Abstract
Purpose: To assess the feasibility of recruitment procedures and delivery of a Norwegian adaptation of a manualized cognitive intervention to a civilian sample with traumatic brain injury (TBI).
Materials and methods: Six individuals received a 10-week group-based intervention (Compensatory Cognitive Training, CCT) targeting post-concussive symptom management and cognitive symptoms. Participant engagement (i.e. attendance, level of participation, ability to learn and apply strategies, and homework completion) and satisfaction were assessed by the Therapist Checklist and CCT Feedback Form.
Results: All participants had a diagnosis of concussion, were enrolled on average 4 months post-injury, and were sick-listed at a range of 70–100% at the time of inclusion. Attendance across CCT sessions was 97%. Eight out of nine topics in the CCT-intervention received a rating above 3.5 on a 5-point scale (i.e. towards very helpful). The items that received the highest mean ratings were information about TBI and post-concussive symptoms, and strategies targeting fatigue, prospective memory, and memory and learning. All participants were rated as participating fully (3/6) or moderately (3/6), and most participants (5/6) attempted to apply the trained skills to real-life situations.
Conclusions: The results support the feasibility of a Norwegian adaptation of the intervention for a civilian sample with TBI.
Public Interest Statement
Traumatic brain injury (TBI) may lead to functional impairments and difficulties with performing daily activities, including return to work and maintaining stable employment. This study aimed to assess the feasibility of a group-based cognitive intervention, Compensatory Cognitive Training (CCT), covering psychoeducation and compensatory cognitive strategies, previously administered to veterans with TBI in the US. We delivered a Norwegian adaptation of the intervention to a civilian sample with mild and moderate TBI and assessed the participants’ satisfaction with the intervention and ability to engage with it. The participants found most of the information and strategies provided in the intervention helpful, and were able to apply the skills to a satisfactory degree. The study gave insight into practical aspect that will be important to consider when initiating a larger scale trial evaluating the effect of combining CCT and supported employment on vocational outcome in individuals with traumatic brain injury.
Disclosure statement
The authors report no conflicts of interest.
1. Introduction
Traumatic brain injury (TBI), defined as “an alteration in brain function, or other evidence of brain pathology, caused by an external force” (Menon, Schwab, & Wright et al., Citation2010), is a public health concern and may result in long-term disability, decreased quality of life, and significant personal and socio-economic costs (Corrigan, Selassie, & Orman, Citation2010; Roozenbeek, Maas, & Menon, Citation2013). It is estimated that 50–60 million new cases of TBI occur worldwide each year, of which 2.5 million new cases occur in the European Union, and 3.5 million cases in the US (Maas et al., Citation2017).
Among reported TBIs, approximately 70–90% are classified as mild or moderate (Maas et al., Citation2017). For most individuals in the mild end of the TBI spectrum, symptoms resolve within weeks following the injury (Sigurdardottir, Andelic, Roe, Jerstad, & Schanke, Citation2009). For others, physical, emotional, and cognitive complaints, referred to as post-concussive symptoms, persist beyond this point, which may lead to functional limitations and difficulties coping with the demands of everyday life, such as returning to work, or social activities (Levin & Diaz-Arrastia, Citation2015). A substantial number of TBIs are sustained by adults who are in working age (Roozenbeek et al., Citation2013). The literature suggests that approximately 5–20% of workers who sustain a mild TBI experience persisting problems in the longer term (Cancelliere et al., Citation2014). TBI may also affect vocational outcomes besides return to work (RTW), including employment stability and productivity (Chu, Tsai, Xiao, Huang, & Yang, Citation2017; Ponsford & Spitz, Citation2015; Silverberg, Panenka, & Iverson, Citation2018; Theadom et al., Citation2017).
Although several studies have identified demographic, functional, pre-injury and injury-related factors that may predict RTW after TBI (Saltychev, Eskola, Tenovuo, & Laimi, Citation2013; Shames, Treger, Ring, & Giaquinto, Citation2007; Yasuda, Wehman, Targett, Cifu, & West, Citation2001), systematic reviews assessing vocational rehabilitation following TBI have not shown strong evidence for effectiveness (Fadyl & McPherson, Citation2009). A Campbell review (Graham, West, & Bourdon et al., Citation2016) assessed the effectiveness of vocational interventions aimed at helping individuals with TBI to attain competitive employment. Although finding positive gains, the three randomized controlled trials (RCTs) included in the review showed no greater effect on vocational outcomes than the treatment received by the control groups (Man, Poon, & Lam, Citation2013; Salazar et al., Citation2000; Twamley, Jak, Delis, Bondi, & Lohr, Citation2014; Twamley et al., Citation2015). The study sample in two of the three RCTs were veterans (Salazar et al., Citation2000; Twamley et al., Citation2014, Citation2015). The review concludes that there is a need for more RCTs that assess a broader range of employment outcomes (such as hours worked and wages earned), including studies of adult civilian populations with TBI outside the US. Other reviews have assessed the efficacy of specific approaches, such as cognitive rehabilitation. A recently published Cochrane review evaluated the effects of cognitive rehabilitation on return to work (Kumar, Samuelkamaleshkumar, & Viswanathan et al., Citation2017). The authors identified four randomized controlled trials (Cicerone et al., Citation2008; Salazar et al., Citation2000; Twamley et al., Citation2014; Vanderploeg et al., Citation2008) specifically aiming to improve RTW but did not find sufficient evidence that cognitive rehabilitation improved RTW-rates and noted that the quality of evidence was too low to allow firm conclusions.
There are several factors which underline the importance of studies on vocational rehabilitation in civilian populations outside the US. An obvious reason is that PTSD-related symptomatology likely will be less prevalent when injuries sustained in combat settings are excluded. Socio-economic status may also be expected to vary between military populations in the US, and a civilian population in a high-income country like Norway. Additionally, universal access to healthcare may have an impact on what is considered as “treatment as usual,” and studies comparing interventions to treatment as usual may yield different results depending on where they are performed. Lastly, work-related welfare systems may affect motivation and willingness to return to work.
In sum, few studies have explored the effect of combined cognitive and vocational rehabilitation efforts on vocational outcomes following TBI (Man et al., Citation2013; Twamley et al., Citation2014). In preparation for a larger scale RCT evaluating the effect of combining a cognitive intervention (Compensatory Cognitive Training, CCT) and supported employment (SE) on vocational outcome in individuals with mild-to-moderate TBI, a feasibility study was performed at Oslo University Hospital (OUH), Norway, in the Spring of 2017. The full protocol for the trial has been described in a previous paper (Howe et al., Citation2017). The aim of the feasibility study was to assess the feasibility of recruitment procedures and delivery of a Norwegian adaptation of a manualized cognitive intervention to a civilian sample with mild-to-moderate TBI in the South-Eastern region of Norway. Specifically, the feasibility of recruitment procedures and delivery of the cognitive part of the intervention (i.e. a Norwegian translation and adaptation of the CCT manual) was assessed by exploring whether the procedures were satisfactory in terms of: 1) recruitment and retention (i.e. drop-out), 2) acceptability (i.e. satisfaction with the intervention, load of follow-up), and 3) treatment engagement (i.e. attendance, level of participation, ability to learn and apply strategies). The feasibility of delivering the vocational part of the intervention (supported employment) is not addressed in this paper but will be evaluated in subsequent publications.
The Medical Research Council (MRC) (Craig et al., Citation2008) underlines the importance of feasibility or pilot testing when developing, implementing and evaluating complex interventions. The MRC further points to the impact of the local context in which the intervention is carried out and urges researchers to pay greater attention to feasibility or pilot testing to tailor the intervention to the specific context. This advice might be particularly relevant regarding vocational rehabilitation, as national welfare systems, protection of the workforce, and job markets vary substantially between countries.
2. Materials and methods
2.1. Participants
Individuals with TBI who were referred to the Department of Physical Medicine and Rehabilitation at OUH from the neurosurgical department at OUH, and from general practitioners, were identified as potential participants. Once identified, they were screened according to the following inclusion criteria: residents of Oslo or Akershus county, aged 18–60 years, with mild-to-moderate TBI as measured by a Glasgow Coma Scale (GCS) score of 10–15, loss of consciousness (LOC) for <24 hours and posttraumatic amnesia <7 days (Management of Concussion/mTBI Working Group, Citation2009). The criteria for diagnosing mild TBI developed by the American Congress of Rehabilitation Medicine (ACRM), (Citation1993) were used to establish the presence of mild TBI, either according to patient records or while screening for eligibility. Participants were included if they were employed in a minimum 50% position at the time of injury, and sick-listed 50% or more due to post-concussive symptoms, as assessed by the Rivermead Post Concussion Symptoms Questionnaire (RPQ). Exclusion criteria included inability to speak or read Norwegian, severe pre-existing neurological or psychiatric disorders, and active substance abuse. The study was approved by the Norwegian Regional Committee for Medical and Health Research Ethics (REK nr. 2016/2038) and performed in accordance with the principles of the Declaration of Helsinki. Information about the study was presented to participants in written and oral form, and written informed consent was obtained upon agreement to participate.
2.2. The intervention
Compensatory Cognitive Training, CCT (Storzbach et al., Citation2017), is a further development of Cognitive Symptom Management and Rehabilitation Therapy (CogSMART), developed by Professor Elizabeth W. Twamley and colleagues (Twamley et al., Citation2014, Citation2015). CCT and CogSMART has previously been administered to individuals with severe mental illness (Twamley, Vella, Burton, Heaton, & Jeste, Citation2012) and veterans with a history of mild-to-moderate TBI (Storzbach et al., Citation2017; Twamley et al., Citation2014, Citation2015). When administered to veterans with TBI, CogSMART and CCT has shown to reduce post-concussive symptoms, improve subjective and objective measures of cognitive function, and quality of life (Storzbach et al., Citation2017; Twamley et al., Citation2014, Citation2015).
CCT is a manualized intervention targeting post-concussive symptom management and cognitive symptoms (Storzbach et al., Citation2017). It is a group-based treatment program delivered in 10 two-hour sessions in which the participants receive psychoeducation and learn compensatory cognitive training strategies. The CCT intervention is based on theoretical literature on compensatory strategy training for populations who suffer from cognitive symptoms, such as TBI, severe mental illness, and mild cognitive impairment (MCI) (Storzbach et al., Citation2017). It emphasizes a biopsychosocial understanding of causative and maintaining factors that contribute to a person’s symptoms and level of functioning. CCT aims at providing psychoeducation and teaching strategies to compensate for the functional consequences of post-concussive symptoms. The compensatory cognitive strategies target prospective memory, attention and concentration, learning and memory, problem-solving and cognitive flexibility, while the psychoeducation is focused on the natural course of mild and moderate TBI and post-concussive symptoms. Stress reduction techniques are also an integral part of the intervention, acknowledging that stress may enhance symptom levels. Additionally, the participants receive information about additional services they may find helpful, such as individual/group/family therapy, pain clinics, physiotherapy, and other vocational services. The participants are assigned home exercises after each session for them to practice the strategies and increase the chance of automating and generalizing the skills. Table provides an overview of the content in each of the 10 sessions.
Table 1. Overview of the topics provided the CCT intervention
The CCT intervention manual was translated and adapted to the Norwegian setting by researchers at the Department of Physical Medicine and Rehabilitation, OUH, and Sunnaas Rehabilitation Hospital, in collaboration with the author of the original manual (Professor Twamley) and a representative from the Norwegian user organization, Personskadeforbundet LTN. The main translator (author EIH) is bilingual (Norwegian/English). Supplementary material, including an information leaflet containing information about TBI and post-concussive symptoms, and audio files containing stress-reduction and relaxation techniques, were also translated to Norwegian. When adapting the manual and information leaflet to the Norwegian setting, extensive information about post-traumatic stress disorder (PTSD) and injury mechanisms specifically relating to combat settings, was removed, as the target population in the current study was civilian. Furthermore, some minor changes, including language adjustments, were made in agreement with Professor Twamley. The CCT intervention was delivered at an outpatient clinic at OUH by two clinical psychologists (authors EIH & KPSL), who were responsible for one group each. Prior to starting the intervention, the psychologists received training from experienced senior researchers and discussed practical aspects of delivering the intervention with Professor Twamley.
2.3. Assessment methods
2.3.1. Primary outcome—work participation
Work-related outcome was documented. Questions regarding work participation (percentage sick leave, time until return to part-time or full-time work), work productivity (hours worked, reduced work productivity compared to before the injury, need for increased supervision, alterations in work tasks) and work stability (changes in sick leave percentage) were administered to the participants in an interview format. Sick leave percentage and hours worked at baseline and post-treatment follow-up are reported.
2.3.2. Cognitive function
An IQ estimate was made at baseline based on four subtests (Vocabulary, Similarities, Block Design, and Matrix Reasoning) of the Wechsler Adult Intelligence Scale-Fourth Edition (WAIS-IV) (Wechsler, Citation2008). Additionally, cognitive function in the domains of learning and memory (California Verbal Learning Test-Second Edition, CVLT-II) (Delis, Kramer, & Kaplan et al., Citation2000), prospective memory (Memory for Intentions Screening Test, MIST) (Raskin, Citation2004), and processing speed and executive function (Color Word Interference Test (CWIT) and Trail Making Test (TMT) from the Delis–Kaplan Executive Function System (D-KEFS) (Delis, Kaplan, & Kramer, Citation2001); Coding from WAIS-IV (Wechsler, Citation2008); Ruff 2 and 7 Selective Attention Test (Ruff, Niemann, Allen, Farrow, & Wylie, Citation1992) was assessed.
2.3.3. Emotional symptoms and fatigue
Presence of depressive symptoms was assessed with the Patient Health Questionnaire-9 items (PHQ-9) (Kroenke, Spitzer, & Williams, Citation2001). The PHQ-9 has a score range from 0 to 27, with scores of 5, 10, 15, and 20 representing cut-off values for mild, moderate, moderately severe and severe symptoms of depression, respectively. Symptoms of anxiety were assessed with the Generalized Anxiety Disorder-7 items (GAD-7) (Spitzer, Kroenke, Williams, & Löwe, Citation2006). The GAD-7 has a score range from 0 to 21, with scores of 5, 10, and 15 representing cut-off values for mild, moderate, and severe symptoms. Fatigue was assessed with the Fatigue Severity Scale (FSS) (Krupp, LaRocca, Muir-Nash, & Steinberg, Citation1989). The FSS consists of nine items with a mean score ranging from 0 to 7 (0–3.9 = no fatigue, 4–4.9 = moderate fatigue, 5–7 = severe fatigue) (Lerdal et al., Citation2011).
2.3.4. Post-concussive symptoms
The Rivermead Post Concussion Symptoms Questionnaire (RPQ) (King, Crawford, Wenden, Moss, & Wade, Citation1995) is a self-report checklist consisting of 16 items to evaluate the presence and severity of PCS symptoms. The 16 items are divided into three symptom categories: somatic (headache, dizziness, nausea, noise sensitivity, sleep disturbance, fatigue, blurred vision, light sensitivity), emotional (irritability, depression, frustration, restlessness), and cognitive (poor memory, poor concentration, taking longer to think). Individuals are asked to rate to what degree they have experienced the 16 symptoms over the past 7 days on a 5-point Likert scale ranging from 0 to 4 (0 = not experienced at all, 4 = a severe problem). As advised by King et al. (1995), all scores of 1 (indicating that the problem was the same as before the injury) were removed. The RPQ has been validated in a Norwegian context (Ingebrigtsen, Waterloo, Marup-Jensen, Attner, & Romner, Citation1998).
2.3.5. CCT feedback form
The CCT feedback form was specifically designed to assess participants’ satisfaction with the CCT intervention. Participants were asked to rate the usefulness of the information provided about TBI and post-concussive symptoms, specific strategies for dealing with headaches, fatigue, and sleep problems, and strategies to compensate for cognitive symptoms relating to prospective memory, attention and concentration, learning and memory, problem-solving and cognitive flexibility. The feedback form also included questions about what topic or strategy was most useful, what strategies the participants were using regularly now that they were not using before, if the strategies had helped them in their daily life, and what topic or strategy was least helpful. Questions about additional topics that should be included in the intervention or suggestions to improve the program were also welcomed. Finally, the participants were asked if they would recommend the CCT-intervention to others with similar problems.
2.3.6. The Therapist Checklist
The Therapist Checklist was used to assess participants’ engagement in the intervention. It was originally developed to track participants´ attendance and session-by-session progress in a day treatment program described by Cantor et al. (Citation2014). It is a modified five-item scale where participants are rated according to the level of participation (active/passive), homework completion, interaction with therapist and other participants, and ability to learn and apply skills and strategies. Additionally, the therapists who provided the CCT-intervention kept a log where impressions from each session were documented along with the participants´ attendance levels.
2.4. Assessment timeline
After consenting to participate, socio-demographic, injury- and work-related information was collected. Additionally, the participants underwent a baseline assessment of neurocognitive function and self-reported symptoms. The baseline assessment took approximately 3.5 h to complete and was done on the same day for all participants. Following completion of the CCT intervention (approximately 3 months following inclusion), the participants underwent a post-treatment assessment of self-reported symptoms and vocational outcome. Additionally, the participants rated their satisfaction with the intervention on the CCT feedback form and the therapists who delivered the intervention rated the participants on the Therapist Checklist.
2.5. Statistical methods
Data analyses were completed with IBM SPSS, version 22. Descriptive statistics were used to characterize the sample at baseline. Due to the very small sample size, non-parametric statistical methods with median (interquartile range, IQR) is reported for socio-demographic variables and self-reported symptoms. A Wilcoxon Signed Rank Test was applied to assess changes in post-concussive symptoms from baseline to post-treatment follow-up. For neuropsychological test results at baseline, the participants´ performance are characterized as deviance from the normative mean (in SD).
2.6. Success criteria
To assess whether the proposed procedures were satisfactory, we pre-defined success criteria based on a previous pilot study by Twamley et al. (Citation2014) and studies that have been performed at the Department of Physical Medicine and Rehabilitation at OUH (Hellstrom et al., Citation2016): three quarters of the patients who were asked to participate would agree, less than 30% dropout, the participants would tolerate the burden of the follow-up procedures, 90% attendance at CCT sessions, and subjective satisfaction with the CCT-intervention would be comparable to that reported in the pilot study by Twamley et al. (Citation2014).
3. Results
3.1. Recruitment
The feasibility study was carried out in the spring of 2017. During March and April, a total of 14 individuals were screened according to the eligibility criteria. Five individuals did not meet the criteria due to place of residence, receiving work assessment allowance, or having recovered. The remaining nine patients were asked to participate, whereof eight agreed (89%), and one declined. One patient (12%) dropped out prior to starting the intervention preferring another treatment option, and one (12%) dropped out after two sessions due to having a low symptom burden. This left a total of six participants (75%) being enrolled in the feasibility study. Figure shows a flow chart of the inclusion procedure.
3.2. Baseline socio-demographic and injury characteristics
The participants were enrolled on average 4 months (range 3–5 months) after the injury. Baseline socio-demographic and injury characteristics are presented in Table .
Table 2. Baseline socio-demographic and injury characteristics
3.3. Work participation
All participants were employed in full-time positions at the time of injury, with a number of years in the current job ranging from 0 to 16 years, with a median (IQR) of 2 (7). At the time of inclusion, they were all sick-listed above 50% (range 70–100%). Immediately following the CCT intervention, three participants had decreased their percentage of sick leave, while one participant had increased their level. Table shows the percentage of sick leave and hours worked for each of the participants at baseline and at the post-treatment follow-up.
Table 3. Sick leave percentage and hours worked at baseline and post CCT-treatment follow-up
3.4. Cognitive function
A baseline estimation of premorbid cognitive function (four subscales from the General Ability Index, WAIS-IV) revealed that all patients were within normal range (IQ estimates range 96–129). With very few exceptions, measures of neurocognitive functioning (CVLT-II, Coding, Ruff 2 and 7, CWIT, TMT, MIST) were within normal range (± 1 SD from the mean).
3.5. Emotional symptoms and fatigue
Baseline assessment of self-reported depressive symptoms (PHQ-9) revealed a median (IQR) score of 11.5 (6). Two participants reported no significant or minimal symptoms, two reported mild symptoms, while one reported moderate symptoms. A measure of self-reported symptoms of anxiety (GAD-7) showed a median (IQR) score of 7 (7). Two participants reported no or minimal symptoms, two reported mild symptoms, while one reported moderate symptoms. Moreover, the patients reported moderate to severe levels of fatigue (FSS) with a median (IQR) score of 5 (2). Three participants reported moderate symptoms and three reported severe fatigue.
3.6. Post-concussive symptoms
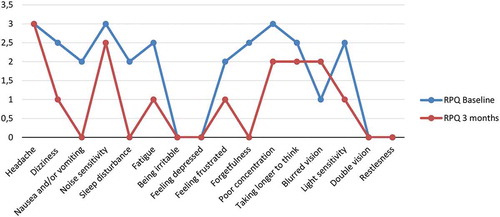
All participants reported post-concussive symptoms that represented more of a problem than before the injury at baseline. The symptoms that were most frequently reported as a moderate or severe problem (reported by three or more participants) were headache, dizziness, noise sensitivity, fatigue, forgetfulness, poor concentration, taking longer to think, and light sensitivity.
A Wilcoxon Signed Rank Test revealed a statistically significant decline in RPQ-scores from baseline to the post-treatment control, z = −2.201, p = < 0.05, with a large effect size (r = 0.63). The median score on the RPQ decreased from baseline (Md = 31) to the follow-up after completing the CCT-intervention (Md = 17). Comparing the total RPQ scores for each of the individual participants revealed that all had a reduction of symptoms from baseline to the post-treatment follow-up. Figure shows the median scores for each of the 16 symptoms at baseline and at the post-treatment follow-up.
3.7. Treatment satisfaction
Table shows the number of participants who rated each of the items on the CCT feedback form on a scale ranging from 1 to 5 (not helpful to extremely helpful), while the column to the right indicates the overall score. The items that received the highest mean ratings were information about TBI and post-concussive symptoms, information about fatigue, prospective memory, and memory and learning. Information about additional services received the lowest mean rating. With exception of information about additional services, all items received a rating above 3.5 (i.e. towards very helpful). Five participants indicated that they would recommend the intervention to others with similar problems. Some of the qualitative comments to the question “what strategies are you using regularly now that you weren’t using before” included:
“Breaks, relaxation, breathing exercises.”
“Mindfulness, breaks, eliminating distractions, new ways of learning.”
“Has made me think about my life and take the breaks that I need.”
“Categorizing tasks and prioritizing. Acronyms.”
Table 4. Participants rating of satisfaction with the intervention (CCT feedback form)
The participants were also asked what topic or strategy they found least helpful, and some of their comments included:
“Calendar use. I already knew this.”
“Relaxation, done a lot of this before, well known to me.”
“Problem solving and cognitive flexibility plus a bit too much focus on calendar use and organization. I do a lot of this already.”
“Planning, organization, life style strategies are very relevant, I already do this, but very relevant for those who do not!”
3.8. Treatment engagement
Overall attendance across the 10 sessions of the CCT-intervention was 97%. With exception of one participant who missed two sessions due to personal reasons, all participants attended all 10 sessions. The therapists´ rating of the participants on the Therapist Checklist showed that all the participants participated fully or moderately. Four participants completed the homework to a satisfactory degree, while two did not. Five participants interacted well with the other participants and the therapists, while one participant was rated to interact negatively. Four participants acquired the strategies and skills that were taught to a good degree, while two participants were rated as modest and minimally competent. Five participants attempted to apply the skills and strategies to real-life situations, and one participant made minimal or no use of the strategies. Table shows the number of participants who were rated on the five items of the Therapist Checklist.
Table 5. Number of participants rated on each item of the Therapist Checklist
4. Discussion
The purpose of this study was to assess the feasibility of recruitment procedures and delivery of an adaptation of a cognitive intervention to the Norwegian context and to a civilian sample. The cognitive intervention comprises psychoeducation and compensatory cognitive strategies, in addition to stress reduction techniques. The feasibility study was performed in preparation for a full-scale RCT that will assess the efficacy of a combined cognitive and vocational intervention on vocational and other outcomes in individuals with mild-to-moderate TBI. The study allowed us to gain information about potential issues that will need to be addressed when performing the clinical trial.
4.1. Feasibility of recruitment procedures
Eighty-nine per cent of the individuals who were asked to participate in the study consented, which is well above the pre-defined success criterion of 75%. Two (25%) of the eight patients who initially consented dropped out. This is also below the success criterion of 30%, and below the number of drop-outs reported in Twamley’s pilot study, where nine (36%) of the 25 individuals who initially consented and were randomized to receive CogSMART, dropped out (Twamley et al., Citation2014). Even though the baseline assessment was time consuming, and it was necessary to incorporate several breaks due to fatigue and other symptoms, all participants completed the assessment in one session. The load of follow-up assessments was therefore deemed acceptable.
4.2. Feasibility of the CCT intervention
When adapting the CCT manual to the Norwegian setting, a representative from the collaborating user organization (Personskadeforbundet LTN) forwarded the manual and additional material to additional members of the organization. The feedback from the user organization was overwhelmingly positive and gave important insights on the appropriateness of the translation and content. While the overall content of the CCT manual remained the same, important changes were made to increase the cultural relevance of the treatment to the Norwegian civilian population. For example, as the original manual contained information on injury mechanisms relating to combat settings and extensive information about post-traumatic stress disorder, adjustments to the content was made with contextual differences in mind. Tailoring interventions to fit the target population is important to increase treatment engagement and effectiveness (Ramos & Alegria, Citation2014).
The findings of the study demonstrated the feasibility of the CCT intervention. Moreover, the results indicate that the adaptations of the manual were appropriate for a civilian sample in the Norwegian context. All six participants completed the intervention, and the percentage of CCT sessions attended was above 97%. This is comparable to Twamley et al. (Citation2014) pilot study where approximately 94% of the participants receiving both CogSMART and SE attended all sessions. With the exception of information about additional services, all items on the CCT feedback form received a mean rating of 3.5 or more, indicating that the participants found the information and strategies useful. In Twamley’s pilot, all items received a mean score of 3.5 or more, and the item receiving the highest rating was memory strategies with a mean score of 4 (i.e. very useful). In this feasibility study, information about post-concussive symptoms and TBI, strategies to deal with fatigue, prospective memory, and memory and learning were all rated as very useful. The qualitative feedback further indicated that the participants found the psychoeducation and relaxation techniques helpful. However, the feedback also indicated that they did not find the strategies relating to organization and calendar use as helpful. This may reflect methodological differences in that our participants, in contrast to those in Twamley and colleagues´ study, were employed at the time of injury, and already had a system for organizing their daily routines.
Most participants interacted well with the therapists and the other group members and participated in group discussions and assignments to a satisfactory degree. Moreover, five of the six participants tried to apply the skills they had learned to real-life situations. However, two participants did not complete the assigned homework. Reported rates of compliance with homework assignments in clinical trials range from 49% to 94% (Kazantzis, Deane, & Ronan, Citation2004), and the 67% homework completion rate in this study is in accordance with this. Even though one participant had a legitimate reason, failing to complete homework may limit the ability to generalize from the intervention. Thus, motivating the participants to complete home assignments and underlining the importance of practice to automate skills should be addressed to a greater degree in the further RCT.
At the end of the 10 CCT sessions, there were positive reductions of self-reported post-concussive symptoms in the following areas: dizziness, nausea and/or vomiting, noise sensitivity, sleep disturbance, fatigue, feeling frustrated, forgetfulness, concentration, taking longer to think, and light sensitivity. The only symptoms showing no decrease were headache and blurred vision. This is in line with previous studies that have reported positive effects of cognitive interventions on self-reported symptoms (Storzbach et al., Citation2017; Twamley et al., Citation2014, Citation2015; Vikane et al., Citation2017). Moreover, the observed changes corresponded with the strategies and information that received the highest mean ratings on the CCT Feedback Form. Regarding symptoms of irritability and depression, double vision and restlessness, the participants had a median score of 0 at both baseline and post-treatment follow-up. Severity of symptoms of headache remained unchanged between the two time points, with a median score of 3. The only symptom which increased in severity, was blurred vision, with a median severity score of 1 at baseline and 2 at the post-treatment control. These symptoms were probably not in focus at baseline as they were subtle and may have been masked by the other post-concussion symptoms. Thus, as the other symptoms decrease in severity, the participants may become more aware of blurred vision. Furthermore, the CCT intervention does not provide vision therapy, and there is not free access to an optometrist for visual evaluations.
There were trends towards reductions of sick leave percentage and increased hours worked for half of the participants. Two participants demonstrated the same level of sick leave and hours worked at baseline and post-intervention follow-up, while one participant had increased their sick leave percentage. The participant who showed a worsening resigned from their job during the study period and would therefore not be expected to show improvement on these measures. The participants received the intervention shortly after their injury (3–5 months). No previous studies have assessed the effect of cognitive interventions on vocational outcome this shortly after TBI, and the results are therefore difficult to compare to the existing literature.
4.3. Limitations
It is important to note that the findings should be interpreted with caution due to the lack of a control group and the relatively small sample size. However, the purpose of this study was not first and foremost to determine the effect of the intervention, but to assess the feasibility of it. Stallard (Citation2012) has recommended that the sample size in pilot studies should be approximately 0.03 times the intended sample size for the definitive clinical trial. The calculated sample size for this RCT is 120 participants, with 60 in each group (Howe et al., Citation2017). Thus, six participants constitute 10% of the total number of participants that will receive the intervention and is well above the recommended sample size.
All the participants that were included had sustained mild TBIs. The RCT will include participants with both mild and moderate TBI histories, and more severe injury could potentially bring about issues that have not been addressed in this feasibility study. It may be necessary to increase the assessment time at baseline in the RCT, or even to perform the assessment over two days due to reduced capacity and fatigue. During the recruitment period for the feasibility study, no patients with moderate TBI were eligible for inclusion, and we chose to move forward due to time constraints. However, the CogSMART intervention has previously been administered to participants with moderate TBI in the US and found to be feasible (Twamley et al., Citation2014).
4.4. Conclusion
The findings from this study indicate that the participants found most of the information and strategies provided in the CCT intervention helpful. The attendance rate was high, and the participants were able to interact well with the therapists and other group members, and participate in group discussions, acquire skills and apply the skills to a satisfactory degree. Most of the individuals who were asked to participate agreed, and the participants tolerated the follow-up procedures. In sum, the results demonstrate that the delivery of a Norwegian adaptation of the CCT intervention to a civilian sample with TBI is feasible. We also found that the recruitment and follow-up procedures were feasible. As a result, no major protocol adjustments were made. However, the knowledge gained provided important information on acceptability and treatment engagement. It also gave insight into relevant practical aspects that will be taken into consideration before initiating the RCT.
Competing interests
The authors declare no competing interests.
Acknowledgements
We would like to thank all the participants. We would also like to thank the representative from the user organization (Personskadeforbundet, LTN), Birthe Sand Rismyhr.
Additional information
Funding
Notes on contributors
Emilie Isager Howe
This article was written by a multinational, multidisciplinary group of researchers with wide-ranging research interests and expertise in quantitative and qualitative research methodology. The main research interest of the group is to contribute to development of knowledge in the trauma population across recovery phases and sectors involved in patient care and social support. All authors are associated with a larger scale project aiming to evaluate the efficacy of a combined cognitive and vocational intervention on vocational and functional outcomes following traumatic brain injury.
References
- American Congress of Rehabilitation Medicine. (1993). Definition of mild traumatic brain injury. Journal of Head Trauma Rehabilitation, 8(3), 86–16. doi:10.1097/00001199-199309000-00010
- Cancelliere, C., Kristman, V. L., Cassidy, J. D., Hincapié, C. A., Côté, P., Boyle, E., … Borg, J. (2014, March). Systematic review of return to work after mild traumatic brain injury: Results of the international collaboration on mild traumatic brain injury prognosis. Archives of Physical Medicine and Rehabilitation, 95(3 Suppl.), S201–S209. PubMed PMID: 24581906. doi:10.1016/j.apmr.2013.10.010
- Cantor, J., Ashman, T., Dams-O’Connor, K., Dijkers, M. P., Gordon, W., Spielman, L., … Oswald, J. (2014, January). Evaluation of the short-term executive plus intervention for executive dysfunction after traumatic brain injury: A randomized controlled trial with minimization. Archives of Physical Medicine and Rehabilitation, 95(1), 1–9 e3. PubMed PMID: 23988395. doi:10.1016/j.apmr.2013.08.005
- Chu, S. Y., Tsai, Y. H., Xiao, S. H., Huang, S.-J., & Yang, -C.-C. (2017). Quality of return to work in patients with mild traumatic brain injury: A prospective investigation of associations among post-concussion symptoms, neuropsychological functions, working status and stability. Brain Injury, 31(12), 1674–1682. PubMed PMID: 28872344. doi:10.1080/02699052.2017.1332783
- Cicerone, K. D., Mott, T., Azulay, J., Sharlow-Galella, M. A., Ellmo, W. J., Paradise, S., & Friel, J. C. (2008, December). A randomized controlled trial of holistic neuropsychologic rehabilitation after traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 89(12), 2239–2249. PubMed PMID: 19061735. doi:10.1016/j.apmr.2008.06.017
- Corrigan, J. D., Selassie, A. W., & Orman, J. A. (2010, March-April). The epidemiology of traumatic brain injury. The Journal of Head Trauma Rehabilitation, 25(2), 72–80. PubMed PMID: 20234226. doi:10.1097/HTR.0b013e3181ccc8b4
- Craig, P., Dieppe, P., Macintyre, S., Michie, S., Nazareth, I., & Petticrew, M. (2008, September 29). Developing and evaluating complex interventions: The new medical research council guidance. BMJ, 337, a1655. PubMed PMID: 18824488; PubMed Central PMCID: PMCPMC2769032. doi:10.1136/bmj.a1655
- Delis, D. C., Kaplan, E., & Kramer, J. H. (2001). Delis Kaplan executive function system: Examiners manual. San Antonio, TX: The Psychological Corporation.
- Delis, D. C., Kramer, J. H., Kaplan, E., & Ober, B. A. (2000). California verbal learning test (2nd ed.). Adult Version. Manual. The Psychological Corporation.
- Fadyl, J. K., & McPherson, K. M. (2009, May-June). Approaches to vocational rehabilitation after traumatic brain injury: A review of the evidence. The Journal of Head Trauma Rehabilitation, 24(3), 195–212. PubMed PMID: 19461367. doi:10.1097/HTR.0b013e3181a0d458
- Graham, C. W., West, M. D., Bourdon, J. L., Inge, K. J., Seward, H. E., & Graham, C. W. (2016). Employment interventions for return to work in working age adults following traumatic brain injury (TBI): A systematic review. Campbell Systematic Reviews, 6. doi:10.4073/csr.2016.6
- Hellstrom, T., Westlye, L. T., Server, A., Løvstad, M., Brunborg, C., Lund, M. J., … Andelic, N. (2016). Volumetric and morphometric MRI findings in patients with mild traumatic brain injury. Brain Injury, 30(13–14), 1683–1691. PubMed PMID: 27996331. doi:10.1080/02699052.2016.1199905
- Howe, E. I., Langlo, K. S., Terjesen, H. C. A., Røe, C., Schanke, A.-K., Søberg, H. L., … Andelic, N. (2017, October 17). Combined cognitive and vocational interventions after mild to moderate traumatic brain injury: Study protocol for a randomized controlled trial. Trials, 18(1), 483. PubMed PMID: 29041954; PubMed Central PMCID: PMCPMC5645893. doi:10.1186/s13063-017-2218-7
- Ingebrigtsen, T., Waterloo, K., Marup-Jensen, S., Attner, E., & Romner, B. (1998, September). Quantification of post-concussion symptoms 3 months after minor head injury in 100 consecutive patients. Journal of Neurology, 245(9), 609–612. PubMed PMID: 9758300.
- Kazantzis, N., Deane, F. P., & Ronan, K. R. (2004, June). Assessing compliance with homework assignments: Review and recommendations for clinical practice. Journal of Clinical Psychology, 60(6), 627–641. PubMed PMID: 15141396. doi:10.1002/jclp.10239
- King, N. S., Crawford, S., Wenden, F. J., Moss, N. E., & Wade, D. T. (1995, September). The rivermead post concussion symptoms questionnaire: A measure of symptoms commonly experienced after head injury and its reliability. Journal of Neurology, 242(9), 587–592. PubMed PMID: 8551320.
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001, September). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. PubMed PMID: 11556941; PubMed Central PMCID: PMCPMC1495268.
- Krupp, L. B., LaRocca, N. G., Muir-Nash, J., & Steinberg, A. D. (1989, October). The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Archives of Neurology, 46(10), 1121–1123. PubMed PMID: 2803071.
- Kumar, K. S., Samuelkamaleshkumar, S., Viswanathan, A., & Macaden, A. S. (2017, June 20). Cognitive rehabilitation for adults with traumatic brain injury to improve occupational outcomes. Cochrane Database of Systematic Reviews (Online), 6, CD007935. PubMed PMID: 28631816. doi:10.1002/14651858.CD007935.pub2
- Lerdal, A., Bakken, L. N., Rasmussen, E. F., Beiermann, C., Ryen, S., Pynten, S., … Kim, H. S. (2011). Physical impairment, depressive symptoms and pre-stroke fatigue are related to fatigue in the acute phase after stroke. Disability and Rehabilitation, 33(4), 334–342. PubMed PMID: 20521900. doi:10.3109/09638288.2010.490867
- Levin, H. S., & Diaz-Arrastia, R. R. (2015, May). Diagnosis, prognosis, and clinical management of mild traumatic brain injury. Lancet Neurology, 14(5), 506–517. PubMed PMID: 25801547. doi:10.1016/S1474-4422(15)00002-2
- Maas, A. I. R., Menon, D. K., Adelson, P. D., Andelic, N., Bell, M. J., Belli, A., … Yaffe, K. (2017, December). Traumatic brain injury: Integrated approaches to improve prevention, clinical care, and research. Lancet Neurology, 16(12), 987–1048. PubMed PMID: 29122524. doi:10.1016/S1474-4422(17)30371-X
- Man, D. W., Poon, W. S., & Lam, C. (2013). The effectiveness of artificial intelligent 3-D virtual reality vocational problem-solving training in enhancing employment opportunities for people with traumatic brain injury. Brain Injury, 27(9), 1016–1025. PubMed PMID: 23662639. doi:10.3109/02699052.2013.794969
- Management of Concussion/mTBI Working Group. (2009). VA/DoD clinical practice guideline for management of concussion/mild traumatic brain injury. Journal of Rehabilitation Research and Development, 46(6), Cp1–68. PubMed PMID: 20108447; eng.
- Menon, D. K., Schwab, K., Wright, D. W., & Maas, A. I. (2010, November). Position statement: Definition of traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 91(11), 1637–1640. PubMed PMID: 21044706. doi:10.1016/j.apmr.2010.05.017
- Ponsford, J. L., & Spitz, G. (2015, May-June). Stability of employment over the first 3 years following traumatic brain injury. The Journal of Head Trauma Rehabilitation, 30(3), E1–E11. PubMed PMID: 24816157. doi:10.1097/HTR.0000000000000033
- Ramos, Z., & Alegria, M. (2014, April). Cultural adaptation and health literacy refinement of a brief depression intervention for latinos in a low-resource setting. Cultural Diversity & Ethnic Minority Psychology, 20(2), 293–301. PubMed PMID: 24588455. doi:10.1037/a0035021
- Raskin, S. (2004). Memory for intentions screening test (abstract). Journal of the International Neuropsychological Society : 2004;10(Suppl 1):110.
- Roozenbeek, B., Maas, A. I., & Menon, D. K. (2013, April). Changing patterns in the epidemiology of traumatic brain injury. Nature Reviews Neurology, 9(4), 231–236. PubMed PMID: 23443846. doi:10.1038/nrneurol.2013.22
- Ruff, R. M., Niemann, H., Allen, C. C., Farrow, C. E., & Wylie, T. (1992, December). The Ruff 2 and 7 selective attention test: A neuropsychological application. Perceptual and Motor Skills, 75(3 Pt 2), 1311–1319. PubMed PMID: 1484803. doi:10.2466/pms.1992.75.3f.1311
- Salazar, A. M., Warden, D. L., Schwab, K., Spector, J., Braverman, S., Walter, J., … Ellenbogen, R. G. (2000, June 21). Cognitive rehabilitation for traumatic brain injury: A randomized trial. Defense and Veterans Head Injury Program (DVHIP) study group. JAMA, 283(23), 3075–3081. PubMed PMID: 10865301.
- Saltychev, M., Eskola, M., Tenovuo, O., & Laimi, K. (2013). Return to work after traumatic brain injury: Systematic review. Brain Injury, 27(13–14), 1516–1527. PubMed PMID: 24131314. doi:10.3109/02699052.2013.831131
- Shames, J., Treger, I., Ring, H., & Giaquinto, S. (2007, September 15). Return to work following traumatic brain injury: Trends and challenges. Disability and Rehabilitation, 29(17), 1387–1395. PubMed PMID: 17729084. doi:10.1080/09638280701315011
- Sigurdardottir, S., Andelic, N., Roe, C., Jerstad, T., & Schanke, A.-K. (2009, June). Post-concussion symptoms after traumatic brain injury at 3 and 12 months post-injury: A prospective study. Brain Injury, 23(6), 489–497. PubMed PMID: 19484622. doi:10.1080/02699050902926309
- Silverberg, N. D., Panenka, W. J., & Iverson, G. L. (2018, February). Work productivity loss after mild traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 99(2), 250–256. PubMed PMID: 28760573. doi:10.1016/j.apmr.2017.07.006
- Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006, May 22). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. PubMed PMID: 16717171. doi:10.1001/archinte.166.10.1092
- Stallard, N. (2012, May 20). Optimal sample sizes for phase II clinical trials and pilot studies. Statistics in Medicine, 31(11–12), 1031–1042. PubMed PMID: 22052407. doi:10.1002/sim.4357
- Storzbach, D., Twamley, E. W., Roost, M. S., Golshan, S., Williams, R. M., OʼNeil, M., … Huckans, M. (2017, January/Feburary). Compensatory cognitive training for operation enduring freedom/operation iraqi freedom/operation new dawn veterans with mild traumatic brain injury. The Journal of Head Trauma Rehabilitation, 32(1), 16–24. PubMed PMID: 27022961. doi:10.1097/HTR.0000000000000228
- Theadom, A., Barker-Collo, S., Jones, K., Kahan, M., Te Ao, B., McPherson, K., … Feigin, V. (2017, August). Work limitations 4 years after mild traumatic brain injury: A cohort study. Archives of Physical Medicine and Rehabilitation, 98(8), 1560–1566. PubMed PMID: 28188778. doi:10.1016/j.apmr.2017.01.010
- Twamley, E. W., Jak, A. J., Delis, D. C., Bondi, M. W., & Lohr, J. B. (2014). Cognitive Symptom Management and Rehabilitation Therapy (CogSMART) for veterans with traumatic brain injury: Pilot randomized controlled trial. Journal of Rehabilitation Research and Development, 51(1), 59–70. PubMed PMID: 24805894. doi:10.1682/JRRD.2013.01.0020
- Twamley, E. W., Thomas, K. R., Gregory, A. M., Jak, A. J., Bondi, M. W., Delis, D. C., & Lohr, J. B. (2015, November-December). CogSMART compensatory cognitive training for traumatic brain injury: Effects over 1 year. The Journal of Head Trauma Rehabilitation, 30(6), 391–401. PubMed PMID: 25033034. doi:10.1097/HTR.0000000000000076
- Twamley, E. W., Vella, L., Burton, C. Z., Heaton, R. K., & Jeste, D. V. (2012, September). Compensatory cognitive training for psychosis: Effects in a randomized controlled trial. The Journal of Clinical Psychiatry, 73(9), 1212–1219. PubMed PMID: 22939029; PubMed Central PMCID: PMCPMC3593661. doi:10.4088/JCP.12m07686
- Vanderploeg, R. D., Schwab, K., Walker, W. C., Fraser, J. A., Sigford, B. J., Date, E. S., … Warden, D. L. (2008, December). Rehabilitation of traumatic brain injury in active duty military personnel and veterans: Defense and Veterans Brain Injury Center randomized controlled trial of two rehabilitation approaches. Archives of Physical Medicine and Rehabilitation, 89(12), 2227–2238. PubMed PMID: 19061734. doi:10.1016/j.apmr.2008.06.015
- Vikane, E., Hellstrom, T., Roe, C., Bautz-Holter, E., Aßmus, J., & Skouen, J. S. (2017). Multidisciplinary outpatient treatment in patients with mild traumatic brain injury: A randomised controlled intervention study. Brain Injury, 31(4), 475–484. PubMed PMID: 28296510. doi:10.1080/02699052.2017.1280852
- Wechsler, D. (2008). Wechsler adult intelligence scale (4th ed.). San Antionio, TX: Pearson.
- Yasuda, S., Wehman, P., Targett, P., Cifu, D., & West, M. (2001, November). Return to work for persons with traumatic brain injury. American Journal of Physical Medicine & Rehabilitation / Association of Academic Physiatrists, 80(11), 852–864. PubMed PMID: 11805460.