ABSTRACT
Background: Posttraumatic Stress Disorder (PTSD) is associated with high levels of functional impairments such as difficulties in academic or occupational performance and in social relationships. With an increasing number of traumatic event types experienced (trauma load), PTSD risk increases in a dose-dependent manner. Accordingly, high rates of PTSD can impair the reconstruction process in post-conflict societies. In order to meet these high needs for mental health services in societies with little access to professional care, task shifting approaches and community-based interventions have been suggested. Narrative Exposure Therapy (NET) has been developed as a short and pragmatic exposure-based PTSD treatment that can be easily trained to lay personnel. Yet, it remains unclear whether NET can be effectively provided by trained lay counsellors even at high levels of trauma load.
Objective: To investigate whether trauma load influences the treatment effectiveness of NET provided by trained and supervised local lay counsellors.
Method: Linear mixed models were calculated to investigate the influence of trauma load on treatment effectiveness in a sample of N = 323 rebel war survivors from Northern Uganda with PTSD.
Results: We found a strong reduction of PTSD symptoms following NET, which was not influenced by trauma load. However, individuals with higher levels of trauma load reported higher PTSD symptoms before therapy as well as 4 and 10 months following treatment completion compared to individuals with lower trauma load.
Conclusions: Treatment with NET by lay counsellors is effective independent of trauma load. However, individuals with higher trauma load have a higher probability to show residual symptoms, which might require additional time, sessions or treatment modules.
Antecedentes: El trastorno de estrés traumático (TEPT) se asocia con altos niveles de discapacidad funcional, tales como dificultades en el desempeño académico uocupacional yen las relaciones sociales. Con un número creciente de los tipos de eventos traumáticos experimentados (carga traumática), el riesgo de TEPT aumenta en una forma dependiente de la dosis. De la misma forma, altas tasas de TEPT pueden afectar el proceso de reconstrucción en las sociedad post-conflicto. Para abordar estas crecientes necesidades por servicios de salud mental en sociedades con poco acceso acuidado profesional, se ha sugerido el enfoque de cambio de tareas ylas intervenciones basadas en la comunidad. La Terapia de Exposición Narrativa (NET en su sigla en inglés) ha sido desarrollada como un tratamiento de TEPT basado en la exposición, breve ypragmático que puede ser fácilmente entrenado al personal laico. Aun así, permanece incierto si la NET puede ser implementada efectivamente por consejeros laicos entrenados, incluso aaltos niveles de carga traumática.
Objetivo: Investigar si la carga traumática influencia la efectividad del tratamiento de la NET proporcionado por consejeros laicos locales entrenados ysupervisados.
Método: Los modelos mixtos lineales se calcularon para investigar la influencia de la carga traumática en la efectividad del tratamiento, en una muestra de N= 323 sobrevivientes de guerra rebelde desde Uganda del Norte con TEPT.
Resultados: Encontramos una clara reducción de los síntomas TEPT luego de la NET, la cual no fue influenciada por la carga traumática. Sin embargo, los individuos con altos niveles de carga traumática reportaron altos niveles de síntomas TEPT antes de la terapia como también 4 y 10 meses luego del término del tratamiento comparado alos individuos con carga traumáticamás baja.
Conclusiones: El tratamiento con la NET administrada por consejeros laicos es efectiva independiente de la carga traumática. Sin embargo, los individuos con carga traumáticamás alta tienen una probabilidadmás alta de mostrar síntomas residuales, los cuales podrían requerir tiempo, sesiones omódulos de tratamiento adicionales.
背景:创伤后应激障碍 (PTSD) 与高水平的功能损伤相关, 例如学习或职业表现以及社会关系方面的困难。随着经历的创伤事件类型 (创伤负荷) 增加, PTSD风险呈剂量依赖性增加。相应地, 高比例的PTSD会危害到冲突后社会的重建进程。为了在很少能够获得专业护理的社会中满足对心理健康服务的这些高需求, 已经提出了任务转移法和社区干预措施。叙事暴露疗法 (NET) 已发展为一种简短实用的PTSD暴露疗法, 可以轻松地培训非专业人员。然而, 在高创伤负荷的情况下, 受过训练的非专业顾问能否有效地提供NET尚不清楚。
目的:研究创伤负荷是否影响受过训练和监督的当地非专业顾问提供的NET的治疗效果。
方法:在一个323名乌干达北部患有PTSD的叛乱战争幸存者样本中, 计算线性混合模型, 以考查创伤后负荷对治疗有效性的影响。
结果:我们发现NET后PTSD症状明显减轻, 不受创伤负荷的影响。然而, 与创伤负荷较低的个体相比, 创伤负荷较高的个体在治疗前以及治疗完成后4个月和10个月报告了更高的PTSD症状。
结论:非专业顾问提供的NET治疗是有效的, 与创伤负荷无关。但是, 创伤负荷较高的人更有可能出现残留症状, 这可能需要额外的时间, 疗程或治疗模块。
1. Introduction
War, terror, political violence and other atrocities affect a large proportion of civilians worldwide. These experiences can lead to profound mental health consequences such as Posttraumatic Stress Disorder (PTSD), a disorder characterized by strong and intrusive memories of the encountered traumatic experiences, avoidance of trauma reminders, negative alterations of mood and cognitions and hyperarousal (American Psychiatric Association, Citation2013). Furthermore, PTSD involves clinically significant levels of distress or functional impairments, which can manifest as difficulties in academic or occupational performance as well as in social relationships. Therefore, high PTSD rates can impair the reconstruction and rehabilitation process in war-torn countries.
1. 1. PTSD rates in post-conflict settings
Post-conflict populations show high prevalence rates for multiple exposures to traumatic events and trauma-related disorders. In a representative sample of 1,113 young rebel war survivors from Northern Uganda, 98% reported the experience of at least one traumatic event during lifetime (Ertl, Pfeiffer, Schauer-Kaiser, Elbert, & Neuner, Citation2014). Forty-three per cent of this sample had been forcibly recruited by the rebel army, and hence experienced numerous traumatic stressors. Accordingly, the PTSD prevalence rate was 25% in the subgroup of former child soldiers (Ertl et al., Citation2014). Surveys conducted in other war-affected and low-income regions found that prevalence rates of DSM-IV PTSD were, e.g. 37% in Algeria in a sample of survivors of armed conflict, 28% in Cambodia in samples from three selective areas surveying refugee camp returnees, poor population facing continues civil strife and a sample from the capital with a relatively higher living-standard, 18% in refugee camps, cities, and resettlement areas of Gaza, and 16% in Ethiopia in a sample of registered refugees and up to 64% in a sample of Iraqi displaced individuals (de Jong et al., Citation2001; Ibrahim, Catani, Ismail, & Neuner, Citation2019). Both the individual well-being and functioning as well as the development of a peaceful post-war society require effective treatments for individuals with multiple traumatization suffering from PTSD.
1. 2. Treatment for PTSD in overstrained health systems
Effective treatment options for PTSD after single and multiple traumatic incidents include prolonged exposure, cognitive processing therapy, cognitive therapy, cognitive behavioural therapy, eye movement desensitization and reprocessing and narrative exposure therapy (NET) (Courtois & Brown, Citation2019; Cusack et al., Citation2016).
Such empirically based therapies involve common procedural elements, e.g. psychoeducation, imaginative exposure, coping skills, and purported mechanisms of action, e.g. emotion-regulation, cognitive and emotional processing, restructuring and modification of memory processes (Schnyder et al., Citation2015).
Meta-analyses confirm a superiority of these trauma-focused psychotherapies involving exposure for the treatment of PTSD as opposed to supportive treatments (Bisson, Roberts, Andrew, Cooper, & Lewis, Citation2013; Cusack et al., Citation2016; Kline, Cooper, Rytwinksi, & Feeny, Citation2018), but do not reveal a superiority of a certain trauma-focused treatment (Schnyder et al., Citation2015).
In addition to other forms of treatment, NET has been developed to address the particular needs of survivors with multiple different experiences of organized and/or family violence, as it is frequently the case in refugee and post-conflict populations.
It therefore consists of a chronological reconstruction of the client’s life story with a focus on the traumatic experiences and, through the therapeutic process, results in a testimony of the survivor’s life story. The main mode of action of NET is the chronological integration of fragmented emotional trauma memories in the individuals’ life story, leading to a reduction of fear reactions to trauma reminders (Neuner et al., Citation2008; Neuner, Schauer, Klaschik, Karunakara, & Elbert, Citation2004; Schauer, Neuner, & Elbert, Citation2011).
Individual studies on multiply traumatized samples from different cultural settings already demonstrated the feasibility (Neuner et al., Citation2010) and effectiveness (Adenauer et al., Citation2011; Bichescu, Neuner, Schauer, & Elbert, Citation2007; Halvorsen & Stenmark, Citation2010; Halvorsen, Stenmark, Neuner, & Nordahl, Citation2014; Heilsmann & Måkestad, Citation2008; Hensel-Dittmann et al., Citation2011; Hijazi et al., Citation2014; Lely, Smid, Jongedijk, Knipscheer, & Kleber, Citation2019; Neuner et al., Citation2004; Stenmark, Catani, Neuner, Elbert, & Holen, Citation2013) of NET, that is furthermore listed as a suggested, even though not yet strongly recommend intervention by the APA Clinical Practise Guidelines for the Treatment of PTSD (2017). However, it is important to mention that this suggestion is based on the literature available from 1980–2012, acknowledging that this is likely to change based on a more recent literature review and pending future meta-analyses.
However, in overstrained health systems of post-conflict settings, it is not feasible to deliver psychotherapy by academically trained experts to the large number of highly traumatized individuals. Considering that 85% of the current world’s refugees are hosted in developing regions (United Nations High Commissioner for Refugees, Citation2018), with limited health-care systems and lack of personnel, task shifting approaches, i.e. the transfer of tasks to intensely trained lay personnel from the community, is a core principle in order to treat many individuals in need (Kakuma et al., Citation2011; Silove, Ventevogel, & Rees, Citation2017; van Ginneken et al., Citation2013). The treatment of trauma survivors with PTSD by trained local counsellors with NET has been implemented in different clinical trials and proved to be effective (Catani et al., Citation2009; Ertl, Pfeiffer, Schauer, Elbert, & Neuner, Citation2011; Jacob, Neuner, Maedl, Schaal, & Elbert, Citation2014; Neuner et al., Citation2008; Schauer, Kohila, Catani, Onyut, & Schauer, Citation2005). Similar to studies mainly conducted in Western countries which delivered exposure-based psychotherapy for PTSD by expert clinicians (Hensel-Dittmann et al., Citation2011), approximately two-third of trauma survivors no longer met the diagnostic criteria of PTSD following treatment by local counsellors who were intensely trained in PTSD diagnosis and NET, but did not have an academic degree in psychology (Ertl et al., Citation2011; Wilker et al., Citation2014).
1. 3. The role of trauma load in the development and treatment of PTSD
The dose-dependent relationship between the number of different traumatic event types (trauma load) and PTSD risk is a robust finding (Brewin, Andrews, & Valentine, Citation2000; Kolassa et al., Citation2010; Neugebauer et al., Citation2009; Neuner et al., Citation2004; Steel et al., Citation2009; Tortella-Feliu et al., Citation2019). With accumulating traumatic experiences, the symptom severity increases, and accordingly, the likelihood of spontaneous remission decreases (Kolassa et al., Citation2010). Yet, this effect does not contradict the importance of individual differences in the response to trauma. Especially at low levels of trauma load, there is a high interindividual variability in PTSD vulnerability, which can be explained by individual factors like emotions, beliefs, cognitive distortions and other pre-event factors as described by Bowman (Citation1999) as well as by biological risk factors such as genetics and epigenetics (e.g. Ramo-Fernández, Schneider, Wilker, & Kolassa, Citation2015; Wilker & Kolassa, Citation2013).
Given the relevant role of trauma load in PTSD development, it is of high clinical interest to investigate whether trauma load also impacts the effectiveness of exposure-based treatment for PTSD. One might assume that individuals who experienced a high number of different traumatic event types and accordingly are impaired by more severe PTSD symptoms would respond less to psychotherapy.
However, so far, the evidence regarding the influence of trauma load on psychotherapy is limited. In a study investigating treatment outcomes of survivors of mixed traumas treated with prolonged exposure, individuals who reported more traumatic events showed a reduced PTSD symptom improvement, but only in one of the two samples investigated (van Minnen, Arntz, & Keijsers, Citation2002). By contrast, Ehlers and colleagues conducted a large study on 330 PTSD treatments in a naturalistic setting and did not find an effect of the number of traumas on psychotherapy outcome (Ehlers et al., Citation2013). However, individuals that needed treatment for multiple traumata responded less to psychotherapy and attended the sessions less regularly.
In this line, it remains an open empirical question whether survivors with extreme levels of traumatization who need treatment for multiple traumata can be effectively and safely treated by local lay personnel. One previous study of our work group indicated that individuals treated with NET show a significant PTSD symptom reduction even at high levels of trauma load (Wilker et al., Citation2014). However, since the sample size was relatively low (N = 43), effects of trauma load on therapy effectiveness might not have been detected and the results require replication.
This study therefore aimed at systematically investigating the effect of trauma load on the outcome of exposure-based therapy with NET provided by trained lay counsellors in a large sample of survivors of multiple traumatic experiences from Northern Uganda.
2. Materials and methods
2. 1. Participants
The study was conducted in a sample of survivors of the rebel war led by the Lord’s Resistance Army (LRA) in Northern Uganda. Participants were highly affected by numerous traumatic events including abduction and forced recruitment, killings, mutilations and sexual violence. Data collection took place in villages of Gulu District as well as in former Internal Displaced People (IDP) camps in Amuru District and Nwoya District, Northern Uganda. Inclusion criteria were a current PTSD diagnosis according to DSM-IV (American Psychiatric Association, Citation2000) in conjunction with a PTSD symptom score of at least 10 in the Posttraumatic Stress Diagnostic Scale (PDS; Foa, Cashman, Jaycox, & Perry, Citation1997), no psychotropic medication or former trauma-focused therapy, no current signs of alcohol or substance abuse, absence of psychotic symptoms and age above 18 years. A total of N = 362 individuals who took part in the first diagnostic interview (t1) fulfilled the inclusion criteria and were offered a treatment with NET. The therapy outcome was evaluated by two follow-up assessments at 4 months (t2) and at 10 months (t3) after the end of therapy in order to assess the long-term effects of the treatment and to detect potential relapses. However, N = 7 people refused to participate, and N = 32 dropped out in the course of the study or were excluded from the analyses (See for the participant flow chart). This resulted in a final sample of N = 323 participants (58.51% female, Mdn age = 31.00, range: 18–62). The excluded participants did not differ from the included participants regarding PTSD symptom severity or level of trauma load (Supplementary Table 1).
All participants who were included in the final analyses completed at least one of the follow-up interviews, whereby N = 3 participants could not be found at the 4 months follow-up, and N = 8 at the 10 months follow-up, respectively. Additionally, one interview at the 10 months follow-up was incomplete and had to be excluded.
2. 2. Procedure
Study procedures were approved by the Institutional Review Board of Gulu University, the Lacor Hospital Institutional Research Ethics Committee, the Ugandan National Council for Science and Technology (UNCST), Uganda, and the ethics committee of the German Psychological Society (Deutsche Gesellschaft für Psychologie, DGPs).
Data collection was performed by trained local interviewers. Prior to participation, subjects gave written informed consent after getting detailed information on the study procedures. The informed consent materials and study instruments were translated into the local language of Northern Uganda, Luo, according to scientific standards. In a second step, a blind back-translation was performed to validate the correct interpretation of the questions. Participants fulfilling all inclusion criteria were offered a treatment with NET. The treatment started within 1 month after the diagnostic interview. Interviews and therapies were conducted by trained local counsellors under supervision of expert psychologists specialized in PTSD. Follow-up interviews were conducted by an independent interviewer who did not conduct the treatment.
2. 3. Measures
2. 3. 1. Trauma load
Trauma exposure was assessed with a 62-items event list that has been used in previous studies (Conrad et al., Citation2017; Schneider et al., Citation2018; Wilker et al., Citation2013, Citation2014, Citation2015, Citation2018). The list included general traumatic events (e.g. accidents, natural disasters, rape), war-related events (e.g. fighting in combat, being close to a bomb attack) and the many atrocities specific to the LRA war (e.g. forced to cut ears and lips, forced to eat human flesh).
During the development of the event-list and the interviewer training, careful attention was paid that the event categories are as distinct and precise as possible. Due to the many possible traumatic event types LRA war survivors might have experienced, the long event-list with 62 items was developed. To give one example, individuals might have been mutilated by the LRA, might have witnessed the mutilation of others and might have been forced themselves to mutilate others, resulting in three distinct event types only concerning mutilations. Trauma load was calculated as the sum score of different traumatic event types ever experienced in life. This score is a reliable measurement to assess trauma load (retest-reliability after one week of r = .82) (Wilker et al., Citation2015). Furthermore, in a validation study, the simple sum score of traumatic events predicted lifetime PTSD best, as opposed to more complex measurements additionally considering the frequency of event type exposure or the age at trauma exposure (Wilker et al., Citation2015).
2. 3. 2. PTSD diagnosis and symptom severity
To diagnose current and lifetime PTSD according to DSM-IV, as well as measure current PTSD symptom severity, the Posttraumatic Stress Diagnostic Scale (PDS; Foa et al., Citation1997) was conducted as a structured interview. The employed Luo version of the PDS revealed a very good internal consistency in a prior study (α = 0.89) (Ertl et al., Citation2010). Participants diagnosed with current PTSD according to DSM-IV and a PDS symptom score of at least 10 at the first assessment were offered a treatment with NET. This relatively low cut-off compared to cut-offs suggested by investigations employing the PDS as a self-report (e.g. Ehring, Kleim, Clark, Foa, & Ehlers, Citation2007) was chosen as the PDS was conducted as a diagnostic interview. Assessors were intensely trained in the DSM-IV criteria of PTSD and supervised by expert psychologists, who discussed diagnostic decisions in weekly supervision meetings.
2. 3. 3. NET
Treatments were provided by local counsellors who were trained according to an adapted field version of the NET manual (Schauer et al., Citation2011). The intensive training conducted by a team of international expert psychologists took 8 weeks and included information on the theory of NET, practical exercises in role-plays and the processing of own traumatic experiences. Afterwards, the newly trained counsellors conducted their first treatments while being shadowed by experienced therapists and provided detailed case documentations to the study supervisors. The treatment process and the compliance with the NET manual were further monitored and documented through case discussions and regular supervision meetings with expert psychologists.
The first therapy session included psychoeducation and the lifeline exercise in order to get a chronological overview of the clients’ biography. Hereby, the therapist guided the client to lay down a rope representing the clients’ life from birth to present and put down flowers, indicating positive life events, and stones for negative and traumatic events, respectively. Beginning with the second session, the most severe traumatic experiences were treated by means of exposure therapy following the lifeline’s chronological order. The clients were encouraged to share behavioural, physical, cognitive as well as emotional reactions and sensory impressions experienced during each traumatic event in a detailed manner. The therapist helped the client to chronologically recall the stressors and to re-establish the connections between the emotional-sensory memories and the corresponding autobiographical context information.
Participants received on average 12.05 (SD = 1.93) therapy sessions which took place twice a week, with durations of 90 to 120 minutes. The number of sessions was planned according to the individuals’ lifeline. Therapy was deemed as completed after the main traumatic experiences presented in the lifeline were chronologically discussed. As a result, clients with a longer lifeline tended to receive slightly more sessions.
2. 4. Data analysis
All statistical analyses were performed with the statistical software R version 3.5.1 (R Core Team, Citation2017). To evaluate the effect of trauma load on treatment outcome we calculated linear mixed effect models (R package nlme version 3.1–137; Pinheiro et al., Citation2017) with the PDS sum score as the outcome variable and participant as a random effect, with random intercepts for each participant. All models further included time as a within-subject fixed factor, which represented the therapeutic intervention, with the levels t1 (before therapy), t2 (4 months after therapy) and t3 (10 months after therapy). Models of different complexities were compared with Akaike’s information criteria (AIC; Akaike, Citation1973; Burnham & Anderson, Citation2002) and additionally included the fixed effects of trauma load as well as a potential interaction of time × trauma load, which would represent a differential therapeutic response linked to the amount of traumatic events experienced. The AIC compares models with regard to the accuracy with which a model fits the underlying data generating process and similarly penalizes models of higher complexity (Burnham & Anderson, Citation2002). The model selection procedure is presented in . Since model residuals did not meet the assumption of normality, permutation tests were performed using 10,000 random permutations, leading to similar results. Accordingly, parametric p-values are reported for all analyses. Planned general linear hypotheses were calculated using the R package multcomp version 1.4.8 (Hothorn, Bretz, & Westfall, Citation2008) to investigate the influence of time on changes in PDS symptom score from before treatment to the 4 months follow-up (t1 – t2), between the 4 months and the 10 months follow-up (t2 – t3) and from pre-treatment to the 10 months follow-up (t1 – t3). Cohens d was calculated to report effect sizes. The analyses were repeated to furthermore investigate the influence of trauma load on the symptom change in the three PTSD symptom cluster intrusions, avoidance and hyperarousal.
Table 1. Demographic and clinical information of the sample.
In order to evaluate the proportion of individuals who fulfilled the criteria of a clinically significant improvement, we calculated the reliable change index (RCI; Jacobson & Truax, Citation1991) based on the variability of the PDS score before treatment (t1). We performed t-tests to investigate whether the group of individuals who showed clinically significant improvements from t1 to t3 differed from those who did not regarding trauma load. Similarly, a planned t-test was conducted in order to analyse whether individuals who no longer meet the diagnostic criteria of PTSD had experienced more traumatic experiences compared to those who still suffered from PTSD at the last assessment (t3).
3. Results
PTSD symptoms declined significantly after the completion of NET. A linear mixed effect model including time as the only predictor, which represented the therapeutic intervention, revealed a strong main effect (F2,632 = 453.42, p < .0001), which was further explored in three planned contrasts with adjustments for multiple comparisons. There was a significant symptom reduction from baseline (t1) to the 4 months follow-up (t2) (Z = −26.41, p < .001, d = 1.77) as well from baseline to the 10 months follow-up (t3) (Z = −26.55, p < .001, d = 1.96). Furthermore, we observed a small but significant symptom decline from t2 to t3 (Z = −2.59, p = .026, d = 0.16).
The inclusion of trauma load in the model decisively improved the AIC as a model fit criterion (cf. for an overview of the model selection procedure), while including a potential interaction between trauma load × time did not. Therefore, a main effect model including time and trauma load was chosen as the final model (cf. ) and statistical results are reported for this model. We found a significant main effect of time (F2,632 = 452.58, p < .0001) and trauma load (F1,321 = 39.17, p < .0001) on the PTSD symptom score. The main effect of time, representing the treatment effect, was observable across all levels of trauma load. Furthermore, we additionally included a potential trauma load × time interaction in the model, but found no evidence for such an effect (F2,630 = 1.10, p = . 33). Accordingly, we observed similar symptom trajectories across different levels of trauma load ((a,b)). In other words, individuals with high levels of trauma load presented more PTSD symptoms before and after therapy compared to individuals with less traumatic events. We visualized this effect by artificially splitting the sample into three equal-sized groups according to the number of traumatic events experienced (see (b)).
Figure 2. Symptom development following treatment with NET as a function of trauma load. (a): Bee swarm plots of PTSD symptom severity before therapy and at 4 and 10 months following the end of the treatment. The heat colours represent the levels of traumatic load for each individual, ranging from relatively low levels (represented by white circles) to high levels of traumatic load (represented by red circles). The lines of the plot indicate the median PDS Score (marked in bold) at each measurement point and the interquartile range. (b): Mean PDS symptom scores (standard errors) before as well as 4 and 10 months following the end of the treatment are displayed as a function of trauma load. For a better visualization, the sample has been splitted in tertiles.
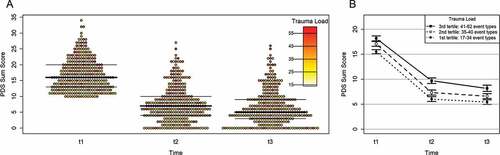
Table 2. Estimated models and model selection procedure.
In order to investigate whether clinically significant changes in PTSD symptoms were associated with trauma load, we calculated the RCI following the procedure suggested by Jacobson & Truax (Citation1991) which was 5.37 in the present sample. Of a total number of 314 individuals with complete diagnostic data at the 10 months’ follow-up assessment (t3), N = 250 (79.62%) met the criteria for clinically significant improvement (see ). We did not find evidence of difference in trauma load between the group of individuals who met the criteria for clinically significant improvement and those who did not (tdf=98.26 = .96, p = .34). Furthermore, only N = 6 (1.9%) of the sample showed significant symptom worsening. All of these individuals reported the occurrence of newly experienced traumatic events after the end of therapy. Furthermore, N = 2 additionally reported previously undisclosed traumatic events which involved forced perpetration of atrocities, and one individual reported alcohol abuse during and after treatment.
Figure 3. Scatterplot of PTSD symptom severity before treatment and at the 10 months follow-up as a function of trauma load. The bold line indicates no change in symptom severity following treatment with NET, while individual data points below and above the dashed line indicate clinically significant improvement (shaded in dark grey) and worsening (shaded in light grey), respectively. The heat colours represent the levels of traumatic load for each individual, ranging from relatively low levels (represented by white circles) to high levels of traumatic load (represented by red circles). To avoid overplotting, individual data points with the same values regarding PTSD symptom severity before and after each other have been plotted next to each other.
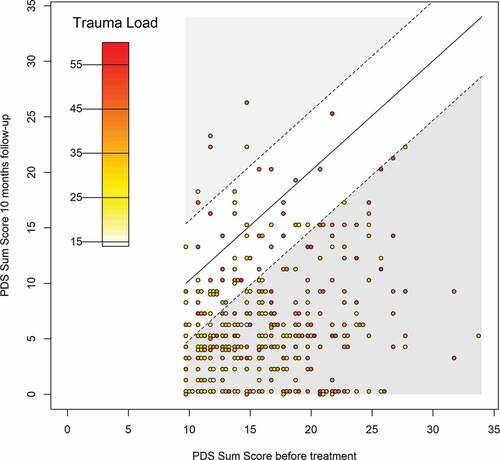
A relationship between the treatment with NET and the worsening of symptoms could not be detected. Individuals who still suffered from clinically relevant symptoms after the completion of the last follow-up were offered further treatment sessions in order to reduce the remaining symptoms.
Finally, we investigated the number of individuals who still met the diagnostic criteria of PTSD. At the last assessment (t3), N = 68 (21.65%) still fulfilled the diagnostic criteria for PTSD. Individuals with a PTSD diagnosis at t3 had a significantly higher trauma load (MPTSD = 39.81, SD = 6.78) as opposed to individuals who no longer met the diagnostic criteria for PTSD (MnoPTSD = 36.42, SD = 7.24, t112.84 = −3.59, p < .001, d = 0.483).
The observed effect of trauma load on treatment outcome was similarly observed when analysing the symptom cluster intrusions, avoidance and hyperarousal separately (). On average, participants received 12 treatment sessions (Mdn sessions = 12.00; range: 6–19). There was a small positive association between the number of sessions and trauma load (τ = 0.16, p < .001). However, the number of sessions did not impact treatment success.
Table 3. Results of linear mixed model for the symptom cluster intrusions, avoidance and hyperarousal.
4. Discussion
The results of this study replicated the high effectiveness of NET for the treatment of PTSD after multiple traumatizations (Ertl et al., Citation2011; Schaal, Elbert, & Neuner, Citation2009; Stenmark et al., Citation2013), when applied by local counsellors with trauma-focused training in resource-poor regions (Jacob et al., Citation2014; Köbach, Schaal, Hecker, & Elbert, Citation2015; Neuner et al., Citation2008). Furthermore, we did not find evidence indicating that community-implemented NET shows a differential effect across the number of traumatic events experienced. In more detail, in an exceptionally large therapy sample, the effect of the treatment was not qualified by an interaction with trauma load. In this line, the occurrence of clinically significant changes as indicated by the RCI was independent of trauma load. This illustrates that individuals who experienced high numbers of different traumatic event types can also experience a significant symptom reduction and long-lasting treatment effects following NET by trained lay personnel. Furthermore, the provision of NET by trained and supervised lay counsellors was safe: We did not encounter any suicides among the individuals treated with NET, and only one person had to be taken over by a professional clinical psychologist due to an extraordinary severity and complexity of the symptoms. Furthermore, the rate of reliable worsening was small (1.9%) and comparable to the observations in a large naturalistic clinical study where clinical experts provided the treatments (Ehlers et al., Citation2013).
Given the high prevalence of PTSD in post-conflict regions, and the minimal availability of trained mental health professionals, the delivery of short-term and pragmatic therapeutic modules such as NET by trained lay personnel from the community can be an effective strategy to meet the large needs, enhance functionality and thereby improve the rebuilding and reconciliation progress. Similar models including task shifting and stepped care are currently discussed to develop enhanced mental health care for refugees in host countries (Böge et al., Citation2019; Elbert, Wilker, Schauer, & Neuner, Citation2017; Sijbrandij et al., Citation2017) and could be inspired by the current study.
However, we have to note that individuals with higher trauma load were more likely to still meet the diagnostic criteria of PTSD following treatment with NET. Accordingly, we found a positive link between trauma load and PTSD symptom severity before and after treatment, indicating that the amount of experienced traumatic events not only predicts the risk for PTSD development and likelihood of spontaneous remission (Kolassa et al., Citation2010; Neuner et al., Citation2004), but also the remaining symptom severity following exposure-based psychotherapy of chronic PTSD.
Additional therapeutic modules might be helpful to assist those survivors with high trauma load who still show PTSD symptoms following NET. Since NET predominantly focuses on the autobiographical reconstruction of past traumatic memories (Schauer, Neuner, & Elbert, Citation2011), survivors of extreme traumatization might additionally benefit from support regarding coping in the here and now (e.g. skills training to enhance emotion regulation, installation of social support, i.e. in self-help groups). In this context, we have to note that in our sample, many survivors of high levels of trauma were former child soldiers who faced severe problems after returning into civil society, including social exclusion, shame, guilt, stigmatization and fear of revenge. Therefore, individuals in our study might have additionally benefitted from psycho-social interventions aiming at the integration and rehabilitation of former child soldiers.
Although our results showed a significant effect of trauma load on PTSD symptoms before and after therapy, trauma load did not influence PTSD symptom reduction. Accordingly, it is important to consider further individual risk and resilience factors that might influence treatment effectiveness. Important candidates represent genetic risk factors (Wilker, Elbert, & Kolassa, Citation2014), social emotions (guilt, shame) and social support, stigmatization, physical health or comorbid mental health disorders (Andrews, Brewin, & Rose, Citation2003; Bowler et al., Citation2017; Corrigan, Citation2004; Corrigan & Watson, Citation2002; Kessler, Sonnega, Bromet, Hughes, & Nelson, Citation1995; Pace & Heim, Citation2011; Pacella, Hruska, & Delahanty, Citation2013; Schneider et al., Citation2018). Yet, the results of this study clearly show that studies investigating factors associated with trauma therapy outcome need to consider trauma load in their analyses as this factor strongly influences PTSD symptom severity.
Strengths of the study include the standardized diagnostic interviews, the exceptionally large therapy sample, the assessment of two follow-up diagnostic interviews in order to detect potential symptom relapses after the end of NET provided by lay counsellors, the manualized treatment, the high attrition rate, and the unique sample from Northern Uganda, which allowed for the investigation of a broad range of trauma load.
However, a potential limitation is the retrospective assessment of trauma load, which might lead to biased reports. Indeed, there is evidence for an increase of the reported traumatic events over time, and this unreliability was associated with PTSD symptom severity (Heir, Piatigorsky, & Weisæth, Citation2009; Hepp et al., Citation2006; Krinsley, Gallagher, Weathers, Kutter, & Kaloupek, Citation2003). Yet, Bramsen et al., (Citation2001) did not observe a systematic change of the retrospective report of traumatic events over time. In a previous study, we investigated the reliability of our employed measurement for trauma load and found a good test-retest reliability (r = .82). Further, we also found no evidence for a systematic change of the reported number of traumatic events over time (Wilker et al., Citation2015). However, we have to note that the time interval was only one week, preventing any conclusions regarding memory alterations over longer time intervals.
Another possible limitation is the fact that the number of sessions was not standardized. By contrast, the number of sessions was planned according to most severe traumatic experiences obtained from the diagnostic interview and the lifeline exercise. However, this led to a more naturalistic setting where therapists plan the therapy sessions according to the needs of the client. Further, since the study aimed to investigate factors influencing treatment success with NET, we should indicate that we did not have a control group. Although the evidence regarding NET (Jacob, Wilker, & Isele, Citation2017) makes it likely that symptom reductions can be attributed to the treatment, the present design does not test this statement.
In this line, since all study participants received a treatment with NET, the interviewers who conducted the follow-up assessments were not blind to the treatment conditions. However, they did not conduct the treatment of the participants they interviewed. Finally, the few individuals who dropped out of the treatment were not available for follow-up interviews (e.g. because they moved away to a distinct location) which made it not feasible to include them in the statistical analyses.
In summary, the results provide strong evidence that community-implemented trauma treatment with NET by trained local counsellors is followed by a clinically significant symptom reduction in a large proportion of patients treated, and that this symptom reduction occurs similarly at different levels of trauma load. Therefore, treatment by lay counsellors can provide an important amelioration of PTSD symptoms and should be considered as a treatment option in overstrained health systems (Böge et al., Citation2019; Elbert et al., Citation2017; Kakuma et al., Citation2011; Sijbrandij et al., Citation2017; van Ginneken et al., Citation2013). These results were obtained in a naturalistic setting where lay counsellors decide together with their clinical supervisors how many sessions each individual needs according to amount of traumatic events experienced. Nevertheless, trauma load affected the PTSD symptom severity before and after treatment in a main effect manner. Therefore, trauma load should be considered in future PTSD research investigating individual factors related to treatment outcome. Most importantly, from a clinical perspective, future studies should investigate which additional therapeutic modules might further assist trauma survivors who experienced high levels of trauma load and still meet PTSD criteria following treatment.
Author’s contribution
SW and ITK developed the study concept. AS, SW and AP collected the data under the supervision of ITK and with valuable support by TE. AS performed the statistical analyses and interpretation with critical input and supervision of SW. AS drafted the paper with the input of DC and SW. All authors critically revised the manuscript and approved the final version of the paper for submission.
Supplemental Material
Download MS Word (31.3 KB)Acknowledgments
M.Sc.-Psych. Daniela Conrad received a PhD scholarship from the Hector Fellow Academy. We thank our team of Ugandan counsellors for their outstanding empathy and professionalism in the conduction of interviews and therapies.
Disclosure statement
The authors have no conflicts of interest to declare.
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Adenauer, H. , Catani, C. , Gola, H. , Keil, J. , Ruf, M. , & Schauer, M. (2011). Narrative exposure therapy for PTSD increases top-down processing of aversive stimuli - evidence from a randomized controlled treatment trial. BMC Neuroscience , 12. doi:10.1186/1471-2202-12-127
- Akaike, H. (1973). Information theory and an extension of the maximum likelihood principle. In B. N. Petrov , (Ed.) Proceedings of the Second International Symposium on Information Theory (pp 267–13). Budapest: Akademiai Kiado.
- American Psychiatric Association . (2000). Diagnostic and statistical manual of mental disorders . Washington, DC: Author.
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders . Washington, DC: Author.
- Andrews, B. , Brewin, C. R. , & Rose, S. (2003). Gender, social support, and PTSD in victims of violent crime. Journal of Traumatic Stress , 16, 421–427.
- Bichescu, D. , Neuner, F. , Schauer, M. , & Elbert, T. (2007). Narrative exposure therapy for political imprisonment-related chronic posttraumatic stress disorder and depression. Behaviour Research and Therapy , 45, 2212–2220.
- Bisson, J. I. , Roberts, N. P. , Andrew, M. , Cooper, R. , & Lewis, C. (2013). Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database of Systematic Reviews . doi:10.1002/14651858.CD003388.pub4
- Böge, K. , Karnouk, C. , Hahn, E. , Schneider, F. , Habel, U. , & Banaschewski, T. (2019). Mental health in refugees and asylum seekers (MEHIRA): Study design and methodology of a prospective multicentre randomized controlled trail investigating the effects of a stepped and collaborative care model. European Archives of Psychiatry and Clinical Neuroscience , 270(1), 95–106. doi:10.1007/s00406-019-00991-5
- Bowler, R. M. , Adams, S. W. , Gocheva, V. V. , Li, J. , Mergler, D. , Brackbill, R. , et al. (2017). Posttraumatic stress disorder, gender, and risk factors: World trade center tower survivors 10 to 11 Years after the September 11, 2001 attacks. Journal of Trauma Stress , 30(6), 564–570. doi:10.1002/jts.22232
- Bowman, M. L. (1999). Individual differences in posttraumatic distress: Problems with the DSM- IV model. The Canadian Journal of Psychiatry , 44, 21–33.
- Bramsen, I. , Dirkzwager, A. J. E. , van Esch, S. C. M. , & van der Ploeg, H. M. (2001). Consistency of self-reports of traumatic events in a population of Dutch peacekeepers: Reason for optimism? Journal of Traumatic Stress , 14, 733–740.
- Brewin, C. R. , Andrews, B. , & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology , 68, 748–766.
- Burnham, K. P. , & Anderson, D. R. (2002). Model selection and multi-model inference: A practical information-theoretic approach . New York: Springer.
- Catani, C. , Kohiladevy, M. , Ruf, M. , Schauer, E. , Elbert, T. , & Neuner, F. (2009). Treating children traumatized by war and Tsunami: A comparison between exposure therapy and meditation-relaxation in North-East Sri Lanka. BMC Psychiatry , 9, 22.
- Conrad, D. , Wilker, S. , Pfeiffer, A. , Lingenfelder, B. , Ebalu, T. , Lanzinger, H. , … Kolassa, S. (2017). Does trauma event type matter in the assessment of traumatic load? European Journal of Psychotraumatology , 8, 1344079.
- Corrigan, P. (2004). How stigma interferes with mental health care. American Psychologist , 59, 614–625.
- Corrigan, P. , & Watson, A. (2002). Understanding the impact of stigma on people with mental illness. World Psychiatry : Official Journal of the World Psychiatric Association (WPA) , 1, 16–20.
- Courtois, C. A. , & Brown, L. S. (2019). Guideline orthodoxy and resulting limitations of the American psychological association’s clinical practice guideline for the treatment of PTSD in adults. Psychotherapy , 56, 329–339.
- Cusack, K. , Jonas, D. E. , Forneris, C. A. , Wines, C. , Sonis, J. , Middleton, J. C. , & Gaynes . (2016). Psychological treatments for adults with posttraumatic stress disorder: A systematic review and meta-analysis. Clinical Psychology Review , 43, 128–141.
- de Jong, J. T. M. , Komproe, I. H. , Van Ommeren, M. , El Masri, M. , Araya, M. , Khaled, N. , et al. (2001). Lifetime events and posttraumatic stress disorder in 4 postconflict settings. JAMA , 286(5), 555–562. doi:10.1001/jama.286.5.555
- Ehlers, A. , Grey, N. , Wild, J. , Stott, R. , Liness, S. , Deale, A. , & Clark, D. M. (2013). Implementation of Cognitive Therapy for PTSD in routine clinical care: Effectiveness and moderators of outcome in a consecutive sample. Behaviour Research and Therapy , 51, 742–752.
- Ehring, T. , Kleim, B. , Clark, D. M. , Foa, E. B. , & Ehlers, A. (2007). Screening for posttraumatic stress disorder: What combination of symptoms predicts best? The Journal of Nervous and Mental Disease , 195, 1004–1012.
- Elbert, T. , Wilker, S. , Schauer, M. , & Neuner, F. (2017). Dissemination psychotherapeutischer Module für traumatisierte Geflüchtete: Erkenntnisse aus der Traumaarbeit in Krisen- und Kriegsregionen. Nervenarzt , 88, 26–33.
- Ertl, V. , Pfeiffer, A. , Saile, R. , Schauer, E. , Elbert, T. , & Neuner, F. (2010). Validation of a mental health assessment in an African conflict population. Psychological Assessment , 22, 318–324.
- Ertl, V. , Pfeiffer, A. , Schauer, E. , Elbert, T. , & Neuner, F. (2011). Community-implemented trauma therapy for former child soldiers in Northern Uganda: A randomized controlled trial. JAMA , 306, 503–512.
- Ertl, V. , Pfeiffer, A. , Schauer-Kaiser, E. , Elbert, T. , & Neuner, F. (2014). The challenge of living on: Psychopathology and its mediating influence on the readjustment of former child soldiers. PloS One , 9, e102786.
- Foa, E. B. , Cashman, L. , Jaycox, L. , & Perry, K. (1997). The validation of a self-report measure of posttraumatic stress disorder: The posttraumatic diagnostic scale. Psychological Assessment , 9, 445–451.
- Halovorsen, J. , & Stenmark, H. (2010). Narrative exposure therapy for posttraumatic stress disorder in tortured refugees: A preliminary uncontrolled trial. Scandinavian Journal of Psychology , 51, 495–502.
- Halovorsen, J. , Stenmark, H. , Neuner, F. , & Nordahl, H. M. (2014). Does dissociation moderate treatment outcomes of narrative exposure therapy for PTSD? A secondary analysis from a randomized controlled clinical trial. Behaviour Research and Therapy , 57, 21–28.
- Heilsmann, K. R. , & Måkestad, E. (2008). Narrative exposure therapy as treatment for posttraumatic stress disorder: An intervention study. Retrieved from http://www.biblioteca.cij.gob.mx/Archivos/Materiales_de_consulta/Migracion/Articulos/salud_mental.pdf
- Heir, T. , Piatigorsky, A. , & Weisæth, L. (2009). Longitudinal changes in recalled perceived life threat after a natural disaster. British Journal of Psychiatry , 194, 510–514.
- Hensel-Dittmann, D. , Schauer, M. , Ruf, M. , Catani, C. , Odenwald, M. , Elbert, T. , & Neuner, F. (2011). Treatment of traumatized victims of war and torture: A randomized controlled comparison of narrative exposure therapy and stress inoculation training. Psychotherapy and Psychosomatics , 80, 345–352.
- Hepp, U. , Gamma, A. , Milos, G. , Eich, D. , Ajdacic-Gross, V. , Rössler, W. , … Schnyder, U. (2006). Inconsistency in reporting potentially traumatic events. British Journal of Psychiatry , 188, 278–283. doi:10.1192/bjp.bp.104.008102
- Hijazi, A. , Lumley, M. , Ziadni, M. , Haddad, L. , Rapport, L. , & Arnetz, B. (2014). Brief Narrative exposure therapy for posttraumatic stress in Iraqi refugees: A preliminary randomized clinical trial. Journal of Traumatic Stress , 27, 314–322.
- Hothorn, T. , Bretz, F. , & Westfall, P. (2008). Simultaneous inference in general parametric models. Biometrical Journal , 50, 346–363.
- Ibrahim, H. , Catani, C. , Ismail, A. A. , & Neuner, F. (2019). Dimensional structure and cultural invariance of DSM-V posttraumatic stress disorder among Iraqi and Syrian displaced people. Frontiers in Psychology , 10. doi:10.3389/fpsyg.2019.01505
- Jacob, N. , Neuner, F. , Maedl, A. , Schaal, S. , & Elbert, T. (2014). Dissemination of psychotherapy for trauma spectrum disorders in postconflict settings: A randomized controlled trial in Rwanda. Psychotherapy and Psychosomatics , 83, 354–363.
- Jacob, N., Wilker, S., & Isele, D . (2017). Narrative Expositionstherapie zur Behandlung von Traumafolgestörungen. Schweizer Archiv für Neurologie und Psychiatrie , 168, 99–106.
- Jacobson, N. S. , & Truax, P. (1991). Clinical significance : A statistical approach to denning meaningful change in psychotherapy research. 59(1), 12–19. doi:10.1037/0022-006x.59.1.12
- Kakuma, R. , Minas, H. , Van, G. N. , Poz, M. R. D. , Desiraju, K. , Morris, J. E. , & Scheffler, R. M. (2011). Human resources for mental health care: Current situation and strategies for action. The Lancet , 378, 1654–1663.
- Kessler, R. C. , Sonnega, A. , Bromet, E. , Hughes, M. , & Nelson, C. B. (1995). Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry , 52, 1048–1060.
- Kline, A. C. , Cooper, A. A. , Rytwinksi, N. K. , & Feeny, N. C. (2018). Long-term efficacy of psychotherapy for posttraumatic stress disorder: A meta-analysis of randomized controlled trials. Clinical Psychology Review , 59, 30–40.
- Köbach, A. , Schaal, S. , Hecker, T. , & Elbert, T. (2015). Psychotherapeutic intervention in the demobilization process: Addressing combat-related mental injuries with narrative exposure in a first and second dissemination stage. Clinical Psychology & Psychotherapy , 24(4), 807–825. doi:10.1002/cpp.1986
- Kolassa, I. T. , Ertl, V. , Eckart, C. , Kolassa, S. , Onyut, L. P. , & Elbert, T. (2010). Spontaneous remission from PTSD depends on the number of traumatic event types experienced. Psychological Trauma: Theory, Research, Practice, and Policy , 2, 169–174.
- Krinsley, K. E. , Gallagher, J. G. , Weathers, F. W. , Kutter, C. J. , & Kaloupek, D. G. (2003). Consistency of retrospective reporting about exposure to traumatic events. Journal of Traumatic Stress , 16, 399–409.
- Lely, J. C. G. , Smid, G. E. , Jongedijk, R. A. , Knipscheer, J. , & Kleber, R. J. (2019). The effectiveness of narrative exposure therapy: A review, meta-analysis and meta-regression analysis. European Journal of Psychotraumatology , 10, 1550344.
- Neugebauer, R. , Fisher, P. W. , Turner, J. B. , Yamabe, S. , Sarsfield, J. A. , & Stehling-Ariza, T. (2009). Post-traumatic stress reactions among Rwandan children and adolescents in the early aftermath of genocide. International Journal of Epidemiology , 38, 1033–1045.
- Neuner, F. , Kurreck, S. , Ruf, M. , Odenwald, M. , Elbert, T. , & Schauer, M. (2010). Can asylum-seekers with posttraumatic stress disorder be successfully treated? A randomized controlled pilot study. Cognitive Behaviour Therapy , 39, 81–91.
- Neuner, F. , Onyut, P. L. , Ertl, V. , Odenwald, M. , Schauer, E. , & Elbert, T. (2008). Treatment of posttraumatic stress disorder by trained lay counselors in an African refugee settlement: A randomized controlled trial. Journal of Consulting and Clinical Psychology , 76, 686–694.
- Neuner, F. , Schauer, M. , Karunakara, U. , Klaschik, C. , Robert, C. , & Elbert, T. (2004). Psychological trauma and evidence for enhanced vulnerability for posttraumatic stress disorder through previous trauma among West Nile refugees. BMC Psychiatry , 4, 34.
- Neuner, F. , Schauer, M. , Klaschik, C. , Karunakara, U. , & Elbert, T. (2004). A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an african refugee settlement. Journal of Consulting and Clinical Psychology , 72, 579.
- Pace, T. W. , & Heim, C. M. (2011). A short review on the psychoneuroimmunology of posttraumatic stress disorder: From risk factors to medical comorbidities. Brain, Behavior, and Immunity , 25, 6–13.
- Pacella, M. L. , Hruska, B. , & Delahanty, D. L. (2013). The physical health consequences of PTSD and PTSD symptoms: A meta-analytic review. Journal of Anxiety Disorders , 27, 33–46.
- Pinheiro, J. , Bates, D. , DebRoy, S. , Sarkar, D. , Heisterkamp, S. , Van , & Willigen, B. (2017). nlme: Linear and nonlinear mixed effects models. R package (3rd ed., pp. 1–336). Retrieved from https://cran.r-project.org/web/packages/nlme/nlme.pdf
- R Core Team . (2017). R: A language and environment for statistical computing . Vienna: R Foundation for Statistical Computing. Retrieved from http://www.r-project.org
- Ramo-Fernández, L. , Schneider, A. , Wilker, S. , & Kolassa, I.-T. (2015). Epigenetic alterations associated with War Trauma and childhood maltreatment. Behavioral Sciences & the Law , 33, 701–721.
- Schaal, S. , Elbert, T. , & Neuner, F. (2009). Narrative exposure therapy versus interpersonal psychotherapy. A pilot randomized controlled trial with Rwandan genocide orphans. Psychotherapy and Psychosomatics , 78, 298–306.
- Schauer, E. , Kohila, M. , Catani, C. , Onyut, L. P. , & Schauer, M. (2005). Building local capacity for mental health service provision in the face of large-scale traumatisation: A cascade-model from Sri Lanka; in: Annual Meeting of the European Society of Traumatic Stress Studies . Stockholm.
- Schauer, M. , Neuner, F. , & Elbert, T. (2011). Narrative Exposure Therapy. A short-term intervention for traumatic stress disorders after war, terror or torture . Göttingen: Hogrefe & Huber.
- Schneider, A. , Conrad, D. , Pfeiffer, A. , Elbert, T. , Kolassa, I. T. , & Wilker, S. (2018). Stigmatization is associated with increased PTSD risk after traumatic stress and diminished likelihood of spontaneous remission - A study with east African conflict survivors. Frontiers in Psychiatry , 9, 1–10.
- Schnyder, U. , Ehlers, A. , Elbert, T. , Foa, E. B. , Gersons, B. P. R. , Resick, P. A. , … Cloitre, M. (2015). Psychotherapies for PTSD: What do they have in common? European Journal of Psychotraumatology , 6, 28186. https://doi.org/10.3402/ejpt.v6.28186
- Sijbrandij, M. , Acarturk, C. , Bird, M. , Bryant, R. A. , Burchert, S. , Carswell, K. , … Cuijpers, P. (2017). Strengthening mental health care systems for Syrian refugees in Europe and the Middle East: Integrating scalable psychological interventions in eight countries. European Journal of Psychotraumatology , 8(1), 1388102. doi:10.1080/20008198.2017.1388
- Silove, D. , Ventevogel, P. , & Rees, S. (2017). The contemporary refugee crisis: An overview of mental health challenges. World Psychiatry : Official Journal of the World Psychiatric Association , 16, 130–139.
- Steel, Z. , Chey, T. , Silove, D. , Marnane, C. , Bryant, R. A. , & van Ommeren, M. (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA , 302, 537–549.
- Stenmark, H. , Catani, C. , Neuner, F. , Elbert, T. , & Holen, A. (2013). Treating PTSD in refugees and asylum seekers within the general health care system. A randomized controlled multicenter study. Behaviour Research and Therapy , 51, 641–647.
- Tortella-Feliu, M. , Fullana, M. A. , Pérez-Vigil, A. , Torres, X. , Chamorro, J. , Littarelli, S. A. , & Fernández de la Cruz, L. (2019). Risk factors for posttraumatic stress disorder: An umbrella review of systematic reviews and meta-analyses. Neuroscience & Biobehavioral Reviews , 107, 154–165.
- United Nations High Commissioner for Refugees . (2018). Global trends - Forced displacement in 2017 . Geneva.
- van Ginneken, N. , Tharyan, P. , Lewin, S. , Rao, G. , Meera, S. , Pian, J. , et al. (2013). Non-specialist health worker interventions for the care of mental, neurological and substance-abuse disorders in low- and middle-income countries. Cochrane Database of Systematic Reviews (Online), (11), CD009149. doi:10.1002/14651858.CD009149.pub2
- van Minnen, A. , Arntz, A. , & Keijsers, G. P. J. (2002). Prolonged exposure in patients with chronic PTSD: Predictors of treatment outcome and dropout. Behaviour Research and Therapy , 40, 439–457.
- Wilker, S. , Elbert, T. , & Kolassa, I. T. (2014). The downside of strong emotional memories: How human memory-related genes influence the risk for posttraumatic stress disorder - A selective review. Neurobiology of Learning and Memory , 112, 75–86.
- Wilker, S. , & Kolassa, I. T. (2013). The formation of a neural fear network in posttraumatic stress disorder: Insights from molecular genetics. Clinical Psychological Science , 1, 452–469.
- Wilker, S. , Kolassa, S. , Vogler, C. , Lingenfelder, B. , Elbert, T. , Papassotiropoulos, A. , & Kolassa, I.-T. (2013). The role of memory-related gene WWC1 (KIBRA) in lifetime posttraumatic stress disorder: Evidence from two independent samples from African conflict regions. Biological Psychiatry , 74, 664–671.
- Wilker, S. , Pfeiffer, A. , Kolassa, S. , Elbert, T. , Lingenfelder, B. , & Ovuga, E. (2014). The role of FKBP5 genotype in moderating long-term effectiveness of exposure-based psychotherapy for posttraumatic stress disorder. Translational Psychiatry , 4, e403.
- Wilker, S. , Pfeiffer, A. , Kolassa, S. , Koslowski, D. , Elbert, T. , & Kolassa, I.-T. (2015). How to quantify exposure to traumatic stress? Reliability and predictive validity of measures for cumulative trauma exposure in a post-conflict population. European Journal of Psychotraumatology , 6. doi:10.3402/ejpt.v6.28306
- Wilker, S. , Schneider, A. , Conrad, D. , Pfeiffer, A. , Boeck, C. , Lingenfelder, B. , & Kolassa, I.-T. (2018). Genetic variation is associated with PTSD risk and aversive memory: Evidence from two trauma-Exposed African samples and one healthy European sample. Translational Psychiatry , 8, 251.