ABSTRACT
Percutaneous nephrolithotomy (PCNL) is the treatment of choice for pediatric nephrolithiasis more than 20 mm. Prone position was the preferred position for decades. Recently, supine position has gained more interest. This meta-analysis aims to evaluate the safety and efficacy of PCNL in supine versus prone position in pediatric population. A systematic search of PubMed, Scopus, Web of Science, and Cochrane Library was performed till 28 February 2024. The study included comparative studies comparing both positions in children that were written in English. A total of three randomized studies and three retrospective studies were included with a total number of 290 patients. Cochrane risk-of-bias tool for randomized trials was used for quality assessment, while Newcastle–Ottawa scale was used for non-randomized controlled trials. The meta-analysis was conducted using Review Manager software. Numerical data were analyzed using standardized mean difference (SMD), while the risk ratio was used for analysis of categorical data. Fixed or random effects models were used according to heterogeneity. There were statistically insignificant differences between both groups for stone-free rate (RR 1.08, 95% CI [0.98–1.18], p = 0.11) and overall complications (RR 0.93, 95% CI [0.59–1.47], p = 0.76). Operation time was significantly shorter in supine group (SMD −0.99, 95% CI [−1.67 to −0.30], p = 0.005). Therefore, comparable efficacy and safety outcomes were proved between both supine and prone positions for PCNL in pediatrics.
Introduction
PCNL has been established as a gold standard minimally invasive procedure for treatment of pediatric nephrolithiasis more than 20 mm [Citation1]. PCNL has been performed in the prone, but the supine position has proven to be a good option with a number of benefits [Citation2]. The first publication of supine PCNL in pediatrics was through the report of Clinical Research Office of the Endourological Society (CROES), where 12% of included pediatric patients were performed in supine position [Citation3].
Prone position gained its popularity as it provides a wider surface area, a more distended pelvicalyceal system, and easier identification of renal anatomy which led to easier puncture [Citation4]. However, it can have some disadvantages too. It requires changing of position after ureteral catheter fixation. Also, it has its drawbacks for anesthesia, especially in patients with cardiac and pulmonary diseases or those who are obese [Citation5].
On the other hand, the supine position is easier for ventilation and carries a lower risk for anesthesia, which is relevant especially in children [Citation6]. In addition, there is no need for repositioning, and it allows simultaneous use of ureteroscopy, which can be helpful in management of complex stones. However, it has some drawbacks like limiting the surface area for puncture that can increase the risk of trauma to intrarenal vessels [Citation7].
Given those controversies between the two positions, the debate over the advantages and limitations of both approaches and which one is better will continue. This meta-analysis aims to compare the efficacy and safety of supine versus prone PCNL in pediatric population.
Methods
Search strategy
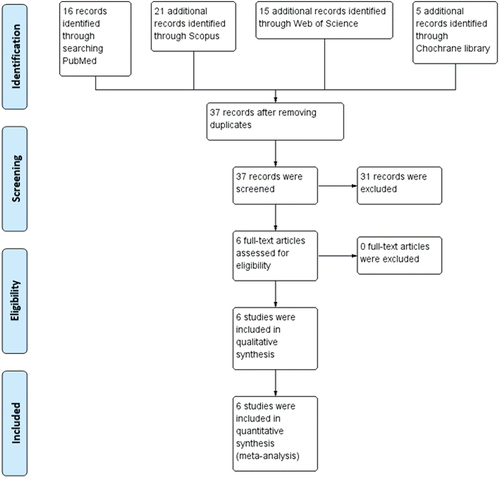
A literature search was carried out through PubMed, Scopus, Web of science and Cochrane library for studies comparing supine and prone PCNL in pediatric population till 28 February 2024. The search strategy included the following terms: Supine AND Prone AND (‘Percutaneous Nephrolithotomy’ OR ‘PCNL’) AND (‘child*’ OR ‘Pediatric’). Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for conducting meta-analyses were followed [Citation8].
Inclusion criteria
Inclusion criteria included comparative studies written in English, comparing prone and supine PCNL in pediatric patients, and reporting efficacy and safety outcomes.
Data extraction and quality assessment
Endnote X8 (Clarivate Analytics, London, UK) was used for duplicate removal then the Rayyan web application was used for screening [Citation9]. Data extraction was done using Microsoft Excel. The extracted data were publication year, number of patients in each arm, patients’ characteristics, stone characteristics, operative data, outcomes, and complications. The Cochrane risk-of-bias tool for randomized trials [Citation10] was used for quality assessment of RCT. The Newcastle–Ottawa Scale (NOS) was used for quality assessment of non-RCT [Citation11].
Statistics
Review Manager software (Cochrane Collaboration, Oxford, UK) was used for statistical analysis. Continuous data were analyzed using standardized mean difference (SMD) with 95% confidence interval (CI), while the risk ratio (RR) was used for analysis of dichotomous data. Heterogeneity was evaluated with the chi-square test. If heterogeneity was detected, a sensitivity analysis in multiple scenarios, excluding one study in each scenario was conducted. A p < 0.1 was considered significant. Random or fixed effects models were used according to heterogeneity. A p value of <0.05 was used to indicate statistical significance.
Results
Search strategy and screening results are shown in the PRISMA flow chart (). Six studies were included in the meta-analysis: three RCT [Citation12–14] and three retrospective comparative studies [Citation15–17]. Risk of bias assessment results for RCT are shown in , while risk of bias assessment for non-RCT is shown in .
Figure 2. Risk of bias summary: review authors’ judgements about each risk of bias item for included randomized controlled trials.
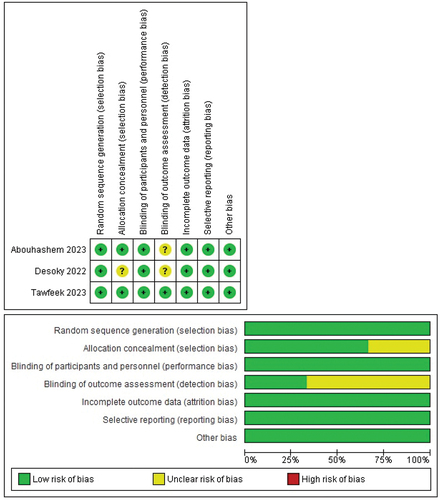
Table 1. Quality assessment of non-randomized controlled trials.
shows the characteristics of the included studies, which contained 290 patients. shows patients and stone characteristics. In all studies, fluoroscopy was used for gaining percutaneous renal access except two studies [Citation15,Citation17] where ultrasound and fluoroscopy were used. Mini-PCNL was used in five studies, with a percutaneous sheath size of 16 F in two studies [Citation13,Citation14], 14–18 F in one [Citation17], 15–20 F in one [Citation15], and 14–20 F in one, while ultra-mini-PCNL of 13 F was used in one [Citation12]. Holmium Laser lithotripsy was used for stone disintegration in all studies.
Table 2. Characteristics of the included studies.
Table 3. Patients and stone characteristics.
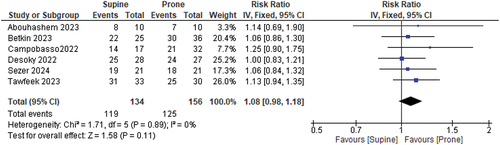
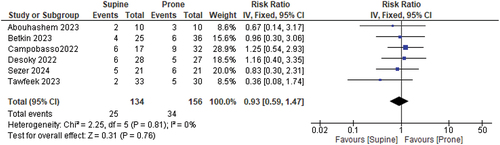
Stone-free rate
Stone-free rate was defined as no residual stones >4 mm in all studies except one [Citation15] where residual fragments ≤3 mm were considered clinically insignificant. KUB and ultrasound were used for the detection of residual stones in two studies [Citation12,Citation14], KUB only was used in one [Citation17], KUB and NCCT were used in one [Citation13] and KUB, ultrasound, and NCCT in one [Citation15].
The overall risk ratio between supine and prone was comparable (RR 1.08, 95% CI [0.98–1.18], p = 0.11). Pooled studies were homogeneous (Chi-square p = 0.89, I-square = 0%) ().
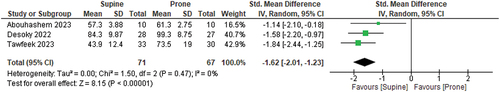
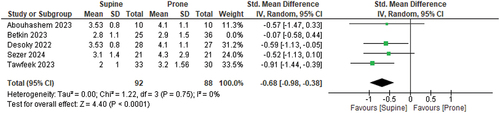
Operative time
The overall SMD between supine and prone groups favored supine (SMD −0.99, 95% CI [−1.67 - −0.30], p = 0.005). Pooled studies were heterogeneous (Chi-square p < 0.00001, I-square = 86%).
Heterogeneity was resolved by excluding the three non-RCTs [Citation15–17] (p = 0.2, I-square = 0%). After removing them from the meta-analysis model, the overall SMD was still in favor of supine PCNL (SMD −1.62, 95% CI −2.01 to −1.23, p < 0.00001) ().
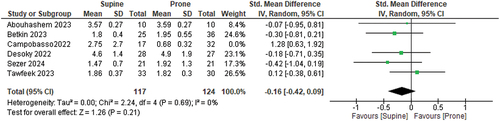
Fluoroscopy time
The overall SMD between supine and prone was comparable (SMD 0.06, 95% CI [−0.41–0.53], p = 0.80). Pooled studies were heterogeneous (Chi-square p = 0.002, I-square = 73%).
Heterogeneity was resolved by excluding Campobasso 2022 [Citation15] (p = 0.69, I-square = 0%). After removing it from the meta-analysis model, the overall SMD was still insignificant (SMD −0.16, 95% CI −0.42 to 0.09, p = 0.21) ().
Length of hospital stay
Hospital stay was reported in all studies except one [Citation15]. The overall SMD between supine and prone groups favored supine (SMD −0.52, 95% CI [−0.87 to −0.26], p < 0.0001). Pooled studies were heterogeneous (Chi-square p = 0.27, I-square = 23%).
Heterogeneity was resolved by excluding Bitkin 2023 [Citation17] (p = 0.75, I-square = 0%). After removing it from the meta-analysis model, the overall SMD was still in favor of supine PCNL (SMD −0.68, 95% CI −0.98 - −0.38, p < 0.0001) ().
Complications
The overall risk ratio of complications between supine and prone was comparable (RR 0.93, 95% CI [0.59–1.47], p = 0.76) (). Pooled studies were homogenous (Chi-square p = 0.81, I-square = 0%).
Sensitivity analysis
When only RCTs [Citation12–14] were included for sensitivity analysis, similar results were obtained in all outcomes. Therefore, the results are considered stable ().
Table 4. Sensitivity analysis of randomized controlled trials.
Discussion
Prone PCNL has been performed for years. It has been familiar for urologists, and it provides wider operative field and adequate pelvicalyceal system. However, it has its issues, especially in children as it can be difficult to observe a child in a prone position by anesthesiologist [Citation18]. Recently, supine PCNL has gained more interest, most probably because of being more comfortable for surgeons and no need for repositioning the patient in addition to the ability to do combined intrarenal surgery [Citation19]. It is very important to keep in mind that supine PCNL is still a new technique for most urologists that needs a learning curve.
Our meta-analysis revealed comparable results in stone-free and complication rates between supine and prone PCNL. While operative time and length of hospital stay was shorter in the supine position. This ensures that supine PCNL is a safe and effective approach.
Even though prone PCNL can give a better stone-free rate due to full exposure of the lumbar area allowing multiple puncture sites and better access to the upper pole [Citation20], our meta-analysis showed no difference in stone-free rate between both positions.
Results of meta-analyses conducted to compare supine and prone PCNL in adults showed controversial results. A study by Yuan showed a higher stone-free rate in prone position [Citation21]. This was explained by the more space available for manipulation of the nephroscope in prone position in addition to some difficulties with following migratory stones in supine PCNL as well as difficulties with upper pole access. Another meta-analysis [Citation22] in adults concluded a comparable stone-free rate. Furthermore, a meta-analysis of RCT in adults showed a comparable stone-free rate between the two positions [Citation23].
The need to change position after ureteral catheter fixation of prone PCNL usually prolongs the operation time. Our study confirmed this with statistically significant shorter operation time in supine position than in prone one. This is consistent with the results of a meta-analysis comparing the two positions in adults, which also showed longer operative time in prone position [Citation21].
The overall complications showed no difference between the two positions. However, reporting complications was not detailed in our studies with different definitions and scales used. We believe that using a standardized approach for reporting complications like the modified Clavien–Dindo classification would give better evidence and data [Citation24].
Supine pediatric PCNL has some potential advantages. The surgeon is working while sitting, the anesthetist had easier monitoring of the endotracheal tube, and the child is subjected to less manipulation in repositioning [Citation25]. Nevertheless, supine position is still less familiar for many urologists, and there is a smaller operative field with possible hypermobility of the kidney during tract dilatation [Citation26].
It is worth mentioning that several limitations should be considered. There is a paucity of randomized controlled trials in the literature comparing supine and prone PCNL in pediatric population. In addition, sample size was small in one study [Citation13]. Different stone characteristics, surgeons’ experience, supine position, PCNL techniques in addition to some non-detailed data on outcomes and complications could also be a shortcoming.
Finally, assessment of outcomes in all studies was done using objective measures like stone-free rate. We can consider this as a limitation as there has been a paradigm shift in the last few years toward subjective measures of outcomes which are important to ensure delivery of care in a patient centered manner [Citation27]. New grading systems and nomograms have been developed in endourology such as tools for predicting stone recurrence and tools related to postoperative complications [Citation28]. In addition, artificial intelligence and machine learning have been used to build algorithms to predict outcomes of PCNL [Citation29].
Conclusions
Supine PCNL showed comparable stone-free and complication rates with prone PCNL in children. Longer operative time was observed in prone PCNL. Therefore, no technique has its absolute superiority with each one having its own advantages and disadvantages. Additionally, more prospective randomized controlled trials are needed in pediatric populations for better conclusions.
Abbreviations
| CI | = | confidence interval |
| cm | = | centimeter |
| HU | = | Hounsfield unit |
| KUB | = | Kidney, Ureter, and Bladder X-ray |
| mm | = | millimeter |
| N. | = | number |
| NCCT | = | non-contrast computerized tomography |
| PCNL | = | Percutaneous Nephrolithotomy |
| PRISMA | = | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| RCT | = | Randomized controlled trial |
| RR | = | risk ratio |
| SD | = | standard deviation |
| SMD | = | standardized mean difference |
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Lao M, Kogan BA, White MD, et al. High recurrence rate at 5-year followup in children after upper urinary tract stone surgery. J Urol. 2014;191(2):440–444. doi: 10.1016/j.juro.2013.09.021
- Valdivia Uría JG, Valle Gerhold J, López López JA, et al. Technique and complications of percutaneous nephroscopy: experience with 557 patients in the supine position. J Urol. 1998;160(6 Part 1):1975–1978. doi: 10.1016/S0022-5347(01)62217-1
- Guven S, Frattini A, Onal B, et al. Percutaneous nephrolithotomy in children in different age groups: data from the clinical research office of the endourological society (CROES) percutaneous nephrolithotomy global study. BJU Int. 2013;111(1):148–156. doi: 10.1111/j.1464-410X.2012.11239.x
- Dogan HS, Kilicarslan H, Kordan Y, et al. Percutaneous nephrolithotomy in children: does age matter? World J Urol. 2011;29(6):725–729. doi: 10.1007/s00345-011-0692-1
- de la Rosette Jjmch, Tsakiris P, Ferrandino MN, et al. Beyond prone position in percutaneous nephrolithotomy: a comprehensive review. Eur Urol. 2008;54(6):1262–1269. doi: 10.1016/j.eururo.2008.08.012
- Ozdemir H, Erbin A, Sahan M, et al. Comparison of supine and prone miniaturized percutaneous nephrolithotomy in the treatment of lower pole, middle pole and renal pelvic stones: a matched pair analysis. Int Braz J Urol. 2019;45(5):956–964. doi: 10.1590/s1677-5538.ibju.2019.0049
- Steele D, Marshall V. Percutaneous nephrolithotomy in the supine position: a neglected approach? J Endourol. 2007;21(12):1433–1438. doi: 10.1089/end.2006.0375
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339(jul21 1):b2700. doi: 10.1136/bmj.b2700
- Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4
- Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898
- Luchini C, Stubbs B, Solmi M, et al. Assessing the quality of studies in meta-analyses: advantages and limitations of the Newcastle Ottawa Scale. WJG. 2017;5(4):80. doi: 10.13105/wjma.v5.i4.80
- Desoky EAE, Sakr AM, ElSayed ER, et al. Ultra-mini-percutaneous nephrolithotomy in flank-free modified supine position vs prone position in treatment of pediatric renal pelvic and lower caliceal stones. J Endourol. 2022;36(5):610–614. doi: 10.1089/end.2021.0557
- Abouhashem S, Almednini M, Abdelfattah E, et al. Prone versus flank-free modified supine position mini percutaneous nephrolithotomy in pediatric age group. Zagazig Univ Med J. 2023;29:293–299.
- Tawfeek AM, Arafa H, Higazy A, et al. Is supine a preferred position for percutaneous nephrolithotomy in the pediatric age group? A randomized controlled study. Minerva Urol Nephrol. 2024;76(1):81–87. doi: 10.23736/S2724-6051.23.05496-4
- Campobasso D, Bocchialini T, Bevilacqua L, et al. Comparison between prone and supine nephrolithotomy in pediatric population: a double center experience. Int Urol Nephrol. 2022;54(12):3063–3068. doi: 10.1007/s11255-022-03341-y
- Sezer A, Turedi B, Guzel R, et al. Comparison of two centers’ experience in pediatric supine and prone miniaturized percutaneous nephrolithotomy with propensity match analysis. J Endourol. 2024;38:121–128. doi: 10.1089/end.2023.0278
- Bitkin A, Özlü DN, Ekşi M, et al. A comparative analysis of the efficacy and safety of mini-percutaneous nephrolithotomy performed in the supine and prone positions for the treatment of pediatric kidney stones: a single-center experience. Urolithiasis. 2023;51(1):122. doi: 10.1007/s00240-023-01497-5
- Pelosi P, Croci M, Calappi E, et al. The prone positioning during general anesthesia minimally affects respiratory mechanics while improving functional residual capacity and increasing oxygen tension. Anesth Analg. 1995;80(5):955–960. doi: 10.1213/00000539-199505000-00017
- Miano R, Scoffone C, De Nunzio C, et al. Position: prone or supine is the issue of percutaneous nephrolithotomy. J Endourol. 2010;24(6):931–938. doi: 10.1089/end.2009.0571
- Karaolides T, Moraitis K, Bach C, et al. Positions for percutaneous nephrolithotomy: thirty-five years of evolution. Arab J Urol. 2012;10(3):307–316. doi: 10.1016/j.aju.2012.06.005
- Yuan D, Liu Y, Rao H, et al. Supine versus prone position in percutaneous nephrolithotomy for kidney calculi: a meta-analysis. J Endourol. 2016;30(7):754–763. doi: 10.1089/end.2015.0402
- Liu L, Zheng S, Xu Y, et al. Systematic review and meta-analysis of percutaneous nephrolithotomy for patients in the supine versus prone position. J Endourol. 2010;24(12):1941–1946. doi: 10.1089/end.2010.0292
- Li J, Gao L, Li Q, et al. Supine versus prone position for percutaneous nephrolithotripsy: a meta-analysis of randomized controlled trials. Int J Surg. 2019;66:62–71. doi: 10.1016/j.ijsu.2019.04.016
- Tefekli A, Ali Karadag M, Tepeler K, et al. Classification of percutaneous nephrolithotomy complications using the modified clavien grading system: looking for a standard. Eur Urol. 2008;53(1):184–190. doi: 10.1016/j.eururo.2007.06.049
- Nerli R, Mungarwadi A, Ghagane S, et al. Supine percutaneous nephrolithotomy in children. J Sci Soc. 2018;45(2):63. doi: 10.4103/jss.JSS_24_18
- Hopper KD, Sherman JL, Luethke JM, et al. The retrorenal colon in the supine and prone patient. Radiol. 1987;162(2):443–446. doi: 10.1148/radiology.162.2.3797658
- Mehmi A, Jones P, Somani BK. Current status and role of patient-reported outcome measures (PROMs) in endourology. Urology. 2021;148:26–31. doi: 10.1016/j.urology.2020.09.022
- Jones P, Pietropaolo A, Chew BH, et al. Atlas of scoring systems, grading tools, and nomograms in endourology: a comprehensive overview from the TOWER endourological society research group. J Endourol. 2021;35(12):1863–1882. doi: 10.1089/end.2021.0124
- Geraghty RM, Thakur A, Howles S, et al. Use of temporally validated machine learning models to predict outcomes of percutaneous nephrolithotomy using data from the British association of urological surgeons percutaneous nephrolithotomy audit. Eur Urol Focus. 2024. doi: 10.1016/j.euf.2024.01.011