Abstract
This study evaluated changes in energy expenditure in six to eight-year-old children after a two year pedagogical intervention on healthy habits. Methods: This was a longitudinal descriptive observational study in children at a private school in Bogotá. Outcomes: change in the average energy expenditure(Kcal/day) and time dedicated to physical activity. The children’s physical activity(PA) was objectively assessed for six days using a multi-sensor device(Actiheart®). Results: A total of ten girls (52.63%) and nine boys (47.37%) were included. At the end of the follow-up, the energy expenditure had increased by 457.30 Kcal/day (p < 0.001), activities requiring <1.5 MET had decreased by 237.40 minutes (p < 0.001), and physical activity between 3–6 MET had increased by 88.90 minutes(p = 0.001). Conclusions: Children decreased their sedentary lifestyle and increased energy expenditure and physical activity, suggesting a possible change in them as a consequence of the intervention.
PUBLIC INTEREST STATEMENT
A sedentary lifestyle is one of the risk behaviors for developing cardiovascular disease in adult life. Worldwide, it has been documented that up to 80% of children do not meet the international recommendations given by the World Health Organization. This study describes changes in physical activity in six to eight-year-old children after a two-year pedagogical intervention on healthy habits. At baseline, 10.0 % of the girls complied with the recommended 60 minutes/day of moderate to vigorous physical activity, in contrast to 66.6% of the boys. At the end of the follow-up period, 100% of both girls and boys complied with this recommendation and decreased the time spent at rest activity. The results suggest a possible change in physical activity as a consequence of the pedagogical intervention.
1. Introduction
A sedentary lifestyle is one of the risk behaviors for developing cardiovascular disease in adult life (Deshmukh-Taskar et al., Citation2006; Freedman, Khan, Dietz, Srinivasan, & Berenson, Citation2001; Briceño, Citation2015). Worldwide, it has been documented that up to 80% of adolescents do not meet the international recommendations given by the World Health Organization (WHO) of 60 minutes/day of moderate to vigorous physical activity for at least five days a week (Andersen et al., Citation2006; Calahorro, Citation2014; Calahorro, Torres-Luque, & Ivan, Citation2015; Demant Klinker, Schipperijn, Toftager, Kerr, & Troelsen, Citation2015; Janssen & Leblanc, Citation2010; Mathus-Vliegen et al., Citation2012; Ruiz et al., Citation2011). Boys are generally more active than girls, while the decrease in physical activity reported during school age is higher in boys than girls (Andersen et al., Citation2006; Blaes, Baquet, Van Praagh, & Berthoin, Citation2011; Foster, Moore, Singletary, & Skelton, Citation2018; Swinburn & Vandevijvere, Citation2016). In the pediatric age bracket, there is a higher level of physical activity on weekdays (Blaes et al., Citation2011).
In Colombia, 57.4% of the global population, as well as 22.6% of 13–14 year old, and 28.4% of 15–17 year old, do not meet the minimum standards of physical activity (Instituto, & Familiar, C. D. B, Citation2005), and levels of sedentarism of up to 78.8% are reported in the 3–17 year old population (Briceño, Citation2015). Furthermore, in children 5–12 years old, overweight and obesity increased from 18.8% in 2010 to 24.4% in 2015 (ICBF, I. C. D. B. F, Citation2015).
There are effective strategies aimed at promoting cardiovascular health, which include school and community activities and primary health care, among others. At the school level, multicomponent interventions in physical activity and nutrition that involve the educational community have proven to be successful in the prevention of obesity (Briceño, Citation2018).
The objective of this study was to describe the changes in active energy expenditure (AEE) of six to eight-year-old children at a school in an urban area, following a 2 year plus structured pedagogical intervention on healthy habits.
2. Methods
This study is part of the CARDIECOL-Colciencias research network cardiovascular health research line. From May 2014 to August 2016, a longitudinal descriptive observational study was conducted, with a non-probabilistic sampling of consecutive cases, of children at a private school located in the urban area of Bogotá, with an appropriate physical activity space and infrastructure. Additionally, in order to be selected, the school could not have received any physical activity intervention in the year prior to the start of the study or be planning to receive any such intervention during the follow-up period. The study was approved by the institutional review board (IRB00007736), obtaining informed consent from parents and informed assent from children, with quality control follow-up by the study coordinator and the researchers.
The study was designed to detect differences of up to 70 Kcal/day in activity energy expenditure due to physical activity, with a power of 80% and a 95% level of confidence.
2.1. Study measurements
The primary outcome was the average change in AEE (Kcal/day). Secondary outcomes were changes in minutes per day spent at different intensities of activity, measured in Metabolic Equivalent of Task units (METs), with one unit being defined as the amount of oxygen uptake at rest, and equal to 3.5 mL∙Kg−1 min−1. The intensity of physical activity is classified according to METs in the following categories: rest activity, such as sitting watching television, or sleeping (<1.5 METs); light activity, such as board games, reading a book, daily activities, or walking 1.7–2.5 Km/h (1.5–3 METs); moderate activity, such as walking 3.0–3.4 km/h or riding a bicycle <10 Km/h (3–6 METs); or vigorous activity, such as running, jumping or jogging (>6 METs) (Norton, Norton, & Sadgrove, Citation2010).
Physical activity was measured by accelerometers (Actiheart), that are technically reliable and valid instruments for the use of AEE determination. A validation study reported a strong linear relationship between movement and acceleration (R2= 0.99, P < 0.001). The 95% limits of agreement between Actiheart and electrocardiogram were −4.2–4.3 beats per minute. Correlations with intensity were generally high (R2 > 0.84, P < 0.001) (Brage, Brage, Franks, Ekelund, & Wareham, Citation2005; Takken et al., Citation2010) The Actiheart is a compact, chest-worn monitoring device that records heart rate, Inter-Beat-Interval, and physical activity in one combined, light-weight waterproof unit. It is designed for calculating and measuring Energy Expenditure in free living. The Actiheart has two clips which attach directly to standard ECG electrodes. Usually one electrode is adhered at V1 or V2 (4th intercostal) and the second electrode is placed approximately 10 cm away on the left side at V4 or V5, although this placement can be adjusted to be comfortable for the subject. The number of R-waves detected is recorded in 15, 30, or 60 second epochs. Simultaneously, an internal accelerometer senses the frequency and intensity of the subject’s torso movements.
Assessment recordings had to be available for 24 hours, including two weekend days and two school days(Addy, Trilk, Dowda, Byun, & Pate, Citation2014). Heart rate in beats per minute and one-dimensional bodily acceleration in counts per minute were recorded using 15 s epochs. AEE was calculated using the branched model approach, with Actiheart®‘s captive software (Corder, Brage, Wareham, & Ekelund, Citation2005).
2.2. Intervention
The pedagogical intervention lasted two years and was based on health promotion models and social cognitive theory, taking into account the uptake of parent and teacher caregiver role models. These were articulated with the Institutional Educational Project through the pedagogical component, integrating three areas: physical activity, healthy eating, and knowledge of the body and heart, with the dynamics of the educative community.
The intervention was directed towards children, their parents and teachers. For children, it included the evaluation of cardiovascular risk factors at the beginning and end of follow-up, school activities (a minimum of two/week, with a high-impact physical activity led by two physical activity research team members during the morning break once a semester), and the use of educational materials for developing the pedagogical activities (posters and an educative guide). For parents, it included three workshops/year (two hours each) on the intervention areas, healthy notes sent home once a month, and the celebration of healthy family day (one/year). For teachers, it included three workshops/year (two hours each) on the intervention areas, planning and conducting pedagogical activities with the students (a minimum of two activities/week) and follow-up visits to the school by the research team (one/month).
2.3. Statistical analysis
The variables obtained by the multi-sensor device were the AEE in Kcal/day, and mean daily minutes of rest, light, moderate, and vigorous activity. The assumption of normality was verified using the Shapiro-Wilk test. Physical activity data are presented as means and standard deviations, and the differences between groups are shown with the mean and 95% confidence intervals. A paired t-test or the nonparametric Wilcoxon signed ranks test were used, as appropriate, to compare physical activity between first and second measurement in days of the week. Nonparametric Mann–Whitney U test was used to compare physical activity between boys and girls.
Analyses were conducted using the STATA 13.1 statistical software. For all statistical tests, significance was set at p < 0.05.
3. Results
A total of 10 girls (52.63%) and 9 boys (47.37%) were included. At baseline, the child mean (SD) age and BMI were 6.98 (0.76) years and 16.05(1.61) kg/m2, and in the second measurement were 9.44(0.6) years and 16.94(2.27) kg/m2, with no statistically difference in BMI, p = 0.173.
3.1. Days of the week
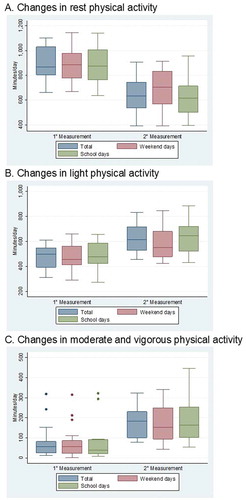
At the end of the follow-up period, the study population had improved AEE, decreased rest activity, and increased physical activity in general, especially on school days (Table , Figure ). After the follow-up period, children spent significantly more time in rest activities on weekend days, p = 0.033 (Figure ).
Table 1. Change in energy expenditure and physical activity by days of the week
There were other changes, but none statistically significant. At baseline, children spent more time in moderate and vigorous physical activities on weekend days, but these activities were higher on school days after the intervention.
3.2. Gender
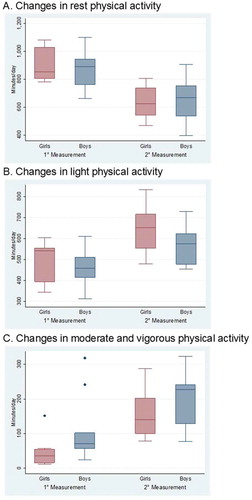
In general, in first and second measurements, AEE and moderate physical activity, was higher in boys than in girls, but only vigorous physical activity after the intervention was statistically significant, p = 0.021 (Table , Figure ).
Table 2. Change in energy expenditure and physical activity by gender
At baseline, 10.0 % of the girls complied with the recommended 60 minutes/day of moderate to vigorous physical activity, in contrast to 66.6% of the boys, p = 0.010. In the second measurement, 100% of both girls and boys complied with this recommendation.
There were other no statistically significant changes greater in girls after the follow-up period. The increase in time spent in light physical activity was greater in girls (155.80 minutes) than in boys (116.13 minutes), with a difference of 39.67 minutes. The increase in time spent in moderate physical activity was 104.18 minutes for girls and 71.94 minutes for boys, with a difference of 32.24 minutes.
The decrease in time spent at rest activity after the intervention was greater in girls (265.98 minutes) than in boys (205.67 minutes), with a difference of 60.31 minutes.
4. Discussion
At the end of the follow-up period, the study population had improved energy expenditure, decreased rest activity and increased light, moderate and vigorous activities, especially on school days, with a greater increase of time spent in light physical activities and energy expenditure for girls.
Child BMI was not significantly different after the intervention. This could be explained by three reasons. First, the growth is a dynamic process in children and usually there is an increase of 1 unit in BMI (kg/m2) between seven and nine years old; second, it’s possible losing fat but gaining muscle at the same time with no change in BMI; third, the small sample size has no power to detect this change in BMI.
4.1. Days of the week
At the end of follow-up, the increase in physical activity on school days and weekend days was clinically and statistically significant.
The study population spent more time in rest activities on weekend days, and more time in light, moderate and vigorous physical activities on school days. Additionally, they had a greater energy expenditure on school days. These findings are similar to those reported in other studies (Blaes et al., Citation2011; Gavarry, Giacomoni, Bernard, Seymat, & Falgairette, Citation2003), and could be explained by sociocultural factors, and the effect of the school intervention.
4.2. Gender
The time per day spent at different intensities of physical activity was higher in boys than in girls, except for light activity, which was higher in girls. The literature is controversial on this topic. Some studies show similar findings to our study, but others report that boys spend more time in light, moderate and vigorous physical activity than girls (Bielemann, Cascaes, Reichert, Domingues, & Gigante, Citation2013; Colley et al., Citation2011; Riddoch et al., Citation2004). Our results could be explained could be explained by the age of the children and the girls´ practice of non-competitive physical activity.
Both boys and girls improved energy expenditure and physical activity in the second measurement, including the proportion of children who met the recommended goal of 60 minutes of moderate to vigorous physical activity. However, the change was greater in girls, suggesting a possible additional positive effect in them due to sociocultural factors or the influence of the role models involved in this intervention itself (Table ). A less likely cause is age, since the literature describes a decrease in physical activity at older ages (Sallis, Prochaska, & Taylor, Citation2000). Another explanation could be that girls were less active than boys at baseline, and therefore had a larger potential for change (Grydeland et al., Citation2013; Kettner et al., Citation2013).
The increase in energy expenditure after the intervention was greater in girls (474.08 Kcal/day) than in boys (438.67 Kcal/day), with a difference of 35.41 kcal/day, p = 0.879. Additionally, changes in the time spent in light and moderate physical activity for girls were greater than for boys (Table 3). These findings differ from those in other studies where boys performed more physical activity than girls (Goran, Gower, Nagy, & Johnson, Citation1998). Our results suggest an intervention effect, just as other multicomponent interventions involving the school community have shown effects on physical activity (WHO Guidelines Approved by the Guidelines Review Committee, Citation2009). Additionally, the intervention involved parents and teachers, which could increase the perception of the benefits and the practice of physical activity in children; as well as music and dance which engaged and motivated girls´ participation (Briceño, Citation2018; Loprinzi & Trost, Citation2010).
The study has some limitations. It is a descriptive study, which limits the scope of the conclusions. A randomized, controlled study is needed to evaluate the effectiveness of the intervention. The sample size was calculated to evaluate changes in AEE in children, but not in the intensity of physical activity, nor changes according to gender.
Although recent studies show no effects on physical activity evaluated with accelerometers in children (Lawlor, El Anderson, Ld Howe, & Moure-Fernandez et al., Citation2016; Wyatt, Creanor, Green, & Hillsdon et al., Citation2018), based on the information obtained in this study, which was targeted to six to eight year old children, and included more class activities and intensive family and community interventions, the authors designed and are currently planning a cluster randomized controlled trial. This trial will take into account other variables that may explain the effect on AEE and the time spent in different intensities of physical activity, such as age, sex, nutritional status, school policies, and changes in the physical activity habits of children´s parents and teachers.
5. Conclusions
At the end of follow-up, the study population had improved AEE, decreased rest activity and increased light, moderate and vigorous physical activities, especially on school days.
Both boys and girls improved AEE and physical activity, with the change being greater in girls, which suggests a possible change in them as a consequence of the intervention.
Acknowledgements
The authors thank everyone who helped and supported the development of the study. The authors are indebted to the families and children for their invaluable participation in the study.
Additional information
Funding
Notes on contributors
Germán Briceño
Germán Briceño, pediatrician and clinical epidemiologist, works in the Research department of the Fundación CardioInfantil in Colombia, in a line of research of cardiovascular health promotion beginning in children, instilling proper lifestyle behaviors at an early age, which, in turn, can be brought into adulthood. This line of research has reported that an educational intervention in healthy habits among preschoolers was feasible and effective to change knowledge, attitudes and habits related to a healthy diet and active lifestyle. This paper support pedagogical interventions in children to improve the physical activity as part of the components of the cardiovascular health.
References
- Addy, C. L., Trilk, J. L., Dowda, M., Byun, W., & Pate, R. R. (2014). Assessing preschool children’s physical activity: How many days of accelerometry measurement. Pediatric Exercise Science, 26(1), 103–10. doi:10.1123/pes.2013-0021
- Andersen, L. B., Harro, M., Sardinha, L. B., Froberg, K., Ekelund, U., Brage, S., & Anderssen, S. A. (2006). Physical activity and clustered cardiovascular risk in children: A cross-sectional study (The European youth heart study). Lancet, 368(9532), 299–304. doi:10.1016/s0140-6736(06)69075-2
- Bielemann, R. M., Cascaes, A. M., Reichert, F. F., Domingues, M. R., & Gigante, D. P. (2013). Objectively measured physical activity in children from a southern Brazilian city: A population-based study. Journal of Physical Activity & Health, 10(8), 1145–1152.
- Blaes, A., Baquet, G., Van Praagh, E., & Berthoin, S. (2011). Physical activity patterns in French youth–From childhood to adolescence–Monitored with high-frequency accelerometry. American Journal of Human Biology: The Official Journal of the Human Biology Council, 23(3), 353–358. doi:10.1002/ajhb.21142
- Brage, S., Brage, N., Franks, P. W., Ekelund, U., & Wareham, N. J. (2005). Reliability and validity of the combined heart rate and movement sensor Actiheart. European Journal of Clinical Nutrition, 59(4), 561–570. doi:10.1038/sj.ejcn.1602118
- Briceño, G. (2015). Prevalencia elevada de factores de riesgo cardiovascular en la población pediatra. Biomédica, 35, 219–226. doi:10.1590/S0120-41572015000200010
- Briceño, G. (2018). La actividad fisica y el deporte como medida de salud pública. In P. Rosselli (Ed.), La actividad física, el ejercicio y el deporte en niños y adolescentes: Recomendaciones en la salud y en la enfermedad (Vol. 1, pp. 160–175). Bogotá: Editorial médica Panamericana.
- Calahorro, F. (2014). Physical activity levels and accelerometry: Recommendations and patterns in school-aged subjects. Servicio de Publicaciones de la Universidad de Murcia Cuadernos de Psicología del Deporte, 14, 3, 129-140.
- Calahorro, F., Torres-Luque, G., & Ivan, L.-F. (2015). Actividad física y acelerometría; orientaciones meteorológicas, recomendaciones y patrones. Nutrición Hospitalaria, 31(1): 115–128.
- Colley, R. C., Garriguet, D., Janssen, I., Craig, C. L., Clarke, J., & Tremblay, M. S. (2011). Physical activity of Canadian children and youth: Accelerometer results from the 2007–2009 Canadian health measures survey. Health Reports, 22(1), 15–23.
- Corder, K., Brage, S., Wareham, N. J., & Ekelund, U. (2005). Comparison of PAEE from combined and separate heart rate and movement models in children. Medicine and Science in Sports and Exercise, 37(10), 1761–1767.
- Demant Klinker, C., Schipperijn, J., Toftager, M., Kerr, J., & Troelsen, J. (2015). When cities move children: Development of a new methodology to assess context-specific physical activity behaviour among children and adolescents using accelerometers and GPS. Health & Place, 31, 90–99. doi:10.1016/j.healthplace.2014.11.006
- Deshmukh-Taskar, P., Nicklas, T. A., Morales, M., Yang, S. J., Zakeri, I., & Berenson, G. S. (2006). Tracking of overweight status from childhood to young adulthood: The Bogalusa heart study. European Journal of Clinical Nutrition, 60(1), 48–57. doi:10.1038/sj.ejcn.1602266
- Foster, C., Moore, J. B., Singletary, C. R., & Skelton, J. A. (2018). Physical activity and family-based obesity treatment: A review of expert recommendations on physical activity in youth. Clinical Obesity, 8(1), 68–79. doi:10.1111/cob.12230
- Freedman, D. S., Khan, L. K., Dietz, W. H., Srinivasan, S. R., & Berenson, G. S. (2001). Relationship of childhood obesity to coronary heart disease risk factors in adulthood: The Bogalusa heart study. Pediatrics, 108(3), 712–718.
- Gavarry, O., Giacomoni, M., Bernard, T., Seymat, M., & Falgairette, G. (2003). Habitual physical activity in children and adolescents during school and free days. Medicine and Science in Sports and Exercise, 35(3), 525–531. doi:10.1249/01.mss.0000053655.45022.c5
- Goran, M. I., Gower, B. A., Nagy, T. R., & Johnson, R. K. (1998). Developmental changes in energy expenditure and physical activity in children: Evidence for a decline in physical activity in girls before puberty. Pediatrics, 101(5), 887–891.
- Grydeland, M., Bergh, I. H., Bjelland, M., Lien, N., Andersen, L. F., Ommundsen, Y., … Anderssen, S. A. (2013). Intervention effects on physical activity: The HEIA study - a cluster randomized controlled trial. The International Journal of Behavioral Nutrition and Physical Activity, 10, 17. doi:10.1186/1479-5868-10-17
- Instituto Colombiano de Bienestar Familiar (ICBF). (2005). ENSIN - Encuesta Nacional de Situación Nutricional en Colombia. Retrieved from https://www.icbf.gov.co/icbf/directorio/portel/libreria/php/03.03081103.html. Consultado en 3/12/02018.
- Instituto Colombiano de Bienestar Familiar (ICBF). (2015). ENSIN - Encuesta Nacional de Situación Nutricional en Colombia. Retrieved from https://www.icbf.gov.co/icbf/directorio/portel/libreria/php/03.03081103.html. Consultado en 3/12/02018.
- Janssen, I., & Leblanc, A. G. (2010). Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. The International Journal of Behavioral Nutrition and Physical Activity, 7, 40. doi:10.1186/1479-5868-7-40
- Kettner, S., Kobel, S., Fischbach, N., Drenowatz, C., Dreyhaupt, J., Wirt, T., … Steinacker, J. M. (2013). Objectively determined physical activity levels of primary school children in south-west Germany. BMC Public Health, 13, 895. doi:10.1186/1471-2458-13-895
- Lawlor, D. A., El Anderson, K. R., Ld Howe, C. C., Moure-Fernandez, A. (2016). Active for life year 5: A cluster randomised controlled trial of a primary school-based intervention to increase levels of physical activity, decrease sedentary behaviour and improve diet. Public Health Res, 4(7).
- Loprinzi, P. D., & Trost, S. G. (2010). Parental influences on physical activity behavior in preschool children. Preventive Medicine, 50(3), 129–133. doi:10.1016/j.ypmed.2009.11.010
- Mathus-Vliegen, L., Toouli, J., Fried, M., Khan, A. G., Garisch, J., Hunt, R., … Riccardi, G. (2012). World gastroenterology organisation global guidelines on obesity. Journal of Clinical Gastroenterology, 46(7), 555–561. doi:10.1097/MCG.0b013e318259bd04
- Norton, K., Norton, L., & Sadgrove, D. (2010). Position statement on physical activity and exercise intensity terminology. Journal of Science and Medicine in Sport, 13(5), 496–502. doi:10.1016/j.jsams.2009.09.008
- Riddoch, C. J., Bo Andersen, L., Wedderkopp, N., Harro, M., Klasson-Heggebo, L., Sardinha, L. B., … Ekelund, U. (2004). Physical activity levels and patterns of 9- and 15-yr-old European children. Medicine and Science in Sports and Exercise, 36(1), 86–92. doi:10.1249/01.mss.0000106174.43932.92
- Ruiz, J. R., Ortega, F. B., Martinez-Gomez, D., Labayen, I., Moreno, L. A., De Bourdeaudhuij, I., … Sjostrom, M. (2011). Objectively measured physical activity and sedentary time in European adolescents: The HELENA study. American Journal of Epidemiology, 174(2), 173–184. doi:10.1093/aje/kwr068
- Sallis, J. F., Prochaska, J. J., & Taylor, W. C. (2000). A review of correlates of physical activity of children and adolescents. Medicine and Science in Sports and Exercise, 32(5), 963–975.
- Swinburn, B., & Vandevijvere, S. (2016). WHO report on ending childhood obesity echoes earlier recommendations. Public Health Nutrition, 19(1), 1–2. doi:10.1017/s1368980015003663
- Takken, T., Stephens, S., Balemans, A., Tremblay, M. S., Esliger, D. W., Schneiderman, J., … Feldman, B. M. (2010). Validation of the Actiheart activity monitor for measurement of activity energy expenditure in children and adolescents with chronic disease. European Journal of Clinical Nutrition, 64(12), 1494–1500. doi:10.1038/ejcn.2010.196
- WHO Guidelines Approved by the Guidelines Review Committee. (2009). In Interventions on diet and physical activity: What works: Summary report. Geneva: World Health Organization Copyright (c) World Health Organization 2009.
- Wyatt, K. L. J., Creanor, S., Green, C. D. S., Hillsdon, M.,… Public Health Research. (2018). Cluster randomised controlled trial and economic and process evaluation to determine the effectiveness and cost-effectiveness of a novel intervention [Healthy Lifestyles Programme (HeLP)] to prevent obesity in school children. Public Health Res, 6(1).