/fcjmb.2019.00002. PMID: 30719428.
- Kellingray L, Le Gall G, Defernez M, Beales ILP, Franslem-Elumogo N, Narbad A. Microbial taxonomic and metabolic alterations during faecal microbiota transplantation to treat Clostridium difficile infection. J Infect. 2018;77(2):107–118. doi:10.1016/j.jinf.2018.04.012. PMID: 29746938.
- Collins J, Auchtung JM. Control of Clostridium difficile infection by defined microbial communities. Microbiol Spectr. 2017;5(5). doi:10.1128/microbiolspec.BAD-0009-2016. PMID: 28936948.
- Hudson LE, Anderson SE, Corbett AH, Lamb TJ. Gleaning insights from fecal microbiota transplantation and probiotic studies for the rational design of combination microbial therapies. Clin Microbiol Rev. 2017;30(1):191–231. doi:10.1128/CMR.00049-16. PMID: 27856521.
- Shankar V, Hamilton MJ, Khoruts A, Kilburn A, Unno T, Paliy O, Sadowsky MJ. Species and genus level resolution analysis of gut microbiota in Clostridium difficile patients following fecal microbiota transplantation. Microbiome. 2014;2:13. doi:10.1186/2049-2618-2-13. PMID: 24855561.
- Amrane S, Hocquart M, Afouda P, Kuete E, Pham TPT, Dione N, Ngom II, Valles C, Banchar D, Raoult D, et al. Metagenomic and culturomic analysis of gut microbiota dysbiosis during Clostridium difficile infection. Sci Rep. 2019;9:12807. doi:10.1038/s41598-019-49189-8. PMID 31488869.
- Mullish BH, JAK M, Pechlivanis A, Allegratti JR, Kao D, Barker GF, Kapila D, Petrof EO, Joyce SA, Gahan CGM, et al. Microbial bile salt hydrolases mediate the efficacy of faecal microbiota transplant in the treatment of recurrent Clostridioides difficile infection. Gut. 2019;11. PMID: 30816855. doi:10.1136/gutjnl-2018-317842.
- Thoma C. Bile salt involved in the effectiveness of FMT for Clostridium difficile infection. Nat Rev Gastroenterol Hepatol. 2019;16(4):198. doi:10.1038/s41575-019-0128-8. PMID: 30837698.
- Hatziioanou D, Gherghisan-Filip C, Saalbach G, Horn N, Wegmann U, Ducan SH, Flint HJ, Mayer MJ, Narbad A. Discovery of a novel lantibiotic nisin O from Blautia obeum A2-162, isolated from the human gastrointestinal tract. Microbiology. 2017;163(9):1292–1305. doi:10.1099/mic.0.000515. PMID: 28857034.
- Tvede M, Rask-Madsen J. Bacteriotherapy for chronic relapsing Clostridium difficile diarrhoea in six patients. Lancet. 1989;1(8648):1156. doi:10.1016/s0140-6736(89)92749-9. PMID: 2566734.
- Bäumer AJ, Sperandio V. Interactions between the microbiota and pathogenic bacteria in the gut. Nature. 2016;535(7610):85–93. doi:10.1038/nature18849. PMID: 27383983.
- Ng SC, Kamm MA, Yeoh YK, Chan PKS, Zuo T, Tang W, Sood A, Andoh A, Ohmiya N, Zhou Y, et al. Scientific frontiers in faecal microbiota transplantation: joint document of Asia-Pacific association of gastroenterology (APAGE) and Asia-Pacific Society for digestive endoscopy (APSDE). Gut. 2019;14. PMID: 31611298. doi:10.1136/gutjnl-2019-319407.
- Mirpuri J, Raetz M, Sturge CR, Wilhelm CL, Benson A, Savani RC, Hooper LV, Yarovinsky F. Proteobacteria-specific IgA regulates maturation of the intestinal microbiota. Gut Microb. 2014;5(1):28–39. doi:10.4161/gmic.26489. PMID: 24637807.
- Ross CL, Spinter JK, Savidge TC. Structural and functional changes within the gut microbiota and susceptibility to Clostridium difficile infection. Anaerobe. 2016;41:37–43. doi:10.1016/j.anaerobe.2016.05.006. PMID: 2718006.
- Ni J, Wu GD, Albenberg L, Tomov VT. Gut microbiota and IBD: causation or correlation? Nat Rev Gastroenterol Hepatol. 2017;14(10):573–584. doi:10.1038/nrgastro.2017.88. PMID: 28743984.
- Pitts AC, Tuck LR, Faulds-Pain A, Lewis RJ, Marles-Wright J. Structural insight into the Clostridium difficile ethanolamine utilisation microcompartment. PLoS One. 2012;7(10):e48360. doi:10.1371/journal.pone.0048360. PMID: 23144756.
- Stecher B. The roles of inflammation, nutrient availability and the commensal microbiota in enteric pathogen infection. Microbial Spectr. 2015;3(3). doi:10.1128/microbiolspec.MBP-0008-2014. PMID: 26185088.
- Ng KM, Ferreyra JA, Higginbottom SK, Lynch JB, Kashyap PC, Gopinath S, Naidu N, Choudhury B, Weimer BC, Monack DM, et al. Microbiota-liberated host sugars facilitate post-antibiotic expansion of enteric pathogens. Nature. 2013;502(7469):96–99. doi:10.1038/nature12503. PMID: 23995682.
- Passmore IJ, Letertre MPM, Preston MD, Bianconi I, Harrison MA, Nasher F, Kaur H, Hong HA, Baines SD, Cutting SM, et al. Paracresol production by Clostridium difficile affects microbial diversity and membrane interplay of Gram-negative bacteria. PLoS One. 2018;14(9):e1007191. doi:10.1371/journal.ppat.1007191. PMID: 30208103.
- Vidal-Lletjós S, Beaumont M, Torné D, Benamouzig R, Blachier F, Lan A. Dietary protein and amino acid supplementation in inflammatory bowel disease course: what impact on the colonic mucosa? Nutrients. 2017;9(3):310. doi:10.3390/nu9030310. PMID: 28335546.
- Hellmann J, Andersen H, Fei L, Linn A, Bezold R, Lake K, Jackson K, Meyer D, Dirksing K, Bonkowski E, et al. Microbial shifts and shorter time to bowel resection surgery associated with C. difficile in pediatric Crohn´s disease. Inflamm Bowel Dis. 2019;14. PMID 31725875. doi:10.1093/ibd/izz263.
- Crost EH, Tailford LE, Le Gall G, Fons M, Henrissat B, Juge N. Utilisation of mucin glycans by the human gut symbiont Ruminococcus gnavus ls strain-dependent. PLoS One. 2013;8(10):e76341. doi:10.1371/journal.pone.0076341. PMID: 24204617.
- Milani C, Ticinesi A, Gerritsen J, Nouvenne A, Lugli GA, Mancabelli L, Turroni F, Duranti S, Mangifecta M, Viappiani A, et al. Gut microbiota composition and Clostridium difficile infection in hospitalized elderly individuals: a metagenomic study. Sci Rep. 2016;6:25945. doi:10.1038/srep25945. PMID:27166072.
- Shin JH, Gao Y, II JH M, Bolick DT, Kolling GL, Wu M, Warren CA. Innate Immune response and outcome of Clostridium difficile infection are dependent on fecal bacterial composition in the aged host. J Infect Dis. 2018;217(2):188–197. doi:10.1093/infdis/jix414. PMID:28968660.
- Hamilton MJ, Weingarden AR, Unno T, Khoruts A, Sadowsky MJ. High-throughput DNA sequence analysis reveals stable engraftment of gut microbiota following transplantation of previously frozen fecal bacteria. Gut Microbes. 2013;4(2):125–135. doi:10.4161/gmic.23571. PMID: 23333862.
- Zhang X, Deeke SA, Ning Z, Starr AE, Butcher J, Li J, Mayne J, Cheng K, Liao B, Li L, et al. Metaproteomics reveals associations between microbiome and intestinal extracellular vesicle proteins in pediatric inflammatory bowel disease. Nat Commun. 2018;9:2873. doi:10.1038/s41467-018-05357-4. PMID: 30030445.
- Cascio V, Gittings D, Merloni K, Hurton M, Laprade D, Austriaco N. S-Adenpsyl-L. Methionine protects the probiotic yeast, Saccharomyces boulardii, from acid-induced cell death. BMC Microbiol. 2013;13:35. doi:10.1186/1471-2180-13-35. PMID: 23402325.
- Walker LJ, Aldhous MC, Drummond HE, Smith BR, Nimmo ER, Arnott ID, Satsangi J. Anti-Saccharomyces cerevisiae antibodies (ASCA) in Crohn´s disease are associated with disease severity but not NOD2/CARD15 mutations. Clin Exp Immunol. 2004;135(3):490–496. doi:10.1111/j.1365-2249.2003.02392.x. PMID: 15008984.
- Levy AN, Allegretti JR. Insights into the role of transplantation for the treatment of inflammatory bowel disease. Therap Adv Gastroenterol. 2019;12. doi:10.1177/1756284819836893. PMID: 24241245.
- Fisher M, Kao D, Kelly C, Kuchipudi A, Jafri SM, Blumenkehl M, Rex D, Mellow M, Kaur N, Sokol H, et al. Fecal microbiota transplantation is safe and efficacious for recurrent or refractory Clostridium difficile infection with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22(10):2402–2409. doi:10.1097/MIB0000000000000908. PMID: 27580384.
- Chin SM, Sauk J, Mahabamunuge J, Kaplan JL, Hohmann EL, Khalili H. Fecal microbiota transplantation for recurrent Clostridium difficile infection in patients with inflammatory bowel disease: a single center experience. Clin Gastroenterol Hepatol. 2017;15(4):597–599. doi:10.1016/j.cgh.2016.11.028. PMID: 27923723.
- Khoruts A, Rank KM, Newman KM, Viskocil K, Vaughn BP, Hamilton MJ, Sadowsky MJ. Inflammatory Bowel Disease affects the outcome of fecal microbiota transplantation for recurrent Clostridium difficile infection. Clin Gastroenterol Hepatol. 2016;14(10):1433–1438. doi:10.1016/j.cgh.2016.02.018. PMID: 26905904.
- Meighani A, Hart BR, Bourgi K, Miller N, John A, Ramesh M. Outcome of fecal microbiota transplantation for Clostridium difficile infection in patients with IBD. Dig Dis Sci. 2017;62(10):2870–2875. doi:10.1007/s10620-017-4580-4. PMID: 28451916.
- Kahn S, Kahn S, Kashyap P, Laine L, Rubin D, Atreja A, Moore T, Wu G. Update on FMT 2015: indications, methodologies, mechanisms and outlook. Gastroenterology. 2016;159(1):223–237. doi:10.1053/j.gastro.2015.05.008. PMID: 25982290.
- Wang B, Zhang L, Zhu SW, Zhang JD, Duan LP. Short chain fatty acids contribute to gut microbiota-induced promotion of colonic melatonin receptor expression. J Biol Regul Homeost Agents. 2019;33(3):763–771. PMID:31204469.
- Ling Z, Liu X, Jia X, Cheng Y, Luo Y, Yuan L, Wang Y, Zhao C, Guo S, Li L, et al. Impacts of infection with different toxigenic Clostridium difficile strains on feacal microbiota. Sci Rep. 2014;4:7485. doi:10.1038/srep07485. PMID: 25501371.
- Li N, Tian H. Current research progress and thinking of fecal microbiota transplantation for the treatment of gastrointestinal disorders. Zhunghua Wei Chang Ke Za ZHi. 2017;20(10):1104–1108. PMID:29130220.
- Qazi T, Amaratunga T, Barnes EL, Fisher M, Kassam Z, Allegretti JR. The risk of inflammatory bowel disease flares after fecal microbiota transplantation: systematic review and meta-analysis. Gut Microbes. 2017;8(6):574–588. doi:10.1080/19490976.2017.1353848. PMID: 28723262.
- Terveer EM, van Gool T, Ooijevaar RE, Sanders IMJG, Boeije-Koppenol E, Keller JJ, Bart A, Kuijper EJ, Terveer EM, Vendrik K, et al. Human transmission of Blastocystis by fecal microbiota transplantation without development of gastrointestinal symptoms in recipients. Clin Infect Dis. 2019;15. PMID: 31728525. doi:10.1093/cid/ciz1122.
- Zhang T, Lu G, Zhao Z, Liu Y, Shen Q, Li P, Chen Y, Yin H, Wang H, Marcella C, et al. Washed microbiota transplantation vs. manual fecal microbiota transplantation: clinical findings, animal studies and in vitro screening. Protein Cell. 2020;9. PMID: 31919742. doi:10.1007/s13238-019-00684-8.
- Bassos PJ, NOS C, Sales-Campos H. Microbial-based therapies in the treatment of inflammatory bowel disease- an overview of human studies. Front Pharmacol. 2019;9:1571. doi:10.3389/fphar.2018.01571. PMID: 30687107.
- Li Y, Liu M, Zhou J, Hou B, Su X, Liu Z, Yuan J, Li M. Bacillus licheniformis Zhengchangsheng attenuates DSS-induced colitis and modulates the gut microbiota in mice. Benef Microbes. 2019;10(5):543–553. doi:10.3920/BM2018.0122. PMID: 31122042.
- Bjarnason I, Sission G, Hayee B. A randomised, double-blind, placebo-controlled trial of a multi-strain probiotic in patients with asymptomatic ulcerative colitis and Crohn’s disease. Inflammopharmacology. 2019;27(3):446–473. doi:10.1007/s10787-019-00595-4. PMID: 31054010.
- Nagamine T, Matsumoto Y, Nakamura M. Combination probiotics may prevent Clostridium difficile infection among elderly patients undergoing an orthopedic surgery. Biosci Microbiota Food Health. 2019;38(1):31–33. doi:10.12938/bmfh.18-009. PMID: 30705800.
- Mills JP, Rao K, Young VB. Probiotics for prevention of Clostridium difficile infection. Curr Opin Gastroenterol. 2018;34(1):3–10. doi:10.1097/MOG.0000000000000410. PMID: 29189354.
- Dai D, Wang T, Wu S, Gao NL, Chen WH. Metabolic dependencies underlie interaction patterns of gut microbiota during enteropathogenesis. Front Microbiol. 2019;10:1205. doi:10.3389/fmicb.2019.01205. PMID: 31214144.