?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract:
Abstract: Post-operative sepsis tends to complicate the recovery course of many patients. Across the globe, the proportion of post-operative sepsis varied from 2.9% to 30% in various studies. To determine mean proportion of post-operative sepsis in Maternity and General Surgical wards (GSW) and establish whether there was a significant difference in the proportion of post-operative sepsis between the two departments. The design was part of an Unmatched Retrospective Cohort study of post-operative patients admitted to the Maternity and General Surgical ward over the past 6 months. Random samples of 169 respondents from Maternity and 245 respondents from GSW were compared. Mean proportion of post-operative sepsis was 4.4% and 3.1% for Maternity ward and GSW, respectively. Test statistic, Z2 (4.98) , Z1 (1.96), fell in the rejection region; hence, Ho was rejected (significant difference in the proportion of sepsis). In the Maternity ward, the risk of post-operative sepsis was more among the unmarried (p = 0.023, COR = 5.550 [1.272–24.219] at 95% CI). In General Surgical Ward (GSW), emergency surgery (11.9%) and complex surgeries (16.3%) carried more risk. Risk of post-operative sepsis in maternity was more among the unmarried (27.3%). For GSW, emergency surgery (11.9%) and complex surgeries (16.3%) carried more risk. Therefore, more effort is needed to combat post-operative sepsis.
PUBLIC INTEREST STATEMENT
Post-operative wound infections, also known as surgical site infections (SSIs), tend to complicate the recovery course of many patients. These infections typically occur within 30 days of an operation at the site or part of the body where the surgery took place. Sometimes it occurs within a year if an implant is left in place and the infection is thought to be secondary to surgery. Bacterial colonization on the patient’s skin and alimentary and genital tract is the principal contributing sources that lead to SSIs. Thus, Surgical site infections (SSIs) are infections of the incision or organ or space that occur after surgery. Surgical patients were initially seen with more complex comorbidities and the emergence of antimicrobial-resistant pathogens increased the cost and challenge of treating SSIs. Therefore, this investigation is worth it.
1. Introduction
1.1. Background to the study
Post-operative wound infections, also known as surgical site infections (SSIs), tend to complicate the recovery course of many patients. These infections typically occur within 30 days of an operation at the site or part of the body where the surgery took place. Sometimes it occurs within a year if an implant is left in place and the infection is thought to be secondary to surgery. Bacterial colonization on the patient’s skin and alimentary and genital tract is the principal contributing sources that lead to SSIs (Azoury et al., Citation2015). Surgical site infections (SSIs) are infections of the incision or organ or space that occur after surgery. Surgical patients initially seen with more complex comorbidities and the emergence of antimicrobial-resistant pathogens increase the cost and challenge of treating SSIs (Berríos-Torres et al, Citation2017).
Post-operative sepsis remains a significant cause of morbidity and mortality, with early recognition of post-operative sepsis remaining problematic in some hospitals (Diane, Citation2006). In another study on post-operative sepsis among cancer patients, it was concluded that postoperative sepsis was the only major post-operative event associated with long-term mortality and that it (Postoperative sepsis) may reflect a deep impairment of immune response, which is potentially associated with cancer recurrence and mortality (Mokart et al., Citation2016). In fact, Sood et al. (Citation2017) found that out of 2954 post-operative cancer patients, overall, 4.3% of patients developed post-operative sepsis.
The development of sepsis after elective surgical procedures imposes a significant clinical and resource utilization burden in the United States. It was found that 78,669 cases (1.21%) who underwent general surgery developed post-operative sepsis. The factors associated with the development of sepsis were patients’ age, race, gender, hospital bed size, hospital location, hospital teaching status and patient income, among others (Todd et al., Citation2010). It has also been argued that sepsis is more common after surgery for several reasons; first, urinary tract infections are more common after surgery and these infections can lead to sepsis. The risk of death is significant if post-operative sepsis leads to a complication, septic shock, with approximately 40% of septic shock patients dying, even with treatment. Secondly, an incision is an opening into the body through which infection can begin. Surgery takes a toll on the body and weakens the immune system, even if the procedure is a minor one, which can make infections more likely (Whitlock & Fogoros, Citation2018). At the global level, a similar study by Woelber et al. (Citation2016) found that the overall proportion of operations leading to Surgical Site Infection was 9.9%. This is form of post-operative sepsis.
The determinants or risk factors associated with post-operative sepsis vary. A study by Ellen, et al. (Citation2013) found that risk factors consistently identified as associated with SSI included comorbidities, advanced age, risk indices, patient frailty and surgical complexity, as well as long duration surgical procedures.
Mokart et al. (Citation2005) argued that sepsis after major surgery is common in patients admitted to intensive care units (ICU). It has become the most common cause of mortality in surgical ICU. Latest therapeutic advances have enabled clinicians to reduce early post-operative mortality and/or morbidity. Despite those advances, patients remained at high risk for infection and the associated increased morbidity and mortality. The suppression of the immune system after surgery predisposes the patients to develop sepsis. The post-surgical immune-suppression may be related to the direct effects of anaesthetic drugs, hormonal changes related to stress, effects of haemorrhage and transfusion, occurrence of ischaemia–reperfusion, and extent of surgical trauma. The underlying illness, comorbidity and factors like age or gender also played a pivotal role in modulating the immune system. A study by Namba et al. (Citation2012) found the incidence of SSI was 0.51% (155 of 30,491). Patient factors associated with SSI included female gender, obesity, and the American Society of Anesthesiologists (ASA) score ≥3. Age, diagnosis, diabetes and race were not associated with SSI. The only surgical factor associated with SSI was a bilateral procedure. Surgeon and hospital volumes, use of antibiotic-laden cement, fixation method, laminar flow, body exhaust suits, surgical approach and fellowship training were not associated with risk of SSI. A comprehensive infection surveillance system, combined with techniques, identified patient and surgical factors associated with SSI. They recommended that obesity and chronic medical conditions should be addressed prior to Total Hip Replacement (THR).
This article entails background of the study, study area, problem statement, objectives, review of relevant literature, methods and results among others.
1.2. Background of the study area
Gulu Regional Referral Hospital (GRRH), commonly known as Gulu Hospital, is located in Gulu, Northern Uganda. Gulu is the largest metropolitan area in Uganda’s Northern Region. The hospital, however, serves a wide catchment area which includes the following districts: Amuru, Gulu, Kitgum, Lamwo and Pader. It is affiliated with Gulu University, where it serves as a teaching hospital for the Faculty of medicine_ medical students.
GRRH is about 343 km (213 miles), by road, north of Kampala, Uganda’s capital, and largest city. GRRH is a public hospital, funded by Uganda Ministry of Health (MoH) and general care in the hospital is free (Elective Network, Citation2018).The hospital is one of the 14 Regional Referral Hospitals in Uganda, with the capacity of 350 beds. The Standard unit of Output (SUO) is 674,146 which is fourth highest among the 14 Regional Referral Hospitals in Uganda. The Bed Occupancy Rate (BOR) is 105% and Average Length of Stay (ALOS) is 3.9 days whereas the Caesarean Section Rate (CSR) of the hospital is 16%. The hospital conducted 653 Caesarean Sections and 2,160 major surgeries in the financial year 2016/2017 (MoH, Citation2017).
1.3. Statement of the problem
Post-operative sepsis remains a significant cause of morbidity and mortality (Diane, Citation2006). In fact, Sood et al. (Citation2017) found that out of 2954 post-operative cancer patients; overall, 4.3% of patients developed post-operative sepsis. Another study at global level by Woelber et al. (Citation2016) found that the overall proportion of operations leading to Surgical Site Infection was 9.9%. This is form of post-operative sepsis.
Therefore, the major problem is that there could be significant difference in the proportion of post-operative sepsis between maternity and general surgical wards, the two hospital departments with leading number of operations (surgery). The effect could be a significant variation in infection rates between the two departments. It is hereby presumed that this proportion could even be much higher in general surgical ward, and yet few researches have been done to ascertain this presumption. The researchers, therefore, set out to test hypothesis against this presumption in Gulu Regional Referral Hospital but also ascertain the determinants of sepsis in the two departments (Maternity and General surgical ward).
1.4. Research hypotheses
The researcher has hypothesized as per the Null hypothesis (H0) and Alternative hypothesis (H1) below;
1.4.1. Null hypothesis (H0)
The null hypothesis was stated as H0:1—
2 = 0[There is no significant difference in the proportion of post-operative sepsis between maternity (
1) and General Surgical ward (
2)].
Where:
(1) = Proportion of post-operative sepsis in random sample from maternity ward
(2) = Proportion of post-operative sepsis in random sample from General surgical ward
1.4.2. Alternative hypothesis (H1)
The Alternative hypothesis was stated as H1: 1—
2
0 (There is significant difference between proportion of post-operative sepsis between Maternity and General Surgical ward)
Assuming normal distribution of the data, the hypotheses were tested at 5% level of significance, confidence interval—95%
1.5. Objectives of the Study
The specific objectives of the study were as follows:
To determine the mean monthly proportion of post-operative sepsis in Maternity and General Surgical wards of Gulu Regional Referral Hospital between May 2018 and November 2018
To establish whether there was a significant difference in the proportion of post-operative sepsis between maternity and General Surgical wards of Gulu Regional Referral Hospital between May 2018 and November 2018
To ascertain the determinants of post-operative sepsis in maternity and General Surgical wards of Gulu Regional Referral Hospital between May 2018 and November 2018
To ascertain the lived experiences of patients who developed post-operative sepsis in Maternity and General Surgical wards of Gulu Regional Referral Hospital between May 2018 and November 2018
2. Review of literature
2.1. Mean proportion of post-operative sepsis in maternity and surgical wards
Post-operative wound infections, also known as surgical site infections (SSIs), tend to complicate the recovery course of many patients. These infections typically occur within 30 days of an operation at the site or part of the body where the surgery took place. Sometimes it occurs within a year if an implant is left in place and the infection is thought to be secondary to surgery (Azoury et al., Citation2015). Surgical site infections (SSIs) are infections of the incision or organ or space that occur after surgery. Surgical patients initially seen with more complex comorbidities and the emergence of antimicrobial-resistant pathogens increase the cost and challenge of treating SSIs (Berríos-Torres et al, Citation2017).
In their study to assess the mortality impact of hospital-acquired post-operative sepsis up to 1 year after hospital discharge among adult non-short-stay elective surgical patients, Ou et al. (Citation2017) found that 144,503 survivors, 1857 (1.3%) had experienced post-operative sepsis.
According to the World Health Organization [WHO, n.d], the invasive nature of surgery introduces a high risk for the transfer of pathogens that may cause blood-borne infections in patients and/or the surgical team, including post-operative surgical site infection (SSI). This risk may be reduced by implementing protective barriers, such as wearing surgical gloves.
Again, Woelber et al. (Citation2016), concluded that Post-discharge Surgical Site Infections constitute the majority of these infections and pose a substantial disease burden for surgical patients globally and for different surgery types. Further examination is warranted to determine the methodological and clinical factors moderating the proportion of post-discharge SSIs. In fact, they found that the overall proportion of operations leading to Surgical Site Infection (a form of post-operative sepsis) was 9.9%. In a related study whose aim was to define the real burden of infectious complications after pancreaticoduodenectomy (post-operative sepsis), De-Pastena et al. (Citation2017) argued that infectious complications after pancreatico-duodenectomy (surgery for pancreas and duodenum) occur in about one-third of the cases. In their study, Meghraj et al. (Citation2017) concluded that surgical infections (post-operative sepsis) particularly, surgical site infections, have always been a major complication of surgery and trauma. The overall prevalence of surgical site wound infection in the surgical ward was 10.4%. They found that the proportion of males who had post-operative sepsis was slightly more than females. In a study by Gur et al. (Citation2015) in maternity ward, it was found that the Surgical site infection (Post-operative sepsis) rates varied from 2.9% to 30% in various studies. In a prospective observation study, it was found that the average incidence of SSI in mainland China was 4.5% (95% CI: 3.1–5.8) from 2001 to 2012 (Yunzhou et al., Citation2014).
A Facility-based retrospective observational study was carried out purposely to assess the prevalence of surgical site infections and associated risk factors among mothers who had delivery-related surgery. This was at the obstetric ward of Assela teaching referral hospital. A total of 384 women who had surgery for delivery were included in the study. The rate of surgical site infection was found to be 9.4% (36/384) (M. Teshager et al., Citation2017).
According to Ou et al. (Citation2017), out of 144, 503 survivors to discharge studied, 1857 (1.3%) had experienced post-operative sepsis. Their post-discharge mortality rates at 30 days, 60 days, 90 days, and 1 year were 4.6%, 6.7%, 8.1%, and 13.5% (vs 0.7%, 1.2%, 1.5%, and 3.8% in the non-sepsis cohort), respectively (P < 0.0001 for all).
2.2. Significance difference in proportions of post-operative sepsis
Overall, it is estimated that Surgical Site Infections (a form of post-operative sepsis) occur following 1–3.1% of all surgical procedures and account for approximately 2.0% of deaths due to healthcare-associated infections. With regard to abdominal surgery, the rate of wound infection may be much higher, with several prospective studies reporting an incidence of 15–25% depending on the level of contamination (Azoury et al., Citation2015). Some researchers found that surgical infections, particularly surgical site infections, have always been a major complication of surgery and trauma. The overall prevalence of surgical site wound infection in the surgical ward was 10.4% (Meghraj et al., Citation2017). There are, however, few literatures of this proportion and it’s believed that post-operative sepsis is more likely due to the surgical intervention. This view is supported by the work of Uçkay et al. (Citation2010). They coined that most Surgical Site Infections (post-operative sepsis) are believed to be acquired during surgery. This is supported by the success of SSI prevention measures directed towards activities in the operating theatre. However, despite much research on SSI, there are currently no data on the actual proportion acquired in the operating theatre versus post-operative care on the wards. Similarly, within the subgroup of SSIs acquired during surgery, the proportion originating from the patient versus that transmitted by the surgical staff, operating theatre procedure, or the environment remains unknown.
In maternity ward, on the other hand, it was found that the rate of surgical site infection after caesarean section ranges from 3% to 15%. This depends on the surveillance methods used to identify infections, the patient population, and the use of antibiotic prophylaxis. Majority of surgical site infections become apparent within 30 days of an operative procedure and most often between the 5th and 10th post-operative days. The Surgical site infection rates varied from 2.9% to 30% in various studies (Gur et al., Citation2015). Another study by Ashish et al. (Citation2014) found the Surgical Site Infection (post-operative infection) rate among the 720 patients investigated, to be 5%. Another maternity ward study in Ethiopia by M. Teshager et al. (Citation2017), found that out of a total of 384 women who had surgery for delivery, the rate of surgical site infection was 9.4% (36/384). In fact, according to
Things like hospital heating, ventilation and air-condition installations are said to be effective tools in the fight against nosocomial infections. These provide adequate indoor environmental conditions in hospitals, thus accommodating human health (Gonzalo & Justo, Citation2019). In a related study, it is argued that the choice of whether to use vertical or integrated approach in solving health problems is determined by the peculiarity of the challenges. They further added that vertical programs imply a variety of specific interventions which have not been fully integrated into the health system (Olayinka & Aanuoluwapo, Citation2020).
2.3. Lived experiences of patients who developed post-operative sepsis
In one study, the author asserted that patients with SSI experienced an unfolding situation, often initiated by extreme and sudden pain and profuse wound leakage, where they had to deal with significant physical and emotional distress while seeking an explanation of their symptoms. This was characterized in their literature as “suffering, not being taken seriously”; “waiting in discomfort”; and “searching for answers” (Currie et al., Citation2018). They argued that irrespective of infection or colonization type, there was low patient concern regarding the quality of interactions with Health Care Providers (HCPs). Not being taken seriously was highlighted by some patients with SSI, who knew there was something wrong but felt staffs were dismissive of their symptoms. Many patients had limited understanding of their illness or management and experienced frustration when trying to obtain information from HCPs (Currie et al., Citation2018).
One study found this complication resulted in an average excess length of stay of 26 days and 117,815 USD (USD) in additional charges; another study found an excess length of stay of 23.52 days and even higher excess charges of 261,173.3 USD (Agency for Healthcare Research and Quality, n.d)
A qualitative study by Tanner et al. (Citation2012) found that patients lacked overall awareness, concern and understanding of SSIs. For example, seven (7) patients didn’t know completely that they had SSIs and judging from patients’ accounts, staffs could have contributed to the lack of awareness by not informing patients of SSIs or downplaying their existence. The authors further noted that almost all of the participants were not concerned about the possibility of developing a wound infection following their surgery. Their experiences were quoted as below:
“The thought of an infection never even crossed my mind.
(participant 4)”
“It never entered my head. (participant 2)”
Another related study (Gelhorn et al., Citation2017) found similar results. All of the patients mentioned that the infection had impacted their physical functioning and daily activities. Most of the patients spoke about increased pain and numbness, described as “constant”, “severe”, “sharp” and “excruciating”. Many of them reported difficulties with the most basic aspects of physical functioning such as standing, walking and getting out of bed. One patient stated:
“Hip patient: ‘I was unable to do anything physically around the house, I had to pay someone to mow my lawn … yeah, it was horrible … I couldn’t have been prepared enough for it, I really didn’t realize it was going to be so bad’.”
These bad lived experiences are sometime aggravated by the limited knowledge of some HCPs. In fact, a study in Ethiopia, that the proportion of nurses who were knowledgeable about prevention of surgical site infection (post-operative sepsis) was found to be as low as 40.7%. This finding indicated that more than half of the nurses working in the two referral hospitals demonstrated inadequate knowledge on the prevention of surgical site infections, a finding in line with many of similar and related studies in Africa and western countries (F. A. Teshager et al., Citation2015).
Tartari et al. (Citation2017) concluded that the impact of post-operative sepsis (SSIs) both on patients and healthcare organizations is profound; therefore, efforts should focus on implementing diverse multidisciplinary prevention strategies. Patient engagement in preventing SSI might be an effective and useful strategy adding to the already existent surgical site care bundles.
According to Wound Source (Citation2018), post-operative sepsis, especially SSIs, are the most common and costly hospital-acquired infections. It is estimated to account for approximately 20% of all hospital-acquired infections and 38% of all post-operative complications. This equates to approximately 160,000 to 300,000 SSIs per year in the United States. They further argued that increases in hospital length of stay associated with SSIs range from 7 to 11 additional days. Patients with SSIs have a 2 to 11 times higher risk of death. Depending on the type of surgical procedure and type of infecting pathogen, the financial impact of SSIs is approximately 10 USD billion annually. Lakomkin et al. (Citation2016) also argued that post-operative sepsis is associated with high mortality and the national costs of septicemia exceed those of any other diagnosis.
Similarly, World Health Organization [WHO] (Citation2016) argued that surgical site infections are not just a problem for poor countries. In the United States, they contribute to patients spending more than 400 000 extra days in hospital at a cost of an additional US$ 900 million per year. Ou et al. (Citation2017) argued that post-operative sepsis is a leading cause of multiple organ dysfunction and in-hospital mortality. The U.S. Centre for Disease Control and Prevention reported that about 1 in 25 patients experience at least one healthcare-associated infection during hospitalization. Patients who are admitted with or who develop sepsis in hospital also have an increased risk of death following hospital discharge. Such sepsis-associated risk of death is higher than in the general population and remains higher for up to 5 years following hospital discharge. Above all, long-term healthcare costs for sepsis survivors are higher.
Ou et al. (Citation2017) stated that researchers in a recent study reported that 42.7% of severe sepsis survivors were re-hospitalized within 90 days incurring higher costs. This is especially in the first year after hospital discharge, when costs are approximately three times the costs in the following 2–3 years. Given such high prevalence, significant risk of mortality, poor prognosis, and high healthcare resource consumption, they argued that proposed “post-operative sepsis” is a key patient safety indicator, aiming to monitor potentially preventable surgical complications among elective surgical patients without serious medical conditions at admission.
A similar qualitative study revealed a lot of inconvenient experiences patients go through. For example, one patient reported as below:
“The strategy should be executed depending on the condition of the patient … people like these critically ill ones require being in the hospital for frequent monitoring by the doctors. But someone who does everything by herself, is strong … could be discharged to go and be injected at home if her guardian manages to inject so that she can perform other household chores.”
P9, Female patient, community-based care
This is just one of the many lived experiences patients have when they develop sepsis or even any other form severe and traumatizing illness (Cohen, et al. and Yang et al., Citation2018).
2.4. Determinants of post-operative sepsis
A study by Ellen et al. (Citation2013) found that risk factors consistently identified as associated with SSI included co-morbidities, advanced age, risk indices, patient frailty, surgery duration, and surgery complexity. In a retrospective study performed as part of the Surgical Quality Improvement Program, which included 136 respondents, similar results were found. It found that rates of developing sepsis varied among specialties. Indeed, the following factors attributed; the infection rates were higher in emergency procedures, procedures with long operative duration, more complex procedures, open wound dressing, bleeding disorders, and smoking, among others (Wound Source, Citation2018)
In their study of 93 consecutive patients who were prospectively included in the study, Mokart et al. (Citation2005) had no eligible patient excluded. All patients underwent tracheal extubation after surgery and yet 19 patients developed severe sepsis (sepsis group) from day 4 to day 9. The univariate analysis showed that male gender, Charlson comorbidity index, and ASA more than II (all preoperative factors) were significantly associated with post-operative severe sepsis.
In another study, Georgeto, et al. (Citation2011), of 648 surgical patients (mortality rate was 19.3%), the incidences of severe sepsis and septic shock were 6.6% and 12.7%, respectively. Multivariate analysis showed that the following variables were associated with sepsis: urgent surgery (OR = 6.92, 95% CI = 4.34 to 11.03), emergency surgery (OR = 5.36, 95% CI = 2.86 to 10.05), POSSUM physiologic variables (OR = 1.03, 95% CI = 1.01 to 1.06), POSSUM surgical variables (OR = 1.09, 95% CI = 1.05 to 1.13), mechanical ventilation (OR = 7.20, 95% CI = 3.78 to 13.71), and Sequential Organ Failure Assessment at ICU admission (OR = 1.13, 95% CI = 1.05 to 1.22). Lakomkin et al. (Citation2016), concluded that there is a significantly greater incidence of post-operative sepsis in the trauma cohort. Clinicians should be aware of these predictive characteristics, seek to counsel at-risk patients and consider addressing modifiable risk factors, such as hypertension and corticosteroid use preoperatively.
A study by Namba et al. (Citation2012) found the incidence of SSI was 0.51% (155 of 30,491). Patient factors associated with SSI included female gender, obesity, and the American Society of Anesthesiologists (ASA) score ≥3. Age, diagnosis, diabetes and race were not associated with SSI. The only surgical factor associated with SSI was a bilateral procedure. Surgeon and hospital volumes, use of antibiotic-laden cement, fixation method, laminar flow, body exhaust suits, surgical approach and fellowship training were not associated with risk of SSI. A comprehensive infection surveillance system, combined with techniques, identified patient and surgical factors associated with SSI. They recommended that obesity and chronic medical conditions should be addressed prior to Total Hip Replacement (THR).
Among elective surgical patients, post-operative sepsis is independently associated with increased post-discharge mortality up to 1 year after hospital discharge. This risk is particularly high in the first month, in older age patients and in the presence of severe/very severe co-morbidities (Ou et al., Citation2017).
A study by Ellen et al. (Citation2013) found a number of factors associated with post-operative sepsis, and they are increased surgery duration, increased length of stay, surgical complexity, and emergency surgery, among others.
In this study (Ellen et al., Citation2013), a number of estimates failed to achieve statistical significance, although a large majority of unadjusted and adjusted point estimates indicated certain trend towards increased risk. Co-morbidities were consistently found to be associated with SSI incidence. The most frequently considered comorbidity was diabetes, which was included in 13 adjusted analyses, and 85% of these reported a statistically significant association. They argued that 10 studies considered risk factors describing patient dependence and frailty, which were characterized in a variety of ways, including independence and activities of daily living, incontinence and admission from a long-term healthcare facility. The majority of these factors were only considered in unadjusted analyses; adjusted estimates include an odds ratio for SSI of 4.35 (95% CI: 1.64–11.11) associated with admission from a long-term health facility and an odds ratio for SSI of 2.75 (95% CI: 1.16–6.46) associated with requiring assistance with three or more activities of daily living. Variables describing the complexity and/or duration of surgery were also found to be associated with the risk of SSI in 16 studies. Duration was defined either relative to a cut-point (example; 75th percentile, 120 minutes, 180 minutes), as a continuous measure per minute of surgery, or as a multi-level categorical variable. Across definitions, increased duration of surgery was consistently found to be associated with increased risk of SSI. When results were restricted to 16 studies that used a binary cut-point to compare shorter vs. longer surgeries, 15 of 16 estimates suggested an increased risk of SSI for longer surgeries; 11 of these were statistically significant, with estimated odds ratios ranging from 1.2 to 3.8 with a median value of 2.3. Pre-operative length of stay was identified as a significantly associated risk factor for SSI in 12 studies. Odds ratios for SSI per additional day of pre-operative stay ranged from 1.0 to 2.0, with a median of 1.1. Odds ratios associated with surgeries requiring a prior overnight stay were estimated to be 1.4 and 4.6. One study found that pre-operative hospitalizations of up to 7 days were not associated with a significant risk of SSI, but that pre-operative stays of 8 days or longer were associated with an approximate 10-fold increased risk of SSI (Ellen et al., Citation2013). In another study, however, Todd et al. (Citation2009), concluded that sepsis and death were more likely after non-elective than elective surgery.
Most cases of sepsis are predominantly caused by bacterial infection. Cheng et al. (Citation2008) asserted that sepsis is a progressive injurious process resulting from a systemic inflammatory response to infection. In developed countries, sepsis is an important cause of mortality: in the United States alone, up to 750,000 people annually suffer from severe sepsis—mostly bacterial in aetiology—of whom 29% may die. The authors came up with a number of possible interventions for the management of sepsis in Resource-Constrained settings. These range from strategies on how to do it to antibiotic therapy and source control.
2.5. Post-operative infection control strategies
Finding ways to improve outcomes for sepsis patients is a high priority for health systems across the United States. Horstmeier (Citation2015), asserts that the health system needs to reduce sepsis for many reasons, including:
Sepsis costs lives - 2014 report from the Advisory Board revealed that sepsis contributes to more than 17% of hospital deaths.
Sepsis adds significant costs to care - The 2011 Healthcare Cost and Utilization Project (HCUP) report from the Agency for Healthcare Research and Quality identifies sepsis as the most expensive condition that hospitals treat, costing 20.3 USD billion in 2011 alone.
High sepsis rates lead to financial penalties – It is said that a ruling was passed under the hospital-acquired condition (HAC) reduction program to encourage providers to improve their post-operative sepsis care. The ruling, which took effect in October 2014, levies financial penalties on hospitals with high post-operative sepsis rates.
One study also that found this complication (from sepsis) resulted in an average excess length of stay of 26 days and 117,815 USD (USD) in additional charges; another study found an excess length of stay of 23.52 days and even higher excess charges of 261,173.3 USD (Agency for Healthcare Research and Quality, n.d). Good post-operative infection control might help improve on a number of health outcomes, such as reduced mortality, improved safety of care, reduced readmissions, good patient experience, improved effectiveness of care, timeliness of care and efficient use of medical imaging, among others (Tinker, Citation2018). The author defines an outcome measure as a “change in the health of an individual, group of people, or population that is attributable to an intervention or series of interventions.” Outcome measures (mortality, readmission, patient experience, etc.) are the quality and cost targets healthcare organizations should try to improve. World Health Organization [WHO], Citationn.d.a, 2007 & 2009 approves of a number of hygiene practices that need to be adopted for use in hospitals. These practices range from hand washing to isolation of contaminated patients, among others.
Avenue Hospital (n.d), for example, work with community, including staff, patients and visitors, to protect all from transmission of infectious agents. They achieve this through staff and patient education, promotion of hand hygiene to all, stringent surveillance, staff immunisation, and implementation of evidence-based infection control interventions. Infection rates are benchmarked against other private and public hospitals using the Australian Council on Healthcare Standards Clinical Indicator program and remain consistently low when compared with other rates throughout Australia. According to Hughes et al. (Citation2013), when infection control audits are undertaken and adherence to infection control standard maintained, reduced infection rates will be realized.
The ”Global Guidelines for the Prevention of Surgical Site Infection” includes a list of 29 concrete recommendations distilled by 20 of the world’s leading experts from 26 reviews of the latest evidence. The recommendations are designed to address the increasing burden of healthcare associated infections on both patients and healthcare systems globally. In fact, World Health Organization [WHO] (Citation2016) asserts that “No one should get sick while seeking or receiving care.” Their guideline has 13 recommendations for the period before surgery, and 16 for preventing infections during and after surgery. They range from simple precautions, such as ensuring that patients bathe or shower before surgery and the best way for surgical teams to clean their hands, to guidance on when to use antibiotics to prevent infections, what disinfectants to use before incision and which sutures to use. Health Catalyst (2018) also asserts that the sepsis improvement team needs to be in place and continues to meet regularly. To support ongoing improvement and dissemination of the most recent evidence-based guidelines, they convened journal clubs to evaluate new evidence and continues to refine the sepsis protocol to align with new evidence, or when new trends are identified in the data. This strategy helped them in keeping sepsis at the forefront of clinicians’ minds (Health Catalyst, 2018). The timely and appropriate use of antibiotics in the early management period is associated with less survival of sepsis and pneumonia (Cheng et al., Citation2008).
Just like WHO strategies, four (4) infection prevention and process improvement experts weigh-in on 10 best strategies for prevention of infections. These include Hand Hygiene, Environmental hygiene, Screening and cohorting patients, Vaccination, Surveillance, Antibiotic stewardship and care coordination. The others are following the evidence, appreciating all the departments that support the infection prevention program and lastly Comprehensive Unit-based Safety Programs (Anuja, Citation2013).
3. Methodology
3.1. Study design
The design was Unmatched Retrospective Cohort study of post-operative patients admitted in Maternity and General Surgical ward for the past 6 months. It is taken both qualitatively and quantitatively in comparative dimension. The two cohorts from the two departments were compared for their exposure (surgery) and the outcome thereafter (post-operative sepsis).
The choice of the design was based on the fact that retrospective design is a very time efficient and elegant way of answering new questions with existing data. It is further argued that the major advantage of cohort studies in general is the possibility to study multiple exposures and multiple outcomes in one cohort. This study had multiple exposures and outcomes ( , sub-section 3.8 of this report). Even rare exposures can be studied, for the index group can be selected on this exposure. Besides, the combined effect of multiple exposures on disease risk can be determined (Euser et al., Citation2009).
Table 1. Table of study variables used
3.2. Study population
The study populations were post-operative patients admitted to Maternity and General Surgical wards at Gulu Regional Referral Hospital in the past 6 months, between May 2018 and November 2018.
3.3. Study unit
The unit of the study involved a post-operative patient admitted to the Maternity and General Surgical wards of Gulu Regional Referral Hospital in the past 6 months, between May 2018 and November 2018.
3.4. Inclusion and exclusion criteria
Inclusion Criteria: The respondents were included in the study only when they were admitted either to the Maternity ward or General Surgical ward within the past 6 months, between May 2018 and November 2018. They all needed to have undergone surgery (operation) within the said period of admission.
Exclusion Criteria: The respondents were excluded from the study when they were admitted either to the Maternity ward or General Surgical ward outside the past 6 months, between May 2018 and November 2018. They were also excluded if they never underwent any surgery (operation) or underwent surgery outside the said time period.
3.5. Sample size determination
The formula for the calculation of sample size (n) when population size(N) is known, was used to determine the sample size for both group of respondents from Maternity and General Surgical ward. This gave proportionate samples for the respective groups,
This is Taro Yamane formula (1967:886) and it provides a simplified formula to calculate sample sizes (Israel, Citation1992; Polonia, Citation2013). Assuming a 95% confidence level and maximum degree of variability of the attributes in the population, P = 50% (0.5), the sample size was calculated as below:
Thus, using the formula; n =
Where n is the sample size, N is the population size and eis the level of precision (Sampling error—5%).
Note that the degree of variability in the attributes (P) being measured refers to the distribution of attributes in the population. The more heterogeneous a population, the larger the sample size required to obtain a given level of precision. The less variable (more homogeneous) a population, the smaller the sample size. Hence, a proportion of 50% indicates a greater level of variability than either 20% or 80%. This is because 20% and 80% indicate that a large majority do not or do, respectively, have the attribute of interest. Because a proportion of .5 indicates the maximum variability in a population, it is often used in determining a more conservative sample size, that is, the sample size may be larger than if the true variability of the population attribute were used (Israel, Citation1992; Polonia, Citation2013).
Thus;
Maternity ward samples (n1): n1 = =
=168.786 ≈ 169respondents
General Surgical ward samples (n2): n2 = =
= 244.358 ≈ 245 respondents
Eight (8) respondents were purposively selected to ascertain the lived experiences. Three (3) of them were from maternity ward and the rest were from general surgical ward.
3.6. Sampling procedures
A systematic probability sampling method was used to select the patient files of the respondents for both cohorts. The files were arranged in serial order and a starting point for the first respondent file was determined by a simple random technique. Every third (3rd) file was then selected to be in the sample. The process was repeatedly done until all the required number of samples were obtained for the respective cohorts. From the qualitative samples, eight (8) respondents on either side were randomly picked and traced to their homes to obtain their lived experiences. Three (3) of the respondents were from maternity ward whereas five (5) were from the general surgical ward.
3.7. Research variables
The independent variables were “respondent underwent surgery and determinants of post-operative sepsis” whereas the dependent (outcome) variables were mean proportion of post-operative sepsis, differences in proportion of post-operative sepsis, and lastly lived experiences among those who had post-operative sepsis.
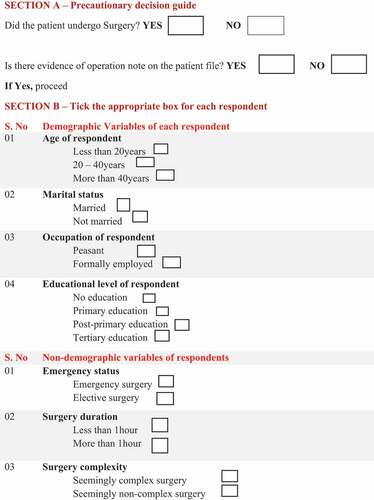
The determinants of sepsis studied ranged from demographic to non-demographic variables. The demographic variables were age group, marital status, occupation and educational levels of respondents. The non-demographic variables were Surgery duration, Surgery complexities, Average length of stay (ALOS) and emergency status (emergency versus elective surgeries). See .
3.8. Data collection sources, tools and techniques
Data Sources: Both secondary and primary data were used. The secondary data from patient files (hospital record) for the past 6 months from May 2018 to November 2018 were retrieved. These were the records of patients admitted to Maternity and General Surgical wards and who underwent surgery. Only these categories were analysed for both cohorts. The use of secondary data in this study is justified based on the generation of new insights and possible longitudinal study among other advantages. It also provides the basis for comparison between departments, as described by the Management Study Guide (2019).
However, eight (8) respondents (three from the maternity ward cohort and five from each general surgical ward cohort) were traced to their homes and primary data on their lived experiences was collected. This choice is in line with a similar qualitative study by Yang et al. (Citation2018).
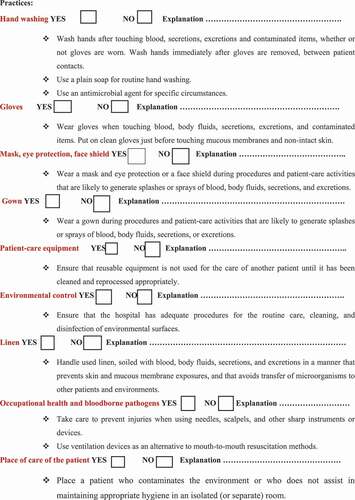
Data Collection Tools and Techniques: The researcher used Data abstraction Sheet (Document Review Guide), Observation guide, and Interview Guide (for the primary data) tools. Data Abstraction Sheet has been used in a number of studies (Centre for Disease Control and Prevention, Denver, Long Beach and San Francisco, 2004). This Data Abstraction Sheet used had all the types of data that needed to be extracted from each respondent record written on it. This made it easier for the researcher to obtain the needed data per patient record. The researcher used this Sheet as a guide to extract the appropriate data patient-by-patient. This also served as an observation guide for each patient record/file. Additional observation guide was developed and used by the researcher to observe the hygiene practices in the two hospital departments. This guide had all the observatory areas clearly labelled.
Likewise, the Interview guide was used to collect data on lived experiences of the respondents. It guided the researcher in knowing which questions to ask. Data were then handwritten as well as video recorded for later analysis. Probing was done to dig deeper into the respondents’ experiences.
3.9. Data analysis and presentation methods
The data generated were then entered into Microsoft Excel and Statistical Package for Social Sciences (SPSS) software of a computer for analysis. With the use of these software, analysis was made easier. Quantitative calculation for testing hypothesis was done manually. Likewise, the qualitative data were coded, transcribed and content analysis done.
The data were then mathematically presented, as well as using tables and graphs.
3.10. Quality control measures
In evaluating the measurement methods, the researcher considered two general dimensions: reliability and validity.
Reliability: Reliability refers to the consistency of a measure. According to Price et al. (Citation2018), researchers consider three types of consistency: over time (test–retest reliability), across items (internal consistency) and across different researchers (inter-rater reliability). This study, however, focused on internal consistency and test–retest reliability. Assessing test–retest reliability requires using the measure on a group of people at one time, using it again on the same group of people at a later time and then looking at test–retest correlation between the two sets of scores. For this study, pre-testing and retesting of the construct was done to ascertain the reliability, without test correlation. Similarly, internal consistency, which is the consistency of people’s responses across the items on a multiple-item measure, was done. The data generated were double-checked for completeness, appropriateness and correctness before entering in the Microsoft Excel Sheet and Statistical Package for Social Sciences (SPSS) for analysis. After entry, another counter-check was made.
Validity: Validity is the extent to which the scores from a measure represent the variable they are intended to. Researchers need to make this judgment. They consider one factor that they take into account—reliability. When a measure has good test–retest reliability and internal consistency, researchers should be more confident that the scores represent what they are supposed to (Price et al., Citation2018). There are three basic kinds: face validity, content validity, and criterion validity. Face validity is the extent to which a measurement method appears “on its face” to measure the construct of interest. Content validity is the extent to which a measure “covers” the construct of interest. For this study, therefore, both face and content validity checks were ensured by the researcher. For the qualitative data, repeated replay was made to appreciate the information and make substantive meaning out of it, that is, content checking. This enabled the development of the appropriate thematic areas (Yang et al., Citation2018)
4. Results
4.1. Demographic characteristics of persons studied
The demographic characteristics of the two cohorts of respondents were summarized as shown in .
Table 2. Socio-demographic characteristics of respondents
From , for both categories of cohorts, majority of the respondents were in the age group 20–40 years accounting 46.7% and 42.4% for Maternity ward and General Surgical ward in that respective order. However, for Maternity ward, this was followed by the age group more than 40 years (29%) whereas for General Surgical ward, the group less than 20 years followed (29.4%). Most of the respondents in either cohort were married, 93.5% and 62.4% for Maternity and General Surgical ward, respectively. Few of the respondents were formally employed, accounting 31.4% and 22.9% for Maternity and General Surgical ward in that order. For Maternity ward, most of the respondents either completed primary education or post-primary education, each standing at 26.6%. For the group in General Surgical ward, majority (42%) had primary education followed by no education (27.3%).
4.2. The mean monthly proportion of post-operative sepsis in maternity & GSW
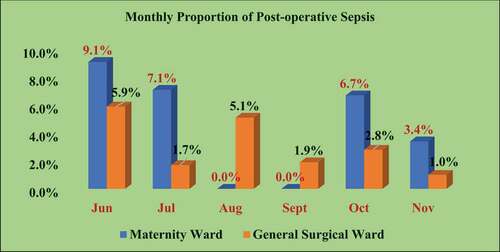
From the respondents’ in-patient records, data were extracted about their post-operative diagnosis before discharge. The total number of post-operative sepsis managed was then computed for each month. The mean proportion, for the past 6 months, was then calculated for each cohort of respondents drawn from the Maternity and General Surgical ward (GSW). The results are shown in .
Generally, the monthly proportion of post-operative sepsis was higher in Maternity ward compared to General Surgical ward, except for the months of August and September where Maternity ward had no post-operative sepsis and General Surgical had 5.1% and 1.9%, respectively (Refer to ).
Therefore, following from , the mean proportion of post-operative sepsis was calculated as below:
Monthly Mean Proportion for Maternity ward = =
= 4.38333333 ≈ 4.4%
Monthly Mean Proportion for General Surgical ward = =
= 3.06666666667 ≈ 3.1%
Therefore, the study found the mean proportion of post-operative sepsis to be 0.044 (4.4%) and 0.031 (3.1%) for Maternity ward and General Surgical ward, respectively.
4.3. Significant difference in the proportion of post-operative sepsis
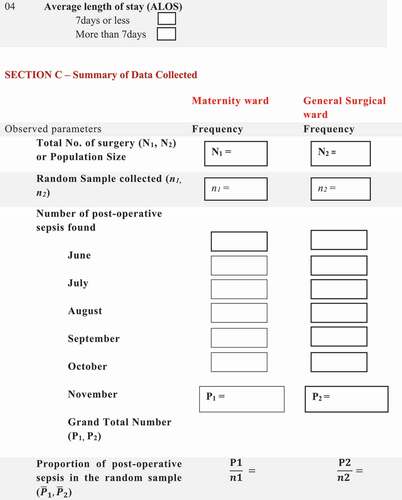
Hypothesis testing (comparison of two proportions), assuming normal distribution, was done to test whether there was a significant difference in the proportion of post-operative sepsis between Maternity and General Surgical wards. Out of total number (292) of surgeries conducted within the study period in maternity ward, a random sample of 169 was selected. From this random sample, 13 post-operative sepsis cases were found. Similarly, out of total number (628) of surgeries conducted within the study period in General Surgical ward, a random sample of 245 respondent files was selected. From this random sample, 18 post-operative sepsis cases were found. The data collected for the two groups of cohorts were summarized as per ;
Table 3. Summary of data collected for hypothesis testing
Step1: Stating Null (HO) and Alternative (H1) hypotheses
HO: 1—
2 = 0 (There is no difference between the proportions)
H1:1—
2
0 (There is significant difference between proportion of post-operative sepsis between Maternity and General Surgical ward)
Step 2: Significant level
The significant level is 0.05 (
Step 3: Calculating critical value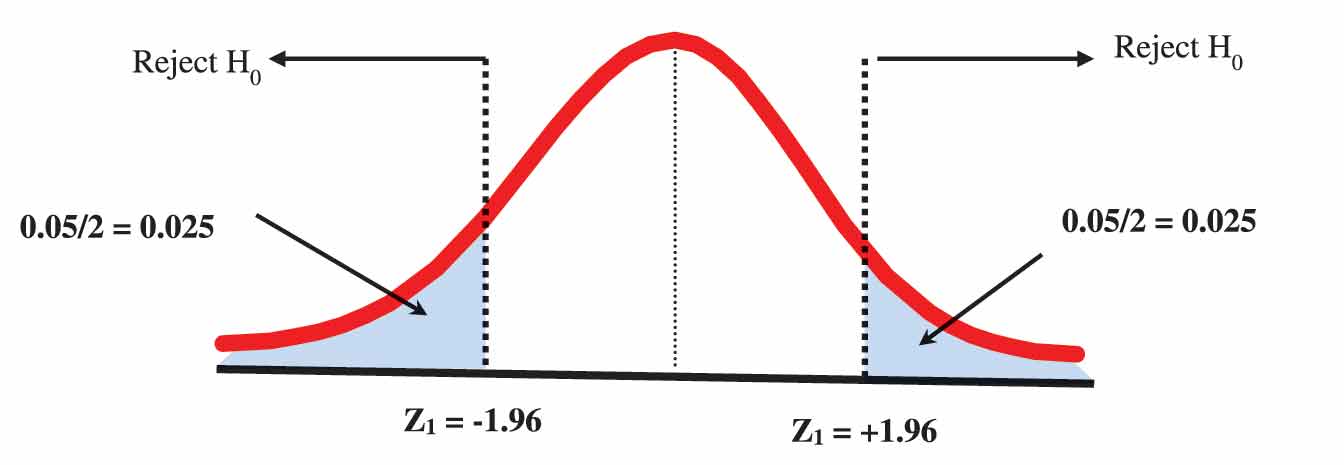
Given that , and looking for the value of Z1 under the Z—Score table, we get Z1 =
1.96
Step 4: Calculating the test statistic (Z2)
Z2 = (i)
Where P = Pooled estimate of overall proportion and calculated as below:
P = (ii)
From equation (ii) above, we compute P
∴P = =
= 0.07488
Now we calculate Z2 from equation (i) as follows:
Z2 = =
=
= 4.981 ≈ 4.98
∴ Z2 = 4.98
Step 5: Comparing the test statistic (Z2) with critical value (Z1)
Since Z2 (4.98) Z1 (1.96), falling in the rejection region, we reject Ho
Step 6: Conclusion
There was significant difference in the proportion of post-operative sepsis between Maternity ward and General Surgical wards of Gulu Regional Referral Hospital.
The proportion of post-operative sepsis is higher in maternity ward than in the General Surgical ward).
4.4. Determinants of post-operative sepsis in maternity and GSW
The results on both wards have been summarized as below. The demographic and non-demographic variables were analysed using binary logistic regression and cross tabulation
4.3.1: Maternity Ward: Cross tabulation and binary logistic regression in bivariate analysis were done to determine the major determinants of post-operative sepsis in the Maternity ward. The results as shown in showed statistical significance for only one variable, marital status. Therefore, the risk of post-operative sepsis was more (27.3%), among those respondents who were not married (p = 0.023, COR = 5.550 [1.272–24.219] at 95% CI). Whereas other factors, such as surgery duration more than 1 hour (8.0%), complex surgery (9.7%), emergency surgery (9.0%), and average length of stay more than 7 days (8.2%) could have contributed to post-operative sepsis, findings were not statistically significant.
Table 4. Summary of bivariate binary logistic regression analysis in maternity ward respondents
Abbreviations: CI = Confidence Interval, COR = Crude Odds Ratio, AOR = Adjusted Odds Ratio, **Statistically significant & variable used in multivariate analysis,*Not statistically significant &Variable used in multivariate analysis
However, at multivariate binary logistic regression analysis, age group remained statistically not significant (p = 0.095, Adjusted OR = 0.481[0.204–1.137] at 95% CI) as shown in .
Table 5. Summary of multivariate binary logistic regression analysis in maternity ward respondents
4.3.2: General Surgical Ward (GSW): Cross tabulation and binary logistic regression in bivariate analysis was done to determine the major determinants of post-operative sepsis in the General Surgical ward. The results, as shown in , showed statistical significance for two variables, surgery complexity and emergency status of surgery. Therefore, emergency surgery (11.9%) and complex surgeries (16.3%) carried more risk of post-operative sepsis (p = 0.029, COR = 0.322 [0.117–0.89] and p = 0.001, COR = 7.535 [2.396–23.697] 95% CI) respectively.
Table 6. Summary of bivariate binary logistic regression analysis in GSW
Emergency status and occupation of respondents were then run in multivariate analysis. There was no significant finding for the occupation of respondents at this level of analysis (p = 0.13, Adjusted OR = 0.457 [0.166–1.1258] at 95% CI). However, not being married (8.7%), age group more than 40 years (11.6%), no education (9.0%), and complex surgery (16.3%), among other factors, could have increased the risk of post-operative sepsis but the results were not statistically significant. Refer to
Abbreviations: CI = Confidence Interval, COR = Crude Odds Ratio, AOR = Adjusted, GSW = General Surgical Ward.
Odds Ratio, **Statistically significant& variable used in multivariate analysis,*Not statistically significant & variable used in multivariate analysis
Using observation checklist, an observation of hygiene practices in both wards was done by the researcher. It was found that whereas hand washing culture exists, the level of practice was still low. Similarly, the wards had limited isolation rooms for highly infectious patients.
4.5. Lived experiences of patients who developed post-operative sepsis
Four females and four male respondents aged between 25 and 50 years (median 37 years) were interviewed to ascertain their lived experiences from both cohorts. Six (6) of the patients were married, one separated and one was single. All the respondents at least had a child. Four of them were currently employed, while another four (4) were unemployed. Five of the respondents were admitted in General Surgical ward whereas three (3) were admitted to the Maternity ward. See .
Table 7. Characteristics of respondents who shared their lived experiences
Themes were developed through reading, analysis, reflection and classification of the data. This thematic analysis of the interviews resulted in four themes: “experiences related to the pain”, “experiences related to financial cost”, “thoughts and feelings of dying” and “dealing with discomfort”. The themes are further described below. The respondents, drawn from either cohort, who had post-operative sepsis were traced and qualitatively probed to shared their lived experiences. They were coded 1, 2, 3, 4, 5, 6, 7 & 8. Content analysis of their experiences was done and reported as per the respective them developed.
4.5.1. Theme 1 -Experiences related to pain
All the respondents experienced a lot of pain following the development of post-operative sepsis. Two of the respondents from the Maternity ward, who developed post-operative sepsis, were the first to be traced back to their homes and asked to share their lived experiences following the sepsis. Both of them had their unexpected painful experiences. One of them reported as below:
“ … Yeah, my hospital experience was really not nice. I never thought that I would take long in the hospital or even be operated. Because I went expecting to deliver normally but along the way I was told by the midwife that I needed to be operated or else my baby will die. After surgery, I thought I would just take a few days in hospital but I ended up staying for long. The pain was too much. But I had nothing to do about as … .”,[Reports, Respondent 3].
The second respondent reported as:
“ … . For me, my wound healed well at first and I was discharged home within 1 week. But when I stayed at home for another 2 weeks, I got very sharp pain at the operation site. When I squeezed, I saw pus. I hurried to the hospital where they washed the wound and gave me more medicine to be taking from home. This time … .”,[Said, Respondent 6].
Similar painful experiences were also reported by the rest of the respondents, including those from the general surgical ward.
4.5.2. Theme 2 -Experiences related to financial cost
As expected, all the eight (8) respondents reported some significant degree of exaggerated cost incurred in the treatment of their wound.
“ … . This was because I had infection of the area … … It increased my overall financial cost although I cannot tell how much … .”,[Reports, Respondent 1].
Another respondent associated the increased cost with having to personally buy some requirements (supplies) from nearby private clinic. Two respondents from General Surgical ward who were later traced for their experiences reported likewise. They had similar experiences as their counterparts from the Maternity ward. However, one of them had some unique experience related to higher financial cost associated with full recovery.
“ … . sometimes I would buy my own medicine and it was very expensive for me since I also didn’t have enough money. My children also needed money from me for school fees at the same time. Things were not easy. But anyway, … .”[Reports, Respondent 4].
Respondent 8 attributed the cost to his other social aspect of life. All the respondents could not quantify the financial cost they incurred in seeking treatment. They could not also relate with how much they would incur if they never had sepsis.
4.5.3. Theme 3 -Experiences related to thoughts and feelings of dying
When asked to share their thoughts and feelings, one respondent who recovered fully had this to say:
“ … Eh! Don’t even remind me. I never thought I would survive. I thought I would die. You see me like this but I came from very far. Very far, eh! … .” [said Respondent 7]
Most of the respondents were, however, hopeful of survival. They never thought of dying even if they had post-operative sepsis (respondents 1, 2, 3, 4, 5, 6 & 8).
4.5.4. Theme 4—Dealing with general discomfort
The event was very discomforting to all the respondents. Many of the respondents thought their infections were simple rashes or wound healing process that was itchy or allergic reactions (respondents 1, 2, 4, 5, 7 and 8). One respondent thought he was having a burst abdomen (respondent 1).
“ … . I never thought it was wound infection. For me, I thought that my abdomen was bursting because of the continued swelling of my abdomen after the surgery. This made me … .” [Respondent 1]
Six respondents were not aware that they had an infection at all, not until they were told by the healthcare providers attending to them.
Therefore, the lived experiences of the patients were more or less similar, irrespective of the cohort from which they were. This qualitative finding is similar to many other researchers.
4.6. Summary of results
The study found the mean proportion of post-operative sepsis to be 0.044 (4.4%) and 0.031 (3.1%) for Maternity ward and General Surgical ward, respectively.
Since Z2 (4.98) Z1 (1.96), falling in the rejection region, the null hypothesis (Ho) was rejected. Therefore, there was a significant difference in the proportion of post-operative sepsis between the Maternity ward and General Surgical wards of Gulu Regional Referral Hospital. In fact, the proportion of post-operative sepsis is higher in maternity ward (4.4%) than in the General Surgical ward (3.1%).
Cross tabulation and binary logistic regression in bivariate analysis were done to ascertain the major determinants of post-operative sepsis in the Maternity and General Surgical wards. For Maternity, the result showed statistical significance for marital status. Therefore, the risk of post-operative sepsis was more (27.3%), among those respondents who were not married (p = 0.023, COR = 5.550 [1.272–24.219] at 95% CI). Other factors such as surgery duration more than 1 hour (8.0%), complex surgery (9.7%), emergency surgery (9.0%), and average length of stay more than 7 days (8.2%) could have contributed to post-operative sepsis but findings were not statistically significant. Likewise, for General surgical ward, the results showed statistical significance for two variables, surgery complexity and emergency status of surgery. Therefore, emergency surgery (11.9%) and complex surgeries (16.3%) carried more risk of post-operative sepsis (p = 0.029, COR = 0.322 [0.117–0.89] and p = 0.001, COR = 7.535 [2.396–23.697] 95% CI) respectively. However, whereas not being married (8.7%), age group more than 40 years (11.6%), no education (9.0%) and complex surgery (16.3%), among other factors, could have increased the risk of post-operative sepsis, the results were not statistically significant.
Using an observation checklist, an observation of hygiene practices in both wards was done. It was found that whereas hand washing culture exist, the level of practice was still low. Similarly, the wards had limited isolation rooms for highly infectious patients
The lived experiences of the patients were related to the fact that they never expected to develop sepsis post-operatively but also incurred additional painful financial cost to recover from the infections.
5. Discussion
This study found the mean proportion of post-operative sepsis to be 0.044 (4.4%) and 0.031 (3.1%) for Maternity ward and General Surgical ward, respectively. Woelber et al. (Citation2016), found that the overall proportion of operations leading to Surgical Site Infection (a form of post-operative sepsis) was 9.9%. In another study, Meghraj et al. (Citation2017) concluded that the overall prevalence of surgical site wound infection in the surgical ward was 10.4%. In a study by Gur et al. (Citation2015) in maternity ward, it was found that the Surgical site infection (Post-operative sepsis) rates varied from 2.9% to 30% in various studies. However, in a prospective observational study, it was found that the average incidence of SSI in mainland China was 4.5% (95% CI: 3.1–5.8) from 2001 to 2012 (Yunzhou et al., Citation2014). Another study in maternity ward in Ethiopia by M. Teshager et al. (Citation2017), found that out of a total of 384 women who had surgery for delivery, the rate of surgical site infection was 9.4% (36/384).
This study found the risk of post-operative sepsis in maternity wards was higher among those respondents who were not married at 27.3%. Likewise, for General surgical ward, emergency surgery (11.9%) and complex surgeries (16.3%) carried more risk of post-operative sepsis. This result is similar to a study by Ellen et al. (Citation2013) who found a number of factors associated with post-operative sepsis. Therefore, all-in-all, the findings of this study are consistent with other studies but interestingly on the lower margin of the proportions found in other studies.
The qualitative lived experiences found were also similar to those found elsewhere. A related study (Gelhorn et al., Citation2017) found similar results. All of the patients mentioned that the infection had impacted their physical functioning and daily activities. Most of the patients spoke about increased pain and numbness, described as “constant”, “severe”, “sharp” and “excruciating”. One patient stated:
“Hip patient: ‘I was unable to do anything physically around the house, I had to pay someone to mow my lawn … yeah, it was horrible … I couldn’t have been prepared enough for it, I really didn’t realize it was going to be so bad’.”
These bad lived experiences are sometime aggravated by the limited knowledge of some Health Care Providers (HCPs). In fact, a study in Ethiopia found that the proportion of nurses who were knowledgeable about prevention of surgical site infection (post-operative sepsis) was found to be as low as 40.7% (F. A. Teshager et al., Citation2015).
6. Conclusion
The proportion of post-operative sepsis is low at Gulu Regional Referral Hospital, falling on the lower margin of the proportions found by many other researchers. However, there is a significant difference in the proportion of post-operative sepsis between the Maternity ward and General Surgical ward. The proportion is higher in Maternity ward. The risk of post-operative sepsis in maternity ward was more among those respondents who were not married at 27.3%. Likewise, for General surgical ward, emergency surgery (11.9%) and complex surgeries (16.3%) carried more risk of post-operative sepsis.
7. Recommendation
Based on the findings and conclusion of this study, the researcher makes the following recommendations:
Whereas the proportion of post-operative sepsis is lower at Gulu Regional Referral Hospital, the hospital still needs to do more infection controls to bring this proportion even lower. This requires strict adherence to infection control model developed by this study, which in essence, is similar to the WHO perspective.
Maternity ward needs to learn and adapt, as well as share good practices with General Surgical ward so as to complement each other on improving infection prevention and control
A similar follow-up comparative study needs to be done to check for progress made in the level of infection prevention and control in the two hospital departments, preferably after a year of dissemination of this finding
Periodic/Continuous Professional Development or Continuous Medical Education must be required on this subject matter
Departmental staffs need to take on proactive roles to improve infection controls in the hospital.
Active patient engagement may be needed to reduce post-operative sepsis in the hospital
Consent for publication
The authors do consent for publication of this article under open access journal. Copy rights are reserved.
Acknowledgements
The author does acknowledge and appreciate the corporation of management of Gulu Regional Referral Hospital for the supportive environment accorded while this research was being conducted. I acknowledge the tremendous supervision and guidance by Prof. John Charles Okiria of Clark International University, Faculty of Health Sciences. Special appreciations go to all my respondents, without whom this research would not be possible.
Disclosure statement
The authors declare no conflict of interest
Additional information
Funding
Notes on contributors

Omona Kizito
Dr Omona Kizito is a Medical Doctor and Lecturer in the Faculty of Health Sciences (FHS) at Uganda Martyrs University, Kampala. He holds a PhD in Mgt [Healthcare Mgt], Master of Science in Health Services Mgt (MSc. HSM), Master of Science in Monitoring and Evaluation (MSc. M & E), Post Graduate Diploma in Project Planning and Mgt (PGD PPM), Post Graduate Certificate in Project Monitoring and Evaluation (PGC M & E), and Bachelor of Medicine and Bachelor of Surgery (MBChB) degree. He is currently engaged in teaching Public Health and Health Services Management at graduate and postgraduate levels, Research Supervision in the said areas and levels and community engagement, among others.
His major research areas are: Clinical Research, Public Health, Maternal and Child health
Researches, Health system research, and others.
References
- Anuja, V. (2013). 10 best strategies for infection prevention and control [blog post]. Available at: https://www.beckershospitalreview.com/quality/10-best-strategies-for-infection-prevention-and-control.html
- Ashish, P., Erika, A. S., Shailendra, S., Vijay, K. M., Harshada, S., & Cecilia, S. L. (2014). Incidence and factors associated with surgical site infections in a teaching hospital in Ujjain, India. American Journal of Infection Control, 42(2014). Available at: https://www.ajicjournal.org/article/S0196-6553(13)01092-4/pdf
- Avenue Hospital. (n.d.) Infection control prevention strategies [blog post]. Available at https://www.theavenuehospital.com.au/For-Patients/Infection-Control-Prevention-Strategies
- Azoury, S., Farrow, N., Hu, Q., Soares, K., Hicks, C., Azar, F., Rodriguez-Unda, N., ...Nguyen, H. and Eckhauser, F. (2015). Postoperative abdominal wound infection – Epidemiology, risk factors, identification and management. Chronic Wound Care Management and Research, 2015 (2). pp. 137–31. https://doi.org/https://doi.org/10.2147/CWCMR.S62514.
- Berríos-Torres, et al.(2017).Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surgery, 1521, 784–791.https://doi.org/https://doi.org/10.1001/jamasurg.2017.0904.
- Centre for Disease Control and Prevention [CDC]. (2009). CDC definitions for surgical site infection surveillance [Pdf on-line]. Available at: https://www.hpsc.ie/a-z/microbiologyantimicrobialresistance/infectioncontrolandhai/surveillance/surgicalsiteinfectionsurveillance/casedefinitions/File,3058,en.pdf
- Cheng, A. C., West, T. E., Limmathurotsakul, D., & Peacock, S. J. (2008). Strategies to reduce mortality from bacterial sepsis in adults in developing countries. Plos, 5(8). doi: https://doi.org/10.1371/journal.pmed.0050175.
- Cohen, D. B., Phiri, M., Banda, H., Squire, S. B., Namakhoma, I., & Desmond, N. (2018). A qualitative evaluation of hospital versus community-based management of patients on injectable treatments for tuberculosis. BMC Public Health, 18(1), 1127. https://doi.org/https://doi.org/10.1186/s12889-018-6015-3
- Currie, K., Melone, L., Stewart, S., King, C., Holopainen, A., Clark, A. M., & Reilly, J. (2018). Understanding the patient experience of health care–associated infection: A qualitative systematic review. American Journal of Infection Control, 46 (8), 936–942.https://doi.org/https://doi.org/10.1016/j.ajic.2017.11.023.
- De-Pastena, M., Paiella, S., Marchegiani, G., Malleo, G., Ciprani, D., Gasparini, C., Secchettin, E., Salvia, R., & Bassi, C. (2017). Postoperative infections represent a major determinant of outcome after pancreaticoduodenectomy: results from a high-volume center. Surgery, 162 (4), 792–801. https://doi.org/https://doi.org/10.1016/j.surg.2017.05.016
- Diane, M. (2006). Postoperative sepsis. Current Anaesthesia and Critical Care, 17(1), 65–70. https://doi.org/https://doi.org/10.1016/j.cacc.2006.05.005
- Elective Network. (2018). GULU REGIONAL REFERRAL HOSPITAL [blog post]. Available at: https://www.electives.net/hospital/6862/preview
- Ellen, K., Karissa, J., Nathalie, W., Frangiscos, S., Hasan, S. J., Mathew, L., & Moe, H. K. (2013). A systematic review of risk factors associated with surgical site infections among surgical patients. PLoS One, 812, https://doi.org/https://doi.org/10.1371/journal.pone.0083743.
- Euser, A. M., Zoccali, C., Jager, K. J., & Dekker, F. W. (2009). Cohort studies: prospective versus retrospective. Nephron. Clinical Practice, 113(3), 214–217.https://doi.org/https://doi.org/10.1159/000235241
- Gelhorn, H. L., Anand, S. B., Parvizi, J., Morrison, T., Yu, H., Pokrzywinski, R., Al-Jassar, G., & Chen, A. F. (2017). Qualitative interviews to identify burden of illness, impacts and costs associated with surgical site infections. Journal of Comparativeness Research, 74, https://doi.org/https://doi.org/10.2217/cer-2017-0075
- Georgeto, A. A. F. S., Elias, Adriana, Tanita, Marcos, Grion, C. M. C., Cardoso, Lucienne, Verri, Paulo, Veiga, C. F. F., Barbosa, Á. R. G., Dotti, A. Z., Matsuo, Tiemi. (2011). Incidence and risk factors for sepsis in surgical patients: a cohort study. Critical Care, 15(2). doi:https://doi.org/10.1186/cc10165
- Gonzalo, S., & Justo, G. S. (2019). Application of predictive maintenance in hospital heating, ventilation and air conditioning facilities. Emerging Science Journal, 3(5). https://doi.org/http://dx.doi.org/10.28991/esj-2019-01196
- Gur, R., Duggal, S. D., Rongpharpi, S. R., Srivastava, R., Kumar, A., Gupta, V., Chawla, D., & Pundhir, S. (2015). Post caesarean surgical siteinfections. Archives of Clinical Microbiology, 6(1). Available at: http://www.acmicrob.com/microbiology/post-caesarean-surgical-site-infections.php?aid=3810
- Horstmeier, P. (2015). Improving outcomes for sepsis patients: 3 key solutions proven to help [blog post]. Available at: https://www.healthcatalyst.com/improving-outcomes-sepsis-patients
- Hughes, C., Tunney, M., & Bradley, M. C.(2013). Infection control strategies for preventing the transmission of meticillin-resistantStaphylococcus aureus(MRSA) in nursing homes for older people. Cochrane Database of Systematic Reviews2013, 11, https://doi.org/https://doi.org/10.1002/14651858.CD006354.
- Israel, G. D. (1992). Determining sample size [pdf on line]. Available at: https://www.tarleton.edu/academicassessment/documents/Samplesize.pdf
- Lakomkin, N., Sathiyakumar, V., Wick, B., Shen, M. S., Jahangir, A. A., Mir, H., Obremskey, W. T., Dodd, A. C., & Sethi, M. K. (2016). Incidence and predictive risk factors of postoperative sepsis in orthopedic trauma patients. Journal of Orthopaedics and Traumatology, 18(2), 151–158. https://doi.org/https://doi.org/10.1007/s10195-016-0437-4
- Meghraj, C., Shobha, S. N., Ganesh, K. K., & Sudhir, B. D. (2017). The incidence of postoperative infection in tertiary rural hospital. International Surgery Journal, 45, https://doi.org/http://dx.doi.org/10.18203/2349-2902.isj20171542
- Ministry of Health [MoH], Uganda. (2017). Annual health sector performance report 2016/2017. kampala: author. Also available at: http://health.go.ug/content/annual-health-sector-performance-report–201617
- Mokart, D., Giaoui, E., Barbier, L., Lambert, J., Sannini, A., Chow-Chine, L., Brun, J.-P., Faucher, M., Guiramand, J., Ewald, J., Bisbal, M., Blache, J.-L., Delpero, J.-R., Leone, M., & Turrini, O. (2016). Post-operative sepsis in cancer patients undergoing major elective digestive surgery is associated with increased long-term mortality. Journal of Critical Care, 31(1), 48–53. https://doi.org/https://doi.org/10.1016/j.jcrc.2015.10.001
- Mokart, D., Leone, M., Sannini, A., Brun, J. P., Tison, A., Delpero, J. R., Houvenaeghel, G., Blache, J. L., & Martin, C. (2005). Predictive perioperative factors for developing severe sepsis after major surgery. British Journal of Anaesthesia, 95(6), 776–781. Available at: https://doi.org/https://doi.org/10.1093/bja/aei257.
- Namba, R. S., Inacio, M. C., & Paxton, E. W. (2012). Risk factors associated with surgical site infection in 30,491 primary total hip replacements. The Journal of Bone and Joint Surgery, 94(10), 1330–1338. https://doi.org/https://doi.org/10.1302/0301-620X.94B10.29184
- Olayinka, I., & Aanuoluwapo, A. (2020). Time to move from vertical to horizontal approach in our COVID-19 response in Nigeria. SciMedicine Journal, 2. 2020. https://doi.org/https://doi.org/10.28991/SciMedJ-2020-02-SI-3
- Ou, L., Chen, J., Hillman, K., Flabouris, A., Parr, M., Assareh, H., & Bellomo, R. (2017). The impact of post-operative sepsis on mortality after hospital discharge among elective surgical patients: A population-based cohort study. BMC _ Critical Care, 21(1), 34.https://doi.org/https://doi.org/10.1186/s13054-016-1596-7
- Polonia, G. (2013). Analysis of sample size in consumer surveys [Pdf on line]. Availableat: http://ec.europa.eu/economy_finance/db_indicators/surveys/documents/workshops/2013/pl-gfk_k._pusczak_-_sample_size_in_customer_surveys_v2_2.pdf
- Price, P. C., Jhangiani, R., & Chiang, I. A. (2018).RESEARCH METHODS IN PSYCHOLOGY [blog post]. Available at: https://opentextbc.ca/researchmethods/chapter/reliability-and-validity-of-measurement/
- Sood, A., Abdollah, F., Sammon, J. D., Arora, N., Weeks, M., Peabody, J. O., Menon, M., & Trinh, Q. (2017). Post-operative sepsis prediction in patients undergoing major cancer surgery. Journal of Surgical Research, 209, pp. 60–69. https://doi.org/https://doi.org/10.1016/j.jss.2016.09.059
- Tanner, J., Padley, W., Davey, S., Murphy, K., & Brown, B. (2012). Patient narratives of surgical site infection:implications for practice. Journal of Hospital Infection, 83(1), 41–45. https://doi.org/http://dx.doi.org/10.1016/j.jhin.2012.07.025 . 2013
- Tartari, E., Weterings, V., Gastmeier, P., Rodríguez Baño, J., Widmer, A., Kluytmans, J., & Voss, A. (2017). Patient engagement with surgical site infection prevention: An expert panel perspective. BMC _ Antimicrobial Resistance & Infection Control, 6(1), 45. 2017 : https://doi.org/https://doi.org/10.1186/s13756-017-0202-3
- Teshager, F. A., Engeda, E. H., & Worku, W. Z. (2015). Knowledge, practice, and associated factors towards prevention of surgical site infection among nurses working in amhara regional state referral hospitals, Northwest Ethiopia. Surgery Research and Practice,Vol 2015. https://doi.org/http://dx.doi.org/10.1155/2015/736175.
- Teshager, M., Tilaye, W. A., Tesfaye, Y. C., & Antehun, A. A. (2017). Risk factors for surgical site infections in obstetrics: A retrospective study in an Ethiopian referral hospital. Patient Safety Journal, 2017 (11). https://doi.org/[10.1186/s13037-017-0138-9].
- Tinker, A. (2018). The top seven healthcare outcome measures and three measurement essentials [blog post]. Available at: https://www.healthcatalyst.com/insights/improving-patient-reported-outcomes
- Todd, R. V., Viktor, Y. D., Jeffrey, L. C., Alan, M. G., & Stephen, F. L. (2010). Postoperative sepsis in the United States. Annals of Surgery, 252(6), 1065–1071. https://doi.org/https://doi.org/10.1097/SLA.0b013e3181dcf36e
- Todd, R. V., Viktor, Y. D., & Stephen, F. L. (2009). Trends in postoperative sepsis: are we improving outcomes? Surgery Infection, 10(1), 71–78. https://doi.org/https://doi.org/10.1089/sur.2008.046
- Uçkay, I., Harbarth, S., Peter, R., Lew, D., Hoffmeyer, P., & Pittet, D. (2010). Preventing surgical site infections. Expert Review Anti Infectious Therapy, 8 (6), 657–670. https://doi.org/https://doi.org/10.1586/eri.10.41.
- Whitlock, J., & Fogoros, R. N. (2018).Difference between sepsis infection and septic shock [blog post]. Available at: https://www.verywellhealth.com/sepsis-and-septic-shock-3156848
- Woelber, E., Schrick, E. J., Gessner, B. D., & Evans, H. L. (2016). Proportion of surgical site infections occurring after hospital discharge: a systematic review. Surgical Infections, 17(5), 510–519. https://doi.org/https://doi.org/10.1089/sur.2015.241
- World Health Organization [WHO]. (2007).Infection prevention and control of epidemic-and pandemic-prone acute respiratory diseases in health care. Geneva: Author. Also available at: https://www.who.int/csr/resources/publications/WHO_CDS_EPR_2007_6c.pdf?ua=1
- World Health Organization [WHO]. (2009). Infection control principles & strategies:focus on the outbreak context. geneva: author. Also available at: https://www.who.int/diseasecontrol_emergencies/publications/idhe_2009_london_infection_control.pdf
- World Health Organization [WHO]. (2016). WHO recommends 29 ways to stop surgical infections and avoid superbugs [Blog Post]. Available at: https://www.who.int/news-room/detail/03-11-2016-who-recommends-29-ways-to-stop-surgical-infections-and-avoid-superbugs
- World Health Organization [WHO]. (n.d.a) WHO surgical site infection prevention guidelines [pdf online]. Available at: http://www.who.int/gpsc/appendix21.pdf
- World Health Organization [WHO]. (n.d.b) Hospital hygiene and infection control [Pdf online]. Available at: https://www.who.int/water_sanitation_health/medicalwaste/148to158.pdf
- Wound Source. (2018). Surgical site infections: risk factors and prevention strategies. [Blog Post]. Available athttps: //www.woundsource.com/blog/surgical-site-infections-risk-factors-and-prevention-strategies
- Yang, F., Zhang, Q., Kong, W., Shen, H., Lu, J., Ge, X., & Zhuang, Y. (2018). A qualitative study on the attitudes of patients with gastrointestinal cancer toward being informed of the truth. Patient Preference and Adherence, 12, 2283–2290. https://doi.org/https://doi.org/10.2147/PPA.S179465.
- Yunzhou, F., Zhaoxia, W., Weiwei, W., Li, T., Hongbo, J., Lihong, T., Yuguang, C., & Shaofa, N. (2014). The incidence and distribution of surgical site infection in Mainland China: A meta-analysis of 84 prospective observational studies. Scientific Reports, 2014; 4: 6783. https://doi.org/https://doi.org/10.1038/srep06783.