ABSTRACT
Objectives
This study aimed to characterize distinct patterns of change in health beliefs and their dimensions of COVID-19 vaccination and to evaluate the predictors of various trajectory groups.
Methods
A total of 1129 participants who completed two doses of COVID-19 vaccines in China were included in this prospective study. Participants’ characteristics and health beliefs regarding COVID-19 vaccination were collected before and after the two doses of COVID-19 vaccination. A group-based trajectory model was used to identify the distinct longitudinal patterns of health beliefs and their dimensions. A multinomial logistic regression model was conducted to determine the predictors of different trajectory groups.
Results
The group-based trajectory model identified two to four distinct patterns of global health beliefs and their domains, namely, very low-stable (16.1%), low-stable (30.2%), medium-stable (45.6%), and high-stable (8.1%) trajectories for global health beliefs. And the five domains of health beliefs showed two or three trajectory stable progression, which were similar to the global health beliefs trajectories. Sex, occupation post, adverse reactions foreboding, and quality of life were associated with the trajectory of global health beliefs or at least one domain of health beliefs.
Conclusions
During the study, individuals’ health beliefs about COVID-19 vaccination were stable without the interference of external factors. Based on the impact of sex, occupation post, adverse reactions foreboding, and quality of life on individuals’ health beliefs, personalized interventions can be developed to improve public health beliefs about COVID-19 vaccination and reduce vaccination hesitancy.
Introduction
Coronavirus disease 2019 (COVID-19) is a new acute respiratory infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that has become a major global public health concern.Citation1 The virus, SARS-CoV-2, can cause massive inflammatory responses, resulting in local and systemic tissue damage.Citation2 The COVID-19 pandemic has seriously threatened global health, economics, and social stability.Citation3 There are no specific antiviral treatments of COVID-19 through its pandemic is continuing to wreak havoc across the world albeit in a more subdued manner compared to the initial days. Vaccination against COVID-19 has become one of the most effective and cost-effective interventions for controlling and preventing the viral disease.Citation4 Although many new SARS-CoV-2 variants (e.g., Omicron) have shown strong immune escape to COVID-19 vaccines, it is undeniable that the vaccines still play a crucial role in reducing the severity of the disease, its incidence, and fatality rate.Citation5,Citation6 Moreover, the risk of sudden breakthrough of infection increases with the length of time from the initial vaccination, as the vaccine-induced neutralizing antibody titers decrease over time.Citation7 Hence, additional doses of COVID-19 vaccines are pivotal to broaden neutralizing antibody responses against SARS-CoV-2 variants.
As series of reports about vaccine side-effects and vaccine scandals, and the relatively stable prevention and control of COVID-19, hesitancy, and distrust of COVID-19 vaccination have been increasing.Citation8,Citation9 Many studies have been conducted to explain COVID-19 vaccine acceptance by different theories, such as the theory of planned behavior,Citation10 protection motivation theoryCitation11and the health belief model.Citation12 Based on the theory of planned behavior, individuals’ attitudes, subjective norms, and perceived behavioral control are critical factors for predicting their intentions to get vaccination.Citation10 Protection motivation theory is a social cognition theory that can predict an individual’s self-protective motivation about perceived threat and is considered a good candidate theory to understand the underlying reasons for individual’s intention to uptake vaccination.Citation11 Compared to these two theories, health belief model is one of the most commonly used theories in explaining and predicting health and illness behaviors.Citation12 According to health belief model, health beliefs refer to an individual’s view of health and disease, which mainly comprises perceived susceptibility, perceived severity, perceived benefits, perceived barriers, and cues to action.Citation12 Perceived susceptibility refers to individuals’ beliefs about the likelihood of contacting a disease, whereas perceived severity refers to individuals’ beliefs about the severity of the disease threatening their own health. In relation to vaccination, perceived benefits refer to individuals’ beliefs regarding the positive effects of vaccination, perceived barriers are defined as individuals’ beliefs regarding the obstacles to receiving vaccines, and cues to action refer to the external factors (such as information, events, and people) that guide individuals to receive vaccination. Health belief model stated that the stronger an individual’s health beliefs in maintaining their own health, the more likely they are to carry out healthy behaviors.Citation13 Nowadays, the health beliefs regarding COVID-19 vaccination seem to have undergone a change across various contexts, which has been confirmed as a dominant factor associated with the acceptance rate of COVID-19 vaccination.Citation14 Hence, it is crucial to explore the health beliefs regarding COVID-19 vaccination at various stages in population and understand their predictors, which of great theoretical and practical significance for the formulation of national epidemic prevention and control policies.
Group-based trajectory model (GBTM) is an application of a finite mixture model aimed at identifying clusters of individuals with similar development progression patterns.Citation15 It explores various trajectories for populations longitudinally by mapping the development of an outcome over time, which account for populations’ variable behavioral patterns. Therefore, it is helpful to identify health beliefs about COVID-19 vaccination in groups of people who share common characteristics using GBTM.
In this regard, we investigated the health beliefs regarding COVID-19 vaccination before and after two doses of COVID-19 vaccines, aiming to develop group-based trajectories of participants who have similar characteristics and identify the predictors associated with each trajectory.
Methods
Study design and participants
This study was a prospective analysis of people who received COVID-19 vaccines in Shenzhen, China from 1 July 2021 to 1 September 2021. Participants’ health beliefs regarding COVID-19 vaccination before and after receiving COVID-19 vaccines were investigated using a self-administered questionnaire (Supplementary Material) based on health belief model. The first stage of the survey was conducted from 1 July 2021 to July 31, where 1383 participants received the first dose of COVID-19 vaccine and completed the self-administered questionnaire before and after the vaccine was administered. The second stage of the survey was conducted from 1 August 2021 to 1 September 2021, with 1170 participants who received the second dose of COVID-19 vaccine and completed the self-administered questionnaire before and after the vaccine. Finally, 1129 participants who received both doses of COVID-19 vaccines and completed two stages of survey were included in our study cohort. In our cohort, all participants completed a self-administered questionnaire three times (before the first dose of COVID-19 vaccination, after the first dose of COVID-19 vaccination, and after the second dose of COVID-19 vaccination) and were thereafter included in the final data analysis. The study design is illustrated in . This study was approved by the Ethics Committee of Shenzhen Bao’an District Traditional Chinese Medicine Hospital (approval number: KY202101001).
Survey instrument
A self-administered questionnaire based on health belief model was developed using the Delphi method by a panel of epidemiologists, clinicians, and public health specialists to assessed (1) sociodemographic characteristics, (2) vaccine-related characteristics, (3) quality of life, and (4) health beliefs about COVID-19 vaccination. (see Supplementary Material)
Sociodemographic characteristics included sex, age, marital status, education level, occupation post, health insurance and suffering from a chronic disease.
Vaccine-related characteristics included vaccine type and adverse reactions foreboding. Adverse reactions foreboding is an apprehension of adverse reactions after COVID-19 vaccine injection, which was collected by asking the question, “Do you feel that you will have adverse reactions after receiving COVID-19 vaccination?”
Quality of life was assessed using a 12-item short-form (SF-12) health survey, previously designed and developed by Ware et al.Citation16 It measures eight health concepts using eight subscales: physical functioning (two items), role-physical (two items), bodily pain (one item), general health (one item), vitality (one item), social functioning (one item), role-emotional (two items), and mental health (two items). The eight health concepts are summarized into physical component summary (PCS, which is weighed by physical functioning, role-physical, bodily pain, and general health) and mental component summary (MCS, which is weighed by role-emotional, vitality, mental health, and social functioning). Both PCS and MCS were scored using norm-based methods. The higher the score, the better the participants’ quality of life. In this study, the overall Cronbach’s α coefficient of the SF-12 scale was 0.800, and the Cronbach’s α coefficients of PCS and MCS were 0.715 and 0.714, respectively.
Health beliefs about COVID-19 vaccination were measured using health belief scale. The health belief scale has a solid theoretical background as it was adapted from previously well-designed scale and developed by two rounds of expert consultation, which is based on health belief model.Citation12–17–Citation20 The health belief scale comprises five dimensions: (1) perceived susceptibility, which refers to the participants’ perception of the possibility of being infected by COVID-19, measured by three items; (2) perceived severity, which refers to the participants’ perception of the severity of COVID-19 threatening their health, measured by three items; (3) perceived benefits, referring to an individual’s perception of the positive health outcomes of receiving COVID-19 vaccines, measured by three items; (4) perceived barriers, referring to participants’ perception of obstacles to receiving COVID-19 vaccines, measured by five items; and (5) cues to action, which refers to the influence of external factors (such as recommendation from doctors on COVID-19 vaccination or health education messages) on prompting people to get COVID-19 vaccination, measured by six items. The responses were measured on a 5-point-Likert scale depicting how they agreed with each statement. The summed score for each dimension was calculated accordingly, and the score of global health beliefs about COVID-19 vaccination was calculated using five dimensions’ summary scores. The score of global health beliefs was 20 to 100, with the higher the score, the better the participants’ health beliefs about COVID-19 vaccination (however, the higher the score, the lower the perceived barriers). The participants were more likely to adopt preventive behaviors if they perceived that they were susceptible to infection, the outcomes of infecting disease were severe, the behaviors adopted were beneficial, the barriers were minimal, or cues to action were high.Citation13,Citation21 The Cronbach’s α coefficient of the entire health belief scale and its five dimensions ranged 0.76–0.89, showing good internal consistency reliability. The content validity index (S-CVI) of the entire health belief scale was 0.80, and the content validity index of each item (I-CVI) ranged from 0.90 to 1.00, indicating good content validity.
Data analysis
Descriptive statistics were performed for participants characteristics including mean and standard deviation for continuous variables and frequency and percentage for categorical variables.
Group-based trajectory modeling
Group-based trajectory models can identify clusters of individuals with different developmental trajectories in a cohort.Citation22 In this study, individuals in the same clusters following similar progressions in targeted behavior over time. The group-based trajectory model can capture different symptom patterns over time using a variety of straight and curved trajectories. Each trajectory revealed a distinct pattern for each of the three outcomes. For model selection, it was crucial to determine the number of groups and shape of each group. Different models have different numbers of groups and shapes and must be compared to find the best-fit model. To find the best-fit model, we used the following statistical criteria and model-fit indices:Citation15 (1) average posterior probability (AvePP): which measures the probability of a group individual belonging to this specific trajectory group. The AvePP of group membership for each group was set at greater than 0.7. (2) A minimum membership of 5% is required in each specific trajectory group, based on the posterior probability of the group member. (3) Bayesian information criterion (BIC): BIC values were compared between the different models. Smaller BIC values denote a better-fit model. In our analysis, according to criteria described above, we first set all groups as a quadratic equation to fit two to four groups models in turn to determine the optimal number of groups and then determined the optimal shape of each group. Furthermore, clinical relevance and usability in practice are also important considerations when selecting the best model.Citation23
For all outcomes, the differences in trajectory groups from the final model among different participants characteristics were assessed using univariate analysis (chi-square test for categorical variables and ANOVA for continuous variables). Variables with p < 0.05 in univariate analysis were included in the multinomial logistic regression to determine independent predictors of each trajectory group.
The software used in the GBTM was Stata version 16 (StataCorp LLC). An added-on user-written Stata command called “Traj,” developed by Jones et al. was used for trajectory modeling.Citation24 Other statistical analyses were performed using SPSS version 23. P values of 0.05 or less were determined to be statistically significant throughout.
Results
Study cohort characteristics
The final data analysis included 1129 participants who completed both the stage I and stage II surveys and received two doses of COVID-19 vaccines (). The baseline characteristics of the participants are presented in . Among the total, 67.4% were men, 14.5% were 40 and older years old, 62.8% were unmarried, and 39.9% were farmers or industrial workers. The education level of nearly half of the respondents were junior high or below (42.2%). Almost all participants had health insurance (84.6%) and did not have any chronic diseases (92.7%). At the first assessment time point, participants’ heath beliefs regarding COVID-19 vaccination scored 73.8 (10.2), which was medium to high.
Table 1. Participants’ baseline characteristics (N = 1129).
Trajectory analysis
According to the statistical criteria and model-fit indices described previously, we determined the best-fit trajectory model for health beliefs, and their five dimensions, and the two component summaries (PCS and MCS) of quality of life (see , and ).
Figure 2. (a) the four-group health beliefs trajectory (group 1: Very low-stable; group 2: Low-stable; group 3: Medium-stable; group 4: High-stable). (b) the two-group perceived susceptibility trajectory (group 1: Low-stable; group 2: High-stable). (c) the three-group perceived severity trajectory (group 1: Low-stable; group 2: Medium-stable; group 3: High-stable). (d) the two-group perceived benefits trajectory (group 1: Low-stable; group 2: High-stable). (e) the three-group perceived barriers trajectory (group 1: Low-stable; group 2: Medium-stable; group 3: High-stable). (f) the three-group cues to action trajectory (group 1: Low-stable; group 2: Medium-stable; group 3: High-stable).
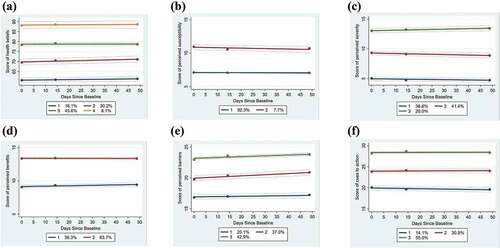
Figure 3. (a) the three-group physical component summary trajectory (group 1: Low-declining; group 2: Medium-stable; group 3: High-slow increasing-stable). (b) the three-group mental component summary trajectory (group 1: Low-declining; group 2: Medium-stable; group 3: High-stable).
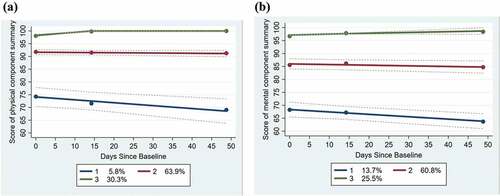
Table 2. Summary of group-based trajectory analysis.
Two to four distinct trajectories were identified in the selected model for global health beliefs and their domains (). For the global health beliefs trajectory, four subgroups started at very low (16.1%), low (30.2%), medium (45.6%) and high (8.1%) level, respectively, and then remained stable over time ( A). The five domains of health beliefs showed two or three trajectory groups with stable progression, which were similar to the global health beliefs trajectories ( B, C, D, E, F).
Predictors related to trajectory subgroup membership
For each outcome, variables with p < 0.05 in the univariate analysis were further examined using multinomial regression analysis to identify the effect of independent characteristics on trajectory groups. As for the global health beliefs trajectory (), as compared to the trajectory of very low-stable global health beliefs: enterprise staffs had a higher likelihood of being in the medium-stable global health beliefs trajectory; the PCS trajectory of medium-stable had a lower likelihood of being in the high-stable global health beliefs trajectory; the MCS trajectory of low-declining had a lower likelihood of being in the low-stable, medium-stable and high-stable global health beliefs trajectory; the MCS trajectory of medium-stable had a lower likelihood of being in the medium-stable and high-stable global health beliefs trajectory. As for the perceived susceptibility trajectory (), the PCS trajectory of low-declining was more likely to be in the high-stable perceived susceptibility trajectory than the low-stable perceived susceptibility trajectory. As for perceived severity trajectory (), as compared to the low-stable perceived severity trajectory: men had a higher likelihood of being in the high-stable perceived severity trajectory; those who did not have adverse reactions foreboding were less likely to be in the medium-stable and high-stable perceived severity trajectory; the PCS trajectory of low-declining was more likely to be in the medium-stable and high-stable perceived severity trajectory; the PCS trajectory of medium-stable had a higher likelihood of being in the medium-stable perceived severity trajectory. As for the perceived benefit trajectory (), the PCS trajectory of low-declining and medium-stable, and the MCS trajectory of low-declining and medium-stable had a lower likelihood of being in the high-stable perceived benefits trajectory than the low-stable perceived benefits trajectory. As for perceived barriers trajectory (), as compared to the low-stable perceived barriers trajectory: enterprise staffs had a higher likelihood of being in the medium-stable and high-stable perceived barriers trajectory; participants who did not have adverse reactions foreboding were more likely to be in the high-stable perceived barriers trajectory; the PCS trajectory of low-declining and medium-stable, and the MCS trajectory of low-declining and medium-stable had a lower likelihood of being in the high-stable perceived barriers trajectory. As for the cues to action trajectory (), compared to the low-stable cues to action trajectory: enterprise staffs had a higher likelihood of being in the medium-stable and high-stable cues to action trajectory; the PCS trajectory of low-declining and medium-stable, and the MCS trajectory of low-declining and medium-stable had a lower likelihood of being in the high-stable cues to action trajectory.
Table 3. Multinomial logistic regression to assess predictors associated with global health beliefs trajectory.
Table 4. Multinomial logistic regression to assess predictors associated with perceived susceptibility and perceived severity trajectory.
Table 5. Multinomial logistic regression to assess predictors associated with perceived benefits, perceived barriers and cues to action trajectory.
Discussion
To our knowledge, this study is the first to examine the group trajectory of health beliefs and their domains regarding COVID-19 vaccination across the period of completion two doses of COVID-19 vaccination and to identify the predictors associated with these group trajectories. The level of health beliefs regarding COVID-19 vaccination in this study can be measured by the health belief scale with numerical values, as it has been proven to have good reliability (Cronbach’s α = 0.76 0.89) and validity (CVI = 0.80 1.00). Previous studies have confirmed that some aspects of beliefs can be statistically analyzed in the form of numbers.Citation20–25–Citation28 Many scholars developed questionnaires with numerical values based on the health belief model to measure an individual’s health beliefs about various diseases and health behaviors, such as oral health beliefs in adolescence,Citation25 popular beliefs about COVID-19 infection risks,Citation27 beliefs about colorectal cancer screening prevention,Citation20 and health beliefs about breast screening behaviors.Citation28
In this study, two to four distinct trajectories were identified in global health beliefs and their five domains, which showed similar stable progression trajectories (). We can understand the progression patterns of the health belief trajectory from the perspective of the formation process of belief. Belief refers to the psychological cognition, emotional reactions, and behavioral tendency of individuals toward specific events or information.Citation29 The formation or change of beliefs or attitudes must go through three processes: compliance, identification, and internalization.Citation30,Citation31 Compliance is the act of changing one’s behavior as per requirement, but they do not believe that it is the right thing to do. Identification is the idea that individuals change their belief, behavior, or both because the valued “others” do it and it can help them maintain or develop a particular social status. And internalization is described as a complete change of individuals’ belief and behavior because they believe it is right, rather than being influenced by others. The formation of belief does not develop sequentially according to the three processes, but goes through these steps repeatedly, something becoming stable at a certain stage. That is to say, in a brief period, the initial health belief level almost determines the final health belief level and behavioral tendency without the interference of external factors.
Prior studies have found that health beliefs are important predictors of individuals’ quality of life,Citation32–34 while the current study found that quality of life is also a crucial predictor of individuals’ health beliefs. Our study found that participants who were in a low-declining PCS trajectory were more likely to be in a low-stable perceived benefits, perceived barriers, and cues to action trajectory. The low-declining PCS trajectory expressed low PCS scores during the period in which two doses of the COVID-19 vaccination, and this level decline over time, which may be related to the adverse reactions of the vaccine. Individuals with low physical status were more likely to have adverse reactions after COVID-19 vaccination, and having had high side-effects symptoms after the first vaccination was predictive of more severe symptoms after the second vaccination.Citation35 Evidently, individuals’ concerns about the safety of COVID-19 vaccines may reduce their perception of the benefits of COVID-19 vaccination. Under the dual influence of physical discomfort and psychological concerns, people will have higher mental barriers to COVID-19 vaccination. This also showed that groups with adverse reactions foreboding were more likely to be in a low-stable perceived barriers trajectory and a high-stable perceived severity trajectory. There is no doubt that concerns about the side-effects and efficacy of vaccines are the dominant barriers for people to receive vaccines.Citation36 Although there are many COVID-19 vaccines available worldwide, it is necessary to enhance the safety and efficacy standards of COVID-19 vaccines and explore safer and more effective COVID-19 vaccines with the emergence of the immune escape of SARS-CoV-2 mutant variants.
Furthermore, the current study found that groups with low-declining PCS trajectory were more likely to be in a high-stable perceived susceptibility and perceived severity trajectory, and which is mostly explained by the different risks and outcomes of COVID-19 infection among people with different levels of physical health. Individuals who have been running errands despite poor health conditions are more vulnerable to getting infected with the COVID-19 virus.Citation37 Previous studies reported that patients with comorbidities (such as hypertension, coronary artery disease, obesity, and chronic kidney disease) and immunocompromised patients had poorer COVID-19 outcomes and a higher risk of developing a complicated COVID-19 infection, in addition to higher mortality rates.Citation37–40 Moreover, COVID-19 produces more severe symptoms and higher mortality among men than women which may account for our findings that men were more likely to be in the high-stable perceived severity trajectory compared to women.Citation41,Citation42
It is worth noting that groups in low-declining or medium-stable PCS trajectories were more likely to be in the very-low global health beliefs trajectory, although they trended to be in the high-stable perceived susceptibility and perceived severity trajectories, probably since the high perception of barriers to COVID-19 vaccination and the low perception of benefits about COVID-19 vaccination overrides the high perception of susceptibility and severity about COVID-19. Surprisingly, a previous study found that fake or faulty COVID-19 vaccines were not a significant barrier to vaccination willingness because the high perception of severity and consequences of COVID-19 infection overrides concerns about fake or faulty vaccines.Citation36 A previous study indicated that individuals who perceived infection with COVID-19 as serious were more likely to accept vaccines.Citation17 Hence, warranting public enlightenment in terms of not underestimating the severity of COVID-19 and the possibility of outbreak resurgence is necessary. Individualized health education strategies should be developed to enhance the public’s perception of the severity of COVID-19 and their trust in COVID-19 vaccines, especially among women. Efforts are needed to increase vaccination uptake and confidence among people, particularly among people with low quality of life, by removing barriers to access and addressing concerns about vaccines. Enhancing community participation and engagement in containing and managing COVID-19, addressing tailored vaccine education and awareness to highlight the importance of vaccines, and clarifying misinformation are necessary, which can promote wellbeing and resilience through social identification and cohesion.Citation43
The MCS had similar influence on health beliefs regarding COVID-19 vaccination as PCS. Similar to PCS, individuals who were in a low-declining MCS trajectory were more likely to be in low-stable perceived benefits, perceived barriers and cues to action trajectories. In contrast to PCS, MCS had no effect on the perceived susceptibility and perceived severity trajectories. This is mostly explained by the different effects of physical and mental health on the risk of COVID-19 and disease prognosis.Citation37 Physical health has a significant impact on the risk of COVID-19 infection and disease outcome, whereas mental health has a negligible impact on these.Citation44–46
Furthermore, our study found that enterprise staffs were more likely to be in the high-stable perceived barriers and cues to action trajectories, which may be attributed to the high mobility of the working environment, absence of workplace safety, and low stability of career status among enterprise staffs.Citation47–49 These occupational factors exacerbated the psychological insecurity of enterprise staffs during the COVID-19 pandemic, indicting a higher demand for COVID-19 vaccination.Citation47
In view of the previously described factors affecting the trajectory of health beliefs, tailored interventions should be implemented to increase the public’s health beliefs about COVID-19 vaccination, which can address the public’s vaccine hesitancy despite vaccine equity.Citation12,Citation13,Citation17 For example, individualized health education based on gender should be implemented to increase the perceived severity of the infection, especially among women, as they tend to be in a very-low stable perceived trajectory. For individuals with low quality of life, health education should focus on advocating the benefits of COVID-19 vaccination and the low rate of adverse reactions to reduce their distrust and concerns regarding vaccination. Groups with high occupational exposure should strengthen their education on preventive health behaviors and prioritize getting vaccinated. Furthermore, enhancing the participation of communities in managing COVID-19 vaccination, such as ‘door-to-door vaccination’ services for the older adults or those with limited mobility, can effectively address vaccination hesitancy.Citation43
In underdeveloped or developing nations, where COVID-19 is continues to spread, health beliefs regarding COVID-19 vaccination may be higher compared to China, as they have a higher risk of being infected by COVID-19. The health belief model can also be used to identify individuals’ health beliefs regarding COVID-19 vaccination and the influencing factors in these countries, except for in China, as it has been confirmed as one of the most commonly used models to explain and predict health and illness behaviors worldwide.Citation12–Citation13-18–Citation21-27 Many studies have been conducted based on health belief model to assess preventive health behaviors associated with COVID-19.Citation19,Citation50
Limitations
It is worth noting a few limitations of this study when interpreting the results. First, the small number of measurement time points may have affected the estimated trajectory group shape and classes. Future follow-up studies with more time measurements are necessary to add more information for trajectories identified, as well as associated factors of health beliefs about COVID-19 vaccination. Second, the voluntary rather than random selection of participants may account for selection bias. Third, the health beliefs in individuals who received a single dose, no dose of vaccine, were immunocompromised, or had comorbidities (particularly diabetes and hypertension) were not evaluated in this study, as they might have shown different health beliefs trajectories than the people who have completed two doses of the COVID-19 vaccination. The differences of health beliefs about COVID-19 vaccination among these groups should be estimated in the future. Fourth, health beliefs are different from blood pressure or, blood levels, or platelet counts; using a questionnaire to measure these values may not reflect the true conditions of the individual; due to the self-report responses, there may be self-reporting bias and a tendency to report socially desirable responses. Future studies should identify a more scientific and reasonable method for measuring health beliefs. Fifth, this study did not control for people’s trust in the healthcare system which was considered as an important confounder.Citation51 Sixth, this study did not use a standardized instrument (i.e., Motors/Drivers of COVID-19 Vaccination Acceptance Scale) to understand beliefs regarding the COVID-19 vaccine.Citation52–56 Finally, high health beliefs regarding COVID-19 vaccination do not necessarily translate to actual health promotion behavior. Despite these limitations, we believe that our findings contribute tremendously to understanding public health beliefs about COVID-19 vaccination and promote the progression of a country’s immunization program.
Conclusion
In conclusion, the group-based trajectory model featured in this study reveals the progression patterns of health beliefs and their dimensions over time. Several factors (including sex, occupation post, adverse reactions foreboding and quality of life) were associated with each trajectory providing valuable information on how to improve health beliefs regarding COVID-19 vaccination. Our findings have important implications for facilitating government authorities to design and deliver targeted intervention programs to improve individuals’ preventive behaviors and promote the progression of a country’s immunization program.
Abbreviations
Authors’ contributions
We attest that each author has provided substantial contributions to the conception and design of the study, participate the investigation, and write a draft or revision of the article. LLK and YJW performed the statistical analyses and drafted the original manuscript. THT and CWC participated in the methodology assessment, interpreting the results and in drafting the manuscript. SZX and HL performed the investigation. All authors read and approved the final manuscript.
Ethics approval
This study was approved by the Ethics Committee of Shenzhen Bao’an District Traditional Chinese Medicine Hospital (approval number: KY202101001). The aim of study and study procedure were explained to participants clearly before the study was conducted. The informed consent of respondents was implied on the completion of the questionnaire.
Supplemental Material
Download MS Word (55.9 KB)Acknowledgements
We would like to thank all participants of the study for their cooperation and support.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2091899.
Additional information
Funding
References
- Merad, M , Blish, CA , Sallusto, F , and Iwasaki, A. The immunology and immunopathology of COVID-19Science 2022;375(6585): 1–11. doi: 10.1126/science.abm8108.
- Anka AU, Tahir MI, Abubakar SD, Alsabbagh M, Zian Z, Hamedifar H, Sabzevari A, Azizi G. Coronavirus disease 2019 (COVID-19): an overview of the immunopathology, serological diagnosis and management. Scand J Immunol. 2021;93(4):e12998. doi:10.1111/sji.12998.
- Alwan NA. Surveillance is underestimating the burden of the COVID-19 pandemic. Lancet (London, England). 2020;396(10252):e24. doi:10.1016/s0140-6736(20)31823-7.
- Lurie N, Saville M, Hatchett R, Halton J. Developing Covid-19 vaccines at pandemic speed. N Engl J Med. 2020;382(21):1969–1973. doi:10.1056/NEJMp2005630.
- Garcia-Beltran WF, St Denis KJ, Hoelzemer A, Lam EC, Nitido AD, Sheehan ML, Berrios C, Ofoman O, Chang CC, Hauser BM, et al. mRNA-Based COVID-19 vaccine boosters induce neutralizing immunity against SARS-CoV-2 Omicron variant. Cell. 2022;185(3):457–466.e4. doi:10.1016/j.cell.2021.12.033.
- Accorsi EK, Britton A, Fleming-Dutra KE, Smith ZR, Shang N, Derado G, et al. Association between 3 doses of mRNA COVID-19 vaccine and symptomatic infection caused by the SARS-CoV-2 Omicron and delta variants. JAMA. 2022;327(7):639–651. doi:10.1001/jama.2022.0470.
- Lopez Bernal J, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, Stowe J, Tessier E, Groves N, Dabrera G, et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (delta) variant. N Engl J Med. 2021;385(7):585–594. doi:10.1056/NEJMoa2108891.
- Trogen B, Oshinsky D, Caplan A. Adverse consequences of rushing a SARS-CoV-2 vaccine: implications for public trust. JAMA. 2020;323(24):2460–2461. doi:10.1001/jama.2020.8917.
- Yang R, Penders B, Horstman K. Addressing vaccine hesitancy in China: a scoping review of Chinese scholarship. Vaccines. 2019;8(1):2. doi:10.3390/vaccines8010002.
- Fan C-W, Chen IH, N-Y K, Yen C-F, Lin C-Y, Griffiths MD, Pakpour AH. Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: an online survey study. Hum Vaccin Immunother. 2021;17(10):3413–3420. doi:10.1080/21645515.2021.1933687.
- Huang P-C, Hung C-H, Kuo Y-J, Chen Y-P, Ahorsu DK, Yen C-F, Lin C-Y, Griffiths MD, Pakpour AH. Expanding protection motivation theory to explain willingness of COVID-19 vaccination uptake among Taiwanese university students. Vaccines. 2021;9(9):1046. doi:10.3390/vaccines9091046.
- Wong LP, Alias H, Wong PF, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccin Immunother. 2020;16(9):2204–2214. doi:10.1080/21645515.2020.1790279.
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988;15(2):175–183. doi:10.1177/109019818801500203.
- Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, Fang H. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines. 2020;8(3):482. doi:10.3390/vaccines8030482.
- Nagin DS. Group-based modeling of development. Cambridge (MA): Harvard University Press; 2005.
- Ware J, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi:10.1097/00005650-199603000-00003.
- Wong MCS, Wong ELY, Huang J, Cheung AWL, Law K, Chong MKC, Ng RWY, Lai CKC, Boon SS, Lau JTF, et al. Acceptance of the COVID-19 vaccine based on the health belief model: a population-based survey in Hong Kong. Vaccine. 2021;39(7):1148–1156. doi:10.1016/j.vaccine.2020.12.083.
- Tao L, Wang R, Han N, Liu J, Yuan C, Deng L, Han C, Sun F, Liu M, Liu J, et al. Acceptance of a COVID-19 vaccine and associated factors among pregnant women in China: a multi-center cross-sectional study based on health belief model. Hum Vaccin Immunother. 2021;17(8):2378–2388. doi:10.1080/21645515.2021.1892432.
- Al-Metwali BZ, Al-Jumaili AA, Al-Alag ZA, Sorofman B. Exploring the acceptance of COVID-19 vaccine among healthcare workers and general population using health belief model. J Eval Clin Pract. 2021;27(5):1112–1122. doi:10.1111/jep.13581.
- Sung JJY, Choi SYP, Chan FKL, Ching JYL, Lau JTF, Griffiths S. Obstacles to colorectal cancer screening in Chinese: a study based on the health belief model. Am J Gastroenterol. 2008;103(4):974–981. doi:10.1111/j.1572-0241.2007.01649.x.
- Becker MH, Maiman LA, Kirscht JP, Haefner DP, Drachman RH. The health belief model and prediction of dietary compliance: a field experiment. J Health Soc Behav. 1977;18(4):348–366. doi:10.2307/2955344.
- Nagin DS, Odgers CL. Group-Based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6(1):109–138. doi:10.1146/annurev.clinpsy.121208.131413.
- Franklin JM, Shrank WH, Pakes J, Sanfélix-Gimeno G, Matlin OS, Brennan TA, Choudhry NK. Group-Based trajectory models: a new approach to classifying and predicting long-term medication adherence. Med Care. 2013;51(9):789–796. doi:10.1097/MLR.0b013e3182984c1f.
- Jones BL, Nagin DS. A note on a stata plugin for estimating group-based trajectory models. Sociological Methods Res. 2013;42(4):608–613. doi:10.1177/0049124113503141.
- Bishop F, Yardley L. The development and initial validation of a new measure of lay definitions of health: the wellness beliefs scale. Psychol Health. 2010;25(3):271–287. doi:10.1080/08870440802609980.
- Broadbent JM, Thomson WM, Poulton R. Oral health beliefs in adolescence and oral health in young adulthood. J Dent Res. 2006;85(4):339–343. doi:10.1177/154405910608500411.
- Costa MF. Health belief model for coronavirus infection risk determinants. Rev Saude Publica. 2020;54:47. doi:10.11606/s1518-8787.2020054002494.
- Noman S, Shahar HK, Rahman HA, Ismail S, Aljaberi MA, Abdulrahman MN. Factor structure and internal reliability of breast cancer screening champion’s health belief model scale in Yemeni women in Malaysia: a cross-sectional study. BMC Womens Health. 2021;21(1):437. doi:10.1186/s12905-021-01543-7.
- Kuzmanovic B, Rigoux L, Tittgemeyer M. Influence of vmPFC on dmPFC predicts valence-guided belief formation. J Neurosci. 2018;38(37):7996–8010. doi:10.1523/JNEUROSCI.0266-18.2018.
- Tinc PJ, Sorensen JA, Goodspeed MM, Jenkins PL. Do Cialdini’s “principles of influence” motivate safe practices on farms? J Agromedicine. 2021;1–12. doi:10.1080/1059924X.2021.1950591.
- Tinc PJ, Goodspeed MM, Sorensen JA. Understanding trends in PTO shielding using Kelman’s processes of change. J Agromedicine. 2021;26(2):193–198. doi:10.1080/1059924X.2020.1795030.
- Zelikovsky N, Nelson E. Illness perceptions and beliefs about medication: impact on health-related quality of life in adolescent kidney transplant recipients. Pediatr Transplant. 2021;25(3):e13988. doi:10.1111/petr.13988.
- Gomes AC, Rebelo MAB, de Queiroz AC, de Queiroz Herkrath APC, Herkrath FJ, Rebelo Vieira JM, et al. Socioeconomic status, social support, oral health beliefs, psychosocial factors, health behaviours and health-related quality of life in adolescents. Qual Life Res. 2020;29(1):141–151. doi:10.1007/s11136-019-02279-6.
- Johnson AC, Mays D, Rehberg K, Shad A, Tercyak KP. Knowledge and beliefs about oncofertility and associations with quality of life among adolescent and young adult survivors of pediatric cancer. J Adolesc Young Adult Oncol. 2018;7(4):424–429. doi:10.1089/jayao.2018.0014.
- Coggins SAA, Laing ED, Olsen CH, Goguet E, Moser M, Jackson-Thompson BM, Samuels EC, Pollett SD, Tribble DR, Davies J, et al. Adverse effects and antibody titers in response to the BNT162b2 mRNA COVID-19 vaccine in a prospective study of healthcare workers. medRxiv. 2021. doi:10.1101/2021.06.25.21259544.
- Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP, Marques ETA. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. PLoS Negl Trop Dis. 2020;14(12):e0008961. doi:10.1371/journal.pntd.0008961.
- Singu S, Acharya A, Challagundla K, Byrareddy SN. Impact of social determinants of health on the emerging COVID-19 pandemic in the United States. Front Public Health. 2020;8:406. doi:10.3389/fpubh.2020.00406.
- Meletis CD, Wilkes K. Immune competence and minimizing susceptibility to COVID-19 and other immune system threats. Altern Ther Health Med. 2020;26:94–99.
- Shahid Z, Kalayanamitra R, McClafferty B, Kepko D, Ramgobin D, Patel R, Aggarwal CS, Vunnam R, Sahu N, Bhatt D, et al. COVID -19 and older adults: what we know. J Am Geriatr Soc. 2020;68(5):926–929. doi:10.1111/jgs.16472.
- Dong G, Du Z, Zhu J, Guo Y, Gao W, Guo W, Wang T, Jiang B. The clinical characteristics and prognosis of COVID-19 patients with comorbidities: a retrospective analysis of the infection peak in Wuhan. Ann Transl Med. 2021;9(4):280. doi:10.21037/atm-20-4052.
- Takahashi T, Ellingson MK, Wong P, Israelow B, Lucas C, Klein J, Silva J, Mao T, Oh JE, Tokuyama M, et al. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature. 2020;588(7837):315–320. doi:10.1038/s41586-020-2700-3.
- White A. Men and COVID-19: the aftermath. Postgrad Med. 2020;132(sup4):18–27. doi:10.1080/00325481.2020.1823760.
- Kharshiing KD, Kashyap D, Gupta K, Khursheed M, Shahnawaz MG, Khan NH, Uniyal R, Rehman U. Quality of life in the COVID-19 pandemic in India: exploring the role of individual and group variables. Community Ment Health J. 2021;57(1):70–78. doi:10.1007/s10597-020-00712-6.
- Samaan F, Carneiro de Paula E, de Lima Souza FBG, Mendes LFC, Rossi PRG, Freitas RAP, Nakagawa FT, Maciel AT, Aranha S, Osawa E, et al. COVID-19-Associated acute kidney injury patients treated with renal replacement therapy in the intensive care unit: a multicenter study in São Paulo, Brazil. PloS One. 2022;17(1):e0261958. doi:10.1371/journal.pone.0261958.
- Petersen A, Bressem K, Albrecht J, Thieß H-M, Vahldiek J, Hamm B, Makowski MR, Niehues A, Niehues SM, Adams LC, et al. The role of visceral adiposity in the severity of COVID-19: highlights from a unicenter cross-sectional pilot study in Germany. Metabolism. 2020;110:154317. doi:10.1016/j.metabol.2020.154317.
- Lang S, Liu Y, Qu X, Lu R, Fu W, Zhang W, Wang H, Hong T. Association between thyroid function and prognosis of COVID-19: a retrospective observational study. Endocr Res. 2021;46(4):170–177. doi:10.1080/07435800.2021.1924770.
- Giorgi G, Lecca LI, Alessio F, Finstad GL, Bondanini G, Lulli LG, Arcangeli G, Mucci N. COVID-19-related mental health effects in the workplace: a narrative review. Int J Environ Res Public Health. 2020;17(21):7857. doi:10.3390/ijerph17217857.
- Sasaki N, Kuroda R, Tsuno K, Kawakami N. Workplace responses to COVID-19 associated with mental health and work performance of employees in Japan. J Occup Health. 2020;62(1):e12134. doi:10.1002/1348-9585.12134.
- Choudhari R. COVID 19 pandemic: mental health challenges of internal migrant workers of India. Asian J Psychiatr. 2020;54:102254. doi:10.1016/j.ajp.2020.102254.
- Shahnazi H, Ahmadi-Livani M, Pahlavanzadeh B, Rajabi A, Hamrah MS, Charkazi A. Assessing preventive health behaviors from COVID-19: a cross sectional study with health belief model in Golestan Province, Northern of Iran. Infect Dis Poverty. 2020;9(1):157. doi:10.1186/s40249-020-00776-2.
- Ahorsu DK, Lin C-Y, Yahaghai R, Alimoradi Z, Broström A, Griffiths MD, Pakpour AH. The mediational role of trust in the healthcare system in the association between generalized trust and willingness to get COVID-19 vaccination in Iran. Hum Vaccin Immunother. 2022;18(1):1–8. doi:10.1080/21645515.2021.1993689.
- Fan C-W, Chen J-S, Addo F-M, Adjaottor ES, Amankwaah GB, Yen C-F, Ahorsu DK, Lin C-Y. Examining the validity of the drivers of COVID-19 vaccination acceptance scale using Rasch analysis. Expert Rev Vaccines. 2022;21(2):253–260. doi:10.1080/14760584.2022.2011227.
- Yeh Y-C, Chen IH, Ahorsu DK, N-Y K, Chen K-L, P-C L, Yen C-F, Lin C-Y, Griffiths MD, Pakpour AH, et al. Measurement invariance of the drivers of COVID-19 vaccination acceptance scale: comparison between Taiwanese and Mainland Chinese-speaking populations. Vaccines. 2021;9(3):297. doi:10.3390/vaccines9030297.
- Chen I-H, P-L W, Yen C-F, Ullah I, Shoib S, Zahid SU, Bashir A, Iqbal N, Addo F-M, Adjaottor ES, et al. Motors of COVID-19 vaccination acceptance scale (MoVac-COVID19S): evidence of measurement invariance across five countries. Risk Manag Healthc Policy. 2022;15:435–445. doi:10.2147/RMHP.S351794.
- Chen I-H, Ahorsu DK, Ko N-Y, Yen C-F, Lin C-Y, Griffiths MD, Pakpour AH. Adapting the motors of influenza vaccination acceptance scale into the motors of COVID-19 Vaccination Acceptance Scale: Psychometric evaluation among mainland Chinese university students. Vaccine. 2021;39(32):4510–4515. doi:10.1016/j.vaccine.2021.06.044.
- Ahorsu DK, Lin C-Y, Chen IH, Ullah I, Shoib S, Zahid SU, Adjaottor ES, Addo F-M, Pakpour AH. The psychometric properties of motors of COVID-19 vaccination acceptance scale (MoVac-COVID19S): a dataset across five regions. Data Brief. 2022;42:108103. doi:10.1016/j.dib.2022.108103.