Abstract
Objective: To study the association between ventilatory function and cognitive and behavioral impairment in ALS patients accounting for the effects of pertinent covariates. Methods: Four hundred and eighty-one patients were identified from the Mayo Clinic Florida ALS registry who had concurrent forced vital capacity (FVC) and cognitive and behavioral testing using the ALS Cognitive Behavioral Screen (ALS-CBS). Multiple linear regression analysis was used to study the effects of FVC and relevant covariates on the ALS-CBS cognition score, subscores, and caregiver behavioral inventory. Results: FVC was positively correlated to the cognitive and behavioral subscores on the ALS-CBS (p < 0.001), and the correlation was independent of the effects of site of ALS onset, age, and years of education. Conclusion: Cognitive and behavioral function may be adversely affected by ventilatory impairment in ALS. The presence of cognitive and behavioral impairment warrants a detailed assessment of ventilatory function.
Keywords:
1. Introduction
Cognitive and behavioral impairment may occur in nearly half of ALS patients and negatively contributes to morbidity and survival (Citation1–3). Although cognitive and behavioral change is likely primarily attributable to neurodegenerative pathologic changes in the frontal and temporal lobes (Citation4,Citation5), ventilatory impairment may represent an additional contributing factor. Previous studies have suggested an association between decreased performance on cognitive testing and abnormal pulmonary function measures (Citation6–9). Improvement in cognitive function following the initiation of noninvasive ventilation has also been described (Citation10). These studies, however, were limited by small sample sizes, used cognitive testing not previously validated in ALS cohorts, and did not adequately account for the effects of other patient and disease factors affecting both ventilatory and cognitive function. Various individual patient and disease factors are interdependent upon one another in ALS; therefore, adjusting for multiple pertinent covariates in a large cohort is required to understand the individual effect on outcomes (Citation11). The purpose of this study was to further explore the relationship between forced vital capacity (FVC) and cognitive and behavioral function measured by the ALS Cognitive Behavioral Screen (ALS-CBS). The study benefits from a large cohort of ALS patients and the evaluation of potential confounders in multiple regression analysis.
2. Methods and materials
2.1. Subjects and data acquisition
The study was approved by the Mayo Clinic IRB (#16-009393). The Mayo Clinic Florida ALS Clinic registry was queried for patients satisfying the revised El Escorial criteria for probable or definite ALS who underwent cognitive and behavioral testing and assessment of ventilatory function for routine evaluation in the multidisciplinary clinic. The age at onset of first weakness, sex, site of onset of first weakness (bulbar or spinal), and disease duration from onset of first weakness were abstracted. The revised ALS functional rating scale (ALSFRS-R) was administered by the clinical team, and the total, bulbar, and motor function subscores were calculated. Screening assessment of cognition and behavior was performed routinely during the clinic visit using the ALS-CBS, which consists of a brief cognitive screen performed by the clinician and a written behavioral inventory (CBI) completed by the patient’s caregiver (Citation6). In addition to a total cognition score (CBS-T), the ALS-CBS also yields subscores from each of the following cognitive domains: concentration (CBS-C), attention (CBS-A), mental tracking and monitoring (CBS-T), and word initiation and retrieval (CBS-I). The ALS-CBS was administered by research coordinators formally trained by a neuropsychologist (OP). Pulmonary function was assessed by measurement of the FVC and maximal inspiratory pressure (MIP) with the patient sitting upright by a respiratory therapist. Prior to 2019, spirometry was performed using a Puritan Bennett Renaissance II Spirometry Kit and since 2019 using a Vyaire (CareFusion) (San Diego, CA). The best of three attempts of FVC and MIP were reported. FVC was reported as the percentage of predicted calculated using the NHANES III registry and the MIP reported as pressure in cm of H2O (Citation12).
2.2. Statistical analysis
Baseline patient characteristics were summarized using the median and interquartile range (IQR) for continuous variables and frequencies for categorical variables. To illustrate the ALS-CBS total cognition and behavioral inventory scores and subscores, means and standard deviation were calculated for groups of patients with FVC < 50%, 50–80%, and ≥80% of predicted. Correlation for each cognitive and behavioral score and the continuous variables FVC and MIP was measured using the Kendall tau B method.
Multiple linear regression analysis was performed to study the magnitude and significance of the relationship between each variable and the ALS-CBS cognition and behavioral inventory scores. Predictors used in the analysis included age at onset, months of disease duration at the time of evaluation, sex, and NIV usage at the time of evaluation, the bulbar and motor subscores of the ALSFRS-R, and either the FVC or MIP. The bulbar subscore of the ALSFRS-R was used in the analysis to understand the association of bulbar impairment with cognitive and behavioral function. The motor subscore of the ALSFRS-R rather than the total ALSFRS-R was used to avoid collinearity with the respiratory component of the ALSFRS-R and ventilatory function measures. The models were computed separately for FVC and MIP to see if the findings were consistent with different measures of ventilatory function. Standardized coefficients were used to compare the effect size of different predictors. Subjects with missing data were excluded from multiple regression analysis. A p value <0.05 was used to determine significance of correlation coefficients. Statistical analysis was performed using IBM SPMSS (version 25 for Windows, IBM, Armonk, NY).
3. Results
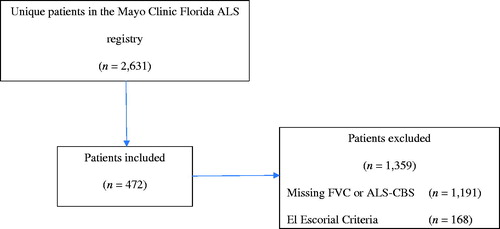
The cohort included 481 patients with clinically probable or definite ALS who had complete ALS-CBS cognitive testing and/or behavioral inventory data and either FVC or MIP. Missing spirometry data at the time of evaluation were the most common reason for exclusion (). The patient characteristics are summarized in . The median age of disease onset was 62 years (IQR 55–68), 229 subjects (47.6%) were female, and 126 (24.6%) had bulbar onset disease. Sixteen subjects (3.3%) had respiratory onset disease. Patients were evaluated at a median of 15 months (IQR 9–25 months) following reported onset of weakness. 18.5% of patients reported using noninvasive ventilation at the time of assessment. Of the 481 patients, 439 (91.2%) had a completed CBI and 480 patients completed the cognitive assessment. Based upon the cutoff values described by Woolley et al., 320 patients (63.4%) scored in the cognitively impaired range (CBS-T between 10 and 17), 127 (28.9%) scored in the behavioral impairment range (CBI < 36), and 62 (12.9%) met criteria for frontotemporal dementia (CBS-T ≤ 10). The CBS-T and the CBI were significantly correlated with FVC and MIP ().
Table 1 Patient characteristics.
Table 2 ALS Cognitive Behavioral Screen scores, mean (SD).
The results of the ALS-CBS are summarized in . The mean CBS-T, CBI, and subscores with the exception of concentration showed modest but significant correlations with both FVC and MIP. Multiple regression analysis revealed that both FVC and MIP were independently associated with the CBS-T and CBI scores (). In addition, age at onset (p < 0.001), the ALSFRS-R bulbar subscore, and years of education (p < 0.001) were also independently associated with CBS-T and the latter was also independently associated with CBI (p < 0.001). The standardized correlation coefficients for FVC and MIP were comparable to other statistically significant predictors. There was no statistically significant association seen with female sex, ALSFRS-R motor subscore, symptom duration, or usage of NIV at the time of evaluation.
Table 3 Linear regression analysis.
4. Discussion
This study explored the relationship between cognitive and behavioral impairment and ventilatory function in patients with ALS. Cognitive and behavioral function measured by the ALS-CBS was found to negatively correlate with ventilatory function in ALS patients. The ALS-CBS subscores of attention, tracking and monitoring, and verbal fluency were also shown to be negatively associated with ventilatory function. These relationships were independent of the age of ALS onset, years of education, and degree of bulbar and motor impairment. Although statistically significant, the magnitude of the associations between ventilatory measures and the ALS-CBS scores was modest. This is likely because the primary driver of cognitive and behavioral impairment in ALS is the underlying neurodegenerative process, and the results of our study suggest that poor ventilatory function may exacerbate cognitive and behavioral impairment.
Although previous studies have suggested associations between cognitive and behavioral impairment and ventilatory impairment in ALS patients, the findings in different cognitive and behavioral assessments have been inconsistent. A prospective study of 100 ALS patients demonstrated significantly worse scores in memory and attention measured by Addenbrooke’s Cognitive Examination in patients with FVC less than 75%, but no significant differences were seen in language, fluency, or visuospatial performance (Citation8). Another study also showed worse performance in memory retention and retrieval efficiency measured by the Rey Auditory Verbal Learning Test in ALS patients with nocturnal oxygen desaturations measured with nocturnal oximetry; however, there were no significant differences between groups in verbal fluency or the Frontal Assessment Battery in patients with or without desaturations (Citation13). Strutt et al. found no statistically significant differences in performance in a comprehensive neuropsychometric battery between patients with ventilatory impairment versus those without; however, caregiver-reported impairment measured by the Frontal Systems Behavioral Scale was higher in patients with ventilatory impairment. The differences in these studies and ours may in part be explained by differences in sample size and cognitive and behavioral assessment methodologies. Additionally, in these previous studies, the authors used FVC to dichotomize patients into groups of patients with and without ventilatory impairment which may have limited the statistical power to detect a significant relationship between ventilatory function and cognitive and behavioral measures (Citation14).
The severity of bulbar involvement measured by the ALSFRS-R in our study was associated with cognitive and behavioral scores. This finding is in agreement with prior studies which observed higher rates of cognitive and behavioral impairment in patients with bulbar onset (Citation15–17) in patients with bulbar onset. Age of ALS onset and year of education independently correlated with performance on the ALS-CBS, which are consistent with observations in many studies using cognitive testing. Motor impairment reported by the ALSFRS-R was also correlated with the CBI. This observation has previously been described and may relate to the difficulty in disentangling motor impairment with some frontal behavioral impairments such as apathy or social withdrawal (Citation6).
Cognitive impairment may be exacerbated by neuromuscular ventilatory failure by multiple mechanisms. Neuromuscular ventilatory failure is associated with sleep-disordered breathing, which can cause chronic intermittent hypoxia, hypoventilation, and sleep deprivation (Citation18). Nocturnal hypoventilation and hypoxemia associated with obstructive sleep apnea have been linked with cognitive impairment in the absence of known neurodegenerative disease leading to a similar pattern of cognitive impairment seen in ALS, including deficits in attention, memory, executive function, psychomotor function, and language (Citation19,Citation20). In an ALS mouse model, experimentally induced chronic intermittent hypoxia resulted in accelerated motor neuron death and cognitive dysfunction (Citation9). Chronic intermittent hypoxia has also been associated with NMDA-induced excitotoxicity and neuronal apoptosis promoted by upregulated p38MAPK expression (Citation21–23), both of which have been implicated in ALS pathogenesis (Citation24–29).
FVC is one of the most widely used measures of respiratory impairment in ALS; however, it may be insensitive to early ventilatory failure and unreliable in patients with bulbar dysfunction (Citation16,Citation30). Therefore, the 50% of predicted FVC threshold to initiate NIV proposed by the AAN consensus practice guidelines may not be sensitive to patients with early ventilatory failure (Citation31). Given timely institution of NIV has been shown to improve survival, quality of life, and slow progression of ventilatory weakness, a detailed inventory of clinical symptoms should be sought from patients with FVC values greater than 50% to screen for symptoms of early ventilatory failure (Citation32,Citation33). Although we recommend routine screening of ventilation and cognitive and behavioral function in the care of patients with ALS, any concern for cognitive and behavioral impairment should trigger a detailed assessment of ventilatory function (and vice versa) when routine assessment is not possible.
This study has important limitations. Low FVCs may be seen in patients with bulbar dysfunction in the absence of true respiratory muscle weakness due to difficulty maintaining a seal around the spirometer (Citation16). Some of the difference in cognitive and behavioral scores observed in groups with reduced FVC may be related to technically inadequate spirometry in conjunction with a higher frequency of cognitive impairment in patients with bulbar dysfunction. The effect of cognitive impairment on the quality of spirometry has not previously been studied in ALS patients, although studies examining the quality of spirometry in elderly patients have found cognitive dysfunction to be a significant cause of poor spirometry quality (Citation34,Citation35). Further studies using alternative means of assessing ventilatory function less reliant on patient factors, such as nocturnal oximetry and/or capnography, as well as peak cough flow are needed to better understand the effect of neuromuscular ventilatory failure on cognitive function in ALS.
Acknowledgements
The authors would like to acknowledge Dr. Kevin Boylan for the creation of the Mayo Clinic Florida ALS patient registry.
Declaration of interest
Jaimin Shah, MD – grants: MDA; industry grants: Corbus Pharmaceuticals. Otto Pedraza, Ph.D. – no pertinent disclosures or conflict of interest. Emir Festic – no pertinent disclosures or conflict of interest.
Data availability statement
The data that support the findings of this study are available from the corresponding author, JSS, upon reasonable request.
References
- Chiò A, Ilardi A, Cammarosano S, Moglia C, Montuschi A, Calvo A. Neurobehavioral dysfunction in ALS has a negative effect on outcome and use of PEG and NIV. Neurology. 2012;78:1085–9.
- Govaarts R, Beeldman E, Kampelmacher MJ, van Tol MJ, van den Berg LH, van der Kooi AJ, et al. The frontotemporal syndrome of ALS is associated with poor survival. J Neurol. 2016;263:2476–83.
- Ringholz GM, Appel SH, Bradshaw M, Cooke NA, Mosnik DM, Schulz PE. Prevalence and patterns of cognitive impairment in sporadic ALS. Neurology. 2005;65:586–90.
- Wilson CM, Grace GM, Munoz DG, He BP, Strong MJ. Cognitive impairment in sporadic ALS: a pathologic continuum underlying a multisystem disorder. Neurology. 2001;57:651–7.
- Lowe J. New pathological findings in amyotrophic lateral sclerosis. J Neurol Sci. 1994;124:38–51.
- Woolley SC, York MK, Moore DH, Strutt AM, Murphy J, Schulz PE, et al. Detecting frontotemporal dysfunction in ALS: utility of the ALS Cognitive Behavioral Screen (ALS-CBS). Amyotroph Lateral Scler. 2010;11:303–11.
- Strutt AM, Palcic J, Wager JG, Titus C, Macadam C, Brown J, et al. Cognition, behavior, and respiratory function in amyotrophic lateral sclerosis. ISRN Neurol. 2012;2012:912123.
- Huynh W, Sharplin LE, Caga J, Highton-Williamson E, Kiernan MC. Respiratory function and cognitive profile in amyotrophic lateral sclerosis. Eur J Neurol. 2020;27:685–91.
- Kim S-M, Kim H, Lee J-S, Park KS, Jeon GS, Shon J, et al. Intermittent hypoxia can aggravate motor neuronal loss and cognitive dysfunction in ALS mice. PLoS One. 2013;8:e81808.
- Newsom-Davis IC, Lyall RA, Leigh PN, Moxham J, Goldstein LH. The effect of non-invasive positive pressure ventilation (NIPPV) on cognitive function in amyotrophic lateral sclerosis (ALS): a prospective study. J Neurol Neurosurg Psychiatry. 2001;71:482–7.
- Traxinger K, Kelly C, Johnson BA, Lyles RH, Glass JD. Prognosis and epidemiology of amyotrophic lateral sclerosis: analysis of a clinic population, 1997–2011. Neurol Clin Pract. 2013;3:313–20.
- Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–87.
- Park S-Y, Kim S-M, Sung J-J, Lee K-M, Park K-S, Kim S-Y, et al. Nocturnal hypoxia in ALS is related to cognitive dysfunction and can occur as clusters of desaturations. PLoS One. 2013;8:e75324.
- Altman DG, Royston P. The cost of dichotomising continuous variables. BMJ. 2006;332:1080.
- Portet F, Cadilhac C, Touchon J, Camu W. Cognitive impairment in motor neuron disease with bulbar onset. Amyotroph Lateral Scler Other Motor Neuron Disord. 2001;2:23–9.
- Hadjikoutis S, Wiles CM. Respiratory complications related to bulbar dysfunction in motor neuron disease. Acta Neurol Scand. 2001;103:207–13.
- Strong MJ, Grace GM, Orange JB, Leeper HA, Menon RS, Aere C. A prospective study of cognitive impairment in ALS. Neurology. 1999;53:1665–70.
- Perrin C, Unterborn JN, Ambrosio CD, Hill NS. Pulmonary complications of chronic neuromuscular diseases and their management. Muscle Nerve. 2004;29:5–27.
- Olaithe M, Bucks RS, Hillman DR, Eastwood PR. Cognitive deficits in obstructive sleep apnea: insights from a meta-review and comparison with deficits observed in COPD, insomnia, and sleep deprivation. Sleep Med Rev. 2018;38:39–49.
- Saunamäki T, Jehkonen M. A review of executive functions in obstructive sleep apnea syndrome. Acta Neurol Scand. 2007;115:1–11.
- Ji W, Zhang Y, Ge RL, Wan Y, Liu J. NMDA receptor-mediated excitotoxicity is involved in neuronal apoptosis and cognitive impairment induced by chronic hypobaric hypoxia exposure at high altitude. High Alt Med Biol. 2020;22:45–57.
- Ren H, Qiu W, Lu Q, Peng C, Ding Y, Zhu B, et al. Potential contribution of microRNA-125b targeting p38MAPK to relieving intermittent hypoxia-induced dementia of rat models. J Clin Neurosci. 2019;64:234–41.
- Lladó J, Tolosa L, Olmos G. Cellular and molecular mechanisms involved in the neuroprotective effects of VEGF on motoneurons. Front Cell Neurosci. 2013;7:181.
- Bendotti C, Atzori C, Piva R, Tortarolo M, Strong MJ, DeBiasi S, et al. Activated p38MAPK is a novel component of the intracellular inclusions found in human amyotrophic lateral sclerosis and mutant SOD1 transgenic mice. J Neuropathol Exp Neurol. 2004;63:113–9.
- Bendotti C, Bao Cutrona M, Cheroni C, Grignaschi G, Lo Coco D, Peviani M, et al. Inter- and intracellular signaling in amyotrophic lateral sclerosis: role of p38 mitogen-activated protein kinase. Neurodegener Dis. 2005;2:128–34.
- Tolosa L, Mir M, Olmos G, Lladó J. Vascular endothelial growth factor protects motoneurons from serum deprivation-induced cell death through phosphatidylinositol 3-kinase-mediated p38 mitogen-activated protein kinase inhibition. Neuroscience. 2009;158:1348–55.
- Xu L, Guo YS, Liu YL, Wu SY, Yang C, Wu DX, et al. Oxidative stress in immune-mediated motoneuron destruction. Brain Res. 2009;1302:225–32.
- Heath PR, Shaw PJ. Update on the glutamatergic neurotransmitter system and the role of excitotoxicity in amyotrophic lateral sclerosis. Muscle Nerve. 2002;26:438–58.
- King AE, Woodhouse A, Kirkcaldie MT, Vickers JC. Excitotoxicity in ALS: overstimulation, or overreaction? Exp Neurol. 2016;275:162–71.
- Jackson CE, Rosenfeld J, Moore DH, Bryan WW, Barohn RJ, Wrench M, et al. A preliminary evaluation of a prospective study of pulmonary function studies and symptoms of hypoventilation in ALS/MND patients. J Neurol Sci. 2001;191:75–8.
- Miller RG, Jackson CE, Kasarskis EJ, England JD, Forshew D, Johnston W, et al. Practice parameter update: the care of the patient with amyotrophic lateral sclerosis: multidisciplinary care, symptom management, and cognitive/behavioral impairment (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2009;73:1227–33.
- Bourke SC, Bullock RE, Williams TL, Shaw PJ, Gibson GJ. Noninvasive ventilation in ALS: indications and effect on quality of life. Neurology. 2003;61:171–7.
- Bourke SC, Tomlinson M, Williams TL, Bullock RE, Shaw PJ, Gibson GJ. Effects of non-invasive ventilation on survival and quality of life in patients with amyotrophic lateral sclerosis: a randomised controlled trial. Lancet Neurol. 2006;5:140–7.
- Allen S, Yeung P, Janczewski M, Siddique N. Predicting inadequate spirometry technique and the use of FEV1/FEV3 as an alternative to FEV1/FVC for patients with mild cognitive impairment. Clin Respir J. 2008;2:208–13.
- Carvalhaes-Neto N, Lorino H, Gallinari C, Escolano S, Mallet A, Zerah F, et al. Cognitive function and assessment of lung function in the elderly. Am J Respir Crit Care Med. 1995;152:1611–5.