ABSTRACT
Human trafficking is a public health issue that requires a trauma-informed survivor focused response from healthcare providers. While some of the unique healthcare needs of trafficking survivors have been studied, there is still a lack of research and insight into the best approaches for the treatment of lasting psychological trauma experienced by trafficking victims. The trauma experienced within this patient population is frequently chronic and complex, and may coincide with time frames of brain development leading to specific manifestations of complex post-traumatic stress disorder (complex PTSD), intermixed with trauma-coerced attachment (TCA) – often referred to as trauma bonding- to the abuser(s). Healthcare providers need to consider incorporating both psychological and pharmacological treatments to adequately address complex PTSD with concurrent TCA. However, more research and a better understanding of effective approaches for treating trafficking-related PTSD are essential to better inform survivor-centered care. Here, we present a conceptual understanding of trauma-coerced attachment and complex PTSD in trafficking victims, as well as an approach to comprehensive, trauma-informed care used at our medical safe haven (MSH). Improving the ability of healthcare professionals to effectively treat the psychological trauma of trafficked persons in a trauma-informed manner contributes to UN Sustainable Development Goal 16: Promote peaceful and inclusive societies for sustainable development, provide access to justice for all and build effective, accountable and inclusive institutions at all levels.
Introduction
As public health researchers and healthcare providers are increasingly recognizing, human trafficking exerts a significant and often lasting toll on the physical, psychological, and psychosocial health and wellness of its survivors (Goldberg et al., Citation2017; Lederer & Wetzel, Citation2014; Zimmerman et al., Citation2003). In the U.S., it is estimated that over 400,000 people may be trafficked currently, though many suggest these estimations are low due to the difficulty of tracking human trafficking and its underreporting (Lo & Chambers, Citation2016; National Human Trafficking Hotline, n.d.; The Global Slavery Index, 2018; UNODC, 2021). Approximately a quarter of human trafficking victims worldwide are children, and many adult victims report either first being trafficked as children or having a history of childhood abuse prior to their trafficking experience (Counter-Trafficking Data Collaborative, Citationn.d.). For survivors of trafficking, this often means a lifelong history of abuse and trauma which creates the foundation of trauma-coerced attachment and the lasting, potentially worsening symptoms of PTSD and other psychological disorders (Counter-Trafficking Data Collaborative, Citationn.d.; Doychak & Raghavan, Citation2020).
Persons experiencing human trafficking are examined by healthcare providers in clinics around the world. While most go unrecognized (Lederer & Wetzel, Citation2014; Lo & Chambers, Citation2016; Lumpkin & Taboada, Citation2017), medical professionals and organizations are increasingly being educated and implementing protocols to identify victims of human trafficking and facilitate their initial steps out of their trafficking situations (Barrows & Finger, Citation2008; Chambers, Citation2019; Lo & Chambers, Citation2016; O’Callaghan, Citation2012). Unfortunately, this focus leads to most efforts being aimed solely at the urgent or acute needs of these patients and fails to address their long-term recovery. Healthcare providers should also develop an understanding of the longitudinal care needs of this patient population with a heightened focus on the ramifications of trafficking, including complex PTSD and trauma-coerced attachment (TCA). By addressing these specific morbidities of trafficking, healthcare providers can embrace trauma-informed care principles and utilize appropriate survivor-centered care modalities, medications and treatment plans, thus equipping these patients with the resources necessary to reclaim their freedom and livelihood.
Work with survivors of human trafficking has led to the development of a medical safe haven (MSH), “an umbrella term used to describe clinics providing longitudinal care for patients who have experienced trafficking using validated victim-centered trauma-informed care techniques and incorporating survivor-informed practices” (Chambers, Citation2019, p. 344). Established in 2015 the MSH program has provided over 3,000 patient visits where providers see patients across all age ranges, although most report being trafficked beginning as minors. An overarching goal of the MSH is to provide comprehensive trauma-informed care for patients experiencing complex PTSD which often coincides with trauma-coerced attachment (Chambers, Citation2019; Chambers et al., Citation2019). While a more formal evaluation is underway, patients and their advocates have reported overwhelmingly positive experiences and decreased re-traumatization at our MSH (Chambers, Citation2019). Based on our experience, we have developed a conceptual model to describe the relationship between complex trauma, PTSD, TCA, and recidivism from safe placement (i.e., returning to trafficking) that guides our treatment of human trafficking survivors. This paper describes the development of complex PTSD and TCA and the impact of human trafficking on survivors; presents our conceptual model; summarizes the evidence for psychological and pharmacological interventions in this population; and outlines the treatment approach at our MSH. In this paper the term “survivor” is predominately used for persons who have experienced exploitation via human trafficking; however the authors recognize the term is not without criticism as it may imply a sociopolitical context shifting of the onus onto the victim to fulfill a societal expectation to “survive” and “thrive” in spite of the trauma.
Development of Complex PTSD and Trauma-coerced Attachment
Understanding the trauma experienced by survivors of abuse is important to our understanding of the most effective care for their complex and unique needs. Non-complex PTSD may arise from a single traumatic event. Neuroimaging in such cases may demonstrate decreased hippocampal volume without noted changes in amygdala volume, hyperactivation of amygdala, and hypoactivation of the prefrontal cortex and hippocampus (Giourou et al., Citation2018). Complex PTSD results from complex trauma. Known as “developmental” trauma when it happens during childhood, complex trauma involves exposure to varied and multiple traumatic events usually over a prolonged period of time, often of an interpersonal nature, from which escape is difficult or impossible (Center for Substance Abuse Treatment (US), Citation2014). These types of traumatic incidents often first occur early in life and typically involve a caregiver, which can interfere with a child’s normal development and ability to form secure, healthy attachments. Neuroimaging in these cases may reveal hippocampal dysfunction and decreased gray matter, prefrontal cortex activation disturbances, and more severe functional changes in neural imaging than in the case of non-complex PTSD (Giourou et al., Citation2018). Additionally, the experience of being trafficked, especially in the case of childhood victims who may have been trafficked by a family member or other trusted person, is itself a lasting complex trauma that impacts all aspects of normal physical and mental health and development (Counter-Trafficking Data Collaborative, Citationn.d.; International Organization for Migration, Citation2017). Many survivors of human trafficking face this double trauma, where the initial developmental trauma made them vulnerable to the subsequent manipulation and trauma of trafficking itself.
One aspect of human trafficking that is particularly insidious is the use of coercion by perpetrators to influence, control, and victimize their targets (Baldwin et al., Citation2015; Withers, Citation2016). Traffickers often target the most vulnerable individuals for exploitation, especially homeless and run-away youth; survivors of previous abuse and trauma; those with substance use disorders; and those with mental illness (Choi, Citation2015; Lo & Chambers, Citation2016; Polaris Project, Citation2019a). Traffickers employ multiple coercive tactics, such as encouraging substance use or manipulation of their victims’ vulnerabilities to gain control. They may use aspects of positive reinforcement such as promises of love, security, or gifts in exchange for compliance, or they may use negative coercion such as threats of violence, abandonment, or immigration and law enforcement authorities to force their victims into submission (Counter-Trafficking Data Collaborative, Citationn.d.; Polaris Project, Citation2019a). Often, a combination of both positive and negative coercion tactics is employed to manipulate, destabilize, and undermine those they have chosen to target. These abusive techniques used by traffickers can result in a specific aspect of trauma called trauma-coerced attachment, or trauma bonding.
Trauma bonding was first defined by Patrick Carnes as “the misuse of fear, excitement, sexual feelings, and sexual physiology to entangle another person,” with recurring cycles of intermittent reinforcement of reward and punishment that create an emotional bond between victim and abuser which is difficult to break (as explained in Rosenberg, Citation2019, p. 2). Furthermore, Doychak and describe trauma-coerced attachment as involving “a powerful emotional dependency on the abusive partner and a shift in world- and self- view, which can result in feelings of gratitude or loyalty toward the abuser and denial or minimization of the coercion and abuse” (p. 339). TCA can lead to the survivor taking responsibility for the abuser’s crimes and even protecting them from legal or social repercussions. This type of attachment can continue even after the relationship between survivor and abuser has ended and can result in behavior that is difficult to predict and understand by others, including healthcare providers. Given this, TCA is relatively rare in the diagnostic world; however it does exist. TCA has been identified in many power imbalance and abuse situations that have psychological captivity including domestic violence and cults, and the describes symptoms of TCA and PTSD under other dissociative disorders (Wang, Citation2018). In ICD-11, complex trauma includes components of TCA. Survivors experiencing trauma-coerced attachment are more likely to return to their captors and/or return to the trafficking lifestyle. Therefore, addressing the underlying psychological responses that both lead to and result from TCA is essential for a survivor’s journey to recovery.
Clinical Impact of Human Trafficking on Survivors
To better understand and care for survivors of a complex trauma such as human trafficking, a better understanding of the psychological repercussions of trauma-coerced attachment and complex PTSD is needed. Through our experiences caring for this population, we concur that chronic trauma leads to altered development. In normal development, the caregiver’s attuned response to the child’s distress imparts the ability for the child to regulate his/her arousal system. In the absence of that (i.e., in the presence of developmental trauma), and/or with the experience of overwhelming threats (i.e., repeated exposure to traumatic experiences), the threat response system is chronically dysregulated, either responding too much (e.g., hypervigilance, “fight or flight,” insomnia, nightmares, panic) or too little (e.g., “numbed out,” dissociated, ignoring danger signs, thrill-seeking). Individuals with this developmental upbringing seek some sort of “caregiver,” and, in the absence of an adequate one, will settle for a relationship with the abuser, ignoring or minimizing any faults out of the need to have someone in their life “caring” for them, thus creating a dysregulated threat response.
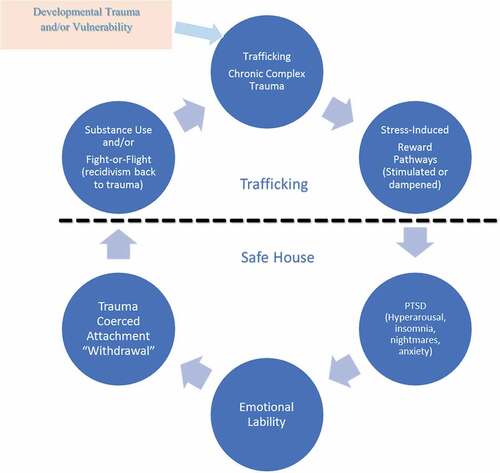
Additionally, our experiences have led us to hypothesize that persistent complex trauma and trauma-coerced attachment alters the reward pathways of the brain’s mesolimbic system, possibly analogous to the use of psychoactive substances (Feltenstein & See, Citation2008), and that this becomes normalized with recurring abuse (). Due to the effects of trauma-coerced attachment, survivors may glamorize the life they had during their trafficking experiences and may seek the “high” of that lifestyle again. In our patients, we frequently encounter recidivism behaviors, where survivors repeatedly return to their trafficker, that mimic those seen in withdrawal from addictive substances. Survivors may experience hyperarousal or acute stress response (“fight or flight”) during their trafficking, which is then withdrawn when they leave that situation. Indeed, dysfunction of the reward circuitry of the brain has been observed in those with PTSD and other psychiatric disorders (Elman et al., Citation2018; Fenster et al., Citation2018; Fonzo, Citation2018).Reward pathway metabolism has been established and visualized using functional MRIs in patients with substance addiction and patients who are normalizing post-withdrawal; this enhances our understanding of how addiction alters neurotransmitter signaling pathways, resulting in dysregulated reward circuitry, impulse control, cognitive control, and other psychological dysfunctions (Fowler et al., Citation2007; Trifilieff & Martinez, Citation2014; Volkow et al., Citation2010). Functional neuroimaging has also demonstrated dysfunctional reward and aversion processing in patients with PTSD (Elman et al., Citation2009, p. 2018; Frewen et al., Citation2012). What we have observed in the clinic poses the question of whether similar pathways may show similar dysfunctional activity with chronic trauma and emotionally intense situations, and then decreased activity or withdrawal when this intensity is removed. These similarities may suggest that altered neurological reward pathways in human trafficking survivors, especially those experiencing complex PTSD and TCA, may increase their likelihood of recidivism. Importantly, this also poses the question of whether medications and psychotherapies aimed at inhibiting dysfunctional reward circuitry may be used to help end the cycle of trauma experienced by trafficking survivors?
Figure 1. Theorized cycle of complex trauma, PTSD with trauma-coerced attachment and recidivism from safe placement experienced by people exploited via human trafficking. Human trafficking victims often experience a positive feedback loop of effects both triggered and heightened by their chronic, complex trauma. This cycle can include PTSD and related psychological effects like anxiety, hyperarousal, and insomnia, as well as emotional lability. Victims may respond to this by misusing substances which influences their fight-or-flight response and alters reward pathways within the brain.
Treatment of Complex Trauma with Trauma-coerced Attachment
As discussed above, survivors of human trafficking frequently exhibit acute and chronic physical signs of abuse and neglect, as well as psychological issues during and following their abuse, including depression, suicidality and self-harm, anti-social behavior, feelings of isolation, personality disorders, anxiety, and chronic/complex PTSD (Lederer & Wetzel, Citation2014). It is not uncommon for survivors to engage in abusing substances and in self-medicating as a means of escape from some of their painful experiences, which may contribute even more to their trauma and increase likelihood of future abuse and traumatization (Cook et al., Citation2018).Appropriately diagnosing and caring for survivors’ mental health needs can be challenging, especially if they are still being abused and victimized. We have noted that many of the survivors we see in our clinic have previously been diagnosed with mental health disorders, but that these disorders were assigned to patients during a timeframe in their lives when they were being concurrently exploited. Additionally, many were abusing psychoactive substances either as a form of self-medication or as controlled by their trafficker. Survivors are rarely recognized within the healthcare setting due to lack of provider training and awareness, so they are frequently given a diagnosis with little to no knowledge of their experience as a victim, or that their symptoms may be influenced by their trauma history (Barrows & Finger, Citation2008; Chisolm-Straker & Richardson, Citation2007; Donahue et al., Citation2019; Lederer & Wetzel, Citation2014; Viergever et al., Citation2015). Our experience is that these disorders are frequently a manifestation of complex trauma/PTSD. Once patients are free of their abuser and we are able to stabilize and comprehensively address their needs in a trauma-informed manner, they cease to exhibit signs and symptoms of their diagnosed disorder(s); subsequently, we are able to remove one or more diagnoses. This begs the question of what is the best approach to treat these diagnosed psychiatric disorders in survivors of human trafficking, while recognizing the effects of their trauma and trauma-coerced attachment to their abusers?
Harm Reduction Model
As in virtually all aspects of care for survivors of human trafficking, a trauma-informed approach is important in assessing and treating mental health issues (Chambers, Citation2019; Chambers et al., Citation2019). One aspect of this approach is the application of a harm-reduction model of care. This model aims at reducing the negative outcomes associated with certain activities which typically are criminalized and involve health risks, such as substance abuse and sex work (Hickle & Hallett, Citation2016). Harm reduction practices involve prioritizing the safety, rights, and dignity of individuals involved in these activities, meeting individuals “where they are” rather than trying to force a specific outcome (Positive Women’s Network USA, n.d.).
When working with survivors of human trafficking, this means working with a survivor-centered lens of understanding, compassion, and patience, as well as practicing informed consent by involving the patient in the decision-making process as much as possible. For survivors with diagnosed mental health disorders, this can mean explaining the treatment process thoroughly as well as acknowledging that treatment and prognosis may change with progression through the recovery process. Importantly, it has been demonstrated that patients with PTSD exhibit greater treatment adherence and reduced symptomology over time when they are able to choose their preferred form of treatment (psychological vs pharmacological), compared to those who are simply prescribed one or the other (Zoellner et al., Citation2019). This suggests that actively involving patients in their mental health care and treatment process may improve outcomes and speed recovery. For many survivors, having an opportunity to gain control over their own treatment can be a large and intimidating step from their previous experiences under the control and manipulation of a trafficker who did not value them or their input, but it is often a significant part of the treatment and recovery process. In our MSH model providers educate survivors on TCA, complex PTSD, and treatment options in a safe, trauma informed space where patients may or may not draw parallels between concepts and their own lived experiences.
Psychological Treatment
Treatment paths for human trafficking survivors experiencing PTSD and related disorders vary greatly, and there is little to no evidentiary support for the different treatment methodologies used to treat survivors survivors of human trafficking specifically. To date, most of the research into treatment efficacy for individuals with PTSD is based on combat soldiers or other survivors of acute trauma who have often experienced trauma and PTSD onset during adulthood (Hoffman et al., Citation2018). This makes it very challenging to translate these data to survivors of human trafficking, who often experience chronic, complex trauma starting as children or adolescents. These challenges are compounded by the frequent presence of trauma-coerced attachment to traffickers, which may be occurring concurrently with treatment and may impact how complex PTSD manifests in these patients.
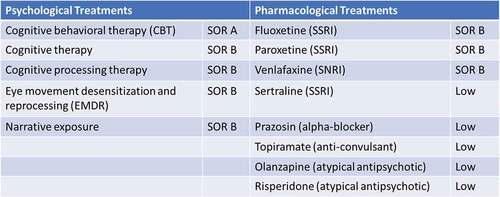
There are several evidence-based psychological treatments for individuals with PTSD, which may also be effective for survivors of human trafficking and related domestic violence (). These include cognitive therapies such as cognitive behavioral therapy (CBT) and cognitive processing therapy (CPT), and other psychotherapies such as eye movement desensitization and reprocessing (EMDR), and exposure therapy (Hoffman et al., Citation2018.These therapies typically have a high strength of recommendation (SOR) for treatment of individuals experiencing PTSD and can be encouraged for survivors of abuse and human trafficking. It is important to note, however, that co-morbidities may influence efficacy. For example, patients who have experienced physical trauma during their trafficking may have evidence of traumatic brain injury (TBI) and TBI-related cognitive impairment may reduce the PTSD response rate to cognitive behavioral therapy by fifty percent (Yedlinsky et al., Citation2019).
Pharmacological Treatment
Evidence-based recommendations for pharmacological treatments for the complex PTSD experienced by survivors of human trafficking is lacking (Torrisi et al., Citation2019). Due to the complex mental healthcare needs of these individuals, as well as the comorbidities and acute symptomology they present with, psychotherapy alone frequently fails to adequately address these concerns in the patients seen in our clinic. Unfortunately, the efficacy and application of pharmacological treatments is poorly understood in the context of complex PTSD, specifically in survivors exhibiting TCA.
There are a few treatments that are considered effective at reducing symptoms of PTSD in adults (though not necessarily in survivors of human trafficking or in minors), and therefore have a moderate strength of recommendation (SOR) () (Hoffman et al., Citation2018; Reisman, Citation2016). These include the selective serotonin reuptake inhibitor (SSRI) antidepressants fluoxetine and paroxetine and the serotonin-norepinephrine reuptake inhibitor (SNRI) venlafaxine, which are typically used to treat psychological conditions associated with PTSD, including depression, generalized and social anxiety disorders, obsessive-compulsive disorder (OCD), and panic disorder. Currently, the only two FDA-approved pharmacotherapies for PTSD are the SSRIs paroxetine and sertraline; however, in general, SSRIs and SNRIs are considered first-line treatments for PTSD (Alexander, Citation2012). It is not clear how serotonergic medications work, but it is theorized that enhancing the mesolimbic serotonin circuits helps the prefrontal cortex or “rational mind” to remain online in the face of significant emotions that would otherwise cripple executive function (Alex & Pehek, Citation2007; Olijslagers et al., Citation2006).
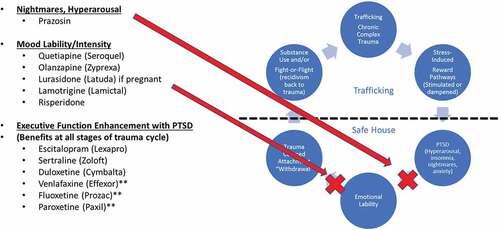
There is conflicting evidence (with low SOR) that other pharmacologic treatments, including atypical antipsychotics (e.g., olanzapine and risperidone) and treatments for insomnia and nightmares (e.g., prazosin and topiramate) may be effective for combat-related PTSD (Adetunji et al., Citation2005; Alexander, Citation2012). As described above, these have not been studied in patients who experienced chronic, complex trauma, such as human trafficking survivors. Atypical antipsychotics likely decrease the intensity of the fight-or-flight threat response at a cortical level (Cai et al., Citation2017), while adrenergic blockers such as prazosin or propranolol do so peripherally (with prazosin having the additional benefit of limiting PTSD-related nightmares) (Hudson et al., Citation2012). We hypothesize that the use of antidepressants or atypical antipsychotics may help disrupt the cycle of trauma-driven complex PTSD, emotional lability, and reward pathway stimulation and withdrawal that challenges survivors and frequently leads to their return to their former life of abuse (). We believe that these treatments may only be needed temporarily to halt this cycle and help stabilize patients long enough for additional treatments (e.g., CBT, CPT, EMDR) and resources such as food, safe housing and case management services provided by community organizations and partners to be provided. Our continued research will address the efficacy of these treatment regimens on overall patient outcomes, so evidence-based recommendations tailored to human trafficking survivors experiencing complex PTSD may be developed. Our anecdotal experience is that a combination of adrenergic blocker (e.g., prazosin), atypical antipsychotic (e.g., quetiapine), and SSRI (e.g., escitalopram) can be instrumental in the initial steps on the road to recovery for many of our patients.
Figure 3. Theorized medication inhibition of cycle of complex trauma, PTSD with trauma-coerced attachment and recidivism from safe placement experienced by people exploited via human trafficking. Pharmacologic treatments for PTSD with trauma-coerced attachment are theorized to block the cycle of complex trauma in multiple ways and, therefore, have the potential to reduce recidivism from safe placement.
In our practice, we have observed that a combination of psychological and pharmacological treatments aimed at improving mental health, (e.g., mood stabilization and treatments for insomnia, nightmares, hyperarousal, depression and anxiety), as well as pharmacological approaches to target physical health outcomes of trafficking (e.g., infections/STIs, unwanted pregnancy, and physiologic addiction and withdrawal) are required for successful comprehensive, trauma-informed care of human trafficking survivors. As described above, involving patients in their own care by providing clear explanations of their diagnosis and treatment, and offering multiple treatment options, whenever appropriate, may improve patient adherence, progress through recovery, and overall health outcomes.
Conclusions
Our experience and observations as front-line healthcare providers for survivors of human trafficking have demonstrated a need for additional research and understanding of trauma-coerced attachment and complex PTSD in patients who have experienced trafficking. We have observed that the complex, chronic trauma experienced by survivors who are trafficked at a young age, especially at the hands of those who should be their protectors, imparts a lasting, unique psychological trauma. This trauma, which may include aspects of TCA, is not necessarily analogous to the trauma experienced by combat veterans, in whom the majority of efficacy research on PTSD treatments is performed. Trauma-informed survivor-centered practice dictates that we must provide evidence-based comprehensive care to survivors of human trafficking. This includes adequately addressing their physical, psychological, and psychosocial healthcare needs while meeting them where they are in their recovery journey. It is critical that we advocate for more research specific to human trafficking survivors, especially in the realm of treatment efficacy for trauma-coerced attachment and complex PTSD.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Adetunji, B., Mathews, M., Williams, A., Budur, K., Mathews, M., Mahmud, J., & Osinowo, T., et al. (2005). Use of antipsychotics in the treatment of post-traumatic stress disorder. Psychiatry (Edgmont), 2(4), 43–47.
- Alex, K. D., & Pehek, E. A. (2007). Pharmacologic mechanisms of serotonergic regulation of dopamine neurotransmission. Pharmacology & Therapeutics, 113(2), 296–320. https://doi.org/10.1016/j.pharmthera.2006.08.004
- Alexander, W. (2012). Pharmacotherapy for post-traumatic stress disorder in combat veterans. Pharmacy and Therapeutics, 37(1), 32–38.
- Baldwin, S. B., Fehrenbacher, A. E., & Eisenman, D. P., et al. (2015). Psychological coercion in human trafficking: an application of biderman’s framework. Qualitative Health Research, 25(9), 1171–1181. https://doi.org/10.1177/1049732314557087
- Barrows, J., & Finger, R. (2008). Human trafficking and the healthcare professional. Southern Medical Journal, 101(5), 521–524. https://doi.org/10.1097/SMJ.0b013e31816c017d
- Cai, H. L., Jiang, P., Tan, Q. Y., Dang, R. L., Tang, M. M., Xue, Y., Deng, Y., Zhang, B. K., Fang, P. F., Xu, P., Xiang, D. X., Li, H. D., & Yao, J. K., et al. (2017). Therapeutic efficacy of atypical antipsychotic drugs by targeting multiple stress-related metabolic pathways. Translational Psychiatry, 7(5), e1130–e1130. https://doi.org/10.1038/tp.2017.94
- Center for Substance Abuse Treatment (US). (2014). Understanding the Impact of Trauma. In Trauma-Informed Care in Behavioral Health Services. Substance Abuse and Mental Health Services Administration. https://www.ncbi.nlm.nih.gov/books/NBK207191/.
- Chambers, R., Cox, J., & Gibbs, H., et al. (2019). Human trafficking medical safe haven program and shared learnings manual. https://www.dignityhealth.org/sacramento/for-physicians/dignity-health-methodist-hospital-of-sacramento-family-medicine-residency-program/human-trafficking-safe-haven-clinic/medical-safe-haven-resources
- Chambers, R. (2019). Caring for human trafficking victims: A description and rationale for the medical safe haven model in family medicine residency clinics. The International Journal of Psychiatry in Medicine, 54(4–5), 344–351. https://doi.org/10.1177/0091217419860358
- Chisolm-Straker, M., & Richardson, L. (2007). Assessment of emergency department (ED) provider knowledge about human trafficking victims in the ED. Academic Emergency Medicine, 14(5 Suppl. 1), S134. https://doi.org/10.1197/j.aem.2007.03.1078
- Choi, K. R. (2015). Risk factors for domestic minor sex trafficking in the United States: A literature review. Journal of Forensic Nursing, 11(2), 66–76. https://doi.org/10.1097/JFN.0000000000000072
- Cook, M. C., Barnert, E., Ijadi-Maghsoodi, R., Ports, K., & Bath, E., et al. (2018). Exploring mental health and substance use treatment needs of commercially sexually exploited youth participating in a specialty juvenile court. Behavioral Medicine, 44(3), 242–249. https://doi.org/10.1080/08964289.2018.1432552
- Counter-Trafficking Data Collaborative. (n.d.). Global data hub on human trafficking. https://www.ctdatacollaborative.org/story/age-victims-children-and-adults
- Donahue, S., Schwien, M., & LaVallee, D., et al. (2019). Educating emergency department staff on the identification and treatment of human trafficking victims. Journal of Emergency Nursing, 45(1), 16–23. https://doi.org/10.1016/j.jen.2018.03.021
- Doychak, K., & Raghavan, C. (2020). “No voice or vote:” trauma-coerced attachment in victims of sex trafficking. Journal of Human Trafficking, 6(3), 339–357. https://doi.org/10.1080/23322705.2018.1518625
- Elman, I., Lowen, S., Frederick, B. B., Chi, W., Becerra, L., & Pitman, R. K., et al. (2009). Functional neuroimaging of reward circuitry responsivity to monetary gains and losses in posttraumatic stress disorder. Biological Psychiatry, 66(12), 1083–1090. https://doi.org/10.1016/j.biopsych.2009.06.006
- Elman, I., Upadhyay, J., Langleben, D. D., Albanese, M., Becerra, L., & Borsook, D., et al. (2018). Reward and aversion processing in patients with post-traumatic stress disorder: functional neuroimaging with visual and thermal stimuli. Translational Psychiatry, 8(1), 240. https://doi.org/10.1038/s41398-018-0292-6
- Feltenstein, M. W., & See, R. E. (2008). The neurocircuitry of addiction: an overview. British Journal of Pharmacology, 154(2), 261–274. https://doi.org/10.1038/bjp.2008.51
- Fenster, R. J., Lebois, L. A. M., Ressler, K. J., & Suh, J., et al. (2018). Brain circuit dysfunction in post-traumatic stress disorder: from mouse to man. Nature Reviews. Neuroscience, 19(9), 535–551. https://doi.org/10.1038/s41583-018-0039-7
- Fonzo, G. A. (2018). Diminished positive affect and traumatic stress: A biobehavioral review and commentary on trauma affective neuroscience. Neurobiology of Stress, 9 (3) , 214–230. https://doi.org/10.1016/j.ynstr.2018.10.002
- Fowler, J., Volkow, N., Kassed, C., & Chang, L., et al. (2007). Imaging the addicted human brain. Science & Practice Perspectives, 3(2), 4–16. https://doi.org/10.1151/spp07324
- Frewen, P. A., Dozois, D. J. A., Neufeld, R. W. J., Lane, R. D., Densmore, M., Stevens, T. K., & Lanius, R. A., et al. (2012). Emotional numbing in posttraumatic stress disorder: A functional magnetic resonance imaging study. The Journal of Clinical Psychiatry, 73(4), 431–436. https://doi.org/10.4088/JCP.10m06477
- Giourou, E., Skokou, M., Andrew, S. P., Alexopoulou, K., Gourzis, P., & Jelastopulu, E., et al. (2018). Complex posttraumatic stress disorder: the need to consolidate a distinct clinical syndrome or to reevaluate features of psychiatric disorders following interpersonal trauma? World Journal of Psychiatry, 8(1), 12–19. https://doi.org/10.5498/wjp.v8.i1.12
- Goldberg, A. P., Moore, J. L., Houck, C., Kaplan, D. M., & Barron, C. E., et al. (2017). Domestic minor sex trafficking patients: A retrospective analysis of medical presentation. Journal of Pediatric and Adolescent Gynecology, 30(1), 109–115. https://doi.org/10.1016/j.jpag.2016.08.010
- Hickle, K., & Hallett, S. (2016). Mitigating harm: considering harm reduction principles in work with sexually exploited young people. Children & Society, 30(4), 302–313. https://doi.org/10.1111/chso.12145
- Hoffman, V., Middleton, J., Feltner, C., Gaynes, B. N., Weber, R., Bann, C., Viswanathan, M., Lohr, K. N., Baker, C., & Green, J., et al. (2018). Psychological and pharmacological treatments for adults with posttraumatic stress disorder: A systematic review update. Agency for Healthcare Research and Quality (AHRQ). https://doi.org/10.23970/AHRQEPCCER207.
- Hudson, S. M., Whiteside, T. E., Lorenz, R. A., & Wargo, K. A., et al. (2012). Prazosin for the treatment of nightmares related to posttraumatic stress disorder: A review of the literature. The Primary Care Companion for CNS Disorders, 14(2): 46–51. https://doi.org/10.4088/PCC.11r01222
- International Organization for Migration. (2017). Family members linked to nearly half of child trafficking: new IOM, polaris data. https://www.iom.int/news/family-members-linked-nearly-half-child-trafficking-new-iom-polaris-data
- Lederer, L. J., & Wetzel, C. A. (2014). The health consequences of sex trafficking and their implications for identifying victims in healthcare facilities. Annals of Health Law, 23(1), 61–87.
- Lo, V., & Chambers, R. (2016). Human trafficking and the role of physicians. Journal of Family Medicine and Community Health, 3(3), 1084.
- Lumpkin, C., & Taboada, A. (2017). Identification and referral for human trafficking survivors in health care settings: survey report. Retrieved from Coalition to Abolish Slavery and Trafficking website. https://www.castla.org/wp-content/themes/castla/assets/files/Identification_and_Referral_in_Health_Care_Settings_survey_report_2017.pdf
- O’Callaghan, M. (2012). The health care professional as a modern abolitionist. The Permanente Journal, 16 (6) , 67–69. Retrieved from: http://www.thepermanentejournal.org/issues/2012/spring/4546-the-health-care-professional-as-a-modern-abolitionist.htmlhttps://doi.org/10.7812/tpp/11-151. http://www.thepermanentejournal.org/issues/2012/spring/4546-the-health-care-professional-as-a-modern-abolitionist.htmlhttps://doi.org/10.7812/tpp/11-151
- Olijslagers, J., Werkman, T., McCreary, A., Kruse, C., & Wadman, W., et al. (2006). Modulation of midbrain dopamine neurotransmission by serotonin, a versatile interaction between neurotransmitters and significance for antipsychotic drug action. Current Neuropharmacology, 4(1), 59–68. https://doi.org/10.2174/157015906775203020
- Polaris Project. (2019a). 2018 U.S. national human trafficking hotline statistics. https://polarisproject.org/2018-us-national-human-trafficking-hotline-statistics/
- Reisman, M. (2016). PTSD treatment for veterans: what’s working, what’s new, and what’s next. Pharmacy and Therapeutics, 41(10), 623–634.
- Rosenberg, J. (2019). Trauma bonding. https://psychologicalhealingcenter.com/trauma-bonding/
- The Global Slavery Index. (2018). Retrieved from:https://www.globalslaveryindex.org/2018/findings/country-studies/united-states/
- Torrisi, S. A., Leggio, G. M., Drago, F., & Salomone, S., et al. (2019). Therapeutic challenges of post-traumatic stress disorder: focus on the dopaminergic system. Frontiers in Pharmacology, 3(10), 404. https://doi.org/10.3389/fphar.2019.00404
- Trifilieff, P., & Martinez, D. (2014). Imaging addiction: D2 receptors and dopamine signaling in the striatum as biomarkers for impulsivity. Neuropharmacology, 76 (4) , 498–509. https://doi.org/10.1016/j.neuropharm.2013.06.031
- Viergever, R. F., West, H., Borland, R., & Zimmerman, C., et al. (2015). Health care providers and human trafficking: what do they know, what do they need to know? findings from the Middle East, the Caribbean, and Central America. Frontiers in Public Health, (3). https://doi.org/10.3389/fpubh.2015.00006
- Volkow, N. D., Wang, G.-J., Fowler, J. S., Tomasi, D., Telang, F., & Baler, R., et al. (2010). Addiction: decreased reward sensitivity and increased expectation sensitivity conspire to overwhelm the brain’s control circuit. BioEssays, 32(9), 748–755. https://doi.org/10.1002/bies.201000042
- Wang, P. (2018). What are dissociative disorders? American Psychiatric Association. https://www.psychiatry.org/patients-families/dissociative-disorders/what-are-dissociative-disorders
- Williamson, E., Dutch, N., & Clawson, H., et al. (2010). Evidence-based mental health treatment for victims of human trafficking. Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. Retrieved from: https://aspe.hhs.gov/report/evidence-based-mental-health-treatment-victims-human-trafficking.
- Withers, M. (2016). Psychological tactics used by human traffickers. https://www.psychologytoday.com/us/blog/modern-day-slavery/201610/psychological-tactics-used-human-traffickers
- Yedlinsky, N. T., Neff, L. A., & Jordan, K. M., et al. (2019). Care of the military veteran: selected health issues. American Family Physician, 100(9), 544–551.
- Zimmerman, C., Yun, K., Shvab, I., Watts, C., Trappolin, I., & Mea, T., et al. (2003). The health risks and consequences of trafficking in women and adolescents: findings from a European study. https://cwhn.ca/en/node/25575
- Zoellner, L. A., Roy-Byrne, P. P., Mavissakalian, M., & Feeny, N. C., et al. (2019). Doubly randomized preference trial of prolonged exposure versus sertraline for treatment of PTSD. American Journal of Psychiatry, 176(4), 287–296. https://doi.org/10.1176/appi.ajp.2018.17090995