ABSTRACT
Background
Sexual assault is associated with a high risk of developing PTSD. Little is known about the PTSD onset in children who have recently been victimized by sexual assault. It is important to identify children at risk for PTSD after sexual assault to prevent chronic problems and revictimization.
Objective
The first aim of this study was to describe the development of post-traumatic stress symptoms in the four weeks after sexual assault. The second aim was to analyse whether pre-assault factors, assault-related factors, social support, and post-traumatic stress, measured at two weeks post-assault, were associated with an indication of PTSD.
Method
From January 2019 to March 2021, data were collected of victims aged 8–17 years (n = 51; mean age = 15.00; SD = 1.78) who had contacted a Sexual Assault Centre. Severity of post-traumatic stress symptoms was measured at two and four weeks post-assault. The study was designed to use a multivariate logistic regression analysis. The study included female victims only.
Results
Most of the victims (58.8%) showed a decline in the severity of post-traumatic stress symptoms in the four weeks after sexual assault. However, 27.4% showed an increase and 13.7% showed no change in symptoms. More than two-thirds of the children (70.6%) showed severe post-traumatic stress symptoms at four weeks post-assault, i.e. had an indication of PTSD. Since only one significant difference was found, the multivariate analysis was not executed. A significant difference was found between severity of symptoms at two weeks and an indication of PTSD at four weeks (t(49) = −5.79; p < .001).
Conclusion
Children with high levels of post-traumatic stress at two weeks post-assault are at risk for PTSD indication at four weeks post-assault. Further research is needed to determine whether early trauma-based treatment for children with high post-traumatic stress symptoms can prevent the development of PTSD.
HIGHLIGHTS
Young victims of recent sexual assault with high levels of post-traumatic stress symptoms at two weeks post-assault are at risk for PTSD indication at four weeks post-assault, although they received immediate psychological care
Antecedentes: La agresión sexual está asociada con un alto riesgo de desarrollar TEPT. Poco se sabe sobre la aparición de TEPTen niños que recientemente han sido víctimas de agresión sexual. Es importante identificar a los niños en riesgo de TEPTdespués de una agresión sexual para prevenir problemas crónicos y revictimización.
Objetivo: El primer objetivo de este estudio fue describir el desarrollo de síntomas de estrés postraumático en las cuatro semanas posteriores a la agresión sexual. El segundo objetivo fue analizar si los factores previos a la agresión, los factores relacionados con la agresión, el apoyo social y el estrés postraumático, medidos dos semanas después de la agresión, estaban asociados con una presentación de síntomas de TEPT.
Método: Desde Enero de 2019 hasta Marzo de 2021, se recogieron datos de víctimas de 8 a 17 años (n = 51; edad media = 15,00; desviación estándar = 1,78) que habían contactado con un Centro de Agresiones Sexuales. La gravedad de los síntomas de estrés postraumático se midió a las dos y cuatro semanas posteriores a la agresión. El estudio fue diseñado para utilizar un análisis de regresión logística multivariado. El estudio incluyó solo a víctimas femeninas.
Resultados: La mayoría de las víctimas (58,8%) mostró una disminución en la severidad de los síntomas de estrés postraumático en las cuatro semanas posteriores a la agresión sexual. Sin embargo, el 27,4% mostró un aumento y el 13,7% no mostró cambios en los síntomas. Más de dos tercios de los niños (70,6%) mostraron síntomas de estrés postraumático severo cuatro semanas después de la agresión, es decir, tenían indicios de TEPT. Dado que solo se encontró una diferencia significativa, no se ejecutó el análisis multivariado. Se encontró una diferencia significativa entre la severidad de los síntomas a las dos semanas y una indicación de TEPT a las cuatro semanas (t(49) = −5.79; p < .001).
Conclusión: Los niños con altos niveles de estrés postraumático a las dos semanas posteriores a la agresión están en riesgo de presentar síntomas de TEPT a las cuatro semanas posteriores a la agresión. Se necesita más investigación para determinar si el tratamiento precoz basado en el trauma para niños con altos síntomas de estrés postraumático puede prevenir el desarrollo de TEPT.
背景: 性侵犯与发展为 PTSD 的高风险相关。对于最近遭受性侵犯儿童的 PTSD 发病情况知之甚少。识别性侵犯后有患 PTSD 风险的儿童对于防止慢性问题和再次受害非常重要。
目的: 本研究的第一个目的是描述性侵犯后四周内创伤后应激症状的发展。第二个目的是分析在侵犯后两周测量的侵犯前因素、侵犯相关因素、社会支持和创伤后应激是否与 PTSD 指征相关。
方法: 从 2019 年 1 月至 2021 年 3 月, 收集了 8 至 17 岁 (n = 51; 平均年龄 = 15.00; SD = 1.78) 曾联系过性侵犯中心的受害者数据。在侵犯后两周和四周测量创伤后应激症状的严重程度。该研究旨在使用多变量逻辑回归分析。该研究仅包括女性受害者。
结果: 大多数受害者(58.8%) 在性侵犯后四周内, 创伤后应激症状的严重程度有所下降。然而, 27.4% 的人症状有所增加, 13.7% 症状没有变化。超过三分之二的儿童 (70.6%) 在侵犯后四周表现出严重的创伤后应激症状, 即有 PTSD 指征。由于仅发现一个显著差异, 因此未执行多变量分析。两周时的症状严重程度与四周时的PTSD 指征之间存在显著差异(t(49) = −5.79; p < .00)。
结论: 在侵犯后两周内具有高水平创伤后应激的儿童在侵犯后 4 周有出现 PTSD 指征的风险。需要进一步的研究来确定对具有高创伤后应激症状的儿童进行早期基于创伤的治疗是否可以预防PTSD的发展。
PALABRAS CLAVE:
1. Introduction
Trauma in children is not uncommon. More than two-third of all children report at least one traumatic event by the age of sixteen (Copeland, Keeler, Angold, & Costello, Citation2007). These events include natural disasters and accidents, as well as interpersonal violence and sexual assault. As a common psychological response, children often show post-traumatic stress symptoms during or in the aftermath of a traumatic event, that mostly decrease naturally (Copeland et al., Citation2007; Hiller, M.,Meiser-Stedman et al. Citation2016; Kessler et al., Citation2017).
A meta-analysis evaluating 72 peer-reviewed articles on 43 independent studies (n = 3563), showed an overall prevalence of 15.9% post-traumatic stress disorder (PTSD) in trauma exposed children and adolescents (Alisic et al., Citation2014). PTSD is diagnosed when, after experiencing a traumatic event, someone suffers from intrusion symptoms, avoidance of trauma-related internal or external stimuli, negative alterations in cognitions and mood, and heightened arousal for at least one month (American Psychiatric Association [APA], Citation2013). Current international treatment guidelines recommend trauma-focused cognitive–behavioural therapy (TF-CBT) or eye movement desensitization and reprocessing (EMDR) therapy for the treatment of PTSD in children and adolescents (National Institute for Health and Care Excellence, Citation2018). Without proper treatment, post-traumatic stress symptoms can prolong or worsen significantly over time, with the tendency to have negative impact on social, emotional, physical development and well-being (Fairbank & Fairbank, Citation2009; Yule, Citation2001). The prognosis for recovery after six months with PTSD without adequate treatment is poor (Gutermann et al., Citation2016; Hiller, M., Meiser-Stedman et al. Citation2016). Moreover, post-traumatic stress symptoms are often accompanied by other serious, long-term comorbidities, like depression or anxiety disorders (Copeland et al., Citation2007).
Relative to other traumatic events, children and adolescents who have been exposed to interpersonal trauma are more likely to develop PTSD (Alisic et al., Citation2014; Elklit & Christiansen, Citation2010; Tiihonen Möller, Bäckström, Söndergaard, & Helström, Citation2014). Kessler et al. (Citation2017) reviewed research on PTSD risk in adults, following traumatic events in 24 countries. They found that intimate partner or sexual violence had a high risk of developing PTSD (Kessler et al., Citation2017). Specifically in young people, a study from Bal, De Bourdeaudhuij, Crombez, and Van Oost (Citation2004) found that adolescent victims of sexual abuse suffer a variety of immediate and severe, negative consequences. In their sample of 100 adolescents aged 12–18 years old who were recruited shortly after disclosure of the abuse, 50% met the criteria of PTSD (DSM-IV). Moreover, another study of maltreated youths in shelter care, aged 8–17 years, showed that those who developed PTSD experienced a significantly greater duration of abuse and, more diagnostic comorbidity, than those who did not develop PTSD (Linning & Kearney, Citation2004). Furthermore, a meta-analysis on 80 studies about victims of sexual abuse showed that the average prevalence of sexual revictimization was 47.9% (Walker, Freud, Ellis, Fraine, & Wilson, Citation2019). Overall, this suggests that victims of sexual assault are at high risk of developing PTSD and the diagnosis PTSD appears to be a risk factor for revictimization.
PTSD symptoms are likely to decrease naturally over time, and they usually stabilize at 3 months post-assault (APA, Citation2013). A longitudinal study in adult victims of rape showed that 78% of the victims had an indication for PTSD one-month post-assault, but this incidence decreased to 67% at two months post-assault and to 41% at four months post-assault (Steenkamp, Dickstein, Salters-Pedneault, Hofmann, & Litz, Citation2012). Rothbaum, Foa, Riggs, Murdock, and Walsh (Citation1992) found similar results in a prospective study in female victims of rape, where 94% of the victims reported severe symptoms of post-traumatic stress at one week post assault, which decreased to 65% after one month and to 47% after three months without treatment (Rothbaum et al., Citation1992). Furthermore, a meta-analysis in children demonstrated that after a traumatic event, the percentage of children with PTSD, reduced by approximately 50% during the first 6 months post-trauma (Hiller, M., Meiser-Stedman et al., Citation2016). However, there is little knowledge to predict in which children PTSD symptoms are likely to decrease and in which children the symptoms are not likely to decrease.
Given that PTSD can be treated effectively (Cohen, Citation2010), it is important to screen and identify children at risk or suffering from PTSD and to offer them appropriate evidence-based and timely treatment, to prevent chronic problems and revictimization. Although research on predictors of PTSD after sexual assault in children is missing, several studies have investigated possible risk factors for the development of PTSD after other traumatic events in children, or after sexual assault in adults. In general, risk factors can be distinguished as pre-assault factors, assault-related factors, and post-trauma factors (Bicanic, Snetselaar, De Jongh, & Van de Putte, Citation2014; Brown, Du Mont, Macdonald, & Bainbridge, Citation2013; Elwood et al., Citation2011).
Regarding pre-assault factors in children who experienced other types of traumatic events, prior psychopathology and previous traumatic events were found to be risk factors for developing PTSD (Cohen, Citation2010; Pine & Cohen, Citation2002), as well as young age at time of exposure to traumatic events (Trickey, Siddaway, Meiser-Stedman, Serpell, & Field, Citation2012). Furthermore, a meta-analysis on risk factors for PTSD in adults found that factors such as education level, prior trauma exposure, and general adverse childhood events predicted PTSD more consistently than other factors such as gender, age at trauma, and race (Brewin, Andrews, & Valentine, Citation2000). However, this study also mentioned that the effect size of all risk factors was modest. Moreover, several factors have been found to put children at risk for a variety of psychopathology, such as parental divorce, living in residential care, and education level, (Rutter, Citation2006). Furthermore, Langley et al. (Citation2013) examined the development of PTSD in 195 children at 15 months after Hurricane Katrina and found that gender and prior trauma exposure significantly predicted PTSD (Langley et al., Citation2013).
Regarding the assault-related factors, factors such as perceived life threat and the severity of the traumatic experience are considered predictors of PTSD as well as post-traumatic stress symptoms and had somewhat larger effect sizes than factors prior to the trauma (Brewin et al., Citation2000). Furthermore, concerning post-trauma factors, pain was found to contribute to the development of PTSD in children and adolescents who were injured after traffic accidents (Hildenbrand, Marsac, Daly, Chute, & Kassam-Adams, Citation2016; Van Meijel et al., Citation2019). Panic symptoms following a traumatic experience are predictive of subsequent PTSD in children (Pfefferbaum, Stuber, Galea, & Fairbrother, Citation2006; Sinclair, Salmon, & Bryant, Citation2007). Additionally, acute stress reactions in the direct aftermath of traumatic events are a common psychological response but can also be seen as predictive for PTSD. A longitudinal study of more than 300 adult female victims of sexual assault found that the presence of acute stress disorder immediately after the assault was a strong risk factor for developing PTSD (Tiihonen Möller et al., Citation2014). Social support has found to be a major protective factor for the initial level of distress of children (Brewin et al., Citation2000; Langley et al., Citation2013; Ozer, Best, Lipsey, & Weiss, Citation2003; Scheeringa, Wright, Hunt, & Zeanah, Citation2006). In line with this finding, parental psychopathology – potentially impeding social support – is one of the most consistent risk factors of the development of PTSD (Alisic, Jongmans, Van Wesel, & Kleber, Citation2011; Trickey et al., Citation2012).
In sum, it is important to identify young victims at risk for developing PTSD to prevent chronic problems and revictimization. Prospective studies in recently abused children, however, are missing. Therefore, the first aim of the current study is to monitor the development of post-traumatic stress symptoms in a sample of young victims who experienced recent sexual assault and sought help from a Sexual Assault Centre. The second aim is to analyse which pre-assault factors, assault-related factors, and post-assault-related factors, measured at two weeks post-assault, are associated with a PTSD indication at four weeks post-assault. We hypothesize that the initial post-traumatic stress symptoms would decrease during the first four weeks post-assault. Furthermore, we hypothesize a significant association between the factors and PTSD indication.
2. Method
2.1. Participants
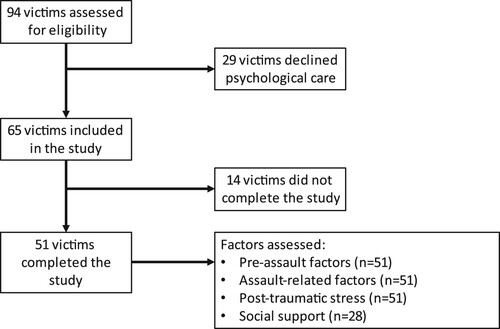
Victims who presented at a Dutch Sexual Assault Centre between January 2019 and March 2021, were screened for study participation. We defined sexual assault as ‘the use of physical or other force to obtain or attempt sexual penetration’ (WHO, Citation2017). In this period, a total of 1112 victims, both children and adults, sought help from the Sexual Assault Centre Brabant Oost, located at the Catharina Hospital. Victims were excluded from the present study if the sexual assault occurred more than seven days ago, if they were younger than 8 years old, or older than 17 years old. Ninety-four victims were included in the study.
2.2. Procedure
This study was designed as a prospective study that describes the development of post-traumatic stress symptoms in children aged 8 through 17 years, who experienced recent sexual assault. Currently, the Netherlands has 16 specialized Sexual Assault Centres, of which one Centre participated in this study. The centres integrate 24/7 medical, forensic, and psychological care for victims of recent sexual assault, within seven days. The participants of this study were referred to the Sexual Assault Centres by themselves, their direct environment, the police, medical practitioners, or other professionals like psychologists or social services.
The medical services of the Sexual Assault Centres aim to provide emergency medical care and treatment for injuries. Victims also receive medication to prevent pregnancy and the contraction of sexually transmitted diseases. The purpose of forensic services is to optimally perform the forensic examination for evidence collection. The standard psychological care offered by a case-manager aims at reducing initial distress by means of active monitoring of the post-traumatic stress symptoms during the first four weeks after the sexual assault (Bicanic et al., Citation2014). Active monitoring is also known as ‘watchful waiting’, where victims are provided with psychoeducation and emotional support and regularly screened for post-traumatic stress symptoms to see if further intervention is needed (National Institute for Health and Care Excellence, Citation2018). The victim is appointed to a case-manager of the Sexual Assault Centre who contacts the victim once in the first seven days post-assault. The follow-up takes place on the second- and fourth week post assault. During watchful waiting, information concerning pre-assault and assault-related factors, social support, and post-traumatic stress symptoms are routinely collected. Thus, this information relies on self-report. The study was performed in accordance with the precepts and regulations for research as stated in the Declaration of Helsinki and the Dutch Medical Research involving Humans Subjects Act (WMO) concerning scientific research. According to the Medical Ethical Committee of the Catharina Hospital Eindhoven, this act was not applicable to the present study (W18.173).
2.3. Measures
2.3.1. Pre-assault factors
Pre-assault factors included gender (female or male), age, learning disabilities (‘yes’ or ‘no’), family structure, (i.e. whether parents were divorced or not), and current living situation (i.e. whether they were living with their parent(s) or in residential care). It also included prior sexual assault (‘yes’ or ‘no’) and use of (prior) mental health services by the victim (‘yes’ or ‘no’). Use of (prior) mental health service was defined as any help that already existed before the sexual assault occurred or was still present while in care at the Sexual Assault Centre.
2.3.2. Assault-related factors
Assault-related factors included use of penetration (‘yes’ or ‘no’), physical violence (‘yes’ or ‘no’), use of alcohol and/or drugs by the victim prior to the assault (‘yes’ or ‘no’), multiple assailants (‘yes’ or ‘no’), and relationship to the assailant(s). The relationship to the assailant was defined as a stranger when the victim had never been in contact before. Otherwise, the relationship was defined as a familiar relationship. This included assailants who were family members, friends, acquaintances, as well as teachers and other authoritative figures.
2.3.3. Post-traumatic stress symptoms
The post-traumatic stress symptoms were assessed at two and four weeks post-assault using the Children's Revised Impact of Event Scale (CRIES-13) (Verlinden et al., Citation2014). The CRIES-13 is a brief, self-report questionnaire designed to screen children for symptoms of PTSD, according to the DSM-IV criteria. It consists of 13 items to assess symptoms of intrusion, avoidance, and arousal. Participants scored the occurrence of these symptoms related to the traumatic event during the past week as 0 (not at all), 1 (rarely), 3 (sometimes) or 5 (often). The total score indicates the severity of post-traumatic stress symptoms and ranges from 0 to 65. A cut-off score of 30 or higher on the total score is used to indicate PTSD at four weeks post-assault (Verlinden et al., Citation2014). The total score on the CRIES-13 questionnaire, assessed two weeks after the sexual assault, was used to measure the severity of early post-traumatic stress symptoms. The outcome variable of indication PTSD at four weeks was defined as yes (total score of 30 or higher) or no (total score below 30).
2.3.4. Social support
Social support was measured by two items from the Kidscreen-27 (Ravens-Sieberer et al., Citation2007). The first question concerned parental support: ‘To what extent have you felt supported by your parents’. The second question was about the support the victims received from their peers: ‘To what extent have you felt supported by your friends?’. Both items were scored at a 5-point Likert scale from zero (not at all) to 4 (very much). For each question separately, the score conducted at two weeks after the assault was used to indicate the level of support the victim felt in the aftermath of sexual assault.
2.4. Data analysis
To monitor the development of post-traumatic stress symptoms, the total scores on the CRIES-13 were assessed at two and four weeks post-assault.
To test whether there was a difference in the incidence or level of factors between the victims with and without indication of PTSD at four weeks post-assault, Chi-Square tests were used for categorical variables and Fisher’s exact test was used when the assumptions of the Chi-square test were not met (small numbers). T-tests (normally distributed), or Mann–Whitney tests (not normally distributed), were used to test a difference in continuous variables between both groups. A p-value < 0.05 was considered statistically significant. The study was originally designed to use a multivariate logistic regression analysis, with indication of PTSD as the dependent variable and the factors that were significantly related to PTSD as independent variables (pre-assault factors, assault-related factors, post-traumatic stress symptoms and social support). However, since only one significant association was found in the univariate analyses, the multivariate analysis was not executed.
3. Results
3.1. Attrition
Ninety-four victims were included in this study. Age ranged from 8 to 17 years, with a mean age of 14.70 years (SD = 1.85). Psychological care was provided to 65 victims, as 29 victims did not accept the offer of psychological care. The main reason given was that the victim was already in care of mental health services (n = 22). Of the 65 included victims, 51 completed the four weeks assessment. Their mean age was 15.00 years (SD = 1.78). The mean age of the 14 non-completers was 14.43 years (SD = 1.95). There was no significant difference between the completers and the non-completers in age (t(63) = 1.04, p = .301).
There was a significant difference between the completers and the non-completers in learning disabilities difficulties (p = .037 Fisher’s exact test) and prior mental health services (χ2 = 3.93, p = .048), in that non-completers were more likely to have learning difficulties and prior mental health services than completers. In the other pre-assault and assault-related characteristics, no differences were found between the completers and the non-completers ().
summarizes the pre-assault and assault-related factors of the sample. The study includes female victims only. Initially, six boys were referred at the centre, however, four of them did not accept psychological care and two of them were non-completers.
Table 1. Pre-assault and assault-related factors of victims who accepted psychological care (n = 65) and victims who completed psychological care four weeks post-assault (n = 51).
3.2. Development of post-traumatic stress symptoms
The post-traumatic stress symptoms were assessed at two and at four weeks post-assault. Of the 51 victims who received and completed psychological care, 42 victims (82.4%) showed severe post-traumatic stress symptoms at two weeks post-assault (i.e. had a CRIES-13 score of 30 or higher). At four weeks post-assault, thirty-six victims (70.6%) showed severe post-traumatic stress symptoms, i.e. had an indication of PTSD.
The average post-traumatic stress scores were 49.65 (SD = 12.25) at two weeks post-assault and 37.65 (SD = 12.40) at four weeks post-assault. Most of the victims (58.8%) showed a decline in post-traumatic stress symptoms between two and four weeks post-assault. Their average score decreased from 44.60 (SD = 11.91) at two weeks to 36.87 (SD = 13.25) at four weeks. However, 14 victims (27.4%) showed an increase in post-traumatic stress symptoms they experienced. These victims initially experienced an average score of 34.14 (SD = 12.10) at two weeks, which increased to 39.71 (SD = 12.96) at four weeks post assault. Finally, 7 victims (13.7%) showed the exact same score in post-traumatic stress symptoms at 2 weeks and at four weeks post-assault (M = 36.86, SD = 7.45).
3.3. Factors associated with PTSD
The associations between the independent variables and an indication for PTSD are presented in (continuous variables) and (categorical variables). Of all independent variables, a significant difference was found between levels of post-traumatic stress symptoms at two weeks and an indication for PTSD, (t(49) = −5.792; p < .0001), meaning that victims with an indication of PTSD at four weeks post-assault experienced higher levels of post-traumatic stress symptoms at two weeks post-assault. Other factors were not found to be related with PTSD indication. Since there was only one significant association found, no multivariate logistic regression analysis was executed.
Table 2. Difference between victims with indication PTSD and victims without indication PTSD in age and post-traumatic stress symptoms.
Table 3. Difference between victims with indication PTSD and victims without indication PTSD in pre-assault and assault-related factors.
Of the 51 victims who received psychological care, social support was assessed in 28 subjects. At four weeks post-assault, 21 of these victims had an indication for PTSD. No significant differences were found between the victims with indication of PTSD and victims without indication of PTSD in the degree to which they experienced support from parents or peers ().
Table 4. Comparison of victims with indication post-traumatic stress symptoms and victims without indication post-traumatic stress symptoms at four weeks post assault in the level of social support.
4. Discussion
This is the first prospective study in young victims, aged 8–17 years, who experienced recent sexual assault. The study described the development of post-traumatic stress symptoms of the victims in the four weeks post-assault, and analysed which factors, defined as pre-assault factors, assault-related factors, social support, and severity of initial post-traumatic stress symptoms, were associated with an indication of PTSD at four weeks post-assault. Our study showed that shortly after the sexual assault occurred, most of the young victims experienced severe post-traumatic stress symptoms. In line with our hypothesis, the initial level of post-traumatic stress decreased during the first four weeks post-assault. Furthermore, we found a significant difference between high levels of post-traumatic stress symptoms at two weeks post-assault and an indication for PTSD at four weeks post-assault. This means that in the current study, victims with higher levels of post-traumatic stress at two weeks post-assault were at risk of PTSD indication at four weeks post-assault. Other factors were not related to an indication of PTSD.
More than half of the victims in our study showed a decline in post-traumatic stress symptoms over time. This is in line with several other studies in adults that demonstrated that severe post-traumatic stress symptoms in the direct aftermath of sexual assault are likely to decrease naturally until three months post-assault (Hiller, M., Meiser-Stedman et al., Citation2016; Rothbaum et al., Citation1992; Steenkamp et al., Citation2012). Nonetheless, the decrease in symptoms in the present study could be the result of the psychological care offered by the Sexual Assault Centre. After sexual assault, watchful waiting was provided as psychological care (National Institute for Health and Care Excellence, Citation2018). Watchful waiting aims at reducing the initial distress by means of active monitoring during the first four weeks after the sexual assault (Bicanic et al., Citation2014). However, still more than two-thirds of the victims in our study showed a score of 30 or higher at four weeks post-assault, meaning that there was an indication of PTSD, and further assessment and treatment may be needed. This result suggests that watchful waiting is not sufficient for reducing the distress of many young victims. The psychological care of the Sexual Assault Centres may be improved or extended with early interventions and immediate evidence-based treatment for those victims and their families.
Yet, research on the effectiveness of early interventions in sexual assault victims are scare. A systematic review and meta-analysis of seven studies, that examined the efficacy of early interventions for PTSD within 3 months after sexual assault, suggested that early interventions can lead to durable effects on PTSD symptoms severity reduction (Oosterbaan, Covers, Bicanic, Huntjens, & De Jongh, Citation2019). However, a recent randomized controlled trial (RCT) on adult victims of rape, who sought help from a Sexual Assault Centre, studied the effectiveness of two sessions of EMDR therapy in comparison to watchful waiting. The results showed that early EMDR interventions were no more effective than watchful waiting in reducing post-traumatic stress symptoms (Covers et al., Citation2021). Roberts, Kitchiner, Kenardy, and Bisson (Citation2009) suggested that early psychological interventions should only be recommended for those who meet the threshold for a clinical diagnosis. Although their study focused on adults and on a variety of traumatic events and not specific sexual assault, their recommendation is in line with the findings of the present study, which showed that of all independent variables, only high levels of early post-traumatic stress symptoms were found to be associated with the development for PTSD. These findings underline the need for further research to reveal more information about the effectiveness of early interventions and immediate evidence-based treatment in young victims, especially for those victims who show high levels of post-traumatic stress symptoms shortly after sexual assault. Moreover, it is of note that the findings on high levels of post-traumatic stress symptoms may seem to resemble acute stress disorder (ASD), however ASD has been found to be lacking power for predicting PTSD (Tiihonen Möller et al., Citation2014), since many victims with PTSD do not initially meet the criteria for ASD (Brewin et al., Citation2000; Elklit & Brink, Citation2004; Kleim, Ehlers, & Glucksman, Citation2007).
In contrast to the hypothesis, all pre-assault, and assault-related factors, as well as social support, were not related to the development for PTSD in children who experienced sexual assault. Regarding pre-assault factors, our study included only female victims. Although the Dutch Sexual Assault Centres have noticed an increase in male referrals over the years (Covers, Teeuwen et al., Citation2021), male victims are still underrepresented. The main reason for underrepresentation is that male victims are less likely to disclose and seek help (De Graaf & Wijsen, Citation2017). In the present study, the male victims who were referred, did not accept psychological care or were non-completers. This means that more needs to be done to reach male victims and to provide them the professional help they need.
Furthermore, although a substantial number of victims in our study reported prior victimization and (prior) use of mental health services, including residential care, we found no association with these factors and the development for PTSD. This outcome is not in line with prior studies in acute assault victims that found these characteristics to be associated with an enhanced risk for PTSD onset (Bicanic et al., Citation2014; Brown et al., Citation2013; Elwood et al., Citation2011). A possible explanation for this finding may be that our sample was biased, since a substantial number of victims who were already in care or (residential) mental health services did not accept the offer of watchful waiting and were thus excluded from the study. Another explanation may be that in our sample, the presence of professional services possibly acted as a buffer for stress in the minor. Also, the findings on divorce showed that divorce had no influence on the development of PTSD. It is likely that the support of parents is more important on the development of PTSD than whether they are living apart or together.
Yet, we also found that a lack of parental support or peer support, did not contribute to the development of PTSD. This result contrasts with many studies that found that social support buffers the development of PTSD, and a negative social environment is an indicator for PTSD (Brewin et al., Citation2000; Ozer et al., Citation2003; Scheeringa et al., Citation2006). However, these prior studies did not measure the impact of support in the direct aftermath of sexual assault as was done in our study. Foremost, victims enter the Sexual Assault Centres are accompanied by a parent or other caregiver. The way in which the adults emotionally support the minor variers from extremely stressful to remarkably calm and supportive. Regarding assault-related factors, our study did not find any associations between assault-related factors and the development of PTSD. In their cognitive model of PTSD, Ehlers and Clark (Citation2020) suggest that negative appraisals, disjointed trauma memories, and unhelpful coping strategies maintain PTSD (Ehlers & Clark, Citation2000). Therefore, it may be that not the assault-related factor in itself, but rather the coping strategies after the assault are important for the development of PTSD.
There are some study limitations. First, all victims who participated in the current study sought help from the Sexual Assault Centre. Therefore, the participating victims could be characterized as a selective group, which limits generalization to those who do not seek help or seek help after more than 7 days post-assault. Second, the study measured the severity of post-traumatic stress at two and four weeks post-assault and if indicated, subsequent referral for evidence-based treatment was made. Therefore, no data is available about the further development or natural recovery of the post-traumatic stress symptoms in children after four weeks post-assault. Third, 29 of the 94 victims that were included in this study did not accept psychological care and could therefore not participate in this study. The main reason given for not accepting psychological care, was that mental health services were already available in 22 of these 29 victims (75.9%). This might suggest that the victims in this study were already at risk of psychopathology prior to the assault. This may also be demonstrated by the fact that according to our study, more than one-third of the victims reported prior victimization (35.3%) This vulnerability is in line with prior studies in acute assault victims (Brown et al., Citation2013; Elwood et al., Citation2011). Future research could explore the role of this vulnerability, including victims who experienced prior sexual assault and where mental health services were already involved, in the development of psychopathology after sexual assault. The fourth limitation was that social support was assessed in only 28 victims. For that reason, the findings for social support may be biased. The last limitation involves the use of the Children’s Revised Impact of Event Scale (CRIES-13) as instrument to assess the post-traumatic stress symptoms (Verlinden et al., Citation2014). Originally, the CRIES-13 was designed to screen children for symptoms of PTSD according to the DSM-IV criteria. However, the CRIES-13 contains items to assess symptoms of intrusion, avoidance, and arousal, and these scales are represented in both DSM-IV and DSM-5. Despite these limitations, this is the first study that prospectively describes the development for post-traumatic stress in young victims of recent sexual assault as well as risk factors for the development of PTSD.
In conclusion, the present study found that more than half of the children who experienced recent sexual assault and who received immediate care at the Sexual Assault Centre, showed a decline in post-traumatic stress symptoms. However, more than two-thirds of the children, had an indication for PTSD after four weeks. Furthermore, high levels of post-traumatic stress at two weeks post-assault were associated with the development of PTSD, whereas other pre-assault factors, assault-related factors, and social support were not. These findings underline the importance of early identification of those victims with severe post-traumatic stress, and the need for further treatment. Future research is needed to determine if the current psychological care for young victims of recent sexual assault could be improved with early interventions and immediate evidence-based treatment for children, to prevent chronic problems and revictimization.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available on request from the corresponding author, M.L. Pijpers. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
References
- Alisic, E., Jongmans, M. J., Van Wesel, F., & Kleber, R. J. (2011). Building child trauma theory from longitudinal studies: A meta-analysis. Clinical Psychology Review, 31(5), 736–747. doi:10.1016/j.cpr.2011.03.001
- Alisic, E., Zalta, A. K., Van Wesel, F., Larsen, S. E., Hafstad, G. S., Hassanpour, K., & Smid, G. E. (2014). Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: Meta-analysis. British Journal of Psychiatry, 204(5), 335–340. doi:10.1192/bjp.bp.113.131227
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
- Bal, S., De Bourdeaudhuij, I., Crombez, G., & Van Oost, P. (2004). Differences in trauma symptoms and family functioning in intra-and extrafamilial sexually abused adolescents. Journal of Interpersonal Violence, 19(1), 108–123. doi:10.1177/088620503259053
- Bicanic, I., Snetselaar, H., De Jongh, A., & Van de Putte, E. (2014). Victims’ use of professional services in a Dutch sexual assault centre. European Journal of Psychotraumatology, 5(1), 23645. doi:10.3402/ejpt.v5.23645
- Brewin, C. R., Andrews, B., & Valentine, J. D. (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766. doi:10.1037/0022-006x.68.5.748
- Brown, R., Du Mont, J., Macdonald, S., & Bainbridge, D. (2013). A comparative analysis of victims of sexual assault with and without mental health histories. Journal of Forensic Nursing, 9(2), 76–83. doi:10.1097/jfn.0b013e31828106df
- Cohen, J. A. (2010). Practice parameter for the assessment and treatment of children and adolescents with posttraumatic stress disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 49(4), 414–430. doi:10.1016/j.jaac.2009.12.020
- Copeland, W. E., Keeler, G., Angold, A., & Costello, E. J. (2007). Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry, 64(5), 577. doi:10.1001/archpsyc.64.5.577
- Covers, M. L. V., De Jongh, A., Huntjens, R. J. C., De Roos, C., van den Hout, M., & Bicanic, I. A. (2021). Early intervention with eye movement desensitization and reprocessing (EMDR) therapy to reduce the severity of post-traumatic stress symptoms in recent rape victims: A randomized controlled trial. European Journal of Psychotraumatology, 12(1). doi:10.1080/20008198.2021.1943188
- Covers, M. L. V., Teeuwen, J., & Bicanic, I. A. E. (2021). Male victims at a Dutch Sexual Assault Center: A comparison to female victims in characteristics and service use. Journal of Interpersonal Violence. doi:10.1177/08862605211015220
- De Graaf, H., & Wijsen, C. (2017). Seksuele gezondheid in Nederland 2017. https://www.rutgers.nl/sites/rutgersnl/files/PDF-Onderzoek/Seksuele_Gezondheid_in_NL_2017_23012018.Pdf.
- Ehlers, A., & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38(4), 319–345. doi:10.1016/s0005-7967(99)00123-0
- Elklit, A., & Brink, O. (2004). Acute stress disorder as a Predictor of post-traumatic stress disorder in physical assault victims. Journal of Interpersonal Violence, 19(6), 709–726. doi:10.1177/0886260504263872
- Elklit, A., & Christiansen, D. M. (2010). ASD and PTSD in rape victims. Journal of Interpersonal Violence, 25(8), 1470–1488.
- Elwood, L. S., Smith, D. W., Resnick, H. S., Gudmundsdottir, B., Amstadter, A. B., Hanson, R. F., … Kilpatrick, D. G. (2011). Predictors of rape: Findings from the national survey of adolescents. Journal of Traumatic Stress, 24(2), 166–173. doi:10.1002/jts.20624
- Fairbank, J. A., & Fairbank, D. W. (2009). Epidemiology of child traumatic stress. Current Psychiatry Reports, 11(4), 289–295. doi:10.1007/s11920-009-0042-9
- Gutermann, J., Schreiber, F., Matulis, S., Schwartzkopff, L., Deppe, J., & Steil, R. (2016). Psychological treatments for symptoms of posttraumatic stress disorder in children, adolescents, and young adults: A meta-analysis. Clinical Child and Family Psychology Review, 19(2), 77–93. doi:10.1007/s10567-016-0202-5
- Hildenbrand, A. K., Marsac, M. L., Daly, B. P., Chute, D., & Kassam-Adams, N. (2016). Acute pain and posttraumatic stress after pediatric injury. Journal of Pediatric Psychology, 41(1), 98–107. doi:10.1093/jpepsy/jsv026
- Hiller, R. M., Meiser-Stedman, R., Fearon, P., Lobo, S., McKinnon, A., Fraser, A., & Halligan, S. L. (2016). Research review: changes in the prevalence and symptom severity of child post-traumatic stress disorder in the year following trauma - a meta-analytic study. Journal of Child Psychology and Psychiatry, 57(8), 884–898. doi:10.1111/jcpp.12566
- Kessler, R. C., Aguilar-Gaxiola, S., Alonso, J., Benjet, C., Bromet, E. J., Cardoso, G., … Koenen, K. C. (2017). Trauma and PTSD in the WHO world mental health surveys. European Journal of Psychotraumatology, 8(Suppl 5), 1353383. doi:10.1080/20008198.2017.1353383
- Kleim, B., Ehlers, A., & Glucksman, E. (2007). Early predictors of chronic post-traumatic stress disorder in assault survivors. Psychological Medicine, 37(10), 1457–1467. doi:10.1017/s0033291707001006
- Langley, A. K., Cohen, J. A., Mannarino, A. P., Jaycox, L. H., Schonlau, M., Scott, M., … Gegenheimer, K. L. (2013). Trauma exposure and mental health problems among school children 15 months post-Hurricane Katrina. Journal of Child & Adolescent Trauma, 6(3), 143–156. doi:10.1080/19361521.2013.812171
- Linning, L. M., & Kearney, C. A. (2004). Post-traumatic stress disorder in maltreated youth. Journal of Interpersonal Violence, 19(10), 1087–1101. doi:10.1177/0886260504269097
- National Institute for Health and Care Excellence. (2018). Post-traumatic stress disorder: Evidence reviews on care pathways for adults, children, and young people with PTSD (NICE Guideline Standard No. NG 116. Retrieved from https://www.nice.org.uk/guidance/ng116. [Google Scholar].
- Oosterbaan, V., Covers, M. L. V., Bicanic, I. A. E., Huntjens, R. J. C., & De Jongh, A. (2019). Do early interventions prevent PTSD? A systematic review and meta-analysis of the safety and efficacy of early interventions after sexual assault. European Journal of Psychotraumatology, 10(1), 1682932. doi:10.1080/20008198.2019/1682932
- Ozer, E. J., Best, S. R., Lipsey, T. L., & Weiss, D. S. (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129(1), 52–73. doi:10.1037/0033-2909.129.1.52
- Pfefferbaum, B., Stuber, J., Galea, S., & Fairbrother, G. (2006). Panic reactions to terrorist attacks and probable posttraumatic stress disorder in adolescents. Journal of Traumatic Stress, 19(2), 217–228. doi:10.1002/jts.20118
- Pine, D. S., & Cohen, J. A. (2002). Trauma in children and adolescents: Risk and treatment of psychiatric sequelae. Biological Psychiatry, 51(7), 519–531. doi:10.1016/s0006-3223(01)01352-x
- Ravens-Sieberer, U., Auquier, P., Erhart, M., Gosch, A., Rajmil, L., Bruil, J., … Kilroe, J. (2007). The KIDSCREEN-27 quality of life measure for children and adolescents: Psychometric results from a cross-cultural survey in 13 European countries. Quality of Life Research, 16(8), 1347–1356. doi:10.1007/s11136-007-9240-2
- Roberts, N. P., Kitchiner, N. J., Kenardy, J., & Bisson, J. I. (2009). Multiple session early psychological interventions for the prevention of post-traumatic stress disorder. Cochrane Database of Systematic Reviews. doi:10.1002/14651858.cd006869.pub2
- Rothbaum, B. O., Foa, E. B., Riggs, D. S., Murdock, T., & Walsh, W. (1992). A prospective examination of post-traumatic stress disorder in rape victims. Journal of Traumatic Stress, 5(3), 455–475. doi:10.1002/jts.2490050309
- Rutter, M. (2006). Genes and Behavior. Nature-nurture interplay explained. Oxford, UK: Blackwell.
- Scheeringa, M. S., Wright, M. J., Hunt, J. P., & Zeanah, C. H. (2006). Factors affecting the diagnosis and prediction of PTSD symptomatology in children and adolescents. American Journal of Psychiatry, 163(4), 644–651. doi:10.1176/ajp.2006.163.4.644
- Sinclair, E., Salmon, K., & Bryant, R. A. (2007). The role of panic attacks in acute stress disorder in children. Journal of Traumatic Stress, 20(6), 1069–1073. doi:10.1002/jts.20272
- Steenkamp, M. M., Dickstein, B. D., Salters-Pedneault, K., Hofmann, S. G., & Litz, B. T. (2012). Trajectories of PTSD symptoms following sexual assault: Is resilience the modal outcome? Journal of Traumatic Stress, 25(4), 469–474.
- Tiihonen Möller, A., Bäckström, T., Söndergaard, H. P., & Helström, L. (2014). Identifying risk factors for PTSD in women seeking medical help after rape. PLoS ONE, 9(10), e111136. doi:10.1371/journal.pone.0111136
- Trickey, D., Siddaway, A. P., Meiser-Stedman, R., Serpell, L., & Field, A. P. (2012). A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review, 32(2), 122–138. doi:10.1016/j.cpr.2011.12.001
- Van Meijel, E. P. M., Gigengack, M. R., Verlinden, E., Van der Steeg, A. F. W., Goslings, J. C., Bloemers, F. W., … Lindauer, R. J. L. (2019). Long-term posttraumatic stress following accidental injury in children and adolescents: Results of a 2–4-year follow-up study. Journal of Clinical Psychology in Medical Settings, 26(4), 597–607. doi:10.1007/s10880-019-09615-5
- Verlinden, E., Van Meijel, E. P. M., Opmeer, B. C., Beer, R., De Roos, C., Bicanic, I. A. E., … Lindauer, R. J. L. (2014). Characteristics of the Children’s Revised Impact of Event Scale in a clinically referred Dutch sample. Journal of Traumatic Stress, 27(3), 338–344. doi:10.1002/jts.21910
- Walker, H. E., Freud, J. S., Ellis, R. A., Fraine, S. M., & Wilson, L. C. (2019). The prevalence of sexual revictimization: A meta-analytic review. Trauma, Violence, & Abuse, 20(1), 67–80. doi:10.1177/1524838017692364
- World Health Organization. (2017). Responding to children and adolescents who have been sexually abused. WHO clinical guidelines. Geneva: World Health Organization. Retrieved from http://www.who.int/reproductivehealth/publications/violence/clinical-response-csa/en/. [Google Scholar].
- Yule, W. (2001). Post-traumatic stress disorder in children and adolescents. International Review of Psychiatry, 13(3), 194–200. doi:10.1080/09540260120074064