?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Background:
Receiving hemodialysis treatment makes end-stage renal disease (ESRD) patients highly vulnerable amidst the COVID-19 pandemic. Hence, their kidney disease quality of life (KDQOL) is affected. We aimed to examine the association between fear of COVID-19 (FCoV-19) and KDQOL, and the effect modification of Health literacy (HL) on this association.
Material and Methods:
A survey was conducted at 8 hospitals from July 2020 to March 2021 on 972 patients. Data collection includes socio-demographic factors, clinical parameters, HL, digital healthy diet literacy (DDL), hemodialysis diet knowledge (HDK), FCoV-19, suspected COVID-19 symptoms (S-COVID-19-S), and KDQOL.
Results:
Higher HL scores B = 0.13 (95% CI = 0.06–0.21, p = 0.001) and HDK scores B = 0.58 (95% CI = 0.31–0.85, p = 0.001) were associated with higher KDQOL scores. Whereas, S-COVID-19-S B = −6.12 (95% CI = −7.66 to – 4.58, p = 0.001) and FCoV-19 B = −0.91 (95% CI = −1.03 to – 0.80, p = 0.001) were associated with lower KDQOL scores. Notably, higher HL scores significantly attenuate the negative impact of FCoV-19 on overall KDQOL and the kidney disease component summary.
Conclusions:
In hemodialysis patients, FCoV-19 and S-COVID-19-S were associated with a lower KDQOL. Health literacy significantly mitigates the negative impact of FCoV-19 on KDQOL. Strategic public health interventions to improve HL are suggested to protect patient’s KDQOL during the pandemic.
Introduction
The COVID-19 pandemic heavily affected individuals’ physical and mental well-being worldwide (Chen et al., Citation2022; WHO, Citation2022). Within vulnerable populations such as patients undergoing hemodialysis, the fear and anxiety stemming from COVID-19 can impair their quality of life (QOL) (Nguyen et al., Citation2021; Park & Park, Citation2023), and exacerbate their existing health concerns (Fishbane et al., Citation2015). Understanding the factors that modify the impact of fear on the quality of life in hemodialysis patients is crucial to developing targeted interventions and support strategies.
Health literacy is a concept that encompasses an individual's knowledge, motivation, and skills to access, understand, evaluate, and use health information effectively (Sørensen et al., Citation2012). It has been shown to influence patients’ ability to navigate the healthcare system, make informed decisions, and effectively manage their health conditions (Al Sayah et al., Citation2013). Given the complexity of hemodialysis treatment and the need for self-care management, HL was particularly important for hemodialysis patients in the context of fear related to COVID-19.
While previous studies examined the impact of COVID-19-related fear on the quality of life in various populations, limited research focused on hemodialysis patients (Beisland et al., Citation2021; Nguyen et al., Citation2021; Yeni et al., Citation2022). Furthermore, the potential moderating role of HL remains to be explored. Therefore, we aimed to investigate the negative impact of COVID-19-related fear on kidney disease quality of life and its subscales, and explore the potential modifying effect of HL on that association in hemodialysis patients.
Methods
Study design and participants
From July 2020 to March 2021, a cross-sectional study was conducted at eight hospitals in Vietnam, including four at the national level and four at the provincial level, to ensure representation from various regions in Vietnam. Eligible participants were hemodialysis patients aged between 18 and 85 who could read and respond to the survey. Patients who had received hemodialysis treatment for less than 3 months were excluded from the study. Importantly, no positive cases of COVID-19 were reported among the patients during the study period. Prior to participating in the research, patients were required to provide informed consent. This study was approved by the Institutional Review Board of Hanoi University of Public Health in Vietnam (IRB No. 225/2020/YTCC-HD3). The study included a total sample size of 972 patients.
Data collection was described in previous studies (Dang et al., Citation2022; Le et al., Citation2023). In brief, a team comprising nephrologists, nurses, and students underwent training to ensure consistent and accurate data collection. Strict COVID-19 control measures, such as the mandatory use of masks, regular hand washing, and maintenance of physical distancing, were implemented throughout the study. The survey took approximately 30 minutes to be completed. Next, the collected data underwent a rigorous process of coding, cleaning, and analysis. This involved assigning appropriate codes to the data, identifying and rectifying any inconsistencies or errors, and preparing the dataset for analysis.
Measurements
Outcome variables
The KDQOL was evaluated using the KDQOL 36-item short-form survey (KDQOL-36; version 1.3), developed by RAND Corporation (Health, Citation2012), which was validated in Vietnam (Vo et al., Citation2018; Vu et al., Citation2021). The KDQOL-36 consists of 5 distinct subscales: the physical component summary (PCS), mental component summary (MCS), burden of kidney disease (BKD), symptoms and problems of kidney disease (SPKD), and effects of kidney disease (EKD). The kidney disease component summary (KDCS) consists of BKD, SPKD, and EKD. Therefore, the overall KDQOL and three scales (MCS, PCS, and KDCS) were analyzed in our study, with the score potentially ranging from 0 to 100 (Cohen et al., Citation2019; Manavalan et al., Citation2017), with higher scores indicating better KDQOL (Ishiwatari et al., Citation2020; Jung et al., Citation2019).
Fear of COVID-19
The fear of COVID-19 was assessed using the 7-item Fear of COVID-19 Scale (FCoV-19S). Respondents were asked to indicate their level of agreement with each item on a scale ranging from 1 to 5, where 1 corresponds to ‘strongly disagree,’ 2 to ‘disagree,’ 3 to ‘neither agree nor disagree,’ 4 to ‘agree,’ and 5 to ‘strongly agree.’ The composite score encompasses values between 7 and 35, with higher scores denoting a greater sense of fear (Nguyen, Do et al., Citation2020). This tool was validated in Vietnam (Doan et al., Citation2021; Nguyen et al., Citation2022).
Health literacy and digital healthy diet literacy
The HL and DDL indices were evaluated using the 12-item short form of the Health Literacy Questionnaire (HLS-SF12) (Duong et al., Citation2019) and the Digital Healthy Diet Literacy Scale (DDL-4) (Duong et al., Citation2020), respectively. Respondents rated the perceived difficulty of each item on a 4-point scale, with 1 representing ‘very difficult,’ 2 for ‘fairly difficult,’ 3 for ‘fairly easy,’ and 4 for ‘very easy.’ The HL and DDL indices were derived using the following formula:
In this equation, ‘Index’ stands for the specific index calculated, ‘Mean’ denotes the mean of all item ratings for each participant. The scores range from 0 to 50, with higher scores indicating elevated levels of HL or DDL. These scales have been validated and used in Vietnam (Sørensen et al., Citation2015; Van Hoa et al., Citation2020).
Covariates
Patient demographic information, such as age, gender, education, working status, marital status, and social status, along with medication payment ability, were collected. Social status was determined through a self-reported question asking participants to assess their social status based on factors such as education, occupation, and income, with response options including ‘low,’ ‘middle,’ and ‘high.’
Clinical parameters were assessed, including comorbidity, suspected COVID-19 symptoms (S-COVID-19-S), hemodialysis vintage (HD vintage, length of time on dialysis) (Chertow et al., Citation2000), edema, hypothyroidism, hyperthyroidism, hospitalization with one month and fear of COVID-19. S-COVID-19-S was identified if participants exhibited any of the following symptoms: fever, cough, fatigue, dyspnea, myalgia, sputum production/expectoration, sore throat, runny nose, confusion, headache, chest pain, rhinorrhea, diarrhea, and/or nausea/vomiting (Practice, Citation2020). Body mass index (BMI) was classified into 2 levels using the cutoff value at 24 kg/m2. This cutoff value was also used in previous studies on hemodialysis patients (Dang et al., Citation2022; Le et al., Citation2023). Physical activiy was assessed using the International Physical Activity Questionnaire short version (IPAQ-SF). The details were described in our previous publications (Dang et al., Citation2022; Le et al., Citation2023). The physical activity score (metabolic equivalent task-MET) was calculated by multiplying minutes spent on activities (sitting, walking, moderate, and vigorous activity) by 1.0, 3.3, 4.0, and 8.0, respectively. The MET was scored in minutes per week (MET-min/wk) and classified by tertiles.
Comorbidities were assessed using the Charlson comorbidity index (CCI) items which were modified in ESRD patients (Hemmelgarn et al., Citation2003). Each comorbid condition was assigned a specific score, e.g. 1 point was given to Peripheral vascular disease, Dementia, Chronic lung disease, Rheumatologic disease, Peptic ulcer disease, Diabetes with complications; 2 points were given to Myocardial infarction, Congestive heart failure, Cerebral vascular disease, Diabetes, Moderate/severe liver disease, Leukemia; 5 points were given to Lymphoma; and 10 points were given to Metastatic disease. The total score is calculated by summing up the scores of all the comorbidities present in a patient. The higher the score, the higher the predicted risk of mortality (Charlson et al., Citation2022).
Hemodialysis dietary knowledge (HDK) was evaluated using a 10-question scale that assessed participants’ knowledge about the hemodialysis diet, specifically focusing on water, potassium, phosphorus, sodium, and protein (Ryu et al., Citation2014). Each question had three response options: ‘correct,’ ‘incorrect,’ and ‘not sure.’ The correct answer was treated as ‘correct’, 1 point was given, and incorrect or ‘not sure’ answers were treated as ‘incorrect’, 0 point was given. The average score ranged from 0 to 1, with higher scores indicating greater knowledge. This questionnaire has been validated and utilized in previous research in hemodialysis patients (Le et al., Citation2022).
Statistical analysis
The distributions of variables were analyzed and presented as count (n), percentage (%), mean, and standard deviation (SD) appropriately. Group differences in KDQOL scores were explored using t-tests or one-way ANOVA tests. To identify factors associated with KDQOL and its subscales, bivariate linear regression analysis was conducted. Based on a simulation study on confounder-selection strategies, factors showing an association with KDQOL at a p-value < 0.2 in the bivariate model were included in the multivariate model to eliminate the residual effects of the studied factors (Maldonado & Greenland, Citation1993). Prior to performing the multivariate linear regression, correlations among the independent variables were examined to avoid issues of multi-collinearity. Independent variables with Spearman correlation coefficients below 0.3 were considered acceptable for inclusion in the multivariate model (Supplementary Tables S1–S4). Interaction analyses, utilizing interaction terms, were conducted to investigate the modifying effect of HL on the association between fear of COVID-19 and overall KDQOL and its subscales. Models 1 and 2 involved three terms, namely X1, X2, and X1*X2, where X1 represents the main effect of fear of COVID-19, X2 represents the main effect of the modifying factor, and X1*X2 represents the interaction between the two factors.
Finally, we employed PROCESS 4.2 within SPSS to delve into the modified impact of HL on the association between fear of COVID-19 and overall KDQOL or KDCS. To enhance comprehension of the simple slope analysis, we employed figures to visually elucidate the results. These plots were created by computing the anticipated outcomes (overall KDQOL and KDCS) across three HL values: one standard deviation above the mean (+1 SD), the mean, and one standard deviation below the mean (−1 SD). All statistical analyses were performed using IBM SPSS Version 26.0 (IBM Corp., Armonk, NY, USA), with statistical significance was established at p < 0.05.
Results
Participants’ characteristics
presents participants’ characteristics with 517 men (53.5%), 450 women (46.54%), 585 patients (60.2%) aged 18–59 years. Kidney disease quality of life was significantly varied across several variables, including age, gender, social status, medication payment ability, suspected COVID-19 symptoms, edema, hyperthyroidism, hospitalization within one month, level of physical activity, and HD vintage (p < 0.05). Specifically, the mental component summary (MCS) score was significantly varied by social status, medication payment ability, suspected COVID-19 symptoms, edema, hospitalization within one month, and physical activity. Similarly, the physical component summary (PCS) score was significantly varied by age, education level, marital status, social status, medication payment ability, suspected COVID-19 symptoms, hyperthyroidism, hospitalization within one month, and physical activity. Additionally, the kidney disease component summary (KDCS) score was significantly varied by age, gender, social status, medication payment ability, suspected COVID-19 symptoms, edema, hyperthyroidism, hospitalization within one-month, physical activity, and HD vintage ().
Table 1. Patients’ characteristics, kidney disease quality of life, and subscales (N = 972).
Associated factors of kidney disease quality of life
showed the results of bivariate and multivariate linear regression models of overall KDQOL. In the bivariate model, the determinants of overall KDQOLwere age, gender, social status, medication payment ability, suspected COVID-19 symptoms, BMI, edema, hypothyroidism, hyperthyroidism, hospitalization within one month, level of physical activity, HD vintage, CCI, fear of COVID-19, HL index, DDL index, and HDK. We found that medical payment ability was correlated with physical activity at rho = 0.31, CCI was correlated with edema at rho = 0.34, and HL was correlated with DDL at rho = 0.75 (Table S1). Therefore, edema, physical activity, and HL were analyzed in the multivariate model together with other factors that show a significant association with overall KDQOL in the bivariate model. The results show that the factor associated with higher the overall KDQOL score was social status ‘unstandardized regression coefficient’, B = 2.70 (95% confidence interval, 95% CI = 1.13–4.28, p = 0.001), edema B = 1.14 (95% CI = 0.01–2.88, p = 0.049), physical activity B = 1.33 (95% CI = 0.43–2.22, p = 0.004), HL B = 0.13 (95% CI = 0.06–0.21, p = 0.001), HDK B = 0.58 (95% CI = 0.31–0.85, p = 0.001). Conversely, S-COVID-19-S B = − 6.12 (95% CI = −7.66 to − 4.58, p = 0.001), hyperthyroidism B = −6.84 (95% CI = −10.58 to − 3.10, p = 0.001), hospitalization within one month B = − 6.74 (95% CI = −9.79 to −3.68, p = 0.001), and fear of COVID-19 B = −0.91 (95% CI = −1.03 to −0. 80, p = 0.001) were associated with lower the overall KDQOL score.
Table 2. Associated factors of kidney disease quality of life via bivariate and multivariate linear regression analysis.
Factors associated with subscales of kidney disease quality of life
In the bivariate analysis, the determinants of MCS were social status, medication payment ability, suspected COVID-19 symptoms, edema, hospitalization within one-month, physical activity, HD vintage, CCI, fear of COVID-19, HL index, and DDL index. We found that medical payment ability was correlated with physical activity at rho = 0.31, CCI was correlated with edema at rho = 0.34, and HL was correlated with DDL at rho = 0.75 (Table S2). Therefore, CCI, HL index, and physical activity were analyzed in the multivariate model together with other factors that showed a significant association with MCS in the bivariate model. The results show that factors associated with higher MCS scores were physical activity B = 1.19 (95% CI = 0.18–2.19, p = 0.021). Conversely, S-COVID-19 S B = −2.36 (95% CI = − 4.01 to −0.71, p = 0.005), hospitalization with one month B = −5.63 (95% CI = −9.04 to −2.22, p = 0.001), HD vintage B = −1.33 (95% CI = −2.40 to −0.26, p = 0.015), CCI B = − 0.43 (95% CI = −0.67 to −0.19, p = 0.001), and fear of COVID-19 B = −0.51 (95% CI = −0.64 to − 0.38, p = 0.001) were associated with lower MCS scores ().
Table 3. Associated factors of subscales of kidney disease quality of life via bivariate and multivariate linear regression analysis.
In the bivariate analysis, the determinants of PCS were age, gender, education, married status, social status, medication payment ability, S-COVID-19 S, hyperthyroidism, hospitalization within one-month, physical activity, HD vintage, CCI, fear of COVID-19, HL index, and DDL index. We found that medical payment ability was correlated with physical activity at rho = 0.31, and HL was correlated with DDL at rho = 0.75 (Table S3). Therefore, CCI and HL were analyzed in the multivariate model together with other factors that showed a significant association with PCS in the bivariate model. The results show that factors associated with higher PCS scores were physical activity B = 1.44 (95% CI = 0.56–2.32, p = 0.001) and HL B = 0.13 (95% CI = 0.05–0.20, p = 0.001). Conversely, age B = −1.48 (95%CI = −2.84 to −1.13, p = 0.031), education B = −0.84 (95% CI = −1.66 to −0.01, p = 0.047), hyperthyroidism B = −5.07 (95% CI = −9.57 to −1.60, p = 0.005), hospitalization within one month B = −4.77 (95% CI = −7.98 to −1.55, p = 0.004), and fear of COVID-19 B = −0.22 (95% CI = −0.33 to −0.10, p = 0.001) were associated with lower PCS scores. However, we didn’t find a significant association between HL and either MCS scores or PCS scores ().
In the bivariate analysis, the determinants of KDCS were age, gender, social status, medication payment ability, S-COVID-19-S, BMI, edema, hypothyroidism, hyperthyroidism, hospital within one-month, physical activity, HD vintage, CCI, fear of COVID-19, HL index, DDL index, and HDK. We found that medical payment ability was correlated with physical activity at rho = 0.31, CCI was correlated with edema at rho = 0.34, and HL was correlated with DDL at rho = 0.75 (Table S4). Therefore, edema, physical activity, and HL were analyzed in the multivariate model together with other factors that show a significant association with QOL in the bivariate model. The results show that factors associated with higher KDCS scores were social status B = 3.46 (95%CI = 1.37–5.55, p = 0.001), edema B = 2.46 (95% CI = 0.56–4.37, p = 0.011), physical activity B = 1.41 (95% CI = 0.23–2.60, p = 0.02), HL B = 0.15 (95% CI = 0.05–0.15, p = 0.003), and HDK B = 0.80 (95%CI = 0.44–1.16, p = 0.001). Conversely, age B = −2.03 (95%CI = −3.81 to −0.24, p = 0.026), S-COVID-19 S B = −8.21 (95% CI = −10.25 to −6.17, p = 0.001), hyperthyroidism B = −9.94 (95%CI = −14.91 to −4.98, p = 0.001), hospitalization within one month B = −6.93 (95% CI = −10.98 to −2.97, p = 0.001), and fear of COVID-19 B = −1.19 (95% CI = −1.34 to −1.03, p = 0.001) were correlated with lower scores of KDCS ().
Interaction of health literacy with fear of COVID-19 on kidney disease quality of life
illustrates how the association between fear of COVID-19 and KDQOL was modified by HL. Specifically, patients with one score increment in both fear of COVID-19 and health literacy exhibited higher overall KDQOL B = 0.011 (95%CI = 0.000–0.021, p = 0.042), and KDCS B = 0.015 (95%CI = 0.001–0.028, p = 0.038).
Table 4. Interaction of health literacy with fear of COVID-19 on KDQOL and KDCS.
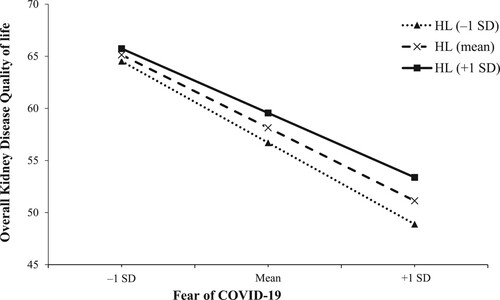
illustrates the results of the simple slope analysis, revealing that as HL increased, the association between fear of COVID-19 and overall KDQOL diminished. A higher HL score mitigates the negative impact of COVID-19-related fear on overall KDQOL, transitioning from B = −1.01 (95%CI = −1.16 to −0.86, p = 0.001) at one standard deviation below the mean, to B = −0.91 (95%CI = −1.03 to −0.79, p = 0.001) at the mean, and B = −0.81 (95%CI = −0.96 to −0.65, p = 0.001) at one standard deviation above the mean.
Figure 1. Simple slope plot of interaction between health literacy and fear of COVID-19 on overall kidney disease quality of life. SD, standard deviation; HL, health literacy.
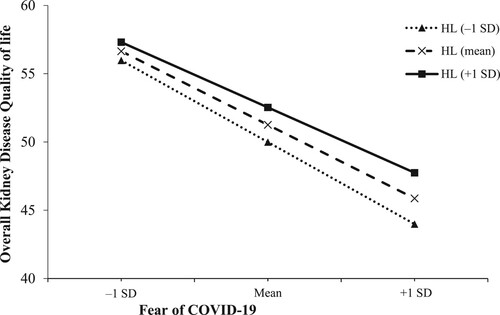
Similarly, demonstrates that as HL increased, the association between fear of COVID-19 and KDCS diminished. A higher HL score mitigates the negative impact of COVID-19-related fear on KDCS, transitioning from B = −1.32 (95%CI = −1.52 to −1.12, p = 0.001) at one standard deviation below the mean, to B = −1.18 (95%CI = −1.34 to −1.03, p = 0.001) at the mean, and B = −1.04 (95%CI = −1.25 to −0.84, p = 0.001) at one standard deviation above the mean.
Discussion
In the current study, the results showed that more fear of COVID-19 was associated with a lower overall KDQOL score and its subscales (PCS, MCS, and KDCS), indicating the detrimental impact of fear on the well-being of these patients. This finding is consistent with previous studies that have examined the impact of fear of COVID-19 on the quality of life in hemodialysis patients (Parlak & Akgün Şahin, Citation2021), as well as in other populations, such as inpatients, outpatients, general publics, and healthcare workers (Abdelghani et al., Citation2022; Baysal et al., Citation2022; Demirbas & Kutlu, Citation2022; Nguyen et al., Citation2021).
Fear of COVID-19 can affect the quality of life of hemodialysis patients through increased stress, anxiety, and psychological distress (Beaini et al., Citation2021; Lee et al., Citation2020). The fear and anxiety surrounding the pandemic can lead to stress and emotional strain, which can negatively impact their mental health and overall quality of life. Hemodialysis patients were particularly vulnerable when they accessed the treatment weekly (2-3 times a week) in the dialysis center which may cause more fear, panic, and increased risk of infection (Lee et al., Citation2020). During the pandemic, patients with the less social support, limited access to resources, and feelings of loneliness and isolation, all of which can contribute to a decline in their quality of life (Hwang et al., Citation2020). Furthermore, Fear of COVID-19 further exacerbates existing health concerns among hemodialysis patients (Nadort et al., Citation2022). The stress and anxiety associated with the pandemic can impact patient’s physical well-being, potentially leading to disrupted sleep patterns, increased fatigue, and decreased overall functional capacity (Lee et al., Citation2020). This further diminishes their quality of life and negatively impacts their ability to cope with the challenges of managing their kidney disease. By identifying fear of COVID-19, and its impact on quality of life, our study emphasizes the need for targeted interventions and support strategies to mitigate the negative impact of COVID-19-related fear in hemodialysis patients.
The higher HL levels were associated with higher overall KDQOL scores and all subscales. HL further diminishes the negative impact of COVID-19-related fear on overall KDQOL and KDCS components. HL was found to play a critical role in shaping health outcomes and patients’ ability to effectively manage their health conditions (Chow et al., Citation2024; Liu et al., Citation2020).
During the data analysis, the protective effect of HL against the negative impact of fear on the MCS and PCS of quality of life was not found in the current study. This may be influenced by several factors. In contrast, the MCS and PCS components of the KDQOL™−36 are more generic measures of mental and physical well-being and may be influenced by a wider range of factors beyond fear and HL alone. Take into account, HL may have a more specific influence on certain dimensions of QOL, particularly those related to kidney disease and its management. In light of a previous study, HL was proven to reduce anxiety among hemodialysis patients (Yoon & Lee, Citation2023). This finding suggests that interventions aimed at improving HL in hemodialysis patients may have a positive impact on their quality of life, especially in the face of fear and anxiety related to COVID-19.
Besides, we found that S-COVID-19-S was negatively associated with overall KDQOL and all subscales. This result is similar to the previous study in the outpatients (Nguyen, Nguyen et al., Citation2020). Suspected COVID-19 symptoms, such as fever, cough, fatigue, dyspnea, myalgia, and others, can cause physical discomfort and hinder daily activities (Sharp et al., Citation2021). These symptoms can directly impact a person's ability to engage in routine tasks. Experiencing symptoms associated with COVID-19 can induce anxiety, fear, and psychological distress. The fear of having a potentially severe illness or the uncertainty surrounding the symptoms can negatively affect a person's mental well-being. Taken together, these lead to a decrease in their quality of life.
Among the clinical factors considered, edema had a negative impact on the overall KDQOL and its subscales in hemodialysis patients, apart from the PCS subscale. It has been observed that individuals dealing with chronic edema experience diminished health conditions and a more pronounced influence on various aspects of HRQOL (Moffatt et al., Citation2017). Our findings are consistent with a previous study (Pretto et al., Citation2020) conducted on hemodialysis patients, where a connection between edema and a diminished quality of life was established. The negative effect of edema on quality of life suggests that the presence of edema is associated with poorer well-being and functioning in various aspects of the patients’ lives. However, it is important to note that the impact of edema on quality of life may vary across different subscales. In the case of the PCS subscale, which primarily focuses on the physical health and functioning of individuals, the presence of edema may not show a significantly negatively association. This could imply that the impact of edema may show the impact on other aspects of quality of life, such as mental well-being, emotional functioning, and the burden of kidney disease-related symptoms.
Moreover, we also explored that a longer HD vintage and a higher CCI score were associated with a lower overall KDQOL score. Specifically, patients with more than 10 years of HD vintage had lower quality of life across all subscales, except PCS. A previous study showed a significant decrease in the PCS score as dialysis vintage lengthened, while no association was found with a change in the MCS score. The MCS score declined over time in older patients, particularly those aged 80 years and older, after 2 years of follow-up (Ishiwatari et al., Citation2020). However, in our population, individuals aged 18–59 accounted for 60.2%. Therefore, HD vintage seems to have a greater effect on MCS than PCS in young HD patients. Conversely, intensive physical activity was positively associated with overall KDQOL. Physical activity has also been proven to relate to a higher overall KDQOL in other populations (Anokye et al., Citation2012; Puciato et al., Citation2018; Wei et al., Citation2022), specifically in hemodialysis patients with comorbidities, where improvement can be achieved through early intervention involving regular moderate-intensity physical activity (Wu et al., Citation2022). Recent studies have also shown the positive effects of intradialytic exercise on quality of life (Greenwood et al., Citation2021). Therefore, we need to encourage HD patients to engage in more physical activity.
The results of this study have important implications for healthcare professionals, policymakers, and patient advocacy groups in designing tailored interventions and educational programs to address the unique needs of hemodialysis patients during the COVID-19 pandemic and beyond. Recognizing the significant impact of COVID-19-related fear on overall KDQOL, healthcare providers can prioritize interventions. These may include providing protective measures for both COVID-19 and non-COVID-19 patients, implementing vaccination programs for all patients, and offering support to alleviate fear and anxiety within this population (Chirico & Teixeira da Silva, Citation2023). Furthermore, considering the potential moderating role of HL, interventions aimed at its enhancement may positively influence quality of life. To achieve this, patient education programs tailored specifically to hemodialysis patients should be implemented. These programs ought to encompass crucial topics, including kidney disease, hemodialysis treatment procedures, dietary restrictions, medication management, and recognizing signs of complications. Additionally, one-on-one counseling sessions should be offered by healthcare providers, nurses, dietitians, and pharmacists to address patients’ specific questions and concerns regarding their treatment plans, medications, and lifestyle adjustments (Murdeshwar & Anjum, Citation2024). Peer support groups can also be facilitated, allowing hemodialysis patients to connect with others facing similar challenges, exchange experiences, and offer practical advice for managing their condition. Regular assessments of patients’ health literacy levels should be conducted to pinpoint areas for improvement, enabling tailored educational interventions (Dineen-Griffin et al., Citation2019).
Despite its contributions, this study has some limitations. First, the cross-sectional design of the study limits the ability to establish causal relationships between the variables of interest. Longitudinal studies are suggested that will provide more robust evidence on the temporal associations between fear of COVID-19, HL, and KDQOL in hemodialysis patients. Secondly, the study was conducted in Vietnam, which may limit the generalizability of the findings to other cultural and healthcare contexts. Finally, the study relied on self-reported measures, which are subject to recall and social desirability biases. The inclusion of objective measures and additional sources of data would enhance the validity of the findings. Future research should aim to replicate these findings in diverse populations and settings, utilizing more comprehensive and disease-specific questionnaires for HL.
Conclusions
In this study, fear of COVID-19, symptoms like COVID-19, hemodialysis vintage, and comorbid conditions were negatively associated with KDQOL and subscales. Fortunately, HL, DDL, and physical activity were positively associated with overall KDQOL and its subscales. In addition, a higher health literacy score was linked to a mitigation of the negative impact fear of COVID-19 on both overall KDQOL and KDCS. These results provide significant evidence supporting the implementation of targeted measures aimed at alleviating fear and improve quality of life in hemodialysis patients.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and was approved by an Institutional Review Board/Ethics committee. See details under Methods
Supplementary.docx
Download MS Word (24.5 KB)Acknowledgments
The authors would like to thank all of the healthcare providers and patients who participated in this study from Bach Mai Hospital, Military Hospital 103, General Hospital of Agricultural, National Thai Nguyen Hospital, Hai Phong University of Medicine and Pharmacy Hospital, Hai Phong International Hospital, Quang Ninh General Hospital, and Bai Chay Hospital.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Abdelghani, M., Hamed, M. G., Said, A., & Fouad, E. (2022). Evaluation of perceived fears of COVID-19 virus infection and its relationship to health-related quality of life among patients with diabetes mellitus in Egypt during pandemic: A developing country single-center study. Diabetology International, 13(1), 108–116. https://doi.org/10.1007/s13340-021-00511-8
- Anokye, N. K., Trueman, P., Green, C., Pavey, T. G., & Taylor, R. S. (2012). Physical activity and health related quality of life. BMC Public Health, 12(1), 624. https://doi.org/10.1186/1471-2458-12-624
- Baysal, E., Selçuk, A. K., Aktan, G. G., Andrade, E. F., Notarnicola, I., Stievano, A., & Blanque, R. R. (2022). An examination of the fear of COVID-19 and professional quality of life among nurses: A multicultural study. Journal of Nursing Management, 30(4), 849–863. https://doi.org/10.1111/jonm.13550
- Beaini, C., Aoun, M., El Hajj, C., Sleilaty, G., Haber, N., Maalouf, G., & Abi Rached, E. (2021). The impact of the SARS-CoV-2 pandemic on the mental health of hemodialysis patients in Lebanon. Journal of Medicine and Life, 14(4), 523–530. https://doi.org/10.25122/jml-2020-0165
- Beisland, E. G., Gjeilo, K. H., Andersen, J. R., Bratås, O., Bø, B., Haraldstad, K., Hjelmeland, I. H. H., Iversen, M. M., Løyland, B., Norekvål, T. M., Riiser, K., Rohde, G., Urstad, K. H., Utne, I., Flølo, T. N., & the, L. n. (2021). Quality of life and fear of COVID-19 in 2600 baccalaureate nursing students at five universities: A cross-sectional study. Health and Quality of Life Outcomes, 19(1), 198. https://doi.org/10.1186/s12955-021-01837-2
- Charlson, M. E., Carrozzino, D., Guidi, J., & Patierno, C. (2022). Charlson comorbidity index: A critical review of clinimetric properties. Psychotherapy and Psychosomatics, 91(1), 8–35. https://doi.org/10.1159/000521288
- Chen, X., Lin, F., Gao, H., & Zou, Y. (2022). Stratified changes in emotional distress during the COVID-19 pandemic: Evidence from a longitudinal survey of residents in Hubei province, China. Journal of Psychosomatic Research, 160, 110959. https://doi.org/10.1016/j.jpsychores.2022.110959
- Chertow, G. M., Johansen, K. L., Lew, N., Lazarus, J. M., & Lowrie, E. G. (2000). Vintage, nutritional status, and survival in hemodialysis patients. Kidney International, 57(3), 1176–1181. https://doi.org/10.1046/j.1523-1755.2000.00945.x
- Chirico, F., & Teixeira da Silva, J. A. (2023). Evidence-based policies in public health to address COVID-19 vaccine hesitancy. Future Virology, https://doi.org/10.2217/fvl-2022-0028
- Chow, B. C., Jiao, J., Duong, T. V., Hassel, H., Kwok, T. C. Y., Nguyen, M. H., & Liu, H. (2024). Health literacy mediates the relationships of cognitive and physical functions with health-related quality of life in older adults. Frontiers in Public Health, 12), https://doi.org/10.3389/fpubh.2024.1355392
- Cohen, D. E., Lee, A., Sibbel, S., Benner, D., Brunelli, S. M., & Tentori, F. (2019). Use of the KDQOL-36™ for assessment of health-related quality of life among dialysis patients in the United States. BMC Nephrology, 20(1), 112. https://doi.org/10.1186/s12882-019-1295-0
- Dang, L. T., Luong, T. C., Nguyen, D. H., Hoang, T. A., Nguyen, H. T., Nguyen, H. C., Duong, T. H., Tran, T. T., Pham, L. V., & Ngo, T. V. (2022). The associations of suspected COVID-19 symptoms with anxiety and depression as modified by hemodialysis dietary knowledge: A multi-dialysis center study. Nutrients, 14(12), 2364. https://doi.org/10.3390/nu14122364
- Demirbas, N., & Kutlu, R. (2022). Effects of COVID-19 fear on society’s quality of life. International Journal of Mental Health and Addiction, 20(5), 2813–2822. https://doi.org/10.1007/s11469-021-00550-x
- Dineen-Griffin, S., Garcia-Cardenas, V., Williams, K., & Benrimoj, S. I. (2019). Helping patients help themselves: A systematic review of self-management support strategies in primary health care practice. PLoS One, 14(8), e0220116. https://doi.org/10.1371/journal.pone.0220116
- Doan, Q. H., Tran, N. N., Than, M. H., Nguyen, H. T., Bui, V. S., Nguyen, D. H., Vo, H. L., Do, T. T., Pham, N. T., Nguyen, T. K., Cao, D. C., Nguyen, V. T., Tran, T. T., Pham, B. H., Tran, A. L., Nguyen, V. T., Nguyen, V. T., Tran, X. T., Nguyen, T. L., … Otsu, S. (2021). Associated factors with perceived fear of COVID-19 among Vietnamese hospital healthcare workers during fourth wave of the COVID-19 pandemic: Policy implications for interconnected and social- and personal-based health support. Healthcare (Basel), 9(12). https://doi.org/10.3390/healthcare9121713
- Duong, T. V., Aringazina, A., Kayupova, G., Nurjanah Pham, T. V., Pham, K. M., Truong, T. Q., Nguyen, K. T., Oo, W. M., Su, T. T., Majid, H. A., Sørensen, K., Lin, I.-F., Chang, Y., Yang, S.-H., & Chang, P. W. S. (2019). Development and validation of a New short-form health literacy instrument (HLS-SF12) for the general public in Six Asian countries. HLRP: Health Literacy Research and Practice, 3(2), e91–e102. https://doi.org/10.3928/24748307-20190225-01
- Duong, T. V., Pham, K. M., Do, B. N., Kim, G. B., Dam, H. T. B., Le, V.-T. T., Nguyen, T. T. P., Nguyen, H. T., Nguyen, T. T., Le, T. T., Do, H. T. T., & Yang, S.-H. (2020). Digital healthy diet literacy and self-perceived eating behavior change during COVID-19 pandemic among undergraduate nursing and medical students: A rapid online survey. International Journal of Environmental Research and Public Health, 17(19), 7185. https://doi.org/10.3390/ijerph17197185
- Fishbane, S., Hazzan, A. D., Halinski, C., & Mathew, A. T. (2015). Challenges and opportunities in late-stage chronic kidney disease. Clinical Kidney Journal, 8(1), 54–60. https://doi.org/10.1093/ckj/sfu128
- Greenwood, S. A., Koufaki, P., Macdonald, J., Bhandari, S., Burton, J., Dasgupta, I., Farrington, K., Ford, I., Kalra, P. A., Kean, S., Kumwenda, M., Macdougall, I. C., Messow, C. M., Mitra, S., Reid, C., Smith, A. C., Taal, M. W., Thomson, P. C., Wheeler, D. C., … Mercer, T. H. (2021). The PrEscription of intraDialytic exercise to improve quAlity of life in patients with chronic kidney disease trial: Study design and baseline data for a multicentre randomized controlled trial. Clinical Kidney Journal, 14(5), 1345-1355. https://doi.org/10.1093/ckj/sfaa107
- Health, R. (2012). Kidney Disease Quality of Life Instrument (KDQOL).
- Hemmelgarn, B. R., Manns, B. J., Quan, H., & Ghali, W. A. (2003). Adapting the charlson comorbidity index for use in patients with ESRD. American Journal of Kidney Diseases, 42(1), 125–132. https://doi.org/10.1016/S0272-6386(03)00415-3
- Hwang, T. J., Rabheru, K., Peisah, C., Reichman, W., & Ikeda, M. (2020). Loneliness and social isolation during the COVID-19 pandemic. International Psychogeriatrics, 32(10), 1217–1220. https://doi.org/10.1017/S1041610220000988
- Ishiwatari, A., Yamamoto, S., Fukuma, S., Hasegawa, T., Wakai, S., & Nangaku, M. (2020). Changes in quality of life in older hemodialysis patients: A cohort study on dialysis outcomes and practice patterns. American Journal of Nephrology, 51(8), 650–658. https://doi.org/10.1159/000509309
- Jung, H.-Y., Jeon, Y., Park, Y., Kim, Y. S., Kang, S.-W., Yang, C. W., Kim, N.-H., Choi, J.-Y., Cho, J.-H., Park, S.-H., Kim, C.-D., & Kim, Y.-L. (2019). Better quality of life of peritoneal dialysis compared to hemodialysis over a Two-year period after dialysis initiation. Scientific Reports, 9(1), 10266. https://doi.org/10.1038/s41598-019-46744-1
- Le, L. T., Dang, L. T., Wang, T.-J., Do, T. G., Nguyen, D. H., Hoang, T. A., Pham, M. D., Do, B. N., Nguyen, H. C., & Tran, T. T. (2022). Osteoporosis risk in hemodialysis patients: The roles of gender, comorbidities, biochemical parameters, health and diet literacy. Nutrients, 14(23), 5122. https://doi.org/10.3390/nu14235122
- Le, L. T. H., Tran, T. T., Duong, T. V., Dang, L. T., Hoang, T. A., Nguyen, D. H., Pham, M. D., Do, B. N., Nguyen, H. C., Pham, L. V., Nguyen, L. T. H., Nguyen, H. T., Trieu, N. T., Do, T. V., Trinh, M. V., Ha, T. H., Phan, D. T., Nguyen, T. T. P., Nguyen, K. T., & Yang, S.-H. (2023). Digital healthy diet literacy and fear of COVID-19 as associated with treatment adherence and Its subscales among hemodialysis patients: A multi-hospital study. Nutrients, 15(10), 2292. https://doi.org/10.3390/nu15102292
- Lee, J., Steel, J., Roumelioti, M. E., Erickson, S., Myaskovsky, L., Yabes, J. G., Rollman, B. L., Weisbord, S., Unruh, M., & Jhamb, M. (2020). Psychosocial impact of COVID-19 pandemic on patients with End-stage kidney disease on hemodialysis. Kidney360, 1(12), 1390–1397. https://doi.org/10.34067/KID.0004662020
- Liu, C., Wang, D., Liu, C., Jiang, J., Wang, X., Chen, H., Ju, X., & Zhang, X. (2020). What is the meaning of health literacy? A systematic review and qualitative synthesis. Family Medicine and Community Health, 8(2), https://doi.org/10.1136/fmch-2020-000351
- Maldonado, G., & Greenland, S. (1993). Simulation study of confounder-selection strategies. American Journal of Epidemiology, 138(11), 923–936. https://doi.org/10.1093/oxfordjournals.aje.a116813
- Manavalan, M., Majumdar, A., Harichandra Kumar, K. T., & Priyamvada, P. S. (2017). Assessment of health-related quality of life and its determinants in patients with chronic kidney disease. Indian Journal of Nephrology, 27(1), 37–43. https://doi.org/10.4103/0971-4065.179205
- Moffatt, C. J., Aubeeluck, A., Franks, P. J., Doherty, D. C., Mortimer, P., & Quere, I. (2017). Psychological factors in chronic edema: A case–control study. Lymphatic Research and Biology, 15(3), 252–261. https://doi.org/10.1089/lrb.2017.0022
- Murdeshwar, H. N., & Anjum, F. (2024). Hemodialysis. In Statpearls. StatPearls Publishing.
- Nadort, E., Rijkers, N., Schouten, R. W., Hoogeveen, E. K., Bos, W. J. W., Vleming, L. J., Westerman, M., Schouten, M., Dekker, M. J. E., Smets, Y. F. C., Shaw, P. C., Farhat, K., Dekker, F. W., van Oppen, P., Siegert, C. E. H., & Broekman, B. F. P. (2022). Depression, anxiety and quality of life of hemodialysis patients before and during the COVID-19 pandemic. Journal of Psychosomatic Research, 158, 110917. https://doi.org/10.1016/j.jpsychores.2022.110917
- Nguyen, M. H., Do, T. X., Nguyen, T. T., Pham, M. D., Pham, T. T. M., Pham, K. M., Kim, G. B., Do, B. N., Nguyen, H. T., Nguyen, N.-M., Dam, H. T. B., Nguyen, Y. H., Nguyen, K. T., Nguyen, T. T. P., Nguyen, T. T., & Duong, T. V. (2022). Fear of COVID-19, healthy eating behaviors, and health-related behavior changes as associated with anxiety and depression among medical students: An online survey [original research]. Frontiers in Nutrition, 9. https://doi.org/10.3389/fnut.2022.938769
- Nguyen, H. T., Do, B. N., Pham, K. M., Kim, G. B., Dam, H. T. B., Nguyen, T. T., Nguyen, T. T. P., Nguyen, Y. H., Sørensen, K., Pleasant, A., & Duong, T. V. (2020). Fear of COVID-19 scale—associations of Its scores with health literacy and health-related behaviors among medical students. International Journal of Environmental Research and Public Health, 17(11), 4164. https://doi.org/10.3390/ijerph17114164
- Nguyen, H. C., Nguyen, M. H., Do, B. N., Tran, C. Q., Nguyen, T. T. P., Pham, K. M., Pham, L. V., Tran, K. V., Duong, T. T., Tran, T. V., Duong, T. H., Nguyen, T. T., Nguyen, Q. H., Hoang, T. M., Nguyen, K. T., Pham, T. T. M., Yang, S. H., Chao, J. C., & Duong, T. V. (2020). People with suspected COVID-19 symptoms were more likely depressed and Had lower health-related quality of life: The potential benefit of health literacy. Journal of Clinical Medicine, 9(4), https://doi.org/10.3390/jcm9040965
- Nguyen, M. H., Pham, T. T. M., Nguyen, K. T., Nguyen, Y. H., Tran, T. V., Do, B. N., Dao, H. K., Nguyen, H. C., Do, N. T., Ha, T. H., Phan, D. T., Pham, K. M., Pham, L. V., Nguyen, P. B., Nguyen, H. T. T., Do, T. V., Ha, D. T., Nguyen, H. Q., Ngo, H. T. M., … Duong, T. V. (2021). Negative impact of fear of COVID-19 on health-related quality of life Was modified by health literacy, eHealth literacy, and digital healthy diet literacy: A multi-hospital survey. International Journal of Environmental Research and Public Health, 18(9). https://doi.org/10.3390/ijerph18094929
- Park, Y., & Park, K. (2023). Health-related quality of life and depressive symptoms of patients with chronic diseases and the general population before and during the COVID-19 pandemic in Korea. Frontiers in Psychology, 14), https://doi.org/10.3389/fpsyg.2023.1117369
- Parlak, A. G., & Akgün Şahin, Z. (2021). The effect of COVID-19 fear on quality of life in hemodialysis patients: A correlation study in Turkey. Samsun Sağlık Bilimleri Dergisi, 6, 367–382. https://doi.org/10.47115/jshs.882164
- Practice, B. B. (2020). Coronavirus Disease 2019 (COVID-19), History and Exam. https://bestpractice.bmj.com/topics/en-gb/3000201/history-exam (accessed on 29 December 2022).
- Pretto, C. R., Winkelmann, E. R., Hildebrandt, L. M., Barbosa, D. A., Colet, C. F., & Stumm, E. M. F. (2020). Quality of life of chronic kidney patients on hemodialysis and related factors. Revista Latino-Americana de Enfermagem, 28, e3327. https://doi.org/10.1590/1518-8345.3641.3327
- Puciato, D., Rozpara, M., & Borysiuk, Z. (2018). Physical activity as a determinant of quality of life in working-Age people in wrocław, Poland. International Journal of Environmental Research and Public Health, 15(4), https://doi.org/10.3390/ijerph15040623
- Ryu, H., Jeon, H. J., Sun, H.-K., Han, K. H., Whang, C. G., & Han, S. Y. (2014). Repeated education improves diet compliance in maintenance hemodialysis patients. International Urology and Nephrology, 2, 63–68.
- Sayah, A., Majumdar, F., Williams, S. R., Robertson, B., Johnson, S., & A, J. (2013). Health literacy and health outcomes in diabetes: A systematic review. Journal of General Internal Medicine, 28(3), 444–452. https://doi.org/10.1007/s11606-012-2241-z
- Sharp, A. L., Huang, B. Z., Broder, B., Smith, M., Yuen, G., Subject, C., Nau, C., Creekmur, B., Tartof, S., & Gould, M. K. (2021). Identifying patients with symptoms suspicious for COVID-19 at elevated risk of adverse events: The COVAS score. The American Journal of Emergency Medicine, 46, 489–494. https://doi.org/10.1016/j.ajem.2020.10.068
- Sørensen, K., Pelikan, J. M., Röthlin, F., Ganahl, K., Slonska, Z., Doyle, G., Fullam, J., Kondilis, B., Agrafiotis, D., Uiters, E., Falcon, M., Mensing, M., Tchamov, K., Broucke, S. v. d., Brand, H., & Consortium, o. b. o. t. H.-E. (2015). Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). The European Journal of Public Health, 25(6), 1053–1058. https://doi.org/10.1093/eurpub/ckv043
- Sørensen, K., Van den Broucke, S., Fullam, J., Doyle, G., Pelikan, J., Slonska, Z., Brand, H., Health Literacy, C., & Project, E. (2012). Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health, 12(1), 80. https://doi.org/10.1186/1471-2458-12-80
- Van Hoa, H., Giang, H. T., Vu, P. T., Van Tuyen, D., & Khue, P. M. (2020). Factors associated with health literacy among the elderly people in Vietnam. BioMed Research International, 2020, 3490635. https://doi.org/10.1155/2020/3490635
- Vo, T. Q., Tran, T. Q., Duong, K. N. C., & Pham, K. C. (2018). Impact of chronic kidney disease on health-related quality of life: A prospective observational study using the KDQOL-36 instrument. Journal of Clinical and Diagnostic Research, 12(6), LC66–LC71.
- Vu, L. N., Nghia, N. Q., Tuan, T. M., Phuong, T. H., Vo, H. L., Viet, K. N., & Giang, T. B. (2021). Measuring health-related quality of life in Vietnamese patients after kidney transplantation. Frontiers in Surgery, 8, 646629. https://doi.org/10.3389/fsurg.2021.646629
- Wei, L., Hu, Y., Tao, Y., Hu, R., & Zhang, L. (2022). The effects of physical exercise on the quality of life of healthy older adults in China: A systematic review. Frontiers in Psychology, 13), https://doi.org/10.3389/fpsyg.2022.895373
- WHO. (2022). The impact of COVID-19 on mental health cannot be made light of. World Health Organization. https://www.who.int/news-room/feature-stories/detail/the-impact-of-covid-19-on-mental-health-cannot-be-made-light-of
- Wu, Y. H., Hsu, Y. J., & Tzeng, W. C. (2022). Physical activity and health-related quality of life of patients on hemodialysis with comorbidities: A cross-sectional study. International Journal of Environmental Research and Public Health, 19(2), https://doi.org/10.3390/ijerph19020811
- Yeni, K., Tulek, Z., & Terzi, M. (2022). A year with the fear of COVID-19 in multiple sclerosis patients: Examination of depression, sleep quality and quality of life before and after the pandemic. Multiple Sclerosis and Related Disorders, 57, 103370. https://doi.org/10.1016/j.msard.2021.103370
- Yoon, I. J., & Lee, S. J. (2023). Health literacy and anxiety among hemodialysis patients during the coronavirus disease pandemic. Psychology Research and Behavior Management, 16:1051–1061. doi:10.2147/PRBM.S395479