Abstract
Sickle Cell Disease (SCD) has many psychosocial impacts and affects social participation of young people. In Guadeloupe (French West Indies), where this blood disease is a major concern, young patients face a doubly constraining environment, on both social and physical aspects. Based on the Disability Creation Process (DCP), an ecological model of disability and health, this controlled study aimed to assess the perceived influence of social and physical factors. The study involves 80 young patients (Mage = 11.25 ± 3.23, 36 females, 44 males) with severe Sickle Cell Disease (Major Syndrome or Sβ0-thalassemia) and 45 healthy children and adolescents (Mage = 10.55 ± 2.93 years; 22 females, 23 males). The Measure of the Quality of the Environment (MQE) was used, after adaptation of the scale to the socio-cultural context. Results show that environmental factors are more negatively perceived among SCD participants, physical factors constituting strong barriers, and social determinants being weaker facilitators. In the micro and meso-environment, SCD patients face more difficulty; finally, findings suggest that more inclusive spaces are needed in school settings, sports and leisure activities, as well as in the cultural offer.
1. Introduction: conceptualization of terms
1.1. An ecologic-systemic explanatory model of diseases: the Disability Creation Process (DCP)
Understanding chronic diseases and disability situations, their production mechanisms and their consequences from a social and inclusive perspective remains a crucial challenge. Successive theoretical approaches have been proposed since the 1950s, and can be conceptualized in five major models: biomedical, economic, social, embodied, and lastly, human rights based (Fougeyrollas et al., Citation2019). Although a consensus has been reached in the international community stating that disability is the product of social and environmental practices, a strong conceptual and operational framework is still needed (Ibid.).
The Disability Creation Process model (DCP, Fougeyrollas et al., Citation1998, ; Fougeyrollas et al., Citation2019) has been a powerful tool in providing conceptual and operational definitions of participation -and disability situations. Used in a broader range of contexts, and on a practical level, it has also helped in the development of policies and guided service delivery (Boucher et al., Citation2018; Fougeyrollas & Grenier, Citation2018). This model, based on the anthropological model of human development and disability, and on the human rights paradigm, explains the causes and consequences of disease, trauma, or other damage to the individual’s integrity or development. It states that the disability process cannot be grasped without considering the dynamic and interactive process between personal (intrinsic) factors and environmental (extrinsic) factors. This process determines the situational result of social participation, operationalized as the degree to which life habits are performed, on a continuum going from disability situation (participation restriction) to optimal (full) participation. These life habits—current or daily activities and social roles—are related to the individual’s age, gender, and sociocultural identity (Fougeyrollas & Charrier, Citation2013).
In the DCP, environmental components have a direct impact on, and are incorporated as a determinant of, social participation, similarly to intrinsic factors. Based on Bronfenbrenner’s ecological theory (Bronfenbrenner, Citation1979, Citation1994) this conceptual field is divided in three special levels, from micro (intimate analysis of the immediate living environment), to meso (local or community analysis), and then macro (analysis of society as a whole) level. This spatial perspective is relevant for the modulation of intervention strategies (Edwards et al., Citation2014; Noreau et al., Citation2015).
Environmental components refer to social or physical dimensions that determine a society’s organization and context in relation to the individual. Therefore, this classification is appropriate for every human, regardless of their level of disability, in different geographical or cultural contexts. In interaction with personal determinants, when it supports the accomplishment of life habits and provides optimal participation, an environmental factor is considered as a facilitator; in contrast, when contributing to disability situations or limiting the fulfillment of life habits, it is an obstacle.
1.2. Understanding Sickle Cell Disease: interaction between intrinsic and environmental factors
Sickle Cell Disease (SCD) is an hemoglobinopathy that belongs to a group of inherited autosomal recessive disorders, characterized by the production of abnormal hemoglobin (Bonner et al., Citation2010). SCD is the most widespread genetic disorder in the world (Wastnedge et al., Citation2018), and in Guadeloupe (French West Indies, Saint-Martin et al., Citation2013) where it affects approximately 1 in every 300 newborns. Its prevalence warrants a systematic neonatal screening throughout this territory (HAS, Citation2010). The severity of symptoms alters daily life and has led to its recognition as a disability, in the broader category of “disabling diseases” (Lespinet-Najib & Belio, Citation2013).
SCD places a significant emotional and physical burden on patients (Osunkwo et al., Citation2021). To experience this disease is, first and foremost, to experience chronic pain (Taylor et al., Citation2010; Wilkie et al., Citation2010), with unpredictable, repeated and painful crises that lead to the interruption of everyday activities, with sometimes very long stays in the hospital (Panepinto et al., Citation2005). As SCD is a genetic condition present from birth, this disease is likely to interact at an early age with developmental and personal factors, which have implications for cognitive and psychosocial functioning (Bonner et al., Citation2010; Prussien et al., Citation2020. Tarazi et al., Citation2007). The disorder thus affects mental health and quality of life of young patients, as shown by the prevalence of depressive syndromes and anxiety disorders within this population (Jerrell et al., Citation2011; Moody et al., Citation2019), and more generally, a lower quality of life (Graves et al., Citation2016; Houwing et al., Citation2022).
The metabolic and physiological SCD complications (anemia, vaso-occlusive crises), and impairments (in motricity due to osteonecrosis of the femoral head), in relation to the psychological dimensions (stress adaptation strategies), play a role in the limitations of children’s participation, and must be considered in connection with the individual’s environment.
A complex, social approach to this disease is thus necessary as it has historically been investigated more from a biomedical perspective, with political or social considerations in studies on hemoglobinopathies being more recent (Dyson & Atkin, Citation2012; Lainé & Tchernia, Citation2010). The theoretical and methodological anchoring of our study to a systemic and holistic approach such as the DCP model is thus relevant, as highlighted by our previous work (Ruffié et al., Citation2021; Cholley-Gomez et al., Citation2021).
Young SCD patients must face a doubly constraining environment, on both social and physical aspects. From an early age, medical recommendations are given to SCD children and their family, due to their vulnerability to, among various things, temperature variations, infectious risks, or physical effort (HAS, ibid.; American Society of Hematology—ASH, Citation2016; Tanabe et al., Citation2019), where environment plays a crucial role. In a daily life requiring constant monitoring, young sicklers face many activity restrictions. Limitations particularly concern sports and leisure activities, which have a strong social and cultural dimension, especially in the French Caribbean context (Pruneau et al., Citation2008). Analyzing the impact of SCD in a controlled study using the Life-H scale (life habits), we (Cholley-Gomez et al., Citation2021), highlighted a lower social participation score in young SCD Guadeloupians compared to controls. The accomplishment of daily activities and social roles was thus more impeded, in particular for leisure activities, community life, schooling and mobility.
Devoid of prospect of recovery, chronic illness involves, contrary to transitional acute illness, a constant management. It is not a rare life episode but a permanent state that merges with the life itself (Baszanger, Citation1986; Pierret, Citation1997). This feature—being a long-term or permanent component in an individual’s life—invites a sociological analysis of this experience, with emphasis on its timeframe (Bury, Citation1982, Citation1991), from the “biographical disruption” caused by the announcement of the diagnosis (Bury, Citation1982; Corbin & Strauss, Citation1987). Sociological research has shown the impact of such a turmoil on the patient’s experience and on his social interactions (Strauss & Glaser, Citation1975), according to the interactionist concept of “career”. It is thus possible to identify an “illness trajectory” characterized by organization of work, involving biographical and identity reorganizations—developed since the diagnostic, and then throughout the evolution of illness, to control it. In the case of SCD, the disruption is less experienced by the young sicklers, “born with illness” and diagnosed at birth, than by their parents, who face significant changes of their daily lives.
Negative social treatment of SCD also provides information on how patients face their social environment. Young SCD patients are caught between a familial micro-environment, which is protective, and negative social treatment of the disease. Works in the field of sociology and using an interactional approach offer a glimpse of the way in which SCD is experienced from a stigmatizing and exclusion angle, or of the self-exclusion from social spaces, by considering that the stigma is, within an interaction, what affects, by discrediting it, the social identity of an individual (Goffman, Citation1963).
Indeed, SCD is a stigmatized pathology (Bougerol, Citation1994; Bulgin et al., Citation2018; Lainé, Citation2009). Its categorization as “Blood disease”, by questioning heredity, conveys complex identity and symbolic meanings (Bonnet, Citation2001, Citation2009; Bonniol & Benoist, Citation1994). In the French Caribbean culture, traditional elements thus influence the social representation of this pathology, leading to a weak social visibility of it. In a previous work, Pruneau et al. (Citation2009) showed that the content of the social representation of SCD in young Guadeloupians was far from the biomedical definition, and underlined by social and identity issues. The notions of exclusion and contagion are part of a complex perception of the disease, which carries contrasted elements and is the result of a conflict between bad “reception” and bad “perception” (Ibid). Stigmatization thus operates at the crossroads of social and identity-related processes, orienting interaction postures just as much as avoidance strategies.
As they face an asymmetric interaction (Goffman, Citation1963) young patients may suffer from exclusion from social spaces-sometimes leading to negative self-perception. Therefore, SCD children grow up “with and despite the disease” by implementing strategies depending on social context (Atkin & Ahmad, Citation2001; Ciribassi & Patil, Citation2016). Family environment appears to be resilient, protective, even overprotective (Atkin & Ahmad, Citation2000; Bonnet, Citation2004, Citation2009; Reader et al., Citation2020;). In contrast, outside of the family unit, interpersonal relationships are more difficult and, sometimes ignoring recommendations, young patients with SCD try to be “secret keepers” (Héjoaka, Citation2012). This is particularly the case for physical and sport activities, where the challenge is “to restore a positive relationship with a bruised body” (Pruneau et al., Citation2008, p. 16). At school, they have a paradoxical desire for recognition, adjacent to a wish of normalization and “normal sociability” (Ibid.) -and often refuse to disclose their illness (Bibrac & Etienne-Julan, Citation2004).
2. Issue
Young children and teenagers with SCD thus evolve in a diversity of environments and various socializing contexts, which constitute barriers, or on the contrary, improve their social participation. These various settings—micro, family environment; meso, school and community environment; and macro-environment, at the level of society—in which they live with their functional limits or their particular capacities, shape the consciousness of their singularity.
What contextual determinants, social and physical factors of their environment, respectively, limit, and improve the accomplishment of their daily habits? How do youths with SCD perceive the Guadeloupean context, compared to their healthy peers?
3. Method
3.1. Study design and population
The study took place at the Sickle Cell Disease Transversal Unit (UTDFootnote1). The initial group of subjects included young patients (n = 102, from 6 to 16 years old, 49 females, 53 males), who suffered from severe forms of SCD (i.e., Major Sickle Cell Syndrome or Sβ0-thalassemiaFootnote2) and were monitored at the UTD. Other inclusion criteria for the study were the following: having been diagnosed during the neo-natal or natal period and having provided a declaration of non-opposition to the study (also signed by their legal representative). Out of the total cohort of 102 patients, our sample included 80 participants (Mage = 11.25 ± 3.23, 36 females, 44 males).
A control group, composed of healthy children (n = 45, age range = 6–16 years old, Mage = 10.55 ± 2.93, 22 females, 23 males) who were randomly selected and did not present any chronic disease, was also integrated into the study. The aim was to neutralize any possible effect linked to the context, as no study using the DCP model and evaluating social participation, or the perception of social and physical environmental factors, has been conducted within the specific context of Guadeloupe.
3.2. Assessment tool
Environmental factors were estimated with the Measure of the Quality of the Environment (Mesure de la Qualité de l’Environnement, Fougeyrollas et al., Citation1999, Citation2008), using prior adjustments of items to the population and the socio-cultural context (details of this adaptation of the tool are presented in our work, Cholley-Gomez et al., 2020). Based on the DCP conceptual framework, the MQE assesses the influence, or the perceived quality, of environmental factors divided into two sub-categories: social and physical factors (Fougeyrollas, Citation2010). These factors are grouped into areas/domains of the environment: politico-economics and socio-cultural for the social factors, and nature and land-use planning for the physical ones. Their influence is assessed on a 7-point scale ranging from major facilitator (+3) to major or complete obstacle (−3).
For further analyses, in addition to the score calculation, each answer/factor can be coded into three categories: obstacle, facilitator or no influence (Fougeyrollas, Citation2010). details, for each score on the assessment scale, its appreciation, and the corresponding definition.
Table 1. Detailed presentation of the Measure of the Quality of the Environment (MQE scale, adapted from Fougeyrollas, Citation2010)
Due to the complexity of some items (e.g., concerning political systems, social-health services), assessment sometimes required that a parent or a relative be present with the child, in case they were too young to fully understand the statement.
Additional socio-demographic data included: place of residence (recoded into 3 modalities: Grande-Terre, Basse-Terre, Central ZoneFootnote3), parents’ occupation (recoded into 3 modalities: Inactive, Worker-Employee, Intermediary-Upper level; Unknown-Deceased was also available but was not included in the analysis, where the data was considered as [missing data]) and their marital situation (recoded into 2 modalities depending on the family-structure of the child’s household: single parent vs. parents together, including new union situations), along with the number of siblings (including those from the previous or current union of each of the parents, recoded into 2 modalities: only child vs. presence of sibling(s)).
The main setting of the study was the UTD, within the University Hospital Centre (CHU) of Pointe-à-Pitre (n = 75) or, for patients who came from the Basse-Terre area, and depending on another hospital structure, the Basse-Terre Hospital Centre, CHBT (n = 5). For the control group, data was collected at convenient places for the subjects, mainly at home. Data was entirely collected using an eCRF.Footnote4
Analysis
Statistical analyses were conducted using Statistica and R 3.6.1 software. Discrete and continuous variables were compared using Khi2 test and Student’s t-test (for two groups) or ANOVA (for more than 2 groups) respectively. Normality of distribution was assessed with Kolmogorov–Smirnov tests; group sizes allowed us to perform parametric tests (Student’s t-test, ANOVA). Concerning the ANOVA, assumption of homogeneity of variance was examined with Levene’s test.
4. Results
4.1. Participant data
The sociodemographic characteristics of participants are presented and compared in . Characteristics of the participants were described using means and standard deviations or frequencies and percentages according to the type of variable (continuous or categorical, respectively) and compared across groups.
Table 2. Comparison of participant characteristics between SCD group and control group
4.2. MQE data analysis
Independent Sample t-test results (i.e., between SCD group, n = 80 and Control Group (CG, n = 45) are reported below, in . Mean scores (±Standard Deviation, SD) are presented for each contextual factor assessed by the MQE (n = 11 categories), including the physical environment subscore (comprising the following categories: traffic lanes, natural elements), the social environment subscore (social network, attitudes of entourage, sources of income, socio-health services, education services, public infrastructures, community-based organizations, social rules and political systems), and lastly, the overall environment score -i.e., the general perceived quality of the context.
Table 3. Mean scores (SD) of MQE factors according to group and T-Student results (p value)
Analyses showed a strong effect of the group variable on main outcomes: firstly, for global environment, i.e., the general perceived quality of the context, with a lower score in the SCD group compared to controls. Environmental factors were positively perceived by both, but lower in the SCD group. Physical environment was negatively rated by SCD participants, while it was positively assessed by controls, a statistically significant difference. Social factors were positively perceived by both groups, but the assessment score was significatively lower within the SCD group. Among the eleven categories composing the MQE, most of them were more negatively rated by SCD children than by their healthy peers (for the positive scores, perceived as being a weaker facilitator, and for the negative ones, as being a stronger obstacle). There was an exception, however, for socio-health services and Political systems: indeed, results indicated a positive rating, and a lower negative assessment (i.e., close to a lack of influence), respectively, with scores being similar for both groups (p = .61, and p = .91, respectively).
Other independent variables (socio-demographic data) were also statistically analyzed. Among them, gender had no influence on the quality of global environment (p = 51), boys and girls having similar scores (M = 0.82 ± 1.06 vs M = 8.21 ± 1.33). It did not either have any impact on the perception of social (p = .32) or physical (p = .47) components.
To briefly summarize family configurations, as these specific analyses were detailed in a parallel work (Cholley-Gomez et al., Citation2021), results showed that marital situation did not have an impact on the perception of overall, physical, or social environments for the SCD Group (p = 0.4, p = 0.1, and p = 0.7, respectively). It did, however, have an effect on the perception of overall environment, as well as on the social environment sub-category for controls (both for p < .05). Presence vs absence of siblings did not make any significant difference within the SCD Group concerning the overall, physical or social environment (p = 0.3, p = 0.9, and p = 0.3, respectively). The occupational category of the parents did impact the perception of environment. Indeed, the global environment score, as well as the social sub-category, were both significantly lower for SCD subjects with inactive parents, in comparison to those with parents who were workers or employees (p = 0.01, p < .01).
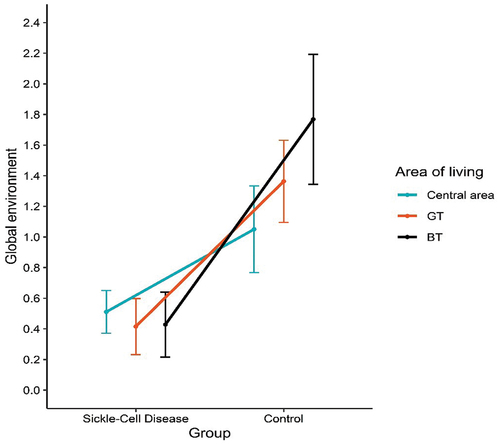
Contrary to expectation, the analysis of variance did not allow to conclude that the area of residence had a main effect on global environment perception, nor on the social or physical subcategories (p = 0.16, p = 0.19, and p = 0.15, respectively), scores between Basse–Terre (BT), Grande-Terre (GT) and the central area of the island being equivalent.
However, the interaction term of the ANOVA 3 (area of living)-by-2 (group) was significant when assessing overall environment (F (2, 119) = 5.33, p < .01). As shown in following graphical representation (), among the SCD group, all participants, regardless of their area of living, had a similar perception. Among the control group, residents of BT had a more positive perception of their global context (M = 1.75 ± 0.15) than residents of GT (M = 1.36 ± 0.10) and of the central area (M = 1.05 ± 0.14), the difference between these two last subgroups being significant.
The interaction term was also significant on physical (F (2, 119) = 7.75, p < .001) and, more moderately, on social (F (2, 119) = 3.54, p < .05) factors. In CG, concerning physical factors, BT score (M = 1.17 ± 0.21) was significatively higher than those from GT (M = 0.88 ± 0.14) and central area (M = 0.18 ± 0.19), with the two latter significantly differing from each other. Regarding the social context, the pattern of results was different: still for CG, BT score of assessment (M = 1.92 ± 0.17) was higher than GT (M = 1.49 ± 0.11) and central area (M = 1.24 ± 0.15), the difference between the last two being significant.
Identifying key drivers and constraints in the micro and meso-environments
As previously mentioned, social network is perceived as a facilitator for the young SCD patients. In a previous work (Cholley-Gomez et al., Citation2021) concerning the social participation of Guadeloupian SCD participants vs control group, we found that, concerning the life habit related to interpersonal relationships, both had similar performance scores. However, further analyses helped to clarify that although the relations within close family and friends were similar between groups, the broader relations, with non-family and peers, were more difficult for the young with SCD.
In the present work, through analyzing items from MQE social factors, we aimed to identify which social spaces and social interactions could provide resources or facilitators in the social environment of SCD children. Results are outlined in .
Table 4. Mean score (SD) of MQE social factors according to group, and T-Student (p value)
Briefly, among items composing the social network, support from family and loved ones has the highest score. Support from friends was perceived as a facilitator, but a less important one among patients. Similarly, in the school context, support from classmates was a lower facilitator among the SCD group, and this pattern of results was also noted with support from teaching staff.
Attitudes from entourage provided, in the micro-environment of young SCD patients, a minor facilitator (M = 0.92 ± 1.16), but all its components were systematically and significantly lower rated by SCD respondents, except for attitudes from the school doctor and attitudes from family and circle, both dimensions being similarly perceived; and except for religious beliefs, which provided a stronger driver among the SCD group. Among the social circle, only items relating to attitudes from persons belonging to group, and unknown people were negatively perceived. Attitudes from friends, attitudes from teaching staff and attitudes from sports teacher were more negatively perceived and assessed as weaker facilitators among SCD participants.
As previously noted, the education services score was lower among SCD respondents. In this category, except for the orientation service and school catering service showing no difference between groups (p = 0.12; p = 0.48), all the items were more negatively perceived by SCD participants. Moreover, two components were assessed as obstacles by young patients: physical layout of school buildings and school hours (M = −0.15 ± 1.40, M = −0.46 ± 1.46, respectively).
On the larger scale of the environment, factors related to cultural establishments (M = 0.82 ± 1.10 vs M = 1.95 ± 1.65, p < .001), recreational and sports organizations (M = 0.77 ± 1.43 vs M = 2.16 ± 1.15, p < .001), and public services (M = 0.82 ± 1.37 vs M = 1.38 ± 1.41, p < .001) provided less facilitators in the SCD patient’s daily life. While family incomes were described as a major facilitator by controls, the score was lower (i.e., slightly negative) among SCD participants (M = −0.06 ± 1.89 vs M = 2.00 ± 1.48, p < .001). In this regard, support provided by national Health Insurance & MDPH (departmental center for persons with disabilities) were strong facilitators (M = 2.04 ± 1.58) despite the negative perception of administrative procedures (M = −0.59 ± 1.89 vs M = 0.61 ± 1.91, p < .001).
The macro-level of political system and its components related to public programs and policy were, in an equivalent manner for both groups, minor obstacles in daily life. Media was more positively perceived by controls (M = 0.77 ± 1.63 vs M = 1.97 ± 1.09, p < .001).
Ultimately, although the analyses primarily focused on social contexts, results related to physical environments indicated that these factors restrain the daily activities of young patients with SCD, whereas they provide facilitators in controls’ everyday life. This was particularly the case for climatic conditions (M = −1.37 ± 1.22), access to drinking water (M = −1.13 ± 1.35), and land-use planning (M = −0.22 ± 1.22).
5. Discussion
As patients are faced with disease, environmental and psychosocial challenges, the significant impact of SCD on quality of life across a large group of diverse countries has been amply demonstrated (Graves et al., Citation2016; Sahil et al., 2019; Osunkwo et al., Citation2021; Houwing et al., Citation2022). However, to date, no previous study has investigated the social participation of SCD patients with an interactionist and systemic framework such as the Disability Creation Process. Yet a connection must be made between deficiencies, cognitive limitations or psychological determinants, and extrinsic factors, on different levels of the environment, in order to contextualize the mechanisms of disease and its consequences on the accomplishment of daily activities.
The aim of this study was to assess the perceived quality of environmental factors, both on their physical and social aspects and with a focus on social contexts, among young Guadeloupians with SCD, compared to a control group of healthy peers living in the same socio-cultural and geographical context. The main objective was to highlight the impact on social components, by stratifying them, e.g., family context, friend circle, school environment, or community level, and identifying in each setting the facilitators and obstacles to social participation. As we supported in a previous work (Cholley-Gomez et al., Citation2021) the hypothesis of an impact of living with SCD on the accomplishment of daily activities is evident, and we can here further understand the extrinsic limits to this participation.
Results emphasized that this restricted accomplishment occurs in a complex environment in which physical factors (e.g., land and infrastructure planning, natural elements) constitute strong barriers, and social determinants (e.g., support from friends, attitudes of schoolmates) are weaker facilitators. In short, key findings showed that all environmental factors assessed by the MQE were more negatively perceived among SCD participants, except for socio-health services (described as facilitators by both groups) and political systems (similarly rated as obstacles). Concerning this last macro-environmental factor, it must again be noted that due to the complexity of the items (e.g., public policy), assessment sometimes required that a parent or a relative be present with the child, if their age did not allow them to fully understand. Nevertheless, we observed the contextual effect that could be a potential bias and thus justified the control group in the study. Indeed, it appears that the perception of this contextual political factor was independent of health conditions, but rather should be replaced in the socio-cultural framework of Guadeloupe.
Concerning the positive perception of socio-health services, this result could reveal evidence of a social desirability bias among patients, as the assessment was made in a hospital context, in a specific care unit dedicated to SCD. In many cases, the investigator (social sciences researcher) was confusedly assimilated to a member of the medical staff. Data is not detailed in the current work, but our study design also included a qualitative axis with biographical interviews, often conducted at the home of patients and family, which provided more information, and qualified the quantitative data collected with questionnaires.
Results relating to socio-demographic characteristics also demonstrated that among the SCD group, only the occupational category of the family unit (and more precisely, the absence of a professional activity), had an impact on their perception of environmental factors, particularly social factors. Contrary to our previous findings showing the positive contribution of marital situation on patients’ social participation, it appears here that single parenthood does not worsen the perceived quality of the environment. However, family support is a major facilitator, as is the support of friends although in a weaker manner. Sickle Cell Disease is a specific chronic condition, being more collective than personal, as it highly involves family (Mitchell et al., Citation2007; Reader et al., Citation2020). Indeed, this is firstly the case due to its genetic and hereditary nature, and secondly because of the daily and collective management it involves (frequent hospitalizations, knowledge necessary to avoid and recognize vaso-occlusive crises or symptoms, reducing or ceasing professional activities).
In the micro and meso-environment, SCD patients face more difficulty in interpersonal relationships outside of their close social circle. Despite a larger media coverage at a local and national level, the disease is still stigmatized (Bulgin et al., Citation2018; Lainé, Citation2009; Pruneau et al., Citation2009, Pruneau et al., Citation2008), and more so in a school context. Indeed, in a previous work, our findings highlighted that participation in the school context was impacted by SCD status (Cholley-Gomez et al., Citation2021). In this setting, this limited accomplishment of their activity was, in addition, less compensated by positive environmental factors: schoolmates and teachers’ attitudes, and more widely education services, were classified as resources, but less strongly compared to the perception of healthy participants. In this category, obstacles were non-human elements (i.e., physical disposition and schedule).
SCD patients’ schooling is sometimes chaotic, with many gaps and absences, due to the frequency of crises and/ or hospitalizations (Dampier et al., Citation2010; Poku et al., Citation2018). At school, despite the progress made in terms of accompanying measures and information provided to education staff, some teachers can misunderstand the disease, believing that the child is lazy or plaintive (Pondarré et al., Citation2020). In a recent study investigating the relationships between cognitive and academic skills, (Pondarré et al., Citation2020), in line with previous work on cognitive functioning in SCD children (Bernaudin et al., Citation2000; Puffer et al., Citation2010; Schatz et al., Citation2002), noted that SCD does not systematically lead to visible difficulties or impairments, even though young individuals with SCD can easily tire, suffer from attention, concentration and memorization limitations, and thus should receive further attention from education staff.
Lastly, on a macro-environment level, public orientations and policies are negatively perceived by most participants, regardless of their health condition, and these factors do not improve the social participation of young patients with SCD. Disabilities generated by this condition make it necessary, on a local level, to create more inclusive spaces in school settings, professional training, sports and leisure activities, as well as in the cultural offer.
6. Conclusion
In applying the comprehensive DCP model to understand how these young patients interact with their family, and in educational or community-based settings, this work is in line with previous studies investigating multiple sclerosis, HIV or cystic fibrosis (Ferez et al., Citation2021, Ferez et al., Citation2015; Lacroix et al., Citation2016).
This study highlights the complex environment that young patients face, including physical and social components, and provides information for clinicians and researchers interested in understanding and improving quality of life and social participation in this young population. At a practical level, the DCP model (Badley, Citation2008; Whiteneck & Djikers, Citation2009) has been widely used to guide policy development and service delivery within the province of Quebec, has supported the development of rehabilitation programs, in addition of having being a useful framework for aligning research with clinical practice (Fougeyrollas, Citation2010; Fougeyrollas et al., Citation2019).
Our findings have implications for practices of professionals and local stakeholders who work at the various levels and within the different spheres of a young patient (e.g., medical and educational professionals, local political authorities, members of local associations, relevant institutions). In particular, healthcare professionals play a crucial role for patients and families, as socio-health services are positively perceived and are a facilitator in the child’s environment. School is also an important setting for the social participation of a child. In order to promote optimal relationship with peers, and academic functioning, teachers and school-based caregivers should provide more support for children with SCD (e.g., by allowing learning accommodations and recourse to education services).
Finally, additional analyses will complete this data by considering the dynamic interaction between environmental and individual factors (e.g., clinical manifestations of SCD, neuro-psychological disorders) when examining the social participation of individuals with SCD. These conclusions will stimulate reflection concerning the challenges and opportunities offered by the transdisciplinarity of this project and its conceptual rooting in a complex model such as the DCP, issues that are the focus of an ongoing discussion (Ruffié et al., 2020).
Disclosure statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.Citation2021
Additional information
Funding
Notes
1. The Unité Transversale de la Drépanocytose—UTD, Reference centre for sickle cell disease, part of the Pointe-à-Pitre hospital, initiates a complex and diverse approach to care, through the combination of medical, psychological and social monitoring. Paediatricians, neuropsychologists and computer engineers of the Clinical Investigation Centre of the hospital also participated in this research.
2. Other major sickle cell syndromes present compound heterozygous forms in which haemoglobin is associated with certain abnormal haemoglobins; S/C, S/D Punjab, S/Lepore, S/E forms (Etienne-Julan & Saint-Martin, 2005) but are less symptomatic and are not taken into account in this project.
3. The Guadeloupean landscape presents various territorial, climatic and cultural specificities. The Northern or superior part, named Grande-Terre and more urban, is more exposed to the trade winds and is much dryer than Basse-Terre due to the lower elevation (maximum 125 metres above sea-level) and the geology. The surface hydrography there is low; the island of Basse-Terre, more rural and where the Soufrière volcano can be found, along with the humid tropical forest covering its mountainous heights, is marked by a higher altitude and more relief, as well as more frequent rain (Pagney, Citation1991). The part known as Central (including Baie-Mahault, Pointe-à-Pitre and the Abymes) constitutes the active heart, the industrial and commercial area of Jarry being considered the economic lungs of the territory.
4. An eCRF is a digital form, the goal of which is to obtain information useful to a clinical research project.
References
- American Society of Hematology – ASH. (2016). Clinical practice guidelines on Sickle Cell Disease. https://ashpublications.org/ashclinicalnews/news/5229/ASH-Releases-Clinical-Practice-Guidelines-on
- Atkin, K., & Ahmad, W. (2000). Family care-giving and chronic illness: How parents cope with a child with a sickle cell disorder or Thalassaemia. Health & Social Care in the Community, 8(1), 57–15. https://doi.org/10.1046/j.1365-2524.2000.00211.x.
- Atkin, K., & Ahmad, W. (2001). Living a ‘normal’ life: Young people coping with Thalassaemia major or sickle cell disorder. Social Science & Medicine, 53(56), 615–626. https://doi.org/10.1016/s0277-9536(00)00364-6.
- Badley, E. (2008). Enhancing the conceptual clarity of the activity and participation components of the international classification of functioning, disability, and health. Social Science & Medicine, 66(11), 2335–2345. https://doi.org/10.1016/j.socscimed.2008.01.026
- Baszanger, I. (1986). Les maladies chroniques et leur ordre négocié. Revue Française de Sociologie, 27(1), 3–27. DOI : 10.2307/3321642.
- Bernaudin, F., Verlhac, S., Fréard, F., Roudot-Thoraval, F., Benkerrou, M., Thuret, I., Mardini, R., Vannier, J. P., Ploix, E., Romero, M., Cassé-Perrot, C., Helly, M., Gillard, E., Sebag, G., Kchouk, H., Pracros, J. P., Finck, B., Dacher, J. N., Ickowicz, V., & Brugières, P. (2000). Multicenter prospective study of children with Sickle Cell Disease: Radiographic and psychometric correlation. Journal of Child Neurology, 15(5), 333–343. https://doi.org/10.1177/088307380001500510
- Bibrac, A., & Etienne-Julan, M. (2004). Le centre caribéen de la drépanocytose « Guy Mérault »: Un modèle de prise en charge globale et intégré. In A. Lainé (Ed.), La Drépanocytose. Regards croisés sur une maladie orpheline (pp. 376). Karthala.
- Bonner, M. J., Puffer, E. S., & Willard, V. W. (2010). Sickle Cell Disease. In R. J. Shaw & D. R. DeMaso (Eds.), Textbook of pediatric psychosomatic medicine (pp. 259–274). American Psychiatric Publishing, Inc.
- Bonnet, D. (2001). Rupture d’alliance contre rupture de filiation. Le cas de la drépanocytose en Côte d’Ivoire. In J. P. Dozon & D. Fassin (Eds.), La Culture selon la santé publique (pp. 332). Balland.
- Bonnet, D. (2004). Drépanocytose et ethnicité. In A. Lainé (Ed.), La drépanocytose: Regards croisés sur une maladie orpheline (pp. 45–73). Karthala.
- Bonnet, D. (2009). Repenser l’hérédité. Éditions des archives contemporaines.
- Bonniol, J.-L., & Benoist, J. (1994). Hérédités plurielles, représentations populaires et conceptions savantes du métissage. Ethnologie française, 24(1), 58–69. http://classiques.uqac.ca/contemporains/bonniol_jean_luc/heredites_plurielles/heredites_plurielles.html.
- Boucher, N., Dumont, I., Fougeyrollas, P., Ruel, J., & Moreau, A. (2018). Perspective d’analyse comparée des effets des plans d’action à l’égard des personnes handicapées sur les territoires des villes de Sherbrooke, de Trois-Rivières, Victoriaville et de Cowansville, 2011-2015. Rapport. Bibliothèque et Archives nationales du Québec.
- Bougerol, C. (1994). Approche anthropologique de la drépanocytose chez des malades antillais. Sciences sociales et santé, 12(3), 48–68. https://doi.org/10.3406/sosan.1994.1300.
- Bronfenbrenner, U. (1979). The ecology of human development. Experiments by nature and design. Harvard University Press.
- Bronfenbrenner, U. (1994). Ecological models of human development. The International Encyclopedia of Education, 3(2), 1643–1647.
- Bulgin, D., Tanabe, P., & Jenerette, C. (2018). Stigma of Sickle Cell Disease: A systematic review. Issues in Mental Health Nursing, 39(8), 675–686. https://doi.org/10.1080/01612840.2018.1443530
- Bury, M. (1982). Chronic illness as a biographical disruption. Sociology of Health & Illness, 4(2), 167–182 DOI: 10.1111/1467-9566.ep11339939.
- Bury, M. (1991). The sociology of chronic illness: A review of research and prospects. Sociology of Health & Illness, 13(4), 451–468 https://doi.org/10.1111/j.1467-9566.1991.tb00522.x.
- Cholley-Gomez* M, Ruffié* S, Villoing G, Boucher N and Fougeyrollas P. (2021). Évaluer la participation sociale de jeunes drépanocytaires. Recherche transdisciplinaire et adaptation des outils de recueil de données MHAVIE et MQE au contexte socioculturel de la Guadeloupe1. aequitas, 26(2), 43–64. 10.7202/1075205ar
- Ciribassi, R. M., & Patil, C. L. (2016). “We don’t wear it on our sleeve”: Sickle cell disease and the (in)visible body in parts. Social Science & Medicine, 148, 131–138. https://doi.org/10.1016/j.socscimed.2015.11.033
- Corbin, J., & Strauss, A. (1987). Accompaniments of chronic illness: Changes in body, self, biography and biographical time. Research in the Sociology of Health Care, 6, 249–281. https://doi.org/10.1177/1049732302239603.
- Dampier, C., Lieff, S., LeBeau, P., Rhee, S., McMurray, M., Rogers, Z., Smith-Whitley, K., & Wang, W., Comprehensive Sickle Cell Centers (CSCC) Clinical Trial Consortium (CTC). (2010). Health-related quality of life in children with Sickle Cell Disease: A report from the comprehensive Sickle Cell Centers clinical trial consortium. Pediatric Blood & Cancer, 55(3), 485–494. https://doi.org/10.1002/pbc.22497
- Dyson, S., & Atkin, K. M. (2012). Sickle cell and Thalassaemia: Global public health issues come of age. In S. Dyson & K. Atkin (Eds.), Genetics and global public health (pp. 1–13). Routledge.
- Edwards, G., Noreau, L., Boucher, N., Fougeyrollas, P., Grenier, Y., McFadyen, B. J., Morales, E., & Vincent, C. (2014). Disability, rehabilitation research and post-cartesian embodied ontologies has the research paradigm changed? Environmental Contexts and Disability, 8, 73–102. https://doi.org/10.1108/S1479-354720140000008005
- Ferez, S., Silvestri, L., & Issanchou, D. (2021). Les obstacles à la participation professionnelle rencontrés par les jeunes atteints de mucoviscidose: Le poids de l’environnement humain. Revue française des affaires sociales, 4, 137–157. https://doi.org/10.3917/rfas.214.0137
- Ferez, S., Wallach, I., Gaucher, C., Heas, S., Ruffié, S., Thomas, J., Gaissad, L., Perez, M., Duval, E., Cervera, M. et al. (2015). Effets du diagnostic d’infection au VIH sur la participation sociale: Enjeux de l’application du processus de production du Handicap à une maladie chronique. Développement humain, handicap et changement social, 21(2), 75–88. https://doi.org/10.7202/1086470ar
- Fougeyrollas, P. (2010). Le Funambule, le fil et la toile. Transformations réciproques du sens du handicap. Québec, Presses Universitaires de Laval.
- Fougeyrollas, P., Bergeron, H., Cloutier, R., Côté, J., & St-Michel, G. (1998). Classification québécoise: Processus de production du handicap. Québec, Réseau international sur le processus de production du handicap, RIPPH/SCCIDIH, 166p.
- Fougeyrollas, P., Boucher, N., Edwards, G., Grenier, Y., & Noreau, L. (2019). The disability creation process model: A comprehensive explanation of disabling situations as a guide to developing policy and service programs. Scandinavian Journal of Disability Research, 21(1), 25–37. https://doi.org/10.16993/sjdr.62
- Fougeyrollas, P., & Charrier, F. (2013). Modèle du Processus de production du handicap. EMC –Kinésithérapie-Médecine physique-Réadaptation, 9(3), 1–8 doi:10.1016/S1283-0887(13)56628-X.
- Fougeyrollas, P., & Grenier, Y. (2018). Monitoring disability policies and legislation towards effective exercise of rights to equality and inclusive access for persons with disabilities: The case of the Quebec model. Societies, 8(2), 41. https://doi.org/10.3390/soc8020041.
- Fougeyrollas, P., Noreau, L., St-Michel, G., & Boschen, K. (1999). Mesure de la Qualité de l’Environnement. Lac St-Charles (Québec): CQCIDIH.
- Fougeyrollas, P., Noreau, L., St-Michel, G., & Boschen, K. (2008 https://ripph.qc.ca/wp-content/uploads/2017/09/MQE_Guide-long_francais_reproduction-interdite.pdf). Mesure de la Qualité de l’Environnement, MQE 2.0. RIPPH - C.P. 225. Lac St-Charles (Québec).
- Goffman, E. (1963). Stigmates, les usages sociaux des handicaps. Éditions de Minuit.
- Graves, J. K., Hodge, C., & Jacob, E. (2016). Depression, anxiety, and quality of life in children and adolescents with Sickle Cell Disease. Journal of Pediatric Nursing, 42(3), 113–144. https://doi.org/10.1182/bloodadvances.2017006940
- Haute Autorité de Santé, H.A.S (2010). Syndromes drépanocytaires majeurs de l’enfant et de l’adolescent -protocole national de diagnostic et de soins pour une maladie rare – Actualisé en 2014. https://www.has-sante.fr/jcms/c_938890/fr/ald-n-10-syndromes-drepanocytaires-majeurs-de-l-enfant-et-de-l-adolescent
- Héjoaka, F. (2012). L’enfant gardien du secret. Vivre et grandir avec le sida et ses traitements à Bobo Dioulasso (Burkina Faso). [Thèse]. Ecole des Hautes Etudes en Sciences Sociales.
- Houwing, M. E., Muntendam, M. J., van Muilekom, M. M., Teela, L., Fijnvandraat, K., de Pagter, A., Heijboer, H., van Oers, H. A., Cnossen, M. H., & Haverman, L. (2022). Health-related quality of life in infants, toddlers and young children with Sickle Cell Disease. Pediatric Blood & Cancer, 69(1), e29358. https://doi.org/10.1002/pbc.29358
- Jerrell, J. M., Tripathi, A., & McIntyre, R. S. (2011). Prevalence and treatment of depression in children and adolescents with sickle cell disease: a retrospective cohort study. The Primary Care Companion for CNS Disorders, 13(2). PCC.10m01063. https://doi.org/10.4088/PCC.10m01063
- Lacroix, N., Boucher, N., & Villeneuve, P. (2016). Participation sociale et sclérose en plaques: Réalité particulière. Service Social, 62(2), 94–113. https://doi.org/10.7202/1038579ar.
- Lainé, A. (2009 https://hal.archives-ouvertes.fr/hal-00436022). Constructions d’un stigmate sanitaire: La drépanocytose, entre situations locales et globales. Université Jean-Moulin-Lyon 3.
- Lainé, A., & Tchernia, G. (2010, 3). « L’émergence » d’une maladie multimillénaire. Circulations de savoir et production d’inégalités face à la drépanocytose. In V. Chasles (Ed.), Santé et mondialisation (pp. 239–261). Université Jean-Moulin-Lyon.
- Lespinet-Najib, V., & Belio, C. (2013). Classification des handicaps: Enjeux et controverses. Hermès, La Revue, 66(2), 104–110. https://doi.org/10.4267/2042/51561
- Mitchell, M. J., Lemanek, K., Palermo, T. M., Crosby, L. E., Nichols, A., & Powers, S. W. (2007). Parent perspectives on pain management, coping, and family functioning in pediatric Sickle Cell Disease. Diagnostique, 46(4), 115–124. https://doi.org/10.1177/153450849902401-411
- Moody, K. L., Mercer, K., & Glass, M. (2019). An integrative review of the prevalence of depression among pediatric patients with Sickle Cell Disease. Social Work in Public Health, 34(4), 343–352. https://doi.org/10.1080/19371918.2019.1606754
- Noreau, L., Boucher, N., Edwards, G., Fougeyrollas, P., Routhier, F., & Vincent, C. (2015). Enhancing independent community access and participation: Services, technologies and policies. Oxford Textbook of Neurorehabilitation, 33, 399–418. https://doi.org/10.1093/med/9780199673711.003.0033
- Osunkwo, I., Andemariam, B., Minniti, C. P., Inusa, B. P. D., El Rassi, F., Francis‐Gibson, B., Nero, A., Trimnell, C., Abboud, M. R., Arlet, J.-B., Colombatti, R., Montalembert, M., Jain, S., Jastaniah, W., Nur, E., Pita, M., DeBonnett, L., Ramscar, N., Bailey, T., and James, J. (2021). Impact of sickle cell disease on patientsʼ daily lives, symptoms reported, and disease management strategies: Results from the international Sickle Cell world assessment survey (SWAY). American Journal of Hematology, 96(4), 404–417 https://doi.org/10.1002/ajh.26063.
- Pagney, J. (1991). Le climat des Antilles. Masson.
- Panepinto, J. A., Brousseau, D. C., Hillery, C. A., & Scott, J. P. (2005). Variation in hospitalizations and hospital length of stay in children with vaso-occlusive crises in sickle cell disease. Pediatric Blood & Cancer, 44(2), 182–186. https://doi.org/10.1002/pbc.20180
- Pierret, J. (1997). Un objet pour la sociologie de la maladie chronique: La situation de séropositivité au VIH ? Sciences Sociales et Santé, 15(4), 97–120 https://doi.org/10.3406/sosan.1997.1413.
- Poku, B. A., Caress, A. L., & Kirk, S. (2018). Adolescents’ experiences of living with sickle cell disease: An integrative narrative review of the literature. International Journal of Nursing Studies, 80, 20–28. https://doi.org/10.1016/j.ijnurstu.2017.12.008
- Pondarré, C., Lemmet, C., Ducros-Mirallès, E., Chomentowski, M., Rebmeister, B., & Ruffieux, N. (2020 https://bit.ly/chicreteil-drepanocytose.). DREPASCOL: Synthèse scientifique de la recherche.
- Pruneau, J., Ferez, S., Maillard, F., Philippon, B., & Hue, O. (2009). « Accès à la culture biomédicale et enjeux socio-symboliques des représentations de la drépanocytose dans une population scolaire de Guadeloupe ». Etudes caribéennes, 12 https://doi.org/10.4000/etudescaribeennes.3684. [En ligne], mis en ligne le 9 septembrehttp://etudescaribeennes.revues.org/document3684.html
- Pruneau, J., Philippon, B., Maillard, F., & Hue, O. (2008). Sport et drépanocytose: Le paradoxe dans l’itinéraire thérapeutique des adolescents drépanocytaires « SS » en Guadeloupe ». Sciences sociales et santé, 26(2), 5–32. https://doi.org/10.3917/sss.262.0005.
- Prussien, K. V., Siciliano, R. E., Ciriegio, A. E., Anderson, A. S., Sathanayagam, R., DeBaun, M. R., Jordan, L. C., & Compas, B. E. (2020). Correlates of cognitive function in Sickle Cell Disease: A meta-analysis. Journal of Pediatric Psychology, 45(2), 145–155. https://doi.org/10.1093/jpepsy/jsz100
- Puffer, E. S., Schatz, J. C., & Roberts, C. W. (2010). Relationships between somatic growth and cognitive functioning in young children with Sickle Cell Disease. Journal of Pediatric Psychology, 35(8), 892–904. https://doi.org/10.1093/jpepsy/jsp124
- Reader, S. K., Pantaleao, A., Keeler, C. N., Ruppe, N. M., Kazak, A. E., Rash-Ellis, D. L., Wadman, J., Miller, R. E., & Deatrick, J. A. (2020). Family resilience from the perspective of caregivers of youth With Sickle Cell Disease. Journal of Pediatric hematology/oncology, 42(2), 100–106. https://doi.org/10.1097/MPH.0000000000001682
- Ruffié S, Cholley Gomez M, Villoing G, Ferez S, Boucher N and Fougeyrollas P. (2021). Penser les effets du désavantage social liés à la maladie chronique : enjeux épistémologiques d’un projet transdisciplinaire sur des jeunes drépanocytaires en Guadeloupe. Alter, 15(2), 177–189. 10.1016/j.alter.2020.07.003
- Saint-Martin, C., Romana, M., Bibrac, A., Brudey, K., Tarer, V., Divialle-Doumdo, L., Petras, M., Keclard-Christophe, L., Lamothe, S., Broquere, C., & Etienne-Julan, M. (2013). Universal newborn screening for haemoglobinopathies in Guadeloupe (French West Indies): A 27-year experience. Journal of Medicine Screen, 20(4), 177–182. https://doi.org/10.1177/0969141313507919
- Schatz, J., Finke, R. L., Julie, M. K., Kellett, M. J., & Kramer, H. K. (2002). Cognitive functioning in children with Sickle Cell Disease: A meta-analysis. Journal of Pediatric Psychology, 27(8), 739–748. https://doi.org/10.1093/jpepsy/27.8.739
- Strauss, A., & Glaser, B. (1975). Chronic illness and quality of life. Mosby.
- Tanabe, P., Spratling, R., Smith, D., Grissom, P., & Hulihan, M. (2019). Understanding the complications of Sickle Cell Disease. American Journal of Nursing, 119(6), 26–35. https://doi.org/10.1097/01.NAJ.0000559779.40570.2c
- Tarazi, R. A., Grant, M. L., Ely, E., & Barakat, L. P. (2007). Neuropsychological functioning in preschool-age children with sickle cell disease: The role of illness-related and psychosocial factors. Child Neuropsychology: a Journal on Normal and Abnormal Development in Childhood and Adolescence, 13(2), 155–172. https://doi.org/10.1080/09297040600611312
- Taylor, L. E., Stotts, N. A., Humphreys, J., Treadwell, M. J., & Miaskowski, C. (2010). A review of the literature on the multiple dimensions of chronic pain in adults with sickle cell disease. Journal of Pain and Symptom Management, 40(3), 416–435. https://doi.org/10.1016/j.jpainsymman.2009.12.027
- Wastnedge, E., Waters, D., Patel, S., Morrison, K., Goh, M. Y., Adeloye, D., & Rudan, I. (2018). The global burden of sickle cell disease in children under five years of age: A systematic review and meta-analysis. Journal of Global Health, 8(2), 021103. https://doi.org/10.7189/jogh.08.021103
- Whiteneck, G., & Djikers, M. P. (2009). Difficult to measure constructs: Conceptual and methodological issues concerning participation and environmental factors. Archives of Physical Medicine and Rehabilitation, 90(11), S22–S35. https://doi.org/10.1016/j.apmr.2009.06.009
- Wilkie, D. J., Molokie, R., Boyd-Seal, D., Suarez, M. L., Young, K., Zong, S., Wittert, H., Zhao, Z., Saunthararajah, Y., & Wang, Z. J. (2010). Patient-reported outcomes: Descriptors of nociceptive and neuropathic pain and barriers to effective pain management in adult outpatients with Sickle Cell Disease. Journal of the National Medical Association, 102(1), 18–27. https://doi.org/10.1016/S0027-9684(15)30471-5