ABSTRACT
Background:
Antibiotics have significantly reduced mortality and improved outcomes across various medical fields; however, the rise of antibiotic resistance poses a major challenge, causing millions of deaths annually. Deprescribing, a process that involves discontinuing unnecessary antibiotics, is crucial for combating this threat. This study was designed to assess the knowledge, perceptions, and practices of physicians regarding antibiotic deprescribing in Jordan.
Methods:
A cross-sectional survey was conducted between January-February 2024 to assess the knowledge, perceptions, and practices of physicians regarding antibiotic deprescribing in Jordan. An electronic questionnaire served as the data collection tool. Descriptive analysis was performed using SPSS software version 26. Additionally, logistic regression analysis was carried out to identify independent factors associated with physicians’ willingness to deprescribe antibiotics.
Results:
The study involved 252 physicians, primarily male (n = 168, 67.7%), with a median age of 33 years. Regarding antibiotics deprescribing, 21.8% (n = 55) expressed willingness to deprescribe inappropriate antibiotics.
High awareness of deprescribing was evident, with 92.9% (n = 234) familiar with the concept, 94% (n = 237) knowledgeable about appropriate situations, and 96.8% (n = 244) recognising its potential benefits. Furthermore, 81.8% (n = 205) reported having received formal training in antibiotics deprescribing, and 85.3% (n = 215) were informed about the availability of deprescribing tools.
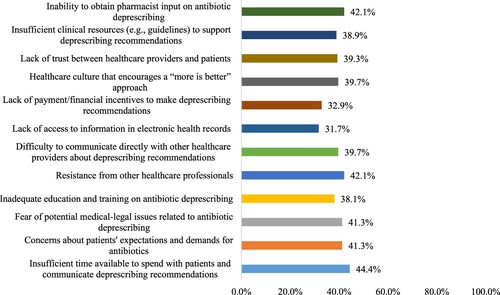
Physicians highlighted challenges including insufficient time (44.4%, n = 112) and resistance from patients (41.3%, n = 104) and colleagues (42.1%, n = 106). Despite challenges, a significant proportion regularly assessed antibiotic necessity (46.9%, n = 117) and educated patients about antibiotic-related harms (40.5%, n = 102). Logistic regression analysis revealed no significant demographic factors influencing physicians’ willingness to deprescribe antibiotics (p > 0.05).
Conclusion:
Physicians in Jordan exhibit high awareness of antibiotics deprescribing and recognise its benefits. Challenges such as time constraints and communication barriers need to be addressed to facilitate effective deprescribing practices. Comprehensive guidelines and interdisciplinary collaboration are essential for promoting judicious antibiotic use and combating antimicrobial resistance.
1. Introduction
Antibiotics inauguration is deemed a major medical revolution and one of the main modern medicine approaches to fight infections, lowering death rates, and addressing various infectious disease-related problems (Gould, Citation2016; Mohr, Citation2016). Antibiotics have played a crucial role in the success of numerous medical fields, including rheumatology, cancer, and invasive operations such as organ transplantation (Ventola, Citation2015). The accessibility of antibiotic therapy has greatly decreased mortality, raising average life expectancy (Adedeji, Citation2016).
The 1930s to the 1960s were considered the ‘great era’ of antibiotics, during which numerous antibiotics were developed. Unfortunately, this era ended because researchers were unable to maintain the pace of antibiotic discovery in the face of emerging resistant pathogens (Nathan & Cars, Citation2014). A growing number of bacteria are developing resistance to several antibiotics already in use, leading to the emergence of multidrug-resistant bacteria (Tanwar et al., Citation2014). Antibiotic-resistant bacteria pose a serious challenge to current healthcare due to the lack of new antimicrobial medications and the rising number of treatment failures caused by multidrug-resistant bacteria (Read & Woods, Citation2014; Spellberg et al., Citation2013).
Antibiotic-resistant bacteria may arise from various causes, such as the overuse of antibiotics in humans and animals, over-the-counter antibiotic purchases, increased worldwide travel, inadequate hygiene, and antibiotic overprescribing (Llor & Bjerrum, Citation2014; Van Boeckel et al., Citation2015). In 2019, antibiotic-resistant bacterial infections were estimated to cause 1.27 million deaths globally and by 2025, approximately 10 million deaths are expected to occur annually (Aslam et al., Citation2018; O'Neill, Citation2016). Specifically, these types of infection have been shown to result in longer hospitalisations, increased mortality, and higher medical expenses (Conlon-Bingham et al., Citation2019; Cosgrove, Citation2006).
Antimicrobial prescribing is a complex process influenced by various elements, including the healthcare system, physicians, other healthcare professionals, and patients (Rodrigues et al., Citation2013). Strong evidence links the consumption of antibiotics to the presence of antibiotic-resistant bacteria in both the community and the individual (Costelloe et al., Citation2010). There is strong evidence that reducing cumulative antibiotic consumption lowers the likelihood of antibiotic-resistant bacteria (Llewelyn et al., Citation2017).
When it comes to the management of infectious diseases, inappropriate antibiotic prescriptions include those written for unnecessary purposes, chosen incorrectly, or administered for the wrong duration of time (Alsayed et al., Citation2022; Fu et al., Citation2023; Mahmood et al., Citation2022). In such cases, deprescribing may be considered for the patient's benefit to prevent adverse reactions from recurring. Deprescribing is defined as the process of discontinuing an unsuitable medicine under the supervision of a medical professional to manage polypharmacy and enhance results (Woodford & Fisher, Citation2019).
Reports indicate that antibiotic-resistant bacteria are widely present in Jordanian hospitals. Methicillin-resistant Staphylococcus aureus (MRSA) is particularly common, with a rate of 45% (Karasneh et al., Citation2021). Various strategies have been developed to decrease the improper use of antibiotics in healthcare settings. In Jordan, the majority of efforts have concentrated on decreasing the initiation of unnecessary antibiotic treatments and have targeted prescribers (Al-Taani, Al-Azzam, Karasneh, Ababneh, et al., Citation2022; Al-Taani, Al-Azzam, Karasneh, Sadeq, et al., Citation2022; Karasneh et al., Citation2021). However, no efforts have been made to stop the already-initiated inappropriate antibiotics.
In Jordan, deprescribing is primarily the responsibility of physicians. Therefore, to design guidelines and methods to optimise appropriate medication usage, it is crucial to investigate physicians’ knowledge and desire to support effective deprescribing. Hence, the purpose of this was to assess the knowledge, perceptions, and practices of physicians regarding the deprescribing of antibiotics in Jordan.
2. Methods
2.1. Study design, sample, and setting
This research is a cross-sectional study aimed to assess the knowledge, perceptions, and practices of physicians regarding the deprescribing of antibiotics in Jordan. The study was conducted between January-February 2024, among physicians in Jordan. The study population comprised physicians registered with the Jordanian Medical Association, encompassing a wide range of sectors including private practices, public hospitals, and clinics. Inclusion criteria allowed for any actively practicing physician registered in Jordan, irrespective of specialty or sector. There were no specific exclusion criteria, except that participants needed to be currently practicing physicians. The survey reached physicians across all major cities and regions in Jordan, ensuring comprehensive national representation.
2.2. Data collection
To mitigate selection bias and enhance the study's validity, we implemented several strategies during the data collection phase. Physicians were selected using a mixed approach combining convenience and snowball sampling to capture a diverse demographic and professional spread, which helps in reducing the impact of selection bias typical to convenience sampling alone. The survey was distributed through social media platforms such as Facebook, WhatsApp, and LinkedIn. Research assistants and medical school professors were also involved to extend the reach. The questionnaire included a brief introductory paragraph specifying the target group and ensuring that only eligible physicians participated.
2.3. Survey development
We designed a survey to comprehensively assess the knowledge, perceptions, and practices of physicians regarding the deprescribing of antibiotics in Jordan. The questionnaire underwent validation for content and face validity by two experts in clinical pharmacy. It comprised five sections. The first covers demographic characteristics (e.g. age, gender, specialisation, years of experience, country of graduation, and number of daily consultation), The second section comprises closed-ended questions assessing physicians’ knowledge of Antibiotics deprescribing. The third section includes questions exploring physicians’ perception towards antibiotics deprescribing, and the fourth section evaluates physicians’ perception towards the potential challenges against antibiotic deprescribing. The last section assesses physicians’ previous practice in antibiotic deprescribing.
A pilot study was carried out with five physicians to evaluate the questionnaire's format, clarity, length, and general impression. Following their feedback, modifications were made to some of the questions. The data from this pilot study were excluded from the final analysis. The internal consistency of the questionnaire was confirmed with Cronbach's alpha values of 0.722, 0.953, and 0.845 for sections three, four, and five, respectively, indicating satisfactory reliability of the items in these sections (Taber, Citation2018).
2.4. Sample size determination
The sample size was calculated based on the number of subjects per predictor needed for regression analysis of factors affecting physicians’ willingness to deprescribe antibiotics (Tabachnick & Fidell, Citation2006). Adhering to Tabachnick and Fidell guidelines for sample size calculation while conducting regression analysis, 5–20 subjects are required per each predictor (Tabachnick & Fidell, Citation2006), and since six predictors are hypothetically assumed to influence physicians’ responses in the current study, the minimum sample size required to ensure satisfactory statistical power was found to be equal to 120 participants.
2.5. Ethical considerations
Ethical approval was obtained from the Institutional Review Board (IRB) at the Applied Science Private University [Approval Number 2024-PHA-1], and electronic informed consent was secured from each participating physician. The study strictly adhered to the ethical standards outlined in the Declaration of Helsinki.
2.6. Statistical analysis
Data were compiled and analysed using the statistical package for social science (SPSS) version 26 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were employed to summarise the distribution of variables. Qualitative variables were analysed using frequency and percentage, while continuous variables were analysed using median and interquartile range (IQR). Normality was checked using the Kolmogorov – Smirnov test and histograms, with p ≤ 0.05 indicating non-normal distribution.
Logistic regression analysis was carried out to screen for independent factors associated with physicians’ willingness to deprescribe antibiotics. Following simple logistic regression, any variable with a p-value < 0.250 was considered eligible for entry in multiple logistic regression analysis. Before conducting multiple logistic regression analysis, variables were checked for the absence of multicollinearity (i.e. Pearson correlation coefficient <0.9 for any two variables). A P-value of ≤0.05 was considered statistically significant. Regarding the internal consistency of the study survey, a Cronbach alpha value > 0.7 was considered to indicate an acceptable internal consistency (Taber, Citation2018).
3. Results
The study comprised 252 physicians, with a median age of 33 years and an interquartile range of 11 years. Of the respondents, 67.7% were male (n = 168). The majority held the title of general practitioner with varying years of professional experience (median = 6 years). A significant proportion (n = 183, 72.6%) graduated from Jordanian medical schools. Physicians reported various daily consultation numbers, with 46% (n = 116) seeing over 20 patients per day. Regarding antibiotics deprescribing, 21.8% (n = 55) were willing to deprescribe any inappropriate antibiotic during their practice ().
Table 1. Sociodemographic characteristics of the study sample (n = 252).
The study showed that most physicians in the sample exhibit substantial awareness of antibiotics deprescribing. Specifically, 92.9% (n = 234) were familiar with the concept, 94% (n = 237) were knowledgeable about appropriate situations for deprescribing, 96.8% (n = 244) recognised its potential benefits, and 91.7% (n = 231) were aware of potential risks. Moreover, 81.8% of the participants (n = 205) had received formal training in antibiotics deprescribing, and 85.3% (n = 215) were informed about the availability of deprescribing tools ().
Table 2. Physicians’ awareness about antibiotic deprescribing (n = 252).
Physicians’ perceptions regarding antibiotics deprescribing were investigated, revealing significant insights (). The majority (n = 229, 90.9%) recognised the importance of antibiotic prescribing in compacting antibiotic resistance, and a significant proportion (n = 216, 85.7%) believed it to be a feasible practice in their clinical setting. Notably, a considerable number (n = 200, 79.4%) acknowledged the influence of patients’ expectations, often leading to antibiotics overprescribing. Physicians thought that patients are generally open to antibiotic deprescribing recommendations (n = 115, 45.6%), and they believed that deprescribing has as potential to improve patient outcomes (n = 137, 54.4%), and felt confidence in communicating about deprescribing (n = 157, 62.3%). Concerns were expressed about potential complications and admission resulting from antibiotics deprescribing (68.3% agreed/strongly agreed). Furthermore, the majority of physicians (n = 206, 81.7%) believed that antibiotic deprescribing should be included in clinical guidelines, while 73.4% (n = 185) acknowledged that withdrawing antibiotics prescribed by colleagues is unethical.
Table 3. Physicians’ perception towards antibiotic deprescribing (n = 252).
Physicians perceived several challenges to antibiotic deprescribing, the most prominent being the insufficient time available to discuss deprescribing with patients (n = 112, 44.4%). Equally notable were barriers such as the inability to obtain pharmacist input and resistance from other healthcare professionals (n = 106, 42.1% for both). Concerns about medical-legal implications and patients’ expectations both present considerable challenges, each cited by 41.3% of physicians (n = 104). Other issues included disruption between providers and patients, a culture of more-is-better in healthcare, and communication barriers, each just under 40%. Less cited challenges involved the absence of financial motivation and restricted access to patient information in electronic health records, with proportions of 32.9% (n = 83) and 31.7% (n = 80), respectively ().
Figure 1. Potential challenges against antibiotic deprescribing as perceived by the physicians (n = 252).
illustrates physicians’ practices in antibiotics deprescribing. Notably, 46.9% of respondents (n = 117) reported regular assessment of the need for deprescribing, while 42.9% (n = 108) assessed antibiotics for potential patient risks. Educating patients about potential antibiotic-related harm was reported by 40.5% of physicians (n = 102). Recommendations for antibiotic deprescribing, especially when patient preferred not to continue antibiotics, were always made by 29.4% (n = 74). A preference for delayed antibiotic prescribing over deprescribing when antibiotics were considered unnecessary was indicated by 34.5% of the participants (n = 87). Additionally, 28.2% (n = 71) would only deprescribe if patient had taken antibiotics for at least five days, and 29% (n = 73) agreed to deprescribe to reduce antimicrobial resistance. Furthermore, 23.4% (n = 59) agreed to withdraw antibiotics initiated by patients themselves, and 31.3% (n = 33) agreed to do so if antibiotics were obtained without prescription from a pharmacy.
Table 4. Physicians’ practice in antibiotic deprescribing (n = 252).
Logistic regression analysis for factors influencing associated with physicians’ willingness to deprescribe antibiotics () showed that none of the studied demographic factors had a significant association with physicians’ willingness to deprescribe antibiotics (p > 0.05 for all).
Table 5. Assessment of factors associated with physicians’ willingness to deprescribe antibiotics (n = 252).
4. Discussion
Although deprescribing is mainly linked to chronic medical conditions, the minimisation of unnecessary antibiotic use is equally important. Antibiotic deprescribing reduces antimicrobial resistance and reduces the risk of adverse events of antibiotics that have been prescribed for sufficient appropriate duration or not indicated (Hansen et al., Citation2019). Since physicians assume the responsibility of deprescribing, it is imperative to explore their knowledge of and attitudes toward the deprescribing process. Physicians in our study were aware of the importance of antibiotic deprescribing and its influence on the emergence and spread of resistance. Similar findings were revealed in studies conducted in Nigeria and Saudi Arabia (Akande-Sholabi et al., Citation2023; AlRasheed et al., Citation2018). However, evidence from a randomised controlled trial showed that the clinical outcomes of patients who underwent antibiotic deprescribing were similar to those who continued the antibiotic therapy (Llor, Moragas, et al., Citation2022).
The majority of physicians in this study were unwilling to deprescribe antibiotics, they were concerned that patients may not be receptive and may not welcome deprescribing. In consistence, some physicians believed that discontinuation of antibiotics might harm their relationship with their patients (Urbiztondo et al., Citation2018). Furthermore, patients’ negative perception was reported as a deprescribing barrier owing to their self-interpretations of this intervention as a demission of patient care and a process for cost savings (Okeowo et al., Citation2023). On the other hand, Lukacena et al revealed that 83.5% of their study population expressed willingness to deprescribing if it was approved by their clinicians (Lukacena et al., Citation2022). Physicians also expressed their concerns that antibiotic deprescribing may increase complications and hospital admissions. However, in general, hospital admissions and increased length of stay are caused by adverse drug reactions caused by polypharmacy which in turn can be reduced by deprescribing (Formica et al., Citation2018). Moreover, in this study, more than two-thirds of the physicians believed that deprescribing should be included in clinical guidelines. This perception was similarly reported by health professionals in other studies (Reeve et al., Citation2017; Wu et al., Citation2021). Han Kua et al. (Citation2019) revealed that health professional considered systemic practices of deprescribing and educational tools as enablers of the process. Health professionals require guidelines and explicit algorithms that provide sufficient guidance and evident steps in the process that guarantee patient safety and satisfaction. Indeed, the presence of specific guidelines would represent a reference point for all parties involved in the management of the patient care process.
Many structured deprescribing guidelines are available but are not confined to a certain drug and none were assessed by randomised controlled trials to provide evidence that these measures have positive effects on the clinical outcomes (Scott et al., Citation2017). Many guidelines which are in the form of recommendations, and communication between the healthcare professionals, caregivers, and patients are highly encouraged to manage the care plan and reduce emergency admissions (Crisafulli et al., Citation2022). Guidelines for deprescribing implementation in older patients’ setting are abundant (O'Mahony et al., Citation2015; Thompson et al., Citation2019), mostly were developed to overcome the problem of polypharmacy which is very common encountered in this population and resulted in higher rate of visits to the emergency department (Doumat et al., Citation2023). Moreover, antibiotics are overprescribed for many asymptomatic elderly patients suspected of urinary tract infection (Álvarez Artero et al., Citation2019). Consequently, deprescribing is one possible strategy to reduce polypharmacy and improve safety and mortality, if applied in the form of patient-specific interventions (Page et al., Citation2016).
Barriers to deprescribing may be related to the patient, physician, and/or the medical institution (Gupta et al., Citation2019). Physicians in this study reported insufficient time as a challenge in the deprescribing process since these comprehensive conversations with the patients are time consuming and may not be feasible in some clinical settings.
Lack of communication and inability to gain information from other relevant medical resources is another barrier perceived by the participants. Deprescribing is a multifaceted process and requires the cooperation of various medical specialties, which necessitates better communication at the organisational and personal level (Pereira & Veríssimo, Citation2023). The absence of a full profile of the patient medical condition can pose a potentially significant impediment to deprescribing (Akande-Sholabi et al., Citation2023). A research project in the United Arab Emirates assessed the knowledge, attitudes, and practices of community pharmacists regarding deprescribing, identifying numerous obstacles they encounter, including significant resistance from patients and insufficient resources (El-Dahiyat et al., Citation2023). This highlights the necessity for training workshops and enhanced interdisciplinary collaboration to enhance deprescribing methods to guarantee medication safety (El-Dahiyat et al., Citation2023; Nashwan et al., Citation2024).
Physicians believed that patients may not welcome a de-escalation in their medication. However, Gilpin et al. (Citation2022) revealed that hospital inpatients had positive attitudes toward deprescribing and did not interpret this process as abandoning them. To achieve that, the shared decision to deprescribe must involve the patients and their caregivers after informing them of potential benefits (Jansen et al., Citation2016). Unfortunately, this shared decision-making is not an easy process and engaging patients, especially the elderly, can be difficult and needs training, communication skills, and guidance which is not available (Bynum et al., Citation2014).
Most physicians reported that withdrawing medications prescribed by another clinician is an ethical challenge. This was also considered as a potential ethical barrier to deprescribing by Norton et al. (Citation2023) in 3000 primary care physicians who care for older adults with dementia. Physicians are more eager to deprescribe antibiotics initiated by themselves than when the therapy was initiated by others (Llor, Cordoba, et al., Citation2022). It is considered a ‘professional etiquette’ not to controvert the decision of another colleague and considered culturally unacceptable (Doherty et al., Citation2020). The participants in our study were young and mainly general practitioners, specialised and senior clinicians may be more confident in reassessing the decision of other colleagues and stopping unnecessary antibiotics.
Strengths of the study include the fact that this is the first study in Jordan to evaluate the knowledge and attitudes of physicians towards deprescribing since they are the main prescribers. The study provided an understanding of the challenges that face deprescribing process which must be addressed for successful implementation. Limitations include the relatively young age of the participating physicians, and more than half of participants were general practitioners which confines the representation of older, more experienced, and specialised physicians. The use of electronic forms through social media did not allow us to obtain a response rate. Another limitation is that attitudes are different than actual practice, despite the positive attitude we cannot anticipate similar behaviour in the real world.
Future work should assess the actual practice of deprescribing antibiotics, the guidelines used, and the clinical outcomes of this process. Additionally, assessing the predictors of antibiotic deprescribing practice whether related to the physician, the patient, or organisation can provide important information.
5. Conclusion
Physicians in Jordan are aware of the deprescribing process of antibiotics and recognise its benefits. Additionally, many received training in antibiotics deprescribing which provides a strong basis for the implementation of this process. However, deprescribing is a transverse process that requires the involvement of all healthcare professionals to insure a clear overall clinical picture of the patient and a rigorous follow up. Effective communication with the patients and their caregivers is also imperative to engage them in the process to achieve shared decisions. The challenges on the patient, physician, and organisational levels that must be addressed and requires the establishment of policies that guarantee the implementation of tools and guidelines for deprescribing.
Ethics approval and consent to participate
Ethical approval for the study was granted by the Institutional Review Board at the Applied Science Private University (Approval number: 2024-PHA-1). Electronic informed consent was obtained from all participants before the study participation.
Data availability and materials statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Authors’ contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Adedeji, W. A. (2016). The treasure called antibiotics. Annals of Ibadan Postgraduate Medicine, 14(2), 56–57.
- Akande-Sholabi, W., Ajilore, C. O., & Ilori, T. (2023). Evaluation of physicians’ knowledge of deprescribing, deprescribing tools and assessment of factors affecting deprescribing process. BMC Primary Care, 24(1), 31. https://doi.org/10.1186/s12875-023-01990-1
- Al-Taani, G., Al-Azzam, S., Karasneh, R. A., Ababneh, M., Al-Batayneh, O. B., Khader, Y. S., Conway, B. R., & Aldeyab, M. A. (2022). Antibiotic use and resistance: Information sources and application by dentists in Jordan. The Journal of Infection in Developing Countries, 16(10), 1607–1613. https://doi.org/10.3855/jidc.16540
- Al-Taani, G. M., Al-Azzam, S., Karasneh, R. A., Sadeq, A. S., Mazrouei, N. A., Bond, S. E., Conway, B. R., & Aldeyab, M. A. (2022). Pharmacists’ knowledge, attitudes, behaviors and information sources on antibiotic use and resistance in Jordan. Antibiotics, 11. https://doi.org/10.3390/antibiotics11020175
- AlRasheed, M. M., Alhawassi, T. M., Alanazi, A., Aloudah, N., Khurshid, F., & Alsultan, M. (2018). Knowledge and willingness of physicians about deprescribing among older patients: A qualitative study. Clinical Intervention in Aging, 13, 1401–1408. https://doi.org/10.2147/CIA.S165588
- Alsayed, A. R., Darwish El Hajji, F., Al-Najjar, M. A. A., Abazid, H., & Al-Dulaimi, A. (2022). Patterns of antibiotic use, knowledge, and perceptions among different population categories: A comprehensive study based in Arabic countries. Saudi Pharmaceutical Journal, 30(3), 317–328. https://doi.org/10.1016/j.jsps.2022.01.013
- Álvarez Artero, E., Campo Nuñez, A., Garcia Bravo, M., Cores Calvo, O., Belhassen Garcia, M., & Pardo Lledias, J. (2019). Urinary infection in the elderly. Revisita Clinica Espanola, 219(4), 189–193. https://doi.org/10.1016/j.rce.2018.10.009
- Aslam, B., Wang, W., Arshad, M. I., Khurshid, M., Muzammil, S., Rasool, M. H., Nisar, M. A., Alvi, R. F., Aslam, M. A., & Qamar, M. U. (2018). Antibiotic resistance: A rundown of a global crisis. Infection and Drug Resistance, 1645–1658. https://doi.org/10.2147/IDR.S173867
- Bynum, J. P., Barre, L., Reed, C., & Passow, H. (2014). Participation of very old adults in health care decisions. Medical Decision Making, 34(2), 216–230. https://doi.org/10.1177/0272989X13508008
- Conlon-Bingham, G. M., Aldeyab, M., Scott, M., Kearney, M. P., Farren, D., Gilmore, F., & McElnay, J. (2019). Effects of antibiotic cycling policy on incidence of healthcare-associated MRSA and Clostridioides difficile Infection in secondary healthcare settings. Emerging Infectious Diseases, 25(1), 52–62. https://doi.org/10.3201/eid2501.180111
- Cosgrove, S. E. (2006). The relationship between antimicrobial resistance and patient outcomes: Mortality, length of hospital stay, and health care costs. Clinical Infectious Diseases, 42(Suppl 2), S82–S89. https://doi.org/10.1086/499406
- Costelloe, C., Metcalfe, C., Lovering, A., Mant, D., & Hay, A. D. (2010). Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: Systematic review and meta-analysis. BMJ, 340(may18 2), cc2096. https://doi.org/10.1136/bmj.c2096
- Crisafulli, S., Poluzzi, E., Lunghi, C., Di Francesco, V., Pellizzari, L., Pasina, L., Elli, C., Trotta, F., Cangini, A., Trevisan, C., Zazzara, M. B., Onder, G., & Trifirò, G. (2022). Deprescribing as a strategy for improving safety of medicines in older people: Clinical and regulatory perspective. Frontiers in Drug Safety and Regulation, 2. https://doi.org/10.3389/fdsfr.2022.1011701
- Doherty, A. J., Boland, P., Reed, J., Clegg, A. J., Stephani, A. M., Williams, N. H., Shaw, B., Hedgecoe, L., Hill, R., & Walker, L. (2020). Barriers and facilitators to deprescribing in primary care: A systematic review. BJGP Open, 4(3), https://doi.org/10.3399/bjgpopen20X101096
- Doumat, G., Daher, D., Itani, M., Abdouni, L., El Asmar, K., & Assaf, G. (2023). The effect of polypharmacy on healthcare services utilization in older adults with comorbidities: A retrospective cohort study. BMC Primary Care, 24(1), 120. https://doi.org/10.1186/s12875-023-02070-0
- El-Dahiyat, F., Jairoun, A. A., Al-Hemyari, S. S., Shahwan, M., Hassan, N., Jairoun, S., & Jaber, A. A. S. (2023). Are pharmacists’ knowledge and practice the key to promoting deprescribing of potentially inappropriate medication: A missing link between treatment and outcomes. International Journal of Pharmacy Practice, 31(4), 387–395. https://doi.org/10.1093/ijpp/riad027
- Formica, D., Sultana, J., Cutroneo, P. M., Lucchesi, S., Angelica, R., Crisafulli, S., Ingrasciotta, Y., Salvo, F., Spina, E., & Trifirò, G. (2018). The economic burden of preventable adverse drug reactions: A systematic review of observational studies. Expert Opinion on Drug Safety, 17(7), 681–695. https://doi.org/10.1080/14740338.2018.1491547
- Fu, M., Gong, Z., Zhu, Y., Li, C., Zhou, Y., Hu, L., Li, H., Wushouer, H., Guan, X., & Shi, L. (2023). Inappropriate antibiotic prescribing in primary healthcare facilities in China: A nationwide survey, 2017-2019. Clinical Microbiology and Infection, 29(5), 602–609. https://doi.org/10.1016/j.cmi.2022.11.015
- Gilpin, R., McDade, O. C., & Edwards, C. (2022). Attitudes toward deprescribing for hospital inpatients. Clinical Medicine, 22(1), 58–62. https://doi.org/10.7861/clinmed.2021-0445
- Gould, K. (2016). Antibiotics: From prehistory to the present day. Journal of Antimicrobial Chemotherapy, 71(3), 572–575. https://doi.org/10.1093/jac/dkv484
- Gupta, S., Miller, R., Cahill, J. D., Gupta, S., Cahill, J., & Miller, R. (2019). 47C3Barriers to deprescribing: Origins and solutions. In S. Gupta, R. Miller, & J. D. Cahill (Eds.), Deprescribing in Psychiatry (p. 47). Oxford University Press.
- Hansen, M. P., Scott, A. M., McCullough, A., Thorning, S., Aronson, J. K., Beller, E. M., Glasziou, P. P., Hoffmann, T. C., Clark, J., & Del Mar, C. B. (2019). Adverse events in people taking macrolide antibiotics versus placebo for any indication. Cochrane Database of Systematic Reviews, 2019(1), Cd011825. https://doi.org/10.1002/14651858.CD011825.pub2
- Jansen, J., Naganathan, V., Carter, S. M., McLachlan, A. J., Nickel, B., Irwig, L., Bonner, C., Doust, J., Colvin, J., Heaney, A., Turner, R., & McCaffery, K. (2016). Too much medicine in older people? Deprescribing through shared decision making. BMJ, 353, i2893. https://doi.org/10.1136/bmj.i2893
- Karasneh, R. A., Al-Azzam, S. I., Ababneh, M. A., Basheti, I. A., Al-Azzeh, O., Al Sharie, S., Conway, B. R., & Aldeyab, M. A. (2021). Exploring information available to and used by physicians on antibiotic use and antibiotic resistance in Jordan. Antibiotics, 10(8). https://doi.org/10.3390/antibiotics10080963
- Kua, C. H., Mak, V. S., & Lee, S. W. H. (2019). Perspectives of health professionals towards deprescribing practice in Asian nursing homes: A qualitative interview study. BMJ Open, 9(10), e030106. https://doi.org/10.1136/bmjopen-2019-030106
- Llewelyn, M. J., Fitzpatrick, J. M., Darwin, E., SarahTonkin, C., Gorton, C., Paul, J., Peto, T. E. A., Yardley, L., Hopkins, S., & Walker, A. S. (2017). The antibiotic course has had its day. BMJ, 358, j3418. https://doi.org/10.1136/bmj.j3418
- Llor, C., & Bjerrum, L. (2014). Antimicrobial resistance: Risk associated with antibiotic overuse and initiatives to reduce the problem. Therapeutics Advances in Drug Safety, 5(6), 229–241. https://doi.org/10.1177/2042098614554919
- Llor, C., Cordoba, G., de Oliveira, S. M., Bjerrum, L., & Moragas, A. (2022). Antibiotic deprescribing: Spanish general practitioners’ views on a new strategy to reduce inappropriate use of antibiotics in primary care. European Journal of General Practice, 28(1), 217–223. https://doi.org/10.1080/13814788.2022.2130887
- Llor, C., Moragas, A., Bayona, C., Cots, J. M., Hernández, S., Calviño, O., Rodríguez, M., & Miravitlles, M. (2022). Efficacy and safety of discontinuing antibiotic treatment for uncomplicated respiratory tract infections when deemed unnecessary. A multicentre, randomized clinical trial in primary care. Clinical Microbiololgy and Infection, 28(2), 241–247. https://doi.org/10.1016/j.cmi.2021.07.035
- Lukacena, K. M., Keck, J. W., Freeman, P. R., Harrington, N. G., Huffmyer, M. J., & Moga, D. C. (2022). Patients’ attitudes toward deprescribing and their experiences communicating with clinicians and pharmacists. Therpeutic Advances in Drug Safety, 13, 204209862211164. https://doi.org/10.1177/20420986221116465
- Mahmood, R. K., Gillani, S. W., Alzaabi, M. J., & Gulam, S. M. (2022). Evaluation of inappropriate antibiotic prescribing and management through pharmacist-led antimicrobial stewardship programmes: A meta-analysis of evidence. European Journal of Hospital Pharmacy, 29(1), 2–7. https://doi.org/10.1136/ejhpharm-2021-002914
- Mohr, K. I. (2016). Current topics in microbiology and immunology of antibiotics research. Current Topics in Microbiololgy and Immunology, 398, 237–272. https://doi.org/10.1007/82_2016_499
- Nashwan, A. J., Barakat, M., Niaz, F., Tariq, S., Ahmed, S. K., & Tariq Sr, S. (2024). Antimicrobial resistance: Stewardship and one health in the eastern Mediterranean region. Cureus, 16(4).
- Nathan, C., & Cars, O. (2014). Antibiotic resistance–problems, progress, and prospects. New England Journal of Medicine England Journal of Medicine, 371(19), 1761–1763. https://doi.org/10.1056/NEJMp1408040
- Norton, J. D., Zeng, C., Bayliss, E. A., Shetterly, S. M., Williams, N., Reeve, E., Wynia, M. K., Green, A. R., Drace, M. L., Gleason, K. S., Sheehan, O. C., & Boyd, C. M. (2023). Ethical aspects of physician decision-making for deprescribing among older adults with dementia. JAMA Network Open, 6(10), e2336728. https://doi.org/10.1001/jamanetworkopen.2023.36728
- Okeowo, D. A., Zaidi, S. T. R., Fylan, B., & Alldred, D. P. (2023). Barriers and facilitators of implementing proactive deprescribing within primary care: A systematic review. International Journal of Pharmacy Practice, 31(2), 126–152. https://doi.org/10.1093/ijpp/riad001
- O'Mahony, D., O'Sullivan, D., Byrne, S., O'Connor, M. N., Ryan, C., & Gallagher, P. (2015). STOPP/START criteria for potentially inappropriate prescribing in older people: Version 2. Age and Ageing, 44(2), 213–218. https://doi.org/10.1093/ageing/afu145
- O'Neill, J. (2016). Tackling drug-resistant infections globally: Final report and recommendations.
- Page, A. T., Clifford, R. M., Potter, K., Schwartz, D., & Etherton-Beer, C. D. (2016). The feasibility and effect of deprescribing in older adults on mortality and health: A systematic review and meta-analysis. British Journal of Clinical Pharmacology, 82(3), 583–623. https://doi.org/10.1111/bcp.12975
- Pereira, A., & Veríssimo, M. (2023). Deprescribing in older adults: Time has come. European Geriatric Medicine, 14(1), 1–3. https://doi.org/10.1007/s41999-022-00716-3
- Read, A. F., & Woods, R. J. (2014). Antibiotic resistance management. Evolution, Medicine, and Public Health, 2014(1), 147. https://doi.org/10.1093/emph/eou024
- Reeve, E., Thompson, W., & Farrell, B. (2017). Deprescribing: A narrative review of the evidence and practical recommendations for recognizing opportunities and taking action. European Journal of Internal Medicine, 38, 3–11. https://doi.org/10.1016/j.ejim.2016.12.021
- Rodrigues, T., Roque, A., Falcao, F., Figueiras, A., Herdeiro, A., & T, M. (2013). Understanding physician antibiotic prescribing behaviour: A systematic review of qualitative studies. International Journal of Antimicrobial Agents, 41(3), 203–212. https://doi.org/10.1016/j.ijantimicag.2012.09.003
- Scott, I., Anderson, K., & Freeman, C. (2017). Review of structured guides for deprescribing. European Journal of Hospital Pharmacy, 24(1), 51–57. https://doi.org/10.1136/ejhpharm-2015-000864
- Spellberg, B., Bartlett, J. G., & Gilbert, D. N. (2013). The future of antibiotics and resistance. New England Journal of Medicine, 368(4), 299–302. https://doi.org/10.1056/NEJMp1215093
- Tabachnick, B. G., & Fidell, L. S. (2006). Using multivariate statistic (5th ed.). Allyn and Bacon Inc.
- Taber, K. S. (2018). The use of Cronbach’s Alpha when developing and reporting research instruments in science education. Research in Science Education, 48(6), 1273–1296. https://doi.org/10.1007/s11165-016-9602-2
- Tanwar, J., Das, S., Fatima, Z., & Hameed, S. (2014). Multidrug resistance: An emerging crisis. Interdisciplinary Perspectives on Infectious Disease, 2014, 541340. https://doi.org/10.1155/2014/541340
- Thompson, W., Lundby, C., Graabaek, T., Nielsen, D. S., Ryg, J., Søndergaard, J., & Pottegård, A. (2019). Tools for deprescribing in frail older persons and those with limited life expectancy: A systematic review. Journal of the American Geriatrics Society, 67(1), 172–180. https://doi.org/10.1111/jgs.15616
- Urbiztondo, I., de Oliveira, S. M., Hernández-Flores, N., Caballero, L., Suarez, M. A., Bjerrum, L., & Cordoba, G. (2018). General practitioners’ views on the acceptability and applicability of using quality indicators as an intervention to reduce unnecessary prescription of antibiotics in four South American countries. Antibiotics (Basel), 7(3), https://doi.org/10.3390/antibiotics7030057
- Van Boeckel, T. P., Brower, C., Gilbert, M., Grenfell, B. T., Levin, S. A., Robinson, T. P., Teillant, A., & Laxminarayan, R. (2015). Global trends in antimicrobial use in food animals. Proceeding of the National Academy of Sciences, 112(18), 5649–5654. https://doi.org/10.1073/pnas.1503141112
- Ventola, C. L. (2015). The antibiotic resistance crisis: Part 2: Management strategies and new agents. Pharmacy and Therapeutics, 40(5), 344–352. https://www.ncbi.nlm.nih.gov/pubmed/25987823
- Woodford, H. J., & Fisher, J. (2019). New horizons in deprescribing for older people. Age and Ageing, 48(6), 768–775. https://doi.org/10.1093/ageing/afz109
- Wu, H., Kouladjian, O., Donnell, L., Fujita, K., Masnoon, N., & Hilmer, S. N. (2021). Deprescribing in the older patient: A narrative review of challenges and solutions. International Journal of General Medicine, 14, 3793–3807. https://doi.org/10.2147/IJGM.S253177
