ABSTRACT
Background: Trauma-affected refugee patients benefit from psychological treatment to different degrees. Only a handful of studies has investigated potential predictors of treatment outcome that could throw light on the great variability in outcomes reported for this group. Such knowledge may be vital to better tailor prevention and treatment efforts to the needs of different individuals and subgroups among these patients.
Objective: In a naturalistic and longitudinal study, the aim was to analyse demographics and traumatic exposure as potential predictors of the participants’ long-term trajectories of mental health symptoms and quality of life.
Method: A group of 54 multi-origin adult refugee patients with complex traumatic exposure, such as armed conflicts, persecution, torture, and childhood adversities, were interviewed face to face over up to 10 years; at therapy admittance, and at varying points in time during and after psychotherapy. Checklists of war-related and childhood trauma, mental health symptoms, and quality of life were included in the interviews. In linear mixed effects analyses, interaction was analysed with potential predictors included separately because of the sample size. Time was modelled as continuous from inclusion into the study.
Results: Gender predicted the course of symptoms of post-traumatic stress, anxiety, and depression, and of quality of life in physical health and social relationships. Childhood family violence and experiences of torture predicted the course of depression, whereas the extent of exposure to war-related trauma events and having experienced torture predicted the course of anxiety.
Conclusions: The results indicated greater chronicity in male refugees, in refugees who had experienced domestic violence during childhood, in refugees who had experienced torture, and in refugees with more numerous types of potentially traumatic war-related experiences. The findings highlight the need for gender-sensitive research, rehabilitative efforts, and treatment.
HIGHLIGHTS
In a 10 year longitudinal and naturalistic therapy follow-up study of traumatized refugees, female gender, childhood trauma, war trauma, and torture predicted mental health and quality of life outcomes.
Male participants responded less than females to therapy.
Antecedentes: Los pacientes refugiados afectados por el trauma se benefician del tratamiento psicológico en diferentes grados. Sólo un puñado de estudios han investigado los posibles predictores del resultado del tratamiento que podrían arrojar luz sobre la gran variabilidad de los resultados registrados en este grupo. Este conocimiento puede ser vital para adaptar mejor los esfuerzos de prevención y tratamiento a las necesidades de los diferentes individuos y subgrupos de estos pacientes.
Objetivo: En un estudio naturalista y longitudinal, el objetivo fue analizar los datos demográficos y la exposición traumática como posibles predictores de las trayectorias a largo plazo de los síntomas de salud mental y la calidad de vida de los participantes.
Método: Un grupo de 54 pacientes adultos refugiados de múltiples orígenes con exposición traumática compleja, como conflictos armados, persecución, tortura y adversidades en la infancia, fueron entrevistados cara a cara durante un período de hasta 10 años; al ingreso en la terapia, y en diferentes momentos durante y después de la psicoterapia. En las entrevistas se incluyeron listas de comprobación de traumas relacionados con la guerra y la infancia, síntomas de salud mental y calidad de vida. En los análisis lineales de efectos mixtos, se analizó la interacción con los posibles predictores incluidos por separado debido al tamaño de la muestra. El tiempo se modeló como continuo desde la inclusión en el estudio.
Resultados: El género predijo la evolución de los síntomas de estrés postraumático, ansiedad y depresión, y de la calidad de vida en cuanto a salud física y relaciones sociales. La violencia familiar en la infancia y las experiencias de tortura predijeron el curso de la depresión, mientras que el grado de exposición a eventos traumáticos relacionados con la guerra y el haber experimentado la tortura predijeron el curso de la ansiedad.
Conclusiones: Los resultados indicaron una mayor cronicidad en los refugiados varones, en los refugiados que habían sufrido violencia doméstica durante la infancia, en los refugiados que habían sufrido tortura y en los refugiados con más tipos de experiencias potencialmente traumáticas relacionadas con la guerra. Los resultados ponen de manifiesto la necesidad de realizar investigaciones, esfuerzos de rehabilitación y tratamientos que tengan en cuenta el género.
背景:受创伤影响的难民患者在不同程度上受益于心理治疗。只有少数研究考查了可以揭示该群体报告结果巨大差异的治疗结果潜在预测因素。这些知识对于更好地根据这些患者中不同个体和亚群需求调整预防和治疗工作可能至关重要。
目的:在一项自然主义和纵向研究中,旨在分析人口统计学和创伤暴露作为参与者心理健康症状和生活质量长期轨迹的潜在预测因素。
方法:对 一个54 名经历了武装冲突、迫害、酷刑和童年期逆境等复杂性创伤的多来源成年难民患者群体进行长达 10 年的面对面访谈;在接受治疗时,以及在心理治疗期间和之后的不同时间点。采访中包括了战争相关和童年期创伤、心理健康症状和生活质量的检查表。在线性混合效应分析中,由于样本量原因,分析了单独纳入潜在预测因素的交互作用。时间从纳入研究开始被建模为连续变量。
结果:性别预测创伤后应激、焦虑和抑郁症状病程,以及身体健康和社会关系中的生活质量。童年期家庭暴力和酷刑经历预测了抑郁病程,而暴露于战争相关创伤事件和经历酷刑程度预测了焦虑病程。
结论:结果表明,男性难民、童年期遭受家庭暴力的难民、遭受酷刑的难民以及有更多类型潜在创伤性战争相关经历的难民具有更高的持续性。研究结果强调了对性别敏感的研究、康复工作和治疗的必要性。
1. Introduction
Trauma-affected refugees benefit from therapy to individually varying degrees, yet few studies have investigated potential predictors of treatment outcome (Sonne, Mortensen, Silove, Palic, & Carlsson, Citation2021). It is vital to untangle the factors underlying individual differences in response to treatment are vital, as differential preventive and therapeutic approaches may be needed for subgroups of trauma-affected refugees. In this study of potential predictors of long-term mental health and quality of life (QoL) outcomes, we will focus on selected pretreatment variables: demographics (gender, age, education, length of stay in the host country, host country language competence, and employment) and trauma exposure (childhood adversities and trauma related to war and human rights abuses).
There are increasing numbers of refugees in the world, many of whom resettle in countries that are distant in terms of geography, language, and culture (UNHCR, Citation2021). Many refugees have suffered severe traumatic events in their countries of origin or during flight, and carry with them great losses and horrific experiences (Kingsley, Citation2016). Thus, newly arrived refugees generally have a high level of mental health symptoms (Hassan, Ventevogel, Jefee-Bahloul, Barkil-Oteo, & Kirmayer, Citation2016; Walther, Fuchs, Schupp, & von Scheve, Citation2020). Accommodating to new living conditions and vocational requirements, perhaps after little or no schooling, takes considerable resources. Challenges in the host country, such as learning to navigate in a new society, and postmigration difficulties, such as marginalization, discrimination, and worries about family members left behind, may complicate the integration process and add to their psychological burden (Bruhn, Rees, Mohsin, Silove, & Carlsson, Citation2018; Li, Liddell, & Nickerson, Citation2016). In a systematic review encompassing 5143 adult refugees and asylum seekers in 26 studies across 15 countries, the prevalence of post-traumatic stress disorder (PTSD) was found to be 31.5%, depression 31.5%, anxiety 11%, and psychosis 1.5% (Blackmore et al., Citation2020). In this review, the prevalence of anxiety was higher for those with shorter stay (< 4 years), but longer stay in the host country was not significantly associated with decreases in symptoms of PTSD or depression. The authors therefore concluded that PTSD and depression seem to persevere for many years after displacement. In view of the reported prevalences of mental health disorders, it is particularly worrying that access to healthcare services for refugees and other migrants has been found to be fragmented or unavailable in European countries, owing to linguistic, cultural, or administrative barriers (Riza et al., Citation2020).
1.1. Predictors of treatment outcome
In general clinical populations, the initial severity of functional impairment, problem or symptom chronicity, and lower socio-economic status have been found to predict poorer psychotherapy outcome (Lutz, de Jong, Rubel, & Delgadillo, Citation2021). The factors influencing the process and outcome of psychotherapy are complex, entailing the interaction between patient, therapist, and extratherapeutic factors in the context of treatment type and setting (Lutz et al., Citation2021, p. 252). A literature search for studies, published during the last 10 years, of predictors of treatment/therapy outcome for adult refugees settled in high-income countries, indicated that studies of predictors of treatment outcome among trauma-affected refugee clients are few. Several of the studies are from the same institutions, by the same authors. Studies comprising predictors that are included in the present study are presented in . The time span from baseline to the last follow-up ranged from about 5 to 39 months.
Table 1. Literature findings regarding pretreatment demographics and trauma load as predictors of treatment outcome in clinical groups of adult refugees.
Studies of age and gender as predictors of treatment outcome in clinical groups of refugees have yielded mixed results (Buhmann, Mortensen, Nordentoft, Ryberg, & Ekstrøm, Citation2015; Nordin & Perrin, Citation2019; Sonne et al., Citation2021; Stammel et al., Citation2017; Stenmark, Guzey, Elbert, & Holen, Citation2014; van Wyk, Schweitzer, Brough, Vromans, & Murray, Citation2012). Two studies found that gender significantly predicted treatment outcome (Buhmann, Nordentoft, Ekstroem, Carlsson, & Mortensen, Citation2018; Stenmark et al., Citation2014), while gender did not significantly predict outcome in five other studies (). Younger age was associated with greater improvements in both PTSD and depression (Sonne et al., Citation2021), and in somatoform symptoms (Stammel et al., Citation2017), and older age with a small negative effect on PTSD (Nordin & Perrin, Citation2019). In five other studies, age was not found to significantly predict any outcome variables (). In their discussion, Sonne et al. (Citation2021) suggested that older age and longer time in the host country (see below) may indicate symptom chronicity. Higher levels of education correlated significantly and negatively with improvement in anxiety and depression, and also negatively, but not significantly, with improvement of PTSD (Sonne, Carlsson, Bech, Vindbjerg, et al., Citation2016), but in four other studies were not found to be significantly related to outcome (). According to Sonne, Carlsson, Bech, Vindbjerg, et al. (Citation2016), a negative effect of education has been found in two other refugee studies, and also in a study of non-refugee PTSD patients, for reasons yet to be understood. Next, length of time in the host country was found to be significantly and negatively related to symptom improvement in PTSD (Sonne et al., Citation2021), and with unspecified change(s) in another study (Sander, Laugesen, Skammeritz, Mortensen, & Carlsson, Citation2019). In two other studies, length of stay was not significantly associated with outcomes (). We find that competence in the language of the host country language may have implications for health literacy, help seeking, participation in work and community life, and a general feeling of security and well-being. Interpreter use is included here as an indication of poor or lacking host country language skills. Interpreter use was, in one study, found to significantly predict poorer treatment outcomes in PTSD, anxiety, depression, and several other outcome variables (Sander et al., Citation2019), while interpreter use was not found to be a significant predictor of outcome in two other studies (Buhmann et al., Citation2015; Haagen, ter Heide, Mooren, Knipscheer, & Kleber, Citation2017). Employment was found to be a significant predictor of outcome in all three studies where it was examined (Buhmann et al., Citation2015; Sonne, Carlsson, Bech, Vindbjerg et al., Citation2016; Sonne et al., Citation2021).
Many of the studies reported in have a high proportion of participants who have experienced torture. Having been subjected to torture, and the magnitude of exposure to other potentially traumatic experiences (PTEs) related to mass conflict and persecution, have repeatedly been found to be associated with poorer mental health in refugee populations (e.g. Song, Subica, Kaplan, Tol, & de Jong, Citation2018; Steel et al., Citation2009). However, only one of the included studies reported that less exposure to traumatic events (assumed by the authors from status as family reunified in contrast to refugee status) was significantly associated with symptom improvement in PTSD after treatment (Sonne et al., Citation2021). Moreover, contrary to what may be expected, in six of the other studies, the number and kind of traumatic experiences were not found to significantly predict treatment outcome (). Possible reasons may be that there was little variance in trauma exposure among participants in these studies, or that traumatic experiences were well addressed in the therapies, and thus did not affect treatment outcome negatively.
Other predictors studied in one or more of the articles will be mentioned briefly here, but will not be further discussed. Improvement in one or more outcome variables was found to be predicted by higher PTSD, anxiety and depression symptom scores, and a higher level of functioning at baseline (Buhmann et al., Citation2018; Sonne et al., Citation2021), having obtained refugee status in the course of treatment (Drožđek et al., Citation2013), by personality functioning, characterized by reality-oriented perception (Opaas, Hartmann, Wentzel-Larsen, & Varvin, Citation2016), and by patients from Afghanistan, although they were also younger, had lived for a shorter time in Denmark, had more education, and had less need for an interpreter than the other participants (Buhmann et al., Citation2018). Predictors of poorer outcome included self-report of having been a violent offender, and intensity of pretreatment anger and depression (Stenmark et al., Citation2014); higher preintervention PTSD, anxiety, and somatization scores (van Wyk et al., Citation2012); more severe pre-treatment depression and a diagnosis of major depressive disorder (Haagen et al., Citation2017); postmigration living difficulties (Buhmann et al., Citation2018; Schick et al., Citation2018); disability (Friis Jørgensen, Auning-Hansen, Ottesen Kennair, & Elklit, Citation2017); pain in the arms (Buhmann et al., Citation2015; Nordin & Perrin, Citation2019); pain, low scores on upbringing, limited cognitive resources, few social relationships, poor integration, previously having received psychiatric treatment without effect, and poor acceptability of psychotherapy (Sonne, Carlsson, Bech, Vindbjerg, et al., Citation2016), and being Muslim (Buhmann et al., Citation2018). Furthermore, none of the following variables, in any of the included studies, was found to significantly predict outcome: refugee status, postmigration living difficulties, and number of service consultations (van Wyk et al., Citation2012); severity of baseline symptoms of PTSD, anxiety, and depression (Buhmann et al., Citation2015); refugee status, pretreatment PTSD severity, number of psychotherapy sessions, and treatment dropout (Haagen et al., Citation2017); and country of origin (Stammel et al., Citation2017).
As can be seen from the summary of the research presented above, there are varied yet few consistent findings regarding predictors of mental health treatment outcome for traumatized refugees. Despite some common characteristics between individuals, great individual variation in other characteristics may account for the differing findings. And, as noted previously, once psychotherapy has started, the reciprocal process between patient and therapist may moderate the importance of common categories such as gender, age, ethnicity/minority status, and other demographic characteristics (Lutz et al., Citation2021).
Although it will not apply to all results, we suggest that one way to sum up various findings regarding predictors of treatment outcome may be to gather variables that predict a positive outcome (such as employment, exile language competence, a higher global level of functioning, and reality-oriented perception) under the heading ‘agency/opportunities to actively influence one’s life’, and factors associated with poorer outcome (such as chronic depression, disability, chronic pain, limited cognitive resources, education/competence that cannot be used or is not acknowledged in exile, exile language problems, longer time in the host country without the wanted progress, previous unsuccessful psychiatric treatment, and few social relationships) under the heading ‘passivity/lack of possibility to actively influence one’s life’.
Thus, to our knowledge, research has only just started to elucidate factors contributing to the highly variable, and sometimes discouraging, effects of treatment among refugees with trauma-related mental health problems. Researchers in the refugee field have called for longitudinal studies to identify variables with implications for long-term mental health, QoL, and exile life functioning (e.g. Giacco & Priebe, Citation2018). Such knowledge is vital to better tailor interventions for those who do not seem to benefit from existing treatment efforts. The present study, with its very long follow-up period, will contribute towards filling a knowledge gap regarding pretreatment variables that may predict long-term outcome after having received psychotherapy. Along these lines, we aimed to examine the following variables, measured at baseline, as potential predictors of long-term outcome in symptoms of post-traumatic stress, anxiety, and depression, and in four aspects of QoL (physical health, psychological health, social relationships, and environmental conditions) among trauma-affected refugee patients: (1) demographics: gender, age, education from country of origin, length of stay in the host country, employment, and host country language proficiency, and (2) exposure to PTEs: war-related trauma, torture, and rape, and childhood trauma within and outside the family.
2. Method
2.1. Background to the study
This naturalistic and longitudinal study followed 54 trauma-affected refugee patients with repeated face-to-face interviews and assessments for up to 10 years after their entry to psychological treatment in specialist-level mental health outpatient services for the adult population in the Oslo region, Norway. Previous publications can be referred to for baseline results, 3 year follow-up, 6.5 year follow-up for a subgroup of 22, and 10 year trajectories of the participants’ mental health, quality of life, personality, and exile life functioning (Opaas et al., Citation2016; Opaas & Hartmann, Citation2013, Citation2021; Opaas & Varvin, Citation2015; Opaas, Wentzel-Larsen, & Varvin, Citation2020). At the 3 year follow-up, including almost all of the participants, and where time-points were fixed (at treatment start, after 1 year, and after 3 years), effect sizes of symptoms and QoL changes were large to medium. The present study was built on the 10 year follow-up study that was completed after data collection was terminated in 2017 (Opaas et al., Citation2020). The analysis included all assessments performed with the 54 participants during the data collection period, obtained at individually different intervals, over different lengths of time, and varying among the participants from once to seven times over the years. The mean number of assessment points in time with each individual was 3.7 (the first time-point included five to seven interview meetings, and at later time-points one to three meetings). In the 10 year study, the linearly modelled analyses demonstrated significant improvements of small effect sizes in anxiety, depression, and PTSD, and in the QoL domain Environmental Conditions, and of medium effect sizes in the QoL domains Psychological Health and Physical Health. For comparison, regarding the smaller effect size of improvement found across 10 years, relative to the 3 year follow-up, a decline in outcome was also found after 5 years in a 7 year follow-up after treatment of Iranian and Afghan patients with PTSD in the Netherlands (Drožđek, Kamperman, Tol, Knipscheer, & Kleber, Citation2014). Since the modelled linear trajectories of changes in mental health and QoL in the 2020 study (Opaas et al., Citation2020) contained great individual variation, we aspire to learn more about their possible contributory factors in the present study.
2.2. Participants
Participants were 35 male and 19 female adult mental health patients newly admitted to therapy, with a refugee background from 15 different countries in Asia, Europe, and Africa. Participants with Iraqi background constituted the largest group (31.5%, n = 17) . See for details. Although the mean stay in Norway was 10.5 years at T1/baseline, only half of the participants could communicate in Norwegian during the research interviews. Of the 12 participants who held employment at T1, all were on sick leave. Of the 54 participants, 40.7% (n = 22) had previously attended mental health treatment, but this had usually been of short duration. In addition to the many different war-related PTEs (range 5–30) suffered before or during flight, 92% of the participants had suffered childhood adversities such as domestic violence, violence external to the home, sudden losses of caregivers or siblings, or severe illness. For further details of experienced war-related and childhood trauma, we refer to Opaas & Varvin (Citation2015).
Table 2. Demographics, traumatic experiences, mental health, and quality of life at T1.
2.3. Procedures
Participants were recruited consecutively from specialist mental health services in the Oslo area, Norway, during the years 2006–2009. Inclusion criteria were: refugee background, age 18 years or more, and currently referred and admitted to psychological treatment owing to a mental health disorder related to having experienced traumatic events before or during flight. Exclusion criteria were: psychosis or substance abuse, if severe enough to hinder assessment. A PTSD diagnosis was not required. The Norwegian South-East Regional Committee for Medical and Health Research Ethics approved the study (20911 S-06195). Participation was voluntary. Of the 72 patients who were asked to take part in the study, 54 gave their written, informed consent (75% inclusion). There were no systematic differences in terms of gender or country of origin between those who consented and those who did not. The participants consented at first for 3 years; after 3 years, 74.1% of the participants consented to taking part in the study for additional years. However, participants were free to withdraw from the study at any time. Almost all patients (51 of 54) contributed to the study for 3 years, after which time participants dropped out of the study little by little.
All qualitative interviews and quantitative assessments were performed one to one, by the same two researchers over the years – one specialist in clinical psychology and one psychoanalyst/specialist in psychiatry. An interpreter assisted when needed. The first round of interviews and assessments at T1 took five to seven meetings to complete. Assessments after 1 year (T2), after 3 years (T3), and then more irregularly every second or third year, each consisted of one to three meetings with each participant. Depending on the participant’s endurance, not all questionnaires were completed each time. Care was taken, as far as possible, to make the interviews a good experience for the participants. They could reach both researchers by telephone after the interviews for questions or support. The participants took part in the study from 1 to 10.9 years (M = 5.2 years, SD = 2.7), usually dropping out gradually some months or years after therapy termination.
2.4. Therapy
Therapies were performed independent of the research project and varied in length, were not part of a special programme for refugees, were not manualized, and were performed by therapists with different theoretical orientations. However, therapies were often relational in orientation, psychodynamic or eclectic, and adapted to the patient’s needs and to the frames of the treatment setting. All treatments addressed the participants’ traumatic experiences to a greater or lesser extent, as well as their current situation. The therapies were performed mainly by specialists in clinical psychology, some by specialists in psychiatry, and a few by clinical social workers and nurses with therapy training. The therapies lasted from a few weeks to more than 6 years, with a mean of 61.3 sessions (SD = 74.5) over a mean of 3.4 years (SD = 3.1). See Opaas et al. (Citation2020).
2.5. Clinically assessed diagnoses
The official diagnostic system used in the Norwegian healthcare system is the International Classification of Mental and Behavioural Disorders, 10th Revision (ICD-10) (World Health Organisation, Citation1994). The diagnostic evaluation by the clinical units evidenced considerable comorbidity among the participants. The participants were each given a mean of 2.2 (SD = 0.9) diagnoses: 63% (n = 34) were diagnosed with PTSD (F43.1); 22.2% (n = 12) with enduring personality change after catastrophic experience (F62.0) – a proxy for complex PTSD; 14.8% (n = 8) with adjustment disorders (F43); 68.5% (n = 37) with a depression disorder (F32, F33, F34); 18.5% (n = 10) with an anxiety disorder (F40.1, F41.0, F41.1, F41.2); 11.1% (n = 6) with a dissociative disorder (F44); 13.0% (n = 7) with a somatoform diagnosis (F45); 7.4% (n = 4) with a personality disorder (F60); and 5.6% (n = 3) with psychotic features or a psychotic disorder (F32.3, F23, F29).
2.6. Instruments
2.6.1. Potentially traumatic childhood experiences
In Opaas and Varvin’s (Citation2015) study, 25 different kinds of adverse and potentially traumatic events experienced before the age of 18 years were extracted from the qualitative interviews with this particular group of refugee patients, and categorized into four subcategories. Here, we used only the two categories that were found to be associated with mental health and QoL among the participants at the 3 year follow-up: Childhood Family Violence (three items, scoring range 0–3), consisting of a parent’s violence towards his spouse, and towards the participant as a child, or his or her siblings, and parent’s drug or alcohol abuse during the participant’s upbringing; and Childhood External Violence (seven items, scoring range 0–7), consisting of childhood experiences of warfare, witnessing someone being killed, participant having been persecuted, imprisoned, or taken captive as a minor, and enrolment as a child soldier in military service or armed resistance.
2.6.2. Harvard Trauma Questionnaire
The Harvard Trauma Questionnaire (HTQ) (Mollica, McDonald, Massagli, & Silove, Citation2004) Part I (HTQ Trauma Events) is a checklist of PTEs related to war, persecution, and human rights violations (HRVs), such as armed attacks and other life-threatening dangers, lack of food and shelter, killings of loved ones, combat, persecution, captivity, imprisonment, sexual assault and harassment, and torture. The checklist consists of 37 different types of experiences. HTQ Part IV is a checklist of symptoms of PTSD, consisting of 16 items according to the criteria for PTSD in the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) (American Psychiatric Association, Citation1994), which was the edition in use when the study started. Each item is scored from 1 (not at all) to 4 (extremely). The clinical cut-off is ≥ 2.5. The mean of all 16 items (PTSD Total), and the means of the three symptom clusters; PTSD Reexperiencing (questions 1, 2, 3, and 16), PTSD Arousal (questions 6, 7, 8, 9, and 10), and PTSD Avoidance (questions 4, 5, 11, 12, 13, 14, and 15), were computed.
2.6.3. Hopkins Symptom Checklist-25
Hopkins Symptom Checklist-25 (HSCL-25) (Mollica et al., Citation2004) consists of 10 items tapping anxiety (non-specific) and 15 items tapping symptoms of Major Depression. Each item is scored from 1 (not at all) to 4 (extremely). The clinical cut-off is > 1.75.
2.6.4. WHO Quality of Life BREF
The World Health Organization Quality of Life BREF (WHOQOL-BREF) (Skevington, Lotfy, & O'Connell, Citation2004; WHOQOL Group, Citation1998) consists of 26 items organized into Domain 1, Physical Health (seven items); Domain 2, Psychological Health (six items); Domain 3, Social Relationships (three items); and Domain 4, Environmental Conditions (eight items). Each item is scored on a Likert scale from 1 (not at all/very dissatisfied/disagree strongly) to 5 (completely/very satisfied/agree strongly). Following the most commonly used option in the WHOQOL-BREF Manual, we converted the raw scores to a scale from 0 (very poor) to 100 (excellent).
The HTQ, HSCL-25, and WHOQOL-BREF have been frequently used in studies of refugees’ mental health and well-being (for further description, see Opaas & Hartmann, Citation2013).
2.6.5. Daily life functioning
Daily life functioning was represented by two variables: Host country language competence, tapping whether or not the participant’s language competence was sufficient to take part in the research interviews in Norwegian, and Employment, tapping whether or not the participant was employed, part-time or full-time, including those who were temporarily on sick leave. Both variables were dichotomously scored 1 (yes) or 0 (no), and expressed by the percentage of participants scoring yes. The scoring of the participants’ host country language competence was based on our experience with them in the interviews. The scoring of the participants’ employment status was based on their report.
2.6.6. Variables related to treatment
Treatment ‘dose’, represented by the variables Number of sessions and Treatment length (in years) were calculated from information in the treatment records and from therapists’ reports in our final interviews with them. When there was more than one treatment episode during our study, we added the number of sessions and months of each treatment.
2.6.7. Clinically assessed diagnoses
The clinical diagnoses were derived from the treatment charts for each patient participating in the study, and from written information provided by the therapists.
2.7. Statistical procedures
In the study by Opaas et al. (Citation2020), changes in mental health symptoms and QoL over the entire 10 year research period were analysed by linear mixed effects models, where all measures obtained at different times and intervals for the 54 participants were included. Linear mixed effects models are especially suitable for analysing data where the response time and number of observations vary. Time was modelled as continuous from T1. For the present study, potential predictors of the long-term trajectories were examined, using mixed effects models including interaction between each predictor and time. Several variables assessed at study inclusion/treatment start (T1), shown to be important in the literature, were selected for the study of possible predictors, comprising: (1) demographics: gender, age, education from country of origin, length of stay in host country, host country language competence, and employment; and (2) exposure to PTEs: childhood family violence, childhood external violence, HTQ trauma events, torture (one item in HTQ), and sexual abuse (two items in HTQ, combined: rape + sexual abuse, scored dichotomously (yes, if a person had experienced either or both; no, if neither was experienced). The predictors were included separately because of the sample size. Results with sub-significant p-values (.05 ≤ p ≤ .10) are included as tentative. Descriptive statistics were analysed by IBM SPSS Statistics, version 26. Predictions were analysed by mixed effects models with R package nlme (R Foundation for Statistical Computing, Vienna, Austria, Citation2013).
3. Results
3.1. Predictors of change in mental health symptoms and quality of life
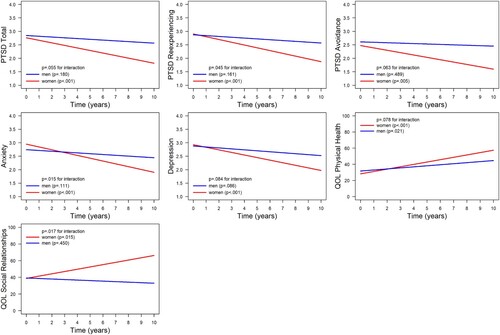
The values for interactions between outcome scores, time, and gender varied from p = .015 (Anxiety) to p = .084 (QoL Physical Health). Thus, the non-significant interactions must be interpreted tentatively. See . Among the demographic variables, female gender significantly predicted a decrease in scores over time in PTSD Total (p = .008), PTSD Reexperiencing (p < .001), PTSD Avoidance (p = .005), Anxiety (p < .001), and Depression (p < .001). Female gender also significantly predicted an increased QoL in Social Relationships (p = .015). The improvement in QoL for Physical Health was significant for both women and men (p < .001 and p = .021, respectively), seemingly with a steeper course of improvement for women (). Overall, the models may indicate that female participants improved more over time compared to male participants. The results for men were generally not significant, but for many outcomes, there seemed to be little or no improvement for men.
Figure 1. Prediction of the long-term course of mental health symptoms and quality of life (QoL) by gender. Mixed effects modelling of the trajectories of mental health symptoms and QoL based on the interaction between gender and time. Symptoms of post-traumatic stress disorder (PTSD) were measured by the Harvard Trauma Questionnaire (Mollica et al., Citation2004); anxiety and depression were measured by the Hopkins Symptom Checklist-25 (Mollica et al., Citation2004); QoL was measured by the World Health Organization Quality of Life BREF questionnaire (WHOQOL-BREF) (WHOQOL Group, Citation1998). The plot illustrates the trajectories over the 10 years of follow-up.
None of the remaining demographic T1 variables significantly predicted the participants’ change over time in any outcome variables: Age [p-values ranged from .175 (QoL Physical Health) to .929 (Depression)]; Years of education from country of origin [p = .103 (QoL Physical Health) to .985 (PTSD Avoidance)]; Years in host country [p = .303 (QoL Psychological Health) to .939 (PTSD Avoidance)]; Host country language competence [p = .154 (PTSD Arousal) to .983 (QoL Physical Health)]; or Employment [p = .172 (PTSD Arousal) to .889 (Depression)].
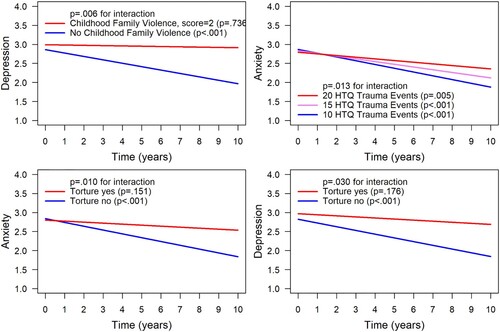
For the following relationships, the interactions between trauma variable, time, and the outcome variable were significant, see . Childhood Family Violence significantly predicted the course of depression (p = .006). (top left) shows that having experienced no childhood family violence predicted a course of improvement in depression over the years (p < .001). For participants who had experienced such adverse events during childhood, the same high level of depression seemed to persist over the course of follow-up. However, this part of the result is subject to considerable uncertainty/variability (p = .736). The HTQ Trauma Events variable significantly predicted the course of anxiety over time (p = .013). (top right) shows that the higher the number of different kinds of war-related PTEs, the smaller the improvement in anxiety over time. Torture interacted significantly with time and predicted the course of both anxiety (p = .010) and depression (p = .030). (bottom left) shows that having experienced no torture significantly predicted a decline in symptoms of anxiety (p < .001), while having experienced torture, with more uncertainty (p = .151), predicted only meagre improvement. (bottom right) shows a similar and significant decline in symptoms of depression for those who had not experienced torture.
Figure 2. Prediction of the long-term course of anxiety and depression by trauma experiences. Mixed effects modelling of the trajectories of mental health symptoms and quality of life (QoL) based on the interaction between trauma variables and time. HTQ Trauma Events and symptoms of post-traumatic stress disorder (PTSD) were measured by the Harvard Trauma Questionnaire (Mollica et al., Citation2004); anxiety and depression were measured by the Hopkins Symptom Checklist-25 (Mollica et al., Citation2004); childhood family violence was assessed for this sample by Opaas & Varvin (Citation2015). The plot illustrates the trajectories over the 10 years of follow-up.
Childhood External Violence did not significantly predict the course of mental health symptoms or QoL variables, with p-values from .150 (PTSD Reexperiencing) to .962 (QoL Psychological Health). Sexual Abuse also did not significantly predict any of the outcome trajectories, with p-values ranging from .245 (Reexperiencing Symptoms of PTSD) to .992 (QoL Physical Health).
4. Discussion
At the time of treatment start and inclusion in this 10 year follow-up study, almost all of the 54 trauma-affected refugee patients had been granted permanent stay in Norway, and were living in ordinary housing in the community (Opaas & Varvin, Citation2015). Furthermore, at treatment start, the mean length of stay in the host country was about 10 years, half of the participants could communicate in Norwegian, 96% qualified for PTSD and 98% for major depression, according to the checklists used, and 41% had previously attended some mental health consultations. During the course of the study, the participants attended a mean of 61 therapy sessions, although with great variation. The high level of pretreatment depression in our study, the length of stay, and the frequency of participants with previous treatment experiences may indicate considerable chronicity among the participants (e.g. Haagen et al., Citation2017; Sonne, Carlsson, Bech, Vindbjerg et al., Citation2016; Sonne et al., Citation2021). Across the 10 years of follow-up, gender was a pervasive predictor of outcome. The results indicated that female refugee patients benefited from treatment on most outcome variables, whereas mean outcomes for males were close to nil, but more uncertain.
4.1. Demographic variables predicting outcome
Female refugee patients in our study benefited from treatment more than males. Female gender significantly predicted reductions in symptoms of PTSD, anxiety, and depression, and improved QoL concerning physical health and social relationships. In other client populations with PTSD, women usually benefit more from psychotherapy than men (Olff, Citation2017). However, for the general patient population, a summary of the existing knowledge concluded that there are no consistent gender differences in therapy outcome (Lutz et al., Citation2021, p. 228).
The more unfavourable outcomes for male participants in the present study are in line with the finding by Stenmark et al. (Citation2014) that male gender predicted a lack of response to treatment. There could be several reasons for the poorer outcomes for men in our study. Male refugees seem more likely to be subjected to torture than female refugees (Dalgaard, Bjerre, & Thøgersen, Citation2021; Mundy, Foss, Poulsen, Hjorthøj, & Carlsson, Citation2020; Song et al., Citation2018), an extreme experience likely to create deep psychological wounds. The extreme passivity installed during torture may counteract the potential protective effect of activity, in which men often engage to overcome danger and meet the demands of life (Varvin, Fischmann, Jovic, Rosenbaum, & Hau, Citation2012). We may speculate that if the proclivity for active problem solving (other than verbal) is not restored during therapy, it will be of little effect. We hereby tentatively place torture under the heading ‘passivity’ of the agency/passivity dimension suggested to organize predictors of treatment outcome in the introduction (Section 1.1).
The other demographic variables, the participants’ age, their education from their country of origin, their length of stay in Norway, and their ability to speak Norwegian, did not significantly predict the participants’ mental health or QoL trajectories. The participants’ employment status also did not predict any of the outcomes in our study, in contrast to the previous finding that employment status correlated significantly with changes in PTSD symptoms (Sonne, Carlsson, Bech, Vindbjerg et al., Citation2016). As noted in the introduction, significant findings for demographic predictor variables in the refugee literature are inconclusive. We believe that results may vary with the size and composition of the study, in terms of the refugee patients’ national origins, age, gender, traumatic exposure, and length of stay in the host country, and the timing of interventions. Other factors that we have not examined here, such as the therapeutic approach, the therapists' cultural sensitivity, match between therapist and patient, and overall structure of mental health care in different countries and regions, may also affect whether and how psychotherapy reaches and is of benefit to different individuals and groups of trauma-affected refugees.
4.2. Traumatic experiences predicting outcome
Most of our participants had experienced adverse events within or outside the home in their childhood, and, mostly in their young adult years, 52% had experienced torture, and 30% had experienced sexual abuse. All participants had experienced traumatic events related to mass conflict, persecution, and flight. Three of the five trauma variables studied predicted a differential development of anxiety and/or depression over the course of time. We found that having experienced violence within the family during childhood predicted a lack of improvement in depression, although with much uncertainty. However, not having experienced family violence in childhood significantly predicted a beneficial outcome on symptoms of depression. The initial frequency of depression in this sample was close to 100%, and, according to Opaas et al. (Citation2020), the effect size of the reductions in depressive symptoms across the whole study period was low (r = .07). Thus, domestic violence and abuse during the refugees’ childhood accounted for some of the intractability of depression in this study. Of relevance is that Wells, Vanderlind, Selby, and Beevers (Citation2014) found that self-reported severity of childhood abuse was associated with increased vulnerability to depression in young adults. Childhood traumas have often gone unnoticed in the assessment of adult refugee patients, perhaps because of cultural aspects, language barriers, time, and money for interpreters, and perhaps not least because of the impact on therapists of refugees’ horrific experiences related to war, imprisonment, rape, and torture. Early developmental timing of trauma may be associated with attachment disturbance, and with aggravated PTSD symptoms for adults with a broad range of lifetime traumas (Ogle, Rubin, & Siegler, Citation2015; Riber, Citation2017). Childhood adversities and trauma may thus exacerbate the adverse effects of later war, flight, and exile hardships. Therefore, childhood trauma among refugees deserves special attention in the clinic.
Even though many studies have found that experiences of torture are associated with poorer mental health in refugee populations (e.g. Dalgaard et al., Citation2021), the three studies in our literature review that investigated torture as a potential predictor (Haagen et al., Citation2017; Sander et al., Citation2019; Stenmark et al., Citation2014) did not find that torture predicted therapy outcome. However, in the present study, we found that not having experienced torture significantly predicted a decline in both anxiety and depression, while the results for those who reported experiences of torture indicated little or no improvement, although with more uncertainty. Lastly, in line only with the study of Sonne et al. (Citation2021), we found that the number of PTEs related to war and persecution significantly predicted outcomes. In our study, fewer such experiences predicted a better outcome in anxiety, and conversely, a greater number predicted a more modest decline in anxiety. Finally, childhood experiences of violence external to the home and (HTQ-reported) sexual assaults did not significantly predict outcome in our study.
4.3. Summary
Gender was the only predictor of the outcome of PTSD symptoms, with the modelled interactions showing that female refugee patients improved significantly through therapy and over the years in symptoms of PTSD. Gender, having experienced torture, and the number of different war-related experiences predicted the trajectory of anxiety: female refugee patients, refugee patients with fewer PTEs related to war, persecution, and human rights violations, and refugee patients who had not experienced torture improved significantly in the symptoms of anxiety. Gender, torture, and childhood family violence predicted the trajectory of depression: female participants, participants who had not experienced violence within the family during childhood, and participants who had not been subjected to torture improved significantly in terms of depression. Finally, gender predicted the trajectories of experienced QoL regarding physical health and social relationships. Both men and women had significant trajectories of improvement in their QoL regarding physical health, although the model showed a slightly steeper course of improvement in women. Only women had a significant trajectory of improvement in their QoL regarding social relationships. The modelled trajectories of the male participants, and of participants who had been exposed to childhood family violence and to torture, showed little or no improvement across all outcomes, although these results were fraught with uncertainty. The non-significant prediction of these trajectories was probably produced by the great variability in individual outcomes. This complies with findings of great variability in individual outcomes in previous clinical refugee studies (Sonne et al., Citation2021). Judging from the present study, male refugees may be substantially at risk, by having experienced pervasive traumatic experiences, and by not benefiting from the psychotherapy that was offered. Especially for male refugees with severe mental health problems, we may need a broader approach to mental health care, possibly emphasizing active solutions to postmigration mental, physical, and practical problems.
4.4. Strengths and limitations
Few other studies have so far reported predictors of therapy outcome for trauma-affected refugees. We found several predictors that may explain some of the great individual variation in outcome for this group. Strengths of the study were the naturalistic setting, the very few exclusion criteria, and the high inclusion rate at T1, securing a representative sample of newly admitted patients with a refugee and trauma background within the respective clinical units at the time of inclusion. Other strengths were the negligible attrition rate during the first years of participants’ partaking in the study, and the long follow-up and repeated measuring points for most of the participants. However, the relatively small number of participants represents a major limitation, which restricted the possibility to include possible mediators in the analyses; for example, whether gender would have mediated the findings for the trauma-related predictors, or vice versa. The small sample size may also have resulted in few significant predictors being detected. The sample size limits the potential to generalize from this study to other clinical refugee populations and therapy trials. Although we investigated many aspects of the participants’ lives, we did not systematically assess their physical health problems and pain, resilience, social support, or hardships encountered in the host country, which could also have impacted the outcome of therapy. The position in time of the therapies reported in this study, starting within the period 2006–2009 and mostly completed sometime between 2007 and 2012, also represents a potential limitation in generalization to present-day therapies with traumatized refugees. However, we believe that the study findings highlight important aspects to bear in mind when planning research, therapy programmes, or psychosocial interventions for this group.
5. Conclusion and implications
Gender, childhood experiences of violence within the family, the number of different kinds of traumatic experiences related to war, persecution and human rights violations, and the experience of torture individually and significantly predicted the course of mental health symptoms and QoL for refugee patients in this 10 year longitudinal study. Female gender predicted significant improvements in PTSD, anxiety, depression, and QoL. However, male participants appeared relatively unchanged, although the lack of statistical significance for the results for men probably indicated great individual variability. Torture, being victimized by a great number of traumatic events, and early developmental trauma may be examples of experiences that may install passivity and hopelessness regarding the possibility to influence one’s life. To study further whether the suggested division of predictors into ‘agency/opportunities to actively influence one’s life’ and ‘passivity/lack of possibility to actively influence one’s life’ is a useful way to systematize predictors of treatment outcome, more studies, as well as qualitative enquiries, will be necessary.
The inconsistent, but meagre, results for men are a cause for concern. Providing adequate treatment at an earlier time in the host country may be one way to enhance the outcome for male (and female) refugees. Moreover, gender-sensitive approaches and individually tailored therapeutic interventions are needed to meet the diverse needs of traumatized refugees. Many forms of psychotherapy may function well for women, as indicated by the group-level improvement in this study, where therapeutic approaches differed. Placing greater weight on facilitating employment, men’s role as breadwinners, and facilitating other forms of active efforts by male refugees to improve their living conditions may, in combination with psychotherapy, be ways to improve their emotional health and well-being. It seems that for male participants in this study, their social life often waned. Therefore, interventions that promote social contact and counteract isolation could also be important.
Childhood adverse and traumatic experiences may directly (family violence) or indirectly (violence outside the home) be related to attachment security or insecurity. Also, intensely traumatizing interpersonal experiences in adulthood, such as torture, may affect trust and the ability to retain or form close relationships, thus hindering social support and possibly prolonging mental health suffering. This supports the view that psychotherapy and other psychosocial interventions for traumatized refugees should be oriented towards fostering relational safety and competence in a context of psychosocial rehabilitation (Varvin, Citation2015, Citation2020).
Our findings demonstrate the importance of differentiating between genders when studying treatment outcome. More research on gender differences and predictors of therapy outcome, specifically conducted in refugee populations, is needed to make sense of divergent research findings, and to guide clinicians’ and policymakers’ efforts to improve the health and functioning of trauma-affected refugees. Discerning which characteristics may determine who will benefit from psychotherapy, and which barriers may be at play for those who do not seem to benefit, is vital to be able to help as many of these patients as possible and to use existing resources in a good way. Gender-sensitive and culturally sensitive treatment programmes for trauma-affected refugees that take research findings as well as the individual patient’s needs and resources into account, may, in the end, be less costly and better serve refugees and society at large.
Data availability statement
The data that support the findings of this study are available on reasonable request from the corresponding author, Marianne Opaas. The data are not publicly available owing to ethical concerns, i.e. information on open data sharing was not given to participants at inclusion in the study in 2006–2009 and ethical clearance has not been given for such sharing.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders, fourth edition (DSM-IV). Washington, DC: American Psychiatric Association.
- Blackmore, R., Boyle, J. A., Fazel, M., Ranasinha, S., Gray, K. M., Fitzgerald, G., et al. (2020). The prevalence of mental illness in refugees and asylum seekers: A systematic review and metaanalysis. PLoS Medicine, 17(9), e1003337. doi:10.1371/journal.pmed.1003337
- Bruhn, M., Rees, S., Mohsin, M., Silove, D., & Carlsson, J. (2018). The range and impact of postmigration stressors during treatment of trauma-affected refugees. The Journal of Nervous and Mental Disease, 206(1), 61–68. doi: 10.1097/NMD.0000000000000774
- Buhmann, C. B., Mortensen, E. L., Nordentoft, M., Ryberg, J., & Ekstrøm, M. (2015). Follow-up study of the treatment outcomes at a psychiatric trauma clinic for refugees. Torture, 25, 1–16.
- Buhmann, C. B., Nordentoft, M., Ekstroem, M., Carlsson, J., & Mortensen, E. L. (2018). Long-term treatment effect of trauma-affected refugees with flexible cognitive behavioural therapy and antidepressants. Psychiatry Research, 264, 217–223. doi: 10.1016/j.psychres.2018.03.069
- Dalgaard, N. T., Bjerre, K., & Thøgersen, M. H. (2021). Twenty seven years of treating survivors of torture and organized violence – Associations between torture, gender and ethnic minority status among refugees referred for treatment of PTSD. European Journal of Psychotraumatology, 12(1), 1904712. doi: 10.1080/20008198.2021.1904712
- Drožđek, B., Kamperman, A. M., Tol, W. A., Knipscheer, J. W., & Kleber, R. J. (2014). Seven-year follow-up study of symptoms in asylum seekers and refugees with PTSD treated with trauma-focused groups. Journal of Clinical Psychology, 70(4), 376–387. doi:10.1002/jclp.22035
- Drožđek, B., Kamperman, A. M., Wietse, A., Tol, W. A., Knipscheer, J. W., & Kleber, R. J. (2013). Is legal status impacting outcomes of group therapy for posttraumatic stress disorder with male asylum seekers and refugees from Iran and Afghanistan? Psychiatry, 13, 148. http://www.biomedcentral.com/1471-244X/13/148.
- Friis Jørgensen, S., Auning-Hansen, M., Ottesen Kennair, L. E., & Elklit, A. (2017). Can disability predict treatment outcome among traumatized refugees? Torture, 27(2), 12–26. doi: 10.7146/torture.v27i2.97208
- Giacco, D., & Priebe, S. (2018). Mental health care for adult refugees in high-income countries. Epidemiology and Psychiatric Sciences, 27(2), 109–116. doi.10.1017/S2045796017000609
- Haagen, J. F. G., ter Heide, F. J. J., Mooren, T. M., Knipscheer, J. W., & Kleber, R. J. (2017). Predicting post-traumatic stress disorder treatment response in refugees: Multilevel analysis. British Journal of Clinical Psychology, 56, 69–83. doi: 10.1111/bjc.12121
- Hassan, G., Ventevogel, P., Jefee-Bahloul, H., Barkil-Oteo, A., & Kirmayer, L. J. (2016). Mental health and psychosocial wellbeing of Syrians affected by armed conflict. Epidemiology and Psychiatric Sciences, 25(2), 129–141. doi: 10.1017/S2045796016000044
- Kingsley, P. (2016). “Prisoners of Europe”: The everyday humiliation of refugees stuck in Greece. The Guardian. https://www.theguardian.com/world/2016/sep/06/prisoners-of-europe-the-everyday-humiliation-of-refugees-stuck-in-greece-migration
- Li, S. S., Liddell, B. J., & Nickerson, A. (2016). The relationship between post-migration stress and psychological disorders in refugees and asylum seekers. Current Psychiatry Reports, 18(9), 1–9. doi:10.1007/s11920-016-0723-0
- Lutz, W., de Jong, K., Rubel, J. A., & Delgadillo, J. (2021). Measuring, predicting, and tracking change in psychotherapy. In M. Barkham, W. Lutz, & L. G. Castonguay (Eds.), Bergin and Garfields Handbook of Psychotherapy and Behavior Change, 50th Anniversary Edition, 4 (pp. 89–133). Hoboken, NJ: Wiley & Sons.
- Mollica, R. F., McDonald, L. S., Massagli, M. P., & Silove, D. M. (2004). Measuring trauma, measuring torture. Instructions and guidance on the utilization of Hopkins Symptom Checklist-25 (HSCL-25) & the Harvard Trauma Questionnaire (HTQ). Harvard program in refugee trauma, http://hprt-cambridge.org. CD, retrieved 2006.
- Mundy, S. S., Foss, S. L. W., Poulsen, S., Hjorthøj, C., & Carlsson, J. (2020). Sex differences in trauma exposure and symptomatology in trauma-affected refugees. Psychiatry Research, 293, 113445. doi:10.1016/j.psychres.2020.113445
- Nordin, L., & Perrin, S. (2019). Pre-treatment pain predicts outcomes in multimodal treatment for tortured and traumatized refugees: A pilot investigation. European Journal of Psychotraumatology, 1–10. doi:10.1080/20008198.2019.1686807
- Ogle, C. M., Rubin, D. C., & Siegler, I. C. (2015). The relation between insecure attachment and posttraumatic stress: Early life versus adulthood traumas. Psychological Trauma: Theory, Research, Practice, and Policy, 7(4), 324–332. doi:10.1037/tra0000015
- Olff, M. (2017). Sex and gender differences in post-traumatic stress disorder: An update. European Journal of Psychotraumatology, 8, 1351204. doi:10.1080/20008198.2017.1351204
- Opaas, M., & Hartmann, E. (2013). Rorschach assessment of traumatized refugees: An exploratory factor analysis. Journal of Personality Assessment, 95, 457–470. doi:10.1080/00223891.2013.781030
- Opaas, M., & Hartmann, E. (2021). Traumatized refugees in psychotherapy: Long-term changes in personality, mental health, well-being, and exile life functioning. Journal of Nervous and Mental Disease, 1–13. doi:10.1097/NMD.0000000000001396
- Opaas, M., Hartmann, E., Wentzel-Larsen, T., & Varvin, S. (2016). Relationship of pretreatment Rorschach factors to symptoms, quality of life, and real-life functioning in a three-year follow-up of traumatized refugee patients. Journal of Personality Assessment, 98, 247–260. doi:10.1080/00223891.2015.1089247
- Opaas, M., & Varvin, S. (2015). Relationships of childhood adverse experiences with mental health and quality of life at treatment start for adult refugees traumatized by pre-flight experiences of war and human right violations. Journal of Nervous and Mental Disease, 203, 684–695. doi:10.1097/NMD.0000000000000330
- Opaas, M., Wentzel-Larsen, T., & Varvin, S. (2020). The 10-year course of mental health, quality of life, and exile life functioning in traumatized refugees from treatment start. PLoS ONE, 15(12), e0244730. doi:10.1371/journal.pone.0244730
- R Foundation for Statistical Computing, Vienna, Austria. (2013). https://www.r-project.org/foundation/
- Riber, K. (2017). Trauma complexity and child abuse: A qualitative study of attachment narratives in adult refugees with PTSD. Transcultural Psychiatry, 54(5–6), 840–869. doi: 10.1177/1363461517737198
- Riza, E., Karnaki, P., Gil-Salméron, A., Zota, K., Ho, M., Petropoulou, M., … Linos, A. (2020). Determinants of refugee and migrant health status in 10 European countries: TheMig-HealthCare project. International Journal of Environmental Resarch and Public Health, 17, 1–13. doi:10.3390/ijerph17176353
- Sander, R., Laugesen, H., Skammeritz, S., Mortensen, E. L., & Carlsson, J. (2019). Interpreter-mediated psychotherapy with trauma-affected refugees – A retrospective cohort study. Psychiatry Res 271, 684–692. doi:10.1016/j.psychres.2018.12.058
- Schick, M., Morina, N., Mistridis, P., Schnyder, U., Bryant, R. A., & Nickerson, A. (2018). Changes in post-migration living difficulties predict treatment outcome in traumatized refugees. Frontiers in Psychiatry, 9, 476. doi:10.3389/fpsyt.2018.00476
- Skevington, S. M., Lotfy, M., & O'Connell, K. A. (2004). The World Health Organization's WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL Group. Quality of Life Research, 13, 299–310. doi: 10.1023/B:QURE.0000018486.91360.00
- Song, S. J., Subica, A., Kaplan, C., Tol, W., & de Jong, J. (2018). Predicting the mental health and functioning of torture survivors. Journal of Nervous and Mental Disease, 206, 33–39. doi: 10.1097/NMD.0000000000000678
- Sonne, C., Carlsson, J., Bech, P., Vindbjerg, E., Mortensen, E. L., & Elklit, A. (2016). Psychosocial predictors of treatment outcome for trauma-affected refugees. European Journal of Psychotraumatology, 7, 1. doi:10.3402/ejpt.v7.30907
- Sonne, C., Carlsson, J., Beck, P., Elklit, A., & Mortensen, E. L. (2016). Treatment of trauma-affected refugees with venlafaxine versus sertraline combined with psychotherapy – A randomised study. BMC Psychiatry, 16(383), 3–13. doi:10.1186/s12888-016-1081-5
- Sonne, C., Mortensen, E. L., Silove, D., Palic, S., & Carlsson, J. (2021). Predictors of treatment outcomes for trauma-affected refugees – Results from two randomised trials. Journal of Affective Disorders, 282, 194–202. doi:10.1016/j.jad.2020.12.095
- Stammel, N., Knaevelsrud, C., Schock, K., Walther, L. S., Wenk-Ansohn, M., & Böttche, M. (2017). Multidisciplinary treatment for traumatized refugees in a naturalistic setting: Symptom courses and predictors. European Journal of Psychotraumatology, 8(sup2), 1377552. doi:10.1080/20008198.2017.1377552
- Steel, Z., Chey, T., Silove, D., Marnane, C., Bryant, R. A., & Van Ommeren, M. (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA, 302(5), 537–549. doi:10.1001/jama.2009.1132
- Stenmark, H., Guzey, I. C., Elbert, T., & Holen, A. (2014). Gender and offender status predicting treatment success in refugees and asylum seekers with PTSD. European Journal of Psychotraumatology, 5(1), 20803. doi:10.3402/ejpt.v5.20803
- UNHCR. The UN Refugee Agency, June 2021, retrieved Oct. 13, 2021. https://www.unhcr.org/figures-at-a-glance.html.
- van Wyk, S., Schweitzer, R., Brough, M., Vromans, L., & Murray, K. (2012). A longitudinal study of mental health in refugees from Burma: The impact of therapeutic interventions. Australian & New Zealand Journal of Psychiatry, 46(10), 995–1003. doi: 10.1177/0004867412443059
- Varvin, S. (2015). Psychoanalysis with the traumatized patient: Helping to survive extreme experiences and complicated loss. International Forum of Psychoanalysis, doi:10.1080/0803706X.2014.1001785
- Varvin, S. (2020). Specialist services. In D. Bughra (Ed.), Oxford Textbook of Migrant Psychiatry (pp. 449–458). Oxford: Oxford University Press.
- Varvin, S., Fischmann, T., Jovic, V., Rosenbaum, B., & Hau, S. (2012). Traumatic dreams: Symbolization gone astray. In P. Fonagy, H. Kächele, M. Leuzinger-Bohleber, & D. Taylor (Eds.), The Significance of Dreams (182–211). London: Karnac Books.
- Walther, L., Fuchs, L. M., Schupp, J., & von Scheve, C. (2020). Living conditions and the mental health and well-being of refugees: Evidence from a large-scale German survey. Journal of Immigrant and Minority Health, 22(5), 903–913. doi:10.1007/s10903-019-00968-5
- Wells, T. T., Vanderlind, W. M., Selby, E. A., & Beevers, C. G. (2014). Childhood abuse and vulnerability to depression: Cognitive scars in otherwise healthy young adults. Cognition & Emotion, 28(5), 821–833. doi:10.1080/02699931.2013.864258
- WHOQOL Group. (1998). Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological Medicine, 28, 551–558. doi: 10.1017/S0033291798006667
- World Health Organisation. (1994). Pocket guide to ICD-10 classification of mental and behavioural disorders: With glossary and Diagnostic Criteria for Research DCR-10. (J. E. Cooper, ed.) Geneva: World Health Organisation/Churchill Livingstone.
