Abstract
Abstract: Superior oblique palsy is known to be caused by a defect of the trochlear nerve which could lead to horizontal and most times noticeable vertical misalignment of the eye. A case of superior oblique palsy (SOP) determined during a routine eye examination of a 16-year-old female with a complaint of blurring of vision at far and near with intermittent vertical diplopia while reading was presented. She showed right hypertropia and left exotropia of 10ΔBD and 9ΔBI, respectively, at far with fast recovery on right head tilt. Also, 12ΔBI and 12ΔBD for near with the left eye fixing. Parks–Bielschowsky three-step test showed that the patient’s hypertropia and vision increased on the right in the primary position while diplopia decreases when chin is depressed and her head is tilted to the left. Congenital superior oblique palsy can present with vertical diplopia in childhood or adulthood when contralateral head tilt is no longer enough to compensate for the vertical imbalance due to the decompensation of the vertical fusional reserve. Therefore, child’s old pictures are very important in confirming longstanding SOP and patching can be used to relief the diplopia.
PUBLIC INTEREST STATEMENT
The case report titled ”Superior Oblique palsy: A case report” focused on vertical diplopia. Patients with vertical diplopia complain of seeing two images, one atop or diagonally displaced from the other. It can occur due to a palsy of the third, fourth or sixth cranial nerve. Vertical diplopia due to cranial nerve IV palsy is not a common symptom in children because children more often present with an anomalous head position rather than diplopia. The case descripted the clinical presentation and management. It provides evidence that trochlear nerve palsy can cause vertical diplopia in children when the vertical fusional reserve is decompensated and it can be managed with occlusion. From the case, you can learn the skill in diagnosis of diplopia and broaden your thought. Hence, the case is valuable as a tutorial material.
1. Introduction
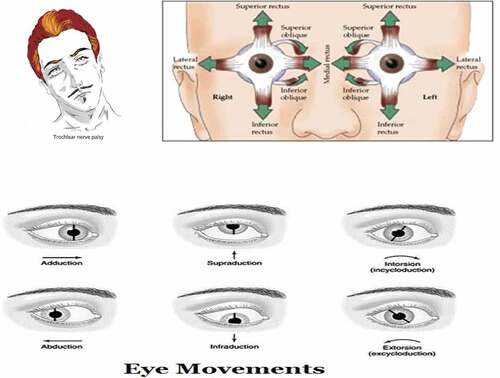
Fourth nerve innervates the superior oblique muscle so weakness of the nerve is known as superior oblique palsy (SOP) or trochlear nerve palsy (Chang et al., Citation2016). It is the most (80%) common cyclovertical muscle palsy (Plager, Citation1999) and is usually encountered in both pediatric and adult strabismus (Dosunmu et al., Citation2018). SOP can be congenital or acquired (Prieto-Díaz et al., Citation2003). Children with congenital SOP usually present with an anomalous head posture consisting of chin-down and head tilt to the opposite side (Lau et al., Citation2009). Occasionally, congenital SOP is accompanied by facial asymmetry with relative hypoplasia on the side of the tilt (Yang et al., Citation2012). Acquired SOP often causes vertical or oblique torsional diplopia which worsens in contralateral gaze and in downgaze, as a result, patients may have difficulty reading and walking downstairs (Wiwatwongwana & Lyon, Citation2013).
Table 1. Visual acuity
Table 2. Dry refraction
Table 3. Wet refraction or cycloplegic refraction
Table 4. Final prescription
Table 5. Other preliminary tests
2. Case presentation
A 16-year-old female was referred to the University of the West Indies (UWI) Optometry clinic for binocular vision assessment. The patient complained of intermittent double vision worst especially when reading school work which began 1 year ago. When asked if the double vision was side by side or up and down. She said it was up and down and gets better sometimes when she tilts her head to the left. She also said that it is not always there but comes most times when she bends down to read or looks down. The patient also denied having any pain, history of fall or injury. The Medical report showed no medical conditions or allergies. The last general health exam was in 2016 and the outcome was normal. The Patient’s old pictures showed compensatory head tilt. The patient was also observed to be depressing the chin while reading.
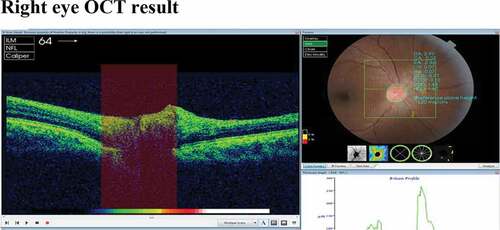
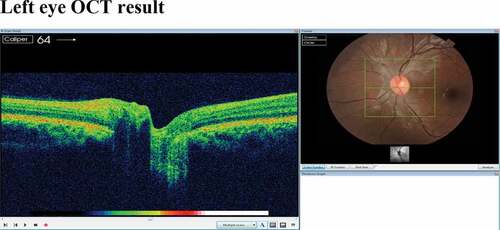
3. Ocular assessment
3.1. Binocular vision assessment
Distance cover test showed 9 prism dioptre (PD) left exotropia with 10 prism dioptre right hypertropia. Also, speed of movements and recovery were the same. Near cover test showed 12 PD left exotropia with 12 PD right hypertropia.
Hirschberg test was 15 PD right hypertropia (1 mm inferior) and 15 PD left exotropia (1 mm). On right gaze, the tropia increased from 15 prism dioptre to 20 PD right hypertropia. There was no stereopsis (with Lang and Frisby test).
The Park-Bielschowsky three-step test showed a 10Δ hyper-deviation when her head was tilted to the right, 7Δ hyper-deviation when tilted to the left and 10Δ hyper-deviation at straight-ahead position. Vertical fusional reserve was 6 PD and Lancaster Hess screen test showed SO under-action. Normal vertical fusional amplitudes range from one to four prism diopters, whereas patients with congenital CN IV palsy may demonstrate up to 10 to 15 prism diopters of vertical fusion amplitude (Cornblath, Citation2014; Peragallo & Newman, Citation2016). Maddox wing and Double Maddox rod results showed absence of torsional diplopia.
After the first visit the patient was told to return for additional testing. She was also told to bring in old photo in order to differentiate between longstanding and sudden head tilt. The patient’s old pictures revealed that the tilting of head was long standing.
4. Differential diagnosis
Based on the reported symptoms, the possible differential diagnosis are Brown syndrome, myasthenia gravis, thyroid eye diseases (TED), SOP or fourth nerve palsy and skew deviation. Brown syndrome is characterized by restriction of the superior oblique trochlea-tendon complex such that the affected eye does not elevate in adduction (Yang et al., Citation2017). Individuals with Brown syndrome may exhibit compensatory head turn or chin-up head posture and, occasionally, amblyopia; which was not the case in our patient as she had chin down rather than up; therefore, Brown syndrome was ruled out.
Myasthenia gravis is a chronic autoimmune, neuromuscular disease that causes weakness in the skeletal muscles that worsens after periods of activity and improves after periods of rest (Myasthenia gravis Fact sheet, Citation2020). Myasthenia gravis was ruled out because the patient had no bulging eye ball, drooping lids, facial paralysis and other symptoms associated with myasthenia gravis.
TED is a type of an eye condition that causes the immune system to attack the muscles and other tissues around the eyes. TED can cause inflammation that may affect the muscles and other tissues around the eyes. Symptoms often include pain in the eyes when looking up, down, or sideways, dryness, itching, dry eyes, diplopia, photophobia and difficulty with moving the eyes (Giugni et al., Citation2013). Our patient had diplopia that was not associated with aforementioned symptoms which means that the condition was unlikely to be a TED. Moreover, there was no record of thyroid problem on her medical report.
Palsy of the fourth cranial nerve (trochlear nerve) is one of the causes of paralytic strabismus and can result from lesions anywhere along its path between the fourth nerve nucleus in the midbrain and the superior oblique muscle within the orbit (Chang et al., Citation2016). Fourth nerve palsy (SOP) could be very difficult to distinguish from a skew deviation since both conditions may be associated with a positive head-tilt or three-step test (Donahue et al., Citation2001). However, patients with skew deviation typically have binocular torsion as opposed to none or ex-cyclotorsion of just one eye seen in a fourth nerve palsy (Liu et al., Citation2001). However, our patient did not exhibit any of the characteristics consistent with skew deviation during our examination. The condition was therefore diagnosed as SOP. The diagnosis was made based on the results of the Park three steps test, double Maddox rod test, and Lancaster Hess screen test.
Patients may present with fourth cranial nerve palsy at any age and in either gender (Dosunmu et al., Citation2018). Many cases report a male predominance, presumably because of the greater incidence of trauma in young males (Dosunmu et al., Citation2018).
SOP could be congenital, acquired or idiopathic. In adults, SOP is mostly acquired and the most common cause is injury (Chang et al., Citation2016). The long course of the fourth cranial nerve renders it particularly prone to injury from blunt head trauma or compression from changes in intracranial pressure, brain tumors, or swelling anywhere along its course. Fourth nerve injury can occur with injuries that cause whiplash or concussions (Plager, Citation1999). Another common cause is from poor blood flow related to diabetes. SOP that is caused by injury may not go away. In adults, many cases of fourth nerve palsy that are not caused by injury are idiopathic and that often presents with pains above the eyebrows which goes away once vertical diplopia starts (Plager, Citation1999). The idiopathic cases usually resolve in few weeks which is why it is advisable to defer additional neuro-radiologic testing until two months have passed without improvement.
Acquired and Idiopathic SOP were ruled out since our patient did not have any history of injury, fall, infection, disease, pain above the eye brow and the vertical diplopia did not go away for more than six months. However, head tilting in the old pictures, chin depression, vertical fusional reserve of 6PD as against maximum of 3PD seen in normal people (Bharadwaj et al., Citation2007) and the fact that our patient is a child suggest that our patient has congenital right SOP. Moreover, most cases of congenital SOP are diagnosed based on a history of ocular torticollis since early childhood, increased vertical fusional amplitudes and absence of torsional diplopia (Kaeser et al., Citation2012).
Congenital SOP usually presents with the eye on the affected shooting upwards when the child looks to the opposite side. To compensate for the vertical and torsional imbalance of the eyes a parent may notice the child often tilting and/or turning the head to one side. Most children with SOP do not complain of double vision because they have a good binocular vision with the aid of their head posture. They do not normally need glasses. However, they might become symptomatic when the vertical fusional vergence is decompensated. That means it is no longer capable of preventing the eye from moving up or down.
5. Management or treatment
The first step in treating cranial nerve palsies is to determine the etiology once the etiology is found, then treatment can begin (Mollan et al., Citation2009; Tamhankar et al., Citation2013). High satisfaction with prismatic correction has been reported in patients with decompensated SOP (Bagheri et al., Citation2010). Younger patients may use Fresnel’s prisms as a temporary option. However, excyclotorsion and incomitance of the deviation may leave some patients unsatisfied with prisms. If the fourth nerve palsy is due to previous trauma and has recently decompensated, the diplopia can be managed by the placement of vertical prisms in spectacles. When managing isolated CN IV palsy, it is advisable to delay prescribing permanent prisms for at least three months in order to allow for the palsy to recover. Otherwise, glasses with permanent prism correction can induce vertical diplopia should the palsy recover. Others, particularly those with ischemic palsies, in whom recovery is expected, can occlude the lower half of the lens over the affected eye (Prieto-Díaz et al., Citation2003). Opaque or black tape, for instance, can also be used to occlude the affected eye in the direction of action of the superior oblique muscle (Bagheri et al., Citation2010; Gunderson et al., Citation2001; Prieto-Díaz et al., Citation2003).
No treatment is needed if the child is developing equal vision in both eyes, has good binocular vision and does not have a troublesome head posture. In these cases, only periodic observation in the clinic will be required. If a child is finding it difficult to control the squint, even when using a head posture and/or if the binocular vision begins to deteriorate, use of prisms may be recommended to help with anomalous head position. Also, larger deviations may benefit from surgery.
Patients with persistent fourth nerve palsies who are unsatisfied with prisms or patching may require strabismus surgery (Lau et al., Citation2009; Park et al., Citation2008). Botulinum Toxin (BOTOX) can also be used as a neuromuscular agent to suppress any further effects after surgery (Bagheri et al., Citation2010).
The decision to intervene surgically is based on the presence of increasing symptoms of double vision and an inability to carry on normal activities combined with stable measurements over a period of several months (Gunderson et al., Citation2001). Procedures vary by surgeon; one technique is superior oblique tucking.
Superior oblique tucking is the strengthening procedure for the superior oblique by double folding the tendon in an adjustable manner (Li & Zhao, Citation2014). The goal of the surgery is to decrease the double vision and stop the compensating head tilt (Chang et al., Citation2016). The prognosis is good for younger children with fusional ability (Bagheri et al., Citation2010). Idiopathic cases tend to sometimes resolve on their own and traumatic or acquired cases tend to have poorer outcomes given less functional recovery after surgery (Lau et al., Citation2009). In traumatic cases of SOP, magnetic resonance imaging (MRI) and computerized tomography (CT) scan are advised to be done prior to management in order to rule out subarachnoid haemorrhaging (Demer et al., Citation2011; Machandia & Demer, Citation2011).
In this case, the patient was educated on her present condition. The final spectacle prescription was not given because of the diplopia. Base-down prism over her final prescription on the right eye did not improve the patient’s condition. She preferred chin depression and tilting her head opposite side to overcome the diplopia. Going forward, she was instructed to remain keenly aware of her double vision. Additionally, she was informed to return to the clinic if the problem persists and affects her normal daily activities.
5.1. First follow-up visit
Some weeks later, patient returned to the clinic with the same complaints. Patching of the paretic eye (right eye) was recommended for the patient in order to help with the diplopia.
5.2. Second follow-up visit
The patient came back two weeks later for follow up and reported great improvement with patching. Prisms were tried but the result gotten was not reliable. Patient was advised to continue with patching and return to the clinic in two weeks.
6. Discussion
SOP can be congenital or acquired, unilateral or bilateral, each of which may present with a distinct clinical picture and is known to be the most common cyclovertical muscle palsy (Chang et al., Citation2016; P. Merino et al., Citation2004; P. S. Merino et al., Citation2014). In children younger than 19 years of age, the annual incidence is 3.4 cases per 100,000 (Tollefson et al., Citation2006). The most common cause of SOP was identified to be congenital (49%) (P. S. Merino et al., Citation2014) and it was found to be higher in males than females (Martinez‐Thompson et al., Citation2014; P. S. Merino et al., Citation2014). The acquired causes were primarily due to trauma, hypertension, diabetes mellitus, post-neurosurgeries and intracranial neoplasms (Donahue et al., Citation2001; Khawam et al., Citation2000). Yang et al. (Citation2012) reported the two major causes of congenital SOP as cranial dis-innervation syndrome characterized by the absence of the trochlear nerve all together seen in 73% of cases and secondary atrophy to the superior oblique muscle, such as an abnormal superior oblique tendon which is usually seen in 23% of medical cases (Dosunmu et al., Citation2018). Dosunmu et al. (Citation2018) study in the USA showed that most cases of congenital CNIV palsy presented in the fourth decade of life.
The trochlear nerve arises from the trochlear nucleus of the brain, emerging from the posterior aspect of the midbrain (it is the only cranial nerve to exit from the posterior midbrain) (Brazis, Citation1993). It runs anteriorly and inferiorly within the subarachnoid space before piercing the dura mater adjacent to the posterior clinoid process of the sphenoid bone. The nerve then moves along the lateral wall of the cavernous sinus (along with the oculomotor nerve, the abducens nerve, the ophthalmic and maxillary branches of the trigeminal nerve and the internal carotid artery) before entering the orbit of the eye via the superior orbital fissure. The trochlear nerve innervates the superior oblique, which is a muscle of oculomotion (Kim et al., Citation2020). The tendon of the superior oblique is tethered by a fibrous structure known as the trochlea, giving the nerve its name. Although the mechanism of action of the superior oblique is complex, in clinical practice it is sufficient to understand that the overall action of the superior oblique is to depress and intort the eyeball (Morillon & Bremner, Citation2017).
A fourth nerve palsy often presents suddenly, but may result from decompensation of a longstanding or congenital palsy and the onset just seems sudden. In order to differentiate these two types of palsies, ask for old photographs. A patient with a decompensated, longstanding palsy will present with a compensatory head tilt that often can be identified in photographs. Usually, patients are not even aware of their head tilt. In the case of complicated fourth nerve palsies (those that present with other concurrent neurological dysfunction), the patient should undergo neuro-radiological studies. The accompanying signs and symptoms typically dictate the extent of these evaluations.
In the case of isolated fourth nerve palsies caused by recent trauma, the patient should also undergo neuro-radiological studies of the head to dismiss the possibility of a concurrent subarachnoid hemorrhage (Demer et al., Citation2011; Machandia & Demer, Citation2011). If the fourth nerve palsy is not associated with recent trauma, a history of past trauma should be investigated. If the patient is elderly and has a fourth nerve palsy of truly recent origin, an ischemic vascular evaluation should be undertaken to search for diabetes and hypertension.
In childhood, the vast majority of fourth nerve palsies are congenital or acquired (traumatic) so neuroimaging is not necessary (P. S. Merino et al., Citation2014). It is reserved for those with associated neurological signs or symptoms, or progression (Barton, Citation2006). Moreover, patients with congenital SOP may still present very late in life only when their fusional amplitude has deteriorated (Yau et al., Citation2015).
7. Conclusion
Congenital superior oblique palsy can present with vertical diplopia in childhood or adulthood when contralateral head tilt is no longer enough to compensate for the vertical imbalance due to the decompensation of the vertical fusional reserve. Therefore, child’s old pictures are very important in confirming longstanding SOP and patching can be used to relief the diplopia.
Additional information
Funding
Notes on contributors
Ngozika Esther Ezinne
I am Dr Ngozika Esther Ezinne. I have a Doctor of optometry (OD) degree from Abia State University, Nigeria and Master of Optometry from the University of KwaZulu-Natal, South Africa. I am a lecturer at the University of the West Indies St Augustine campus, Trinidad and Tobago. My research interests are binocular vision, orthoptics, pediatric optometry, ocular surface, myopia, contact lens and public health optometry. The authors of this paper including Dr Kingsley Ekemiri and Aliyah Khan worked as a team to articulate this case study of a 16-year-old female with superior oblique palsy. In this paper, the authors presented a case of vertical diplopia due to trochlear nerve palsy and how it was managed.
References
- Bagheri, A., Fallahi, M. R., Abrishami, M., Salour, H., & Aletaha, M. (2010). Clinical features and outcomes of treatment for fourth nerve palsy. Journal of Ophthalmic & Vision Research, 5(1), 27–9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3380667/
- Barton, J. J. S. (2006). The symptomatic IV nerve palsy. Neuro-ophthalmology, 28(4), 171–178. https://doi.org/10.1080/01658100490887760
- Bharadwaj, S. R., Hoenig, M. P., Sivaramakrishnan, V. C., Karthikeyan, B., Simonian, D., Mau, K., Rastani, S., & Schor, C. M. (2007). Variation of binocular-vertical fusion amplitude with convergence. Investigative Opthalmology & Visual Science, 48(4), 1592–1600. https://doi.org/doi:10.1167/iovs.06-1018
- Brazis, P. W. (1993). Palsies of the trochlear nerve: Diagnosis and localization—Recent concepts. Mayo Clinic Proceedings, 68(5), 501–509. https://doi.org/doi:10.1016/S0025-6196(12)60201-8.
- Chang, M. Y., Coleman, A. L., Tseng, V. L., & Demer, J. L. (2016). Surgical interventions for vertical strabismus in superior oblique palsy. Cochrane Database of Systematic Reviews, 2016(12), CD012447. https://doi.org/10.1002/14651858.CD012447
- Cornblath, W. T. (2014). Diplopia due to ocular motor cranial neuropathies. Continuum (Minneap Minn), 20(4), 966–980. DOI: 10.1212/01.CON.0000453309.44766.b4
- Demer, J. L., Kung, J., & Clark, R. A. (2011). Functional imaging of human extraocular muscles in head tilt dependent hypertropia. Investigative Ophthalmology & Visual Science, 52(6), 3023–3031. https://doi.org/10.1167/iovs.10-6596
- Donahue, S. P., Lavin, J. P., Mohney, B., & Hamed, L. (2001). Skew deviation and inferior oblique palsy. American Journal of Ophthalmology, 132(5), 751–756. https://doi.org/10.1016/S0002-9394(01)01234-X
- Dosunmu, E. O., Hatt, S. R., Leske, D. A., Hodge, D. O., & Holmes, J. M. (2018). Incidence and etiology of presumed fourth cranial nerve palsy: A population-based study. American Journal of Ophthalmology, 185, 110–114. https://doi.org/10.1016/j.ajo.2017.10.019
- Giugni, A. S., Mani, S., Kannan, S., & Hatipoglu, B. (2013). Exophthalmos: A forgotten clinical sign of Cushing’s Syndrome. Case Reports in Endocrinology, 2013, 205–208. https://doi.org/doi:10.1155/2013/205208
- Gunderson, C. A., Mazow, M. L., & Avilla, C. W. (2001). Epidemiology of CN IV palsies. American Orthoptic Journal, 51(1), 99–102. https://doi.org/10.3368/aoj.51.1.99
- Kaeser, P. F., Klainguti, G., & Kolling, G. H. (2012). Inferior oblique muscle recession with and without superior oblique tendon tuck for treatment of unilateral congenital superior oblique palsy. Journal of American Association for Pediatric Ophthalmology and Strabismus, 16(1), 26–31. https://doi.org/10.1016/j.jaapos.2011.08.012
- Khawam, E., Ghazi, N., & Salti, H. (2000). “Jampolsky syndrome”: Superior rectus overaction-contracture syndrome: Prevalence, characteristics, etiology and management. Binocular Vision & Strabismus Quarterly, 15(4), 331–342.
- Kim, S. Y., Motlagh, M., & Naqvi, I. A. (2020). Neuroanatomy, Cranial Nerve 4 (Trochlear). In StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK537244
- Lau, F. H., Fan, D. S., Sun, K. K., Yu, C. B., Wong, C. Y., & Lam, D. S. (2009). Residual torticollis in patients after strabismus surgery for congenital superior oblique palsy. British Journal of Ophthalmology, 93(12), 1616–1619. https://doi.org/10.1136/bjo.2008.156687
- Li, Y., & Zhao, K. (2014). Superior oblique tucking for treatment of superior oblique palsy. Journal of Pediatric Ophthalmology & Strabismus, 51(4), 249–254. https://doi.org/10.3928/01913913-20140527-01
- Liu, G. T., Volpe, N. J., & Galetta, S. L. (2001). Eye movement disorders: Conjugate gaze abnormalities. In Neuro-ophthalmology: Diagnosis and management (pp. 584–626). WB Saunders.
- Machandia, A. M., & Demer, J. L. (2011). Sensitivity of the three‐step test in diagnosis of superior oblique palsy. Journal of AAPOS, 18(6), 567–571. https://doi.org/10.1016/j.jaapos.2014.08.007
- Martinez‐Thompson, J. M., Diehl, N. N., Holmes, J. M., & Mohney, B. G. (2014). Incidence, types, and lifetime risk of adult‐onset strabismus. Ophthalmology, 121(4), 877–882. https://doi.org/10.1016/j.ophtha.2013.10.030
- Merino, P., Gómez de Liaño, P., García, C., Bartolomé, G., Rodríguez, C., & De Juan, L. (2004). Bilateral superior oblique palsy and botulinum toxin. Archivos de la Sociedad Espanola de Oftalmologia, 79(3), 119–123.
- Merino, P. S., Rojas, P. L., Gómez De Liaño, P. S., Fukumitsu, H. M., & Yáñez, J. M. (2014). Bilateral superior oblique palsy: Etiology and therapeutic options. European Journal of Ophthalmology, 24(2), 147–152. https://doi.org/10.5301/ejo.5000362
- Mollan, S. P., Edwards, J. H., Price, A., Abbott, J., & Burdon, M. A. (2009). Aetiology and outcomes of adult superior oblique palsies: A modern series. Eye (Lond), 23(3), 640–644. https://doi.org/10.1038/eye.2008.24
- Morillon, P., & Bremner, F. (2017). Trochlear nerve palsy. British Journal of Hospital Medicine, 78(3), C38–C40. https://doi.org/10.12968/hmed.2017.78.3.C38
- Myasthenia gravis Fact sheet. (2020). www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Myasthenia-Gravis-Fact-Sheet
- Park, U. C., Kim, S. J., Hwang, J. M., & Yu, Y. S. (2008). Clinical features and natural history of acquired third, fourth, and sixth cranial nerve palsy. Eye (Lond), 22(5), 691–696. https://doi.org/10.1038/sj.eye.6702720
- Peragallo, J., & Newman, N. (2016). Diplopia—An update. Seminars in Neurology, 36(4), 357–361. https://doi.org/10.1055/s-0036-1585428
- Plager, D. A. (1999). Superior oblique palsy and superior oblique myokymia. In A. L. Rosenbaum & A. P. Santiago (Eds.), Clinical Strabismus Management. Principles and Surgical Techniques (pp. 219–229). W.B. Saunders Company.
- Prieto-Díaz, J., Gamio, S., & Prieto-Díaz, F. (2003). Unilateral superior oblique paresis: Deviation patterns and surgical indications. Binocular Vision & Strabismus Quarterly, 18, 201–208.
- Tamhankar, M. A., Biousse, V., Ying, G. S., Prasad, S., Subramanian, P. S., Lee, M. S., Eggenberger, E., Moss, H. E., Pineles, S., Bennett, J., Osborne, B., Volpe, N. J., Liu, G. T., Bruce, B. B., Newman, N. J., Galetta, S. L., & Balcer, L. J. (2013). Isolated third, fourth, and sixth cranial nerve palsies from presumed microvascular versus other causes: A prospective study. Ophthalmology, 120(11), 2264–2269. https://doi.org/10.1016/j.ophtha.2013.04.009
- Tollefson, M. M., Mohney, B. G., Diehl, N. N., & Burke, J. P. (2006). Incidence and types of childhood hypertropia: A population‐based study. Ophthalmology, 113(7), 1142–1145. https://doi.org/10.1016/j.ophtha.2006.01.038
- Wiwatwongwana, A., & Lyon, C. (2013). Eye movement control and its disorders. Handbook of Clinical Neurology, 113, 1505–1513. https://www.sciencedirect.com/science/article/pii/B9780444595652000216
- Yang, H. K., Kim, J. H., & Hwang, J. M. (2012). Congenital superior oblique palsy and trochlear nerve absence: A clinical and radiological study. Ophthalmology, 119(1), 170–177. https://doi.org/10.1016/j.ophtha.2011.06.038
- Yang, H. K., Kim, J. H., Kim, J., & Hwang, J.-M. (2017). Combined Brown syndrome and superior oblique palsy without a trochlear nerve: Case report. BMC Ophthalmology, 17(1), 159. https://doi.org/10.1186/s12886-017-0553-9
- Yau, G. S., Tam, V. T., Lee, J. W., Chan, T. T., & Yuen, C. Y. (2015). Surgical outcomes for unilateral superior oblique palsy in Chinese population: A retrospective study. International Journal of Ophthalmology, 8(1), 107–112. https://doi.org/10.3980/j..2