ABSTRACT
Background
Labour migrants are exposed to potentially traumatic events throughout the migration cycle, making them susceptible to developing mental disorders. Posttraumatic stress disorder (PTSD) is often comorbid with depression. Comorbidity worsens the course of illness, prognosis, treatment response, and increases suicidal risk. Using network analysis, this study examined the structure of PTSD and depression in a sample of migrant domestic workers, an especially vulnerable community of labour migrants. This study sought to derive the central or most important symptoms, strongest edges or relationships among symptoms, and bridge symptoms between PTSD and depression.
Methods
Data were obtained from 1,375 Filipina domestic workers in Macao SAR, China. Data from a subsample of 1,258 trauma-exposed participants were analysed using R software.
Results
Most of the strongest edges were within the same disorder and, for PTSD, within the same symptom cluster. Highest node centrality were PCL-5’s ‘avoid thoughts’, ‘lose interest’, ‘negative emotions’, and ‘not concentrate’, and PHQ-9’s ‘sleep difficulties’. The bridge symptoms were PHQ-9’s ‘sleep difficulties,’ ‘psychomotor agitation/retardation,’ and ‘fatigue,’ PCL-5’s ‘not concentrate’, and PHQ-9’s ‘worthlessness’ and ‘anhedonia’.
Limitations
Results may not generalize to Filipino migrant workers in other occupations and to male migrant workers. Potentially relevant symptoms like somatic symptoms and fear of somatic and mental symptoms were not included.
Conclusions
Central and bridge symptoms are the most important nodes in the network. Developing interventions targeting these symptoms, particularly depression symptoms, is a promising alternative to PTSD treatment given substantial barriers to specialist care for this population.
Antecedentes: Los trabajadores migrantes están expuestos a eventos potencialmente traumáticos durante el ciclo migratorio, tornándolos susceptibles de desarrollar trastornos mentales. El trastorno de estrés postraumático (TEPT) es frecuentemente comórbido con la depresión. La comorbilidad empeora el curso, pronóstico y respuesta al tratamiento de la enfermedad, e incrementa el riesgo suicida. Empleando el análisis en redes, este estudio evaluó la estructura del trastorno de estrés postraumático y la depresión en una muestra de trabajadoras domésticas migrantes, una comunidad especialmente vulnerable de trabajadores migrantes. Este estudio buscó encontrar los síntomas centrales o más importantes, las aristas o relaciones más fuertes entre síntomas, y los síntomas puente entre el TEPT y la depresión.
Métodos: Se obtuvo la información de 1375 trabajadoras domésticas filipinas en la Región Administrativa Especial de Macao, China. La información de un subgrupo de 1258 participantes expuestos a trauma fue analizada empleando el lenguaje de programación R.
Resultados: La mayoría de las aristas más fuertes se encontraban dentro del mismo trastorno y, para el TEPT, dentro del mismo racimo de síntomas. Los más altos en centralidad fueron ‘evitar pensamientos’, ‘pérdida de interés’, ‘emociones negativas’, y ‘falta de concentración’ de la Lista de Chequeo de Síntomas Postraumáticos para el DSM-5 (PCL-5, por sus siglas en inglés), y ‘dificultades en el sueño’ del Cuestionario sobre la Salud del Paciente (PHQ-9, por sus siglas en inglés). Los síntomas puente fueron ‘dificultades en el sueño’, ‘agitación/retraso psicomotor’ y ‘fatiga’ del PHQ-9, ‘falta de concentración’ de la PCL-5, e ‘inutilidad’ y ‘anhedonia’ del PHQ-9.
Limitaciones: Los resultados pueden no ser generalizables a trabajadores migrantes filipinos de otras ocupaciones, y a trabajadores migrantes varones. No se incluyeron síntomas potencialmente relevantes, tales como síntomas somáticos, y miedo a los síntomas somáticos y mentales.
Conclusiones: Los nodos más importantes en las redes fueron los síntomas centrales y los síntomas puente. Una alternativa promisoria para tratar estos síntomas es el desarrollar intervenciones específicas para estos, en particular hacia síntomas depresivos, dadas las barreras sustanciales para el acceso a tratamiento especializado para esta población.
背景: 劳务移民在整个移民周期都暴露于潜在创伤事件, 使其易感精神疾病。创伤后应激障碍 (PTSD) 常与抑郁症共病。并发症会加重病程, 预后, 治疗反应并增加自杀风险。本研究使用网络分析在一个移民家庭佣工样本中考察了PTSD和抑郁症的结构, 此样本是劳务移民中尤其易感的群体。本研究试图得出核心或最重要的症状, 最强边或症状之间的关系, 以及PTSD和抑郁症之间的桥症状。
方法: 数据来自中国澳门特区的1375名菲律宾家庭佣工。使用R软件分析了1258名创伤暴露参与者子样本的数据。
结果: 大多数最强边在同一疾病内, 对于PTSD则在同一症状簇内。中心性最高的是PCL-5的‘回避想法’, ‘兴趣缺失’, ‘负性情绪’和‘注意力不集中’, 以及PHQ-9的‘睡眠困难’。桥症状是PHQ-9的‘睡眠困难’, ‘精神运动性激越/迟滞’和‘疲劳’, PCL-5的‘注意力不集中’以及PHQ-9的‘无价值感’和‘快感缺失’。
局限性: 结果可能无法推广到其他职业的菲律宾移民工人和男性移民工人。未纳入潜在的相关症状, 如躯体症状以及对躯体和精神症状的恐惧。
结论: 中心和桥症状是网络中最重要的结点。鉴于针对此人群的专科护理存在重大障碍, 针对这些症状 (尤其是抑郁症状) 的干预措施是有希望替代PTSD治疗的方法。
There are 11.5 million migrant domestic workers around the globe (Gallotti & Branch, Citation2015; Jones, Ma, & McNally, Citation2017). Migrant domestic workers are valuable in their home countries and receiving countries. They send remittances to their families regularly, which are then used to pay for daily expenses and children’s education (Garabiles, Ofreneo, & Hall, Citation2017). They are important to receiving countries not just in terms of caregiving but also economically. For example, migrant domestic workers contribute 21 billion USD a year in Malaysia, Hong Kong, and Singapore (Experian Asia Pacific & Enrich HK, Citation2019).
Figure 1. Network of PTSD and depression symptoms in a sample of Filipina domestic workers. Parsimonious network using LASSO estimation is shown. There are 190 non-zero edges (represented by lines linking the symptoms) out of total 378 possible edges.
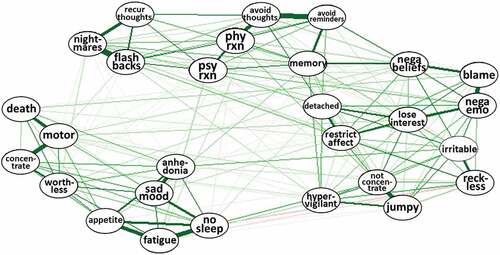
Figure 2. Strength centrality index of the network structure of PTSD and depression symptoms (in standardized z-scores). Nodes with higher strength are represented by higher z-scores.
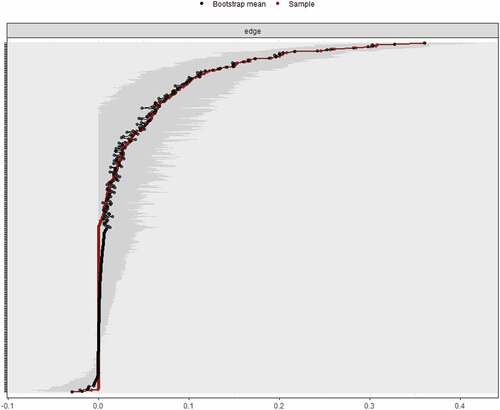
Figure 3. Bootstrapped difference tests result between node strength. Black boxes represent significant differences between nodes.
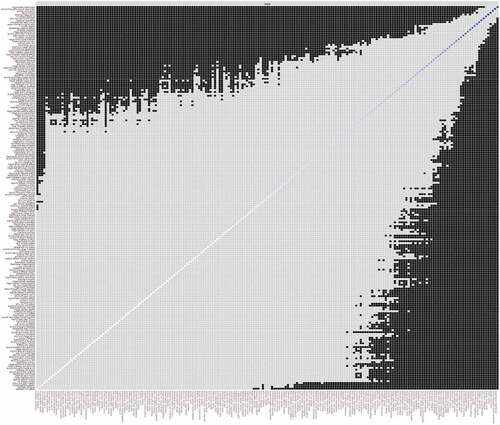
Figure 4. Network of PTSD and depression symptoms showing bridge symptoms in a sample of Filipina domestic workers.
Figure 5. Bridge strength centrality index of the network structure between PTSD and depression symptoms. Bridge symptoms with higher strength are represented by higher z-scores.
Figure 6. Bridge strength centrality index of the network structure between PTSD and depression symptoms. Bridge symptoms with higher strength are represented by higher z-scores.
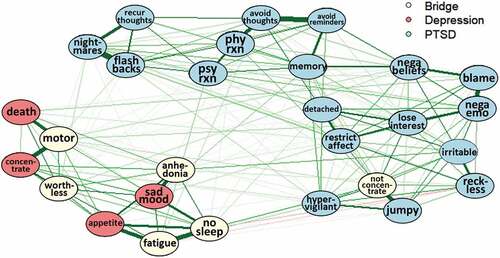
Figure 5. Bridge strength centrality index of the network structure between PTSD and depression symptoms. Bridge symptoms with higher strength are represented by higher z-scores.
In spite many contributions, migrant workers are often exposed to many potentially traumatic events (PTEs) when they were still in their home countries, while in transit, and while abroad (Zimmerman, Kiss, & Hossain, Citation2011). Migrant domestic workers are especially vulnerable to exploitation and physical, verbal, and sexual abuse (Hall, Garabiles, & Latkin, Citation2019; Ignacio & Mejia, Citation2009; Lee, Citation2012; Vargas, Garabiles, & Hall, Citation2020). They experience labour violations, including lack of working contracts, long working hours, underpayment, and lack of rest days, annual leaves, food, and appropriate sleeping accommodations (Hall et al., Citation2019; Ignacio & Mejia, Citation2009; Vargas et al., Citation2020). They also experience familial problems, including lack of finances for their families’ needs, misunderstandings with children, and jealousy and infidelity from their spouses (Garabiles et al., Citation2017; Hall et al., Citation2019; Vargas et al., Citation2020). In addition to these postmigration stressors that worsen mental health, PTEs experienced historically during migration and indirectly to their family members increase the risk for posttraumatic stress disorder (PTSD; Hall et al., Citation2019).
PTSD is a common mental disorder, experienced after a traumatic life event, and consists of four symptom clusters: intrusion symptoms or re-experiencing of traumatic event; persistent avoidance; negative alterations in cognitions and mood; and alterations in arousal and reactivity (American Psychiatric Association, Citation2013). PTSD is a debilitating disorder that is linked to significant disability, physical and somatic complaints, and impaired functioning (Greene, Neria, & Gross, Citation2016).
PTSD is highly comorbid with other common mental disorders, such as depression (Brady, Killeen, Brewerton, & Lucerini, Citation2000; Greene et al., Citation2016; La Greca, Danzi, & Chan, Citation2017; Spinhoven, Penninx, van Hemert, de Rooij, & Elzinga, Citation2014). Among those diagnosed with PTSD, 23%-71% (Greene et al., Citation2016) and as high as 90% (Ramsawh et al., Citation2014) to 95% (Bleich, Koslowsky, Dolev, & Lerer, Citation2018) also had comorbid depression. Comorbidity complicates the course of illness and response to treatment (Mueser & Drake, Citation2007). Those diagnosed with both PTSD and with depression also have a poorer prognosis (Campbell et al., Citation2007; Green et al., Citation2006) and are at greater risk for suicide than those with only PTSD or only depression (Campbell et al., Citation2007; Ramsawh et al., Citation2014).
Comorbidity has traditionally been viewed from the latent variable perspective, which posits that comorbidity is due entirely to a common, unobserved factor (Cramer, Waldorp, van der Maas, & Borsboom, Citation2010; Eaton, Citation2015; Krueger, Citation1999). Therefore, the correlation between PTSD and depression is caused by a higher-order latent variable, which should then be the treatment focus (Cramer et al., Citation2010). A study found that the PTSD dysphoria factor accounted for the shared variance between PTSD and somatic depression, while PTSD’s negative alterations in cognitions and mood factor and arousal factor accounted for the shared variance between PTSD and non-somatic depression (Contractor, Greene, Dolan, & Elhai, Citation2018).
An alternative approach is the network model framework, which has increasingly been applied in psychopathology research. The network model emphasizes the role of symptoms, their interactions, and how they overlap and influence each other (Borsboom & Cramer, Citation2013; Cramer et al., Citation2010; Hofmann, Curtiss, & McNally, Citation2016). The network model posits that comorbidity is due to direct relationships between symptoms from two disorders, which are called bridge symptoms (Cramer et al., Citation2010). When bridge symptoms are targeted during treatment, their suppression may stop the activation of other symptoms (Afzali et al., Citation2017; Borsboom & Cramer, Citation2013; Cramer et al., Citation2010; Fried et al., Citation2017; Hofmann et al., Citation2016; McNally, Citation2016). A PTSD and depression comorbidity study found several bridge symptoms, namely, sleep problems, irritability, and concentration difficulties, from both disorders (Afzali et al., Citation2017). Without overlapping symptoms, bridge symptoms included PTSD symptom flashbacks and foreshortened future, and depression symptom guilt, sadness, and psychomotor retardation (Afzali et al., Citation2017).
The network model also investigates centrality which indicates the most important symptoms, also called nodes, within the network (Epskamp, Borsboom, & Fried, Citation2018). When central symptoms are targeted in treatment, symptom severity decreases across the entire symptom network (Papini, Rubin, Telch, Smits, & Hien, Citation2019). Network analysis studies that just investigated PTSD network structures (sans depression symptoms) found different central symptoms, such as concentration difficulties (Birkeland & Heir, Citation2017; Sullivan, Smith, Lewis, & Jones, Citation2016), intrusive thoughts/memories (Fried et al., Citation2018; Mancini, Littleton, Grills, & Jones, Citation2019; Mitchell et al., Citation2017; Sullivan et al., Citation2016), detachment (Birkeland & Heir, Citation2017; Fried et al., Citation2018; Sullivan et al., Citation2016), irritability, foreshortened future (Bryant et al., Citation2017), persistent negative emotional state, avoiding reminders/thoughts, inability to experience positive emotions, and distressing dreams (Mitchell et al., Citation2017). There is also cross-cultural variability. For example, symptoms of somatic distress and fear of anxiety (e.g. fear of having tired limbs, having cold hands and feet, having tinnitus) are important to Cambodian culture, along with PTSD avoidance/numbing cluster (Hinton & Lewis-Fernandez, Citation2011; Hinton, McNally, Fairfax, & Harachi, Citation2020). In a sample of refugees and asylum seekers in Switzerland, central PTSD symptoms include emotional and physical cue reactivity, self-destructive behaviour, negative emotional state, and exaggerated startle response (Spiller et al., Citation2017), whereas in a sample of Chinese earthquake survivors, central symptoms include hypervigilance, concentration impairments, dreams about trauma, and foreshortened future (McNally et al., Citation2015). These inconsistencies suggest that findings cannot simply be generalized to different populations. Therefore, additional studies are warranted especially within unique populations.
Another vital element in the network model are edges, which represent relationships between two symptoms or nodes (Epskamp et al., Citation2018). Edges differ in terms of edge weights or strength of linkages. In a study on comorbidity between PTSD and depression, strongest edge weights consisted of edges between PTSD symptom detachment and emotional numbness, and being on guard and easily startled; and edges between depression symptom discouragement and hopelessness, and reduced appetite and weight loss (Afzali et al., Citation2017). Without overlapping symptoms, the strongest edges were between PTSD and depression symptoms: unable to recall events and guilt; flashbacks and guilt; and foreshortened future and depression symptoms thinking of death, sadness, and hopelessness (Afzali et al., Citation2017).
This study uses network analysis to investigate the structure of PTSD in a sample of Filipina migrant domestic workers and its comorbidity with depression. There are roughly 500,000 Filipina migrant domestic workers across the globe, which is one-fourth of all Overseas Filipino Workers (Philippine Statistics Authority, Citation2017). In Macao SAR, People’s Republic of China where this study was conducted, Filipina migrant workers make up half of all migrant domestic workers in the territory (Government of the Macao Special Administrative Region – Labour Affairs Bureau, Citation2019).
This study contributes to scant literature that utilized network modelling in culturally diverse communities. Using the network model enables identification of bridge and central symptoms. Knowledge of bridge symptoms would allow for greater targeted treatment, whereas knowledge of central symptoms will help determine other important symptoms in the network. These are especially crucial for individuals with PTSD and depression who are more likely to drop out from treatment (Flory & Yehuda, Citation2015). Further, more targeted treatment is especially important when working with marginalized groups like migrant domestic workers. Apart from problems at work and with their families, their support system, access to services, and their resources – both time and financial – to engage in psychological treatment are also limited (Garabiles et al., Citation2017; Hall et al., Citation2019). These barriers to mental health care suggest that treatment for this population needs to be especially efficient, which may be achieved with the knowledge on the network structure of common mental health disorders like PTSD and depression.
1. Method
1.1. Participants
There were 1,375 Filipina domestic workers recruited through respondent-driven sampling. All were adults, over 18 years of age, and working legally in Macao SAR. For this study, a subsample consisting of 1,258 participants who reported index traumatic event in the LEC-5 and self-reported PTSD symptoms associated with this event was analysed. From this subsample, 27.2% met criteria for PTSD and 39.9% met criteria for depression. Cut-off scores were 25 for PCL-5 and 6 for PHQ-9, which were based on validation studies with Filipina domestic workers (Garabiles et al., Citation2019; Hall et al., Citation2019).
1.2. Measures
1.2.1. LEC-5
Participants answered a 24-item adaptation of the Life Events Checklist for DSM-5 (LEC-5; Weathers et al., Citation2013). The original LEC-5 assesses 17 potentially traumatic events that the participants may have experienced in their lifetime, such as natural disasters, accidents, and assault. Seven items about workplace abuse and trauma associated with separation from family were added. These items were based on a qualitative study on stressors experienced by Filipina domestic workers (Hall et al., Citation2019). Participants indicated if the potentially traumatic events happened to them personally, if they witnessed it happen to another person, if they learned about it happening to a close family member or friend, if it happened to them as part of their job, if they are not sure if they were exposed or if they experienced it, or if they were never exposed or they never experienced the event. They then reported which was the worst traumatic event they were exposed to or experienced.
1.2.2. PCL-5
The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5; Weathers et al., Citation2013) was used. We used 19 of 20 items from the PCL-5. We excluded the sleep item because preliminary analysis showed that including PCL-5 and PHQ-9 sleep items were conceptually redundant. Their correlation was moderately strong (r = 0.487, p < 0.01) and is significantly stronger than the next highest correlation which was between PCL-5’s memory difficulties and PHQ-9’s depressed/sad mood (r = 0.361, p < 0.01), with z score = 3.86, p < 0.001.
Participants rated their PTSD symptoms with regard to the worst traumatic event from LEC-5. PCL-5 items are rated from ‘0’ or ‘not at all’ to ‘4’ or ‘extremely’. Scores range from 0 to 76. Higher scores denote higher posttraumatic stress levels. An item is ‘Feeling distant or cut-off from other people’. A study with Filipina domestic workers found PCL-5 reliable in terms of internal consistency and test-retest analysis (alpha = 0.95 and Spearman’s rank correlation coefficient = 0.58), and demonstrated criterion, discriminant, and convergent validity (Hall et al., Citation2019). In the current study, PCL-5 demonstrated excellent reliability (alpha = 0.96).
1.2.3. PHQ-9
The official Filipino version of Patient Health Questionnaire – 9 (PHQ-9; Kroenke & Spitzer, Citation2002) was used to measure depression. PHQ-9 has nine items which are rated from ‘0’ or ‘not at all’ to ‘3’ or ‘nearly every day’. PHQ-9 includes items like ‘Feeling down, depressed, or hopeless’. Scores range from 0 to 27, with higher scores denoting higher depression levels. A study with Filipina domestic workers showed PHQ-9 to be reliable, with high internal consistency (alpha = 0.78) and acceptable test-retest reliability (Spearman’s rank correlation coefficient = 0.43), and valid (Garabiles et al., Citation2019). Cronbach’s alpha was excellent in the current study (0.88).
1.3. Procedure
Data were collected in Macao SAR. Participants were recruited through respondent-driven sampling, a chain-referral recruitment method (Salganik & Heckathorn, Citation2004). We identified ‘seeds’ or well-networked members of the Filipino community in Macao and trained them to recruit peers into the study. The study was described as having the aim of assessing the overall health of Filipino migrant domestic workers.
Participants were first provided with consent forms. They were assured of the confidentiality of information they will share in the survey. They then answered the survey, which included PCL-5 and PHQ-9. Participants provided their consent and answered the survey using iPads. Research assistants were available to assist them in answering the survey and to answer questions regarding study’s purpose and recruiting participants. After completion of survey, they were given 100 MOP (12 USD) as compensation. They were then asked if they wanted to invite five other domestic workers to become the next ‘chain’ of participants. Those who agreed were trained how to invite participants using recruitment coupons. They were remunerated 20 MOP (2.5 USD) for each recruit who completed the survey. The study was approved by the Research Ethics Panel of the University of Macau, Macao (SAR), China.
1.4. Data analysis
Data from PCL-5 and PHQ-9 were analysed using R, a programming language and statistical software (R Core Team, Citation2018). The R package ‘huge’ was used to make nonparanormal transformation (Jiang et al., Citation2020). To investigate relationships among symptoms, polychoric correlations were computed. Graphical Gaussian Model (GGM) was then estimated using ‘qgraph’ package that uses graphic LASSO and EBIC model (Epskamp et al., Citation2018; Epskamp, Cramer, Waldorp, Schmittmann, & Borsboom, Citation2012). Thicker lines denote stronger relationships between symptoms. Green lines represent positive relationships and red lines represent negative relationships. Strength centrality index was computed to identify central or most important symptoms in the network (Epskamp et al., Citation2018; Fried et al., Citation2018). ‘Bootnet’ package was used to examine strength index stability, with correlation stability coefficient of 0.25 as cut-off (Epskamp et al., Citation2018). We then utilized the bridge function from ‘networktools’ package (Jones, Citation2017) to identify bridge symptoms and to determine bridge strength centrality index, or total connections of a symptom to the other disorder (Jones, Citation2019; Jones et al., Citation2017).
2. Results
shows the items, item content, item abbreviations, sample means, and standard deviations. Overall, participants had low levels of PTSD (M = 17.63, SD = 13.66) and depression symptoms (M = 5.04, SD = 5.39).
Table 1. Item, item content, item abbreviation, means, and standard deviations for PCL-5 and PHQ-9.
The network structure of PTSD and depression in shows that items from the same measure clustered together. We will report the top 30 edges out of the total 190 non-zero edges, all of which differ from at least half of the other edges. All top 30 strong edges were between symptoms from the same disorder (see and ).
Majority of the edges between PCL-5 items were from within the same cluster. Among intrusion symptoms, ‘recurring thoughts’, ‘nightmares’, and ‘flashbacks’ were linked to one another. ‘Psychological reaction’ is also connected to ‘physiological reaction’ and ‘flashbacks’. The two persistent avoidance symptoms (‘avoiding thoughts’ and ‘avoiding reminders’) also formed an edge.
Among symptoms from negative alterations in cognition and mood cluster, ‘loss of interest’ shared the most edges, specifically with ‘negative emotions’, ‘detached’, and ‘restricted affect’. ‘Blame’ was linked to both ‘negative emotions’ and ‘negative beliefs’, while ‘negative beliefs’ also connected with ‘memory difficulties’. ‘Detached’ and ‘restricted affect’ were also connected.
For increased the arousal cluster, ‘jumpy’ was related to ‘concentration difficulties’ and ‘hypervigilant’, whereas ‘irritable’ and ‘reckless’ formed an edge. The remaining three edges between PCL-5 symptoms were from different clusters, namely, between ‘physiological reaction’ and ‘avoiding thoughts’, ‘avoiding reminders’ and ‘memory difficulties’, and ‘psychological reaction’ and ‘avoiding thoughts’.
The rest of the strongest edges were between PHQ-9 items. ‘Depressed/sad mood’ was linked to ‘anhedonia’, ‘sleep difficulties’, ‘worthlessness’, and ‘fatigue’. ‘Sleep difficulties’ were also related to ‘fatigue’ and ‘appetite changes’. ‘Fatigue’ likewise connected with ‘appetite changes’. ‘Concentration difficulties’ were linked to both ‘psychomotor agitation/retardation’ and ‘worthlessness’. Finally, ‘psychomotor agitation/retardation’ and ‘thoughts of death’, and ‘anhedonia’ and ‘appetite changes’ formed edges.
The strength centrality index was stable, C S (cor = 0.7) = 0.75. PCL-5’s ‘avoid thoughts’ had the highest strength, followed by PCL-5’s ‘lose interest’, ‘negative emotions’, and ‘not concentrate’, and PHQ-9’s ‘sleep difficulties’ (see ). Bootstrapped difference test results in showed that the PCL-5 symptoms were significantly different in strength from most of the other nodes, whereas PHQ-9’s ‘sleep difficulties’ did not differ significantly than most nodes.
Bridge strength results indicated six bridge symptoms (see and ). These were PHQ-9’s ‘sleep difficulties’, ‘psychomotor agitation/retardation’, and ‘fatigue’ followed by PCL-5’s ‘not concentrate’. Other bridge symptoms were PHQ-9’s ‘worthlessness’ and ‘anhedonia’.
3. Discussion
This study investigated the network structure of PTSD and depression among Filipina migrant domestic workers. Network modelling is a novel approach to examine comorbidity and has not been extensively applied to culturally diverse populations like migrant domestic workers (e.g. Garabiles, Lao, Xiong, & Hall, Citation2019; Spiller et al., Citation2017). This study contributes to addressing these gaps. This is also the first to examine PTSD and depression’s network structure in a community of migrant domestic workers.
The finding that symptoms from the same disorder converged and that PTSD symptoms from the same cluster grouped together support the distinctiveness between PTSD and depression, and among PTSD clusters. Some of these edges have been found in a past study on PTSD and depression comorbidity, namely, between PTSD symptoms ‘jumpy’ and ‘hypervigilant’, and ‘detached’ and ‘restricted affect’ (Afzali et al., Citation2017). Other edges were also found in past network studies on just PTSD, such as ‘loss of interest’ and ‘detached’, ‘avoiding thoughts’ and ‘avoiding reminders’, ‘concentration difficulties’ and ‘jumpy’, ‘psychological reaction’ and ‘physiological reaction’, ‘irritable’ and ‘reckless’, and among ‘recurring thoughts’, ‘nightmares’, and ‘flashbacks’ (Birkeland & Heir, Citation2017; Bryant et al., Citation2017; Fried et al., Citation2018; Mancini et al., Citation2019; McNally et al., Citation2015; Spiller et al., Citation2017). Past studies on depression and other disorders found similar edges among depression symptoms, such as between ‘depressed’ and ‘anhedonia’, ‘sleep difficulties’ and ‘fatigue’, ‘psychomotor agitation/retardation’ and ‘concentration difficulties’, ‘psychomotor agitation/retardation’ and ‘thoughts of death’, ‘depressed’ and ‘sleep difficulties’, and between ‘depressed’ and ‘fatigue’ (Beard et al., Citation2016; Cramer et al., Citation2010; Garabiles et al., Citation2019; Schuler, Wittmann, Faller, & Schultz, Citation2018).
Depression’s sleep symptom is a bridge symptom and a central node, albeit only stronger than a few other nodes. These findings support a past network analysis on comorbidity between PTSD and depression (Afzali et al., Citation2017). Sleep disturbance was also an issue among labour migrant workers (e.g. caregivers, farmworkers) (Riley, Nazareno, & Malish, Citation2016; Sandberg et al., Citation2012). Sleep disturbance is a hallmark symptom for domestic workers, whose sleep arrangement when abroad is usually suboptimal. Many who live in their employers’ homes sleep in makeshift rooms like balconies or closets (Hall et al., Citation2019; Mission for Migrant Workers, Citation2017). They are expected to stay awake until late hours and wake-up during early morning hours to attend to their employers’ needs (Hall et al., Citation2019; Vargas et al., Citation2020). Maintaining adequate sleep is also problematic among those who live separately from their employers due to overcrowding. They share an apartment designed for a family of 4 with 2–3 times that number of occupants (Hall et al., Citation2019).
PCL-5’s concentration difficulties are also both a central and bridge symptom. This is consistent with earlier findings on comorbidity between PTSD and depression (Afzali et al., Citation2017) and between PTSD and other disorders like GAD and OCD (Jones et al., Citation2017; Jones, Mair, Riemann, Mugno, & McNally, Citation2018). Among migrant domestic workers, difficulty concentrating was associated with stress, burnout, and poor overall mental health (Hall et al., Citation2019). This node may also be a manifestation of the thinking a lot syndrome, which is an idiom of distress reported in various cultures (Hinton, Barlow, Reis, & de Jong, Citation2016) and populations, including among Filipino domestic workers (Hall et al., Citation2019).
PHQ-9 items ‘fatigue’ and ‘psychomotor agitation/retardation’ are likewise important to the network. ‘Fatigue’ is a bridge symptom, which aligns with findings from comorbidity studies, though between depression and anxiety, and PTSD and anxiety (Garabiles et al., Citation2019; Jones et al., Citation2017). ‘Psychomotor agitation/retardation’ was a bridge in a study on PTSD and depression (Afzali et al., Citation2017) and in a comorbidity study on depression, albeit with anxiety instead of with PTSD (Jones et al., Citation2017). Somatic distress was also important in the network structure in a Cambodian population (Hinton et al., Citation2020). Migrant domestic workers engage in highly physical work and long work hours, coupled with Filipinos’ somaticizing tendencies as expression of stress (Mordeno, Carpio, Mendoza, & Hall, Citation2018; Tuliao, Ang, Garabiles, Tuliao, & Samaco-Zamora, Citationin press), make them susceptible to fatigue and motor difficulties (Hall et al., Citation2019).
Depression symptoms ‘anhedonia’ and ‘worthlessness’ are also bridge symptoms. Past studies have shown the importance of anhedonia as a depression symptom, albeit in networks of depression and anxiety (Beard et al., Citation2016; Garabiles et al., Citation2019). A study on Filipina domestic workers found that some experience a depression-like syndrome, which includes the inability to feel better even when trying to engage in coping strategies like praying (Hall et al., Citation2019). Further, it is not uncommon for them to feel worthless. Apart from exposure to PTEs and experience of sadness, migrant domestic workers are often appraised as inadequate by their families and employers (Garabiles et al., Citation2017; Hall et al., Citation2019; Vargas et al., Citation2020). Their sacrifice of working abroad is usually insufficient given the inability to fully deliver as breadwinners and mothers. It is common for them to have employers who are unsatisfied with their output despite their effort and long hours at work.
PTSD symptom ‘avoid thoughts’ is another central node in the network. This supports results from past network analyses on PTSD where avoidance symptoms were central nodes (Hinton et al., Citation2020; Mancini et al., Citation2019; Mitchell et al., Citation2017). This also supports findings that avoidance is salient in groups where it is deemed a culturally acceptable coping mechanism (Hinton & Lewis-Fernández, Citation2011), particularly in collectivist cultures (Chun, Moos, & Cronkite, Citation2006) such as the Philippines. In the case of Filipina domestic workers, one way they avoid negative thoughts is by engaging in religious services as a form of distraction and temporary stress relief (Nakonz & Shik, Citation2009). However, given that PTSD symptom experience of ‘negative emotions’ is also a strong node in the network, avoidance as a coping mechanism might not be effective in the long term.
Further, ‘avoid thoughts’ and ‘negative emotions’ may be manifestations of the thinking a lot syndrome, much like ‘concentration difficulties’ (Hinton et al., Citation2016). Efforts to block thoughts are futile as these come back to mind. When in one’s consciousness again, negative emotions are felt like feeling upset about their situation.
Results point to suggestions for interventions. Most of the bridge symptoms are depression items. Sleep disturbance is a transdiagnostic symptom found in many common mental disorders. Focusing on sleep intervention may be advantageous among communities who seldom have access to trained specialists who can deliver PTSD treatment. Moreover, PTSD and trauma-focused treatments may not be well tolerated during migration given the lack of social support (Hall, Pangan, Chan, & Huang, Citation2019) and the demands of the living and working context. These treatments are also associated with high dropout rates because clients try to avoid recalling traumatic experiences (Flory & Yehuda, Citation2015). Targeting sleep and other depression symptoms that bridge the two disorders could boost retention and potentially reduce PTSD symptoms. Alternative scalable treatment approaches including digital or electronic mental health and behavioural activation may be well tolerated and offer a solution to meet the needs of the wider community (Garabiles, Harper-Shehadeh, & Hall, Citation2019; Hall, Shi, Garabiles, & Chan, Citation2018).
Sleep disturbance, psychomotor agitation/retardation, fatigue, concentration difficulties, and negative emotions could be addressed through psychoeducation. Domestic workers could learn relaxation techniques, eating healthy, and cognitive restructuring. Coaching them to contact families regularly and to seek support while abroad (e.g. from religious figures, NGOs, consulate) could strengthen their support system. At the policy level, work hours and sleeping arrangements need to be regulated so they can recover from their highly physical work. Migration governance of both Philippine and Macao’s governments also needs to be improved to lessen exposure to PTEs like abusive employers, agencies, and unfair labour contracts that can worsen mental health.
This is the first study known to examine patterns of depression and PTSD comorbidity among a population of vulnerable labour migrants. Sample size was large, representing >10% of the target population. The instruments used to assess depression and PTSD were validated for use in this population. The strength centrality index is also highly stable (above 0.50) (Epskamp et al., Citation2018). Despite these strengths, the study has several limitations. Results may not generalize to male overseas Filipino workers and to those employed in other labour sectors. Moreover, the traumatic experiences of participants are varied and accumulative (e.g. exposure to natural disasters, abuse). Results may not generalize to populations exposed to only one type of traumatic experience (e.g. only exposed to abuse). Further, symptoms that may have been relevant to the population (e.g. somatic symptoms and fear of somatic and mental symptoms) were not included in the analyses.
Future research can investigate the efficacy of interventions for this community. One such intervention is sleep-specific cognitive-behavioural therapy, which was found efficacious in treating PTSD symptoms (Ho, Chan, & Tang, Citation2016). Future network analyses can examine relationships of PTSD symptoms with somatic symptoms and fear of somatic and mental symptoms.
Authors’ statement
No funding bodies had any role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Contributors
Conceptualization and research design were by BJH. First draft of the paper was written by MRG. Data were analyzed by MRG, CKL, and SW. Revisions were written by CKL, SW, and BJH. All authors were involved in editing the paper for intellectual content. All authors approved the final paper.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Afzali, M. H., Sunderland, M., Teesson, M., Carragher, N., Mills, K., & Slade, T. (2017). A network approach to the comorbidity between posttraumatic stress disorder and major depressive disorder: The role of overlapping symptoms. Journal of Affective Disorders, 208, 490–13.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author.
- Beard, C., Millner, A. J., Forgeard, M. J. C., Fried, E. I., Hsu, K. J., Treadway, M., … Björgvinsson, T. (2016). Network analysis of depression and anxiety symptom relations in a psychiatric sample. Psychological Medicine, 46(16), 3359–3369.
- Birkeland, M. S., & Heir, T. (2017). Making connections: Exploring the centrality of posttraumatic stress symptoms and covariates after a terrorist attack. European Journal of Psychotraumatology, 8(sup3), 1333387.
- Bleich, A., Koslowsky, M., Dolev, A., & Lerer, B. (2018). Post-traumatic stress disorder and depression: An analysis of comorbidity. British Journal of Psychiatry, 170(5), 479–482.
- Borsboom, D., & Cramer, A. O. J. (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9, 91–121.
- Brady, K. T., Killeen, T. K., Brewerton, T., & Lucerini, S. (2000). Comorbidity of psychiatric disorders and posttraumatic stress disorder. The Journal of Clinical Psychiatry, 61(sup7), 22–32.
- Bryant, R. A., Creamer, M., O’Donnell, M., Forbes, D., McFarlane, A. C., Silove, D., & Hadzi-Pavlovic, D. (2017). Acute and chronic posttraumatic stress symptoms in the emergence of posttraumatic stress disorder: A network analysis. JAMA Psychiatry, 74(2), 135–142.
- Campbell, D. G., Felker, B. L., Liu, C.-F., Yano, E. M., Kirchner, J. E., Chan, D., … Chaney, E. F. (2007). Prevalence of depression-PTSD comorbidity: Implications for clinical practice guidelines and primary care-based interventions. Journal of General Internal Medicine, 22(6), 711–718.
- Chun, C.-A., Moos, R. H., & Cronkite, R. C. (2006). Culture: A fundamental context for the stress and coping paradigm. In P. T. P. Wong & L. C. J. Wong (Eds.), International and cultural psychology series. Handbook of multicultural perspectives on stress and coping (pp. 29–53). Boston, MA: Spring Publications. doi:10.1007/0-387-26238-5_2
- Contractor, A. A., Greene, T., Dolan, M., & Elhai, J. D. (2018). Relations between PTSD and depression symptom clusters in samples differentiated by PTSD diagnostic status. Journal of Anxiety Disorders, 59, 17–26.
- Cramer, A. O. J., Waldorp, L. J., van der Maas, H. L., & Borsboom, D. (2010). Comorbidity: A network perspective. Behavioral and Brain Sciences, 33(2–3), 137–150.
- Eaton, N. R. (2015). Latent variable and network models of comorbidity: Toward an empirically derived nosology. Social Psychiatry and Psychiatric Epidemiology, 50(6), 845–849.
- Epskamp, S., Borsboom, D., & Fried, E. I. (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50(1), 195–212.
- Epskamp, S., Cramer, A. O. J., Waldorp, L., Schmittmann, V., & Borsboom, D. (2012). qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software, 48(4), 1–18.
- Experian Asia Pacific, & Enrich HK. (2019). The value of care: Key contributions of migrant domestic workers to economic growth and family well-being in Asia. Retrieved from http://www.enrichhk.org/wp-content/uploads/2019/02/Final_The-Value-of-Care_Full-Report.pdf
- Flory, J. D., & Yehuda, R. (2015). Comorbidity between post-traumatic stress disorder and major depressive disorder: Alternative explanations and treatment considerations. Dialogues in Clinical Neuroscience, 17(2), 141–150.
- Fried, E. I., Eidhof, M. B., Palic, S., Costantini, G., Huisman-van Dijk, H. M., Bockting, C. L. H., … Karstoft, K.-I. (2018). Replicability and generalizability of posttraumatic stress disorder (PTSD) networks: A cross-cultural multisite study of PTSD symptoms in four trauma patient samples. Clinical Psychological Science, 6(3), 335–351.
- Fried, E. I., van Borkulo, C. D., Cramer, A. O. J., Boschloo, L., Schoevers, R. A., & Borsboom, D. (2017). Mental disorders as networks of problems: A review of recent insights. Social Psychiatry and Psychiatric Epidemiology, 52(1), 1–10.
- Gallotti, M., & Branch, I. L. M. (2015). Migrant Domestic Workers Across the World: Global and regional estimates. International Labour Organization Research Series. https://www.ilo.org/wcmsp5/groups/public/—ed_protect/—protrav/—migrant/documents/briefingnote/wcms_490162.pdf
- Garabiles, M. R., Harper-Shehadeh, M., & Hall, B. J. (2019). The cultural adaptation of scalable WHO eMental health program for overseas Filipino workers. Medical Internet Research-Formative, 3(1), e11600.
- Garabiles, M. R., Lao, C. K., Xiong, Y., & Hall, B. J. (2019). Exploring comorbidity between anxiety and depression among migrant Filipino domestic workers: A network approach. Journal of Affective Disorders, 250, 85–93.
- Garabiles, M. R., Lao, C. K., Yip, P., Chan, E., Mordeno, I., & Hall, B. J. (2019). Psychometric validation of PHQ-9 and GAD-7 in Filipino migrant domestic workers in Macao. Journal of Personality Assessment, 1–12. doi:10.1080/00223891.2019.1644343
- Garabiles, M. R., Ofreneo, M. A. P., & Hall, B. J. (2017). Towards a model of resilience for transnational families of Filipina domestic workers. Plos One, 12(8), e0183703.
- Government of the Macao Special Administrative Region - Labour Affairs Bureau. (2019). Table A1 - Number of non-resident workers by industry and country/region of issuance of identification document - End of January 2019. Retrieved from https://www.dsal.gov.mo/download/pdf_en/statistic/nrworker/A1/A1_2019_01.pdf
- Green, B. L., Krupnick, J. L., Chung, J., Siddique, J., Krause, E. D., Revicki, D., … Miranda, J. (2006). Impact of PTSD comorbidity on one-year outcomes in a depression trial. Journal of Clinical Psychology, 62(7), 815–835.
- Greene, T., Neria, Y., & Gross, R. (2016). Prevalence, detection and correlates of PTSD in the primary care setting: A systematic review. Journal of Clinical Psychology in Medical Settings, 23(2), 160–180.
- Hall, B. J., Garabiles, M. R., & Latkin, C. A. (2019). The social determinants of key health outcomes among Filipino domestic workers in China: A qualitative needs assessment. BMC Public Health, 19. doi:10.1186/s12889-019-6552-4
- Hall, B. J., Pangan, C. A. C., Chan, E. W. W., & Huang, R. L. (2019). The effect of discrimination on depression and anxiety symptoms and the buffering role of social capital among female domestic workers in Macao, China. Psychiatry Research, 271, 200–207.
- Hall, B. J., Shi, W., Garabiles, M. R., & Chan, E. (2018). Correlates of expected eMental health uptake among Filipino domestic workers in China. Global Mental Health, 5, e33.
- Hall, B. J., Yip, P. S. Y., Garabiles, M. R., Lao, C. K., Chan, E. W. W., & Marx, B. P. (2019). Psychometric validation of the PTSD checklist-5 among female Filipino migrant workers. European Journal of Psychotraumatology, 10(1), 1571378.
- Hinton, D. E., Barlow, D. H., Reis, R., & de Jong, J. (2016). A transcultural model of the centrality of “thinking a lot” in psychopathologies across the globe and the process of localization: A Cambodian refugee example. Culture, Medicine, and Psychiatry, 40(4), 570–619.
- Hinton, D. E., & Lewis‐Fernández, R. (2011). The cross‐cultural validity of posttraumatic stress disorder: Implications for DSM‐5. Depression and Anxiety, 28, 783–801.
- Hinton, D. E., McNally, R. J., Fairfax, R. C., & Harachi, T. W. (2020). A network analysis of culturally relevant anxiety sensitivity and posttraumatic stress disorder symptoms in Cambodians. Transcultural Psychiatry. doi:10.1177/1363461520906005
- Ho, F. Y., Chan, C. S., & Tang, K. N. (2016). Cognitive-behavioral therapy for sleep disturbances in treating posttraumatic stress disorder symptoms: A meta-analysis of randomized controlled trials. Clinical Psychology Review, 43, 90–102.
- Hofmann, S. G., Curtiss, J., & McNally, R. J. (2016). A complex network perspective on clinical science. Perspectives on Psychological Science, 11(5), 597–605.
- Ignacio, E., & Mejia, Y. (2009). Managing labour migration - Filipino and Indonesian domestic helpers. Bangkok. Retrieved from https://www.ilo.org/wcmsp5/groups/public/—asia/—ro-bangkok/documents/publication/wcms_101824.pdf
- Jiang, H., Fei, X., Liu, H., Roeder, K., Lafferty, J., Wasserman, L., … Zhao, T. (2020). Package ‘huge’. R package version 1.3.4.1.
- Jones, P. J. (2017). networktools: Tools for identifying important nodes in networks. R package version 1.1.0.
- Jones, P. J. (2019). Bootstrapping bridge centrality using the bootnet package. Retrieved from https://paytonjjones.wordpress.com/2019/02/01/bootstrapping-bridge-centrality-using-the-bootnet-package/?fbclid=IwAR23_X93pf-h0O_rP8dVFOIGeQsa_Kex5l7w7u67h_v5sLlxZ_oY-zAuMQE
- Jones, P. J., Ma, R., & McNally, R. J. (2017). Bridge centrality: A network approach to understanding comorbidity. Multivariate Behavioral Research. doi:10.1080/00273171.2019.1614898
- Jones, P. J., Mair, P., Riemann, B. C., Mugno, B. L., & McNally, R. J. (2018). A network perspective on comorbid depression in adolescents with obsessive-compulsive disorder. Journal of Anxiety Disorders, 53, 1–8.
- Kroenke, K., & Spitzer, R. L. (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals, 32(9), 509–515.
- Krueger, R. F. (1999). The structure of common mental disorders. Archives of General Psychiatry, 56(10), 921–926.
- La Greca, A. M., Danzi, B. A., & Chan, S. F. (2017). DSM-5 and ICD-11 as competing models of PTSD in preadolescent children exposed to a natural disaster: Assessing validity and co-occurring symptomatology. European Journal of Psychotraumatology, 8(1), 1310591.
- Lee, J. C. K. (2012). Research on migrant workers’ rights in Hong Kong. In M. F. M. Workers (Ed.), Migrants review: Researches and essays on migrant domestic workers in Hong Kong (pp. 61–71). Hong Kong: MFMW Ltd.
- Mancini, A., Littleton, H., Grills, A., & Jones, P. J. (2019). PTSD near and far: Symptom networks from two to 12 months after the Virginia tech campus shootings. Clinical Psychological Science, 7, 1340–1354.
- McNally, R. J. (2016). Can network analysis transform psychopathology? Behaviour Research and Therapy, 86, 95–104.
- McNally, R. J., Robinaugh, D. J., Wu, G. W. Y., Wang, L., Deserno, M. K., & Borsboom, D. (2015). Mental disorders as causal systems: A network approach to posttraumatic stress disorder. Clinical Psychological Science, 3(6), 836–849.
- Mission for Migrant Workers. (2017). Pictures from the inside: Investigating living accommodation of women migrant domestic workers towards advocacy and action. Retrieved from https://issuu.com/migrantshk/docs/pictures_from_the_inside_a4
- Mitchell, K. S., Wolf, E. J., Bovin, M. J., Lee, L. O., Green, J. D., Rosen, R. C., … Marx, B. P. (2017). Network models of DSM-5 posttraumatic stress disorder: Implications for ICD-11. Journal of Abnormal Psychology, 126(3), 355–366.
- Mordeno, I. G., Carpio, J. G. E., Mendoza, N. B., & Hall, B. J. (2018). The latent structure of major depressive symptoms and its relationship with somatic disorder symptoms among Filipino female domestic workers in China. Psychiatry Research, 270, 587–594.
- Mueser, K. T., & Drake, R. E. (2007). Comorbidity: What have we learned and where are we going? Clinical Psychology: Science and Practice, 14(1), 64–69.
- Nakonz, J., & Shik, A. W. Y. (2009). And all your problems are gone: Religious coping strategies among Philippine migrant workers in Hong Kong. Mental Health, Religion & Culture, 12(1), 25–38.
- Papini, S., Rubin, M., Telch, M. J., Smits, J. A. J., & Hien, D. A. (2019). Pretreatment posttraumatic stress disorder symptom network metrics predict the strength of the association between node change and network change during treatment. Journal of Traumatic Stress. doi:10.1002/jts.22379
- Philippine Statistics Authority. (2017). 2016 survey on overseas Filipinos. Retrieved from https://psa.gov.ph/content/2016-survey-overseas-filipinos
- R Core Team. (2018). R: A language and environment for statistical computing. Retrieved from http://www.R-project.org
- Ramsawh, H. J., Fullerton, C. S., Mash, H. B. H., Ng, T. H. H., Kessler, R. C., Stein, M. B., & Ursano, R. J. (2014). Risk for suicidal behaviors associated with PTSD, depression, and their comorbidity in the U.S. Army. Journal of Affective Disorders, 161, 116–122.
- Riley, K., Nazareno, J., & Malish, S. (2016). 24-hour care: Work and sleep conditions of migrant Filipino live-in caregivers in Los Angeles. American Journal of Industrial Medicine, 59(12), 1120–1129.
- Salganik, M. J., & Heckathorn, D. D. (2004). Sampling and estimation in hidden populations using respondent‐driven sampling. Sociological Methodology, 34(1), 193–240.
- Sandberg, J. C., Grzywacz, J. G., Talton, J. W., Quandt, S. A., Chen, H., Chatterjee, A. B., & Arcury, T. A. (2012). A cross-sectional exploration of excessive daytime sleepiness, depression, and musculoskeletal pain among migrant farmworkers. Journal of Agromedicine, 17(1), 70–80.
- Schuler, M., Wittmann, M., Faller, H., & Schultz, K. (2018). The interrelations among aspects of dyspnea and symptoms of depression in COPD patients - a network analysis. Journal of Affective Disorders, 240, 33–40.
- Spiller, T. R., Schick, M., Schnyder, U., Bryant, R. A., Nickerson, A., & Morina, N. (2017). Symptoms of posttraumatic stress disorder in a clinical sample of refugees: A network analysis. European Journal of Psychotraumatology, 8(sup3), 1318032.
- Spinhoven, P., Penninx, B. W., van Hemert, A. M., de Rooij, M., & Elzinga, B. M. (2014). Comorbidity of PTSD in anxiety and depressive disorders: Prevalence and shared risk factors. Child Abuse & Neglect, 38(8), 1320–1330.
- Sullivan, C. P., Smith, A. J., Lewis, M., & Jones, R. T. (2016). Network analysis of PTSD symptoms following mass violence. Psychological Trauma: Theory, Research, Practice, and Policy, 10(1), 58–66.
- Tuliao, A. P., Ang, A. V., Garabiles, M. R., Tuliao, M. D., & Samaco-Zamora, M. C. S. (in press). Culture and mental health in the Philippines. In R. Moodley & E. Lee (Eds.), The routledge international handbook of race, ethnicity, and culture in mental health. London, UK: Routledge.
- Vargas, M. C., Garabiles, M. R., & Hall, B. J. (2020). Narrative identities of overseas Filipino domestic worker community in Macao (SAR) China. Journal of Community Psychology, 48(3), 977-993.
- Weathers, F. W., Blake, D. D., Schnurr, P. P., Kaloupek, D. G., Marx, B. P., & Keane, T. M. (Writers). (2013). The life events checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD. Retrieved from www.ptsd.va.gov
- Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2013). The PTSD Checklist for DSM-5 (PCL-5). Instrument available from the National Center for PTSD. Retrieved from www.ptsd.va.gov
- Zimmerman, C., Kiss, L., & Hossain, M. (2011). Migration and health: A framework for 21st century policy-making. PLoS Medicine, 8(5), e1001034.
