Abstract
Hypertension is worldwide and the most common problem in clinical practice in the United States. It is typically treated with medications, but it also responds to various lifestyle principles. This study assessed the effectiveness of reversing hypertension using a multi-lifestyle medical residential intervention. We evaluated retrospective data from the pretest-posttest intervention of the 114 subjects that were hypertensive from among all 173 enrolled in NEWSTART during 2014. Of the 114 individuals with hypertension, there were 37% males and 63% females. Baseline values (Mean±SD) were: 66.5 ± 10.6 years, 31.9 ± 6.6 kg/m2, and 139 ± 20 mmHg. Systolic blood pressure decreased significantly (p < 0.001) within 14 days in all population sub-groups from −8% (diabetic) to −31% (normal weight). Forty percent of subjects achieved <120 mmHg. Medications were discontinued or decreased by 93% of the subjects. This lifestyle intervention is appropriate for first-line treatment of hypertension.
PUBLIC INTEREST STATEMENT
High blood pressure affects people worldwide and is the main cause of doctor’s visits in the U.S. It can be treated with drugs but also with lifestyle. We tested NEWSTART, an 18-day composite lifestyle of Nutrition, Exercise, Water, Sunlight, Temperance, fresh Air, Rest, Trust in divine power, for reversing high blood pressure in those who had come to the program throughout 2014. Systolic blood pressure dropped an average of 19 points in two weeks. It dropped in men and women, and in those with diabetes, high cholesterol or triglycerides, or overweight. Moreover, the use of high blood pressure drugs was decreased or discontinued in 93% of individuals. Continued use of NEWSTART lifestyle should continue its benefits since these are health principles in the Adventist Lifestyle that prevents high blood pressure. This is compelling evidence for use of the NEWSTART lifestyle for reversing high blood pressure.
1. Introduction
Hypertension is recognized as a worldwide problem. It is the most common clinical condition in primary care in the United States and it is associated with increased mortality from cardiovascular disease (James et al., Citation2014). The common form of hypertension among the older population 50 years and older are isolated elevated systolic blood pressure (SBP), an important predictor of coronary heart disease (Basile, Citation2002; Franklin, Khan, Wong, Larson, & Levy, Citation1999). Hypertension is typically treated with medications. The SPRINT report shows that elevated SBP was decreased among non-diabetic patients to 120 mmHg by intensive treatment with medications (Wright et al., Citation2015). It was also shown that a lower blood pressure decreases mortality from cardiovascular disease and this multicenter study set a new lower standard for normal blood pressure. The decreases in SBP, however, were accompanied by serious side effects (Schiffrin, Calhoun, & Flack, Citation2015; Wright et al., Citation2015). These side effects can be avoided if the patient is responsive to a lifestyle intervention for the treatment of hypertension following lifestyle modification as recommended by the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines for patients with hypertension between ≥130 mmHg to <160 mmHg (James et al., Citation2014; Whelton, Carey, Aronow, Casey, & Jones, Citation2018).
Lifestyle interventions are effective because they address unhealthy habits or behaviors that are responsible for hypertension (James et al., Citation2014; Mozaffarian et al., Citation2016). Research on lifestyle interventions have focused on salt restriction, limited alcohol intake, use of fish oil supplements, weight loss, and increased exercise (Appel et al., Citation2003; Saneei, Salehi-Abargouei, Esmaillzadeh, & Azadbakht, Citation2014; Dickinson et al., Citation2006; Gay, Rao, Vaccarino, & Ali, Citation2016; He, Li & Macgregor, Citation2013; Jenkins et al., Citation2015). Vegetarian diets are also known to protect against hypertension (Yokoyama et al., Citation2014), and vegan diets seem to offer additional protection over vegetarian diets and other diet patterns (Le &Sabate, Citation2014). Vegan or near vegan diets are consistently associated with decreases in SBP with or without exercise (Goldhamer, Lisle, Parpia, Anderson, & Campbell, Citation2001; Goldhamer et al., Citation2002; McDougall, Litzau, Haver, Saunders, & Spiller, Citation1995; McDougall et al., Citation2014; Razavi et al., Citation2014; Silberman et al., Citation2010).
Interventions targeting multiple lifestyle modifications appear to be more effective in lowering SBP than those targeting a single or limited number of lifestyle changes (Appel et al., Citation2003; Frisoli, Schmieder, Grodzicki, & Messerli, Citation2011). There is work in progress to assess the effectiveness of interventions addressing multiple lifestyle modification for decreasing hypertension (Li et al., Citation2014). The purpose of this study was to test the effectiveness of NEWSTART, an intense short-term application of eight simultaneous lifestyle principles that are components of the Adventist Lifestyle, a lifestyle that is associated with low risk of hypertension (Pettersen, Anousheh, Fan, Jaceldo-Siegl, & Fraser, Citation2012).
2. Methods
2.1. Study design and population
This is a retrospective pretest-posttest study that by design has no controls. We examined the consecutive 114 subjects who had hypertension (66%) out of the total 173 individuals who attended the NEWSTART lifestyle health program during 2014 at Weimar Institute, Weimar, CA. Each subject was his or her own control for measurements at baseline and at 14 days after beginning lifestyle intervention. Hypertension was defined in this study by one or more of the following criteria: (1) medically diagnosed as hypertensive, or (2) a SBP of ≥130 mmHg (Whelton et al., Citation2018), which is the same as the SPRINT study (Wright et al., Citation2015), or (3) regular use of antihypertensive medications. Many subjects had one or more of the following comorbidities: diabetes (fasting blood glucose ≥6.99 mmol/L [≥125 mg/dL] and/or hemoglobin A1c ≥6.5% or taking medication for diabetes); overweight (BMI ≥25); dyslipidemia (total cholesterol ≥6.22 mmol/L [≥240 mg/dL] and/or HDL-cholesterol <1.04 mmol/L [<40 mg/dL] and/or triglycerides ≥1.69 mmol/L [≥150 mg/dL]). Individuals who were not hypertensive according to the criteria of this study or who had missing data were not included as subjects in this study.
2.2. The NEWSTART program
NEWSTART is an acronym for an 18-day intensive residential multiple lifestyle intervention and education program composed of eight lifestyle health principles that are components of the Adventist Lifestyle that is associated with lower blood pressure (Pettersen et al., Citation2012). These lifestyle principles are individually associated with lower blood pressure—Nutrition (Appel et al., Citation2006), Exercise (Skutnik, Smith, Johnson, Kurti, & Harms, Citation2016), Water (Thorton, Citation2010), Sunlight (Feelisch et al., Citation2010; Mead, Citation2008), Temperance such as abstinence from tobacco and alcohol (Hillbom, Saloheimo, & Juvela, Citation2011; Kannel & Higgins., Citation1990), fresh Air (Mao et al., Citation2012), Rest (Calhoun & Harding, Citation2010; Gangwisch et al., Citation2006), and Trust in God—spirituality (Charlemagne-Badal & Lee, Citation2016; Holt-Lunstad, Steffen, Sandberg, and Jensen (Citation2011); Koenig (Citation2015); Nedley and Ramirez (Citation2014); Tartaro, Luecken, & Gunn, Citation2005). Application of the NEWSTART principles may vary somewhat from place to place and from person to person, particularly with diet—vegan or lacto-ovo-vegetarian diet that includes milk and eggs (Crane & Sample, Citation1994; Slavíček et al., Citation2008). The NEWSTART program at Weimar Institute includes a vegan diet; daily walking in the fresh air and sunlight; drinking substantial quantities of water; regular and adequate daily sleep; avoiding intemperate habits such as smoking or drinking; and fostering trust in God. All the subjects daily follow all the same health principles. The vegan diet consists of legumes, whole grains, vegetables, fruits, nuts, seeds, olives, avocados, soymilk, almond milk, and whole-grain breads. The diet contains 26% of total energy as fat. Salt is used in preparing dishes; it provides 1193 mg sodium/1000 calories and 1380 mg potassium/1000 calories. A voluntary medically directed water-fast of three days precedes the whole-foods vegan diet.
2.3. Measurements
NEWSTART clients receive two major health assessments—at Day 1 (baseline) and at Day 14. Blood pressure was taken at 7:00 to 8:00 AM before breakfast from the forearm while sitting. Blood pressure was measured by a Welch Allyn: 420 Series Serial: 200,413,369 blood pressure meter. (A minimal unknown number of subjects had their blood pressure taken by an Omron model: BP786N Serial: 20,170,300,321 blood pressure meter). The mean systolic blood pressure difference between the 2 m was 1.8%. A chief desire among the incoming subjects was to discontinue their antihypertensive medications. Subjects of NEWSTART are under medical supervision during their stay at this residential medical lifestyle clinic and are given the option at the beginning of the program to decrease the use of antihypertensive medication. Client blood pressure was monitored one or more times daily to encourage compliance as blood pressure decreased. All clinical tests, however, were performed on all subjects at baseline and at 14 days and the blood pressure taken at these two times is what we report here. There are other measurements that are important for assessing cardiovascular health but this study is limited to the clinical measurements that are included in this lifestyle intervention program.
2.4. Statistical analyses
We assessed the pre and post-treatment differences in SBP with paired t-test and the mean differences between groups using ANOVA tests with SPSS statistical package version 23 (IBM Corporation, Citation2015). The Waterfall Plots were done with SPSS and Microsoft Excel, V.12. This research protocol was reviewed and approved by the Andrews University IRB.
3. Results
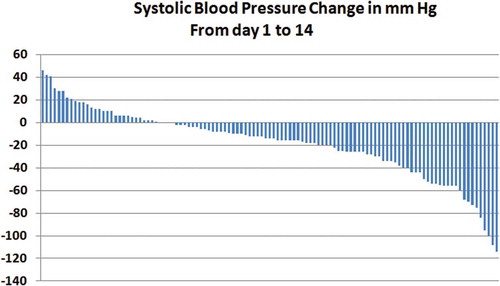
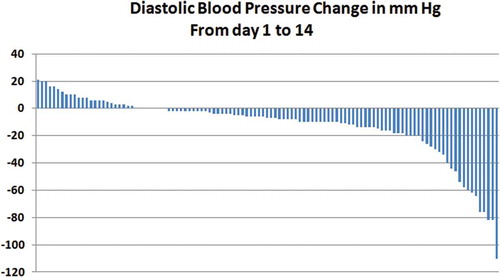
There were 42 men (37%) and 72 women (63%) with elevated SBP (Table ). The baseline characteristics of subjects with hypertension were (mean±SD): age, 66.5 ± 10.6; BMI, 31.9 ± 6.6 kg/m2; and SBP of 139 ± 20 mmHg. SBP decreased highly significantly (−14%, p < 0.001) within 14 days (Table ) and the decrease in diastolic blood pressure was also 14%. SBP decreased in two weeks to <120 mmHg in 40% of the subjects. SBP significantly decreased (p < 0.001) in both men and women; among users or non-users of antihypertensive medications; and among those with or without various comorbidities including diabetes, overweight, or dyslipidemias. The use of medications was discontinued in 69% of subjects and decreased in 24% of them. Figure shows a waterfall plot distribution of the blood pressure changes after the 14-day study period and Figure shows the waterfall plot distribution for diastolic blood pressure.
Table 1. Baseline description of subjects with hypertension who attended NEWSTART Lifestyle Center
Table 2. Changes in systolic blood pressure from Baseline values after two weeks of NEWSTART lifestyle intervention
4. Discussion
NEWSTART was effective in significantly reversing SBP within 14 days among all clinical groups in this study. In addition, the use of antihypertensive medications was reduced or discontinued in 93% of the subjects.
4.1. The effectiveness of NEWSTART
The NEWSTART lifestyle intervention decreased SBP significantly in all subjects (−19 mmHg, −14%) within 14 days (Table ). The decrease of SBP for all the groups in this study varied from −8% for the group with diabetes to −31% for the group with normal weight. Forty percent of the subjects attained a SBP of <120 mmHg by the end of 14 days. The decrease in diastolic blood pressure was the same as the decrease in SBP (−14%). Likewise, the Waterfall plot distribution of SBP and diastolic blood pressure following the 14 days intervention of NEWSTART are similar (Figures and ). Thus, the responses of SBP and diastolic blood pressure to NEWSTART intervention were similar in percent decrease and in their distribution of decrease. The data show that a multiple lifestyle interventions with Adventist Lifestyle health principles is an effective means for decreasing systolic and diastolic hypertension in a senior population of men and women whether or not they take medications, and whether or not they have comorbidities including diabetes, overweight or dyslipidemia.
The SPRINT study that is responsible for the new standard for SBP showed a decrease of (−19 mmHg) in three months by intense medication therapy among non-diabetic patients and there were significant decreases in risk and mortality from cardiovascular disease (Wright et al., Citation2015). It is interesting to note, in comparison, that SBP in our study decreased by −18 mmHg in 14 days among non-diabetic subjects, showing the value of this multiple lifestyle interventions for treating hypertension. Decreases in SBP were also recorded in other studies using the NEWSTART lifestyle intervention. SBP decreased by 23 mmHg (−15%) within 3 weeks of intervention among diabetic patients with neuropathy (Crane & Sample, Citation1994). SBP decreased 6 mmHg in individuals from the general population attending a one-week wellness program using NEWSTART principles (Slavíček et al., Citation2008). Thus, this multiple lifestyle interventions lowers SBP to levels comparable to those observed with intensive therapy of antihypertensive medications (Wright et al., Citation2015), but without the side effects that followed the use of antihypertensive medications (Schiffrin et al., Citation2015; Wright et al., Citation2015).
A 93% drop in the need for antihypertensive medications accompanied the NEWSTART intervention. This decreased need for medication is similar to the reported decrease or discontinuation of antihypertensive medications (87%) within 7 days following a low-sodium, low-fat vegan diet together with exercise (McDougall et al., Citation2014). There was a similar 81% decrease in the use of medications after using a low-sodium, low-fat plant-based diet (Barnard, Zifferblatt, Rosenberg, & Pritikin, Citation1983), or a100% decrease after a medically supervised water-only fast followed by a vegan diet in a 20-day program for patients that had a SBP baseline of >140 mmHg (Goldhamer et al., Citation2001).
4.2. NEWSTART compared to other vegetarian interventions
An early study with a low-sodium, low-fat, plant-based diet together with exercise showed that SBP decreased −4 mmHg within 26 days among those with hypertension and using antihypertensive medications. The decrease in SBP was −14 mmHg among those who were not taking medication (Barnard et al., Citation1983). The comparable decreases in SBP by NEWSTART were −16 mmHg among those using antihypertensive medications and −21 mmHg among those not using them, but our results are for only 14 days rather than 26 days. SBP was decreased by −17 mmHg in 12 days with a whole-foods, sodium restricted, low-fat vegan diet together with exercise (McDougall et al., Citation2014). SBP decreased −37 mmHg (−23%) at 20 days after ingesting a low-sodium, low-fat, whole foods vegan diet which was preceded by an individualized medically supervised water-only fast in individuals with baseline SBP >140 mmHg (Goldhamer et al., Citation2001). The decrease in SBP was −60 mmHg in persons with baseline SBP ≥180 mmHg and −20 mmHg among individuals with a baseline SBP of 129 mmHg with the same fasting design (Goldhamer et al., Citation2002).
4.3. NEWSTART compared to conventional lifestyle interventions
A review on lifestyle interventions and hypertension shows that the average SBP is decreased by conventional therapeutic diets (−4.6 mmHg), exercise (−3.8 mmHg), salt and alcohol restriction (−3.6 mmHg), and fish oil supplements (−2.3 mmHg). The DASH diet is associated with a decrease in SBP from −6.7 mmHg (Saneei et al., Citation2014) to −7.6 mmHg (Dickinson, et al., Citation2006) and with a lower overall risk of cardiovascular disease. The DASH diet focuses on a reduction of sodium, saturated fat, red meats, and snack foods while it encourages the consumption of whole-grain cereals, low-fat dairy products, fruit and vegetables (Wong et al., Citation2016). The Portfolio Diet decreased SBP by −2.1 mmHg more than the DASH diet (Jenkins et al., Citation2015). The Portfolio Diet is a plant-based diet with increased content of viscous fiber, soy protein, plant sterols, and nuts. The PREMIER study (Appel et al., Citation2003) with an arm of behavioral modification plus the DASH diet achieved a drop in SBP of −8 mmHg (−6%) at 3 months, and −11 mmHg (−8%) at six months. None of these interventions were as effective as an intervention with NEWSTART.
4.4. NEWSTART potential mechanism of action
The effectiveness of NEWSTART in reversing SBP is undoubtedly due to its multiple health components—Nutrition, (Appel et al., Citation2006) Exercise (Skutnik et al., Citation2016), Water (Thornton, Citation2010), Sunlight (Feelisch et al., Citation2010; Mead, Citation2008), Temperance (abstinence of tobacco and alcohol) (Hillbom et al., Citation2011; Kannel & Higgins, Citation1990), fresh Air (Mao et al., Citation2012), Rest (Calhoun & Harding, 1010; Gangwisch et al., Citation2006), and Trust in God—spirituality (Charlemagne-Badal and Lee, Citation2016; Holt-Lunstad et al., Citation2011; Nedley and Ramirez, Citation2014; Tartaro et al., Citation2005). These factors may act alone and they may also interact synergistically one with another. While research has focused on the relation of the physical components to lowering SBP, there is evidence that the spiritual component is also important for controlling hypertension (Charlemagne-Badal & Lee, Citation2016; Holt-Lunstad et al., Citation2011; Nedley & Ramirez, Citation2014; Tartaro et al., Citation2005). Dietary factors are perhaps the best-known contributors to controlling hypertension using conventional therapeutic diets (Appel et al., Citation2003; Dickinson et al., Citation2006; Saneei et al., Citation2014; Wong et al., Citation2015, Citation2016) and plant-based diets (Goldhamer et al., Citation2001, Citation2002; McDougall et al., Citation1995, Citation2014; Razavi et al., Citation2014; Silberman et al., Citation2010). The current plant-based diets that are used for controlling hypertension are restricted in fat and/or salt (Barnard et al., Citation1983; McDougall et al., Citation2014).
The multiple lifestyle interventions of NEWSTART is with a vegan diet that is not restricted in neither fat nor salt. The diet contains 26% of energy as fat, but only 5% of energy is from saturated fat. Vegans following the Adventist Lifestyle consume 35% to 38% of energy as fat (Hardinge & Stare, Citation1954; Sanchez, Mejia, Sanchez, & Runte, Citation2019), with saturated fat being <5% of total energy (Sanchez et al., Citation2019). Such vegans have the lowest risk of hypertension as compared to other dietary groups (Pettersen et al., Citation2012). These data show that blood pressure is decreased in the presence of ordinary levels of dietary fat, suggesting that the restriction of vegetable dietary fats may not be an important contributor to lowering blood pressure.
Sodium restriction has been used to control hypertension (Adrogue & Madias, Citation2014; Wong et al., Citation2015, Citation2016). It is hypothesized, however, that the pathogenesis of hypertension is related to not only dietary sodium excess, since the intake of sodium, potassium, and the sodium-to-potassium ratio are all independently associated with hypertension (Du et al., Citation2014; Huggins et al., Citation2011). Potassium intake and decreased sodium intake estimated by excretion were inversely associated with systolic blood pressure (Mente et al., Citation2014; O’Donnell et al., Citation2014) and both were necessary to explain the decreases observed in hypertension (Binia, Jaeger, Hu, Singh, & Zimmermann, Citation2015). The lowest risk of cardiovascular events and deaths occur among populations with sodium intakes between 3 and 5 g sodium/day while the risk is increased at the higher or lower sodium intakes (Graudal, Jürgens, Baslund, & Alderman, Citation2014; Mente et al., Citation2014; O’Donnell, Mente, & Yusuf, Citation2015). The NEWSTART diet contains 1193 mg sodium and 1380 mg potassium per 1000 calories, with a sodium-to-potassium ratio of 0.86. The sodium and potassium content and the sodium-to-potassium ratio of this diet were compatible with reversing elevated SBP.
Plant-based diets are characterized by having no cholesterol, low-saturated fat, high fiber, high phytochemical content, and plant proteins (Altorf-van Berkow & Barnard, Citation2005; der Kuil et al., Citation2010). The NEWSTART vegan diet has all these characteristics, but we find it significant that epidemiological data seem to suggest a dose-related protection of plant proteins against elevated blood pressure. Vegans who consume only plant proteins have the lowest blood pressures, followed by lacto-ovo-vegetarians, while omnivores who consume the least vegetable proteins experience the highest blood pressures (Pettersen et al., Citation2012).
Plant proteins are associated with increased levels of plasma arginine. Arginine is the precursor of nitric oxide, which is a vasodilator as well as an antiatherogenic molecule. Elevated plasma arginine levels are linked to a reduction in hypertension (Boger, Citation2014; Pernow & Jung, Citation2016; Pretnar-Oblak, Citation2014; Sudar-Milovanovic et al., Citation2016). The prolonged administration of arginine increases nitric oxide production and decreases the risk to CVD (Boger, Citation2014). Thus, the higher postprandial and steady-state levels of plasma arginine might be involved in facilitating greater production of nitric oxide and this may be a mechanism for decreasing SBP. There is evidence for plant proteins to increase plasma arginine.
Postprandial fasting plasma arginine levels increases within 30 min and the increase is greater after a drink of soy protein (69% increase) as compared to casein (33% increase) in the same subjects (Sanchez, Filler, Hubbard, & Shavlik, Citation1988). The mean fasting plasma arginine level is also increased by plant protein diets. The mean fasting steady-state plasma arginine level was significantly increased by 18% in human subjects that switched from their typical U.S. diet to a plant–based diet for four weeks—from 61 ± 2 µm/L, mean±SE, to 72 ± 3 µm/L (Sanchez, Horning, Shavlik, Wingeleth, & Hubbard, Citation1985). The fasting steady-state plasma arginine level among long-term vegetarians was (90 ± 4 µm/L), 66% higher (Sanchez A, Mejia MA, and Hubbard RW, unpublished data) when compared to subjects on the typical U.S. diet (Sanchez et al., Citation1985). The role of arginine and NO in relation to hypertension in the NEWSTART vegan diet is unknown.
Arginine, important as it seems, is only one of several dietary contributors to the effective and rapid reversal of systolic blood pressure by the NEWSTART lifestyle intervention. Low fat and low salt are associated with mechanisms for controlling hypertension (McDougall, et al., 214; Wong et al., Citation2016), yet the NEWSTART vegan diet does not fit a paradigm of restricting fat or salt. This diet contains moderate amounts of fat and salt and it is an effective means for reversing SBP. It may be that factors other than diet intervened in lowering SBP, or that a drastic reduction in fat and salt are not as critical in controlling for hypertension as has been thought.
While the level of dietary salt or fat for the control of SBP has not been resolved, we are aware that moderate levels of fat and salt in the NEWSTART vegan diet improve its palatability and this favors adherence to the diet. The taste appeal of a diet is an important issue in life that favorably favors the patient adherence to the treatment and thus impacts public health by the number of persons that will adhere to the lifestyle and are thereby benefited by it.
4.5. A note on fasting
Fasting seems to enhance the decrease of high SBP when it precedes a vegan diet (Goldhamer et al., Citation2001, Citation2002). It has been hypothesized that the mechanism for the benefit of the water-only fast prior to a vegan diet is that it reverts the metabolism from pathological to healthful pathways and thus enhances the reversal of systolic blood pressure (McCarty, Citation2003). No specific metabolic pathway, however, has been suggested for these changes. The NEWSTART dietary intervention begins with a three-day medically supervised water-only fasting followed by a whole-food vegan diet, but the contribution of fasting to the effectiveness of NEWSTART for lowering SBP is unknown.
4.6. NEWSTART clinical implications
This is a limited short-term retrospective study, yet it presents compelling implications. The clinical implications of decreasing SBP by −19 mmHg in all subjects in this short-term study of two weeks could have significant clinical implications as suggested by a meta-analysis of 147 randomized clinical trials with SBP ≥ 130 mmHg (Law, Morris, & Wald, Citation2009). A reduction in SBP of −20 mmHg is achieved using three standard half-dose medications. Such a reduction in SBP is calculated to reduce the risk of coronary heart disease by 40–50% and the risk of stroke by 50–62%. Thus, the reduction in SBP achieved by NEWSTART (−19 mmHg) could have the potential to reduce the risk of coronary heart disease by nearly 50% and the risk of strokes by over 50%, if the levels in blood pressure achieved can be sustained on a long-term basis. This seems feasible based on epidemiological data of vegan subjects who practice the Adventist Lifestyle and have the lowest risk of hypertension (Pettersen et al., Citation2012). The health principles of the Adventist Lifestyle are intensified in the NEWSTART program and this intervention seems to provide an effective new start in life for those who seek to control systolic blood pressure by this lifestyle.
4.7. Conclusion
We conclude that the NEWSTART Lifestyle intervention is an effective and rapid means to decrease SBP in a variety of clinical groups, while eliminating or decreasing the need for antihypertensive medications in nearly all subjects. The long-term effects of this lifestyle with multiple health principles need to be investigated. This lifestyle program should also be studied for its effectiveness in decreasing other comorbidities of cardiovascular disease.
Source of Funding
Funded internally
Acknowledgements
We are grateful to Amy Camille Krueger and Hepisipa Fifita (“Peka”) for digitizing the coded NEWSTART data of 2014 in preparation for statistical analysis.
Additional information
Funding
Notes on contributors
Albert Sanchez
The authors of this paper are a group of individuals with an active interest in the complete health of as many individuals as possible. We have seen the benefits of short-term adoption of the NEWSTART health principals but these results are not widely know because they have not been tested and published. Hence, we are dedicated to scientifically test the health benefits of NEWSTART and have begun with high blood pressure, the most common medical problem in the U.S. We are amazed at how effective and rapid the NEWSTAR lifestyle intervention is for reversing high blood pressure. We look forward to testing other important clinical parameters that affect individual and public health such as diabetes, cardiovascular disease, and overweight to see how lifestyle can improve public health at low cost and without side effects from drugs.
References
- Adrogue, H. J., & Madias, N. E. (2014). The impact of sodium and potassium on hypertension risk. Seminars in Nephrology, 34(3), 257–13. doi: 10.1016/j.semnephrol.2014.04.003.
- Appel, L. J., Brands, M. W., Daniels, S. R., Karanja, N., Elmer, P. J., & Sacks, F. M. (2006). Dietary approaches to prevent and treat hypertension a scientific statement from the american heart association. Hypertension, 47, 296–3089. doi:10.1161/01.HYP.0000202568.01167.B6
- Appel, L. J., Champagne, C. M., Harsha, D. W., Cooper, L. S., Obarzanek, E., Elmer, P. J., … Svetkey, L. P. (2003). Effects of comprehensive lifestyle modification on blood pressure control: Main results of the premier clinical trial. Journal of the American Medial Association, 289, 2083–2093.
- Barnard, R. J., Zifferblatt, S. M., Rosenberg, J. M., & Pritikin, N. (1983). Effects of a high-complex-carbohydrate diet and daily walking on blood pressure and medication status of hypertensive patients. Journal of Cardiac Rehabilitation, 3, 839–850.
- Basile, J. N. (2002). Systolic blood pressure It is time to focus on systolic hypertension—Especially in older people. British Medical Journal, 325, 917–918. doi:10.1136/bmj.325.7370.917
- Berkow, S. E., & Barnard, N. D. (2005). Blood pressure regulation and vegetarian diets. Nutrition Reviews., 63, 1–8. doi:10.1111/j.1753-4887.2005.tb00104.x
- Binia, A., Jaeger, J., Hu, Y., Singh, A., & Zimmermann, D. (2015). Daily potassium intake and sodium-to-potassium ratio in the reduction of blood pressure: A meta-analysis of randomized controlled trials. Journal of Hypertension, 33, 1509–1520. doi:10.1097/HJH.0000000000000611
- Boger, R. H. (2014). The pharmacodynamics of l-arginine. Alternative Therapies in Health and Medicine, 20, 48–54.
- Calhoun, D. A., & Harding, S. M. (2010). Sleep and hypertension. Chest Journal, 138, 434–443. doi:10.1378/chest.09-2954
- Charlemagne-Badal, S. J., & Lee, J. W. (2016). Intrinsic religiosity and hypertension among older North American Seventh-day Adventists. Journal of Religion and Health, 55, 695–708. doi:10.1007/s10943-015-0102-x.
- Crane, M. G., & Sample, C. (1994). Regression of diabetic neuropathy with total vegetarian (vegan) diet. Journal of Nutritional Medicine, 4, 431–439. doi:10.3109/13590849409003592
- der Kuil, A.-V., Engberink, W., Brink, M. F., van Baak, E. J., Bakker, M. A., Navis, S. J., … Geleijnse, J. M. (2010). Dietary protein and blood pressure: A systematic review. PloS One, 5, e12102. doi:10.1371/journal.pone.0012102
- Dickinson, H. O., Mason, J. M., Nicolson, D. J., Campbell, F., Beyer, F. R., Cook, … Ford, G. A. (2006). Lifestyle interventions to reduce raised blood pressure: A systematic review of randomized controlled trials. Journal of Hypertension, 24, 215–233. doi:10.1097/01.hjh.0000199800.72563.26.
- Du, S., Batis, C., Wang, H., Zhang, B., Zhang, J., & Popkin, B. M. (2014). Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. American Journal Clin Nutrition, 99, 334–343. doi:10.3945/ajcn.113.059121
- Feelisch, M., Kolb-Bachofen, V., Liu, D., Lundberg, J. O., Revelo, L. P., Suschek, C. V., & Weller, R. B. (2010). Is sunlight good for our heart? European Heart Journal, 31, 1041–1045. doi:10.1093/eurheartj/ehq069
- Franklin, S. S., Khan, S. A., Wong, N. D., Larson, M. G., & Levy, D. (1999). Is pulse pressure useful in predicting risk for coronary heart disease?: The Famingham heart study. Circulation, 100, 354–360. doi:10.1161/01.cir.100.4.354
- Frisoli, T. M., Schmieder, R. E., Grodzicki, T., & Messerli, F. H. (2011). Beyond salt: Lifestyle modifications and blood pressure. European Heart Journal, 32, 3081–3087. doi:10.1093/eurheartj/ehr379
- Gangwisch, J. E., Heymsfield, S. B., Boden-Albala, B., Buijs, R. M., Kreier, F., Pickering, T. G., … Malaspina, D. (2006). Short sleep duration as a risk factor for hypertension analyses of the first national health and nutrition examination survey. Hypertension, 47, 833–839. doi:10.1161/01.HYP.0000217362.34748.e0
- Gay, H. C., Rao, S. G., Vaccarino, V., & Ali, M. K. (2016). Effects of different dietary interventions on blood pressure: Systematic review and meta-analysis of randomized controlled trials. Hypertension, 67, 733–739. doi:10.1161/HYPERTENSIONAHA.115.06853
- Goldhamer, A., Lisle, D., Parpia, B., Anderson, S. V., & Campbell, T. C. (2001). Medically supervised water-only fasting in the treatment of hypertension. Journal of Manipulative and Physiological Therapeutics, 24, 335–339. doi:10.1067/mmt.2001.115263
- Goldhamer, A. C., Lisle, D. J., Sultana, P., Anderson, S. V., Parpia, B., Hughes, B., & Campbell, T. C. (2002). Medically supervised water-only fasting in the treatment of borderline hypertension. Journal of Alternative and Complementary Medicine, 8, 643–650. doi:10.1089/107555302320825165
- Graudal, N., Jürgens, G., Baslund, B., & Alderman, M. H. (2014). Compared with usual sodium intake, low- and excessive-sodium diets are associated with increased mortality: A meta-analysis. American Journal of Hypertension, 27, 1129–1137. doi:10.1093/ajh/hpu028.
- Hardinge, M., & Stare, F. J. (1954). Nutritional studies of vegetarians 2. Dietary and serum levels of cholesterol. American Journal of Clinical Nutrition, 2, 83–88. doi:10.1093/ajcn/2.2.83
- He, F. J., Li, J., & Macgregor, G. A. (2013). Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. British Medical Journal, 346, f1325. doi:10.1136/bmj.f1164
- Hillbom, M., Saloheimo, P., & Juvela, S. (2011). Alcohol consumption, blood pressure, and the risk of stroke. Current Hypertension Reports, 13, 208–213. doi:10.1007/s11906-011-0194-y.
- Holt-Lunstad, J., Steffen, P. R., Sandberg, J., & Jensen, B. (2011). Understanding the connection between spiritual well-being and physical health: An examination of ambulatory blood pressure, inflammation, blood lipids and fasting glucose. Journal of Behavioral Medicine, 34, 477–488. doi:10.1007/s10865-011-9343-7.
- Huggins, C. E., O’Reilly, S., Brinkman, M., Hodge, A., Giles, G. G., English, D. R., & Nowson, C. A. (2011). Relationship of urinary sodium and sodium-to-potassium ratio to blood pressure in older adults in Australia. The Medical Journal of Australia., 195, 128–13247.
- IBM Corporation. (2015). IBM SPSS Statistics for Windows. Version 23.0. Armonk, NY: Author.
- James, P. A., Oparil, S., Carter, B. L., Cushman, W. C., Dennison-Himmelfarb, C., Handler, J., & Smith, S. C. (2014). Evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). Journal of the American Medical Association, 311, 507–520. doi:10.1001/jama.2013.284427.
- Jenkins, D. J. A., Jones, P. J., Frohlich, J., Lamarche, B., Ireland, C., Nishi, S. K., & Faulkner, D. (2015). The effect of a dietary portfolio compared to a dash-type diet on blood pressure. Nutrition, Metabolism and Cardiovascular Diseases, 25, 1132–1139. doi:10.1016/j.numecd.2015.08.006.
- Kannel, W., & Higgins, M. (1990). Smoking and hypertension as predictors of cardiovascular risk in population studies: Supplement of Official Journal of the International Society of Hypertension. Journal of Hypertension Suppl, 8, S3–8.
- Koenig, H. G. (2015). Religion, spirituality, and health: A review. Advances in Mind Body and Medicine, 29, 19–26.
- Law, M. R., Morris, J. K., & Wald, N. J. (2009). Use of blood pressure lowering drugs in the prevention of cardiovascular disease: Meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. British Medical Journal, 338, b1665. doi:10.1136/bmj.b902
- Le, L. T., & Sabate, J. (2014). Beyond meatless, the health effects of vegan diets: Findings from the Adventist Cohorts. Nutrients, 6, 2131–2147. doi:10.3390/nu6062131
- Li, J., Zheng, H., Du, H. B., Tian, X. P., Jiang, Y. J., Zhang, S. L., … Lu, C. (2014). The multiple lifestyle modification for patients with prehypertension and hypertension patients: A systematic review protocol. British Medical Journal Open, 4, e004920.
- Mao, G. X., Cao, Y. B., Lan, X. G., He, Z. H., Chen, Z. M., Wang, Y. Z., … Yan, J. (2012). Therapeutic effect of forest bathing on human hypertension in the elderly. Journal of Cardiology, 60, 495–502. doi:10.1016/j.jjcc.2012.08.003
- McCarty, M. F. (2003). A preliminary fast may potentiate response to a subsequent low-salt, low-fat vegan diet in the management of hypertension - fasting as a strategy for breaking metabolic vicious cycles. Medical Hypotheses, 60, 624–633.
- McDougall, J., Litzau, K., Haver, E., Saunders, V., & Spiller, G. (1995). Rapid reduction of serum cholesterol and blood pressure by a twelve-day, very low fat, strictly vegetarian diet. Journal of the American College of Nutrition, 14, 491–496.
- McDougall, J., Thomas, L. E., McDougall, C., Moloney, G., Saul, B., Finnell, J. S., … Petersen, K. M. (2014). Effects of 7 days on an ad libitum low-fat vegan diet: The Mcdougall Program Cohort. Nutrition Journal, 13, 1–7. doi:10.1186/1475-2891-13-1
- Mead, M. N. (2008). Benefits of sunlight: A bright spot for human health. Environmental Health Perspectives, 116, A160–A167.
- Mente, A., O’Donnell, M. J., Rangarajan, S., McQueen, M. J., Poirier, P., Wielgosz, A., … Di, C. (2014). Association of urinary sodium and potassium excretion with blood pressure. New England Journal of Medicine, 371, 601–611. doi:10.1056/NEJMoa1311989
- Mozaffarian, D., Benjamin, E. J., Go, A. S., Arnett, D. K., Blaha, M. J., Cushman, M., … Turner, M. B. (2016). Heart disease and stroke statistics-2016 update: A report from the american heart association. Circulation, 133, e38–360 10.1161/CIR.0000000000000350
- Nedley, N., & Ramirez, F. E. (2014). Nedley depression hit hypothesis identifying depression and its causes. American Journal of Lifestyle Medicine, 10, 422–428. doi:10.1177/1559827614550779
- O’Donnell, M., Mente, A., Rangarajan, S., McQueen, M. J., Wang, X., Liu, L., … Devanath, A. (2014). Urinary sodium and potassium excretion, mortality, and cardiovascular events. New England Journal of Medine, 371, 612–623. doi:10.1056/NEJMoa1311889
- O’Donnell, M., Mente, A., & Yusuf, S. (2015). Sodium intake and cardiovascular health. Circulation Research, 116, 1046–1057. doi:10.1161/CIRCRESAHA.116.303771
- Pernow, J., & Jung, C. (2016). The emerging role of arginase in endothelial dysfunction in diabetes. Current Vascular Pharmacology, 14, 155–162.
- Pettersen, B. J., Anousheh, R., Fan, J., Jaceldo-Siegl, K., & Fraser, G. E. (2012). Vegetarian diets and blood pressure among white subjects: Results from the Adventist Health Study-2 (AHS-2). Public Health Nutrition, 15, 1909–1916. doi:10.1017/S1368980011003454
- Pretnar-Oblak, J. (2014). Cerebral endothelial function determined by cerebrovascular reactivity to l-arginine. BioMed Research International, 2014, 601515. doi:10.1155/2014/601515
- Razavi, M., Fournier, S., Shepard, D. S., Ritter, G., Strickler, G. K., & Stason, W. B. (2014). Effects of lifestyle modification programs on cardiac risk factors. PloS One, 9, e114772. doi:10.1371/journal.pone.0114772
- Sanchez, A., Filler, K., Hubbard, R., & Shavlik, G. (1988). Plasma amino-acids after single soy, casein or protein-free meals in normocholesterolemic and hypercholesterolemic men. Nutrition Reports International, 38, 117–128.
- Sanchez, A., Horning, M., Shavlik, G., Wingeleth, D., & Hubbard, R. (1985). Changes in levels of cholesterol associated with plasma amino acids in humans fed plant proteins. Nutrition Reports International, 32, 1047–1056.
- Sanchez, A., Mejia, M. A., Sanchez, J., & Runte, E. (2019). A vegan diet rich in fats of plant origin may reverse coronary artery disease. Medical Hypothesis, 122, 103–105. doi:10.1016/j.mehy.2018.10.027
- Saneei, P., Salehi-Abargouei, A., Esmaillzadeh, A., & Azadbakht, L. (2014). Influence of dietary approaches to stop hypertension (dash) diet on blood pressure: A systematic review and meta-analysis on randomized controlled trials. Nutrition, Metabolism and Cardiovascular Diseases, 24, 1253–1261. doi:10.1016/j.numecd.2014.06.008
- Schiffrin, E. L., Calhoun, D., & Flack, J. M. (2015). Sprint proves that lower is better for nondiabetic high-risk patients, but at a price. American Journal of Hypertension, 29, 2–4. doi:10.1093/ajh/hpv190
- Silberman, A., Banthia, R., Estay, I. S., Kemp, C., Studley, J., Hareras, D., & Ornish, D. (2010). The effectiveness and efficacy of an intensive cardiac rehabilitation program in 24 sites. American Journal of Health Promotion, 24, 260–266. doi:10.4278/ajhp.24.4.arb
- Skutnik, B. C., Smith, J. R., Johnson, A. M., Kurti, S. P., & Harms, C. A. (2016). The effect of low volume interval training on resting blood pressure in pre-hypertensive subjects: A preliminary study. The Physician and Sportsmedicine, 44, 177–183. doi:10.1080/00913847.2016.1159501
- Slavíček, J., Kittnar, O., Fraser, G. E., Medová, E., Konečná, J., Žižka, R., … Novák, V. (2008). Lifestyle decreases risk factors for cardiovascular diseases. Central European Journal of Public Health, 16, 161–164.
- Sudar-Milovanovic, E., Obradovic, M., Jovanovic, A., Zaric, B., Zafirovic, S., Panic, … Isenovic, E. R. (2016). Benefits of l-arginine on cardiovascular system. Mini Reviews in Medicinal Chemistry, 16, 94–103.
- Tartaro, J., Luecken, L. J., & Gunn, H. E. (2005). Exploring heart and soul: Effects of religiosity/spirituality and gender on blood pressure and cortisol stress responses. Journal of Health Psychology, 10, 753–766. doi:10.1177/1359105305057311
- Thornton, S. N. (2010). Thirst and hydration: Physiology and consequences of dysfunction. Physiology & Behavior, 100, 15–21. doi:10.1016/j.physbeh.2010.02.026
- Whelton, P. K., Carey, R. M., Aronow, W. S., Casey, D. E., & Jones, D. W. (2018). 2017 ACC/AHA/AAPA/ABC/ACPM/ABS/APHA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension, 71, 1269–1324 10.1161/HYP.0000000000000066.
- Wong, M. C. S., Kwan, M. W. M., Wang, H. H. X., Fong, B. C. Y., Chan, W. M., Zhang, D. X., … Coats, A. J. S. (2015). Dietary counselling with the dietary approaches to stop hypertension (dash) diet for Chinese patients with grade 1 hypertension: A parallel-group, randomised controlled trial. The Lancet, 386, S8. doi:10.1016/S0140-6736(15)00586-3
- Wong, M. C. S., Wang, H. H. X., Kwan, M. W. M., Li, S. T. S., Liang, M., Fung, F. D. H., … Chan, D. K. L. (2016). The effectiveness of dietary approaches to stop hypertension (dash) counselling on estimated 10-year cardiovascular risk among patients with newly diagnosed grade 1 hypertension: A randomised clinical trial. International Journal of Cardiology, 224, 79–87. doi:10.1016/j.ijcard.2016.08.334
- Wright, J. T., Williamson, J. D., Whelton, P. K., Snyder, J. K., Sink, K. M., Rocco, M. V., … Lewis, C. E. (2015). A randomized trial of intensive versus standard blood-pressure control. New England Journal of Medicine, 373, 2103–2116. doi:10.1056/NEJMoa1511939
- Yokoyama, Y., Nishimura, K., Barnard, N. D., Takegami, M., Watanabe, M., & Miyamoto, Y. (2014). Vegetarian diets and blood pressure: A meta-analysis. JAMA Internal Medicine, 174, 577–587. doi:10.1001/jamainternmed.2013.14547