Abstract
Purpose
The therapeutic relationship between a patient and physiotherapist has been associated with improved physiotherapy outcomes. However, there is no agreed upon measure of therapeutic relationship in physiotherapy. This paper describes a validation study of a new patient-reported measure, the Physiotherapy Therapeutic Relationship Measure (P-TREM).
Methods
In this multi-site validation study, participants with musculoskeletal conditions (n = 163) completed a survey containing the P-TREM, demographic questions, a Trust in Healthcare Providers scale, and a therapeutic relationship global rating for construct validation. We investigated item quality, internal structure using exploratory factor analysis (EFA), unidimensionality, internal consistency, and construct validity. We eliminated poor performing items to optimise the length of the P-TREM.
Results
The final version of the P-TREM has 30 items. EFA suggests two domains: ‘Physiotherapist role’ and ‘Patient role’, correlation between factors was 0.71. Internal consistency was excellent. We found a low-moderate correlation between P-TREM scores and Trust in Healthcare Providers and a strong correlation between P-TREM scores and the therapeutic relationship global rating, confirming our hypotheses for convergent and concurrent validity.
Conclusions
The P-TREM can be considered for use in clinical research to understand therapeutic relationship in the care of people with longstanding musculoskeletal conditions in outpatient, in-person settings.
Introduction
Therapeutic relationship in physiotherapy can be defined as the safe relational space and affective bond between patient and practitioner, developed both professionally and personally, when establishing connections and engaging in the collaborative work of physiotherapy [Citation1]. The therapeutic relationship is gaining attention in physiotherapy as a contextual factor that may contribute to physiotherapy outcomes [Citation2].
Physiotherapy researchers often use Bordin’s tripartite model of working alliance (tasks, goals, bond) [Citation3] from psychotherapy to describe the therapeutic alliance or relationship in physiotherapy. It may be time to consider applying discipline-specific models, given the amount of qualitative research and syntheses of existing literature that exists about the concept of therapeutic relationship in physiotherapy [Citation1,Citation4–10]. While there are areas of overlap with psychotherapy, there are aspects of therapeutic relationship unique to physiotherapy [Citation11]. One key difference is that in physiotherapy, it is often through the patient’s body that the patient and physiotherapist connect in the relationship [Citation12]. This includes communicating about the patient’s body, physical symptoms or health condition, and also connecting through physical contact (i.e. touch) [Citation12].
Quantitative research on the therapeutic relationship in physiotherapy suggests that therapeutic relationship influences clinical outcomes for people with a variety of neurological, musculoskeletal and pain conditions, however there is some uncertainty about whether this influence is clinically important [Citation4,Citation13–20]. For the most part, these studies have been conducted using measures borrowed or adapted from psychotherapy [Citation4,Citation5,Citation17]. However, the validity of using psychotherapy measures in physiotherapy research is questionable given the differences between psychotherapy and physiotherapy therapeutic relationships. Indeed, studies of the measurement properties of psychotherapy measures used in physiotherapy have demonstrated issues with content validity and other measurement properties [Citation13,Citation17,Citation21–24]. More accurate and precise measurement of therapeutic relationship would allow researchers to establish whether clinically important cause-effect relationships exist between therapeutic relationships and outcomes (e.g. pain, physical function). It would also be useful for comparing the effectiveness of interventions aimed at improving therapeutic relationships and understand the relative importance of different components of therapeutic relationship (e.g. trust, individualised treatment, receptivity). Therefore, a discipline-specific, high-quality measurement instrument for capturing the therapeutic relationship in physiotherapy is needed.
With this in mind, we developed a measure of the therapeutic relationship in physiotherapy, called the Physiotherapy Therapeutic RElationship Measure (P-TREM) [Citation25]. The P-TREM is a patient-reported measure with 49 items based on 11 key concepts from Miciak’s Physiotherapy Therapeutic Relationship Framework [Citation1,Citation25,Citation26]. Initial development included generating a pool of potential items, review by experts (patients, clinicians, researchers), a study of content validity, and cognitive interviews with potential respondents [Citation25]. This paper describes a validation study examining the measurement properties and optimising the length of the P-TREM. The specific objectives are to:
Evaluate the quality of items in the P-TREM
Optimise P-TREM scale length through item reduction
Investigate the internal structure of the P-TREM using factor analysis
Comprehensively evaluate the measurement properties of the P-TREM (internal consistency, convergent and concurrent validity).
Methods
Study design
In developing the P-TREM, we adopted the 8-step measurement scale development process of DeVellis as described in Scale Development: Theory and Applications [Citation27]. This process was designed for measuring abstract, multifaceted phenomena – such as therapeutic relationship [Citation27]. Steps 1–4 guided the first phase of P-TREM development [Citation25]. Steps 5–8 guided this study: (5) Consider the inclusion of validation items; (6) Administer items to a development sample; (7) Evaluate the items; and (8) Optimise the scale [Citation27]. We used a cross-sectional, multi-site methodological study design. This study was approved by the University of Alberta’s Health Research Ethics Board (Study ID Pro00086206).
Study participants
Inclusion criteria
Inclusion criteria were: (1) individuals 16 years of age or older, (2) who received 3 or more physiotherapy sessions in the past 3 years, (3) for a condition affecting the musculoskeletal system, (4) in an outpatient in-person setting (e.g. hospital outpatient, publicly-funded rehabilitation and private practice clinics). The physiotherapy sessions must have been with the same physiotherapist, as we were interested in the interpersonal relationship developed between two individuals (physiotherapist and patient dyads). Individuals who did not have an adequate understanding of English (spoken or written) or cognitive impairment limiting their ability to interpret and respond to questions in the P-TREM were excluded. Participants from three patient population subgroups were recruited: (1) individuals with an inflammatory arthritic condition (e.g. rheumatoid arthritis, ankylosing spondylitis and psoriatic arthritis); (2) individuals with haemophilia and related inherited bleeding disorders; or (3) individuals with a musculoskeletal concern seeking treatment in a general physiotherapy practice. Individuals with chronic conditions like inflammatory arthritis and bleeding disorders are often followed by the same clinical team, including a physiotherapist, over long periods of time. This typically results in long-standing relationships between patients and physiotherapists. Individuals from all three populations were involved in the development of the P-TREM [Citation25].
Recruitment
Patients were recruited from 4 private physiotherapy centres and 4 chronic disease hospital-based clinics from June 2020–February 2021, using voluntary sampling techniques. Over these 8 clinics, there were 38 physiotherapists whose patients could have been included in the study. Recruitment coincided with the COVID-19 global pandemic. Recognising the impact of the pandemic on clinic resources, each clinic was given the autonomy to choose the recruitment strategy that would be least burdensome. In five clinics, physiotherapists identified and approached patients for participation, two clinics had independent research assistants approach eligible patients, and one clinic sent an email message to past patients informing them of the study and inviting them to participate. In addition, seven special interest groups representing patients with inherited bleeding disorders (n = 4) and inflammatory arthritis (n = 3) advertised the study to their members. All participants were told that the survey was anonymous, that their physiotherapists would not know whether they participated, and that the physiotherapists will not have access to their responses.
Data collection
Data were collected using an anonymous survey questionnaire that contained the preliminary P-TREM, a demographic questionnaire form, and two measures of related variables included for validation purposes and described below. Participants were given the choice to respond using an electronic, online format or a paper version. All data were collected anonymously. We aimed for a sample size of 245 using Norman and Streiner’s estimated requirements for conducting exploratory factor analysis (EFA) (i.e. a minimum of 5 respondents per item), which would also be sufficient for correlational analyses [Citation28]. However, recruitment was impacted by the global COVID-19 pandemic and our final sample included 169 respondents.
Measures
Physiotherapy RElationship measure (P-TREM)
Measurement purpose
The P-TREM is a patient-reported measure developed to capture the strength (i.e. magnitude) and quality (positive or negative) of a therapeutic relationship between a patient and a specific physiotherapist, as developed over multiple encounters, in the context of outpatient physiotherapy.
Target population
Adult, English-speaking patients with a condition affecting the musculoskeletal system seeking physiotherapy in an outpatient, in-person setting (e.g. hospital outpatient, community and private practice clinics), who have established relationships with their physiotherapist (i.e. not newly developed relationships).
Construct of interest
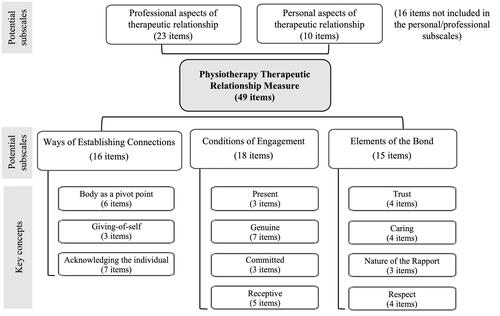
The measurement framework of the P-TREM is a reflective model based on Miciak’s Physiotherapy Therapeutic Relationship Framework [Citation1]. It is described in detail elsewhere [Citation25,Citation26]. Briefly, Miciak’s framework describes the therapeutic relationship between the physiotherapist and patient as having three components: (1) the actions they ‘do’ together that are part of the relationship (i.e. Ways of Establishing Connections); (2) the way they ‘are’ together (i.e. Conditions of Engagement); and (3) the feelings that exist between them (Elements of the Bond). Each component has 3–4 subcomponents which make up the 11 key concepts in the P-TREM measurement framework. In the preliminary version of the P-TREM, each concept was represented by 3–7 items, with the content of the items reflecting the patient’s perspective of those concepts.
Miciak’s Framework also includes three themes that are common to all components and were included in the content of the items. (1) The therapeutic relationship is professional and personal (i.e. it includes the physiotherapist’s professional responsibilities and the activities and goals of physiotherapy, as well as personal aspects like caring about and taking an interest in the other person apart from the activities they do together during rehabilitation). (2) The therapeutic relationship is a ‘mutual endeavor’ (i.e. both the physiotherapist and patient contribute to the therapeutic relationship), and (3) Body is central to the therapeutic relationship (i.e. the patient’s physical body is the main connecting point for the patient and physiotherapist).
Measurement specifications
The preliminary P-TREM had 49 items with a 6-point ordinal response scale (Likert-type) ranging from ‘Strongly disagree’ to ‘Strongly agree’. The total score is obtained by summing a person’s responses across all items, with the total score ranging from 0–245. In alignment with Miciak’s framework, two sets of subscales were proposed in the preliminary version of the P-TREM. The first set contained three subscales, one for each component of therapeutic relationship in the framework (Connections, Conditions, Bond). The second set had two subscales representing the ‘personal’ and ‘professional’ aspects of therapeutic relationship. The items in the personal and professional subscales do not represent unique content, rather they overlap with the items in the three component subscales. There are 16 items which were not deemed clearly professional or personal and were not included in these subscales. summarises the measurement framework and proposed scaling structure for the P-TREM. Supplementary File 1 contains the items in the preliminary version of the P-TREM.
Global rating of therapeutic relationship
We included a patient-reported global rating of the therapeutic relationship (GRTR) for the purpose of concurrent validation. The GRTR asked respondents to rate the overall quality of their relationship with their physiotherapist on a 10-point rating scale, with anchors ‘Very negative (i.e. poor)’ and ‘Very positive (i.e. excellent)’. Although it is unclear if a phenomenon such as a therapeutic relationship can be reliably measured using a single global judgement, there is evidence that a single global rating can be more reliable than a multi-item scale in the assessment of interpersonal and communication skills in a medical setting [Citation29,Citation30].
Trust in healthcare providers
We included a modified version of the ‘Trust in the Medical Profession’ measure of Dugan, Trachtenberg, & Hall (2005) [Citation31]. We modified the items by replacing the word ‘doctor’ with ‘healthcare providers’, which we called ‘Trust in Healthcare Providers’ (THCP). The measure has five items that assess patients’ trust in healthcare providers in general (i.e. not with a specific provider). Responses are on a 5-point Likert-type scale, ‘Strongly disagree’ to ‘Strongly agree’, summed to give a score that ranges from 5–25. Higher values indicate more trust. Internal consistency has been shown to be 0.77 in the general population [Citation31].
Data analyses
Analyses were carried out using Jamovi free and open statistical platform 32 and the ‘psych’ and ‘lavaan’ package in R [Citation33,Citation34,Citation35]. We calculated descriptive statistics for study participant characteristics. We ran a missing data sensitivity analysis by imputing minimum and maximum values to evaluate the potential impact of missing data. There were no meaningful differences in results (<2.5% change in estimates) when imputing minimum, mean, or maximum values. Therefore, we handled missing response data by imputing the mean response to that item.
Item quality analysis
We calculated descriptive statistics for the item responses (mean and median, minimum, maximum, and standard deviations of the responses), as well as the frequency of endorsement (i.e. the proportion of people choosing each response option), and non-response rates. We also created two inter-item correlation matrices, examining both Pearson product-moment and polychoric correlation coefficients. Finally, we examined corrected item-total correlations (i.e. total scale score with the item removed) for the items and the total P-TREM score. We used a Pearson product-moment correlation because it is robust enough against non-normality when calculating relationships between an item with >2 response alternatives and an assumed continuous variable such as total scale scores [Citation30].
Preliminary examination of internal structure
We examined correlations between each item and its corrected item-subscale score for each of the proposed subscales (Connections, Conditions, Bond, Personal and Professional). We compared each item’s correlation with each of the component subscale scores to examine how items fit within the proposed scaling structure of the instrument. We expected an item’s item-subscale correlation to be high with the subscale to which it belongs, and conversely, it’s correlation with the other subscales to be significantly lower.
Optimising scale length
We optimised the length of the P-TREM by examining item quality statistics as well as content. We began by eliminating items with lower corrected item-total correlations. Items were then grouped by content area and examined by one researcher (EM). Items with high inter-item correlation (i.e. greater than 0.8) with other item(s) in their grouping were flagged for further examination of their item quality statistics. Flagged items with one or more problems with the item’s response endorsement frequencies (i.e. non-response rates, item ceiling effects, or low variance of responses), or lower correlation with the corrected total P-TREM score were tentatively eliminated. A second member of the research team reviewed these decisions and disagreements were resolved through discussion. Where a pair of items with redundant content and/or high inter-item correlation had similar item quality statistics, items were eliminated based on the judgement of the two research team members (EM, MM), who relied on data from the instrument development phase [Citation25] and from their knowledge of therapeutic relationship in physiotherapy. Once items were eliminated, the reduced version of the P-TREM was examined to ensure that all 11 content areas were still covered by at least 1 item.
Exploratory factor analysis
This was the first examination of internal structure of the P-TREM, therefore we conducted exploratory factor analysis (EFA) using the ‘fa’ function from the ‘psych’ package in R [Citation33,Citation34]. We used the Kaiser–Meyer–Olkin Measure of Sampling Adequacy (MSA) and Barlett’s test of sphericity to check the factorability of our data. The eigenvalue one test and parallel analysis helped us determine the number of factors to extract. We used the principal axis factoring method with an oblique rotation because we expected our factors to be correlated. We used a critical value of 0.41 to determine whether a factor loading was considered significant, which was determined based on recommendations of Norman & Streiner [Citation28].
Unidimensionality check
We used confirmatory factor analysis (CFA) to assess the unidimensionality of all items in the reduced P-TREM. To do this, we fit a CFA model to the data set using the lavaan package in R with the ‘WSMLR’ estimator [Citation33,Citation35]. We used the criteria of Hu and Bentler: comparative fit index (CFI) >0.95; Tucker-Lewis Index (TLI) >0.95; the root mean square error of approximation (RMSEA) <0.06; and the standardised root mean residuals (SRMR) <0.08 to evaluate the fit of the model [Citation36].
Validation evidence
Descriptive statistics were calculated for the reduced version of the P-TREM total and domain scores, including ceiling effects (proportion of participants scoring the maximum on the P-TREM).
Measurement properties
Coefficient alpha
We calculated an estimate of reliability, co-efficient alpha (α), and a 95% confidence interval (CI) for the P-TREM total score and domain scores found in the EFA. We used Ponterotto & Ruckdeschel’s (2007) criteria for estimating adequacy of internal consistency co-efficient, which are based on sample size and number of items in the scale [Citation37].
Concurrent validation
We examined the magnitude of the association between GRTR and the total P-TREM and domain scores by calculating a Pearson product-moment correlation with a 95% CI. Since these variables are measures of the same construct, our hypothesis was that there would be large, positive associations between GRTR and all three scores (r greater than 0.5) [Citation38].
Convergent validation
We used Pearson product-moment correlation coefficients with a 95% CI to examine the strength of association between total and domain scores and the patients’ THCP scores. Trust in healthcare providers in general is moderately correlated with trust in a specific physician [Citation39]. Considering that trust is a part of therapeutic relationship, it is conceivable that the level of trust a person has in healthcare providers in general will be associated with therapeutic relationship. However, a high correlation with the P-TREM would indicate the P-TREM is not adequately capturing the relationship in a specific patient-physiotherapist dyad. We hypothesised there would be a small to moderate, positive correlation between patients’ trust in healthcare providers and the total and domain scores (r = 0.2 to 0.3) [Citation38].
In order to provide evidence specific to our patient population subgroups (i.e. inherited bleeding disorders, inflammatory arthritis and general musculoskeletal), we conducted the analyses above for the total sample, as well as analyses separated by patient population subgroup.
Results
Sample characteristics
Out of 169 participants, 166 individuals provided complete or nearly complete data (missing 3 or less responses to the P-TREM items). Three participants were excluded because their demographic questions indicated they did not meet eligibility criteria (e.g. <3 encounters with their physiotherapist), leaving 163 participants in the analysis. summarises participant characteristics for the entire sample. The average age was 43.2 years (sd = 16.6), 87 identified as female, 72 as male and 4 preferred not to answer, and 36.8% reported experiencing chronic or persistent pain. There were 87 in the general musculoskeletal patient subgroup, 43 in the inherited bleeding disorders subgroup and 33 in the inflammatory arthritis subgroup. The mean duration of relationship between the physiotherapist and patient was 53.7 months (sd = 73.0), median was 24 months (range = 3 weeks–30 years). The mean total number of appointments was 13.2 (sd = 17.6), the median was 8 (range = 3–150). Information on the characteristics of the inherited bleeding disorders and the inflammatory arthritis subgroups are available as Supplementary material (Supplementary File 2).
Table 1. Participant demographic and clinical characteristics.
Item quality analysis
All items showed a ceiling effect with the majority of participants choosing either the highest or second highest responses (agree, strongly agree) for all items. For two items, >80% of people chose the highest response category. The response options at the lower end of the scales (Disagree, Strongly Disagree) were under-utilized (less than 5%) in all items. Item non-response rates were low with 14 items missing only 1–3 responses. The mean inter-item polychoric correlation was 0.53 (min/max: 0.26–0.95), while the average corrected item-total correlation was 0.75 (min/max: 0.45–0.89). summarises key item analysis statistics from the preliminary version of the P-TREM.
Table 2. Item descriptive statistics.
Preliminary examination of internal structure
The item-total correlation matrix for the proposed subscales is included as Supplementary File 3. Upon examining the corrected item-subscale correlations for the component subscales (Connections, Conditions, Bond), there was no observable pattern suggesting that these proposed subscales were present. Correlation between the proposed Connections and Bond subscales was r = 0.93, between the Connections and Conditions was r = 0.94, and between the Conditions and Bond was r = 0.94.
With regards to the Personal and Professional proposed subscales, all 10 personal items correlated more strongly with its proposed subscale and less with the other subscales, although the differences were small and may not be relevant (mean difference = 0.045, min/max: <0.01–0.12). For the professional subscale, 20/23 items correlated more with its proposed subscale (mean difference = 0.062, min/max: 0.03-0.11). Correlation between the personal and professional proposed subscales was 0.92.
Optimising scale length
Two items that had notably lower corrected item-total correlations than the other items, Item 15 (r = 0.57) and Item 32 (r = 0.47), also had potential issues with relevancy that were observed during the cognitive interviews in the instrument development phase [Citation25]. Twenty more items were identified for elimination by the first researcher. The second researcher disagreed with the retain/eliminate decisions for 10 items. After discussion, decisions for 9 items were changed. In the end, 19 items were eliminated because they had lower corrected item-total correlation (n = 11), lower variability in responses (n = 2), or based on research team opinion (n = 6). The final reduced version of the P-TREM has 30 items, with between 1-6 items per content area.
Exploratory factor analysis
The overall MSA was 0.94, with MSA for all items between 0.88 and 0.97, and Bartlett Sphericity Test was statistically significant ((χ2) = χ2 = 4937.4, p < 0.001) indicating our factor analysis could proceed. Both parallel analysis and the eigenvalue one test suggested there were 2 factors. We attempted to extract between 1 and 4 factors. The 3 and 4 factor solutions were not a good fit, as there were factors on which no items loaded significantly. The one factor solution fit fairly well (factor loadings 0.45–0.88), however the 2-factor solution with an oblique, ‘promax’ rotation produced the best solution with all items loading significantly (>0.41) on a single factor. Factor 1 loadings ranged from 0.50–1.0, Factor 2 loadings ranged from 0.46–0.88. contains the rotated factor loading matrix. Three items tended towards item complexity (loading to some extent on both factors), however, they still loaded significantly on only one factor, and were retained in order to maintain the content of the P-TREM.
Table 3. Rotated factor loading matrix.
Factor 1 was interpreted as ‘Physiotherapist’s Role’ (25 items), comprising the Ways of Connecting (driven by the physiotherapist), the physiotherapist’s contribution to the Conditions of Engagement, and the Bond Elements. Factor 2 was interpreted as ‘Patient’s Role’ (5 items) and consisted of items representing the patient’s contribution to the Conditions of Engagement. Correlation between factors was 0.71 and the model explained 0.61 of the variances in our data.
Unidimensionality check
The model fit indices for a one factor CFA model were CFI = 1.00, TLI = 1.04; RMSEA < 0.001, and SRMR 0.07, which were all within an acceptable range indicating a good fit.
Validation evidence
Descriptive statistics and ceiling effects for the P-TREM are found in . Ceiling effects were present in the total score (21.5%), as well as the Physiotherapist role (28.8%) and Patient role domain scores (47.9%).
Table 4. Descriptive statistics for scale scores.
The correlation between the total P-TREM score and the Physiotherapist role and Patient role domain scores was 0.99 and 0.81, respectively.
Measurement properties
Internal consistency of the P-TREM total and physiotherapist role domain were excellent and the patient role domain was good (see ). We found large correlations between the GRTR and the P-TREM total (r = 0.79, CI:0.72–0.84), Physiotherapist role domain (r = 0.78, CI:0.72–0.84), and Patient role domain (r = 0.58, CI:0.47–0.67), which supports the concurrent validity of the P-TREM. We found low to moderate correlations between the THCP and the P–TREM total (r = 0.26, CI:0.11–0.40), Physiotherapist role domain (r = 0.28, CI:0.10–0.39), and Patient role domain (r = 0.22, CI:0.07–0.36), which offers evidence of convergent validity. contains the validation evidence by population subgroup for the P-TREM total score.
Table 5. Concurrent and convergent validation for P-TREM total score by population subgroups.
Discussion
Evidence of validity
In this study, we investigated the quality of the items in the P-TREM, optimised the length of the P-TREM and demonstrated validity evidence for the use of the P-TREM in outpatient in-person settings, for established therapeutic relationships (3 or more encounters with the physiotherapist).
Construct validation
A hypothetical construct such as therapeutic relationship cannot be directly observed, therefore investigating construct validity involves generating hypotheses about the relationships between the scores on the measure being investigated and other variables based on current knowledge and theory [Citation30,Citation40]. The extent to which those hypotheses are supported provides an indication of construct validity for the measure [Citation30,Citation40]. We made two hypotheses about how scores of the P-TREM were related to a global rating of therapeutic relationship and to trust in healthcare providers in general. Our hypotheses were supported, which provides evidence of the construct validity of the P-TREM. The two-factor structure found in the factor analysis aligns with the theoretical framework informing the P-TREM (discussed in more detail in the section ‘Internal Structure’), which provides some additional evidence to support construct validity.
Content validity was established in the development of the P-TREM, with expert review by patients and physiotherapists, cognitive interviews and a content validation process [Citation25]. In this study, we ensured that the content of the P-TREM was maintained while optimising the length of the P-TREM. We also observed generally high inter-item and item-total correlations, as well as low rates of non-response to items, which also provides evidence to support content validity. The content of the P-TREM is unique from other measures in its focus on the patient and physiotherapist’s connections through the patient’s body, which includes talking about the patient’s physical sensations, as well as physical contact between them (i.e. touch). It also assessed the patient’s participation in the relationship.
The findings of this study supported viewing therapeutic relationship as a unidimensional construct. Although a two-factor model was observed in the EFA, the two factors were strongly correlated, and a single factor CFA model fit the data well. In addition, the overall high item-total correlations suggest a unidimensional structure. A measure should be shown to be unidimensional before it makes sense to assess and report co-efficient alpha, a basic measure of the reliability of a scale [Citation41]. A measure showing unidimensionality also supports the validity of using a simple sum total scoring process for a measure [Citation30]. We calculated coefficient α for P-TREM total, as well as the two domains and found all three to represent good evidence for internal consistency. In fact, the α values for the P-TREM were quite high, suggesting there is redundancy in the items and that further reduction in the number of items in the P-TREM could be possible in future studies [Citation30]. However, this is the first study of P-TREM measurement properties with a modest sample size. We did not want to eliminate too many items and risk the content validity of the P-TREM.
We conducted separate analyses for concurrent and convergent validity, as well as internal consistency (co-efficient α) for the three patient population subgroups in this study (i.e. inherited bleeding disorders, inflammatory arthritis, general musculoskeletal). In all population subgroups, α values for the total score were excellent. The P-TREM score was strongly associated with the participant’s global rating of therapeutic relationship, supporting concurrent validity. The hypothesis for convergent validity was partially supported, as associations between Trust in Healthcare Providers and the P-TREM total score were small to moderate, however not statistically significant for the musculoskeletal and inherited bleeding disorders subgroups. Additionally, patients from all three subgroups and clinicians working with these populations were involved in the development of the instrument, verifying the comprehensiveness and relevancy of the items to their experiences with their physiotherapists. Overall, there is enough evidence to support the use of the P-TREM in these three populations.
Internal structure
The EFA revealed two factors in the P-TREM: ‘Physiotherapist role’ with 23 items and ‘Patient’s role’ with 5 items. These two factors may be considered domains in the P-TREM. The items in the ‘Physiotherapist role’ domain refer to the patient’s perception of the physiotherapist’s actions during encounters (Connections), the physiotherapist’s ‘way of being’ (Conditions) in the relationship, and the Bond elements (i.e. trust, respect, caring, and rapport). The items in the ‘Patient role’ domain refer to the patient’s self-reported participation in the Conditions of Engagement (i.e. being present, being genuine, being committed, being receptive). Miciak described the conditions in the therapeutic relationship as being mutually generated by the patient and physiotherapist [Citation6]. There are no P-TREM items that directly assess the patient’s participation in Establishing Connections because the activities of a physiotherapy session are typically driven by the physiotherapist with the patient acting as a collaborative partner [Citation12].
There seems to be an imbalance between the patient role domain (5 items) and the physiotherapist role domain (25 items). This could be due in part to our current understanding of therapeutic relationship, where the physiotherapist is primarily responsible for establishing and maintaining the relationship. Therefore, it makes sense that the patient’s role contributes less to the total score. However, it is also possible that our understanding of the patient’s role in therapeutic relationship is underdeveloped, and that the content of the items in the Patient role do not capture all aspects of the patient’s role. New items may be needed to comprehensively assess this aspect of therapeutic relationship [Citation1]. A second potential reason relates to the low variance in the responses to the item. It may be that the items in the physiotherapist’s role domain actually constitutes more than one factor, which were not detected in the EFA due to the low variance in the data. For example, the items assessing the Elements of the Bond may be a separate factor from the Physiotherapist role in Connections and Conditions.
The physiotherapist and patient role dimensional structure we found for the P-TREM differs from that found in other measures of therapeutic relationship used in physiotherapy. This is most likely due to how therapeutic relationship is conceptualised in the measurement framework that informed the tool. The Person-Centered Therapeutic Relationship in Physiotherapy Scale (PCTR-PT) is a Spanish-language measure developed for use in all physiotherapy populations. It was found to have a four-dimensional structure: Relational Bond, Individualised Partnership, Therapeutic Communication and Professional Empowerment [Citation42,Citation43]. The PCTR-PT contains items asking about the emotional attachment between the patient and physiotherapist (i.e. there is mutual trust between us) and the way they work together (e.g. My physiotherapist and I agree on what I want to achieve from treatment). However, in contrast to the P-TREM, there are no items directly asking the patient about their individual participation in the therapeutic relationship, which may explain why a patient/physiotherapist dimensional structure is absent. The working alliance inventory (WAI) and its adaptations for rehabilitation, the most commonly used measure in physiotherapy research, is similar to the PCTR-PT in that it assesses emotional attachments and collaboration between the patient and therapist but does not ask the patient directly about their participation [Citation44]. The WAI has three domains: Goals, Tasks and Bond and it is common for the Goals and Tasks items to form one dimension, while the Bond items load as a separate dimension [Citation23,Citation24].
There are some examples of measures where mutuality, or both the patient and healthcare provider’s participation, are present in measures of similar constructs (e.g. patient-healthcare provider communication). One example of this is the Patient Involvement in Communication Scale and its modifications, which ask the patient about the healthcare provider’s behaviour and ‘manner’, as well as the patient’s active involvement in communication, such as offering opinions on their treatment and information about their condition [Citation45,Citation46]. The Roter Interaction Analysis System is used to analyse communication in healthcare encounters and codes both the patient and healthcare provider’s behaviours. Interestingly, the measurement of the concept of patient engagement, related to therapeutic relationship in that it can be defined as the process of gradual connection between the patient and physiotherapist, has the opposite issue [Citation47]. Patient engagement measures often focus on the patient’s actions and perceived attitudes to quantify the quality of engagement, despite the body of evidence that the healthcare provider’s attitudes and actions play an important role in patient engagement [Citation47].
Ceiling effects
Ceiling effects, or a skew towards the favourable end of a response scale, are a common problem, especially when a clinician is being rated [Citation30]. This may be due, in part, to biases inherent to patient responses, such as acquiescence and social desirability bias [Citation30,Citation48]. We implemented three strategies in constructing the P-TREM in an attempt to overcome the problem of ceiling effects. The first was to use a 6-point Likert type scale, which has more potential for variability in response than a scale with fewer points [Citation30]. The second was to ensure the content of the measure was comprehensive, as under-representation of a construct can results in ceiling effects [Citation49]. Related to this, we also included items that directly address negative experiences in rehabilitation (e.g. ‘I think my physiotherapist would acknowledge a mistake if they made one’), which could help capture a broader range of relationship experiences [Citation26]. Despite these strategies, the P-TREM showed ceiling effects in this study, in that 21.5% of participants scored the maximum score possible. This could be due to a bias in the sample, or a property of the P-TREM that will need to be addressed in further studies.
It is possible that there was a bias in the sample in this study due to the recruitment procedures. In the majority of recruitment sites (5 of the 8 clinics), physiotherapists approached their patients for participation using a non-consecutive approach. In these clinics, it seems likely that there could be an unconscious bias on the part of the physiotherapist to approach only those patients with whom they have a good relationship, and also possible that the patients who agreed to participate would be more willing to do so if they had a good relationship with their physiotherapist, since trust in the person asking a potential participant to complete a survey improves participation rates [Citation50]. The recruitment procedures, in addition to very high mean score on the global rating of therapeutic relationship (9.4/10) in our sample, supports the idea that our sample may have better therapeutic relationships than might be expected in our target population. This makes it difficult to parse out whether the ceiling effects observed are true ceiling effects or a product of sampling bias. Another consideration is that we focussed on measuring the therapeutic relationships of relatively long, established relationships (median duration of 2 years in this sample). Presumably, these patients have a good therapeutic relationship if they are returning to their physiotherapist over multiple years. We selected this timeframe given the clinical populations of interest, which typically have longstanding relationships with physiotherapists. However, this could be another explanation for the ceiling effects observed.
Ceiling effects are consistently reported in measures of physiotherapy therapeutic relationships. Therefore, it could also be possible that physiotherapists generally develop positive relationships with their patients. If this is true, a high-quality measure should still have the capacity to differentiate between good, better and excellent therapeutic relationships, therefore more work in the area of addressing ceiling effects is needed. Paap et. al. (2020) used a strategy of replacing a balanced Likert frequency type scale with a Visual Analog Scale with the lower anchor ‘Sometimes’ and the upper anchor ‘Always’ in the WAI-ReD [Citation51]. Their strategy was effective in reducing apparent ceiling effects, but whether that translates into a meaningful increase in the discriminating capacity of the scale still needs to be evaluated. Another strategy that could be implemented is to use an unbalanced Likert scale, with more options on the positive end. For example, in the P-TREM, this might look like a traditional 6-point Likert scale where the ‘average’ or neutral response is closer to the negative anchor descriptor [Citation30].
Strengths and limitations
A strength of this study was our rigorous approach to validity testing, following the recommendations of the Consensus-based Standards for the Selection of health status Measurements Instruments [Citation52]. The survey was anonymous, reducing the likelihood of response bias in participants, and participants were recruited from multiple clinical sites which enhanced the variability of the physiotherapists in the study.
The study sample represented the target population in most respects, however, as discussed above, it is conceivable that the recruitment strategy resulted in a bias in our sample towards participants with better therapeutic relationships than would have been expected with the target population. The skew towards more positive relationships reduced the variability in the responses to the items. This could have impacted this study in several ways. It may have resulted in over-estimation of the ceiling effects of the P-TREM, less variability among the inter-item correlations, making it challenging to distinguish higher quality items from those of lower quality. It also makes it difficult to ascertain whether the validity evidence presented here would apply to a population with poorer therapeutic relationships. Furthermore, as discussed above, significant factors in the internal structure may have been missed, and internal consistency may also have been over-estimated. It also impacted our ability to use item response theory modelling in the scale development because very few respondents chose the response options at the lower end of the scale.
Future directions
Future studies should replicate factor analysis in a larger sample, where participants are recruited by an independent, neutral member of the research team (i.e. not the physiotherapist), using a more rigorous (e.g. concurrent enrolment) approach to sampling. A study with a larger sample size could also optimise the length of the P-TREM using item response theory methods to reduce the number of items and improve its performance in terms of discriminative capacity and ceiling effects. Further validation testing would also be useful to investigate the predictive validity and responsiveness to change of the P-TREM. While we focussed on established therapeutic relationships as our target population, subsequent studies could examine the validity of the P-TREM for therapeutic relationships earlier in their development (e.g. after 2–3 encounters), or focus on a population with generally poorer therapeutic relationships, in which the P-TREM may perform differently.
More research characterising the distinct contributions of the patient and physiotherapist to the therapeutic relationship, perhaps linking with patient engagement research, would be useful to ensure all aspects of the patient’s role in therapeutic relationship are comprehensively assessed by the P-TREM. Understanding how the patient and physiotherapist contribute to the quality of a therapeutic relationship could inform efforts to improve therapeutic relationships in clinical practice.
Future measures should be developed that capture the quality of a therapeutic relationship from the perspective of the physiotherapist and also in more complex scenarios (e.g. individuals with cognitive impairment, pediatrics) where more than two people are involved in the therapeutic relationship. Modifications to the P-TREM for use in telerehabilitation or other clinical settings that do not involve direct patient contact should also be investigated [Citation20].
Final P-TREM specifications
The reduced P-TREM has a total of 30 items, scored 0–5, with the sum total score ranging from 0–150. All items have a 6-point ordinal response scale (Likert-type) ranging from strongly disagree to strongly agree. It is estimated to take 5–10 min to complete. It is intended for use in a population of patients with established therapeutic relationships during outpatient, in-person therapy. The P-TREM represents therapeutic relationship as a unidimensional construct. The magnitude of the total score from the P-TREM should be interpreted as the quality of a physiotherapy therapeutic relationship as a single entity, where a higher score indicates a relationship of higher quality. The final P-TREM scale is available as Supplementary File 4. A full list of the items with their content based on Miciak’s framework is available from the corresponding author.
It should be noted that interpretations should only be made based on the total score from the P-TREM. There is insufficient evidence to interpret scores from each domain. For example, a low score on the Patient role items should not be interpreted as the patient not participating fully in the therapeutic relationship.
Conclusion
To our knowledge, the P-TREM is the first English-language patient-reported measure of therapeutic relationship based on a physiotherapy-specific theoretical framework. This study demonstrated validity evidence and supports the use of the P-TREM as a unidimensional measure in research for the purpose of quantifying the quality of therapeutic relationships in outpatient, in-person physiotherapy. Using the P-TREM could help physiotherapy researchers develop an understanding of the mechanisms of therapeutic relationship and how it impacts treatment outcomes. Further research is needed to evaluate the P-TREM administered earlier in the development of the relationship or within clinical settings that do not involve direct contact with patients (i.e. telerehabilitation).
Author contributions
All authors made a substantial contribution to the design of the work, revised the article critically for important intellectual content and approved the version to be published.
Supplementary_File_4_Final.docx
Download MS Word (29.9 KB)Supplementary_File_3_Final.docx
Download MS Word (23.6 KB)Supplementary_File_2_Final.docx
Download MS Word (21.2 KB)Supplementary_File_1_Final.docx
Download MS Word (33.6 KB)Acknowledgements
The authors would like to thank the participating clinics and patient advocacy organizations for their support and contribution to this study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Miciak M. Bedside Matters: A Conceptual Framework of the Therapeutic Relationship in Physiotherapy. Doctor of Philosophy, University of Alberta; 2015. Available from: https://era.library.ualberta.ca/files/9z903246q#.WEWHhmQrIfE.
- Rossettini G, Carlino E, Testa M. Clinical relevance of contextual factors as triggers of placebo and nocebo effects in musculoskeletal pain. BMC Musculoskelet Disord. 2018;19(1):27.
- Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychother Theory,Res Pract. 1979;16(3):252–260.
- Babatunde F, MacDermid J, MacIntyre N. Characteristics of therapeutic alliance in musculoskeletal physiotherapy and occupational therapy practice: a scoping review of the literature. BMC Health Serv Res. 2017;17(1):375.
- Besley J, Kayes NM, McPherson KM. Assessing therapeutic relationships in physiotherapy: literature review. New Zealand JPhysiother. 2011;39:81–91.
- Miciak M, Mayan M, Brown C, et al. The necessary conditions of engagement for the therapeutic relationship in physiotherapy: an interpretive description study. Arch Physiother. 2018;8:3.
- Morera-Balaguer J, Botella-Rico JM, Martínez-González MC, et al. Physical therapists’ perceptions and experiences about barriers and facilitators of therapeutic patient-centred relationships during outpatient rehabilitation: a qualitative study. Braz J Phys Ther. 2018;22(6):484–492.
- Morera-Balaguer J, Botella-Rico JM, Catalán-Matamoros D, et al. Patients’ experience regarding therapeutic person-centered relationships in physiotherapy services: a qualitative study. Physiother Theory Pract. 2021;37(1):17–27.
- O'Keeffe M, Cullinane P, Hurley J, et al. What influences patient-therapist interactions in musculoskeletal physical therapy? Qualitative systematic review and meta-synthesis. Phys Ther. 2016;96(5):609–622.
- Søndenå P, Dalusio-King G, Hebron C. Conceptualisation of the therapeutic alliance in physiotherapy: is it adequate? Musculoskelet Sci Pract. 2020;46:102131.
- McCabe E, Miciak M, Dennett L, et al. Measuring therapeutic relationship in the care of patients with haemophilia: a scoping review. Health Expect. 2018;21(6):1208–1230.
- Miciak M, Mayan M, Brown C, et al. A framework for establishing connections in physiotherapy practice. Physiother Theory Pract. 2019;35(1):40–56.
- Alodaibi F, Beneciuk J, Holmes R, et al. The relationship of the therapeutic alliance to patient characteristics and functional outcome during an episode of physical therapy care for patients with low back pain: an observational study. Phys Ther. 2021;101(4).
- Ferreira PH, Ferreira ML, Maher CG, et al. The therapeutic alliance between clinicians and patients predicts outcome in chronic low back pain. Phys Ther. 2013;93(4):470–478.
- Fuentes J, Armijo-Olivo S, Funabashi M, et al. Enhanced therapeutic alliance modulates pain intensity and muscle pain sensitivity in patients with chronic low back pain: an experimental controlled study. Phys Ther. 2014;94(4):477–489.
- Hall AM, Ferreira PH, Maher CG, et al. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: a systematic review. Phys Ther. 2010;90(8):1099–1110.
- Kayes NM, McPherson KM. Human technologies in rehabilitation: ‘who’ and ‘how’ we are with our clients. Disabil Rehabil. 2012;34(22):1907–1911.
- Kinney M, Seider J, Beaty AF, et al. The impact of therapeutic alliance in physical therapy for chronic musculoskeletal pain: a systematic review of the literature. Physiother Theory Pract. 2020;36(8):886–898.
- Taccolini Manzoni AC, Bastos de Oliveira NT, Nunes Cabral CM, et al. The role of the therapeutic alliance on pain relief in musculoskeletal rehabilitation: a systematic review. Physiother Theory Pract. 2018;34(12):901–915.
- Lawford BJ, Bennell KL, Campbell PK, et al. Association between therapeutic alliance and outcomes following telephone-delivered exercise by a physical therapist for people with knee osteoarthritis: secondary analyses from a randomized controlled trial. JMIR Rehabil Assist Technol. 2021;8(1):e23386.
- Araujo AC, Filho RN, Oliveira CB, et al. Measurement properties of the Brazilian version of the working alliance inventory (patient and therapist short-forms) and session rating scale for low back pain. BMR. 2017;30(4):879–887.
- Besley J, Kayes NM, McPherson KM. Assessing the measurement properties of two commonly used measures of therapeutic relationship in physiotherapy. New Zealand J Physiother. 2011;39:75–80.
- Hall AM, Ferreira ML, Clemson L, et al. Assessment of the therapeutic alliance in physical rehabilitation: a RASCH analysis. Disabil Rehabil. 2012;34(3):257–266.
- Paap D, Schrier E, Dijkstra PU. Development and validation of the working alliance inventory dutch version for use in rehabilitation setting. Physiother Theory Pract. 2019;35(12):1292–1303.
- McCabe E, Miciak M, Roduta Roberts M, et al. Development of the physiotherapy therapeutic relationship measure. Eur J Physiother. 2021;1–10.
- McCabe E, Miciak M, Mary RR, et al. Measuring therapeutic relationship in physiotherapy: conceptual foundations. Physiother Theory Pract. 1–13. DOI:10.1080/09593985.2021.1987604
- DeVellis RF. Scale development: theory and applications. 4th ed. Los Angeles: SAGE Publications Inc; 2017.
- Norman GR, Streiner DL. Biostatistics: the bare essentials with SPSS. 4th ed. Shelton, Connecticut: People’s Medical Publishing House-USA; 2014.
- Cohen DS, Colliver JA, Marcy MF, et al. Psychometric proporties of a standardized-patient checklist and rating-scale form used to access interpersonal and communication skills. Acad Med. 1996;71:S87–S89.
- Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use. 5th ed. New York, NY, US: Oxford University Press; 2015.
- Dugan E, Trachtenberg F, Hall MA. Development of abbreviated measures to assess patient trust in a physician, a health insurer, and the medical profession. BMC Health Serv Res. 2005;5:64.
- The Jamovi project. Jamovi [Computer Software]. Version 1.6. Sydney, Australia; 2021. Available from: https://www.jamovi.org.
- R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2020. Available from: https://www.R-project.org/
- Revelle W. Psych: procedures for personality and psychological research. R, Evanston, Illinois, USA: Northwestern University; 2020. Available from: https://CRAN.R-project.org/package=psych
- Rosseel Y. Lavaan: an R package for structural equation modeling. J Stat Soft. 2012;48(2):1–36.
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55.
- Ponterotto JG, Ruckdeschel DE. An overview of coefficient alpha and a reliability matrix for estimating adequacy of internal consistency coefficients with psychological research measures. Percept Mot Skills. 2007;105(3 Pt 1):997–1014.
- Cohen J. A power primer. Psychol Bull. 1992;112(1):155–159.
- Hall MA, Camacho F, Dugan E, et al. Trust in the medical profession: conceptual and measurement issues. Health Serv Res. 2002;37(5):1419–1439.
- Terwee CB, Bot SDM, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42.
- Prinsen C, Mokkink L, Bouter L, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1147–1129.
- Rodriguez Nogueira O, Botella-Rico J, Martinez Gonzalez MC, et al. Construction and content validation of a measurement tool to evaluate person-centered therapeutic relationships in physiotherapy services. PLOS One. 2020;15(3):e0228916.
- Rodriguez-Nogueira Ó, Morera Balaguer J, Nogueira López A, et al. The psychometric properties of the person-centered therapeutic relationship in physiotherapy scale. PLOS One. 2020;15(11):e0241010.
- Horvath AO, Greenberg LS. Development and validation of the working alliance inventory. JCouns Psychol. 1989;36(2):223–233.
- Jonsdottir T, Jonsdottir H, Gunnarsdottir S. Validation of the patients’ perceived involvement in care scale among patients with chronic pain. Scand J Caring Sci. 2013;27(3):740–749.
- Smith MY, Winkel G, Egert J, et al. Patient-physician communication in the context of persistent pain: validation of a modified version of the patients’ perceived involvement in care scale. J Pain Symptom Manage. 2006;32(1):71–81.
- Bright F. A S, Kayes NM, Worrall L, et al. A conceptual review of engagement in healthcare and rehabilitation. Disabil Rehabil. 2015;37(8):643–654.
- Couch A, Keniston K. Yeasayers and naysayers: agreeing response set as a personality variable. J Abnorm Soc Psychol. 1960;60:151–174.
- Mokkink LB, Terwee CB, Knol DL, et al. The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: a clarification of its content. BMC Med Res Methodol. 2010;10:22.
- Gideon L. Handbook of survey methodology for the social sciences. New York, NY: Springer New York; 2012.
- Paap D, Schepers M, Dijkstra PU. Reducing ceiling effects in the working alliance inventory-rehabilitation Dutch version. Disabil Rehabil. 2020;42(20):2944–2950.
- Mokkink LB, Prinsen CA, Patrick DL, et al. COSMIN study design checklist for patient-reported outcome measurement instruments; 2019. Available from: https://www.cosmin.nl/wp-content/uploads/COSMIN-study-designing-checklist_final.pdf#.