ABSTRACT
Background
The psychological treatment of comorbid post-traumatic stress disorder (PTSD) and substance use disorder (SUD) is clinically challenging, and outcomes are often poor.
Objective
This paper describes a systematic review and meta-analysis which sought to establish the current efficacy for a number of established psychological approaches for adults and adolescents, in comparison to interventions for SUD alone, or other active approaches, following a pre-registered protocol.
Method
This review followed PRISMA and Cochrane Collaboration guidelines. Data extraction and risk of bias judgements using Cochrane criteria were undertaken by all authors. Primary outcomes were PTSD severity and substance use post-treatment. The quality of findings was assessed using GRADE. Following a comprehensive search, conducted to 13 September 2021, 27 studies were included.
Results
We found a relatively high level of dropout across studies. In our main comparisons, we found no benefits for present-focused treatment approaches aimed at improving coping skills beyond those for SUD-only interventions. We found modest benefits for trauma-focused intervention plus SUD intervention post-treatment for PTSD (standardized mean difference (SMD) = −0.36, 95% confidence interval (CI) −0.64, −0.08), and at 6–13 months for PTSD (SMD = −0.48, 95% CI −0.81, −0.15) and alcohol use (SMD = −0.23, 95% CI −0.44, −0.02). There were no benefits for cognitive restructuring interventions as a group, but we found a modest effect for integrated cognitive behavioural therapy (ICBT) for PTSD post-treatment (SMD = −0.33, 95% CI −0.62, −0.04). There was evidence of some benefit for trauma-focused intervention over present-focused intervention for PTSD from a single study and for reduction in dropout for incentivized attendance for trauma-focused intervention from another single study. Most findings were of very low quality.
Conclusion
There is evidence that trauma-focused therapy and ICBT can improve PTSD for some individuals, but many patients do not fully engage with treatment and average treatment effects are modest.
HIGHLIGHTS
For PTSD, evidence was strongest for trauma-focused CBT-based approaches, but effects were modest.
There was little evidence of any added benefit on substance use, beyond that of standard addiction treatments, for any included intervention.
Dropout from treatment was high
Antecedentes: El tratamiento psicológico del trastorno de estrés postraumático (TEPT) comórbido con trastorno por uso de sustancias (TUS) es un desafío clínico y los resultados suelen ser deficientes.
Objetivo: Este artículo describe una revisión sistemática y meta-análisis, los cuales buscaron establecer la eficacia actual para un determinado número de enfoques psicológicos para adultos y adolescentes, en comparación con intervenciones sólo para TUS, y otros enfoques activos, siguiendo un protocolo previamente registrado.
Método: Esta revisión siguió las guías PRISMA y de Colaboración de Cochrane. Todos los autores realizaron extracción de datos y evaluación de riesgo de sesgos usando los criterios de Cochrane. Los resultados primarios fueron severidad de TEPT y uso de sustancias post-tratamiento. La calidad de los hallazgos fue evaluada utilizando GRADE. Luego de una búsqueda exhaustiva, realizada el 13 de septiembre del 2021, se incluyeron 27 estudios.
Resultados: Encontramos un nivel de abandono relativamente alto en los estudios. En nuestras principales comparaciones no encontramos mayores beneficios en los actuales abordajes de tratamiento focalizados en mejorar las habilidades de afrontamiento en comparación con las intervenciones exclusivas para TUS. Encontramos beneficios modestos para intervenciones centradas en trauma sumada a intervención para TUS post-tratamiento de TEPT (DMP = −0.36 CI-0.64, −0.08), y a los 6–13 meses para TEPT (DMP = −0.48 CI-0.81, −0.15) y uso de alcohol (DMP = −0.23 CI −0.44, −0.02). No hubo beneficios para las intervenciones para reestructuración cognitiva como grupo, pero encontramos un efecto modesto post-tratamiento para la terapia cognitivo conductual integrada (TCCI) para el TEPT (DMP = −0.33 CI −0.62, −0.04). Hubo evidencia de algún beneficio para intervenciones enfocadas en trauma sobre las intervenciones centradas en el presente para TEPT de un solo estudio y para la reducción del abandono para la participación incentivada para la intervención centrada en el trauma de otro estudio aislado. La mayoría de los hallazgos fueron de muy baja calidad.
Conclusión: Concluimos que existe evidencia de que la terapia centrada en el trauma y la TCCI pueden mejorar el TEPT para algunos individuos, pero muchos pacientes no se comprometen totalmente con el tratamiento y los efectos de tratamiento promedio son modestos.
背景: 创伤后应激障碍 (PTSD) 和物质使用障碍 (SUD) 共病的心理治疗在临床上具有挑战性,结果通常很差。
目的: 本文描述了一项旨在确定一些针对成人和青少年已建立的心理方法相较于单独 SUD 干预或其他积极方法的当前疗效的系统综述和元分析,遵循了预注册的方案。
方法: 本综述遵循 PRISMA 和 Cochrane 协作指南。所有作者均使用 Cochrane 标准进行数据提取和误差风险判断。主要结果是 PTSD 严重程度和治疗后的物质使用。使用 GRADE 评估结果的质量。在进行了的全面搜索之后,纳入了 27 项直到2021 年 9 月 13 日的研究。
结果: 我们发现研究中的流失率相对较高。在我们的主要比较中,我们发现目前旨在提高应对技巧的集中治疗方法没有任何超出仅使用 SUD 干预措施的益处。我们发现聚焦创伤干预加 SUD 干预对治疗后的 PTSD (SMD = −0.36 CI-0.64, −0.08)和 6–13 个月时的 PTSD(SMD = −0.48 CI-0.81, −0.15)和饮酒(SMD = −0.23 CI −0.44, −0.02)有一定的好处。作为一个整体,认知重组干预没有任何好处,但我们发现了综合认知行为疗法 (ICBT) 对 PTSD 治疗后的中等效应(SMD = −0.33 CI −0.62, −0.04)。有来自一项研究的证据表明,与目前针对 PTSD 的重点干预相比,聚焦创伤的干预有一些益处,而另一项研究表明,聚焦创伤的干预的激励性出勤减少了流失率。大多数研究结果质量非常低。
结论: 我们的结论是,有证据表明聚焦创伤治疗和 ICBT 可以改善某些个体的 PTSD,但许多患者并未完全参与治疗,平均治疗效果适中。
1. Introduction
Post-traumatic stress disorder (PTSD) and substance use disorder (SUD) are both common disorders which cause significant functional impairment (e.g. Degenhardt et al., Citation2013; Grant et al., Citation2016; Kessler et al., Citation2017; World Health Organization, Citation2011). PTSD and SUD frequently co-occur. In a systematic review including 42 studies, Debell et al. (Citation2014) found reported prevalence rates of comorbid alcohol abuse of 10–61% in those with PTSD, and comorbid rates of PTSD for those with alcohol misuse of 2–63%, with most studies reporting rates over 10%. Similarly high rates have been found for SUD both in epidemiological studies and among clinical samples. In an Australian national survey, nearly 6% of those with an SUD diagnosis met the diagnosis for PTSD; 6.5 times more likely than for those without an SUD. For specific substances, a third of those with an opiate use disorder had probable PTSD, with high rates also reported for those with sedative and amphetamine dependencies (Mills, Teeson, Ross, & Peters, Citation2006). High rates of PTSD diagnosis, of 20–42%, have been reported in a number of prevalence studies conducted with SUD service users (Gielen, Havermans, Tekelenburg, & Jansen, Citation2012; Najavits et al., Citation1998; Reynolds et al., Citation2005; Reynolds, Hinchliffe, Asamoah, & Kouimtsidis, Citation2011; Schäfer et al., Citation2010), with rates as high as 75% among military veterans (Schäfer & Lotzin, Citation2018; Seal et al., Citation2011).
For both disorders, well-established psychological and pharmacological interventions for management and treatment are available. For PTSD, psychological interventions include eye movement desensitization and reprocessing (EMDR), and various forms of trauma-focused cognitive behavioural therapy (CBT), including prolonged exposure (PE), cognitive therapy for PTSD, and cognitive processing therapy (CPT) (Lewis, Roberts, Andrew, Starling, & Bisson, Citation2020). There is uncertainty about the applicability of this literature for those with this comorbidity, as most randomized controlled trials (RCTs) of interventions for PTSD exclude participants based on substance use status (Leeman et al., Citation2017). For SUD, effective psychological interventions include CBT, motivational interviewing, behavioural couples therapy, relapse prevention, and contingency management (NICE, Citation2007; NIDA, Citation2020). Such interventions tend to be more effective when delivered alongside pharmacological substitutes (Jhanjee, Citation2014).
PTSD-SUD comorbidity poses many clinical challenges for treating clinicians. Individuals with PTSD-SUD present with a more severe clinical profile, often have significant case management needs and a higher incidence of childhood trauma, and tend to have poorer functioning and well-being, and inferior treatment outcomes and prognosis (Blakey et al., Citation2021; Roberts, Back, Mueser, & Murray, Citation2020; Schäfer & Lotzin, Citation2018; Schäfer & Najavits, Citation2007; Straus, Haller, Lyons, & Norman, Citation2018). Clinicians view this comorbidity as being substantially more difficult to treat than either disorder alone and there is often great uncertainty about whether and when to offer evidence-based trauma-focused intervention (Roberts et al., Citation2020). Most recent PTSD guidelines (e.g. American Psychological Association, Citation2017; Phoenix Australia, Citation2020; International Society for Traumatic Stress Studies, Citation2018; NICE, Citation2018) did not include scoping questions to address issues of comorbidity, and there are no widely accepted guidelines on how to manage and treat such individuals. The one exception is the US Department of Veterans Affairs/Department of Defense guidelines, which recommended that the presence of comorbidity should not prevent patients from receiving other guideline recommended interventions (VA/DoD, Citation2017).
The traditional model of treatment – often still practised in many places – is a sequential approach where addiction is treated first and trauma-focused therapy is only considered once abstinence or control is achieved (Roberts et al., Citation2020; van Dam, Vedel, Ehring, & Emmelkamp, Citation2012). This often necessitates referral to another clinician or service. For many individuals with PTSD-SUD comorbidity, drug and alcohol use is often at least partly a function of a perceived need to self-medicate to manage trauma symptoms and other negative emotional responses (Dvorak, Pearson, & Day, Citation2014; Kaysen, Stappenbeck, Rhew, & Simpson, Citation2014; Leeies, Pagura, Sareen, & Bolton, Citation2010). This is evidenced by the fact that PTSD symptom severity and symptom worsening often lead to increased substance use, while the reciprocal relationship of substance use being related to the development of subsequent PTSD symptoms is less strong (Langdon et al., Citation2016; Simpson, Stappenbeck, Luterek, Lehavot, & Kaysen, Citation2014; Tripp et al., Citation2020). This relationship between PTSD and SUD symptoms risks causing patients to drop out of treatment prematurely if their PTSD symptoms remain untreated, as they may find it more difficult to manage trauma symptoms, increasing the possibility that they might relapse or lose contact with services (Roberts et al., Citation2020; van Dam et al., Citation2012).
This understanding about the nature of the relationship between PTSD and SUD symptoms has led to the development of a number of integrated approaches where treatments for PTSD and SUD are delivered at the same time. Integrated treatment has been suggested as an effective treatment approach for PTSD and SUD that may be more advantageous than sequential treatment. Integrated treatment is delivered by one therapist or a team of therapists trained in both PTSD and SUD treatment. Care is delivered in a consistent manner, using a common disorder model. Several integrated treatment approaches are described in the literature. Differing terminology is sometimes used to describe these approaches (Hien et al., Citation2022); however, the distinction between present (or non-trauma-focused) and past (or trauma-focused) approaches is common and generally well understood. Present-focused approaches primarily seek to improve coping skills and self-compassion. Seeking Safety, a 25-session manualized intervention, which can be delivered in an individual or a group format (Najavits, Citation2002), is the most widely known and evaluated present-focused model. Other coping skills-focused models include the TARGET approach, which is also provided in groups of up to eight to nine sessions (Ford & Russo, Citation2006). A second type of present-focused interventions includes approaches that primarily aim to help individuals to challenge and manage negative PTSD and SUD-related cognitions and beliefs through cognitive behavioural strategies. The most commonly evaluated model of this type is integrated cognitive behavioural therapy (ICBT) (e.g. McGovern, Lambert-Harris, Alterman, Xie, & Meier, Citation2011). Past-focused approaches seek to actively process distressing trauma experiences by incorporating established evidence-based PTSD psychological interventions. The most well-established approach of this type is concurrent treatment of PTSD and substance use disorders using prolonged exposure (COPE) (Back et al., Citation2014). COPE offers PE alongside relapse prevention, delivered by the same therapist, usually over around 12 sessions.
Four systematic reviews of psychological interventions for PTSD and SUD have previously been published (Roberts, Roberts, Jones, & Bisson, Citation2016 – also summarized in Roberts, Roberts, Jones, & Bisson, Citation2015; Simpson, Lehavot, & Petrakis, Citation2017; Torchalla, Nosen, Rostam, & Allen, Citation2012; van Dam et al., Citation2012). Only one of these reviews (Roberts et al., Citation2015, Citation2016) involved a meta-analysis based on outcomes from RCTs. This review identified 14 studies, 13 of which included only adults and one including adolescents. The findings indicated some benefits for trauma-focused approaches for PTSD symptoms, when combined with treatment for SUD over control interventions, but effects were small. No benefits were found for present-focused approaches beyond those of control interventions. Dropout across studies evaluating both past- and present-focused approaches was high. Similar conclusions were drawn in the more recent narrative review of Simpson et al. (Citation2017), although this review also noted that most of the included studies reported improvements in both experimental and control interventions. Since the publication of these reviews, a number of new trials have been completed. We therefore felt that it was timely to undertake an updated review of the literature. This work was also undertaken to support the development of expert treatment recommendations for the European Society for Traumatic Stress Studies (ESTSS).
2. Method
This review was based on the review by Roberts et al. (Citation2016), which was previously led by the first author and followed guidelines outlined in the Cochrane Handbook (Higgins & Green, Citation2011). This protocol was registered with PROSPERO on 16 November 2020 and is available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID = CRD42020207840.
2.1. Review questions
We established three overarching scoping questions which would be addressed through a number of separate comparisons. The comparisons below were not intended to be exclusive but were what we anticipated would be most meaningful based on our knowledge of the literature. The three scoping questions are numbered, with anticipated comparisons indicated by lettering.
For individuals with PTSD and comorbid SUD, do psychological treatments for PTSD or PTSD and SUD, when compared to treatment as usual (TAU) for SUD only, result in a clinically important reduction of PTSD and SUD symptoms, reduced presence of disorder, decreased dropout, or difference in reported adverse effects? Example comparisons:
Are present-focused treatments (also known as coping-based/non-trauma-focused treatments) plus TAU for SUD more effective than TAU for SUD only?
Are trauma-focused treatments plus TAU for SUD more effective than TAU for SUD only?
Are integrated cognitive restructuring-based interventions (without imaginal and in vivo exposure) for PTSD and SUD plus TAU for SUD more effective than TAU for SUD?
Is EMDR plus TAU for SUD more effective than TAU for SUD only?
For individuals with PTSD and comorbid SUD, do psychological treatments for PTSD and SUD, when compared to other psychological treatments for PTSD and SUD (head-to-head comparisons), result in a clinically important reduction of PTSD and SUD symptoms, reduced presence of disorder, decreased dropout, or difference in reported adverse effects? Example comparisons:
Are trauma-focused treatments more effective than present-focused treatments?
Are trauma-focused treatments more effective than integrated cognitive restructuring-based interventions (without imaginal and in vivo exposure)?
Are integrated cognitive restructuring-based interventions (without imaginal and in vivo exposure) more effective than present-focused treatments?
When compared to sequential treatments, do integrated treatments offered by one therapist OR simultaneous treatments for PTSD and SUD offered by different therapists result in a clinically important reduction of PTSD and SUD symptoms, reduced presence of disorder, decreased dropout, or difference in reported adverse effects?
2.2. Inclusion criteria
2.2.1. Participants
Participants were required to meet the formal diagnosis for PTSD using a structured clinical interview according to the International Classification of Diseases, 10th revision (ICD-10) or Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), or subthreshold PTSD using predefined subthreshold criteria, which included re-experiencing symptoms. This decision was based on the fact that individuals with subthreshold PTSD experience similar levels of distress to those with full PTSD, and the high prevalence of subthreshold PTSD in SUD clinical populations (Jakupcak et al., Citation2007; Vujanovic, Smith, Green, Lane, & Schmitz, Citation2018). A minimum of 60% of participants were required to meet full PTSD diagnosis for a study to be included. Participants were also required to meet the formal diagnosis for SUD using a structured clinical interview according to ICD or DSM. Studies primarily aimed at evaluating PTSD and nicotine dependence were excluded. Studies were eligible for inclusion if a subgroup of participants in a study met the criteria for PTSD and SUD, and were randomly allocated across intervention, and subgroup data were made available. Five studies were included on this basis (Acosta et al., Citation2017; Frisman, Ford, Lin, Mallon, & Chang, Citation2008; Haller et al., Citation2016; Mueser et al., Citation2008; Possemato et al., Citation2019). We did not exclude on the basis of age but decided that studies including children and young people below the age of 18 years would be analysed and presented separately. Participants were not excluded on the basis of other comorbidity.
2.2.2. Type of study and intervention
To be considered for inclusion, studies had to be RCTs or cluster randomized trials, including studies with cross-over designs, evaluating one or more psychological intervention, in comparison to a control condition or an alternative psychological intervention. Interventions that were primarily pharmacological and interventions that were not based on a defined psychological model (e.g. yoga, acupuncture, neurofeedback, or transcranial magnetic stimulation) were not included. Control conditions included TAU for SUD only, waiting list or no treatment, attention control interventions, and other psychological treatments. Studies using a pharmacological intervention only as a control were excluded unless the intervention group also received this pharmacological intervention in addition to a psychological intervention. Studies were excluded if they did not evaluate either PTSD symptoms or substance use outcomes. Studies were not excluded on the basis of sample size or publication status. Controlled studies that did not allocate participants randomly were excluded. Studies not published in English were excluded. Unpublished studies were eligible for inclusion.
2.3. Outcomes
The primary outcomes were PTSD severity (giving primacy to clinician-administered outcomes, followed by self-report measures) and SUD severity (giving primacy to clinician-administered outcomes, followed by biological markers, followed by self-report measures). For SUD severity, alcohol and drug outcomes were considered separately. The primary outcome point was post-treatment. Additional outcome points were: 3–5 months post-treatment, 6–13 months post-treatment, and 13 months and beyond post-treatment. Other outcomes were PTSD and SUD diagnosis post-treatment, dropout/leaving treatment prematurely (using study-defined criteria), and adverse effects.
2.4. Searches
Review searches were based on an update to the search undertaken by Roberts et al. (Citation2016). Searches were conducted from 2015 to the present date and were limited to English-language publications. Search sources included MEDLINE, PsycINFO, Embase, Cochrane CENTRAL, PTSDPubs, PTSD-Repository (https://ptsd-va.data.socrata.com/), ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform. Searches included key words and terms related to the terms PTSD, SUD, alcohol use disorder, and RCTs. See Appendix 1 in the Supplementary material for the search stream applied to MEDLINE, PsycINFO, and Embase. We included studies identified and previously included in Roberts et al. (Citation2016). However, in view of the fact that inclusion criteria related to PTSD diagnosis were slightly revised, we re-reviewed studies from this review that were previously excluded because of these criteria. We also reviewed the references of included studies and relevant systematic reviews for studies that we may have missed.
2.5. Procedure
Titles and abstracts were independently screened by two of the authors, as was the full manuscript of any study that either reviewer thought was potentially eligible for inclusion. Any differences of opinion about whether a study met the review inclusion criteria were discussed among all three authors. All three authors undertook data extraction and risk-of-bias judgements using a pre-established data-extraction template, which was then entered into Review Manager (RevMan) version 5.4.1 (RevMan, Citation2020). Extracted data included: study authors and publication date; study design; study setting; recruitment method; participant type; inclusion and exclusion criteria; baseline characteristics (e.g. number of participants diagnosed with full vs partial PTSD; type of drug/alcohol abuse); demographic features (e.g. age, gender, ethnicity); country where study was undertaken; all baseline and outcome measures; number of individuals screened, recruited, and randomized per arm; description of all experimental and control interventions, including length of treatment and number of sessions offered; outcome data for all review-identified outcomes for each time-point available; mean number of sessions attended; funding source; and key conclusions reached by the study authors.
Risk of bias was assessed using the risk of bias tool in the Cochrane Handbook for Systematic Reviews of Interventions, focusing on the following domains: sequence generation, allocation concealment, blinding of outcome assessors, incomplete outcome data, selective reporting, and other bias (Higgins & Green, Citation2011). Ordinarily, it is not possible to blind participants and therapists to the type of intervention allocation, so this domain was not assessed. Again, differences of opinion were settled following discussion among all authors.
2.6. Main and subgroup analyses
To address the review questions identified in Section 2.1, we grouped and analysed studies separately according to whether they were past focused or present focused and according to the model of intervention (e.g. coping focused, cognitive intervention). Comparisons considered under scoping question 1 included studies where the comparator was intervention for SUD only or SUD plus a minimal attention intervention. When an intervention had been evaluated in both an individual- and a group-based format, data were entered into the same comparison but grouped separately to enable possible differences in outcome to be examined.
2.7. Strategy for data synthesis
Data were synthesized using meta-analysis where sufficiently similar interventions and comparators had been investigated, using the comparisons described above. The synthesis was undertaken using RevMan 5.4.1 software (RevMan, Citation2020). Owing to the degree of clinical or statistical heterogeneity, data were pooled using a random-effects model. Analyses were evaluated using the standardized mean difference (SMD) for continuous outcomes and relative risk (RR) for dichotomous outcomes, and presented with 95% confidence intervals (CIs). We used intention-to-treat data where these were available. Completer-only data were included when these were the only data source available. Where data were incomplete, we made attempts to obtain additional data from the study authors. Heterogeneity was explored by observing the I2 statistic and chi-squared (χ2) test. We specified that we would consider the following possible causes of clinical heterogeneity for exploration of our post-treatment primary outcomes if sufficient data permitted: specified treatment intervention model (e.g. COPE, ICBT, Seeking Safety); participant subgroup (e.g. veterans, victims of sexual, physical, and domestic violence, childhood trauma); specific substances of misuse (e.g. alcohol, opioids, cocaine, amphetamines); and treatment setting (e.g. residential or inpatient treatment, outpatient treatment). We determined that publication bias would be investigated by generating funnel plots and examining them for signs of asymmetry if sufficient studies (≥ 10) were included in a comparison.
The quality of the findings was evaluated according to Grading of Recommendations Assessment, Development and Evaluation (GRADE) (e.g. Guyatt, Oxman, Schünemann, Tugwell, & Knottnerus, Citation2011; Langendam et al., Citation2013). GRADE has four levels of evidence: high, moderate, low, and very low. Following the International Society for Traumatic Stress Studies (ISTSS) PTSD Guidelines (Bisson et al., Citation2019), we decided to set thresholds for the clinical importance of findings for our primary outcomes. A threshold effect size greater than or equal to 0.4 was required for PTSD severity and 0.3 for SUD severity to indicate clinical importance for interventions compared against an SUD only/TAU comparator. We set a lower threshold for SUD severity because we thought that it was likely that participants would normally have received some SUD-based intervention prior to study enrolment, which would mean that it would be harder to detect symptom improvement. A threshold greater than or equal 0.2 was set for interventions compared against another active psychological intervention aimed at treating PTSD and SUD. We decided at the outset of the review that we would interpret these thresholds with caution, given that, to our knowledge, benchmarks for clinically important improvement have not been described in this population previously, and small effects might still have important clinical and functional significance.
3. Results
The final searches took place on 13 September 2021. After deduplication, 2219 new citations were identified, 66 references were read in full by two of the authors, and 13 additional studies were included, alongside the 14 studies identified previously (Roberts et al., Citation2015, Citation2016), giving 27 studies with a total of 2849 participants. shows a flow diagram of the selection process. Characteristics of the included studies can be found in . Twenty-six studies were conducted in adult populations and one in an adolescent population (Najavits, Gallop, & Weiss, Citation2006). Most studies were conducted in the USA, with two studies conducted in Australia (Mills et al., Citation2012; Sannibale et al., Citation2013) and one study in Germany (Schäfer et al., Citation2019). Nine studies with military veterans had mostly male participants (Acosta et al., Citation2017; Back et al., Citation2019; Boden et al., Citation2014; Capone et al., Citation2018; Haller et al., Citation2016; Kehle-Forbes et al., Citation2019; Najavits, Krinsley, Waring, Gallagher, & Skidmore, Citation2018; Norman et al., Citation2019; Possemato et al., Citation2019); samples were female only in six studies all evaluating Seeking Safety (Hien et al., Citation2009; Hien, Cohen, Miele, Litt, & Capstick, Citation2004; Myers, Browne, & Norman, Citation2015; Najavits et al., Citation2006; Schäfer et al., Citation2019; Zlotnick, Johnson, & Najavits, Citation2009) and mixed in the remaining studies. The majority of non-veteran studies recruited from community services, mainly for those with addiction problems. One study recruited from a residential addiction setting (Coffey et al., Citation2016) and one study in a prison setting (Zlotnick et al., Citation2009). Most studies were ethnically diverse, and where reported, most non-veterans’ studies included participants who were mostly from lower socio-economic groups. Studies invariably reported SUD type based on self-reported use at clinical interview. Six studies included only individuals with alcohol use disorder (AUD) (Coffey, Stasiewicz, Hughes, & Brimo, Citation2006; Foa et al., Citation2013; Myers et al., Citation2015; Norman et al., Citation2019; Sannibale et al., Citation2013; Stappenbeck et al., Citation2015), with an additional two studies recruiting on the basis of hazardous drinking, where we obtained subset data for those diagnosed with AUD (Acosta et al., Citation2017; Possemato et al., Citation2019). One study recruited exclusively based on opiate use (Schacht, Brooner, King, Kidorf, & Peirce, Citation2017). All other studies reported inclusion on the basis of polydrug abuse/dependence, or alcohol or polydrug abuse/dependence.
Figure 1. Flow diagram of the systematic review. RCT, randomized controlled trial; PTSD, post-traumatic stress disorder; SUD, substance use disorder.
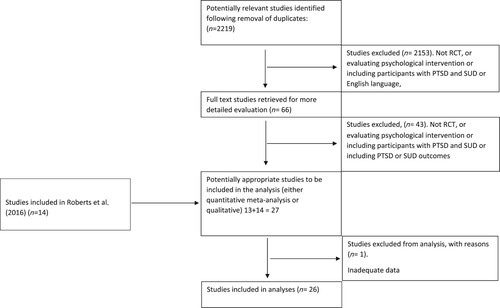
Table 1. Characteristics of the included studies.
3.1. Synthesis of results for adults
Findings of the meta-analyses for all available outcomes are provided in .
Table 2. Summary of meta-analysis of results for each comparison for an experimental psychological intervention vs a substance use disorder (SUD)-based or treatment as usual (TAU) control.
3.1.1. Psychological intervention for PTSD, or PTSD and SUD versus intervention for SUD only
3.1.1.1. Present-focused interventions
Present-focused therapies were compared against SUD-only interventions in seven studies (Boden et al., Citation2014; Frisman et al., Citation2008; Hien et al., Citation2004, Citation2009; Myers et al., Citation2015; Schäfer et al., Citation2019; Zlotnick et al., Citation2009). In all but one of these studies, the present-focused approach was based on Seeking Safety, with the number of sessions offered ranging from eight to 25 sessions. Seeking Safety was delivered through groups, apart from in Hien et al. (Citation2004). The other present-focused approach evaluated was TARGET (Frisman et al., Citation2008), a group-based coping skills-focused therapy. Where reported, participants attended between 36% (Frisman et al., Citation2008) and 62% (Zlotnick et al., Citation2009) of present-focused therapy sessions available to them. Combining data from four studies (Hien et al., Citation2004, Citation2009; Myers et al., Citation2015; Schäfer et al., Citation2019), 51% of participants receiving present-focused intervention were considered completers, based on study-specified definitions. Hien et al. (Citation2004) was a three-arm trial comparing Seeking Safety, relapse prevention, and TAU for SUD only. Participants in the TAU arm were not recruited randomly and data from this arm were not included in meta-analysis. In meta-analysis, we found no benefit beyond that of intervention for SUD only at any time-point for PTSD severity, alcohol use, or substance use. No differences were observed for treatment dropout or adverse effects. Adverse events were not reported for Frisman et al. (Citation2008) or Zlotnick et al. (Citation2009).
All post-treatment analyses of present-focused therapies were based on evaluations of Seeking Safety, and other prespecified study characteristics were too similar for us to consider other meaningful subgroup analyses.
3.1.1.2. Trauma-focused interventions
Seven studies compared trauma-focused interventions plus SUD intervention with SUD-only interventions (Back et al., Citation2019; Coffey et al., Citation2006, Citation2016; Foa et al., 2013; Mills et al., Citation2012; Ruglass et al., Citation2017; Sannibale et al., Citation2013). The trauma-focused approach in all of these studies was based on PE. Three studies were based specifically on the COPE model, where relapse prevention was offered alongside PE (Back et al., Citation2019; Mills et al., Citation2012; Ruglass et al., Citation2017). The number of available sessions ranged from six to 18. Trauma-focused therapy was delivered individually in all studies. Where reported, participants attended between 35.2% (Foa et al., 2013) and 73.3% (Back et al., Citation2019) of trauma-focused therapy sessions available to them. Combining data from five studies (Back et al., Citation2019; Coffey et al., Citation2006, Citation2016; Foa et al., 2013; Sannibale et al., Citation2013), 62% of participants receiving trauma-focused intervention were considered to be treatment completers, based on study-specified definitions. Foa et al. (2013) used a 2 × 2 study design to test the benefits of PE and naltrexone against supportive addiction counselling and placebo medication. As reported in Roberts et al. (Citation2015), we combined the two arms for those receiving PE plus addiction counselling to allow comparison with the two arms receiving supportive addiction counselling. Following Roberts et al. (Citation2015), we also combined the two active treatment arms from Coffey et al. (Citation2016), where PE and PE plus motivational interviewing were compared against an attention control intervention. The trial conducted by Ruglass et al. (Citation2017) had three arms: COPE, relapse prevention, and a waiting list group. There were significant baseline differences between the waiting list arm and the other two arms for PTSD and depression, and we therefore excluded the waiting list arm from our analysis.
In meta-analysis, we found a significant difference in favour of trauma-focused intervention plus SUD intervention for PTSD severity post-treatment (K = 7; N = 544; SMD −0.36, 95% CI −0.64, −0.08; I2 = 54%; GRADE very low). This effect did not reach our threshold for clinical importance. Findings based on three studies were not significant at 3–5 months but were significant, in favour of trauma-focused intervention, at 6–13 months (K = 5; N = 469; SMD −0.48, 95% CI −0.81, −0.15; I2 = 62%; GRADE very low). There was also a difference in favour of trauma-focused intervention for PTSD diagnosis post-treatment based on outcomes from two studies (K = 2; N = 201; RR 0.62, 95% CI 0.46, 0.84; I2 = 30%; GRADE very low). No differences were observed for alcohol or drug use, beyond those achieved for SUD-only intervention, apart from a small effect for alcohol use in favour of trauma-focused intervention at 6–13 months (K = 4; N = 363; SMD −0.23, 95% CI −0.44, −0.02; I2 = 0%; GRADE very low). No differences were observed for treatment dropout or adverse effects. Adverse events were not reported for Coffey et al. (Citation2006) and Coffey et al. (Citation2016).
In view of the limited number of studies, we only investigated subgroup differences by intervention model. For studies evaluating COPE, there were no post-treatment differences for PTSD (K = 3; N = 190; SMD −0.31, 95% CI −0.93, 0.32; I2 = 74%; GRADE very low), alcohol use (K = 1; N = 23; SMD 0.07, 95% CI −0.76, 0.91; GRADE very low), or drug use (K = 3; N = 170; SMD −0.16, 95% CI −0.63, 0.95; I2 = 81%; GRADE very low).
3.1.1.3. Cognitive restructuring-based interventions
Four studies tested integrated cognitive restructuring-based approaches for PTSD and SUD (without imaginal exposure) with interventions for SUD only (Capone et al., Citation2018; Haller et al., Citation2016; McGovern et al., Citation2011, Citation2015). Capone et al. (Citation2018) and McGovern et al. (Citation2011, Citation2015) tested up to 12 sessions of ICBT for PTSD and SUD, while the approach tested by Haller et al, (Citation2016) was based on a form of CPT, where a narrative account of the index trauma experience was excluded. All participants in this study completed 12 sessions of group CBT for SUD and depression before randomization to either 12 individual sessions of CPT for PTSD and SUD, or individual CBT for SUD and depression only. Intervention was offered individually in McGovern et al. (Citation2011, 2015), whereas Capone et al. (Citation2018) offered the first four sessions individually and subsequent sessions were group based. Where reported, participants attended between 45.7% (Capone et al., Citation2018) and 56.3% (Haller et al., Citation2016) of integrated cognitive restructuring sessions available to them. Based on data from two studies (Capone et al., Citation2018; McGovern et al., 2015), 39.4% of participants were considered to be treatment completers. McGovern et al. (2015) included both a relapse prevention and an SUD-only TAU arm. Data from both arms were entered separately into meta-analysis and we followed the guidance in the Cochrane Handbook (Higgins & Green, Citation2011) to ensure that data from the integrated cognitive restructuring arm were not double counted. We found no benefit beyond that of intervention for SUD at any time-point for integrated cognitive interventions for PTSD severity, PTSD diagnosis, alcohol use, or substance use. Outcomes were not reported for treatment dropout or adverse events.
We undertook a subgroup analysis of post-treatment outcomes to investigate the potential benefits of ICBT, excluding Haller et al. (Citation2016) as this study was based on CPT. For PTSD severity, there was a positive effect in favour of ICBT (K = 3; N = 263; SMD −0.33, 95% CI −0.62, −0.04; I2 = 21%; GRADE very low). Effects for alcohol use (K = 3; N = 263; SMD −0.01, 95% CI −0.26, 0.24; I2 = 45%; GRADE very low) and drug use (K = 3; N = 263; SMD −0.16, 95% CI −0.42, 0.09; I2 = 0%; GRADE very low) remained non-significant.
3.1.1.4. Other interventions
No studies tested interventions based on EMDR or any other trauma-focused approach. Data were available for a subset of participants with PTSD and SUD in a study evaluating CBT (without SUD intervention) versus a waiting list control in one study targeted at patients with PTSD and serious mental illness (Mueser et al., Citation2008). The extent to which participants in this study were also receiving intervention specifically for SUD is unknown, so we did not include it in the meta-analyses of integrated cognitive restructuring-based interventions described in Section 3.1.1.3. There was no difference between CBT and the control condition for this SUD subgroup for PTSD severity at any time-point or for PTSD diagnosis. Our other outcomes were not reported. The authors found that across the whole sample, PTSD severity was significantly reduced for those receiving CBT, in comparison to the control.
Data were also available for a subset of participants with PTSD and AUD in a study testing a 12 week web-based CBT intervention (Thinking Forward) plus TAU versus TAU for veterans with PTSD and harmful drinking (Acosta et al., Citation2017). CBT in this intervention did not include a trauma processing or imaginal exposure component. There were no differences for this subgroup on PTSD severity or alcohol use at any time-point. Other outcomes were not reported. The authors reported that across the whole sample (those with AUD and hazardous drinking) there were no significant effects for PTSD, but there were benefits for the web-based CBT for alcohol use and binge drinking.
3.1.2. Active psychological intervention versus other active psychological intervention
Five studies compared two active psychological interventions aimed at treating both PTSD and SUD.
3.1.2.1. Present-focused versus trauma-focused intervention
Norman et al. (Citation2019) compared trauma-focused intervention (COPE) with present-focused intervention (Seeking Safety). Participants received up to 16 sessions of treatment. There was a significant difference in favour of trauma-focused intervention plus SUD intervention for PTSD severity post-treatment (N = 119; SMD −0.49, 95% CI −0.86, −0.13) and at 6–13 months (N = 119; SMD −0.44, 95% CI −0.81, −0.08), but not at 3–5 months. There were no differences for alcohol use, dropout, or adverse events.
3.1.2.2. Present-focused versus integrated CBT intervention
Najavits et al. (Citation2018) tested an integrated past-focused CBT-based approach not including imaginal exposure (Creating Change) with present-focused intervention (Seeking Safety), with participants receiving up to 17 sessions. There were no differences between the two interventions for PTSD severity, or alcohol use at any time-point, or in terms of adverse events.
3.1.2.3. Other active comparisons
Stappenbeck et al. (Citation2015) tested the effectiveness of teaching two coping skills: cognitive restructuring versus experiential acceptance versus attention control. Participants received one session of training followed by up to four coaching calls in the following week. There were no differences between the two interventions for PTSD severity, or alcohol use post-treatment, or treatment dropout. Adverse events were not reported.
Possemato et al. (Citation2019) tested whether there was any benefit in adding peer support to a web-based CBT intervention (Thinking Forward), compared to self-directed web-based CBT, in a small pilot trial aimed at individuals with PTSD and problematic drinking. Data were obtained for a small subset of individuals who met the diagnosis for AUD. There were no differences between the two groups for PTSD or alcohol use outcomes for this subset.
Schacht et al. (Citation2017) tested whether PE where attendance was incentivized with vouchers was superior to PE without incentivization. Participants received up to 12 sessions of treatment. Those in the incentivized arm attended 59.3% of available sessions, with those in the standard PE arm attended 15.0% of sessions. There were no differences between the two interventions for PTSD severity, or alcohol use at any time-point. However, there was a difference in favour of the incentivized approach for treatment dropout (N = 58; RR 10.71, 95% CI 1.46, 78.39).
3.1.3. Sequential psychological intervention versus integrated intervention
Only one study attempted to test sequential versus integrated treatment. Kehle-Forbes et al. (Citation2019) tested the delivery of four sessions of motivational interviewing before 12 sessions of PE against 16 sessions of integrated motivational interviewing and PE. Participants attended 57.3% of available sessions for the sequential approach and 52.2% of sessions for the integrated approach. There were no significant differences between the two approaches for PTSD severity or alcohol use at any time-point (). Dropout, in favour of the sequential approach, approached but did not quite reach significance (N = 183; RR 1.57, 95% CI 0.99, 2.48).
Table 3. Summary of findings for each comparison for two active interventions.
3.2. Synthesis of results for children and young people
Only one pilot study conducted with young people met our inclusion criteria (Najavits et al., Citation2006). This study evaluated an individual present-focused therapy (Seeking Safety + TAU for SUD) in comparison to TAU for SUD in adolescent girls. The study did not provide data usable for secondary analysis post-treatment for PTSD severity or alcohol or drug use. The authors report that outcomes were better for those allocated to Seeking Safety on seven out of 10 substance abuse-related subscales on the Personal Experiences Inventory, which was the study’s primary outcome. Participants in the Seeking Safety group attended a mean of 9.7 (38.7%) of the available treatment sessions. Dropout and adverse events were not reported.
3.3. Methodological quality of included studies
Risk-of-bias judgements for each study are shown in Supplementary Table 1. Eighteen studies were judged to have a low risk of bias for the method of allocation and no studies were judged to be of high risk. Twelve studies provided a clear description of allocation concealment, indicating low risk of bias, and two studies were judged to be at high risk in this domain (Najavits et al., Citation2018; Stappenbeck et al., Citation2015). Adequate blinding of assessment of outcomes measures was indicated in 15 studies, with two studies judged to be at high risk (McGovern et al., Citation2011; Myers et al., Citation2015). Seventeen studies were judged to be at low risk for incompleteness of data, with five studies judged to be at high risk (Coffey et al., Citation2006; Hien et al., Citation2004; Mueser et al., Citation2008; Myers et al., Citation2015; Ruglass et al., Citation2017). Twelve studies, all published since 2011, had registered protocols and were judged to be at low risk of selective reporting, and five studies were judged to be of high risk (Coffey et al., Citation2006; Kehle-Forbes et al., Citation2019; McGovern et al., 2015; Najavits et al., Citation2006; Possemato et al., Citation2019). We considered seven studies to be at low risk of other bias and 16 studies to be at high risk. Reasons for these studies being judged as high risk included possible investigator allegiance to one of the interventions being evaluated (Acosta et al., Citation2017; Back et al., Citation2019; Foa et al., 2013; Najavits et al., Citation2006, NCitation2018; Possemato et al., Citation2019; Ruglass et al., Citation2017), potentially imbalanced use of other interventions (Capone et al., Citation2018; Schäfer et al., Citation2019; Zlotnick et al., Citation2009), possible contamination of treatments (Frisman et al., Citation2008; McGovern et al., 2015; Zlotnick et al., Citation2009), unclear reporting of the number of participants randomized (McGovern et al., 2015), lack of a study intervention manual (McGovern et al., 2015), significant differences in one or more potentially important baseline characteristics (McGovern et al., Citation2011; Mills et al., Citation2012; Myers et al., Citation2015; Najavits et al., Citation2006; Ruglass et al., Citation2017; Stappenbeck et al., Citation2015), differences in the number of available treatment sessions (McGovern et al., Citation2011), divergence from time of planned collection of outcomes (Mills et al., Citation2012), small sample size (Myers et al., Citation2015; Possemato et al., Citation2019), and the use of measures with possibly inadequate validation (Stappenbeck et al., Citation2015). We were unable to investigate for potential publication bias through funnel plots, as there were insufficient studies in each of the analyses to allow us to create these.
4. Discussion
4.1. Main findings
Twenty-seven studies with 2849 participants were included in this review, evaluating a number of mainly CBT-based approaches. For adults, we found evidence that trauma-focused intervention delivered alongside treatment for SUD led to improvements in PTSD symptom severity and diagnosis post-treatment when compared against intervention for SUD only, although the observed effect was below our predefined threshold for a clinically important finding. There was some evidence that PTSD improvements were maintained, and of delayed benefits in reduced alcohol use beyond that of SUD-only intervention, with effects above our threshold of clinical importance for PTSD at 6–13 months, although follow-up data were not available from all trauma-focused studies. A subgroup analysis of studies evaluating the COPE model showed no benefit on any of our primary outcomes over SUD-based intervention alone. However, there was evidence, from one head-to-head study (Norman et al., Citation2019), that trauma-focused intervention in the form of COPE was more effective than present-focused intervention (Seeking Safety) for PTSD severity post-treatment, again with a mixed picture at subsequent follow-up. Although studies evaluating present-focused approaches, mainly evaluating Seeking Safety, reported improvements for PTSD severity and alcohol and drug abuse for participants receiving these interventions, there was no evidence that these approaches led to improvements beyond those found for SUD-only interventions. Although our evaluations of outcomes for all studies evaluating cognitive restructuring-based interventions for PTSD and SUD were not significant, we did find a benefit for ICBT, specifically in improving PTSD severity in a prespecified subgroup analyses (excluding Haller et al., Citation2016). This effect was below our threshold for a clinically important finding. We note that the Haller study was unique in that all participants received 12 sessions of group ICBT for SUD and depression prior to randomization to individual ICBT for SUD and depression only or individual CPT for PTSD and SUD. It is arguable that the two trial interventions in this study were not sufficiently different to be able to demonstrate a meaningful difference between cohorts. There was no evidence of differential benefit for any other intervention evaluated in this review.
Only one study attempted to evaluate the order of intervention delivery (Kehle-Forbes et al., Citation2019). In this study, motivational interviewing was either offered before prolonged exposure or delivered in an integrated way alongside PE. There were no significant differences in outcome. While this study is a welcome addition to the literature, we felt that it did not really address whether the sequential delivery of treatment, as seen in routine clinical practice is any more or any less effective than integrated or combined intervention delivery. Participants in the sequential arm of the study received only four sessions of motivational enhancement therapy (MET) before progressing to PE with the same therapists. They also continued to have their substance use monitored by their therapist, with further MET if needed. It therefore remains very unclear which approach is more suitable in routine clinical practice.
Only one small pilot RCT involving children and adolescents met our inclusion criteria (Najavits et al., Citation2006). This study reported some promising changes in substance abuse-related outcomes and trauma-related beliefs, in favour of Seeking Safety.
GRADE judgements for all positive findings were very low, indicating that we are very uncertain about these estimated effects, which are very likely to change as further studies are reported. Findings received very low ratings for a number of different reasons. Some findings came from single small or moderately powered studies with noted risk of bias concerns. In addition, findings based on meta-analyses of multiple studies tended to be heterogeneous in terms of study populations and study design features, and we could not rule out the possibility of publication bias. Findings in relation to trauma-focused interventions were also rated very low, in part because reported effects were not consistent across the included studies.
The increase in studies from 14 identified by Roberts et al. (Citation2015, Citation2016) to 27 in the current review indicates that this remains an important area of clinical and academic concern for many in the field. The findings from this review in favour of trauma-focused intervention over present-focused approaches are largely consistent with, and reinforce those of earlier reviews (e.g. Roberts et al., Citation2015, Citation2016; Simpson et al., Citation2017; Torchalla et al., Citation2012; van Dam et al., Citation2012), but are based on a larger number of trials. However, to our knowledge, no review has previously reported on small positive outcomes for ICBT for PTSD. Alcohol and substance use reduced across all studies for both experimental and SUD-only treatments, and we saw no evidence of any differential effect for either condition (apart from the small effect in favour of trauma-focused intervention at 6–13 months) across the interventions that we investigated. This is perhaps not surprising given that all participants were able to access some SUD-based intervention, regardless of treatment allocation, and, as participants were normally recruited from addiction services, they were likely to have achieved some reduction in alcohol and drug use consumption before study recruitment occurred. However, we note that the dose of SUD-focused treatment in the experimental integrated treatments that we identified was often significantly less than that offered in the equivalent SUD-only arm, suggesting that on average participants were improving comparably and meaningfully in both conditions. The finding that there was a small difference in alcohol use at 6–13 months in favour of trauma-focused intervention over SUD intervention only is of interest. This difference was seen alongside a similar significant difference in PTSD severity and may indicate a reduced need to self-medicate (Dvorak et al., Citation2014; Kaysen et al., Citation2014; Leeies et al., Citation2010) in those who had received trauma-focused intervention. However, we did not observe a similar improvement in substance use and, given the increased difficulty in obtaining longer-term outcome data, this finding needs to be treated with caution.
Study-defined criteria for a treatment completer were generally modest. As reported previously (Roberts et al., Citation2015, Citation2016; Simpson et al., Citation2017), there was evidence of a high level of dropout across studies and of a relatively low uptake of available treatment sessions, regardless of intervention. Studies also tended to report quite large standard deviations, relative to outcome means, suggesting quite a wide variation in outcome responses. There was evidence from one study (Schacht et al., Citation2017) that dropout was reduced when attendance was incentivized. Patients are known to drop out of treatment for a variety of reasons (Lewis, Roberts, Gibson, & Bisson, Citation2020). There is some evidence from secondary evaluations of some of the larger trials included in this review that a number of factors may influence dropout, including trauma type, rate of PTSD and addiction symptom improvement, between-session alcohol use, educational status, anxiety sensitivity, and more severe baseline PTSD (Belleau et al., Citation2017; Kline, Panza, et al., Citation2021; López-Castro, Zhao, Fitzpatrick, Ruglass, & Hien, Citation2021; Szafranski et al., Citation2017; Zandberg, Rosenfield, Alpert, McLean, & Foa, Citation2016), although PTSD severity is not a consistent finding (Belleau et al., Citation2017). Session attendance has also been found to be influenced by drug-use severity, abstinence status, and employment status (Grundmann et al., Citation2021), and more frequent days of heavy drinking and greater AUD severity (Kline, Straus, et al., Citation2021). There is also some indication that patients who drop out of treatment prematurely and those who do not engage in optimal attendance may still make important improvements (Hien et al., Citation2012; Szafranski et al., Citation2019). However, evidence from the Norman et al. (Citation2019) study indicates that differences in PTSD outcomes in favour of trauma-focused over present-focused therapy intervention were only evident for participants who completed all or most of their treatment sessions (Straus et al., Citation2022).
4.2. Strengths and limitations
This systematic review was undertaken according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Moher, Liberati, Tetzlaff, & Altman, Citation2009) and Cochrane Collaboration guidelines (Higgins & Green, Citation2011) and included registration of a review protocol. We followed a thorough search, screening, and study identification strategy. We searched for both published and unpublished studies, and accessed data from several studies where a subgroup of participants met our inclusion criteria. The methodological quality of included studies was reviewed by all authors and the quality of included studies was comparable to those included in analogous reviews (e.g. Lewis, Roberts, Andrew, et al., Citation2020). Our main methodological concerns were the fact that some studies were conducted by groups with allegiance to interventions that they were investigating and loss to follow-up. Study authors generally took steps to impute missing data through appropriate statistical methods, although reported outcomes for several studies were only based on available follow-up data. An updated Cochrane Collaboration risk-of-bias tool is now available. Our use of the previous version was to maintain continuity with Roberts et al. (Citation2016) and may be viewed as a limitation.
There was significant clinical and statistical heterogeneity in the studies included in this review, and this should be held in mind in interpreting the reported findings. Studies were conducted with a number of different populations, including veterans, victims of domestic abuse, prisoners, and community treatment-seeking patients. Some studies included mainly male samples, while others were female only. Participants also differed in the severity and nature of their addiction use and type of trauma exposure. We grouped interventions for comparison in what we felt was a clinically meaningful way according to our prespecified plan, but within these comparisons there was significant variability in how experimental interventions were delivered and the number of treatment sessions available. There were also significant differences in the nature of control SUD-only interventions that were offered, with some control interventions being more active than others. There was sizeable statistical heterogeneity in some comparisons, but because of the small number of studies contributing to each comparison, we were only able to undertake limited sensitivity/subgroup analyses and we chose to focus on treatment model as we judged that this would be of greatest interest to the reader. Owing to the small number of studies included in each analysis, we were unable to investigate the possibility of publication bias.
4.3. Clinical implications
The number of studies that have evaluated psychological interventions for PTSD and SUD has increased appreciably over the past 5 years, and this review gives a clear indication of interventions that appear to be helpful, particularly in reducing PTSD symptoms, with the strongest findings for trauma-focused interventions. As indicated by Roberts et al. (Citation2015), clinicians should continue to exercise caution when considering whether to provide the interventions identified in this review, as it is unlikely that these interventions will be appropriate for everyone and individual treatment planning will need to be guided by an individual formulation, which takes account of the predictors of outcome, alongside patient-related priorities, risk factors, and preferences (Roberts et al., Citation2020). The studies included in this review mostly continued to exclude on the basis of cognitive impairment, current suicide risk, and severe mental illness, and our findings should not be generalized to individuals with these types of presentation. Going forward, initiatives such as Project Harmony (Saavedra et al., Citation2021), which plan to undertake meta-analysis of individual patient data, are likely to greatly improve our understanding of key patient outcome predictors.
4.4. Implications for research
Given the limited treatment gains described in this review, there is a clear continuing need to develop and evaluate psychological interventions for PTSD and SUD for both adults and younger people. Among children and adolescent populations, we only included one pilot study with female adolescents (Najavits et al., Citation2006). We identified one other adolescent-focused RCT evaluating a family therapy-based intervention (Danielson et al., Citation2020) that did not fulfil our diagnostic inclusion criteria, and a protocol for one study which is currently under way (Mills et al., Citation2020).
There is a need to develop a better understanding of the predictors of symptom improvement and of treatment dropout. It seems of high importance to test whether other non-trauma-focused interventions may be beneficial to patients with PTSD and SUD. The trauma-focused approaches included in this review were all based on prolonged exposure; and there is a need to test whether other established trauma-focused approaches, such as EMDR, cognitive therapy for PTSD, and CPT, can be adapted for this population. There is still considerable uncertainty about how SUD- and PTSD-related interventions should be coordinated and whether sequential, integrated, or combined delivery is most effective or acceptable. Finally, from the PTSD field, several studies have reported on the efficacy of intensive trauma-focused therapies, delivered in a concentrated way over several days (e.g. De Jongh et al., Citation2020; Ehlers et al., Citation2014; Voorendonk, De Jongh, Rozendaal, & Van Minnen, Citation2020). Findings reported for a multicomponent inpatient programme for PTSD patients with significant comorbidity and other complexities have been encouraging in several studies and may warrant evaluation for those with comorbid PTSD (e.g. De Jongh et al., Citation2020; Voorendonk et al., Citation2020; Zoet, Wagenmans, van Minnen, & de Jongh, Citation2018).
Open Scholarship
 This article has earned the Center for Open Science badge for Open Data. The data are openly accessible at https://doi.org/10.34691/FK2/ULMNHV.
This article has earned the Center for Open Science badge for Open Data. The data are openly accessible at https://doi.org/10.34691/FK2/ULMNHV.
Supplemental Material
Download MS Word (51 KB)Acknowledgements
We would like to thank Dr Jana Javakhishvili for initiating this work. We would also like to thank Dr Sudie Back, Dr Julian Ford, Dr Moira Haller, Dr Hsiu-Ju Lin, Dr Sonya Norman, and Dr Kyle Possemato for help in providing additional unpublished data. Neil Roberts had full access to all of the data in this review and takes responsibility for the data integrity and the accuracy of the data analysis.
Disclosure statement
Dr Ingo Schäfer and Dr Annett Lotzin have published one RCT that was included in the review. Dr Neil Roberts reports no competing interests. Dr Roberts has been involved in the development of an internet-based guided self-help intervention for PTSD called SPRING, and may receive future profits if the intervention is monetized.
Data availability statement
This paper does not include any primary data.
References
- Acosta, M. C., Possemato, K., Maisto, S. A., Marsch, L. A., Barrie, K., Lantinga, L., … Rosenblum, A. (2017). Web-delivered CBT reduces heavy drinking in OEF-OIF veterans in primary care with symptomatic substance use and PTSD. Behavior Therapy, 48(2), 262–276. doi:10.1016/j.beth.2016.09.001
- American Psychological Association. (2017). Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults. American Psychological Association. Retrieved from www.apa.org/ptsd-guideline
- Back, S. E., Foa, E. B., Killeen, T. K., Mills, K. L., Teesson, M., Carroll, K. M., et al. (2014). Concurrent treatment of PTSD and substance use disorders using prolonged exposure (COPE): Therapist manual. New York: Oxford University Press.
- Back, S. E., Killeen, T., Badour, C. L., Flanagan, J. C., Allan, N. P., Ana, E. S., … Brady, K. T. (2019). Concurrent treatment of substance use disorders and PTSD using prolonged exposure: A randomized clinical trial in military veterans. Addictive Behaviors, 90, 369–377. doi:10.1016/j.addbeh.2018.11.032
- Belleau, E. L., Chin, E. G., Wanklyn, S. G., Zambrano-Vazquez, L., Schumacher, J. A., & Coffey, S. F. (2017). Pre-treatment predictors of dropout from prolonged exposure therapy in patients with chronic posttraumatic stress disorder and comorbid substance use disorders. Behaviour Research and Therapy, 91, 43–50. doi:10.1016/j.brat.2017.01.011
- Bisson, J. I., Berliner, L., Cloitre, M., Forbes, D., Jensen, T. K., Lewis, C., … Shapiro, F. (2019). The International Society for Traumatic Stress Studies new guidelines for the prevention and treatment of posttraumatic stress disorder: Methodology and development process. Journal of Traumatic Stress, 32(4), 475–483.
- Blakey, S. M., Dillon, K. H., Wagner, H. R., Simpson, T. L., Beckham, J. C., Calhoun, P. S., & Elbogen, E. B. (2022). Psychosocial well-being among veterans with posttraumatic stress disorder and substance use disorder. Psychological Trauma: Theory, Research, Practice and Policy, 14(3), 421–430. doi:10.1037/tra0001018
- Boden, M. T., Kimerling, R., Kulkarni, M., Bonn-Miller, M. O., Weaver, C., & Trafton, J. (2014). Coping among military veterans with PTSD in substance use disorder treatment. Journal of Substance Abuse Treatment, 47(2), 160–167. doi:10.1016/j.jsat.2014.03.006
- Capone, C., Presseau, C., Saunders, E., et al. (2018). Is integrated CBT effective in reducing PTSD symptoms and substance use in Iraq and Afghanistan veterans? Results from a randomized clinical trial. Cognitive Therapy and Research, 42, 735–746. doi:10.1007/s10608-018-9931-8
- Coffey, S. F., Schumacher, J. A., Nosen, E., Littlefield, A. K., Henslee, A. M., Lappen, A., & Stasiewicz, P. R. (2016). Trauma-focused exposure therapy for chronic posttraumatic stress disorder in alcohol and drug dependent patients: A randomized controlled trial. Psychology of Addictive Behaviors, 30(7), 778–790. doi:10.1037/adb0000201
- Coffey, S. F., Stasiewicz, P. R., Hughes, P. M., & Brimo, M. L. (2006). Trauma-focused imaginal exposure for individuals with comorbid posttraumatic stress disorder and alcohol dependence: Revealing mechanisms of alcohol craving in a cue reactivity paradigm. Psychology of Addictive Behaviors, 20(4), 425–435. doi:10.1037/0893-164X.20.4.425
- Danielson, C. K., Adams, Z., McCart, M. R., Chapman, J. E., Sheidow, A. J., Walker, J., … de Arellano, M. A. (2020). Safety and efficacy of exposure-based risk reduction through family therapy for co-occurring substance use problems and posttraumatic stress disorder symptoms among adolescents: A randomized clinical trial. JAMA Psychiatry, 77(6), 574–586. doi:10.1001/jamapsychiatry.2019.4803
- De Jongh, A., Groenland, G. N., Sanches, S., Bongaerts, H., Voorendonk, E. M., & Van Minnen, A. (2020). The impact of brief intensive trauma-focused treatment for PTSD on symptoms of borderline personality disorder. European Journal of Psychotraumatology, 11(1), 1721142. doi:10.1080/20008198.2020.1721142
- Debell, F., Fear, N. T., Head, M., Batt-Rawden, S., Greenberg, N., Wessely, S., & Goodwin, L. (2014). A systematic review of the comorbidity between PTSD and alcohol misuse. Social Psychiatry and Psychiatric Epidemiology, 49(9), 1401–1425. doi:10.1007/s00127-014-0855-7
- Degenhardt, L., Whiteford, H. A., Ferrari, A. J., Baxter, A. J., Charlson, F. J., Hall, W. D., … Vos, T. (2013). Global burden of disease attributable to illicit drug use and dependence: Findings from the Global Burden of Disease Study 2010. The Lancet, 382(9904), 1564–1574. doi:10.1016/S0140-6736(13)61530-5
- Dvorak, R. D., Pearson, M. R., & Day, A. M. (2014). Ecological momentary assessment of acute alcohol use disorder symptoms: Associations with mood, motives, and use on planned drinking days. Experimental and Clinical Psychopharmacology, 22(4), 285–297. doi:10.1037/a0037157
- Ehlers, A., Hackmann, A., Grey, N., Wild, J., Liness, S., Albert, I., … Clark, D. M. (2014). A randomized controlled trial of 7-day intensive and standard weekly cognitive therapy for PTSD and emotion-focused supportive therapy. The American Journal of Psychiatry, 171(3), 294–304. doi:10.1176/appi.ajp.2013.13040552
- Foa, E. B., Yusko, D. A., McLean, C. P., Suvak, M. K., Bux, D. A., Jr, Oslin D., … Volpicelli, J. (2013). Concurrent naltrexone and prolonged exposure therapy for patients with comorbid alcohol dependence and PTSD: A randomized clinical trial. JAMA, 310(5), 488–495. https://doi.org/10.1001/jama.2013.8268
- Ford, J. D., & Russo, E. (2006). Trauma-focused, present-centered, emotional self-regulation approach to integrated treatment for posttraumatic stress and addiction: Trauma Adaptive Recovery Group Education and Therapy (TARGET). American Journal of Psychotherapy, 60(4), 335–355. doi:10.1176/appi.psychotherapy.2006.60.4.335
- Frisman, L., Ford, J., Lin, H.-J., Mallon, S., & Chang, R. (2008). Outcomes of trauma treatment using the TARGET model. Journal of Groups in Addiction & Recovery, 3(3–4), 285–303. doi:10.1080/15560350802424910
- Gielen, N., Havermans, R. C., Tekelenburg, M., & Jansen, A. (2012). Prevalence of post-traumatic stress disorder among patients with substance use disorder: It is higher than clinicians think it is. European Journal of Psychotraumatology, 3, 17734. doi:10.3402/ejpt.v3i0.17734
- Grant, B. F., Saha, T. D., Ruan, W. J., Goldstein, R. B., Chou, S. P., Jung, J., … Hasin, D. S. (2016). Epidemiology of DSM-5 drug use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. JAMA Psychiatry, 73(1), 39–47. doi:10.1001/jamapsychiatry.2015.2132
- Grundmann, J., Lotzin, A., Sehner, S., Verthein, U., Hiller, P., Hiersemann, R., … Schäfer, I. (2021). Predictors of attendance in outpatient group treatment for women with posttraumatic stress disorder and substance use disorder. Psychotherapy Research, 31(5), 632–643. doi: 10.1080/10503307.2020.1817604
- Guyatt, G. H., Oxman, A. D., Schünemann, H. J., Tugwell, P., & Knottnerus, A. (2011). GRADE guidelines: A series of new articles in the Journal of Clinical Epidemiology. Journal of Clinical Epidemiology, 64(4), 380–382. doi:10.1016/j.jclinepi.2010.09.011
- Haller, M., Norman, S. B., Cummins, K., Trim, R. S., Xu, X., Cui, R., … Tate, S. R. (2016). Integrated cognitive behavioral therapy versus cognitive processing therapy for adults with depression, substance use disorder, and trauma. Journal of Substance Abuse Treatment, 62, 38–48. doi:10.1016/j.jsat.2015.11.005
- Hien, D. A., Cohen, L. R., Miele, G. M., Litt, L. C., & Capstick, C. (2004). Promising treatments for women with comorbid PTSD and substance use disorders. American Journal of Psychiatry, 161(8), 1426–1432. doi:10.1176/appi.ajp.161.8.1426
- Hien, D. A., Morgan-Lopez, A. A., Campbell, A. N., Saavedra, L. M., Wu, E., Cohen, L., … Nunes, E. V. (2012). Attendance and substance use outcomes for the Seeking Safety program: Sometimes less is more. Journal of Consulting and Clinical Psychology, 80(1), 29–42. doi:10.1037/a0026361
- Hien, D. A., Wells, E. A., Jiang, H., Suarez-Morales, L., Campbell, A. N. C., Cohen, L. R., et al. (2009). Multisite randomized trial of behavioral interventions for women with cooccurring PTSD and substance use disorders. Journal of Consulting and Clinical Psychology, 77(4), 607–619. doi:10.1037/a0016227
- Hien, D., Fitzpatrick, S., Saavedra, L., Ebrahimi, C., Norman, S., Tripp, J., et al. (2022). What’s in a name? A data-driven method to identify optimal psychotherapy classifications to advance treatment research on co-occurring PTSD and substance use disorders. European Journal of Psychotraumatology, 13, 1. doi:10.1080/20008198.2021.2001191
- Higgins, J. P. T., & Green, S. (2011). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration. Retrieved from www.cochrane-handbook.org
- International Society for Traumatic Stress Studies. (2018). ISTSS prevention and treatment guidelines (2018). Retrieved from https://www.istss.org/treatingtrauma/new-istss-prevention-and-treatment-guidelines.aspx
- Jakupcak, M., Conybeare, D., Phelps, L., Hunt, S., Holmes, H. A., Felker, B., … McFall, M. E. (2007). Anger, hostility, and aggression among Iraq and Afghanistan War veterans reporting PTSD and subthreshold PTSD. Journal of Traumatic Stress, 20(6), 945–954. doi:10.1002/jts.20258
- Jhanjee, S. (2014). Evidence based psychosocial interventions in substance use. Indian Journal of Psychological Medicine, 36(2), 112–118. doi:10.4103/0253-7176.130960
- Kaysen, D., Stappenbeck, C., Rhew, I., & Simpson, T. (2014). Proximal relationships between PTSD and drinking behavior. European Journal of Psychotraumatology, 5, 26518. doi:10.3402/ejpt.v5.26518
- Kehle-Forbes, S. M., Chen, S., Polusny, M. A., Lynch, K. G., Koffel, E., Ingram, E., … Oslin, D. W. (2019). A randomized controlled trial evaluating integrated versus phased application of evidence-based psychotherapies for military veterans with comorbid PTSD and substance use disorders. Drug and Alcohol Dependence, 205, 107647. doi:10.1016/j.drugalcdep.2019.107647
- Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E. J., Cardoso, G., … Koenen, K. C. (2017). Trauma and PTSD in the WHO World Mental Health Surveys. European Journal of Psychotraumatology, 8(sup5), 1353383. doi:10.1080/20008198.2017.1353383
- Kline, A. C., Panza, K. E., Harlé, K. M., Angkaw, A. C., Trim, R. S., Back, S. E., & Norman, S. B. (2021). Within-treatment clinical markers of dropout risk in integrated treatments for comorbid PTSD and alcohol use disorder. Drug and Alcohol Dependence, 221, 108592. doi:10.1016/j.drugalcdep.2021.108592
- Kline, A. C., Straus, E., Lyons, R. C., Angkaw, A. C., Davis, B. C., Haller, M., … Norman, S. B. (2021). Substance use predictors of attendance among veterans in integrated PTSD and alcohol use disorder treatment. Journal of Substance Abuse Treatment, 124, 108278. doi:10.1016/j.jsat.2021.108278
- Langdon, K. J., Fox, A. B., King, L. A., King, D. W., Eisen, S., & Vogt, D. (2016). Examination of the dynamic interplay between posttraumatic stress symptoms and alcohol misuse among combat-exposed Operation Enduring Freedom (OEF)/Operation Iraqi Freedom (OIF) veterans. Journal of Affective Disorders, 196, 234–242. doi:10.1016/j.jad.2016.02.048
- Langendam, M. W., Akl, E. A., Dahm, P., Glasziou, P., Guyatt, G., & Schünemann, H. J. (2013). Assessing and presenting summaries of evidence in Cochrane reviews. Systematic Reviews, 23(2), 81. doi:10.1186/2046-4053-2-81
- Leeies, M., Pagura, J., Sareen, J., & Bolton, J. M. (2010). The use of alcohol and drugs to self-medicate symptoms of posttraumatic stress disorder. Depression and Anxiety, 27(8), 731–736. doi:10.1002/da.20677
- Leeman, R. F., Hefner, K., Frohe, T., Murray, A., Rosenheck, R. A., Watts, B. V., & Sofuoglu, M. (2017). Exclusion of participants based on substance use status: Findings from randomized controlled trials of treatments for PTSD. Behaviour Research and Therapy, 89, 33–40. doi:10.1016/j.brat.2016.10.006
- Lewis, C. E., Roberts, N. P., Gibson, S., & Bisson, J. I. (2020). Dropout from psychological therapies for post-traumatic stress disorder (PTSD) in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1), 1709709. doi:10.1080/20008198.2019.1709709
- Lewis, C., Roberts, N. P., Andrew, M., Starling, E., & Bisson, J. I. (2020). Psychological therapies for post-traumatic stress disorder in adults: Systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1), 1729633. doi:10.1080/20008198.2020.1729633
- López-Castro, T., Zhao, Y., Fitzpatrick, S., Ruglass, L. M., & Hien, D. A. (2021). Seeing the forest for the trees: Predicting attendance in trials for co-occurring PTSD and substance use disorders with a machine learning approach. Journal of Consulting and Clinical Psychology, 89(10), 869–884. doi:10.1037/ccp0000688
- McGovern, M. P., Lambert-Harris, C., Alterman, A. I., Xie, H., & Meier, A. (2011). A randomized controlled trial comparing integrated cognitive behavioral therapy versus individual addiction counseling for co-occurring substance use and posttraumatic stress disorders. Journal of Dual Diagnosis, 7(4), 207–227. doi:10.1080/15504263.2011.620425
- McGovern, M. P., Lambert-Harris, C., Xie, H., Meier, A., McLeman, B., & Saunders, E. (2015). A randomized controlled trial of treatments for co-occurring substance use disorders and post-traumatic stress disorder. Addiction, 110(7), 1194–1204. https://doi.org/10.1111/add.12943
- Mills, K. L., Barrett, E., Back, S. E., Cobham, V. E., Bendall, S., Perrin, S., … Teesson, M. (2020). Randomised controlled trial of integrated trauma-focused psychotherapy for traumatic stress and substance use among adolescents: Trial protocol. BMJ Open, 10(11), e043742. doi:10.1136/bmjopen-2020-043742
- Mills, K. L., Teeson, M., Back, S. E., Brady, K. T., Baker, A. L., Hopwood, S., et al. (2012). Integrated exposure based therapy for co-occurring posttraumatic stress disorder and substance dependence. Journal of the American Medical Association, 308(7), 690–699. doi:10.1001/jama.2012.9071
- Mills, K. L., Teeson, M., Ross, J., & Peters, L. (2006). Trauma, PTSD, and substance use disorders: Findings from the Australian National Survey of Mental Health and Well-Being. American Journal of Psychiatry, 163(4), 652–658. doi:10.1176/appi.ajp.163.4.652
- Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. doi:10.1371/journal.pmed.1000097
- Mueser, K. T., Rosenburg, S. D., Xie, H., Jankowski, M. K., Bolton, E. E., Lu, W., et al. (2008). A randomized controlled trial of cognitive–behavioral treatment for posttraumatic stress disorder in severe mental illness. Journal of Consulting and Clinical Psychology, 76(2), 259–271. doi:10.1037/0022-006X.76.2.259
- Myers, U. S., Browne, K. C., & Norman, S. B. (2015). Treatment engagement: Female survivors of intimate partner violence in treatment for PTSD and alcohol use disorder. Journal of Dual Diagnosis, 11(3-4), 238–247. doi:10.1080/15504263.2015.1113762
- Najavits, L. M. (2002). Seeking safety: A treatment manual for PTSD and substance abuse. New York, NY: Guilford Press.
- Najavits, L. M., Gallop, R. J., & Weiss, R. D. (2006). Seeking Safety therapy for adolescent girls with PTSD and substance use disorder: A randomized controlled trial. Journal of Behavioral Health Services and Research, 33(4), 453–463. doi:10.1007/s11414-006-9034-2
- Najavits, L. M., Gastfriend, D. R., Barber, J. P., Reif, S., Muenz, L. R., Blaine, J., et al. (1998). Cocaine dependence with and without PTSD among subjects in the National Institute on Drug Abuse Collaborative Cocaine Treatment Study. American Journal of Psychiatry, 155, 214–219.
- Najavits, L. M., Krinsley, K., Waring, M. E., Gallagher, M. W., & Skidmore, C. (2018). A randomized controlled trial for veterans with PTSD and substance use disorder: Creating change versus seeking safety. Substance Use & Misuse, 53(11), 1788–1800. doi:10.1080/10826084.2018.1432653
- NICE. (2007). Drug misuse in over 16s: psychosocial interventions. National Institute for Health and Care Excellence. Retrieved from www.nice.org.uk/guidance/cg51
- NICE. (2018). Post-traumatic stress disorder. National Institute for Health and Care Excellence. Retrieved from www.nice.org.uk/guidance/ng116
- NIDA. (2020). Behavioral Therapies. Retrieved from https://www.drugabuse.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition/evidence-based-approaches-to-drug-addiction-treatment/behavioral-therapies on 2021, August 1.
- Norman, S. B., Trim, R., Haller, M., Davis, B. C., Myers, U. S., Colvonen, P. J., … Mayes, T. (2019). Efficacy of integrated exposure therapy vs integrated coping skills therapy for comorbid posttraumatic stress disorder and alcohol use disorder: A randomized clinical trial. JAMA Psychiatry, 76(8), 791–799. doi:10.1001/jamapsychiatry.2019.0638
- Phoenix Australia. (2020). The Australian guidelines for the prevention and treatment of acute stress disorder (ASD), posttraumatic stress disorder (PTSD) and complex PTSD. Retrieved from https://www.phoenixaustralia.org/australian-guidelines-for-ptsd/.
- Possemato, K., Johnson, E. M., Emery, J. B., Wade, M., Acosta, M. C., Marsch, L. A., … Maisto, S. A. (2019). A pilot study comparing peer supported web-based CBT to self-managed web CBT for primary care veterans with PTSD and hazardous alcohol use. Psychiatric Rehabilitation Journal, 42(3), 305–313. doi:10.1037/prj0000334
- Review Manager (RevMan) [Computer program]. Version 5.4.1 Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration. (2020).
- Reynolds, M., Hinchliffe, K., Asamoah, V., & Kouimtsidis, C. (2011). Trauma and post-traumatic stress disorder in a drug treatment community service. The Psychiatrist, 35(7), 256–260. doi:10.1192/pb.bp.110.030379
- Reynolds, M., Mezey, G., Chapman, M., Wheeler, M., Drummond, C., & Baldacchino, A. (2005). Co-morbid post-traumatic stress disorder in a substance misusing clinical population. Drug and Alcohol Dependence, 77(3), 251–258. doi:10.1016/j.drugalcdep.2004.08.017
- Roberts, N. P., Roberts, P. A., Jones, N., & Bisson, J. I. (2015). Psychological interventions for post-traumatic stress disorder and comorbid substance use disorder: A systematic review and meta-analysis. Clinical Psychology Review, 38, 25–38. doi:10.1016/j.cpr.2015.02.007
- Roberts, N. P., Roberts, P. A., Jones, N., & Bisson, J. I. (2016). Psychological therapies for post-traumatic stress disorder and comorbid substance use disorder. Cochrane Database of Systematic Reviews, 2016(4), CD010204. doi:10.1002/14651858.CD010204.pub2
- Roberts, N. P., Back, S. E., Mueser, K. T., & Murray, L. (2020). Treatment considerations for PTSD comorbidities. In D. Forbes, J. I. Bisson, C. Monson, & L. Berliner (Eds.), Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies (3rd ed., pp. 417–450). New York, NY: Guilford Press.
- Ruglass, L. M., Lopez-Castro, T., Papini, S., Killeen, T., Back, S. E., & Hien, D. A. (2017). Concurrent treatment with prolonged exposure for co-occurring full or subthreshold posttraumatic stress disorder and substance use disorders: A randomized clinical trial. Psychotherapy and Psychosomatics, 86(3), 150–161. doi:10.1159/000462977
- Saavedra, L. M., Morgan-López, A. A., Hien, D. A., López-Castro, T., Ruglass, L. M., Back, S. E., … CAST, the Consortium on Addictions, Stress and Trauma (2021). Evaluating treatments for posttraumatic stress disorder, alcohol and other drug use disorders using meta-analysis of individual patient data: Design and methodology of a virtual clinical trial. Contemporary Clinical Trials, 107, 106479. doi:10.1016/j.cct.2021.106479
- Sannibale, C., Teesson, M., Creamer, M., Sitharthan, T., Bryant, R. A., Sutherland, K., et al. (2013). Randomized controlled trial of cognitive behaviour therapy for comorbid post-traumatic stress disorder and alcohol use disorders. Addiction, 108(8), 1397–1410. doi:10.1111/add.12167
- Schacht, R. L., Brooner, R. K., King, V. L., Kidorf, M. S., & Peirce, J. M. (2017). Incentivizing attendance to prolonged exposure for PTSD with opioid use disorder patients: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 85(7), 689–701. doi:10.1037/ccp0000208
- Schäfer, I., Langeland, W., Hissbach, J., Luedecke, C., Ohlmeier, M. D., Chodzinski, C., … TRAUMAB-Study group (2010). Childhood trauma and dissociation in patients with alcohol dependence, drug dependence, or both – A multi-center study. Drug and Alcohol Dependence, 109(1-3), 84–89. doi:10.1016/j.drugalcdep.2009.12.012
- Schäfer, I., & Lotzin, A. (2018). Psychosocial support to tackle trauma-related symptoms and related substance use disorders. Co-operation Group to Combat Drug Abuse and Illicit Trafficking in Drugs, Council of Europe. Retrieved from https://www.drugsandalcohol.ie/30825/
- Schäfer, I., Lotzin, A., Hiller, P., Sehner, S., Driessen, M., Hillemacher, T., … Grundmann, J. (2019). A multisite randomized controlled trial of seeking safety vs. relapse prevention training for women with co-occurring posttraumatic stress disorder and substance use disorders. European Journal of Psychotraumatology, 10(1), 1577092. doi:10.1080/20008198.2019.1577092
- Schäfer, I., & Najavits, L. M. (2007). Clinical challenges in the treatment of patients with posttraumatic stress disorder and substance abuse. Current Opinion in Psychiatry, 20, 614–618. doi:10.1097/YCO.0b013e3282f0ffd9
- Seal, K. H., Cohen, G., Waldrop, A., Cohen, B. E., Maguen, S., & Ren, L. (2011). Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001-2010: Implications for screening, diagnosis and treatment. Drug and Alcohol Dependence, 116(1-3), 93–101. doi:10.1016/j.drugalcdep.2010.11.027
- Simpson, T. L., Lehavot, K., & Petrakis, I. L. (2017). No wrong doors: Findings from a critical review of behavioral randomized clinical trials for individuals with co-occurring alcohol/drug problems and posttraumatic stress disorder. Alcoholism, Clinical and Experimental Research, 41(4), 681–702. doi:10.1111/acer.13325
- Simpson, T. L., Stappenbeck, C. A., Luterek, J. A., Lehavot, K., & Kaysen, D. L. (2014). Drinking motives moderate daily relationships between PTSD symptoms and alcohol use. Journal of Abnormal Psychology, 123(1), 237–247. doi:10.1037/a0035193
- Stappenbeck, C. A., Luterek, J. A., Kaysen, D., Rosenthal, C. F., Gurrad, B., & Simpson, T. L. (2015). A controlled examination of two coping skills for daily alcohol use and PTSD symptom severity among dually diagnosed individuals. Behaviour Research and Therapy, 66, 8–17. doi:10.1016/j.brat.2014.12.013
- Straus, E., Haller, M., Lyons, R. C., & Norman, S. B. (2018). Functional and psychiatric correlates of comorbid post-traumatic stress disorder and alcohol use disorder. Alcohol Research: Current Reviews, 39(2), 121–129.
- Straus, E., Worley, M. J., Lyons, R., Kline, A. C., Tripp, J. C., Davis, B. C., … Norman, S. B. (2022). Examining attendance patterns across integrated therapies for posttraumatic stress disorder and alcohol use disorder. Journal of Anxiety Disorders, 85, 102498. Advance online publication. doi:10.1016/j.janxdis.2021.102498
- Szafranski, D. D., Gros, D. F., Acierno, R., Brady, K. T., Killeen, T. K., & Back, S. E. (2019). Heterogeneity of treatment dropout: PTSD, depression, and alcohol use disorder reductions in PTSD and AUD/SUD treatment noncompleters. Clinical Psychology & Psychotherapy, 26(2), 218–226. doi:10.1002/cpp.2344
- Szafranski, D. D., Snead, A., Allan, N. P., Gros, D. F., Killeen, T., Flanagan, J., … Back, S. E. (2017). Integrated, exposure-based treatment for PTSD and comorbid substance use disorders: Predictors of treatment dropout. Addictive Behaviors, 73, 30–35. doi:10.1016/j.addbeh.2017.04.005
- Torchalla, I., Nosen, L., Rostam, H., & Allen, P. (2012). Integrated treatment programs for individuals with concurrent substance use disorders and trauma experiences: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 42(1), 65–77. doi:10.1016/j.jsat.2011.09.001
- Tripp, J. C., Worley, M. J., Straus, E., Angkaw, A. C., Trim, R. S., & Norman, S. B. (2020). Bidirectional relationship of posttraumatic stress disorder (PTSD) symptom severity and alcohol use over the course of integrated treatment. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors, 34(4), 506–511. doi:10.1037/adb0000564
- VA/DOD. (2017). Clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder: Clinician summary. Retrieved from https://www.healthquality.va.gov/guidelines/mh/ptsd/
- van Dam, D., Vedel, E., Ehring, T., & Emmelkamp, P. M. (2012). Psychological treatments for concurrent posttraumatic stress disorder and substance use disorder: A systematic review. Clinical Psychology Review, 32(3), 202–214. doi:10.1016/j.cpr.2012.01.004
- Voorendonk, E. M., De Jongh, A., Rozendaal, L., & Van Minnen, A. (2020). Trauma-focused treatment outcome for complex PTSD patients: Results of an intensive treatment programme. European Journal of Psychotraumatology, 11(1), 1783955. doi:10.1080/20008198.2020.1783955
- Vujanovic, A. A., Smith, L. J., Green, C. E., Lane, S. D., & Schmitz, J. M. (2018). Development of a novel, integrated cognitive-behavioral therapy for co-occurring posttraumatic stress and substance use disorders: A pilot randomized clinical trial. Contemporary Clinical Trials, 65, 123–129. doi:10.1016/j.cct.2017.12.013
- World Health Organization. (2011). Global Status report on alcohol and health. Retrieved from www.who.int/substance_abuse/publications/global_alcohol_report/msbgsruprofiles.pdf (accessed 1 August 2021).
- Zandberg, L. J., Rosenfield, D., Alpert, E., McLean, C. P., & Foa, E. B. (2016). Predictors of dropout in concurrent treatment of posttraumatic stress disorder and alcohol dependence: Rate of improvement matters. Behaviour Research and Therapy, 80, 1–9. doi:10.1016/j.brat.2016.02.005
- Zlotnick, C., Johnson, J., & Najavits, L. M. (2009). Randomized controlled pilot study of cognitive-behavioral therapy in a sample of incarcerated women with substance use disorder and PTSD. Behavior Therapy, 40(4), 325–336. doi:10.1016/j.beth.2008.09.004
- Zoet, H. A., Wagenmans, A., van Minnen, A., & de Jongh, A. (2018). Presence of the dissociative subtype of PTSD does not moderate the outcome of intensive trauma-focused treatment for PTSD. European Journal of Psychotraumatology, 9(1), 1468707. doi:10.1080/20008198.2018.1468707
