ABSTRACT
Small group discussion (SGD) is a well-known educational method to promote active learning. Best practices for running SGDs in face-to-face events are described in the literature; however, little has been reported regarding synchronous online delivery. The aim of this study was to determine learner and instructor preferences for online SGDs in terms of group size and composition and to formulate best practices based on participant and faculty feedback. We designed an 8-module online course for surgeons managing upper extremity trauma. Participants were pre-assigned into 2 types of group: 1 faculty with 5 participants or 2 faculty with 8 participants. We collected feedback from 91 participants and 34 faculty over the 8 weeks in multiple ways. Participants preferred way to run an online SGD is to have 2 faculty with 4–5 participants (80%), rotating to different faculty every week (67%), and interacting with peers from different countries (95%). Pre-course assessment questions and pre-recorded presentations enhanced the online discussions for 82%. From open text comments, we identified that cases/content, faculty, participant engagement, and technical support worked well. The course could be improved by adding more extensive technical and connectivity checks, having a different time scheduling, and integrating more supporting materials.
Introduction
Orthopaedic and general trauma surgeons are encouraged to maintain their knowledge and keep their daily practice up to date and many continuing medical education (CME) and continuing professional development (CPD) programmes help fulfill this need. Traditionally, these are organised as face-to-face courses [Citation1]. The ability to meet and discuss cases with international expert faculty is a feature of many courses [Citation2]. In 2020, however, most on-site educational activities could not take place due to the exceptional Covid-19 circumstances, and many organisations explored online activities instead. [Citation2–4] To respond to the short-term educational gaps of surgeons in the area of upper extremity trauma, the “AO Trauma Online Course – Upper Extremity (Small Group Discussions)” was delivered. The programme consisted of 8 case-based online synchronous small group discussions (SGDs) and was developed based on the existing Upper Extremity curriculum and course.
The AO Foundation is a medically-guided non-profit organisation that concentrates on education, innovation, and research to treat musculoskeletal trauma and disorders [Citation2]. For several years, small group discussions have been an integral part of AO courses. By discussing fracture management principles in small groups using clinical cases, participants can review their knowledge, exchange experiences, gain new insights, and learn about new approaches and techniques [Citation5,Citation6]. Case-based discussion is a generally accepted learning tool for adult education [Citation5,Citation7–9]. SGDs typically consist of 6 to 10 participants in a semicircle face-to-face environment with a computer and projector and moderated by 2 faculty. [Citation10] Face-to-face SGDs vary between 45 and 90 minutes to present and discuss 3 to 6 clinical cases. The expert faculty promote active participation and evidence-based discussions. The goal is to apply the information from lectures and integrate the participants’ experiences in clinical cases. [Citation2,Citation7]
The “AO Principles of teaching and learning” book [Citation11] was published to present best practices in all areas including small group and case-based discussions, and data were collected from the face-to-face SGDs over many years [Citation2]. However, there are limited publications reporting the learning quality and outcome of online versions of these SGDs.
Some studies have compared online education in general (not SGDs) to traditional education. These showed a wide range of educational designs with varying educational value [Citation12,Citation13]. Some demonstrate that online postgraduate education enhances active group participation and helps acquire information and skills. For our target population of experienced surgeons and residents, this mode of CME can thus be considered a good option. [Citation1,Citation5,Citation13–15]
Studies comparing face-to-face with online small group discussions in a postgraduate setting are scarce. Ryan et al. demonstrated that an online CME course for pharmacists, based on small group discussions and case-based learning, was as effective as the face-to-face mode [Citation1]. The advantages and disadvantages of online case-based interactions were reported by Palan et al in an asynchronous forum format [Citation8]. King et al. found that online synchronous problem-based learning in an interprofessional health science course might be beneficial [Citation15]. A practice session for both faculty and participants to overcome technical issues before starting a module is recommended and the importance of good communication online must be emphasised (since nonverbal communication is limited) [Citation15,Citation16]. Another advantage of online courses is the possibility of a worldwide interaction without the need for travelling [Citation16].
The scarcity of published literature on online SGDs led us to design this educational research project around the AO Trauma Online Course – Upper Extremity (Small Group Discussions). This study aimed to define learner and faculty preferences in online SGDs in terms of group size, faculty to participant ratio, the number of modules and cases, and the technical and educational prerequisites to achieve the desired learning outcomes. Furthermore, we wanted to identify the main difficulties in running live (synchronous) online SGDs with participants and faculty from many countries and to formulate best practices.
Material and Methods
Course Description and Delivery
The AO Trauma Online Course – Upper Extremity (Small Group Discussions) was delivered free of charge as a series of 8 modules, with each one covering 1 anatomical region from the existing AO Trauma Upper Extremity course (clavicle, scapula, proximal humerus, etc.). Participants learned the current patient management of pain, dysfunction, deformity, and cosmesis related to the upper limb’s trauma, including fractures from the sternoclavicular joint to the fingertip. Each week consisted of a 10-minute overview presentation on that week’s topic followed by a set of 3 or 4 prepared cases to be discussed online for 75 minutes. Each case is designed to contain a patient presentation with x-rays, CT scans, a diagnosis section, treatment options, the outcome of the case, and a wrap-up to reinforce the take-home messages. From week 3 onwards, the overview presentations were pre-recorded and available before the module to allow the full 90 minutes for discussion. All materials and links were provided through the course home page in the learning management system (Totara Talent Experience Platform https://www.totaralearning.com/en/products/learning-management-system).
For course delivery, AO compared different online platforms that provide breakout sessions, show multimedia content, provide drawing tools on a presentation, and have high efficiency even with slow bandwidth connections. The New Row Virtual classroom software (from Kaltura, New York https://www.newrow.com/virtual-classroom/) was selected for many events in 2020 and a faculty training plan was developed.
The course was delivered each Wednesday from 6:30 to 8 P.M. Central European Summer Time in September and October 2020, hosted by a technical expert who managed access to the 15 breakout rooms. Experienced international faculty moderated the small groups.
The target audiences were orthopaedic and trauma surgeons and trainees from the Middle East, Africa, and Europe who had at least 3 years of experience and were comfortable discussing cases in English. The technical prerequisites included a webcam, a headset microphone, and a good internet connection. To receive a certificate of completion, participants must attend at least 7 of the 8 modules.
Faculty Selection and Training
34 experienced faculty from the Middle East, Africa, Europe, North and South America volunteered for one or more modules based on their practice and expertise. Each module had an appointed moderator who delivered the overview presentation and selected and finalised 3 or 4 cases from the curriculum. The other faculty were assigned as a case presenter and a small group moderator each week, either on their own or as a pair.
Two weeks before the course started, a 90-minute faculty training session was organised to familiarise everyone with the software, to review the cases, and to agree on the key messages and the learning outcomes. Before each module, a 30-minute faculty meeting was held to ensure the connection was stable, to clarify general and case-specific questions, to review recommendations following the previous week experiences, and to remind everyone of the key points for the case discussion and software use.
Study Design
Participants were pre-assigned into 1 of 2 group structures each week; either 1 faculty with 5 participants or 2 faculty with 8 participants (participants were allocated with surgeons from other hospitals, countries, and regions as much as possible). Participants stayed in the same group for the first 4 weeks and were randomly re-allocated each week for the last 4 sessions. The grouping was not always consistent because participants did not attend all the modules and some new participants registered between weeks 2 and 5. Therefore, we introduced a questionnaire to address the specific issues related to group size and composition. In addition, we conducted 4 dual-moderator focus groups with 7 volunteer participants and 8 volunteer faculty.
Data Collection
Participants received our standard evaluation and assessment questions (7 pre-event and 12 post-event) through SurveyMonkey [Citation17] . In addition, before the course they completed a series of multiple-choice questions (MCQs) presenting decision and management options for clinical scenarios. Feedback was provided on the correct and incorrect answers, along with rationale and references. Faculty also completed the MCQs to become familiar with and align with the content and core messages. The same MCQs were administered after the completion of the course to determine pre-intervention versus post-intervention knowledge improvement.
Weekly feedback was collected after each session, asking to rate content usefulness, faculty performance, and to suggest improvements.
After module 7, participants and faculty received a questionnaire asking about the online experience, the course structure, group size and composition, and their preferences for the future (Appendix 1). The questionnaire included items about the comparison of online experience to face-to-face events, the length of the course with respect to duration per module and the whole set of modules, whether the pre-course questions and the pre-recorded presentations enhanced the online discussions, the preference of the group composition with 1 or 2 faculties, and the best rotation plan for faculty and participants. We also asked “What went well overall?” and “What could we do differently next time?”. Answers were collected to find out if interaction with peers from other countries was relevant, if the online version of this course should stop once the face-to-face meetings are possible again, and if the participants would join an online course like this again.
All data were captured into our management information system and our standard reports were generated and shared with the chairpersons and moderators. All individual responses were anonymised and then exported as a csv-file.
Data Analysis Was Performed with Excel Software
In 4 online focus group meetings, organised after the second and the seventh modules, we collected experiences and recommendations from 8 faculty and 7 volunteer participants.
Results
The course was attended by 91 participants from 37 different countries located in Europe, Africa, and the Middle East (). Participants had a wide range of expertise and experience levels and showed good motivation to learn for all competencies (). 10 participants attended all 8 modules, 22 attended 6 or 7 modules, 32 attended 3 to 5 modules, and 27 attended 1 or 2 modules. On average 50 participants attended the modules each week (range from 38 to 58) supported by 12–18 faculty. The most frequently reported reasons participants did not attend every week were their operating room or work schedule (40%), poor network access (14%), and time of the day was not suitable (12%). 28 participants viewed 5 or more of the pre-recorded overview presentations, while 47 viewed between 1 and 4.
Table 1. Profiles of registered participants obtained from the pre-event standard questionnaire
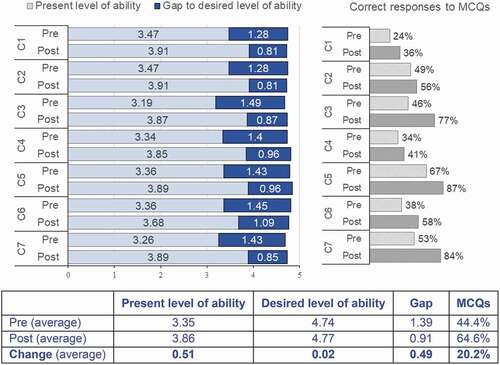
61 of the 91 participants who attended at least one module completed our standard pre- and post-event evaluation and assessment forms [Citation17]. 47 participants completed both pre-and post-course multiple choice assessment questions and showed an average reduction in their gaps (between desired and present level of ability) of 0.49 and their knowledge improved significantly (20% gain, average pre- 44% and post-event 64%) (). On a Likert scale 1–5 (1 lowest and 5 = highest) the average educational impact was 4.72, the objectives met was 4.34, content usefulness was 4.16, faculty effectiveness was 4.21, online venue was 3.49, lack of bias was 4.57, and “recommend the event to colleagues” was 100%. Taken together and compared to the ratings obtained by our face-to-face courses (), these results suggest that the online SGDs were an effective way to deliver educational content for most participants.
Table 2. Comparison of post-course standard evaluation ratings (on a 1 to 5 Likert scale) of face-to-face upper extremity course in 2019 and online offerings in 2020 (in grey the 8 consecutive weeks course)
Figure 1. Pre- and post-course motivation to learn (difference between present and desired level of ability on a 1 to 5 Likert scale) per competency (C) and pre- and post-course knowledge test (multiple-choice questions MCQs)
To define learner and instructor preferences in online SGDs in terms of group size and composition, we asked participants and faculty to complete a short evaluation after each module. We compared the ratings obtained in the 2 experimental groups: 1 faculty with 5 participants, and 2 faculty with 8 participants (). However, none of the parameters analysed showed consistent or significant differences between the 2 groups due to confounders and variable results from week to week (technical problems with connections of participants and faculty, non-attendance of participants in some groups, etc.).
Table 3. Content (cases) and online experience ratings on a 1 to 5 Likert scale for the 8 modules (by subgroup)
We then administered a post-course questionnaire specifically created to address these points and this was completed by 56 participants and 31 faculty. Regarding the group size and composition, 80% of the participants reported that their preferred way to run an online small group discussion is 2 faculty with 4–5 participants. Faculty had almost equal preferences for 2 faculty with 8 participants (83%) and 1 faculty with 4–5 participants (74%) (). The opportunity to interact with colleagues from other countries was appreciated by 95% of participants and 97% of faculty. 67% of participants and 52% of faculty prefer faculty to rotate to a different group every week, while both participants and faculty had almost equal preferences for participants moving to a new group every week and for staying in a fixed group for 4 weeks then switching for 4 more ().
Table 4. Combined results of the post-course questionnaire. N = 56 participants (62% completion rate) and n = 31 faculty (91% completion rate)
Concerning the online course format, 90 minutes for each module was considered adequate for discussing 3 cases for 83% of the participants and 78% of faculty (). 8 consecutive weeks made the online course too long for 46% of participants and 51% of faculty. The pre-course MCQs and pre-recorded presentations enhanced the online discussions for 82% of participants and 81% of faculty (). 85% of participants and 74% of faculty would join an online course like this again, while 26% and 15% respectively would join if some changes were made. 14% of participants and 12% of faculty think that small group discussions online should stop once face-to-face education can resume, which means the vast majority would like the online option to continue. Finally, their level of agreement with the statement “When all the technical issues are addressed, online small group discussions can run just as well as in a face-to-face environment” was 76% for participants (31% agreed strongly and 45% agreed) and 49% for faculty (10% agreed strongly and 39% agreed).
To gain a deeper understanding of the positive elements and challenges that participants and faculty experienced during the course, we included open-field questions in every questionnaire we provided during the course, and we ran focus groups with 8 faculty and 7 participants. From open-field questions we obtained 182 statements between general comments and suggestions for improvement, 167 statements about what went well, and 128 about what we could do differently next time (). Most of the positive aspects mentioned overall were specific to the course content (lectures and cases) (151 comments) and faculty (44 comments). The second most cited positive element from participants and faculty was the high level of engagement of participants in the discussions (39 comments). Also, the overall organisation of the course, the pre-recorded lectures, the presence of attendees from different countries, and the technical support were appreciated. We found almost equal amount of positive (18) and negative (16) comments about the software used for the delivery of the course. The biggest challenge mentioned (80 comments) regarded connectivity or technical problems or background noise and voice interference between breakout rooms. The second challenge was the low attendance rate (11 comments) that made the allocation to the groups quite complicated. Another challenging aspect was the different experience level of participants within each group (9 comments). Among the 58 statements about course and module length, 18 wanted longer modules (110 or 120 minutes), 1 wanted shorter than 90 minutes, 16 wanted a shorter course (fewer weeks), and 6 suggested to change the day or time of the course. Suggestions to improve the course included 35 comments about content enhancement by providing additional resources to encourage pre-course study (7 comments) (e.g. videos of surgical procedures, articles), allowing participants to bring their own cases, and providing the recordings of the discussions. Regarding the discussion in the small groups, a few responders suggested faculty should avoid lecturing and give as much space as possible to participants, and the technical team should not end the session exactly after 90 minutes when some conversations were not finished.
Table 5. Subcategories of statements about what went well and about what we could do differently next time
From the focus groups, it emerged that the online experience was highly valued despite the online setting being more challenging for faculty to keep participants engaged in the discussion compared with face-to-face events. Faculty also mentioned the intensive training sessions necessary to familiarise with the new software and to prepare adequately. Staying in the same group for multiple weeks helped to get to know each other and to improve the flow. In addition, the possibility to have the names of participants visible provided faculty with the opportunity to directly address individuals. Having the second faculty was good for asking questions, monitoring the chat, and jumping in if the other faculty had connection problems. Language issues and connection problems sometimes made the conversation difficult and some responders suggested applying stricter criteria for enrolment in the course. Regarding the overall course length there were two diverging positions: one to make it more compressed, for example in 3 days, and one to keep it as it was.
Discussion
In this study we found that orthopaedic surgeons preferred group size for online SGD among presented options is 2 faculty with 5 participants. This seems to guarantee the best experience despite other group sizes and faculty ratios being acceptable to many. If a group is bigger, there might be numerous different experiences and ideas, but interaction becomes more difficult [Citation6]. It has been suggested that the interactions in the group are more important than the variability of ideas [Citation6]; therefore, keeping the number of participants low is favourable. Having groups with individuals from different countries offers the advantage of providing different perspectives and offers additional educational value. For the same reason, rotating faculty every week is an additional preference for many participants. On the other hand, it seems that maintaining the same participants over several weeks creates a more comfortable environment for discussion. This is also supported by Akcaoglu et al [Citation18] that showed students perceived a higher level of social presence in small groups online compared with the full class. Social presence is intended as the ability of students to identify with the learning community, communicate purposefully in a trusting environment, and develop interpersonal relationships. [Citation19].
Our results suggest that discussing 3 or 4 cases over 90 minutes is good practice and allows all aspects of the topic to be covered adequately. In addition, 8 modules delivered over 8 weeks is not suited for all participants and might be more appropriate for surgeons at the beginning of their career (the weekly format enables them to prepare in advance and to digest and reflect on the content), but may be a challenge for more experienced practicing surgeons. Comparisons of the SGDs show similar ratings for 8-week delivery compared with other types of online events delivered over 3 days or with similar past face-to-face courses. This suggests that online SGDs can achieve good educational outcomes ().
We also learned that our faculty and participants consider that online SGDs can run just as well as in a face-to-face environment, and they are willing to participate in this type of education even once face-to-face events can resume. This is in line with a recent study where neurosurgeons from lower-income nations and regions such as Europe and Central Asia want to see further educational activities in an online format [Citation20].
The AO has established faculty training programmes on a regular basis. The traditional faculty training includes performing a learning gap analysis, giving lectures, and moderating group discussions, and has been shown to be important in improving participants’ ratings and perception of the course relevance over time [Citation2]. Similar findings are reported by Leblanc et al., who organised faculty training for distance teaching [Citation16]. We adapted the standard AO faculty training to the online environment. Faculty perceived the training as quite intensive and time consuming; however, they recognised it was an essential element for success.
One of the main difficulties in running live online SGDs was related to technical/connection problems. To overcome the problems, technical counselling was provided during the online session by email, chat, or phone. However, to mitigate these challenges, we suggest providing tools to measure connection speed and recommending an acceptable range to connect with video and audio in order to be allowed to join the course. In addition, a test site could be provided for participants and faculty to practice using the learning platform.
Based on our data collection and input in the focus groups, we compiled the following recommendations.
Limitations
This course covers the full range of anatomical regions in the upper extremity, and the modules may be of different levels of relevance for participants. In this context, we assume that the participants selected which modules to attend based on interest. For this reason and for some technical issues (e.g. some participants were remembered by the software and placed into the same group in multiple weeks while others were randomised every week), group allocation and making sure that all participants and faculty experienced both types of small group formats during the eight weeks was challenging. Another limitation was that each participant’s level of experience was not used as a criterion for allocating participants; therefore, some groups were more heterogeneous than others giving high variability in the case ratings. In addition, the sample size is small, and the results are related to one educational event.
Conclusion
From our findings we suggest that online small groups are a viable and effective delivery option and need to be further explored for online and for blended learning. It is unclear when the clear longer-term benefits of changes made to the format of an educational course might become apparent; however, we expect that the literature will be expanded considerably in the next year or 2 as a result of many organisations gaining experience and reporting their findings. It might require 3 or more years to become evident, as suggested by Bhashyam et al. [Citation2] The benefit of delivering online SGDs is principally the digitalisation of live interactions facilitating participation from different regions of the world, using multimedia content and recording the sessions for further quality improvement and academic evaluation. Although it cannot replace the live interaction, an online small group case discussion can be of high educational value even when face-to-face courses are possible again.
Supplemental Material
Download MS Word (17.3 KB)Acknowledgments
Thanks to all the faculty and module moderators listed in supplementary material and to Sven Roost, Thommy Ruegg, Alain Rickli, Bettina Bolliger, and Miriam Uhlmann for setting up the online programme and environments and for the faculty training programme. Thanks to the participants and faculty who took part in the 4 focus groups and to the event tests. We thank the members of the AO Trauma Education Commission and the AO Trauma Upper Extremity Education Taskforce for supporting the research.
Disclosure Statement
Monica Ghidinelli and Michael Cunningham are employees of the AO Foundation. No additional potential conflict of interest was reported by the author(s).
Supplementary Material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Ryan G, Lyon P, Kumar K, et al. Online CME: an effective alternative to face-to-face delivery. Med Teach. 2007;29(8):e251–10.
- Bhashyam AR, van der Vliet QMJ, Houwert RM, et al. Redesigning an international orthopaedic CME course: the effects on participant engagement over 5 years. J Eur CME. 2019;8(1):1633193.
- Stambough JB, Curtin BM, Gililland JM, et al. The past, present, and future of Orthopedic education: lessons learned from the COVID-19 pandemic. J Arthroplasty. 2020;35(7):S60–S64.
- Chang D-G, Park J-B, Baek GH, et al. The impact of COVID-19 pandemic on orthopaedic resident education: a nationwide survey study in South Korea. Int Orthop. 2020;44(11):2203–2210.
- Berfield K. How Does the Adult Surgeon Learn? Thorac Surg Clin. 2019;29(3):233–238.
- Edmunds S, Brown G. Effective small group learning: AMEE guide No. 48. Med Teach. 2010;32(9):715–726.
- Steinert Y. Twelve tips for effective small-group teaching in the health professions. Med Teach. 1996;18(3):203–207.
- Palan J, Roberts V, Bloch B, et al. The use of a virtual learning environment in promoting virtual journal clubs and case-based discussions in trauma and orthopaedic postgraduate medical education: the Leicester experience. J Bone Joint Surg Br. 2012;94(9):1170–1175.
- Al-Azri H, Ratnapalan S. Problem-based learning in continuing medical education: review of randomized controlled trials. Can Fam Physician. 2014;60:157–165.
- Fay N, Garrod S, Carletta J. Group discussion as interactive dialogue or as serial monologue: the influence of group size. Psychol Sci. 2000;11(6):481–486.
- Green J, De Boer P, eds. AO principles of teaching and learning. Davos: AO Publishing; 2005.
- Zimitat C. Designing effective on-line continuing medical education. Med Teach. 2001;23(2):117–122.
- Knipfer C, Wagner F, Knipfer K, et al. Learners’ acceptance of a webinar for continuing medical education. Int J Oral Maxillofac Surg. 2019;48(6):841–846.
- Feist M, Ciccarelli M, McFerron BA, et al. Methods and effects of a case-based pediatric gastroenterology online curriculum. J Pediatr Gastroenterol Nutr. 2013;56(2):161–165.
- King S, Greidanus E, Carbonaro M, et al. Synchronous problem-based e-learning (ePBL) in interprofessional health science education. J Interact Online Learn. 2010;9(2): 133–150.
- LeBlanc JM, Pruchnicki MC, Rohdieck SV, et al. An instructional seminar for online case-based discussions. Am J Pharm Educ. 2007;71(3):42.
- Ghidinelli M, Cunningham M, Uhlmann M, et al. Designing and implementing a harmonized evaluation and assessment system for educational events Worldwide. J Orthop Traumatol. 2021;35:S5–S10.
- Akcaoglu M, Lee E. Increasing social presence in online learning through small group discussions. Int Rev Res Open Distrib Learn. 2016;v17(n3):1–17.
- Garrison R. E-learning in the 21st century: a community of inquiry framework for research and practice. New York: Routledge (Taylor & Francis Group); 2017.
- El-Ghandour NMF, Ezzat AAM, Zaazoue MA, et al. Virtual learning during the COVID-19 pandemic: a turning point in neurosurgical education. Neurosurg Focus. 2020;49(6):E18.
Appendix
Overall Impressions from AO Trauma Upper Extremity Online Small Group Discussions (Sept-Oct 2020)
Privacy statement: The information you provide will be anonymised and made available to the faculty and education planning groups in aggregate form. Data will be used for a publication on this research.
Which modules did you attend?
Clavicle
Scapula
Proximal humerus
Humeral shaft
Distal humerus
Elbow and forearm
Distal radius and ulna
Carpus and hand (click if you WILL attend)
During the 8 weeks, what were the reasons you did not attend all modules? (select all that apply)
8 weeks is too much
Some modules are not relevant to me
The time of day was not suitable
I have poor network access
OR or work schedule
Too tired at end of day
I am faculty and can’t attend every module
Other (please specify)
What went well overall?
What could we do differently next time?
What are the best rotation plans for faculty and participants?
From your experiences up to now in the overall course, please rate each of the following ways to run online small groups
Please indicate your level of agreement with each of the statements below.
Would you join an online course like this again?
Yes
Yes if some changes were made
No
Thanks again for your time and feedback. Any final comments?
