ABSTRACT
The likelihood of exposure to overheated indoor environments is increasing as climate change is exacerbating the frequency and severity of hot weather and extreme heat events (EHE). Consequently, vulnerable populations will face serious health risks from indoor overheating. While the relationship between EHE and human health has been assessed in relation to outdoor temperature, indoor temperature patterns can vary markedly from those measured outside. This is because the built environment and building characteristics can act as an important modifier of indoor temperatures. In this narrative review, we examine the physiological and behavioral determinants that influence a person’s susceptibility to indoor overheating. Further, we explore how the built environment, neighborhood-level factors, and building characteristics can impact exposure to excess heat and we overview how strategies to mitigate building overheating can help reduce heat-related mortality in heat-vulnerable occupants. Finally, we discuss the effectiveness of commonly recommended personal cooling strategies that aim to mitigate dangerous increases in physiological strain during exposure to high indoor temperatures during hot weather or an EHE. As global temperatures continue to rise, the need for a research agenda specifically directed at reducing the likelihood and impact of indoor overheating on human health is paramount. This includes conducting EHE simulation studies to support the development of consensus-based heat mitigation solutions and public health messaging that provides equitable protection to heat-vulnerable people exposed to high indoor temperatures.
Introduction
With climate change fueling an increase in the occurrence of hot weather and extreme heat events (EHE), the risk of indoor overheating is expected to rise especially across the planet’s large urban settlements [Citation1,Citation2]. Periods of extreme heat exposure are associated with dramatic increases in short-term mortality [Citation3]. This effect is magnified in those individuals living in large metropolitan centers, where because of the urban heat island (UHI) effect, cities are considerably warmer than the surrounding regions (i.e. UHIs trap hot air, making such areas more vulnerable to subtle changes in temperature) [Citation4-8] Prolonged exposure to heat stress is associated with degradations in physical ability[Citation9], mental health[Citation10-11], cognitive function[Citation12-13], and other health outcomes[Citation3, Citation14]. It creates a cumulative physiological stress on the human body which exacerbates mortality for those with chronic disease such as respiratory and cardiovascular diseases, diabetes mellitus, renal disease, and other medical conditions [Citation15-20]. Social isolation is an equally important mediating factor, with those living alone at a higher risk of heat-related morbidity and mortality, especially in those with reduced mobility or cognitive ability[Citation21-25].
The threat to public health caused by EHE in some countries has been aggravated by various factors, including delays in i) developing explicit national policies to build climate responsive and resilient homes and adapt existing ones, ii) improving equity of access to life-saving cooling strategies, and iii) establishing maximum indoor temperature limits among others. In contrast, for other countries, climate-change-induced temperature increases are serving as a driver for adaptation and prevention programs to improve heat resilience in homes and mitigate or reduce heat-related health risks faced by vulnerable occupants. While our understanding of the association between high outdoor temperatures and the worsening of human health has advanced considerably in recent years, the impact of high indoor temperatures is less understood. This poses a challenge for informing comprehensive policies and actions to safeguard public health across diverse indoor environments. Supported by the fact that most heat-related fatalities occur in the home, indoor overheating is a potentially fatal health hazard [Citation26–28] that requires tailored interventions to protect vulnerable occupants. In the absence of appropriate policy-level changes and the implementation of evidence-based practices to protect at-risk groups from indoor heat, indoor temperatures may continue to be excessively high [Citation27,Citation29]. Consequently, strategies to prevent indoor overheating must continue to be a critical component of heat-health action plans, which are inevitably linked to the adaptability of the built environment.
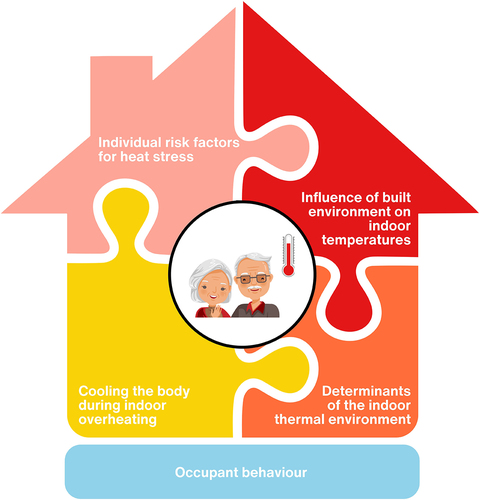
Indoor overheating risk and the impact to health involves a complex interaction between the building’s characteristics and location within the built environment and the occupants’ behavior and susceptibility to heat (). Understanding these factors and identifying ways to modify them appropriately over the immediate-, short- and long-term is essential for mitigating the health risks associated with indoor overheating. This narrative review aims to achieve this goal, by considering the risk factors driving high indoor temperatures, residents’ exposure, and susceptibility to them. We discuss the individual factors that can increase vulnerability to heat exposure, profile the hazards and causes of indoor overheating, assess methods to manage overheating risk and identify heat protective strategies to safeguard vulnerable occupants.
Figure 1. Summary overview of the complex interplay of factors discussed in this review that mediate indoor overheating risk, the adverse health impacts caused by exposure to hot indoor environments and the need for heat protection strategies to protect heat-vulnerable occupants when indoor temperature reach dangerous levels during hot weather or extreme heat events.
Individual risk factors for heat stress
Among the most affected by the adverse health impacts of extreme heat are older adults [Citation3, Citation30–36] (defined as individuals aged ≥65 years [Citation37,Citation38] and those with a range of underlying health conditions linked with heat-susceptibility such as cardiovascular, cerebrovascular, renal, respiratory and neurologic diseases, and diabetes [Citation3,Citation33,Citation39–44]. However, heat-vulnerability is influenced by advanced age more than any other individual risk factor [Citation3,Citation31,Citation45,Citation46], with the threat of heat-related mortality rising with increasing age [Citation3,Citation33,Citation47,Citation48]. The main causes of death during EHE as a result of developing heat-related illnesses (e.g. heat syncope, heat exhaustion, heat stroke), include dehydration, cardiovascular events, renal failure, complications of delirium, and respiratory compromise [Citation26]. Coupled with an aging global population [Citation37,Citation38], and the fact that older adults spend as much as 90% of their time indoors [Citation49,Citation50], more frequent and intense periods of extreme heat [Citation51,Citation52] dictate that a growing number of heat-vulnerable adults, many of whom are living with chronic health conditions are increasingly exposed to hot indoor environments [Citation53]. This underscores a critical need to understand the physiological responses to heat in vulnerable populations and interventions to mitigate heat-related harms.
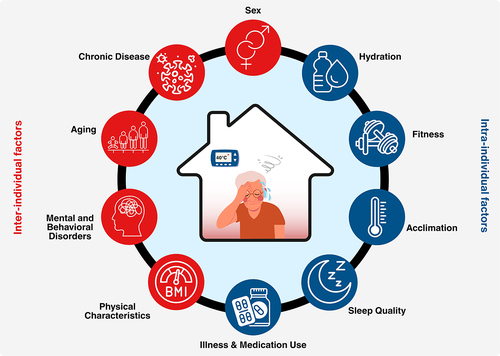
In the following sections, we discuss the current state of knowledge regarding individual factors () mediating thermal resiliency and vulnerability to environmental heat.
Figure 2. Overview of intra- and inter-individual factors that can modulate the body’s physiological capacity to dissipate during a heat stress such as during a daylong exposure to an overheated home in an extreme heat event.
Thermoregulation during heat stress
Except under the most extreme environmental conditions, normal core body temperature under resting conditions is maintained at near constant levels of ~37°C, although significant individual and daily variation (~0.5°C) exists [Citation54]. The thermoregulatory system uses physiological mechanisms to adjust the rate of dry heat loss (via increasing skin blood flow) and evaporative heat loss (via increasing sweating) to the environment to balance the rate at which heat is gained and/or produced within the body [Citation55]. This balance is easily disturbed during exposure to hot environments and/or increases in metabolic heat production due to physical activity. In hot environments, where environmental temperatures exceed skin temperature, the body begins to gain heat, increasing the need for sweating and circulatory adjustments to achieve the rate of whole-body heat dissipation required to maintain heat balance and stable core body temperature [Citation55].
During physical activity such as completing activities of daily living or exercise, the increase in metabolic demand augments the rate at which heat must be dissipated from the body. The primary mechanism of heat loss is through the evaporation of sweat to prevent a dangerous rise in core body temperature. Under circumstances where impairments in the heat loss responses of skin blood flow and sweating lead to an insufficient rate of whole-body heat dissipation to offset an increase in metabolic and/or environmental heat load, core body temperature continually rises and can eventually compromise a person’s health [Citation34,Citation56]. Excessive heat stress can result in a deterioration in physiological function leading to marked reductions in functional ability (e.g. physical performance, exercise capacity) [Citation34,Citation57] as well as a myriad of pathophysiological conditions (e.g. heat exhaustion, acute kidney injury, adverse cardiovascular events, heat stroke) that if left untreated can lead to death [Citation58].
Aging
Age is an important risk modifier of heat-related morbidity and mortality [Citation3,Citation33,Citation59–61]. While vulnerability to heat increases with age, older adults (≥65 years) are among the most vulnerable to the adverse health effects of extreme heat [Citation3,Citation33,Citation60,Citation61] (for a more comprehensive review, readers are referred to Cramer et al. [Citation62] and Meade et al. [Citation60]). The increasing risk for heat-related mortality as people age, can be in large part explained by an impaired ability to sense and respond to heat [Citation33,Citation63] and an attenuated capacity to increase heat loss responses of skin blood flow and sweating necessary to facilitate the dissipation of heat during heat stress [Citation61,Citation64–67]. Consequently, relative to their younger counterparts, older adults store more heat during rest [Citation64,Citation68,Citation69] and physical activity in the heat [Citation60,Citation61,Citation65–67,Citation70–72] leading to more pronounced elevations in core body temperature. Age-related reductions in whole-body heat loss occur at a rate of ~4% per decade, but this rate is not appreciably modified by sex (see below for additional information) [Citation67], although these differences are dependent on the level of heat stress [Citation61,Citation65–67].
To date, much of our understanding of the effects of aging on thermoregulation has come primarily from studies employing exercise-heat stress models, which can overestimate the level of heat strain experienced during indoor overheating [Citation60,Citation61]. Consequently, our understanding of the physiological basis for the increased risk experienced by older adults during EHE has been limited. While some studies have assessed age-associated changes in physiological strain during a resting heat stress, until recently these were limited to short-duration heat exposures (≤3 hours) [Citation64,Citation68,Citation69]. These studies show that relative to their younger counterparts, older adults experience greater elevations in core body temperature and cardiovascular strain during brief exposures to extreme heat [Citation63,Citation64,Citation68,Citation69,Citation73–75]. Two of these studies assessed the time-dependent change in whole-body heat exchange employing a direct air calorimeter (a device that provides a precise measure of the heat dissipated by the human body) [Citation56,Citation76] and showed that older adults can store up to 80% more heat, during a brief exposure to hot (i.e. 2 hours at 36.5°C) [Citation68] and very hot (i.e. 3 hours at 44°C) [Citation69] ambient conditions. However, in both experimental conditions, heat balance was not achieved such that core body temperature had not stabilized suggesting that older adults do not achieve a state of heat balance within these brief 2- to 3-hour exposures. This is because the rate of heat gained by the body (i.e. due to the skin-to-environment gradient) exceeded the body’s ability to increase heat loss sufficiently to achieve heat balance during this brief heat exposure.
Recent day-long heat simulation studies have shown that it can take up to 6 hours for thermal equilibrium to be reflected in stable core body temperatures in young and older adults [Citation77]. However, the older participants stored more heat during the initial hours of exposure, resulting in a greater rise in core body temperature that was sustained for the duration of the day-long heat exposure (). This is consistent with well-established age-related alterations in thermoregulatory function [Citation78,Citation79]. Notably, while most older adults achieved a stable, albeit elevated core body temperature around mid-day, in some instances individuals experienced a sustained rise in core body temperature leading to heat-related exhaustion and/or heat-induced syncope.
Figure 3. Schematic depicting the change in physiological strain and mood state in an older adult exposed to indoor overheating during hot weather or an extreme heat event. Data represents physiological responses measured in older adults (n = 39; 61–78 years; 11 females) during a daylong (9-hour) exposure to indoor overheating (40°C) [Citation77,Citation201]. Tco, core temperature; bpm, beats per minute.
![Figure 3. Schematic depicting the change in physiological strain and mood state in an older adult exposed to indoor overheating during hot weather or an extreme heat event. Data represents physiological responses measured in older adults (n = 39; 61–78 years; 11 females) during a daylong (9-hour) exposure to indoor overheating (40°C) [Citation77,Citation201]. Tco, core temperature; bpm, beats per minute.](/cms/asset/20cebd93-34b1-4856-b232-2db0e4a1725c/ktmp_a_2361223_f0003_oc.jpg)
Age-related alterations in the cardiovascular response to heat stress are also thought to contribute to the increased risk of mortality in older adults during EHE [Citation36,Citation80–82]. This risk is in part mediated by the increased myocardial demand (i.e. increases in heart rate and contractility), which is exacerbated by reductions in coronary blood flow [Citation60,Citation81,Citation83,Citation84]. Heat stress induces an elevated demand on the circulatory system to redistribute blood flow to the skin while also maintaining hemodynamic stability (i.e. arterial pressure and tissue perfusion). The cardiovascular stress is particularly greater in older adults, who rely on a greater percentage of their maximum heart rate (which is reduced with increasing age) to facilitate an increase in cardiac output (i.e. to maintain skin blood flow for heat dissipation) during whole-body heat stress compared to young adults [Citation81,Citation85]. In addition, older adults also exhibit impaired hemodynamic responsiveness during heat stress, characterized by reduced increases in skin blood flow and cardiac output, primarily due to attenuated heart rate, compared to their younger counterparts [Citation86–88]. While the cardiovascular responses to a heat stress are generally sufficient to maintain arterial blood pressure in young adults [Citation89,Citation90], autonomic blood pressure regulation in older adults is blunted [Citation77,Citation80,Citation91], which can further limit the systemic cardiovascular response and regulation of blood pressure during heat stress [Citation77,Citation80,Citation92]. In this context, older adults are less able to redistribute blood from the central (e.g. renal and splanchnic blood flow) to skin vascular beds to support elevated circulatory demands required to increase skin blood flow and enhance heat exchange [Citation80]. These age-related changes place older adults at an elevated risk of heat-induced syncope (i.e. due to progressive deterioration in blood pressure regulation), a response observed during a recent study assessing thermoregulatory and cardiovascular function during a simulated day-long exposure to extreme heat [Citation77].
Heat-related mortality in older adults is also influenced by the duration of the EHE [Citation93], chronic health conditions such as diabetes, hypertension, cardiovascular disease, lung disease, mental and cognitive disorders (e.g. mood and anxiety disorders, schizophrenia) as well as conditions that limit mobility functional ability (e.g. arthritis, Parkinson’s disease) [Citation28,Citation59,Citation62,Citation94–100]. These health conditions can compromise a person’s ability to perceive and/or respond to the threat to health caused by a prolonged exposure to extreme heat [Citation28]. Further, fitness is an important mediator of the age-related decline in whole-body heat loss, such that sedentary individuals with low cardiorespiratory fitness demonstrate a greater age-related decline in whole-body heat loss [Citation65]. Importantly, increased fitness and regular engagement in physical activity has been shown to enhance the body’s physiological capacity to dissipate heat in older adults [Citation58,Citation101], and provide a greater level of protection against the adverse health effects associated with exposure to extreme heat.
Sex
Sex is a key modulator of the body’s physiological capacity to dissipate heat [Citation102,Citation103]. Relative to males, females have a reduced heat loss capacity (~5%) [Citation102–104], which is driven by differences in the activation of heat loss responses (i.e. skin blood flow and sweating) [Citation105]. Although there have been mixed findings with regard to the influence of sex as a mediating factor for heat-related mortality [Citation28,Citation106–110], some studies suggest that females are at a higher risk of heat-related mortality and morbidity compared to males [Citation47,Citation48,Citation106,Citation111–115], especially among older individuals (≥65 years) [Citation110,Citation114,Citation116–118]. For example, while the total number of deaths during the 2021 Western Heat Dome was similar between males and females, a greater proportion of older females died compared to their male counterparts [Citation28]. While the underlying causes for these differences remain unclear, greater cardiovascular strain may place females at higher mortality risk during EHE [Citation28,Citation81,Citation119,Citation120].
Hydration
Dehydration with or without concurrent electrolyte disturbances is an important cause of death during prolonged exposure to extreme heat [Citation121,Citation122]. It can also accelerate the deterioration in thermoregulatory and cardiovascular function, leading to a more severe physiological strain on the body [Citation122]. As water availability in the body decreases, so does the ability to sweat and increase skin blood flow during heat stress [Citation123]. While the evaporation of sweat is the primary avenue of heat dissipation during heat exposure, increases in skin blood flow play an important role in limiting the amount of heat gained from the environment by narrowing the skin-to-air temperature gradient [Citation56]. A dehydration-mediated reduction in skin blood flow would enhance heat gain during exposure to hot environments [Citation61,Citation124], especially in older adults who have a compromised capacity to dissipate heat [Citation61]. This would necessitate a greater sweat production (evaporative heat loss), which is blunted in older adults further compromising thermoregulatory stability during a prolonged exposure to extreme heat [Citation61]. This would be paralleled by greater cardiovascular instability owing to the greater strain placed on the cardiovascular system as the absolute reduction in the volume of fluid in the vascular system (hypovolemia) worsens the heat-induced relative hypovolemia resulting from reduced peripheral resistance [Citation125].
Older adults in particular are also vulnerable to shifts in water balance that can frequently result in dehydration [Citation126–131] especially during a prolonged heat stress [Citation130,Citation132]. This is driven by increased sweat loss, reduced daily fluid intake, diminished thirst response to dehydration, reduced capacity to conserve salt and water [Citation130,Citation133–135] as well as impaired renal water conservation [Citation130,Citation134,Citation136]. Further, medication use that impairs thirst (e.g. selective serotonin reuptake inhibitors, angiotensin converting enzyme inhibitors, anti-Parkinson drugs) or disturbs fluid balance (e.g. diuretic medications) can also worsen this response [Citation128,Citation129,Citation137]. These changes can in turn exacerbate age-related dysregulation in thermoregulatory and cardiovascular function during heat stress [Citation126], leading to heightened risk of adverse health outcomes during EHE [Citation2].
Chronic disease
Chronic diseases can increase the risk of heat-related morbidity and mortality [Citation3,Citation33]. Epidemiological studies show that those with underlying health conditions (e.g. cardiovascular, cerebrovascular, respiratory, renal, and neurologic diseases, and diabetes) are at greater risk of heat-related mortality, even with short periods of heat exposure [Citation3,Citation33,Citation138]. This can occur through decompensation of otherwise stable conditions due to lack of physiological reserve as well as through disease-related impairments in thermoregulatory responses. As overviewed in the following sections, various health conditions can worsen age-related impairments in heat dissipation, compromising heat tolerance and resiliency, leading to adverse health outcomes during indoor overheating.
Type 2 diabetes
Compared to the general population, adults with type 2 diabetes experience higher rates of heat-related morbidity and mortality during an EHE [Citation3,Citation33,Citation138–142]. In parallel, hospitalization, and emergency department visits during an EHE increases for those living with type 2 diabetes, especially in older (>65 years of age) individuals [Citation143]. Exposure to heat can lead to decompensated co-morbid cardiovascular or respiratory disease in patients with type 2 diabetes [Citation33]. Additionally, prolonged heat exposure can worsen glycemic control [Citation138,Citation144,Citation145], mediated by changes in glucose tolerance [Citation138,Citation144], elevations in insulin absorption in insulin-treated diabetic individuals [Citation145] and other alterations.
The many heat-related health risks and excess deaths associated with type 2 diabetes can be linked to a worsening of age-related decrements in the body’s physiological capacity to dissipate heat [Citation146,Citation147]. The presence of peripheral or autonomic neuropathy, duration of diabetes, and hemoglobin A1c are considered important factors mediating the level of impairment in heat loss [Citation33,Citation138,Citation147–151]. The presence of macro- and microvascular complications as well as diabetic kidney disease can further compromise thermoregulatory and cardiovascular function [Citation147]. Moreover, individuals with type 2 diabetes, especially in those with diabetes-related complications are more likely to experience dehydration during an extreme heat exposure, further limiting their ability to mitigate potentially dangerous increases in core temperature [Citation138]. While the presence of type 2 diabetes is associated with a worsening of age-related reductions in local heat loss responses of skin blood flow and sweating, recent reports showed these differences do not translate to differences in whole-body heat loss during rest in hot environments [Citation73]. For example, a brief 3-hour exposure to extreme heat (44°C) induced a similar change in whole-body heat loss and increase in body heat storage and core body temperature in resting individuals with and without controlled type 2 diabetes [Citation73]. This observation was more recently extended to a day-long (9-hour) exposure to hot ambient conditions (40°C) [Citation77].
Hypertension
Hypertension is associated with greater heat-related morbidity and mortality [Citation3,Citation33,Citation40-152], though this is not a universal finding [Citation33]. Hypertension is characterized by elevated peripheral resistance and is accompanied by a variety of peripheral circulatory changes, including hypertrophy of the vascular smooth muscle [Citation153] and vascular rarefaction [Citation154]. Each of these changes can compromise skin blood flow which is essential for the dissipation of heat and the regulation of core body temperature during heat stress [Citation155]. While the effects of hypertension on skin perfusion have yielded mixed findings under laboratory-based heat simulation trials [Citation155–157], reductions in skin blood flow have been consistently observed during physical activity among individuals with controlled hypertension [Citation158,Citation159]. While there has been limited research on the effects of hypertension on sweating, it does not appear to have a marked effect on sweat production [Citation160,Citation161]. This is supported by a recent report that relative to healthy counterparts, individuals with uncomplicated, controlled hypertension do not show a reduced capacity to dissipate heat during physical activity in the heat, regardless of the type of antihypertensive medications [Citation162]. However, it should be noted that the use of antihypertensive medications (i.e. diuretics, vasodilators, β-blockers) may significantly reduce heat tolerance through blunting of vasomotor and hemodynamic impacts [Citation163,Citation164].
Overweight and obesity
Epidemiological studies demonstrate an increase in morbidity and mortality in obese individuals during EHE [Citation3,Citation165]. Overweight and obese individuals demonstrate blunted skin blood flow and sweating during heat stress, which is paralleled by a reduced tolerance to heat [Citation166,Citation167]. An overweight or obese person has a higher body-fat mass, which results in a higher core body temperature for a given rise in body heat storage due to the fact that the specific heat capacity of adipose tissue is less than that of fat-free mass. Moreover, overweight, and obese individuals have a lower surface-area-to-mass ratio that can limit whole-body heat dissipation, exacerbating heat storage during heat exposure. When combined with reductions in heat loss responses of skin blood flow and sweating, overweight or obese individuals are thought to be at greater risk of experiencing a heat-related injury or death [Citation33,Citation168]. Notably, nearly 40% of the decedents of the 1993 heat wave in Philadelphia were overweight, while all of the younger victims (aged <50) were obese [Citation169]. Whether these observations are due to obesity-related impairments in heat dissipation remains unclear.
Obesity can also compound other heat-vulnerability factors. For example, older adults tend to have greater body fat and less muscle mass than younger adults, with these differences being more pronounced in individuals with type 2 diabetes and/or hypertension [Citation170,Citation171]. While these age-related changes are mediated by numerous factors such as changes in hormone signaling, metabolic activity, and diet, their impact on the body’s physiological capacity to dissipate heat can be profound. This is supported by a recent report which showed that in adults aged 20–70 years, higher body fat content was associated with a greater reduction in whole-body heat dissipation [Citation172]. While it is not possible to determine if obesity per se may worsen decrements in heat loss in people with type 2 diabetes, in-patient hospital admissions data demonstrates that obese individuals with and without type 2 diabetes have a comparable relative risk for heat-related illness [Citation33].
Cardiovascular disease
Cardiovascular diseases such as coronary artery disease, congestive heart failure, peripheral arterial disease and others can render older individuals less resilient to heat stress [Citation30,Citation80,Citation173] and more vulnerable to heat-related injuries and death [Citation3,Citation174–177]. When heat-related conditions were identified as a contributing factor, as opposed to the primary cause of death, cardiovascular diseases were often listed as the underlying cause [Citation3,Citation174–178]. Studies show that cardiovascular mortality increases by as much as 6% for a 1°C increase in ambient temperature above normal conditions, with some reporting differences or no changes in the temperature–mortality relationship between males and females [Citation110,Citation179–182]. For example, a recent systematic review which assessed the relationship between cardiovascular disease and heat-related morbidity and mortality in the previous 30 years showed that the relative risk of cardiovascular disease morbidity and mortality increased by 2% and 5% for females compared to males, respectively, for every 1°C increase in ambient temperature above normal levels [Citation183].
Exposure to heat for individuals with cardiovascular disease is associated with a blunted hemodynamic response as evidenced by a reduced heart rate and blood pressure [Citation184–186]. This is also paralleled by reduced skin blood flow [Citation186,Citation187], which exacerbates body heat storage, and increases in core body temperature during heat exposure. For example, individuals with preexisting cardiac dysfunction have a reduced ability to increase cardiac output sufficiently to maintain adequate skin blood flow when core body temperature is elevated [Citation188]. Sweat production does not appear to be affected in individuals with cardiovascular disease [Citation185,Citation186,Citation189]. However, during prolonged exposure to high heat conditions, a sustained elevation in sweat production can lead to a greater state of dehydration, exacerbating the burden placed on thermoregulatory and cardiovascular systems [Citation61]. Even a small reduction in hydration status in older adults (i.e. 1% of body weight deficit) can compromise thermoregulatory and cardiovascular function [Citation61]. Moreover, sustained elevations in sweat production can lead to hemoconcentration that can increase the risk of coagulation, and subsequently cerebral and coronary thrombosis and stroke [Citation190].
Respiratory disease
Exposure to high ambient temperatures can place a significant burden on the respiratory system [Citation48]. Individuals with pulmonary disorders are at higher risk of heat-related morbidity and mortality during an EHE [Citation3,Citation33,Citation39,Citation191], with respiratory-related mortality increasing by 18.7% for each 1°C increase above normal ambient conditions [Citation192]. In the absence of heat-adaptive strategies, rising global temperatures are projected to cause a 1.35-fold increase in heat-related mortality of respiratory disease over the next decades [Citation193]. To date, the physiological mechanisms contributing to the increase in mortality observed during heat exposure in individuals with respiratory disease remains unclear. However, studies suggest that changes in air quality that often accompany warmer conditions may be a mediating factor [Citation194,Citation195].
Cognitive function
Cognitive awareness of environmental conditions and the ability to understand and undertake adaptive behaviors (e.g. increase fluid intake, wearing less clothing, opening windows, going to a cooler basement, using air conditioning) are important factors mediating a person’s risk of experiencing a heat-related injury during hot weather [Citation196]. However, brief exposures to extreme heat can compromise cognitive function (e.g. memory, concentration, attention, reasoning, problem solving and comprehension) especially in older adults and individuals with chronic disease [Citation16,Citation17]. In parallel to their impaired capacity to dissipate heat, older adults have a reduced ability to sense heat and therefore initiate appropriate behaviors to alleviate heat stress. This includes having a lower subjective level of thirst, and reduced water intake while dehydrated relative to younger adults [Citation126,Citation133,Citation136,Citation197].
Healthy older adults require greater changes in thermal and cardiovascular strain before initiating behavioral responses compared to their young adult counterparts [Citation198,Citation199]. The same also appears to be true in older adults with common chronic health conditions such as hypertension and type 2 diabetes [Citation200]. Consequently, they are likely to experience greater physiological strain than healthy young adults while maintaining the same behavioral response. A recent report showed that while older adults experience a heightened thermal strain as assessed during a simulated daylong (9-hour) exposure to indoor overheating (40°C), they did not experience greater self-reported environmental symptoms or mood disturbance relative to young adults [Citation201]. Moreover, older adults with hypertension and/or type 2 diabetes reported lower symptom scores and mood disturbance compared to young adults and their age-matched counterparts despite experiencing similar levels of thermal strain as older adults without these chronic conditions [Citation201]. Taken together, these findings indicate that relative to young adults, older adults may have an altered ability to perceive a heat-induced elevation in physiological strain. Further, while some older individuals change their behavior during an EHE, others do not perceive themselves at risk due in part to the fact that they do not consider themselves to be of old age or at risk during exposure to heat [Citation202]. These findings are important given that perceptions of the health risks of heat can also shape the actions and decisions taken by individuals to reduce these risks [Citation171].
Mental and behavioral disorders
Exposure to high temperatures can worsen symptoms among those with mental and behavioral disorders [Citation10,Citation11] which may compromise their ability to perceive and respond to elevations in physiological strain. Moreover, individuals impacted by these conditions may be less heat tolerant [Citation203]. Compared with the general population, persons with mental health problems and behavioral disorders often experience poorer overall health with higher rates of morbidity and mortality, especially during EHE [Citation3,Citation10,Citation39,Citation203,Citation204], with older adults living with mental health disorders being the most affected [Citation203]. Heat-related deaths during the 2021 Western Heat Dome were higher among persons with depression as well as mood and anxiety disorders [Citation28]. Another recent study which examined the risk of death for people with different chronic conditions during this EHE found that mental illnesses were among the conditions that left people most susceptible to death [Citation205]. In particular, those with schizophrenia were at the highest risk, with a three-fold greater risk of a heat-related death [Citation205]. Moreover, it has also been shown that hospital admissions for individuals with mental and behavioral disorders (e.g. symptomatic mental disorders, dementia, mood (affective) disorders, neurotic, stress related, and somatoform disorders; disorders of psychological development, and senility) increased at temperatures exceeding 26°C [Citation203]. Similarly, nursing home residents with known dementia experienced increased agitation and disruptive behavior while exposed to temperatures higher than 26°C, with dementia deaths increasing during high-temperature extremes [Citation11,Citation203].
Medications used to manage mental and behavioral disorders can also interfere with the body’s normal thermoregulatory responses [Citation93,Citation206,Citation207] resulting in increased hospital admissions [Citation204,Citation208] and mortalities [Citation209–211] during EHEs. Medication such as anti-psychotics, anti-cholinergics, anti-depressants, sedatives, and mood stabilizers, which are used to manage mental and behavioral disorders (e.g. dementia, psychosis, mood and anxiety disorders) can blunt the activation of heat loss responses of skin vasodilation and sweating [Citation212,Citation213], compromising whole-body heat dissipation. In the absence of a sufficient capacity to dissipate heat, potentially dangerous increases in core body temperature can occur during even brief exposures to hot environments. This can be exacerbated by increases in metabolic heat production induced by some medications [Citation56], which would elicit a greater requirement for heat loss to maintain core body temperature within safe limits especially during exposure to hot weather.
Influence of built environment on indoor temperatures during an EHE
The characteristics of the built environment can have profound effects on population exposure to excess heat and play a key role in increasing the risk of overheating in dwellings and heat-related mortality, especially in heat-vulnerable individuals. However, the specific population groups and neighborhoods that are at risk vary between and within cities due to factors associated with differences in climate, culture, demography, and adaptations available [Citation96,Citation214–216]. Individuals living in large urban centers are particularly impacted as they experience higher temperatures and death tolls during an EHE due to the UHI effect.
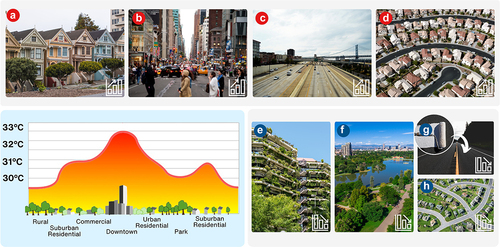
Within cities, the increase in temperature observed during hot weather and EHE is in large part defined by the combination of numerous contributing factors such as high-rise buildings, building density, green space, industrial land use, and anthropogenic heat sources [Citation217]. Consequently, different approaches to urban planning and the diverse nature of city designs can lead to large differences in temperatures between neighborhoods and differences in the risk of heat-related morbidity and mortality [Citation218,Citation219] during an EHE. Implementing local-level adaptation strategies such as increasing vegetation, trees, and green roofs, as well as access to green space can help reduce UHI effects and mitigate this risk. However, this calls for ambitious adaptation that would require significant investment in green infrastructure, which may be costly in older established communities. In this section, we examine how the built environment affects the local thermal environment during EHE, adversely impacting indoor temperature and leading to an increase in heat-related morbidity and mortality in heat vulnerable populations (). Further, we examine how UHI mitigation strategies can measurably reduce this risk.
Figure 4. Determinants of the urban thermal environment. Factors such as high building density (panel A), lack of green space (panel B), paved surfaces (panel C) and others can worsen (upward pointing arrow, bottom right of each panel) the urban heat island effect and indoor overheating. In contrast, the addition of green infrastructure (panel E), parks and bodies of water (panel F), use of high-reflective materials (panel G), increased vegetation and green space around dwellings (panel H) and others can lessen the impact (downward pointing arrow), lowering outdoor temperature and reducing the risk of indoor overheating.
Built environment induced UHI effect
Rapid urbanization over the past few decades has substantially affected urban thermal environments. As a result of such urban growth, local climate conditions can be highly affected, generating an impact on indoor thermal stress due to unintended UHI effects. The thermal properties (i.e. heat absorption, capacity, conductance, and albedo) of the surfaces and materials found in urban landscapes, the diminished evapotranspiration from reduced natural vegetation and increased impervious surfaces (e.g. paved roads, concrete buildings), and the waste heat production from human-related activities all contribute to the UHI effect [Citation220]. However, temperatures across urban neighborhoods and communities during hot weather or an EHE can vary significantly due to local differences in the built environment and the UHI effect.
The UHI effect is observed in any urbanized area, although it is usually more noticeable in larger metropolitan cities as urban expansion replaces natural land cover with dense concentrations of pavement, buildings, and other surfaces that absorb and retain heat [Citation8,Citation152,Citation218,Citation221–224]. The UHI can worsen the effects of EHE [Citation225] as it can typically produce elevations in temperatures by ~2–4°C higher [], and in more extreme conditions increases of as a high as 10°C compared to surrounding rural regions [Citation4–8]. The intensity of the UHI, and temperature differential between urban and rural communities is also worsened by the fact that rainwater runoff from impervious roadways, sidewalks, buildings, and other areas is collected in stormwater drainage systems leaving relatively limited moisture in the urban landscape [Citation226]. This limits evapotranspiration and increases sensible heating (greater heat gain) of the local atmosphere [Citation227]. Increases in anthropogenic heating worsens this response, intensifying the UHI effect and air conditioning energy consumption in urban dwellings [Citation4,Citation228]. Ultimately, changes in land surfaces caused by urbanization lead to potentially harmful urban climates for vulnerable inhabitants during an EHE [Citation227], evidenced by greater rates of heat-related morbidity and mortality occurring in cities as compared to nearby suburban and rural areas [Citation8,Citation223,Citation229–234].
In addition to experiencing higher daytime temperatures, residents living in large urban centers experience higher nighttime temperatures [Citation220]. This is because, the large amount of heat (and solar heating) that is absorbed and stored by the impervious surfaces of surrounding buildings and road (i.e. concrete and paving) is slowly released at night. Consequently, the nighttime is when the temperature difference between urban and rural areas, and hence the UHI intensity, is typically largest [Citation220]. Under such circumstances, the decline in outdoor temperature during the evening is insufficient to promote the cooling of dwellings. Consequently, individuals residing in dense urban communities are exposed to extended periods of elevated temperatures during EHE, which includes elevated nighttime temperatures [Citation235]. The impact of such an elevation of urban temperature on population health was evidenced during the 2003 heat wave in Paris, France, where high nighttime temperatures were associated with increased mortality [Citation236] (readers are referred to Heaviside et al. [Citation237] for a more comprehensive review on the effects of UHI and human health).
Socioeconomic determinants of the urban thermal environment
UHIs are an important community-scale risk factor such that higher UHI intensities tend to occur in centrally located parts of the city, where people are often more likely to be socially disadvantaged. In turn, these socioeconomic factors can modify how harmful the UHI effect can be and increase vulnerability to the UHI effect among urban populations [Citation25,Citation238]. Moreover, several reports have identified a strong relationship between neighborhood social conditions, land cover, and surface temperatures in large metropolitan centers [Citation218,Citation219,Citation239]. Warmer areas within cities are associated with neighborhoods with higher settlement densities and reduced green space that experience higher mortality rates during an EHE relative to less dense areas in the city [Citation218,Citation219,Citation239]. Further, communities most affected by the UHI effect are also associated with populations that have lower levels of social integration and support systems to help cope with extreme heat [Citation222,Citation240]. Notably, these areas are typically representative of the more deprived neighborhoods where excess death during an EHE tend to be the highest [Citation241]. This can in part be attributed to the higher percentage of residents of low socioeconomic status including a higher number of heat-vulnerable residents [Citation219]. The heterogeneity of EHE on heat-related morbidity and mortality across neighborhoods underscores the critical need for improved heat preparedness and management strategies that specifically targets high-risk communities, where the built environment plays a significant mediating effect on human health [Citation242,Citation243]. Factors mediating urban design and social determinants must be considered when weighing the risk(s) of heat-related mortality in different neighborhoods [Citation244].
Reducing the UHI effect to protect health
In recent years, an increasing number of municipalities have implemented UHI-reduction measures to lower outdoor air temperature that would otherwise magnify health risks during EHE []. There are several local adaptations that can be implemented to significantly reduce air temperature and the level of heat stress residents face [Citation245]. These changes focus on modifying the thermal environment of cities by implementing sustainable mitigation strategies that can lower the heat gain and retention and increase the heat loss to reduce the UHI effect and the potential health risks caused by EHE [Citation245] ().
While UHI mitigation strategies can measurably reduce heat exposure [Citation246], identifying neighborhoods or communities of greatest risk and selecting appropriate mitigation strategies can present a significant challenge. UHI intensity can vary significantly across neighborhoods within the large urban centers, such that the thermal environment can be vastly cooler in less built-up areas of the cities while hotter conditions may be observed in highly dense areas during an EHE [Citation218,Citation239]. The highly variable outdoor climates within cities can lead to significant spatial variability in the mortality response to an EHE [Citation219]. The local-scale variability in climate can in large part be attributed to the variations in the built environment due to differences in urban design, land use mix, vegetative cover, and other factors [Citation247]. For example, roadway area density is an important determinant of UHI intensity during hot weather, whereas the tree canopy coverage is a primary factor distinguishing warmer from cooler areas in large metropolitan cities [Citation247]. Increasing the albedo (i.e. how reflective a surface is) of cities by creating green infrastructure in urban areas and employing natural heat sinks to dissipate excess heat is an effective UHI mitigation strategy [Citation248] shown to reduce heat-related mortality by as much as 10% [Citation249–251]. Consequently, identifying and prioritizing local-level mitigation in high-risk neighborhoods, such as prioritizing greenspace, is critical in reducing the risk of overheating in dwellings during hot weather and EHE, ultimately saving lives [Citation3,Citation27,Citation252].
Urban green infrastructure
Increasing the amount of vegetation and trees in a city can be an effective, and relatively affordable method to reduce urban air and surface temperature during hot weather [Citation253–255] and decrease the risk of heat-related morbidity and mortality during EHE [Citation8,Citation27]. Indeed, expanding urban green space and/or adding green corridors cools built-up areas and blunts the UHI effect [Citation256–258] (). A recent report showed that more than 4% of summertime deaths in 93 European cities in 2015 could be traced back to the effects of UHIs. However, they showed that heat-related deaths could be reduced by one-third by simply increasing city tree coverage by 30% [Citation252]. Further, in a recent assessment of heat-related deaths from the 2021 Western Heat Dome, green infrastructure was identified as an important determinant of heat-related mortality [Citation27].
The reduction in environmental temperature is facilitated by both reducing the number of heat-absorbing materials exposed to solar radiation through enhancing tree coverage and increasing evaporative cooling from both the soil surface and vegetation (evapotranspiration) within the environment [Citation259,Citation260]. During evapotranspiration, water is converted to vapor, a process which necessitates water molecules absorb heat. The energy transfer of water into vapor results in a cooling effect like that of sweat evaporation from the skin surface. An increase in evapotranspiration will increase latent cooling and will subsequently decrease local ambient temperatures by as much as 6°C [Citation253,Citation257,Citation258,Citation260–262]. This results in a reduction in conductive and convective heat gain [Citation259] in local area buildings and houses.
In addition to providing cooling (via evapotranspiration) critical for reducing the intensity of the UHI, tree canopies are an optimal solution for shading both canyon surfaces (i.e. a place where the street is flanked by buildings on both sides creating a canyon-like environment) and the pedestrian space (). Thick or dense canopy trees, and in particular broadleaf trees provide particularly good shade [Citation263]. However, while trees can provide shade during hot summer days and reduce the intensity of the UHI effect, they can also trap heat under their canopy at night contributing to the elevations in nighttime temperatures during an EHE [Citation262,Citation264]. Consequently, to enhance the cooling effect on the overheated urban environment, trees in high-temperature zones within the city such as in canyon surfaces, should be adequately spaced to enable good ventilation and heat to escape [Citation259,Citation264]. This will facilitate greater cooling during both the daytime and nighttime.
Ultimately, to substantially reduce urban heating, widespread implementation of green infrastructure is required to maximize the cooling impact of vegetation across neighborhoods. While access to green space in many cities may be limited, studies show that the addition of small courtyards can also provide important benefits in reducing air temperature in highly dense neighborhoods [Citation258]. Increasing vegetation and access to green space especially in heat-vulnerable communities can play an important role in curtailing the level of heat stress individuals may experience during an EHE [Citation231,Citation265], which includes mitigating the risk of indoor overheating [Citation266]. Increasing access to green open space across the city (e.g. grassed areas) with a relatively sparse tree canopy, such as public parks, sports fields, and others can also have a cooling effect on urban environments. They can serve as local cool zones in hot urban areas, that can be easily accessible to people [Citation267]. Depending on their size and position within a neighborhood, air flow across these open spaces can cool urban areas downwind [Citation259,Citation264]. While larger open green spaces within a city may significantly reduce temperatures at the city scale [Citation253,Citation257,Citation258,Citation260–262], many smaller spaces, strategically distributed across the city can also provide significant local cooling benefiting many neighborhoods [Citation268]. This approach may be particularly beneficial for established cities, where incorporating large open green spaces may not be feasible or possible. This is especially important for high-risk communities, where the UHI effect on population health is most evident during EHE [Citation242].
Increasing surface albedo
Within urban environments, roofs, and paved surfaces account for more than 60% of the urban landscape [Citation269] (). Given that roofs and paved surfaces are generally constructed out of materials (e.g. bitumen, concrete, and terracotta) that promote heat storage, their contribution to the UHI effect is significant as they can absorb the sun’s radiation, heating both surface and air temperature [Citation270,Citation271]. The implementation of reflective materials in roofs and pavements can provide considerable cooling and heat mitigation potential [Citation249,Citation271,Citation272]. Increasing surface albedo decreases the absorption of solar radiation (and other radiant heat sources) mitigating the impacts of the UHI by reducing surface and air temperatures. By making exposed impermeable surfaces, like roofs, pavements, and roads more reflective using high-reflective materials (e.g. light colored materials) for their construction, or painting existing surfaces light colors (e.g. white) decreases the absorption of solar radiation (and other radiant heat sources) mitigating the impacts of the UHI by reducing surface and air temperatures [Citation245].
Reflective materials can exhibit surface temperatures up to 15°C cooler than conventional materials of the same color [Citation258,Citation273] (). Consequently, the thermal impact of reflective materials in cities can be significant with some reports demonstrating their use can reduce peak ambient temperature in cities by up to 1.5°C [Citation274]. As discussed, the reduction in air temperature is because heat is less easily absorbed and retained. However, the impact of increasing surface albedo on air temperature is also dependent on several landscape parameters, green spaces, street canyons (i.e. street flanked on either side with tall buildings creating a structure that’s like a canyon) and others. Studies show that greener cities with a higher percentage of urban streets benefit more from a potential albedo increase [Citation275].
Green roofs
While increasing albedo can cool the urban climate and lessen the impacts of EHE, the addition of green roofs is another adaptation strategy that can be implemented relatively quickly while providing a significant cooling benefit especially in high-density urban areas (). Introducing vegetation at roof level increases evapotranspiration, which enhances local cooling including reducing the risk of indoor overheating. Vertical “green walls” or green facades can also serve a similar function as evapotranspiration impacting microclimate cooling.
During the day, roofs are some of the hottest surfaces in urban areas [Citation254]. Green roofs are an ecological solution that can reduce solar radiation exposure to concrete and heat absorbing materials in urban environments [Citation276]. Green roofs display lowered daytime temperatures compared to traditional roofing materials (e.g. asphalt shingles) [Citation277]. Like urban green spaces, introducing vegetation at roof level provides some shading while increasing evapotranspiration, which enhances local cooling. The net result is a cooling of the roof itself and the local environment by 1–2°C [Citation260,Citation278]. One report showed that for every 1,000 m2 increase in green roof area, air temperature decreased by 0.4°C [Citation279]. However, it should be noted that green roofs have the potential to have a small nighttime warming effect due to solar radiation accumulated during daytime hours that is subsequently released during the night [Citation280].
There are several factors that can affect the effectiveness of green roofs (and green walls) in reducing urban heating. This includes local climate, vegetation type, density, soil depth, irrigation, and maintenance. For example, cities in dry climates demonstrate the highest cooling effect of green roofs, while those in hot, humid climates show the lowest cooling potential [Citation281]. Green roofs with unmanaged, relatively dry soil provide limited cooling relative to green roofs with abundant soil moisture [Citation282]. Moreover, those with increased irrigation can have a comparable effect in reducing the UHI intensity to the use of cool roofs (i.e. with an albedo value of 0.7) [Citation282]. However, in many cases the albedo of green roofs may be lower than the reflectivity of the original roofing material [Citation283], thereby limiting their cooling effect. Given that cool roofs are simple in their function of reflecting solar radiation, they may represent a more practical and cost-effective strategy to mitigate UHI intensity as compared to green roofs [Citation283].
Determinants of the indoor thermal environment during an EHE
Indoor overheating is a potentially fatal health hazard evidenced by the fact that most heat-related fatalities occur in the home [Citation26–28,Citation284], where individuals spend ≥80% (older adults as much as 90%) of their time [Citation49,Citation50,Citation285,Citation286]. Without respite and access to cooling, high external ambient temperature can lead to overheating in homes that can have catastrophic consequences on health. Indoor overheating during hot weather or an EHE can adversely impact mental health and physical functioning [Citation287], diminish sleep quality [Citation287,Citation288], reduce thermal comfort [Citation289], and increase morbidity and mortality among the most vulnerable [Citation60,Citation290], especially those living in low-quality housing without mechanical cooling (i.e. air conditioning, heat pumps) [Citation93,Citation291].
To mitigate this risk, health agencies worldwide recommend heat protective measures (e.g. cooling systems, ventilation, shading from direct sunlight) and regulatory action to prevent indoor overheating and safeguard the health and wellbeing of heat-vulnerable occupants [Citation14,Citation292]. However, this requires that the factors that define indoor temperature, such as where people live (i.e. built environment), the types of buildings people occupy and how the dwellings are cooled be considered [Citation44,Citation209]. For example, dwelling characteristics such as building year, lack of thermal insulation, absence of air-conditioning, living on upper floors of apartment buildings and other factors are associated with higher risks of heat-related morbidity and mortality, especially in the most vulnerable [Citation44,Citation47,Citation48,Citation209]. Notably, despite recognition that building characteristics are an important factor mediating heat-related mortality [Citation293], relative to young adults, older individuals are more likely to be living in sub-optimal dwellings that are prone to overheating [Citation294].
In recent years, much attention has been brought to defining the temperature thresholds at which health impacts begin to occur from indoor overheating. However, there has been a high degree of variability in what is considered an acceptable indoor temperature. This is likely because there are differences in how various groups of people respond physiologically and behaviorally to the same living environment. While some have recommended that indoor temperatures should not exceed 26°C to protect the most vulnerable [Citation295–297], others have suggested a lower temperature of 24°C [Citation14]. Health agencies and building standards agencies have also advocated that homes of heat-vulnerable occupants be maintained between 24°C and 28°C to prevent heat-related mortality and morbidity [Citation14].
Until recently, support for indoor temperature guidelines has largely been indirect, based primarily on location-specific outdoor ambient temperature-mortality and morbidity factors [Citation295,Citation296]. This ignores the fact that indoor and outdoor ambient temperatures can diverge markedly depending on the built environment. However, a recent laboratory-based trial quantified the effect of daylong (8-hour) indoor overheating on surrogate physiological outcomes (e.g. thermal and cardiovascular strain) linked with heat-related mortality and morbidity in older adults [Citation297]. Specifically, they assessed responses in older adults (average age 72 years) exposed to ambient conditions simulating an air-conditioned environment (22°C; control), the proposed indoor temperature upper limit (26°C), and temperatures experienced in non-air-conditioned homes (31°C and 36°C). Study findings showed that a single-day exposure to temperatures ≤26°C did not create an undue physiological strain in older adults and is sufficiently protective for vulnerable occupants. However, sustained exposure to temperatures greater than 26°C but less than 31°C could pose a risk to health in some adults, whereas sustained exposure to temperatures ≥31°C should be avoided for heat-susceptible populations whenever possible [Citation297] (). However, to reduce indoor temperature to the minimal risk threshold, and protect vulnerable occupants during EHE, it is important to understand how indoor temperatures vary widely between dwellings, and are influenced by outdoor temperatures, building characteristics and the presence of environmental control systems (i.e. ambient cooling). In the following section, we examine these factors and explore strategies and interventions to reduce overheating risk and protect vulnerable occupants during hot weather and EHE.
Figure 5. Dwellings without an air conditioner system or a heat pump system can overheat during hot weather or an extreme heat event placing the occupant(s) at risk of a heat-related injury or death. A recent report showed that maintaining indoor temperature at or below 26°C will ensure that occupants are protected (see ref [Citation297]).
![Figure 5. Dwellings without an air conditioner system or a heat pump system can overheat during hot weather or an extreme heat event placing the occupant(s) at risk of a heat-related injury or death. A recent report showed that maintaining indoor temperature at or below 26°C will ensure that occupants are protected (see ref [Citation297]).](/cms/asset/385736b1-291a-4e17-bb2d-f6f6df69d330/ktmp_a_2361223_f0005_oc.jpg)
Relationship between outdoor temperatures and indoor overheating risk
In recent years, an increasing number of studies have assessed the heat risk in homes through direct monitoring [Citation298–305] and indirect techniques (modeling) [Citation302,Citation306–310]. These reports demonstrate that occupants can experience periods of excessive heat stress indoors for extended periods during hot weather and EHE, although variation between homes is considerable with building characteristics considered to be an important mediating factor. While outdoor temperature explains only a small proportion of the variance of indoor temperature [Citation304], outside temperature during the preceding day(s) is known to have a larger influence on the indoor temperature than the actual, real time outdoor temperature. For example, one study showed a 1°C increase in the average temperature in the 24 preceding hours was associated with 0.36°C increase in indoor temperatures during the summer period of homes in a temperate continental climate (i.e., Montreal, Canada) [Citation304]. Another report showed that a 72-hour moving average of outdoor temperatures was highly related to indoor temperatures [Citation305]. However, the period of time (i.e. spring versus late summer) when an EHE occurs is also an important factor influencing the level of indoor overheating [Citation311]. This reinforces the fact that dwellings can retain heat from the preceding day(s) of high outdoor temperatures. For example, heat-related deaths attributed to the 2021 Western Heat Dome were recorded up to 11 days post-event due to sustained indoor temperatures [Citation28].
Building characteristics as determinants of propensity to high indoor temperatures
Building characteristics such as year of construction (e.g. dwellings built in the 19th century versus those built after the turn of the century) [Citation229,Citation303,Citation312,Citation313] and type of dwelling (e.g. row housing, detached house/bungalow, apartment) [Citation314], building orientation [Citation315–317] (i.e. cardinal direction of primary living spaces), building construction (e.g. external cladding, paneling and surface materials) [Citation318], level of building (e.g. upper or lower or high-rise apartment living and each distinct thermal zone within the dwelling) [Citation29,Citation319], quality of insulation [Citation320,Citation321], availability of indoor and outdoor adaptive technologies (e.g. air conditioning, window blinds/shutters) [Citation322], and availability of outdoor shading (e.g. vegetation cover, awnings and shaded areas around the home [external shutters, pergolas, and verandas]) [Citation323,Citation324] can enhance or reduce heat gain from the external environment during an EHE. While it is often not feasible to change many of the foundational building characteristics that are important modifiers of the effect of high indoor temperatures on the risk of indoor overheating, there are targeted modifications that can be made to improve the resilience of homes in advance of an EHE (). These are overviewed in the following sections.
Figure 6. Schematic depicting structural and design characteristics of the home that can reduce heat gain and heat retention. Modifying the home with operable energy efficient windows, employing different forms of shading (e.g. window blinds, window awnings, planting trees around the home), utilizing appropriate insulation and attic ventilation techniques can promote greater cooling of the home helping to achieve safe indoor temperature conditions (i.e. 26°C, see ref [Citation297]).
![Figure 6. Schematic depicting structural and design characteristics of the home that can reduce heat gain and heat retention. Modifying the home with operable energy efficient windows, employing different forms of shading (e.g. window blinds, window awnings, planting trees around the home), utilizing appropriate insulation and attic ventilation techniques can promote greater cooling of the home helping to achieve safe indoor temperature conditions (i.e. 26°C, see ref [Citation297]).](/cms/asset/4fcd2311-30e4-4b77-8da3-68cac2f53c7c/ktmp_a_2361223_f0006_oc.jpg)
Old versus new construction and retrofitted homes
Older buildings such as those built in the early to mid 19th century [Citation229,Citation303,Citation312,Citation313], especially in temperate climate zones (e.g. Europe, North America) have not been designed for high outdoor temperatures [Citation229,Citation303,Citation312,Citation313]. Typically, older buildings have a lower level of thermal insulation and a lower heat dissipation capacity, which can lead to high indoor temperatures during EHE [Citation325]. However, relative to older homes constructed of high insulating materials (e.g. brick, natural stone), older dwellings constructed with relatively lower levels of insulation such as vinyl paneling or wood siding, experience some of the highest indoor temperatures due to low heat resiliency [Citation303]. While buildings may act as an important modifier of exposure to the outdoor environment, and therefore the level of indoor overheating during an EHE [Citation300,Citation303,Citation305,Citation326], regardless of the age of the building, the urban landscape surrounding the home, plays an equally important role. Higher surrounding greenness and lower surface temperature are associated with reduced indoor temperatures and heat-related mortality, regardless of the age of the building [Citation231,Citation303,Citation327–329].
While improving home construction (e.g. insulation, windows) and modifying home surroundings could mitigate indoor heat exposure among heat vulnerable populations, overheating is still reported in recently refurbished and newly-built homes including those located in relatively temperate climates [Citation299,Citation301,Citation302,Citation330]. Notably, even energy-efficient retrofitted homes have been associated with increased heat-related mortality risk [Citation299,Citation301,Citation302,Citation330]. Indoor overheating has been shown to occur following complete energy-efficient adaptation of dwellings that includes enhanced insulation (e.g. insulation of walls, roof, and floor, triple glazed windows, other) and air-tightening [Citation221,Citation299,Citation302,Citation331,Citation332]. This effect has also been observed in new home construction, where despite more rigorous building codes mandating more energy-efficiency modifications, the risk of overheating remains high [Citation49,Citation299,Citation332,Citation333]. This may be an unintended consequence of a rapidly changing construction industry and building codes [Citation334] as the requirement for highly insulated and air-tight dwellings may be inadvertently increasing the risk of uncomfortable or excessive indoor temperatures during hot weather [Citation330]. For example, the use of retrofitted internal wall insulation in homes built in temperate continental climate increased living room and bedroom temperatures by 2.2°C and 1.5°C, respectively, compared to a non-insulated house [Citation335]. Similarly, another study showed that new homes constructed in the United Kingdom employing the Passive House Standard (i.e. an international construction standard for thermal resilience dictated by air tightness and insulation whereby buildings do not use more than 60 kWh/m2/year) not only displayed increased nighttime bedroom temperatures compared to typical residential buildings (a building standard whereby dwellings satisfy legal regulation), but 65% of the homes exceeded the safe indoor temperature criteria of 25°C [Citation336].
Home insulation and attic ventilation
Insulating the dwelling is considered to be an effective countermeasure to limit heat exchange between indoor and outdoor environments [Citation332] (). Where adequate insulation is not present, environmental heat (and cold) can enter the household via convection and conduction [Citation337]. While it is important to appropriately insulate the whole house, an often-forgotten entry point for hot air into the home is through the attic space [Citation322]. Poorly insulated attics can reach temperatures well in excess of 50°C, even in cool, temperate climates [Citation338]. Once an attic temperature is elevated, hot air within the attic will enter the home via convective and conductive heat transfer, leading to an increase in indoor temperature and a greater cooling requirement to maintain thermal comfort. However, utilizing appropriate insulation and attic ventilation techniques (e.g. use of ridge and soffit ventilation, hooded vents; see below) can minimize the risk of indoor overheating [Citation339]. For example, installing under roof insulation lowers attic temperatures by ~10°C which can subsequently reduce the indoor ceiling temperature by ~3°C [Citation339]. In addition, utilizing insulation with a higher insulative value within the attic can reduce attic temperature [Citation340].
Ventilation
Promoting natural (e.g. opening windows) or forced air ventilation (e.g. mechanical ventilation/pedestal fans) can mitigate the likelihood of indoor overheating. The process of ventilating an indoor environment is a simple procedure that either requires an input of outside air that flows through the dwelling [Citation341], or utilizes mechanically forced ventilation whereby air flow is promoted within the dwelling [Citation342]. As hot air rises within a confined space or building, air that is restricted to the building will continue to rise to the highest point possible before filling the room or dwelling, resulting in a progressive increase in indoor temperature. For example, within a multi-storey dwelling, vertical temperature can increase by as much 0.5–0.7°C per storey [Citation319]. However, if appropriate ventilation techniques are employed (e.g. opening windows, use of mechanical fan ventilation designed to move hot air away from living spaces and out of the building), warmer air will exit the building through gradient exchange with the outside environment.
Employing passive air ventilation practices such as buoyancy-driven ventilation (i.e. results from the density differences between interior and exterior air) can also promote a “chimney effect” where cooler air enters a home on the lower levels, absorbs heat in the room, rises, and exits through windows in the upper levels or via ventilation units [Citation343], mitigating indoor overheating. A study conducted in Houston, Texas (USA), a humid subtropical climate, showed that employing this technique can reduce internal heat load by as much as 31% [Citation344]. Similarly, utilizing an air exhaust vent installed on the peak of a roof (i.e. ridge vent) and soffit vents, which creates a natural air exchange beneath the roof deck within attic spaces has been shown to promote a 32% reduction in heat gain [Citation345] (). Moreover, mechanical ventilation techniques (i.e. electric fans and forced ventilation) that facilitate the influx and/or re-circulation of cooler air within the dwelling can lower the floor-to-ceiling temperature gradient by ~60%, provided an appropriate outlet for the hotter air is available [Citation346]. In addition, electric fans can be utilized to enhance the removal of hot air within the household by either drawing hot air upwards, or forcing the hotter air out of the building [Citation343].
Opening windows and promoting cross ventilation can be an equally effective strategy to reduce the risk of indoor overheating during hot weather. Utilizing smaller window openings for the inlets and larger openings for the outlets may increase air speed and improve the cooling effect [Citation343]. To highlight this point, predictive modeling performed on six apartment buildings in Melbourne, Australia showed that the number of hours during an EHE where apartment buildings are above maximum indoor temperature thresholds was reduced by ~70% when cross-ventilation practices were employed [Citation347]. However, due to safety concerns and building regulation codes (e.g. in some high rises windows can only be opened to less than 125 mm), this reduction may not be attainable given home occupants may not be willing or able to open windows to a degree sufficient to obtain high natural ventilation rates. In this context, many people during the 1995 Chicago EHE that claimed the lives of 739 individuals, refused to leave their residences, or open windows due to safety concerns (i.e. fear of crime), thus placing them at a heightened risk of exposure to indoor overheating [Citation152]. As noted above, to protect occupants from potential injury or death caused by falls, building codes in many countries limit window openings to no greater than 125 mm [Citation347,Citation348]. Limiting window opening to this level has been shown to restrict heat exchange by 32% from the optimal condition (i.e. fully opened window) [Citation347]. Nonetheless, significant reductions in indoor temperature can still be achieved when utilizing appropriate cross-ventilation techniques.
Shading
The shade canopy provided by trees around the home dissipates solar radiation emitted by the sun before it is in contact with surfaces that will absorb its significant heat load (e.g. concrete, cement, and brickwork) (). Limiting the amount of radiation exposure to the building can reduce surface temperatures by as much as 25°C [Citation349] and decrease the amount of direct radiation that can enter a home through windows and glass doors by ~80% [Citation350]. Given solar radiation can result in significant increases in mean radiant temperature [Citation351] (the area weighted mean temperature of objects surrounding the body [Citation352]) and thermal discomfort for dwelling occupants [Citation353], reducing the impact of solar radiation is critical for the maintenance of indoor temperature and thermal comfort, particularly during an EHE. Increasing tree coverage around the home can reduce conductive and radiative heat transfer to dwellings, lowering the risk indoor overheating and mitigating heat-related mortality during EHE [Citation252].
Shading windows by installing window shutters and awnings, and building shaded areas (i.e. created by pergolas and verandas) can also limit indoor overheating by lessening the amount of radiative heat gain from sun exposure [Citation323] (). In turn this can reduce the risk of heat-related mortality by as much as 60% in various dwelling types [Citation324]. Reports suggest that the use of exterior window shutters on high-rise apartment buildings, which are particularly prone to high-indoor temperatures during EHE, can reduce yearly heat gain by as much as 59% [Citation323], which can translate to indoor temperature reductions of upwards of 6°C [Citation354]. Reductions of 1.3°C to 1.9°C in indoor temperatures have also been modeled for homes employing window shutters during hot weather in temperate continental climates (e.g. United Kingdom) [Citation355]. Similarly, application of external shading reduces the cooling requirement by ~15.5% [Citation356] in homes located in a hot and humid, tropical climatic zone (i.e. Australia). Moreover, while not as effective as external shading systems, installation of interior curtains, drapes or blinds can reduce internal heat gain by as much as 33% [Citation357]. In turn, this can significantly reduce the requirement for mechanical cooling, and lower energy costs by as much as 50% [Citation358]. If access to internal or external shading systems are not a viable option, home occupants can use low-cost window films (i.e. residential window tinting) to reduce solar heat gain within the home.
Advanced reflective cooling materials
In recent years, the use of advanced reflective cooling materials to mitigate increases outdoor and indoor temperatures during hot weather [Citation270] has risen sharply [Citation273,Citation359–361] ( and ). These materials are characterized by high solar reflectance and infrared emittance values that influence the temperature of a surface [Citation362]. Increasing the solar reflectance lowers surface temperature of the material as solar radiation is reflected rather than absorbed. In turn this can decrease ambient temperature both outside and within a dwelling [Citation280,Citation363]. For example, dwellings constructed or retro-fitted with roofs and exterior walls containing cool reflective materials reduces heat storage compared to traditional materials reducing external building surface temperature by ~30°C [Citation363]. In turn this can reduce cooling load lowering energy consumption by ~36%, depending on the ambient conditions [Citation364].
Retrofitting existing roofs and external walls with high-albedo (e.g. light-colored) materials is another cost-effective strategy to mitigate solar heat gain and heat conduction inside the home [Citation365], as they reflect more of the sun’s heat energy relative to dark-colored materials (). Under peak solar loading (~1000 W/m2, such as mid-day during a hot summer day), the temperature of an insulated black surface (e.g. roof top, wall) can reach temperatures in excess of 50°C above ambient air temperature [Citation363]. In contrast, the temperature rise would be approximately 10°C if the roof were a white surface [Citation363]. Thus, employing light-colored materials for the roof or external walls of dwellings can reduce surface temperature and significantly mitigate the risk of indoor overheating [Citation363]. However, it is important to note that emissivity (ability to re-radiate energy absorbed back toward the sky) of the surface material will remain unchanged [Citation363].
When appropriate surface materials that increase albedo and emissivity are chosen in the construction or refurbishment of existing dwellings, there is a significant potential to cool the external and internal environment of the home [Citation366]. For example, the usage of polymer paints that combine high reflectivity with thermal radiation emission, whereby radiant heat is reflected via longwave radiation to colder, outer regions of the atmosphere, can result in radiative daytime cooling effects of ~6°C (i.e. the external surface temperature will be ~6°C lower than the ambient temperature) [Citation367,Citation368]. The flow-on effect of this reduction in surface temperature is a decrease in conductive heat transfer to the indoor environment and lowering of indoor temperature [Citation364].
Cooling the body during indoor overheating
Adaptative modifications in health behavior that include initiating home-based strategies for staying cool (e.g. air conditioner, fan use, misting fans, ice toweling, limb immersion, self-dousing (or showers), cold fluid ingestion) or activities outside the home (e.g. visiting cooling center) can significantly reduce heat-related morbidity or mortality [Citation39,Citation369–371]. This is because personal cooling strategies can increase the evaporative, conductive and convective cooling capacity of the immediate environment surrounding the body, limiting heat gain, and/or enhancing heat loss [Citation368]. In the following section, we examine several different heat-mitigation strategies that individuals can employ to protect themselves during hot weather or an EHE. However, it is important to recognize that the effectiveness of these heat-mitigation strategies is dependent on the ability and willingness of the individual to employ them, access to financial means and the social support needed to facilitate their use [Citation372] as well as appropriate perception of the immediate danger posed by heat stress [Citation201].
Electric fan use
Traditionally, the use of ceiling or pedestal mounted electric fans has been widely recommended by public health agencies worldwide as a strategy to mitigate indoor overheating in the home [Citation373,Citation374]. However, recent meta-analyses on heat-related deaths [Citation33,Citation39] and a Cochrane review [Citation375] failed to show a benefit of pedestal fan use in reducing morbidity and mortality during an EHE. Similarly, pedestal fan use has recently been discouraged when ambient temperatures exceed 35°C [Citation373–375]. Despite these observations, studies conducted in healthy, young adults suggest that pedestal fans may still be effective in mitigating dangerous increases in core body temperature in ambient temperatures as high as 42°C [Citation368,Citation376]. Additionally, some have recommended their use in ambient temperatures as high as 38°C, irrespective of humidity for older adults [Citation368,Citation377]. However, data from a recent biophysical modeling study showed that pedestal fans are not an effective personal cooling intervention when ambient air temperature exceeds 35°C [Citation378].
Electric fans can increase the flow of air around the human body, thereby directly enhancing the rate of heat dissipation by convection and evaporation. The rate of convection (provided ambient temperature does not exceed skin temperature (~35°C)) and evaporation from the skin is determined by the skin-to-environment temperature gradient and vapor pressure (i.e. humidity) gradient. When air temperature is cooler than the skin, the faster moving air displaces the warmer air surrounding the skin thereby increasing the skin-to-environment gradient, enhancing the rate of convective heat loss, which can make a person feel cooler. However, as the air-to-skin temperature narrows, the effectiveness of fans for promoting convective heat loss is reduced. Therefore, when air temperature exceeds skin temperature (~35°C), and the skin-to-environment gradient is reversed (i.e. air temperature exceeds skin temperature), fan use promotes convective heat gain, rather than heat loss. While fan use may still enhance heat dissipation by facilitating evaporative heat loss under such conditions, an elevated sweat production caused by a sustained elevation in core body temperature is required. Thus, fan use may be more beneficial in hot-humid weather (e.g. tropical or subtropical regions) where the evaporation of sweat is diminished, and the sweat produced drips off the body providing no cooling benefit to the body [Citation379,Citation380]. It is also important to consider that in environments characterized by high relative humidity, ambient temperature rarely exceeds skin temperature, thus convective heat loss will likely be facilitated.
While fans have been shown to enhance sweat evaporation [Citation65,Citation67,Citation381], whether this leads to a meaningful reduction in core body temperature (i.e. estimated to be ~0.3°C) [Citation377,Citation382] has not been thoroughly evaluated. Recent small-scale studies have assessed the effect of fans on physiological responses during brief (~120 minutes) exposures to extreme heat, albeit with mixed results [Citation379,Citation380,Citation382–384]. For example, electric fan use (~2 m.s−1) has been shown to limit the rise in core body temperature (−0·1°C) and cardiovascular strain (−8 beats per minute) in healthy young adults when exposed to hot-humid conditions (40°C, 50% relative humidity) [Citation382]. In addition, the same study showed that electric fan use increased the rise in core body temperature and heart rate in hot-dry (47°C, 10% relative humidity) conditions [Citation382]. Moreover, electric fan use (~4 m.s−1) has been shown to delay the rise in core body temperature and heart rate in healthy young adults during short duration (100 to 135 minutes) exposures to hot environments (42°C) with brief, successive increases in humidity over a range from 20% to 70% [Citation379,Citation380]. By contrast, when older adults (average age 68 years) were exposed to similar environmental conditions (42°C, increasing in relative humidity from 30% to 70%) for 100 minutes, electric fans accelerated the rate of core body temperature increase and cardiovascular strain [Citation379,Citation384].
Misting fans
Misting fans are a simple to administer intervention that can be employed in outdoor settings to cool the individual as well as the environment [Citation385]. As water mist is added to the air, ambient temperature decreases as the mist is evaporated [Citation386,Citation387]. Further, when water mist is evaporated from the skin surface, skin temperature and thermal discomfort is reduced [Citation385,Citation388]. Of note, various methods of misting have been shown to confer these cooling benefits [Citation388–393]. In hot-humid environments, where water vapor pressure is high, dry misting systems are preferable compared to traditional wet misting systems [Citation390]. This is because dry misting systems produce ultra-small water droplets that evaporate very quickly, and do not leave a wet sensation on the skin upon contact [Citation390]. In contrast, wet misting systems utilize a greater amount of water, and only a fraction of the moisture evaporates from the skin surface, leaving a wet sensation on the skin and thus compromising the cooling effect [Citation394], particularly when humidity is high. While misting has been shown to lower skin temperature and thermal discomfort [Citation388–392], which may reduce overall physiological strain, it remains unclear if mist cooling elicits significant reductions in core body temperature during rest in the heat especially in heat-vulnerable older adults. To date, one study has demonstrated that when high-school students were exposed to hot environmental outdoor conditions (~35°C) while completing light activities, misting fans lowered skin temperature by ~1.0°C [Citation388]. Therefore, while some studies demonstrate that misting can lower skin temperature and thermal discomfort [Citation388–392], which may reduce overall physiological strain, it remains unclear if mist-based cooling elicits significant reductions in core body temperature during rest in the heat especially in heat-vulnerable populations (e.g. older adults).
While misting fans may elicit some physiological benefits, their use can also influence a person’s perception of the environment [Citation388–392], such that individuals report feeling cooler and more comfortable when utilizing misting fans in hot conditions. This may be of concern for the most vulnerable who already have a reduced ability to sense heat [Citation199] and are less likely to participate in heat protective behaviors [Citation208,Citation369,Citation395]. However, further research is required to understand the interplay between risk perception and behavior change during prolonged exposure to high ambient temperatures.
Cooling towels
Damp-wet and/or iced-towels placed on the skin surface can lower an individual’s level of heat strain during a heat exposure. To elicit this cooling benefit, the wet or damp towel must be maintained at a temperature lower than that of the ambient environment, and the skin (~35°C) [Citation396]. The primary cooling effect provided by the wetted cold towel will be in the form of initial reductions in skin temperature via conduction [Citation397] between the hotter skin and the cold towel. As skin temperature is reduced a widening of the core-to-skin temperature gradient occurs [Citation398], enhancing heat transfer between the body and the environment [Citation399]. The effectiveness of wetted cold towels to reduce body heat storage and core body temperature is primarily governed by the surface area of the body covered by the towel and the temperature difference created [Citation397]. Moreover, as noted above to achieve an optimal cooling effect, it is necessary to ensure that the towel itself is wet. Indeed, as water is a greater conductor of heat than air [Citation400], greater rates of heat transfer will be possible when utilizing wetted cold towels compared to ice wrapped in a dry towel. As the temperature of the towel begins to equilibrate with that of the body, the effectiveness to cool diminishes.
Cold wetted towels have been shown to reduce core body temperature in young adults in hot environmental conditions [Citation396,Citation397]. Specifically, these studies [Citation396,Citation397] involved the use of wet towels containing large quantities of encapsulated ice (2.5–3.0 kg) placed around the neck, on the head, and on the lap during rest breaks in a tennis match [Citation396,Citation397]. While this quantity of ice may be effective in reducing core body temperature, it would require a large amount of freezer space to store the ice in preparation for an EHE and may not represent a feasible cooling option for many individuals. To this point, it is unlikely that the most heat-vulnerable people (e.g. older adults, the chronically ill, materially deprived) would have the physical capacity or financial capacity to employ this approach over extended periods of time without appropriate assistance from caregivers and other supports. Nevertheless, despite a paucity of appropriate supporting evidence, the use of wetted ice towels continues to be promoted as an effective at-home cooling mechanism during an EHE [Citation368]. Together, while potentially providing some cooling benefits, the utility of wetted ice towels as a home-based cooling intervention is currently unknown and requires further investigation, particularly within in-home trials that assess the ecological validity of the intervention.
Limb immersion
Owing to the high heat transfer coefficient of water relative to air [Citation400], limb immersion (or in some cases, the whole body [i.e. bathing]) is a powerful intervention to reduce thermoregulatory, perceptual and cardiovascular strain [Citation368]. Despite the marked reductions in local skin temperature, blood flow through the skin remains high when core body temperature is elevated [Citation401–404], which helps maintain an elevated cooling rate [Citation400]. Most studies investigating the efficacy of limb immersion in mitigating increases in physiological strain have utilized water temperatures ranging between 10°C and 30°C [Citation401–403,Citation405,Citation406]. While it is unsurprising that the cooling effect is amplified with lower water temperatures, the fact that immersion in water offers important cooling benefits even with higher water temperatures (i.e. 20–30°C) is important. From a practical perspective, employing tepid water would be far more appealing and safer (as the risk of cold shock response when immersing the limbs or body in cold water will be alleviated) for use by older adults and other heat-vulnerable groups. However, a recent report showed that submersion of lower legs in 20°C water for the last 40 minutes of each hour over a 6-hour exposure to indoor overheating failed to provide a meaningful reduction on core body temperature and heart rate in older adults (median age 72 years) [Citation407] (). Thus, while considered an accessible and practical in-home strategy, and potentially providing some cooling benefits, the efficacy of limb immersion for eliciting cooling requires further investigation.
Figure 7. While the use of home-based strategies for staying cool such as the use of limb immersion has been widely advocated by public health agencies, recent investigations demonstrate they are not effective for limiting increases in core temperature during indoor overheating. Data represents physiological responses measured in older adults (n = 17; 69–74 years; 8 females) during 6-hour exposure to indoor overheating (38°C) with (left panel) and without (right panel) of the feet to mid-calf in 20°C water for the last 40 minutes of each hour [Citation407]. Tco, core temperature; HR, heart rate.
![Figure 7. While the use of home-based strategies for staying cool such as the use of limb immersion has been widely advocated by public health agencies, recent investigations demonstrate they are not effective for limiting increases in core temperature during indoor overheating. Data represents physiological responses measured in older adults (n = 17; 69–74 years; 8 females) during 6-hour exposure to indoor overheating (38°C) with (left panel) and without (right panel) of the feet to mid-calf in 20°C water for the last 40 minutes of each hour [Citation407]. Tco, core temperature; HR, heart rate.](/cms/asset/16894864-4c84-48bb-8547-fc9f49408c4e/ktmp_a_2361223_f0007_oc.jpg)
Self-dousing
Wetting the skin surface using water dousing or via additional showering has been proposed as an effective method to alleviate heat strain in hot environments, especially when heat-related power outages do not permit the utilization of air conditioning or electric fans [Citation210,Citation408,Citation409]. As in the case of limb immersion, as cool or tepid water covers the skin surface, skin temperature decreases facilitating the widening of the core-to-skin temperature gradient [Citation398], thereby enhancing heat transfer and the cooling of the body. This is further facilitated by the evaporation of water from the wetted skin surface of the individual. While one study showed that water-dousing caused a small reduction in heart rate (~5 beats per minute), sweating and thermal discomfort during the final hour of a 2-hour rest period in both hot, humid and hot, dry environments, no reductions in core body temperature were observed [Citation410]. In contrast, along with a reduction in sweat rate, a reduction in core body temperature from elevated levels was observed in older adults who doused their t-shirts with tap water while resting in hot environments (42°C and 35% relative humidity) over a 2-hour period [Citation411].
Cold fluid ingestion
Dehydration with or without concurrent electrolyte disturbance is an important factor mediating thermoregulatory failure during heat stress. However, the temperature of fluids is an important consideration. Cold fluids are generally considered to be more palatable relative to warm fluids, and are subsequently recommended for maintaining hydration, and therefore thermoregulatory and cardiovascular function in hot environments [Citation412]. Cold fluid ingestion also plays an important role in mitigating increases in core body temperature and thermal discomfort in hot environments. The internal transfer of body heat to the ingested fluid when consuming cold fluid results in a lowering of core temperature [Citation413] and this effect may be further pronounced as fluid temperature decreases toward ~0°C [Citation413]. For example, cold fluid ingestion has been shown to lower core body temperature prior to exercise in athletic [Citation414] and heat vulnerable [Citation415] populations. However, this reduction in core body temperature is short lived as internal temperature quickly returns to similar levels during exercise [Citation416–418]. Moreover, relative to consuming tepid beverages, ingesting cold beverages can blunt the activation of the heat loss responses of skin vasodilation and sweating [Citation416–418], and limits whole-body heat loss [Citation417], leading to a greater increase in core body temperature [Citation419]. This response is thought to be associated with the activation of thermoreceptors in the stomach and esophagus that, in response to the sensation of ingested cold fluid, trigger a suppression of skin blood flow and sweat production [Citation418].
Therefore, in spite of the fact that the ingestion of cold fluids is more palatable and is associated with reductions in thermal discomfort [Citation413,Citation420], ingesting cold fluids (~1°C) may have limited benefits in reducing sustained increases in core body temperature during exposure to extreme heat conditions [Citation416]. However, these responses have yet to be assessed in older adults exposed to daylong indoor overheating who may consume refrigerated beverages throughout the day. Moreover, it is important to note that older adults may be unable to consume cold beverages due to sensitivity to cold and the risk of a cold-induced headache [Citation421,Citation422]. Notably, drinking cold fluids has also been shown to elicit vasovagal reactions in older adults which can lead to collapse [Citation423]. Although offering tepid rather than cold (<5°C) fluids during hot weather defies conventional wisdom, individuals will likely drink more if liquids are not cold [Citation424].
Heat acclimation
As overheating in buildings is expected to increase as global warming continues, proactive measures to increase heat resiliency in heat-vulnerable older adults are needed, especially for those without access to home cooling or reliable sources of electricity. While short-term heat acclimation through exercise in the heat has been shown to increase heat dissipation [Citation146] and decrease both the physical and mental stress imposed on individuals exposed to heat [Citation425], such protocols are not tenable for heat vulnerable older, sedentary adults. However, recent evidence suggests that passive heat acclimation protocols represent a viable alternative to exercise-based acclimation [Citation425], that could potentially be employed to reduce the negative health outcomes associated with exposure to indoor overheating. Recent preliminary observations have shown that brief (60-min) warm-water immersion (38°C) performed over seven consecutive days enhances heat-loss capacity in sedentary older adults (average age of 70 years), while also reducing cardiovascular strain [Citation426]. These preliminary results represent a critical finding as an increase heat-loss capacity would serve as an important safeguard for older adults exposed to indoor overheating due to lack of air-conditioning or EHE-related power disruption. While this preliminary data highlights passive warm water immersion as a promising strategy for increasing heat-resilience in heat vulnerable people, further research is needed to confirm its efficacy in more “real-world” environments and populations.
Ambient cooling
Household air conditioning is considered the single most effective and protective strategy to reduce heat-related mortality and morbidity in older adults and other heat-vulnerable populations [Citation3,Citation39,Citation141,Citation427–430]. Nearly all decedents (93%) of the 2021 Western Heat Dome in British Columbia, Canada resided in homes without an air conditioner or other cooling system [Citation27]. As discussed above, to protect vulnerable occupants, health and building standards agencies recommend maintaining indoor temperature at or below an indoor temperature limit of 24–28°C [Citation14,Citation292]. A recent study showed maintaining indoor temperature at an upper threshold of 26°C can limit thermal and cardiovascular strain and dehydration in community-living older adults [Citation297]. However, this requires that dwellings be equipped with mechanical cooling (i.e. air conditioners, heat pumps) sufficient to maintain indoor temperature at the recommended levels. Marginalized population groups or those living on low, fixed-incomes, may not have access to an air conditioner. People living alone and people who are marginally housed or housing insecure are significantly less likely to have air conditioning [Citation431]. In many cases, those with access to an air conditioner may not use it due to the financial burden of operating the unit as electricity usage can increase by ~40% when air conditioners are employed in homes [Citation432]. Notably, income level has been shown to be an important predictor of the use of an air conditioner [Citation433]. Of the decedents of the 2021 Heat Dome who had access to an air conditioner, only 15% had them operating at the time of death, many were found in warmer areas of the room/home and/or the air conditioner was malfunctioning (i.e. blowing hot air) [Citation27]. This highlights both access considerations, as well as factors that may have affected use (e.g. system malfunction, financial limitations to activating, cognitive impairment impacting ability to use).
While maintaining indoor temperature within the limits prescribed by health and building standards agencies will provide a protective cooling benefit, it may also limit the potential for natural acclimatization if indoor environments are “over-cooled.” A recent report showed that heat exposure during the summer months can enhance heat loss in both young and older adults (referred to as seasonal heat acclimatization). Those improvements led to a greater reduction in body heat storage in older adults indicating that seasonal acclimatization may confer greater thermoregulatory benefits with increasing age [Citation434]. With rising global temperatures and more EHEs, surging heat-related power shortages and outages are expected to become increasingly common as demand for cooling rises. It is important that alternative measures to increase heat resiliency such as heat acclimation (discussed above) in vulnerable populations be considered, especially for those without access to home cooling or reliable sources of electricity. This must include seeking more sustainable solutions such as modifying the built environment, implementing the use of passive cooling strategies, prioritizing greenspace, among others.
Cooling centres
Health agencies including the World Health Organization [Citation435], United States Centers of Disease Control and Prevention (CDC) [Citation436] and Health Canada [Citation374] recommend that a minimum of 1–3 hours per day be spent in an air-conditioned area in order to “ … help your body stay cooler when you go back into the heat” [Citation435]. However, direct evidence linking the use of cooling stations with reduced adverse heat-related health impacts is lacking [Citation436,Citation437]. In fact, a recent CDC-commissioned systematic review found no direct evidence linking cooling centers with reduced mortality or morbidity [Citation436]. Despite this, the CDC continues to recommend the use of cooling centers on the basis of a “high biological plausibility” for their effectiveness [Citation436].
In a recently completed study simulating use of a cooling center, a brief exposure to ambient cooling (2-hours at 23°C) during the mid-point of a day-long (9-hours exposure) to extreme heat (40°C and 10% relative humidity) was shown to cause a decrease in core temperature and cardiovascular strain in older adults (mean age 72 years) [Citation438] (). However, these benefits were transient as core temperature in participants exposed to the cooling intervention returned to levels equivalent to the non-cooled control group within 2 hours after returning to the heated environment. Further, a mid-day cooling center intervention provided a sustained reduction in heat-related illness symptoms and mood disturbance after returning to the heat compared to the control condition [Citation439]. These effects were observed, even though core body temperature returned to elevated pre-cooling levels upon reentry to the heat. This indicates that the older adults accessing the simulated cooling center experienced an altered ability to perceive a heat-induced elevation in physiological strain [Citation439]. Altogether, these findings demonstrate that while accessing cooling centers may provide a temporary abatement strategy, guidance should consider that supplemental interventions to cool the body or the home may be required after individuals leave cooling centers, especially when ambient temperature remains elevated overnight.
Figure 8. Accessing cooling centers for a brief period (1–3 hours) can provide protection for people who are vulnerable to heat-related illnesses. While it has positive effects on physiological and mood-state, these responses are transient. Continued caution and use of appropriate countermeasures to mitigate indoor overheating should be employed upon reentry to the heat. Data represents physiological responses (see ref. [Citation438]) and mood-state (see ref. [Citation439]) measured in older adults (64–79 years) underwent a 9-hour simulated heat wave (40°C) with (cooling group, n = 20, 9 females) or without (control group, n = 20, 8 females) a cooling intervention consisting of 2-hour rest in an air-conditioned room (˜23°C, hours 5–6). Tco, core temperature; HR, heart rate; bpm, beats per min.
![Figure 8. Accessing cooling centers for a brief period (1–3 hours) can provide protection for people who are vulnerable to heat-related illnesses. While it has positive effects on physiological and mood-state, these responses are transient. Continued caution and use of appropriate countermeasures to mitigate indoor overheating should be employed upon reentry to the heat. Data represents physiological responses (see ref. [Citation438]) and mood-state (see ref. [Citation439]) measured in older adults (64–79 years) underwent a 9-hour simulated heat wave (40°C) with (cooling group, n = 20, 9 females) or without (control group, n = 20, 8 females) a cooling intervention consisting of 2-hour rest in an air-conditioned room (˜23°C, hours 5–6). Tco, core temperature; HR, heart rate; bpm, beats per min.](/cms/asset/0fe06b28-91fa-4e22-884d-41288270059c/ktmp_a_2361223_f0008_oc.jpg)
Occupant behavior
Although there are many factors within the built environment that can modify the risk of indoor overheating, how an individual interacts with their environment and behaves inside their home impacts how much the building overheats and the level of physiological strain they may experience during hot weather. Notably, a study assessing 500 Danish dwellings showed that resident behavior was in fact a stronger predictor of adequate air exchange rates within the home than building characteristics [Citation440]. To date however, there remains relatively limited knowledge on the influence of occupant behavior for overheating risk in dwellings during an EHE. While protective measures such as operable windows and mechanical ventilation to enhance air exchange, access to an air conditioner for ambient cooling, use of window blinds and shutters to limit solar heating, and others are effective at limiting indoor overheating, appropriate behavioral strategies to implement these measures (e.g. ability to turn on air conditioner, open window, close window blinds) are necessary. In some cases, such actions may be challenging for the most vulnerable, particularly older adults and individuals with reduced mobility and/or physical capacity [Citation440]. Moreover, a recent study showed that heat stress mitigation measures were underused in older people who are socially isolated [Citation243].
While an upper indoor temperature limit of 26°C has been proposed to be sufficiently protective for heat-vulnerable older occupants [Citation297], this recommendation did not consider the added heat burden associated with increases in internal heat production accompanying activities of daily living or the restriction to heat loss caused by clothing insulation. A recommendation by many health agencies worldwide to prevent heat-related illnesses in older adults is to remain in a cool indoor space, avoid strenuous physical activity, wear lightweight, light-colored clothing, drink plenty of water throughout the day, among others [Citation441]. However, older adults do not sense heat as well as their younger counterparts [Citation63,Citation201]. Consequently, they are likely to overdress despite high indoor temperatures. In other cases, individuals may wear heavy and/or dark-colored garments due to cultural or religious norms and may not align with the need to dress in light clothing during hot weather or EHEs. Moreover, many individuals may be unaware of the consequences of increases in physical activity on heat gain and may therefore not adjust their normal day-to-day activity levels to prevent potentially dangerous rises in body temperature. This includes limiting the use of heat generating activities such as the use of appliances (e.g. cooking meals), televisions and other electronics. Consequently, this may necessitate a lowering of recommended upper indoor temperature limit during an EHE. As the frequency of overheating in homes is expected to increase with rising global temperatures, understanding, and considering occupant behavior especially in disadvantaged population groups [Citation243] as well as interactions with the building design and systems will be a critical cornerstone in addressing indoor overheating and protecting the health of vulnerable populations.
Summary
While there are many factors within the built environment and building design influencing the level of indoor overheating and the risk of heat-related mortality during an EHE, delineating those that may have the largest influence is challenging. Consequently, it can be difficult to assess where change in the built environment or building design may be most effective in mitigating the effects of extreme heat on neighborhood temperature and ultimately indoor temperatures in the homes of heat-vulnerable people. In the absence of appropriate changes to the built environment and building designs, which includes the construction of homes with heat-mitigation controls that can enhance ambient cooling of the dwelling such as the use of shading, natural ventilation, and other passive cooling measures, indoor temperatures may continue to be excessively high.
In the short term, to mitigate the adverse health effects of indoor overheating in heat-vulnerable people, a simple and effective solution could involve the use of environmental surveillance to assess how exposed a neighborhood population may be to high temperatures. Environmental monitoring with appropriate triggers, such as the use of a recommended indoor temperature limit of 26°C [Citation297], could be implemented so that health officials and residents can take appropriate action to mitigate the harmful effects to health caused by indoor overheating. Neighborhoods with excess mortality could be provided additional support when hot weather is forecasted enhancing preparedness. This could include allocating health care support and resources such as facilitating greater access to cooling centers, community shelters for those experiencing homelessness, and others facing insecure housing. Moreover, understanding the environment and needs of these communities will also allow for the implementation of a more effective emergency plan for responding to the needs of heat vulnerable residents during an EHE.
In the longer term, as global temperatures continue to rise, and communities strategize to develop plans to address the worsening extreme heat and its attendant effects on human health, a research agenda focused on developing local-level heat mitigation strategies to lessen the impact of UHI on indoor overheating will be critical. This must include expanding efforts to understand the limits of human heat tolerance and undertaking cutting-edge EHE simulation research to define evidence-based, equitable, globally relevant heat-alleviation solutions and public health guidance to safeguard the health and well-being of vulnerable people from indoor heat. To this end, an effective way to reduce the negative impacts of an EHE is to employ the knowledge generated from such research to develop a comprehensive heat response plan to create heat-resilient communities. As a first step, we have judiciously synthesized the knowledge generated from this narrative review to create a personal heat risk assessment tool and home preparedness checklist to assist the homeowners and tenants in identifying their vulnerability to heat and to guide them in selecting effective immediate, short-term, and long-term home modifications to mitigate indoor overheating (see https://hepru.ca/educational-material).
List of abbreviations
| CDC | = | Centers for Disease Control and Prevention |
| EHE | = | Extreme heat events |
| UHI | = | Urban heat island |
High_resolution_image_supplemental_file_page_3.jpg
Download JPEG Image (9.2 MB)Supplemental_file_in_PDF.pdf
Download PDF (233.1 KB)High_resolution_image_Supplemental_file_page_4.jpg
Download JPEG Image (10.3 MB)High_resolution_image_supplemental_file_page_2.jpg
Download JPEG Image (9.1 MB)High_resolution_image_supplemental_file_page_1.jpg
Download JPEG Image (10.5 MB)Author_bio_and_pics_submission.docx
Download MS Word (385.3 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/23328940.2024.2361223
Additional information
Funding
Notes on contributors

Glen P. Kenny
Dr. Glen P. Kenny, PhD is a Full Professor of Physiology at the University of Ottawa and holds a University Research Chair. He is Director of the Human and Environmental Physiology Research Unit and lead scientist of Operation Heat Shield Canada where his team continues to lead the charge in conducting innovative and cutting-edge research on the assessment of the environmental and human factors affecting a person’s ability to live and work in the heat.

Emily J. Tetzlaff
Ms. Emily Teztlaff, is a PhD Candidate at the Human and Environmental Physiology Research Unit (HEPRU) at the University of Ottawa. Emily has her Master’s in Human Kinetic and Bachelors of Physical and Health Education specializing in Health Promotion from Laurentian University, and has a university certification in Gerontology from Huntington University. Emily also maintains her designation as a Registered Kinesiologist with the College of Kinesiologists of Ontario. Emily has been working with the Climate Change and Health Office (CCHO) since 2021 as a Research Affiliate Program Student and Canadian Institute of Health Research – Health Systems Impact Fellow (2022–2023). Emily’s research with HEPRU and work with the CCHO focuses on heat-health communication in Canada.

W. Shane Journeay
Dr. Shane Journeay, PhD, MPH, MD, FRCPC, BC-Occ Med is currently an Assistant Professor in the Department of Medicine at the University of Toronto and Dalhousie University/Dalhousie Medicine New Brunswick where he is the JD Irving Endowed Chair in Occupational Medicine. He is a Board Certified physician in Occupational & Environmental Medicine and is a graduate of both the Harvard Occupational & Environmental Medicine Residency program and the Harvard School of Public Health (MPH). He is also certified in Physical Medicine & Rehabilitation in Canada (FRCPC) having completed his residency training at the University of Toronto. He is actively involved with research and clinical practice encompassing the relationship between health, function and work.

Sarah B. Henderson
Dr. Sarah B. Henderson, PhD completed a BASc in environmental engineering in 2000 and a PhD in environmental epidemiology in 2009, both from the University of British Columbia. She has been with the BC Centre for Disease Control since 2010, and is now the Scientific Director of Environmental Health Services and the National Collaborating Centre for Environmental Health.

Fergus K. O’Connor
Dr. Fergus O’Connor, PhD completed his PhD at Bond University in 2020. Since then, Fergus has completed a postdoctoral fellowship with the Human and Environmental Physiology Research Unit under the supervision of Prof. Glen Kenny primarily investigating the effects of daylong heat exposure on the physiological outcomes of heat-vulnerable older adults. Dr O’Connor is now a postdoctoral research fellow at Griffith University and The Prince Charles Hospital, Brisbane, investigating cardiovascular disease and climate-related physiological outcomes.
References
- Mora C, Dousset B, Caldwell IR, et al. Global risk of deadly heat. Nat Clim Chang. 2017;7:501–506. doi: 10.1038/NCLIMATE3322
- Tuholske C, Caylor K, Funk C, et al. Global urban population exposure to extreme heat. Proc Natl Acad Sci USA. 2021;118(41). doi: 10.1073/pnas.2024792118
- Ebi KL, Capon A, Berry P, Broderick C, de Dear R, Havenith G, Honda Y, Kovats S, Ma W, Malik A, Morris NB, Nybo L, Seneviratne SI, Vano J, Jay O. Hot weather and heat extremes: health risks. The Lancet 2021;398:698–708. doi: 10.1016/S0140-6736(21)01208-3
- Heaviside C, Macintyre H, Vardoulakis S. The urban heat island: implications for health in a changing environment. Curr Environ Health Rep. 2017;4(3):296–305. doi: 10.1007/s40572-017-0150-3
- Santamouris M. Analyzing the heat island magnitude and characteristics in one hundred Asian and Australian cities and regions. Sci Total Environ. 2015;512–513:582–598.
- Lo CP, Quattrochi DA, Luvall JC. Application of high-resolution thermal infrared remote sensing and GIS to assess the urban heat island effect. Int J Remote Sens. 1997;18(2):287–304. doi: 10.1080/014311697219079
- Vogt JA, Oke TR. Thermal remote sensing of urban climates. Remote Sens Environ. 2003;86:370–384. doi: 10.1016/S0034-4257(03)00079-8
- Wang Y, Berardi U, Akbari H. Comparing the effects of urban heat island mitigation strategies for Toronto, Canada. Energ Buildings. 2016;114(2):2–19. doi: 10.1016/j.enbuild.2015.06.046
- Stotz A, Rapp K, Oksa J, et al. Effect of a brief heat exposure on blood pressure and physical performance of older women living in the community-a pilot-study. Int J Environ Res And Public Health. 2014;11(12):12623–12631. doi: 10.3390/ijerph111212623
- Shiloh R, Munitz H, Stryjer R, et al. A significant correlation between ward temperature and the severity of symptoms in schizophrenia inpatients–a longitudinal study. Eur Neuropsychopharmacol. 2007;17(6–7):478–482. doi: 10.1016/j.euroneuro.2006.12.001
- Tartarini F, Cooper P, Fleming R, et al. Indoor air temperature and agitation of nursing home residents with dementia. Am J Alzheimers Dis Other Demen. 2017;32(5):272–281. doi: 10.1177/1533317517704898
- Trezza BM, Apolinario D, de Oliveira RS, et al. Environmental heat exposure and cognitive performance in older adults: a controlled trial. Age (Dordr). 2015;37(3):9783. doi: 10.1007/s11357-015-9783-z
- Lo YC, Su WP, Mei SH, et al. Association between ambient temperature and cognitive function in a community-dwelling elderly population: a repeated measurement study. BMJ Open. 2021;11(12):e049160. doi: 10.1136/bmjopen-2021-049160
- Kenny GP, Flouris AD, Yagouti A, et al. Towards establishing evidence-based guidelines on maximum indoor temperatures during hot weather in temperate continental climates. Temperature. 2019;6(1):11–36. doi: 10.1080/23328940.2018.1456257
- Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: global dimension and perspectives. Lancet 2013; 382: 260–72.
- Cheng J. et al. Cardiorespiratory effects of heatwaves: A systematic review and meta-analysis of global epidemiological evidence. Environ Res. 2019; Oct:177:108610. doi: 10.1016/j.envres.2019.108610. Epub 2019 Jul 26.
- Song X et al. Environ Sci Pollut Res Int. 2021 Nov;28(41):58035-58049. doi: 10.1007/s11356-021-14568-0. Epub 2019 Jul 26.
- Zanobetti A, O’Neill MS, Gronlund CJ, Schwartz JD. Summer temperature variability and long-term survival among elderly peoplewith chronic disease Proc Natl Acad Sci USA 2012; 109: 6608–13.
- De Blois J, Kjellstrom T, Agewall S, et al. The effects of climate change on cardiac health. Cardiology. 2015;131(4):209–217. doi: 10.1159/000398787
- Wang Y, An S, Xing M, et al. Global warming and heart disease prevention. Eur J Prev Cardiol. 2018;25(12):1342. doi: 10.1177/2047487318774846
- Seebaß K. Who is feeling the heat? vulnerabilities and exposures to heat stress—individual, social, and housing explanations. Nat Cult. 2017;12(2):137–161. doi: 10.3167/nc.2017.120203
- Kim YO, Lee W, Kim H, et al. Social isolation and vulnerability to heatwave-related mortality in the urban elderly population: a time-series multi-community study in Korea. Environ Int. 2020;142:105868. doi: 10.1016/j.envint.2020.105868
- Eisenman DP, Wilhalme H, Tseng CH, et al. Heat death associations with the built environment, social vulnerability and their interactions with rising temperature. Health & Place. 2016;41:89–99. doi: 10.1016/j.healthplace.2016.08.007
- Chakalian PM, Kurtz L, Harlan SL, et al. Exploring the social, psychological, and behavioral mechanisms of heat vulnerability in the city of Phoenix, AZ. J Extreme Events. 2019;6(3n04):2050006. doi: 10.1142/S2345737620500062
- Li Y, Sun Y, Li J, et al. Socioeconomic drivers of urban heat island effect: empirical evidence from major Chinese cities. Sustain Cities Soc. 2020;63:102425. doi: 10.1016/j.scs.2020.102425
- Fouillet A, Rey G, Laurent F, et al. Excess mortality related to the August 2003 heat wave in France. Int Arch Occup Environ Health. 2006;80(1):16–24. doi: 10.1007/s00420-006-0089-4
- Henderson SB, Ke M, Lee MJ, et al. Analysis of community deaths during the catastrophic 2021 heat dome: Early evidence to inform the public health response during subsequent events in greater Vancouver, Canada. Environ Epidemiol. 2022;6(1):e189. doi: 10.1097/EE9.0000000000000189
- British Columbia Coroners Service. Extreme heat and human mortality: A review of heat-related deaths in BC in summer 2021. Report to the Chief Coroner of British Columbia. June 7, 2022. https://www2.gov.bc.ca/assets/gov/birth-adoption-death-marriage-and-divorce/deaths/coroners-service/death-review-panel/extreme_heat_death_review_panel_report.pdf
- Mavrogianni A, Pathan A, Oikonomou E, et al. Inhabitant actions and summer overheating risk in London dwellings. Build Res Info. 2017;45(1–2):119–142. doi: 10.1080/09613218.2016.1208431
- Bobb JF, Obermeyer Z, Wang Y, et al. Cause-specific risk of hospital admission related to extreme heat in older adults. JAMA. 2014;312(24):2659–2667. doi: 10.1001/jama.2014.15715
- Patz JA, Frumkin H, Holloway T, et al. Climate change: challenges and opportunities for global health. JAMA. 2014;312(15):1565–1580. doi: 10.1001/jama.2014.13186
- Watts N, Amann M, Arnell N, et al. The 2020 report of the lancet countdown on health and climate change: responding to converging crises. Lancet. 2021;397(10269):129–170. doi: 10.1016/S0140-6736(20)32290-X
- Kenny GP, Yardley J, Brown C, et al. Heat stress in older individuals and patients with common chronic diseases. CMAJ. 2010;182(10):1053–1060. doi: 10.1503/cmaj.081050
- Kenny GP, Notley SR, Flouris AD, et al. Climate change and heat exposure: impact on health in occupational and general populations. In: Adams W, Jardine J, editors. Exertional heat illness: a clinical and evidence-based guide. Switzerland AG: Springer Cham; 2020. p. 225–261.
- Centre PC. Heat waves and health – a special report on climate change in Canada. Winnipeg, MN: Prairie Climate Centre;2019.
- Khatana SAM, Werner RM, Groeneveld PW. Association of extreme heat with all-cause mortality in the contiguous US, 2008-2017. JAMA Netw Open. 2022;5(5):e2212957. doi: 10.1001/jamanetworkopen.2022.12957
- Suzman R, Beard JR, Boerma T, et al. Health in an ageing world–what do we know? Lancet. 2015;385(9967):484–486. doi: 10.1016/S0140-6736(14)61597-X
- World Health Organization. World report on ageing and health. 2015; https://www.who.int/publications/i/item/9789241565042
- Bouchama A, Dehbi M, Mohamed G, et al. Prognostic factors in heat wave related deaths: a meta-analysis. Arch Intern Med. 2007;167(20):2170–2176. doi: 10.1001/archinte.167.20.ira70009
- Semenza JC, Je M, Flanders WD, et al. Excess hospital admissions during the July 1995 heat wave in Chicago. Am J Prev Med. 1999;16(4):269–277. doi: 10.1016/S0749-3797(99)00025-2
- Curriero FC, Heiner KS, Samet JM, et al. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol. 2002;155(1):80–87. doi: 10.1093/aje/155.1.80
- Basu R, Malig B. High ambient temperature and mortality in California: exploring the roles of age, disease, and mortality displacement. Environ Res. 2011;111(8):1286–1292. doi: 10.1016/j.envres.2011.09.006
- Kravchenko J, Abernethy AP, Fawzy M, et al. Minimization of heatwave morbidity and mortality. Am J Prev Med. 2013;44(3):274–282. doi: 10.1016/j.amepre.2012.11.015
- Vandentorren S, Bretin P, Zeghnoun A, et al. August 2003 heat wave in France: risk factors for death of elderly people living at home. Eur J Public Health. 2006;16(6):583–591. doi: 10.1093/eurpub/ckl063
- Haines A, Ebi K, Solomon CG. The imperative for climate action to protect health. N Engl J Med. 2019;380(3):263–273. doi: 10.1056/NEJMra1807873
- Mayrhuber EA, Duckers MLA, Wallner P, et al. Vulnerability to heatwaves and implications for public health interventions – a scoping review. Environ Res. 2018;166:42–54. doi: 10.1016/j.envres.2018.05.021
- Murage P, Kovats S, Sarran C, et al. What individual and neighbourhood-level factors increase the risk of heat-related mortality? A case-crossover study of over 185,000 deaths in London using high-resolution climate datasets. Environ Int. 2020;134:105292. doi: 10.1016/j.envint.2019.105292
- Kovats RS, Hajat S. Heat stress and public health: a critical review. Annu Rev Public Health. 2008;29(1):41–55. doi: 10.1146/annurev.publhealth.29.020907.090843
- Jang J, Natarajan S, Lee J, et al. Comparative analysis of overheating risk for typical dwellings and passivhaus in the UK. Energies. 2022;15(10):3829. doi: 10.3390/en15103829
- Dogra S, Clarke JM, Copeland JL. Prolonged sedentary time and physical fitness among Canadian men and women aged 60 to 69. Health Rep. 2017;28(2):3–9.
- Barriopedro D, Fischer EM, Luterbacher J, et al. The hot summer of 2010: redrawing the temperature record map of Europe. Science. 2011;332(6026):220–224. doi: 10.1126/science.1201224
- Meehl GA, Tebaldi C. More intense, more frequent, and longer lasting heat waves in the 21st century. Science. 2004;305(5686):994–997. doi: 10.1126/science.1098704
- World Health Organization. Quantitative risk assessment of the effects of climate change on selected causes of death, 2030s and 2050s. 2014. https://www.who.int/publications/i/item/9789241507691
- Del Bene VE. Temperature. In: Walker HK, Hall WD, Hurst JW, editors, Clinical methods: the history, physical, and laboratory examinations, 3rd ed., Chapter 218 Boston: Buttersworths; 1990. pp. 990–993.
- Gagge AP, Gonzales RR. Mechanisms of heat exchange: Biophysics and physiology. In: Blatteis CM, Fregley MJ, editors. Handbook of physiology. Environmental physiology. Vol. II, Sect. 4, Chapter 4. Bethesda, MD: American Physiological Society; 1996. pp. 45–84.
- Kenny GP, Jay O. Thermometry, calorimetry, and mean body temperature during heat stress. Compr Physiol. 2013;3:1–31.
- Flouris AD, Dinas PC, Ioannou LG, et al. Workers’ health and productivity under occupational heat strain: a systematic review and meta-analysis. Lancet Planet Health. 2018;2(12):e521–e531. doi: 10.1016/S2542-5196(18)30237-7
- Kenny GP, Wilson TE, Flouris AD, et al. Heat exhaustion. Handb Clin Neurol. 2018;157:505–529.
- Masselot P, Mistry M, Vanoli J, et al. Excess mortality attributed to heat and cold: a health impact assessment study in 854 cities in Europe. Lancet Planet Health. 2023;7(4):e271–e281. doi: 10.1016/S2542-5196(23)00023-2
- Meade RD, Akerman AP, Notley SR, et al. Physiological factors characterizing heat-vulnerable older adults: a narrative review. Environ Int. 2020;144:105909. doi: 10.1016/j.envint.2020.105909
- Meade RD, Notley SR, Kenny GP. Aging and human heat dissipation during exercise-heat stress: an update and future directions. Curr Opin Physiol. 2019;10:219–225. doi: 10.1016/j.cophys.2019.07.003
- Cramer MN, Gagnon D, Laitano O, et al. Human temperature regulation under heat stress in health, disease, and injury. Physiol Rev. 2022;102(4):1907–1989. doi: 10.1152/physrev.00047.2021
- Dufour A, Candas V. Ageing and thermal responses during passive heat exposure: sweating and sensory aspects. Eur J Appl Physiol. 2007;100(1):19–26. doi: 10.1007/s00421-007-0396-9
- Sagawa S, Shiraki K, Yousef MK, et al. Sweating and cardiovascular responses of aged men to heat exposure. J Gerontol. 1988;43(1):M1–8. doi: 10.1093/geronj/43.1.M1
- Stapleton JM, Poirier MP, Flouris AD, et al. Aging impairs heat loss, but when does it matter? J Appl Physiol. 2015;118(3):299–309. doi: 10.1152/japplphysiol.00722.2014
- Stapleton JM, Poirier MP, Flouris AD, et al. At what level of heat load are age-related impairments in the ability to dissipate heat evident in females? PLOS ONE. 2015;10(3):e0119079. doi: 10.1371/journal.pone.0119079
- D’Souza AW, Notley SR, Kenny GP. The relation between age and sex on whole-body heat loss during exercise-heat stress. Medicine And Science In Sports And Exercise. 2020;52(10):2242–2249. doi: 10.1249/MSS.0000000000002373
- Stapleton JM, Larose J, Simpson C, et al. Do older adults experience greater thermal strain during heat waves? Appl Physiol Nutr Metab. 2014;39(3):292–298. doi: 10.1139/apnm-2013-0317
- Kenny GP, Poirier MP, Metsios GS, et al. Hyperthermia and cardiovascular strain during an extreme heat exposure in young versus older adults. Temperature. 2016;4(1):79–88. doi: 10.1080/23328940.2016.1230171
- Larose J, Boulay P, Sigal RJ, et al. Age-related decrements in heat dissipation during physical activity occur as early as the age of 40. PLOS ONE. 2013;8(12):e83148. doi: 10.1371/journal.pone.0083148
- Larose J, Boulay P, Wright-Beatty HE, et al. Age-related differences in heat loss capacity occur under both dry and humid heat stress conditions. J Appl Physiol. 2014;117(1):69–79. doi: 10.1152/japplphysiol.00123.2014
- Larose J, Wright HE, Stapleton J, et al. Whole-body heat loss is reduced in older males during short bouts of intermittent exercise. Am J Physiol. 2013;305(6):R619–629. doi: 10.1152/ajpregu.00157.2013
- Poirier MP, Notley SR, Boulay P, et al. Type 2 diabetes does not exacerbate body heat storage in older adults during brief, extreme passive heat exposure. Temperature. 2020;7(3):263–269. doi: 10.1080/23328940.2020.1736760
- Drinkwater BL, Bedi JF, Loucks AB, et al. Sweating sensitivity and capacity of women in relation to age. J Appl Physiol. 1982;53(3):671–676. doi: 10.1152/jappl.1982.53.3.671
- Shoenfeld Y, Udassin R, Shapiro Y, et al. Age and sex difference in response to short exposure to extreme dry heat. J Appl Physiol. 1978;44(1):1–4. doi: 10.1152/jappl.1978.44.1.1
- Kenny GP, Notley SR, Gagnon D. Direct calorimetry: a brief historical review of its use in the study of human metabolism and thermoregulation. Eur J Appl Physiol. 2017;117(9):1765–1785. doi: 10.1007/s00421-017-3670-5
- Meade RD, Notley SR, Akerman AP, et al. Physiological responses to 9 hours of heat exposure in young and older adults. Part I: body temperature and hemodynamic regulation. J Appl Physiol. 2023;135(3):673–687. doi: 10.1152/japplphysiol.00227.2023
- Kenney WL, Munce TA. Invited review: aging and human temperature regulation. J Appl Physiol. 2003;95(6):2598–2603. doi: 10.1152/japplphysiol.00202.2003
- Shibasaki M, Okazaki K, Inoue T. Aging and thermoregulation. J Phys Fitness Sports Med. 2013;2(1):37–47. doi: 10.7600/jpfsm.2.37
- Gravel H, Chaseling GK, Barry H, et al. Cardiovascular control during heat stress in older adults: time for an update. Am J Physiol Heart Circ Physiol. 2021;320(1):H411–H416. doi: 10.1152/ajpheart.00536.2020
- Kenney WL, Craighead DH, Alexander LM. Heat waves, aging, and human cardiovascular health. Medicine And Science In Sports And Exercise. 2014;46(10):1891–1899. doi: 10.1249/MSS.0000000000000325
- Astrom DO, Forsberg B, Rocklov J. Heat wave impact on morbidity and mortality in the elderly population: a review of recent studies. Maturitas. 2011;69(2):99–105. doi: 10.1016/j.maturitas.2011.03.008
- Donaldson GC, Keatinge WR, Saunders RD. Cardiovascular responses to heat stress and their adverse consequences in healthy and vulnerable human populations. Int J Hyperthermia. 2003;19(3):225–235. doi: 10.1080/0265673021000058357
- Millyard A, Layden JD, Pyne DB, et al. Impairments to thermoregulation in the elderly during heat exposure events. Gerontol Geriatr Med. 2020;6:2333721420932432. doi: 10.1177/2333721420932432
- Greaney JL, Stanhewicz AE, Proctor DN, et al. Impairments in central cardiovascular function contribute to attenuated reflex vasodilation in aged skin. J Appl Physiol. 2015;119(12):1411–1420. doi: 10.1152/japplphysiol.00729.2015
- Kenney WL, Morgan AL, Farquhar WB, et al. Decreased active vasodilator sensitivity in aged skin. Am J Physiol. 1997;272(4 Pt 2):H1609–1614. doi: 10.1152/ajpheart.1997.272.4.H1609
- Gagnon D, Romero SA, Ngo H, et al. Healthy aging does not compromise the augmentation of cardiac function during heat stress. J Appl Physiol. 2016;121(4):885–892. doi: 10.1152/japplphysiol.00643.2016
- Minson CT, Wladkowski SL, Cardell AF, et al. Age alters the cardiovascular response to direct passive heating. J Appl Physiol. 1998;84(4):1323–1332. doi: 10.1152/jappl.1998.84.4.1323
- Rowell LB. Human cardiovascular adjustments to exercise and thermal stress. Physiol Rev. 1974;54(1):75–159. doi: 10.1152/physrev.1974.54.1.75
- Crandall CG, Wilson TE. Human cardiovascular responses to passive heat stress. Compr Physiol. 2015;5(1):17–43.
- Monahan KD. Effect of aging on baroreflex function in humans. Am J Physiol Regul Integr Comp Physiol. 2007;293(1):R3–R12. doi: 10.1152/ajpregu.00031.2007
- Schlader ZJ, Wilson TE, Crandall CG. Mechanisms of orthostatic intolerance during heat stress. Auton Neurosci. 2016;196:37–46. doi: 10.1016/j.autneu.2015.12.005
- Conti S, Masocco M, Meli P, et al. General and specific mortality among the elderly during the 2003 heat wave in Genoa (Italy). Environ Res. 2007;103(2):267–274. doi: 10.1016/j.envres.2006.06.003
- Luber G, McGeehin M. Climate change and extreme heat events. Am J Prev Med. 2008;35(5):429–435. doi: 10.1016/j.amepre.2008.08.021
- Fuhrmann CM, Sugg MM, Konrad CE 2nd, et al. Impact of extreme heat events on emergency department visits in North Carolina (2007-2011). J Community Health. 2016;41(1):146–156. doi: 10.1007/s10900-015-0080-7
- Hondula DM, Davis RE, Saha MV, et al. Geographic dimensions of heat-related mortality in seven U.S. cities. Environ Res. 2015;138:439–452. doi: 10.1016/j.envres.2015.02.033
- Knowlton K, Rotkin-Ellman M, King G, et al. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect. 2009;117(1):61–67. doi: 10.1289/ehp.11594
- Lin S, Luo M, Walker RJ, et al. Extreme high temperatures and hospital admissions for respiratory and cardiovascular diseases. Epidemiology. 2009;20(5):738–746. doi: 10.1097/EDE.0b013e3181ad5522
- Rey G, Jougla E, Fouillet A, et al. The impact of major heat waves on all-cause and cause-specific mortality in France from 1971 to 2003. Int Arch Occup Environ Health. 2007;80(7):615–626. doi: 10.1007/s00420-007-0173-4
- Robine JM, Cheung SL, Le Roy S, et al. Death toll exceeded 70,000 in Europe during the summer of 2003. C R Biol. 2008;331(2):171–178. doi: 10.1016/j.crvi.2007.12.001
- Cleland VJ, Ball K, Magnussen C, et al. Socioeconomic position and the tracking of physical activity and cardiorespiratory fitness from childhood to adulthood. Am J Epidemiol. 2009;170(9):1069–1077. doi: 10.1093/aje/kwp271
- Garrett AT, Goosens NG, Rehrer NG, et al. Induction and decay of short-term heat acclimation. Eur J Appl Physiol. 2009;107(6):659–670. doi: 10.1007/s00421-009-1182-7
- Gagnon D, Kenny GP. Does sex have an independent effect on thermoeffector responses during exercise in the heat? J Physiol. 2012;590(Pt 23):5963–5973. doi: 10.1113/jphysiol.2012.240739
- Gagnon D, Kenny GP. Sex modulates whole-body sudomotor thermosensitivity during exercise. J Physiol. 2011;589(Pt 24):6205–6217. doi: 10.1113/jphysiol.2011.219220
- Gagnon D, Crandall CG, Kenny GP. Sex differences in postsynaptic sweating and cutaneous vasodilation. J Appl Physiol. 2013;114(3):394–401. doi: 10.1152/japplphysiol.00877.2012
- Jiao A, Yu C, Xiang Q, et al. Impact of summer heat on mortality and years of life lost: application of a novel indicator of daily excess hourly heat. Environ Res. 2019;172:596–603. doi: 10.1016/j.envres.2019.01.056
- Rocklov J, Forsberg B, Ebi K, et al. Susceptibility to mortality related to temperature and heat and cold wave duration in the population of Stockholm County, Sweden. Glob Health Action. 2014;7(1):22737. doi: 10.3402/gha.v7.22737
- DeCastro M, Gomez-Gesteira M, Ramos AM, et al. Effects of het waves on human mortality, Galicia Spain. Clim Res. 2011;48(2):331–341. doi: 10.3354/cr00988
- Basagana X, Sartini C, Barrera-Gomez J, et al. Heat waves and cause-specific mortality at all ages. Epidemiology. 2011;22(6):765–772. doi: 10.1097/EDE.0b013e31823031c5
- Diaz J, Jordan A, Garcia R, et al. Heat waves in Madrid 1986-1997: effects on the health of the elderly. Int Arch Occup Environ Health. 2002;75(3):163–170. doi: 10.1007/s00420-001-0290-4
- Bell ML, Ms O, Ranjit N, et al. Vulnerability to heat-related mortality in Latin America: a case-crossover study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int J Epidemiol. 2008;37(4):796–804. doi: 10.1093/ije/dyn094
- O’Neill MS, Carter R, Kish JK, et al. Preventing heat-related morbidity and mortality: new approaches in a changing climate. Maturitas. 2009;64(2):98–103. doi: 10.1016/j.maturitas.2009.08.005
- Lin S, Hsu WH, Van Zutphen AR, et al. Excessive heat and respiratory hospitalizations in New York State: estimating current and future public health burden related to climate change. Environ Health Perspect. 2012;120(11):1571–1577. doi: 10.1289/ehp.1104728
- van Steen Y, Ntarladima AM, Grobbee R, et al. Sex differences in mortality after heat waves: are elderly women at higher risk? Int Arch Occup Environ Health. 2019;92(1):37–48. doi: 10.1007/s00420-018-1360-1
- Ingole V, Kovats S, Schumann B, et al. Socioenvironmental factors associated with heat and cold-related mortality in Vadu HDSS, western India: a population-based case-crossover study. Int J Biometeorol. 2017;61(10):1797–1804. doi: 10.1007/s00484-017-1363-8
- Folkerts MA, Brode P, Botzen WJW, et al. Sex differences in temperature-related all-cause mortality in the Netherlands. Int Arch Occup Environ Health. 2022;95(1):249–258. doi: 10.1007/s00420-021-01721-y
- Borrell C, Mari-Dell’olmo M, Rodriguez-Sanz M, et al. Socioeconomic position and excess mortality during the heat wave of 2003 in Barcelona. Eur J Epidemiol. 2006;21(9):633–640. doi: 10.1007/s10654-006-9047-4
- Bogdanovic DC, Milosevic ZG, Lazarevic KK, et al. The impact of the July 2007 heat wave on daily mortality in Belgrade, Serbia. Cent Eur J Public Health. 2013;21(3):140–145. doi: 10.21101/cejph.a3840
- Achebak H, Devolder D, Ballester J. Trends in temperature-related age-specific and sex-specific mortality from cardiovascular diseases in Spain: a national time-series analysis. Lancet Planet Health. 2019;3(7):e297–e306. doi: 10.1016/S2542-5196(19)30090-7
- Yanovich R, Ketko I, Charkoudian N. Sex differences in human thermoregulation: relevance for 2020 and beyond. Physiology (Bethesda). 2020;35(3):177–184. doi: 10.1152/physiol.00035.2019
- Davido A, Patzak A, Dart T, et al. Risk factors for heat related death during the August 2003 heat wave in Paris, France, in patients evaluated at the emergency department of the Hopital Europeen Georges Pompidou. Emerg Med J. 2006;23(7):515–518. doi: 10.1136/emj.2005.028290
- Faurie C, Varghese BM, Liu J, et al. Association between high temperature and heatwaves with heat-related illnesses: a systematic review and meta-analysis. Sci Total Environ. 2022;852:158332. doi: 10.1016/j.scitotenv.2022.158332
- Horstman DH, Horvath SM. Cardiovascular and temperature regulatory changes during progressive dehydration and euhydration. J Appl Physiol. 1972;33(4):446–450. doi: 10.1152/jappl.1972.33.4.446
- Meade RD, Notley SR, D’Souza AW, et al. Interactive effects of age and hydration state on human thermoregulatory function during exercise in hot-dry conditions. Acta Physiol (Oxf). 2019;226(1):e13226. doi: 10.1111/apha.13226
- Sawka MN, Cheuvront SN, Kenefick RW. Hypohydration and human performance: impact of environment and physiological mechanisms. Sports Med. 2015;45(1):S51–60. doi: 10.1007/s40279-015-0395-7
- Miescher E, Fortney SM. Responses to dehydration and rehydration during heat exposure in young and older men. Am J Physiol. 1989;257(5 Pt 2):R1050–1056. doi: 10.1152/ajpregu.1989.257.5.R1050
- Ainslie PN, Campbell IT, Frayn KN, et al. Energy balance, metabolism, hydration, and performance during strenuous hill walking: the effect of age. J Appl Physiol. 2002;93(2):714–723. doi: 10.1152/japplphysiol.01249.2001
- Allison SP, Lobo DN. Fluid and electrolytes in the elderly. Curr Opin Clin Nutr Metab Care. 2004;7(1):27–33. doi: 10.1097/00075197-200401000-00006
- Davidhizar R, Dunn CL, Hart AN. A review of the literature on how important water is to the world’s elderly population. Int Nurs Rev. 2004;51(3):159–166. doi: 10.1111/j.1466-7657.2004.00224.x
- Schols JM, De Groot CP, van der Cammen TJ, et al. Preventing and treating dehydration in the elderly during periods of illness and warm weather. J Nutr Health Aging. 2009;13(2):150–157. doi: 10.1007/s12603-009-0023-z
- Watso JC, Farquhar WB. Hydration Status and Cardiovascular Function. Nutrients. 2019;11(8):1866. doi: 10.3390/nu11081866
- Kettaneh A, Fardet L, Mario N, et al. The 2003 heat wave in France: hydratation status changes in older inpatients. Eur J Epidemiol. 2010;25(7):517–524. doi: 10.1007/s10654-010-9478-9
- Phillips PA, Rolls BJ, Ledingham JG, et al. Reduced thirst after water deprivation in healthy elderly men. N Engl J Med. 1984;311(12):753–759. doi: 10.1056/NEJM198409203111202
- Takamata A, Ito T, Yaegashi K, et al. Effect of an exercise-heat acclimation program on body fluid regulatory responses to dehydration in older men. Am J Physiol. 1999;277(4 Pt 2):R1041–1050. doi: 10.1152/ajpregu.1999.277.4.R1041
- Davies I, Pa O, Ka M, et al. Age-associated alterations in thirst and arginine vasopressin in response to a water or sodium load. Age Ageing. 1995;24(2):151–159. doi: 10.1093/ageing/24.2.151
- Mack GW, Weseman CA, Langhans GW, et al. Body fluid balance in dehydrated healthy older men: thirst and renal osmoregulation. J Appl Physiol. 1994;76(4):1615–1623. doi: 10.1152/jappl.1994.76.4.1615
- Westaway K, Frank O, Husband A, et al. Medicines can affect thermoregulation and accentuate the risk of dehydration and heat-related illness during hot weather. J Clin Pharm Ther. 2015;40(4):363–367. doi: 10.1111/jcpt.12294
- Kenny GP, Sigal RJ, McGinn R. Body temperature regulation in diabetes. Temperature. 2016;3(1):119–145. doi: 10.1080/23328940.2015.1131506
- Schwartz J. Who is sensitive to extremes of temperature?: A case-only analysis. Epidemiology. 2005;16(1):67–72. doi: 10.1097/01.ede.0000147114.25957.71
- Hajat S, Haines A, Sarran C, et al. The effect of ambient temperature on type-2-diabetes: case-crossover analysis of 4+ million GP consultations across England. Environ Health. 2017;16(1):73. doi: 10.1186/s12940-017-0284-7
- Semenza JC, Rubin CH, Falter KH, et al. Heat-related deaths during the July 1995 heat wave in Chicago. N Engl J Med. 1996;335(2):84–90. doi: 10.1056/NEJM199607113350203
- Moon J. The effect of the heatwave on the morbidity and mortality of diabetes patients; a meta-analysis for the era of the climate crisis. Environ Res. 2021;195:110762. doi: 10.1016/j.envres.2021.110762
- Gao D, Friedman S, Hosler A, et al. Association between extreme ambient heat exposure and diabetes-related hospital admissions and emergency department visits: A systematic review. Hyg Environ Health Adv. 2022;4:4. doi: 10.1016/j.heha.2022.100031
- Moses RG, Patterson MJ, Regan JM, et al. A non-linear effect of ambient temperature on apparent glucose tolerance. Diabetes Res Clin Pract. 1997;36(1):35–40. doi: 10.1016/S0168-8227(97)01391-0
- Koivisto VA, Fortney S, Hendler R, et al. A rise in ambient temperature augments insulin absorption in diabetic patients. Metabolism. 1981;30(4):402–405. doi: 10.1016/0026-0495(81)90122-0
- Notley SR, Poirier MP, Sigal RJ, et al. Exercise heat stress in patients with and without type 2 diabetes. JAMA. 2019;322(14):1409–1411. doi: 10.1001/jama.2019.10943
- Yardley JE, Stapleton JM, Sigal RJ, et al. Do heat events pose a greater health risk for individuals with type 2 diabetes? Diabetes Technol Ther. 2013;15(6):520–529. doi: 10.1089/dia.2012.0324
- Fealey RD, Low PA, Thomas JE. Thermoregulatory sweating abnormalities in diabetes mellitus. Mayo Clin Proc. 1989;64(6):617–628. doi: 10.1016/S0025-6196(12)65338-5
- Kihara M, Opfer-Gehrking TL, Low PA. Comparison of directly stimulated with axon-reflex-mediated sudomotor responses in human subjects and in patients with diabetes. Muscle Nerve. 1993;16(6):655–660. doi: 10.1002/mus.880160612
- Kirby NV, Meade RD, Poirier MP, et al. Association between haemoglobin A(1c) and whole-body heat loss during exercise-heat stress in physically active men with type 2 diabetes. Exp Physiol. 2023;108(3):338–343. doi: 10.1113/EP090915
- Yardley JE, Stapleton JM, Carter MR, et al. Is whole-body thermoregulatory function impaired in type 1 diabetes mellitus? Curr Diabetes Rev. 2013;9(2):126–136. doi: 10.2174/1573399811309020004
- Klinenberg E. Heat wave: a social autopsy of disaster in Chicago. Chicago, Il: Chicago University Press; 2002.
- Folkow B. Physiological aspects of primary hypertension. Physiol Rev. 1982;62(2):347–504. doi: 10.1152/physrev.1982.62.2.347
- Greene AS, Tonellato PJ, Lui J, et al. Microvascular rarefaction and tissue vascular resistance in hypertension. Am J Physiol. 1989;256(1 Pt 2):H126–131. doi: 10.1152/ajpheart.1989.256.1.H126
- Carberry PA, Shepherd AM, Johnson JM. Resting and maximal forearm skin blood flows are reduced in hypertension. Hypertension. 1992;20(3):349–355. doi: 10.1161/01.HYP.20.3.349
- Drummond PD. Thermoregulatory response to passive body heating in borderline hypertension. Clin Auton Res. 1993;3(4):233–238. doi: 10.1007/BF01829011
- Kellogg J, Morris SR, Rodriguez SB, et al. Thermoregulatory reflexes and cutaneous active vasodialtion during heat stress in hypertensive humans. J Appl Physiol. 1998;85(1):175–180. doi: 10.1152/jappl.1998.85.1.175
- Kenney WL, Kamon E. Comparative physiological responses of normotensive and essentially hypertensive men to exercise in the heat. Eur J Appl Physiol Occup Physiol. 1984;52(2):196–201. doi: 10.1007/BF00433392
- Kenney WL, Kamon E, Buskirk ER. Effect of mild essential hypertension on control of forearm blood flow during exercise in the heat. J Appl Physiol. 1984;56(4):930–935. doi: 10.1152/jappl.1984.56.4.930
- Fonseca SF, Teles MC, Ribeiro VG, et al. Hypertension is associated with greater heat exchange during exercise recovery in a hot environment. Braz J Med Biol Res. 2015;48(12):1122–1129. doi: 10.1590/1414-431x20154532
- Ribeiro GA, Rodrigues LO, Moreira MC, et al. Thermoregulation in hypertensive men exercising in the heat with water ingestion. Braz J Med Biol Res. 2004;37(3):409–417. doi: 10.1590/S0100-879X2004000300019
- Akerman AP, Notley SR, Sigal RJ, et al. Impact of uncomplicated controlled hypertension on thermoregulation during exercise-heat stress. J Hum Hypertens. 2021;35(10):880–883. doi: 10.1038/s41371-020-00402-6
- Lomax P, Schonbaum E. The effects of drugs on thermoregulation during exposure to hot environments. Prog Brain Res. 1998;115:193–204.
- Cheshire WP, Fealey RD. Drug-induced hyperhidrosis and hypohidrosis: incidence, prevention and management. Drug Saf. 2008;31(2):109–126. doi: 10.2165/00002018-200831020-00002
- Hajat S, O’Connor M, Kosatsky T. Health effects of hot weather: from awareness of risk factors to effective health protection. Lancet. 2010;375(9717):856–863. doi: 10.1016/S0140-6736(09)61711-6
- Herman RM, Brower JB, Stoddard DG, et al. Prevalence of somatic small fiber neuropathy in obesity. Int J Obes (Lond). 2007;31(2):226–235. doi: 10.1038/sj.ijo.0803418
- Vroman NB, Buskirk ER, Hodgson JL. Cardiac output and skin blood flow in lean and obese individuals during exercise in the heat. J Appl Physiol Respir Environ Exerc Physiol. 1983;55(1 Pt 1):69–74. doi: 10.1152/jappl.1983.55.1.69
- Chung NK, Pin CH. Obesity and the occurrence of heat disorders. Mil Med. 1996;161(12):739–742. doi: 10.1093/milmed/161.12.739
- Mirchandani HG, McDonald G, Hood IC, et al. Heat-related deaths in Philadelphia–1993. Am J Forensic Med Pathol. 1996;17(2):106–108. doi: 10.1097/00000433-199606000-00004
- Going S, Williams D, Lohman T. Aging and body composition: biological changes and methodological issues. Exerc Sport Sci Rev. 1995;23:411–458. doi: 10.1249/00003677-199500230-00016
- Wing RR, Matthews KA, Kuller LH, et al. Weight gain at the time of menopause. Arch Intern Med. 1991;151(1):97–102. doi: 10.1001/archinte.1991.00400010111016
- McGinn R, Poirier MP, Louie JC, et al. Increasing age is a major risk factor for susceptibility to heat stress during physical activity. Appl Physiol Nutr Metab. 2017;42(11):1232–1235. doi: 10.1139/apnm-2017-0322
- Bunker A, Wildenhain J, Vandenbergh A, et al. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine. 2016;6:258–268. doi: 10.1016/j.ebiom.2016.02.034
- Vaidyanathan A, Malilay J, Schramm P, et al. Heat-Related Deaths – United States, 2004-2018. MMWR Morb Mortal Wkly Rep. 2020;69(24):729–734. doi: 10.15585/mmwr.mm6924a1
- Ishigami A, Hajat S, Kovats RS, et al. An ecological time-series study of heat-related mortality in three European cities. Environ Health. 2008;7(1):5. doi: 10.1186/1476-069X-7-5
- Huynen MM, Martens P, Schram D, et al. The impact of heat waves and cold spells on mortality rates in the Dutch population. Environ Health Perspect. 2001;109(5):463–470. doi: 10.1289/ehp.01109463
- Braga AL, Zanobetti A, Schwartz J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ Health Perspect. 2002;110(9):859–863. doi: 10.1289/ehp.02110859
- Basu R. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Health. 2009;8(1):40. doi: 10.1186/1476-069X-8-40
- Son JY, Lee JT, Anderson GB, et al. The impact of heat waves on mortality in seven major cities in Korea. Environ Health Perspect. 2012;120(4):566–571. doi: 10.1289/ehp.1103759
- Rainham DG, Smoyer-Tomic KE. The role of air pollution in the relationship between a heat stress index and human mortality in Toronto. Environ Res. 2003;93(1):9–19. doi: 10.1016/S0013-9351(03)00060-4
- Basu R, Ostro BD. A multicounty analysis identifying the populations vulnerable to mortality associated with high ambient temperature in California. Am J Epidemiol. 2008;168(6):632–637. doi: 10.1093/aje/kwn170
- Choi GY, Choi JN, Kwon HJ. The impact of high apparent temperature on the increase of summertime disease-related mortality in seoul: 1991-2000. J Prev Med Public Health. 2005;38(3):283–290.
- Liu J, Varghese BM, Hansen A, et al. Heat exposure and cardiovascular health outcomes: a systematic review and meta-analysis. Lancet Planet Health. 2022;6(6):e484–e495. doi: 10.1016/S2542-5196(22)00117-6
- Andersen I, Jensen PL, Junker P, et al. The effects of moderate heat stress on patients with ischemic heart disease. Scand J Work Environ Health. 1976;2(4):256–268. doi: 10.5271/sjweh.2804
- Walsh J, Prpic R, Goodman C, et al. Thermoregulatory responses in post-coronary artery bypass surgery and healthy males during moderate exercise in warm and cool environments. J Cardiopulm Rehabil. 2002;22(1):31–37. doi: 10.1097/00008483-200201000-00004
- Cui J, Arbab-Zadeh A, Prasad A, et al. Effects of heat stress on thermoregulatory responses in congestive heart failure patients. Circulation. 2005;112(15):2286–2292. doi: 10.1161/CIRCULATIONAHA.105.540773
- Green DJ, Maiorana AJ, Siong JH, et al. Impaired skin blood flow response to environmental heating in chronic heart failure. Eur Heart J. 2006;27(3):338–343. doi: 10.1093/eurheartj/ehi655
- Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002;346(25):1978–1988. doi: 10.1056/NEJMra011089
- Cui J, Boehmer JP, Blaha C, et al. Chronic heart failure does not attenuate the total activity of sympathetic outflow to skin during whole-body heating. Circ Heart Fail. 2013;6(2):271–278. doi: 10.1161/CIRCHEARTFAILURE.112.000135
- Keatinge WR, Coleshaw SR, Easton JC, et al. Increased platelet and red cell counts, blood viscosity, and plasma cholesterol levels during heat stress, and mortality from coronary and cerebral thrombosis. Am J Med. 1986;81(5):795–800. doi: 10.1016/0002-9343(86)90348-7
- Zhao Y, Huang Z, Wang S, et al. Morbidity burden of respiratory diseases attributable to ambient temperature: a case study in a subtropical city in China. Environ Health. 2019;18(1):89. doi: 10.1186/s12940-019-0529-8
- O’Neill MS, Hajat S, Zanobetti A, et al. Impact of control for air pollution and respiratory epidemics on the estimated associations of temperature and daily mortality. Int J Biometeorol. 2005;50(2):121–129. doi: 10.1007/s00484-005-0269-z
- Li T, Ban J, Horton RM, et al. Heat-related mortality projections for cardiovascular and respiratory disease under the changing climate in Beijing, China. Sci Rep. 2015;5(1):11441. doi: 10.1038/srep11441
- McCormack MC, Belli AJ, Waugh D, et al. Respiratory effects of indoor heat and the interaction with air pollution in chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2016;13(12):2125–2131. doi: 10.1513/AnnalsATS.201605-329OC
- Shirinde J, Wichmann J. Temperature modifies the association between air pollution and respiratory disease mortality in Cape Town, South Africa. Int J Environ Health Res. 2022;33(11):1–10. doi: 10.1080/09603123.2022.2076813
- Martin-Latry K, Goumy MP, Latry P, et al. Psychotropic drugs use and risk of heat-related hospitalisation. Eur Psychiatry. 2007;22(6):335–338. doi: 10.1016/j.eurpsy.2007.03.007
- Stachenfeld NS, Mack GW, Takamata A, et al. Thirst and fluid regulatory responses to hypertonicity in older adults. Am J Physiol. 1996;271(3 Pt 2):R757–765. doi: 10.1152/ajpregu.1996.271.3.R757
- Collins KJ, Extonsmith AN, Dore C. Urban hypothermia - preferred temperature and thermal perception in old age. Br Med J. 1981;282(6259):175–177. doi: 10.1136/bmj.282.6259.175
- Taylor NA, Allsopp NK, Parkes DG. Preferred room temperature of young vs aged males: the influence of thermal sensation, thermal comfort, and affect. J Gerontol A Biol Sci Med Sci. 1995;50(4):M216–221. doi: 10.1093/gerona/50A.4.M216
- Schlader ZJ, Coleman GL, Sackett JR, et al. Behavioral thermoregulation in older adults with cardiovascular co-morbidities. Temperature. 2018;5(1):70–85. doi: 10.1080/23328940.2017.1379585
- McGarr GW, Meade RD, Notley SR, et al. Physiological responses to 9 hours of heat exposure in young and older adults. Part III: Association with self-reported symptoms and mood-state. J Appl Physiol. 2024;136(2):408–420. doi: 10.1152/japplphysiol.00740.2023
- Abrahamson V, Wolf J, Lorenzoni I, et al. Perceptions of heatwave risks to health: interview-based study of older people in London and Norwich, UK. J Public Health (Oxf). 2009;31(1):119–126. doi: 10.1093/pubmed/fdn102
- Hansen A, Bi P, Nitschke M, et al. The effect of heat waves on mental health in a temperate Australian city. Environ Health Perspect. 2008;116(10):1369–1375. doi: 10.1289/ehp.11339
- Shiloh R, Shapira A, Potchter O, et al. Effects of climate on admission rates of schizophrenia patients to psychiatric hospitals. Eur Psychiatry. 2005;20(1):61–64. doi: 10.1016/j.eurpsy.2004.09.020
- Lee MJ, Ke M, Kuo M, et al. Chronic diseases associated with mortality in British Columbia, Canada During the 2021 Western North America extreme heat event. Geohealth. 2023;7(3):e2022GH000729. doi: 10.1029/2022GH000729
- Flynn A, McGreevy C, Mulkerrin EC. Why do older patients die in a heatwave? QJM. 2005;98(3):227–229. doi: 10.1093/qjmed/hci025
- Hermesh H, Shiloh R, Epstein Y, et al. Heat intolerance in patients with chronic schizophrenia maintained with antipsychotic drugs. Am J Psychiatry. 2000;157(8):1327–1329. doi: 10.1176/appi.ajp.157.8.1327
- Kovats RS, Kristie LE. Heatwaves and public health in Europe. Eur J Public Health. 2006;16(6):592–599. doi: 10.1093/eurpub/ckl049
- Basu R, Samet JM. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev. 2002;24(2):190–202. doi: 10.1093/epirev/mxf007
- Naughton MP, Henderson A, Mirabelli MC, et al. Heat-related mortality during a 1999 heat wave in Chicago. Am J Prev Med. 2002;22(4):221–227. doi: 10.1016/S0749-3797(02)00421-X
- Page LA, Hajat S, Kovats RS, et al. Temperature-related deaths in people with psychosis, dementia and substance misuse. Br J Psychiatry. 2012;200(6):485–490. doi: 10.1192/bjp.bp.111.100404
- Cuddy ML. The effects of drugs on thermoregulation. AACN Clin Issues. 2004;15(2):238–253. doi: 10.1097/00044067-200404000-00010
- Stollberger C, Lutz W, Finsterer J. Heat-related side-effects of neurological and non-neurological medication may increase heatwave fatalities. Eur J Neurol. 2009;16(7):879–882. doi: 10.1111/j.1468-1331.2009.02581.x
- Harlan SL, Declet-Barreto JH, Stefanov WL, et al. Neighborhood effects on heat deaths: social and environmental predictors of vulnerability in Maricopa County, Arizona. Environ Health Perspect. 2013;121(2):197–204. doi: 10.1289/ehp.1104625
- Reid CE, Mann JK, Alfasso R, et al. Evaluation of a heat vulnerability index on abnormally hot days: an environmental public health tracking study. Environ Health Perspect. 2012;120(5):715–720. doi: 10.1289/ehp.1103766
- Davis RE, Knappenberger PC, Michaels PJ, et al. Changing heat-related mortality in the United States. Environ Health Perspect. 2003;111(14):1712–1718. doi: 10.1289/ehp.6336
- Balling RC, Brazel SW. Time and space characteristics of the Phoenix urban heat island. J AZ-NV Acad Sci. 1987;21:75–81.
- Harlan SL, Brazel AJ, Prashad L, et al. Neighborhood microclimates and vulnerability to heat stress. Soc Sci Med. 2006;63(2847–2863):2847–2863. doi: 10.1016/j.socscimed.2006.07.030
- Hondula DM, Davis RE, Leisten MJ, et al. Fine-scale spatial variability of heat-related mortality in Philadelphia County, USA, from 1983-2008: a case-series analysis. Environ Health. 2012;11(1):16. doi: 10.1186/1476-069X-11-16
- Oke T. The energetic basis of the urban heat island. Q J R Meteorol Soc. 1982;108(455):1–24. doi: 10.1002/qj.49710845502
- Taylor J, Wilkinson P, Davies M, et al. Mapping the effects of urban heat island, housing, and age on excess heat-related mortality in London. Urban Clim. 2015;14(4):517–528. doi: 10.1016/j.uclim.2015.08.001
- Harlan SL, Chowell G, Yang S, et al. Heat-related deaths in hot cities: estimates of human tolerance to high temperature thresholds. Int J Environ Res And Public Health. 2014;11(3):3304–3326. doi: 10.3390/ijerph110303304
- Clarke JF. Some effects of the urban structure on heat mortality. Environ Res. 1972;5(1):93–104. doi: 10.1016/0013-9351(72)90023-0
- McCarthy MP, Best MJ, Betts RA. Climate change in cities due to global warming and urban effects. Geophys Res Let. 2010;37(9):L09705. doi: 10.1029/2010GL042845
- Li D, Bou-Zeid E. Synergistic interactions between urban heat islands and heat waves: The impact in cities is larger than the sum of its part. J Appl Meteorol Climatol. 2013;52(9):2051–2064. doi: 10.1175/JAMC-D-13-02.1
- Yang J, Zhao L, Oleson K. Large humidity effects on urban heat exposure and cooling challenges under climate change. Environ Res Lett. 2023;18(4):044024. doi: 10.1088/1748-9326/acc475
- Coutts AM, Beringer J, Tapper NJ. Impact of increasing urban density on local climate: spatial and temporal variations in the surface energy balance in Melbourne, Australia. J Appl Meteorol Clim. 2007;46(4):477–493. doi: 10.1175/JAM2462.1
- Santamouris M. On the energy impact of urban heat island and global warming on buildings. Energy Build. 2014;82:100–113. doi: 10.1016/j.enbuild.2014.07.022
- Farahani AV, Jokisalo J, Korhonen N, et al. Overheating risk and energy demand of nordic old and new apartment buildings during average and extreme weather conditions under a changing climate. Appl Sci. 2021;11(9):3972. doi: 10.3390/app11093972
- Oleson KW, Monaghan A, Wilhelmi O, et al. Interactions between urbanization, heat stress, and climate change. Climate Change. 2015;129(3–4):525–541. doi: 10.1007/s10584-013-0936-8
- Smargiassi A, Goldberg MS, Plante C, et al. Variation of daily warm season mortality as a function of micro-urban heat islands. J Epidemiol Community Health. 2009;63(8):659–664. doi: 10.1136/jech.2008.078147
- Conti S, Meli P, Minelli G, et al. Epidemiologic study of mortality during the Summer 2003 heat wave in Italy. Environ Res. 2005;98(3):390–399. doi: 10.1016/j.envres.2004.10.009
- Hajat S, Vardoulakis S, Heaviside C, et al. Climate change effects on human health: projections of temperature-related mortality for the UK during the 2020s, 2050s and 2080s. J Epidemiol Community Health. 2014;68(7):641–648. doi: 10.1136/jech-2013-202449
- Martinez BF, Annest JL, Kilbourne EM, et al. Geographic distribution of heat-related deaths among elderly persons. Use of county-level dot maps for injury surveillance and epidemiologic research. JAMA. 1989;262(16):2246–2250. doi: 10.1001/jama.1989.03430160068032
- Rogot E, Sorlie PD, Backlund E. Air-conditioning and mortality in hot weather. Am J Epidemiol. 1992;136(1):106–116. doi: 10.1093/oxfordjournals.aje.a116413
- Laaidi K, Zeghnoun A, Dousset B, et al. The impact of heat islands on mortality in Paris during the August 2003 heat wave. Environ Health Perspect. 2012;120(2):254–259. doi: 10.1289/ehp.1103532
- Macintyre HL, Heaviside C, Taylor J, et al. Assessing urban population vulnerability and environmental risks across an urban area during heatwaves – Implications for health protection. Sci Total Environ. 2018;610-611:678–690. doi: 10.1016/j.scitotenv.2017.08.062
- Vardoulakis S, Dear K, Wilkinson P. Challenges and opportunities for urban environmental health and sustainability: the HEALTHY-POLIS initiative. Environ Health. 2016;15(Suppl 1):30. doi: 10.1186/s12940-016-0096-1
- Smoyer KE. Putting risk in its place: methodological considerations for investigating extreme event health risk. Soc Sci Med. 1998;47(11):1809–1824. doi: 10.1016/S0277-9536(98)00237-8
- Hofman J, Shandas V, Pendleton N. The effects of historical housing policies on resident exposure to intra-urban heat: A study of 108 US urban areas. Climate. 2020;8(1):12. doi: 10.3390/cli8010012
- Canoui-Poitrine F, Cadot E, Spira A, et al. Excess deaths during the August 2003 heat wave in Paris, France. Rev Epidemiol Sante Publique. 2006;54(2):127–135. doi: 10.1016/S0398-7620(06)76706-2
- Yardley J, Sigal RJ, Kenny GP. Heat health planning: the importance of social and community factors. Global Environ Change. 2011;21(2):670–679. doi: 10.1016/j.gloenvcha.2010.11.010
- Seino K, Nakamura K, Alemi S. Social interactions and heat stress mitigation among elderly people in a healthy city. Lancet Planet Health. 2024;8(Suppl 1):S12. doi: 10.1016/S2542-5196(24)00077-9
- Huang G, Cadenasso ML. People, landscape, and urban heat island: dynamics among neighborhood social conditions, land cover and surface temperatures. Landsc Ecol Springer Netherlands. 2016;31(10):2507–2515. doi: 10.1007/s10980-016-0437-z
- Akbari H, Cartalis C, Kolokotsa A, et al. Local climate change and urban heat island mitigation techniques – the state of the art. J Civil Eng Manage. 2016;22(2):1–16. doi: 10.3846/13923730.2015.1111934
- Stone B Jr., Vargo J, Liu P, et al. Avoided heat-related mortality through climate adaptation strategies in three US cities. PLOS ONE. 2014;9(6):e100852. doi: 10.1371/journal.pone.0100852
- Hart M, Sailor DJ. Quantifying the influence of land-use and surface characteristics on spatial variability in the urban heat island. J Theor Appl Clim. 2008;95(3–4):397–406. doi: 10.1007/s00704-008-0017-5
- Akbari H, Levinson R, Rainer L. Monitoring the energy-use effects of cool roofs on California commercial buildings. Energy Build. 2005;37(10):1007–1016. doi: 10.1016/j.enbuild.2004.11.013
- Jandaghian Z, Akbari H. Increasing urban albedo to reduce heat-related mortality in Toronto and Montreal, Canada. Energy Build. 2021;237:110697. doi: 10.1016/j.enbuild.2020.110697
- Kalkstein LS. A new approach to evaluate the impact of climate on human mortality. Environ Health Perspect. 1999;96:145–150. doi: 10.1289/ehp.9196145
- Kalkstein K, Sailor L, Shickman D, et al. Assessing the health impacts of urban heat island reduction strategies in the District of Columbia. Global Cool Cities Alliance; 2013. https://efaidnbmnnnibpcajpcglclefindmkaj/https://coolrooftoolkit.org/wp-content/uploads/2014/07/Three-City-Heat-Health-Report-FINAL.pdf
- Iungman T, Cirach M, Marando F, et al. Cooling cities through urban green infrastructure: a health impact assessment of European cities. Lancet. 2023;401(10376):577–589. doi: 10.1016/S0140-6736(22)02585-5
- Bowler DE, Buyung-Ali L, Knight TM, et al. Urban greening to cool towns and cities: a systematic review of the empirical evidence. Landsc Urban Plan. 2010;97(3):147–155. doi: 10.1016/j.landurbplan.2010.05.006
- Norton BA, Coutts AM, Livesley SJ, et al. Planning for cooler cities: a framework to prioritise green infrastructure to mitigate high temperatures in urban landscapes. Landsc Urban Plan. 2015;134:127–138. doi: 10.1016/j.landurbplan.2014.10.018
- Aram F, Higueras Garcia E, Solgi E, et al. Urban green space cooling effect in cities. Heliyon. 2019;5(4):e01339. doi: 10.1016/j.heliyon.2019.e01339
- Rotem-Mindali O, Michael Y, Helman D, et al. The role of local land-use on the urban heat island effect of Tel Aviv as assessed from satellite remote sensing. Appl Geogr. 2015;56:145–153. doi: 10.1016/j.apgeog.2014.11.023
- Coutts AM, Harris R. A multi-scale assessment of urban heating in Melbourne during an extreme heat event and policy approaches for adaptation. Victorian Centre for Climate Change and Adaptation Research, Melbourne; 2013. https://watersensitivecities.org.au/content/vcccar-report-multi-scale-assessment-urban-heating-melbourne-extreme-heat-event-policy-approaches-adaptation/
- Taleghani M, Kleerekoper L, Tenpierik M, et al. Outdoor thermal comfort within five different urban forms in the Netherlands. Build Environ. 2015;83:65–78. doi: 10.1016/j.buildenv.2014.03.014
- Dimoudi A, Nikolopoulou M. Vegetation in the urban environment: Microclimatic analysis and benefits. Energy Build. 2003;35(1):69–76. doi: 10.1016/S0378-7788(02)00081-6
- G-Y Q, H-Y L, Q-T Z, et al. Effects of evapotranspiration on mitigation of urban temperature by vegetation and urban agriculture. J Integ Agric. 2013;12(8):1307–1315. doi: 10.1016/S2095-3119(13)60543-2
- Kurn DM, Bretz SE, Akbari H, et al. The Potential for Reducing Urban Air Temperatures and Energy Consumption Through Vegetative Cooling. 1982. https://www.osti.gov/servlets/purl/10180633
- Spronken-Smith RA, Oke TR. The thermal regime of urban parks in two cities with different summer climates. Int J Remote Sens. 1998;19(11):2085–2104. doi: 10.1080/014311698214884
- Lockwood JM, Wilkins BW, Halliwill JR. H1 receptor-mediated vasodilatation contributes to postexercise hypotension. J Physiol. 2005;563(Pt 2):633–642. doi: 10.1113/jphysiol.2004.080325
- Spronken-Smith R, Oke T. Scale modelling of nocturnal cooling in urban parks. Bound-Lay Meteorol. 1999;93(2):287–312. doi: 10.1023/A:1002001408973
- Owens TW, Carlson TN, Gillies RR. An assessment of satellite remotely-sensed land cover parameters in quantitatively describing the climatic effect of urbanization. Int J Remote Sens Environ. 1998;19(9):1663–1681. doi: 10.1080/014311698215171
- Zuurbier M, van Loenhout JAF, le Grand A, et al. Street temperature and building characteristics as determinants of indoor heat exposure. Sci Total Environ. 2021;766:144376. doi: 10.1016/j.scitotenv.2020.144376
- Giles-Corti B, Broomhall MH, Knuiman M, et al. Increasing walking: how important is distance to, attractiveness, and size of public open space? Am J Prev Med. 2005;28(2 Suppl 2):169–176. doi: 10.1016/j.amepre.2004.10.018
- Coutts AM, Tapper NJ, Beringer J, et al. Watering our cities: The capacity for Water Sensitive Urban Design to support urban cooling and improve human thermal comfort in the Australian context. Prog Phys Geog. 2013;37(1):2–28. doi: 10.1177/0309133312461032
- Akbari H, Menon S, Rosenfeld A. Global cooling: increasing world-wide urban albedos to offset CO2. Clim Change. 2009;13(1):28.
- Cheela VRS, John M, Biswas W, et al. Combating urban heat island effect—a review of reflective pavements and tree shading strategies. Buildings. 2021;11(3):93. doi: 10.3390/buildings11030093
- Rizwan AM, Dennis LY, Chunho LIU. A review on the generation, determination and mitigation of urban heat island. J Environ Sci. 2008;20(1):120–128. doi: 10.1016/S1001-0742(08)60019-4
- Jandaghian Z, Berardi U. Comparing urban canopy models for microclimate simulations in weather research and forecasting models. Sustain Cities Soc. 2020;55:102–1025. doi: 10.1016/j.scs.2020.102025
- Synnefa A, Santamouris M, Apostolakis K. On the development, optical properties and thermal performance of cool colored coatings for the urban environment. Sol Energy. 2007;81(4):488–497. doi: 10.1016/j.solener.2006.08.005
- Santamouris M, Ding L, Fiorito F, et al. Passive and active cooling for the outdoor built environment – analysis and assessment of the cooling potential of mitigation technologies using performance data from 220 large scale projects. Sol Energy. 2017;154:14–33. doi: 10.1016/j.solener.2016.12.006
- Santamouris M, Fiorito F. On the impact of modified urban albedo on ambient temperature and heat related mortality. Sol Energy. 2021;216:493–507. doi: 10.1016/j.solener.2021.01.031
- Wong NH, Chen Y, Ong CL, et al. Investigation of thermal benefits of rooftop garden in the tropical environment. Build Envir. 2003;38(2):261–270. doi: 10.1016/S0360-1323(02)00066-5
- He C, He L, Zhang Y, et al. Potential impacts of cool and green roofs on temperature-related mortality in the Greater Boston region. Environ Res Lett. 2020;15(9):094042. doi: 10.1088/1748-9326/aba4c9
- Saiz S, Kennedy C, Bass B, et al. Comparative life cycle assessment of standard and green roofs. Environ Sci Technol. 2006;40(13):4312–4316. doi: 10.1021/es0517522
- Dong J, Lin M, Zuo J, et al. Quantitative study on the cooling effect of green roofs in a high-density urban Area—A case study of Xiamen, China. J Clean Prod. 2020;255(10):120152. doi: 10.1016/j.jclepro.2020.120152
- Tan H, Kotamarthi R, Wang J, et al. Impact of different roofing mitigation strategies on near-surface temperature and energy consumption over the Chicago metropolitan area during a heatwave event. Sci Total Environ. 2023;860:160508. doi: 10.1016/j.scitotenv.2022.160508
- Jamei E, Chau HW, Seyedmahmoudian M, et al. Review on the cooling potential of green roofs in different climates. Sci Total Environ. 2021;791:148407. doi: 10.1016/j.scitotenv.2021.148407
- Li D, Bou-Zeid E, Oppenheimer M. The effectiveness of cool and green roofs as urban heat island mitigation strategies. Environ Res Lett. 2014;9(5):055002. doi: 10.1088/1748-9326/9/5/055002
- Phelan PE, Kaloush K, Miner M, et al. Urban heat island: mechanisms, implications, and possible remedies. Annu Rev Environ Resour. 2015;40(1):285–307. doi: 10.1146/annurev-environ-102014-021155
- Centers for Disease Control and Prevention. Heat illness and deaths--New York City, 2000-2011. MMWR Morb Mortal Wkly Rep. 2013;62(31):617–621.
- Spalt EW, Curl CL, Allen RW, et al. Erratum: time-location patterns of a diverse population of older adults: the Multi-Ethnic Study of atherosclerosis and air pollution (MESA air). J Expo Sci Environ Epidemiol. 2016;26(4):436. doi: 10.1038/jes.2016.13
- Farrow A, Taylor H, Golding J. Time spent in the home by different family members. Environ Technol. 1997;18(6):605–613. doi: 10.1080/09593331808616578
- van Loenhout JA, le Grand A, Duijm F, et al. The effect of high indoor temperatures on self-perceived health of elderly persons. Environ Res. 2016;146:27–34. doi: 10.1016/j.envres.2015.12.012
- Wang Y, Liu Y, Song C, et al. Appropriate indoor operative temperature and bedding micro climate temperature that satisfies the requirements for sleep thermal comfort. Build Environ. 2015;92:20–29. doi: 10.1016/j.buildenv.2015.04.015
- Hughes C, Sukumar N. Summer thermal comfort and overheating in the elderly. Build Serv Eng Res Technol. 2019;40(4):426–445. doi: 10.1177/0143624419844518
- Rey G, Fouillet A, Bessemoulin P, et al. Heat exposure and socio-economic vulnerability as synergistic factors in heat-wave-related mortality. Eur J Epidemiol. 2009;24(9):495–502. doi: 10.1007/s10654-009-9374-3
- Haines A, Kovats RS, Campbell-Lendrum D, et al. Climate change and human health: impacts, vulnerability, and mitigation. Lancet. 2006;367(9528):2101–2109. doi: 10.1016/S0140-6736(06)68933-2
- World Health Organization. Housing and Health Guidelines. 2018; https://iris.who.int/bitstream/handle/10665/276001/9789241550376-eng.pdf
- Loughnan M, Carroll M, Tapper NJ. The relationship between housing and heat wave resilience in older people. Int J Biometeorol. 2015;59(9):1291–1298. doi: 10.1007/s00484-014-0939-9
- Hamza N, Gilroy R. The challenge to UK energy policy: an ageing population perspective on energy saving measures and consumption. Energy Policy. 2011;39(2):782–789. doi: 10.1016/j.enpol.2010.10.052
- Campell M, McKeown D. Update on Extreme Heat and Maximum Indoor Temperature Standard for Multi-unit Residential Buildings. In: Toronto Public Health; 2015. https://www.toronto.ca/legdocs/mmis/2016/td/bgrd/backgroundfile-90418.pdf
- Chen H, Wang J, Li Q, et al. Assessment of the effect of cold and hot temperatures on mortality in Ontario, Canada: a population-based study. CMAJ Open. 2016;4(1):E48–58. doi: 10.9778/cmajo.20150111
- Meade RD, Akerman AP, Notley SR, et al. Effects of daylong exposure to Indoor Overheating on thermal and cardiovascular strain in older adults: a randomized crossover trial. Environ Health Perspect. 2024;132(2):27003. doi: 10.1289/EHP13159
- Baborska-Narozny M, Stevenson F, Chatterton P. Temperture in housing: Stratification and contextual factors. Eng Sustainability. 2015;9:1–17. doi: 10.1680/jensu.14.00054
- Ji Y, Fitton R, Swan W, et al. Assessing overheating of the UK existing dwellings – a case study of replica Victorian end terrace house. Build Environ. 2014;7:1–11. doi: 10.1016/j.buildenv.2014.03.012
- Mavrogianni A, Davies M, Wilkinson P, et al. London housing and climate change: impact on comfort and health - preliminary results of a summer overheating study. Open House Int. 2010;35(2):49–59. doi: 10.1108/OHI-02-2010-B0007
- Morgan C, Foster JA, Poston A, et al. Overheating in Scotland: contributing factors in occupied homes. Build Res Inf. 2017;45(1–2):143–156. doi: 10.1080/09613218.2017.1241472
- Tillson AA, Oreszczyn T, Palmer J. Assessing impacts of summertime overheating: some adaptation strategies. Build Res Inf. 2013;41(6):652–661. doi: 10.1080/09613218.2013.808864
- White-Newsome JL, Sanchez BN, Jolliet O, et al. Climate change and health: indoor heat exposure in vulnerable populations. Environ Res. 2012;112:20–27. doi: 10.1016/j.envres.2011.10.008
- Smargiassi A, Fournier M, Griot C, et al. Prediction of the indoor temperatures of an urban area with an in-time regression mapping approach. J Expo Sci Environ Epidemiol. 2008;18(3):282–288. doi: 10.1038/sj.jes.7500588
- Wright AJ, Young A, Natarajan S. Dwelling temperatures and comfort during the August 2003 heat wave. Build Serv Eng Res Technol. 2005;26(4):285–300. doi: 10.1191/0143624405bt136oa
- Gul MS, Jenkins D, Patidar S, et al. Communicating future overheating risks to building design practitioners: using the low carbon futures tool. Build Serv Eng Res Technol. 2015;36(2):182–195. doi: 10.1177/0143624414566475
- Taylor J, Davies M, Mavrogianni A, et al. Mapping indoor overheating and air pollution risk modification across Great Britain: a modelling study. Build Environ. 2016;99:1–12. doi: 10.1016/j.buildenv.2016.01.010
- Oikonomou E, Davies M, Mavrogianni A, et al. Modelling the relative importance of the urban heat island and the thermal quality of dwellings for overheating in London. Build Environ. 2012;57:223–238. doi: 10.1016/j.buildenv.2012.04.002
- Symonds P, Taylor J, Mavrogianni A, et al. Overheating in English dwellings: comparison modelled and monitored large-scale. Build Res Inf. 2017;45(1–2):195–208. doi: 10.1080/09613218.2016.1224675
- Mirzaei PA, Haghighat F, Nakhaie AA, et al. Indoor thermal condition in urban heat island - Development of a predictive tool. Build Environ. 2012;57:7–17. doi: 10.1016/j.buildenv.2012.03.018
- Sakka A, Santamouris M, Livada I, et al. On the thermal performance of low income housing during heat waves. Energy Build. 2012;49:69–77. doi: 10.1016/j.enbuild.2012.01.023
- Pathan A, Mavrogianni A, Summerfield A, et al. Monitoring summer indoor overheating in the London housing stock. Energy Build. 2017;141:361–378. doi: 10.1016/j.enbuild.2017.02.049
- Maivel M, Kurnitski J, Kalamees T. Field survey of overheating problems in Estonian apartment buildings. Archi Sci Rev. 2015;58(1):1–10. doi: 10.1080/00038628.2014.970610
- McGill G, Sharpe T, Robertson L, et al. Meta-analysis of indoor temperatures in new-build housing. Build Res Inf. 2017;45(1–2):19–39. doi: 10.1080/09613218.2016.1226610
- Mavrogianni A, Johnson F, Ucci M, et al. Historic variations in Winter indoor domestic temperatures and potential implications for body weight gain. Indoor Built Environ. 2013;22(2):360–375. doi: 10.1177/1420326X11425966
- Arena L, Mantha P, Karagiozis A. Monitoring of internal moisture loads in residential buildings. SSRN Electron J. 2010. doi: 10.2139/ssrn.1761413
- Roberts D, Lay K. Variability in measured space temperatures in 60 homes. United States; 2013. http://efaidnbmnnnibpcajpcglclefindmkaj/https://www.nrel.gov/docs/fy13osti/58059.pdf
- Laouadi A, Bartko M, Gaur A, et al. Climate resilience buildings: guideline for management of overheating risk in residential buildings. National Research Council of Canada. Construction; 2021. https://nrc-publications.canada.ca/eng/view/object/?id=9c60dc19-ca18-4f4c-871f-2633f002b95c
- Dahlblom MJ. Vertical temperature increase in multi-storey buildings. In NSB 2014: 10th Nordic Symposium on Building Physics; 5–19 June 2014; Lund, Sweden.
- Paraschiv S, Paraschiv LS, Serban A. Increasing the energy efficiency of a building by thermal insulation to reduce the thermal load of the micro-combined cooling, heating and power system. Energy Rep. 2021;7:286–298. doi: 10.1016/j.egyr.2021.07.122
- Rehm M, Cheung KS, Filippova O, et al. Stigma, risk perception and the remediation of leaky homes in New Zealand. New Zeal Econ Pap. 2020;54(1):89–105. doi: 10.1080/00779954.2019.1631878
- Lomas KJ, Porritt SM. Overheating in buildings: lessons from research. Build Res Inf. 2017;45(1–2):1–18. doi: 10.1080/09613218.2017.1256136
- Abdullah AK, Darsaleh A, Abdelbaqi S, et al. Thermal performance evaluation of window shutters for residential buildings: a case study of Abu Dhabi, UAE. Energies. 2022;15(16):5858. doi: 10.3390/en15165858
- Taylor J, Wilkinson P, Picetti R, et al. Comparison of built environment adaptations to heat exposure and mortality during hot weather, West Midlands region, UK. Environ Int. 2018;111:287–294. doi: 10.1016/j.envint.2017.11.005
- Haralambopoulos DA, Paparsenos GF. Assessing the thermal insulation of old buildings—the need for in situ spot measurements of thermal resistance and planar infrared thermography. Energy Conversion Manage. 1998;39(1–2):65–79. doi: 10.1016/S0196-8904(96)00176-8
- Carbon Hub Z. Overheating in homes, the big picture, Full report. London; 2015.
- Kestens Y, Brand A, Fournier M. Modelling the variation of land surface temperature as determinant of risk of heat-related health events. Int J Health Geogr. 2011;10(1):7. doi: 10.1186/1476-072X-10-7
- Kilbourne EM, Choi K, Jones TS, et al. Risk factors for heatstroke. A case-control study. JAMA. 1982;247(24):3332–3336. doi: 10.1001/jama.1982.03320490030031
- Uejio CK, Wilhelmi OV, Golden JS, et al. Intra-urban societal vulnerability to extreme heat: the role of heat exposure and the built environment, socioeconomics, and neighborhood stability. Health & Place. 2011;17(2):498–507. doi: 10.1016/j.healthplace.2010.12.005
- Dengel A, Swainson M. Overheating in new homes: a review of the evidence. London: HS BRE Press on behalf of NHBC Foundation; 2012.
- Barbosa R, Vicente R, Santos R. Climate change and thermal comfort in southern Europe housing: a case study from Lisbon. Build Environ. 2015;92:440–451. doi: 10.1016/j.buildenv.2015.05.019
- Fosas D, Coley DA, Natarajan S, et al. Mitigation versus adaptation: does insulating dwellings increase overheating risk? Build Environ. 2018;143:740–759. doi: 10.1016/j.buildenv.2018.07.033
- McLoed RS, Hopfe CJ, Kwan A. An investigation into future performance and overheating risks in Passivhaus dwellings. Build Environ. 2013;70(189–209):189–209. doi: 10.1016/j.buildenv.2013.08.024
- Shrubsole C, MacMillan A, Davies M, et al. 100 unintended consequences of policies to improve the energy efficiency of the UK housing stock. Indoor Built Environ. 2014;23(3):340–352. doi: 10.1177/1420326X14524586
- Tink V, Porritt S, Allinson D, et al. Measuring and mitigating overheating risk in solid wall dwellings retrofitted with internal wall insulation. Build Environ. 2018;141:247–261. doi: 10.1016/j.buildenv.2018.05.062
- Kim Y, Gasparrini A, Hashizume M, et al. Heat-Related Mortality in Japan after the 2011 Fukushima Disaster: An Analysis of Potential Influence of Reduced Electricity Consumption. Environ Health Perspect. 2017;125(7):077005. doi: 10.1289/EHP493
- Government of Canada. Keeping the Heat in. Natural Resources Canada. https://natural-resources.canada.ca/energy-efficiency/homes/make-your-home-more-energy-efficient/keeping-the-heat/15768
- Birchmore R, Davies K, Etherington P, et al. Overheating in Auckland homes: testing and interventions in full-scale and simulated houses. Build Res Inf. 2017;45(1–2):157–175. doi: 10.1080/09613218.2017.1232857
- Ong KS. Temperature reduction in attic and ceiling via insulation of several passive roof designs. Energy Conv Manag. 2011;52(6):2405–2411. doi: 10.1016/j.enconman.2010.12.044
- Tariku F, Iffa E. Effect of attic insulation thickness and solar gain in a mild climate. Energy Procedia. 2015;78:67–72. doi: 10.1016/j.egypro.2015.11.116
- Yang T, Clements-Croome DJ. Natural Ventilation in Built Environment. In: Meyers R, editor Encyclopedia of Sustainability Science and Technology. New York, NY: Springer New York; 2012. pp. 6865–6896.
- Mourkos K, Rs M, Hopfe CJ, et al. Assessing the application and limitations of a standardised overheating risk-assessment methodology in a real-world context. Build Environ. 2020;181:107070. doi: 10.1016/j.buildenv.2020.107070
- National Renewable Energy Laboratory. Cooling Your Home with Fans and Ventilation. Energy Efficiency and Renewable Energy Clearing house. Information and Outreach Program, US Department of Energy. 2001. http://efaidnbmnnnibpcajpcglclefindmkaj/https://www.nrel.gov/docs/fy01osti/29513.pdf
- Peavy B. A model for predicting the thermal performance of ventilated attics. In: Summer Attic and Whole-House Ventilation. Proceedings of a workshop held on July 13, 1978. editor: Reppert MH, 1979; National Bureau of Standards Special Publication 548:119–149. https://www.govinfo.gov/content/pkg/GOVPUB-C13-bc8591331c75e4a6665b403679433827/pdf/GOVPUB-C13-bc8591331c75e4a6665b403679433827.pdf
- Parker DS, Sonne JK, Sherwin JR, et al. Comparative evaluation of the impact of roofing systems on residential cooling energy demand in Florida. Paper presented at: Proceedings of the 2002 ACEEE Summer Study on Energy Efficiency in Buildings, 2002. https://www.fsec.ucf.edu/en/publications/pdf/fsec-cr-1220-00.pdf
- Fan M, Fu Z, Wang J, et al. A review of different ventilation modes on thermal comfort, air quality and virus spread control. Build Environ. 2022;212:108831. doi: 10.1016/j.buildenv.2022.108831
- Jensen CA, Cadorel X, Chu A Ventilation for reduced heat stress in apartments. Back to the Future: The Next 50 Years, 51st International Conference of the Architectural Science Association; 2017. pp. 615–624.
- National Research Council. The National Building Code of Canada. 2020. https://nrc.canada.ca/en/certifications-evaluations-standards/codes-canada/codes-canada-publications/national-building-code-canada-2020
- Akbari H, Kurn DM, Bretz SE, et al. Peak power and cooling energy savings of shade trees. Energy Build. 1997;25(2):139–148. doi: 10.1016/S0378-7788(96)01003-1
- Heisler GM. Effects of individual trees on the solar radiation climate of small buildings. Urban Ecol. 1986;9(3):337–359. doi: 10.1016/0304-4009(86)90008-2
- La Gennusa M, Nucara A, Pietrafesa M, et al. A model for managing and evaluating solar radiation for indoor thermal comfort. Sol Energy. 2007;81(5):594–606. doi: 10.1016/j.solener.2006.09.005
- Li H. Chapter 13 - Impacts of Pavement Strategies on Human Thermal Comfort. In:Li H, editor Pavement Materials for Heat Island Mitigation. Boston: Butterworth-Heinemann; 2016. pp. 281–306.
- Marino C, Nucara A, Pietrafesa M. Thermal comfort in indoor environment: effect of the solar radiation on the radiant temperature asymmetry. Sol Energy. 2017;144:295–309. doi: 10.1016/j.solener.2017.01.014
- Freewan AAY. Impact of external shading devices on thermal and daylighting performance of offices in hot climate regions. Sol Energy. 2014;102:14–30. doi: 10.1016/j.solener.2014.01.009
- Taylor J, Symonds P, Heaviside C, et al. Projecting the impacts of housing on temperature-related mortality in London during typical future years. Energy Build. 2021;249:111233. doi: 10.1016/j.enbuild.2021.111233
- Mohammed A, Tariq MAUR, Ng AWM, et al. Reducing the cooling loads of buildings using shading devices: A case study in darwin. Sustainability. 2022;14(7):3775. doi: 10.3390/su14073775
- US Department of Energy. Efficient Window Coverings. 2023; https://www.energy.gov/energysaver/energy-efficient-window-coverings
- Rheault S, Bilgen E. Experimental study of full-size automated venetian blind windows. Sol Energy. 1990;44(3):157–160. doi: 10.1016/0038-092X(90)90079-R
- Synnefa A, Dandou A, Santamouris M, et al. On the use of cool materials as a heat island mitigation strategy. J Appl Meteorol Clim. 2008;47(11):2846–2856. doi: 10.1175/2008JAMC1830.1
- Bozonnet E, Doya M, Allard F. Cool roofs impact on building thermal response: a French case study. Energy Build. 2011;43(11):3006–3012. doi: 10.1016/j.enbuild.2011.07.017
- Santamouris M, Synnefa MA, Kolokotsa D, et al. Passive cooling of the built environment—use of innovative reflective materials to fight heat island and decrease cooling needs. Int J Low Carbon. 2008;3(2):71–82. doi: 10.1093/ijlct/3.2.71
- Bretz S, Akbari H. Long-term performance of high albedo roof coatings. Building Envir. 1997;25(2):159–167. doi: 10.1016/S0378-7788(96)01005-5
- Simpson JR, McPherson EG. The effects of roof albedo modification on cooling loads of scale model residences in Tucson, Arizona. Energy Build. 1997;25(2):127–137. doi: 10.1016/S0378-7788(96)01002-X
- Rawat M, Singh RN. A study on the comparative review of cool roof thermal performance in various regions. Energy Built Environ. 2022;3(3):327–347. doi: 10.1016/j.enbenv.2021.03.001
- Akbari H. Shade trees reduce building energy use and CO2 emissions from power plants. Environ Pollut. 2002;116:S119–S126. doi: 10.1016/S0269-7491(01)00264-0
- Sen S, Khazanovich L. Limited application of reflective surfaces can mitigate urban heat pollution. Nat Commun. 2021;12(1):3491. doi: 10.1038/s41467-021-23634-7
- Mandal J, Fu Y, Overvig AC, et al. Hierarchically porous polymer coatings for highly efficient passive daytime radiative cooling. Science. 2018;362(6412):315–319. doi: 10.1126/science.aat9513
- Jay O, Capon A, Berry P, et al. Reducing the health effects of hot weather and heat extremes: from personal cooling strategies to green cities. Lancet. 2021;398(10301):709–724. doi: 10.1016/S0140-6736(21)01209-5
- Richard L, Kosatsky T, Renouf A. Correlates of hot day air-conditioning use among middle-aged and older adults with chronic heart and lung diseases: the role of health beliefs and cues to action. Health Educ Res. 2011;26(1):77–88. doi: 10.1093/her/cyq072
- McGeehin MA, Mirabelli M. The potential impacts of climate variability and change on temperature-related morbidity and mortality in the United States. Environ Health Perspect. 2001;109(Suppl 2):185–189. doi: 10.1289/ehp.109-1240665
- Brucker G. Vulnerable populations: lessons learnt from the summer 2003 heat waves in Europe. Euro Surveill. 2005;10(7):147. doi: 10.2807/esm.10.07.00551-en
- Gronlund CJ. Racial and socioeconomic disparities in heat-related health effects and their mechanisms: a review. Curr Epidemiol Rep. 2014;1(3):165–173. doi: 10.1007/s40471-014-0014-4
- World Health Organization. Public health advice on preventing health effects to heat. Regional Office for Europe; 2011. https://www.who.int/publications/i/item/WHO-EURO-2011-2510-42266-58691
- Government of Canada. Extreme heat: heat waves. Health Canada; 2019. https://www.canada.ca/en/health-canada/services/climate-change-health/extreme-heat.html
- Gupta S, Carmichael C, Simpson C, et al. Electric fans for reducing adverse health impacts in heatwaves. Cochrane Database Of Systematic Reviews. 2012;7(7):CD009888. doi: 10.1002/14651858.CD009888.pub2
- World Health Organization. Heat and health in the WHO European Region: updated evidence for effective prevention. In: Copenhagen: WHO Regional Office for Europe Copenhagen; 2021. https://www.who.int/europe/publications/i/item/9789289055406
- Morris NB, Chaseling GK, English T, et al. Electric fan use for cooling during hot weather: a biophysical modelling study. Lancet Planet Health. 2021;5(6):e368–e377. doi: 10.1016/S2542-5196(21)00136-4
- Meade RD, Notley SR, Kirby NV, et al. A critical review of the effectiveness of electric fans as a personal cooling intervention in hot weather and heatwaves. Lancet Planet Health. 2024;8(4):e256–e269. doi: 10.1016/S2542-5196(24)00030-5
- Gagnon D, Romero SA, Cramer MN, et al. Age modulates physiological responses during Fan Use under extreme heat and humidity. Medicine And Science In Sports And Exercise. 2017;49(11):2333–2342. doi: 10.1249/MSS.0000000000001348
- Ravanelli NM, Hodder SG, Havenith G, et al. Heart rate and body temperature responses to extreme heat and humidity with and without electric fans. JAMA. 2015;313(7):724–725. doi: 10.1001/jama.2015.153
- Schmidt MD, Notley SR, Meade RD, et al. Revisiting regional variation in the age-related reduction in sweat rate during passive heat stress. Physiol Rep. 2022;10(7):e15250. doi: 10.14814/phy2.15250
- Morris NB, English T, Hospers L, et al. The effects of electric fan use under differing resting heat index conditions: a clinical trial. Ann Intern Med. 2019;171(9):675–677. doi: 10.7326/M19-0512
- Gagnon D, Crandall CG. Electric fan use during heat waves: turn off for the elderly? Temperature. 2017;4(2):104–106. doi: 10.1080/23328940.2017.1295833
- Gagnon D, Romero SA, Cramer MN, et al. Cardiac and thermal strain of elderly adults exposed to extreme heat and humidity with and without electric fan use. JAMA. 2016;316(9):989–991. doi: 10.1001/jama.2016.10550
- Black-Ingersoll F, de Lange J, Heidari L, et al. A Literature Review of Cooling Center, Misting Station, Cool Pavement, and Cool Roof Intervention Evaluations. Atmosphere. 2022;13(7):1103. doi: 10.3390/atmos13071103
- Farnham C. Quantifying the over-estimation of the perceived cooling from a mist Fan. Envir Sci Eng. 2018;IS-2:5–8.
- Farnham C, Yuan J. Possible perception bias in the thermal evaluation of evaporation cooling with a Misting Fan. Clean Technol. 2021;3(1):183–205. doi: 10.3390/cleantechnol3010011
- Farnham C, Emura K, Mizuno T. Evaluation of cooling effects: outdoor water mist fan. Build Res Inf. 2015;43(3):334–345. doi: 10.1080/09613218.2015.1004844
- Ulpiani G, di Perna C, Zinzi M. Mist cooling in urban spaces: understanding the key factors behind the mitigation potential. Appl Therm Eng. 2020;178:115644. doi: 10.1016/j.applthermaleng.2020.115644
- Zheng K, Yuan C, Wong NH, et al. Dry mist systems and its impact on thermal comfort for the tropics. Sustain Cities Soc. 2019;51:101727. doi: 10.1016/j.scs.2019.101727
- Desert A, Naboni E, Garcia D. The spatial comfort and thermal delight of outdoor misting installations in hot and humid extreme environments. Energy Build. 2020;224:110202. doi: 10.1016/j.enbuild.2020.110202
- Vanos JK, Wright MK, Kaiser A, et al. Evaporative misters for urban cooling and comfort: effectiveness and motivations for use. Int J Biometeorol. 2022;66(2):357–369. doi: 10.1007/s00484-020-02056-y
- Selkirk GA, Tm M, Wong J. Active versus passive cooling during work in warm environments while wearing firefighting protective clothing. J Occup Environ Hyg. 2004;1(8):521–531. doi: 10.1080/15459620490475216
- Belarbi R, Ghiaus C, Allard F. Modeling of water spray evaporation: application to passive cooling of buildings. Sol Energy. 2006;80(12):1540–1552. doi: 10.1016/j.solener.2006.01.004
- Semenza JC, Hall DE, Wilson DJ, et al. Public perception of climate change voluntary mitigation and barriers to behavior change. Am J Prev Med. 2008;35(5):479–487. doi: 10.1016/j.amepre.2008.08.020
- Lynch GP, Périard JD, Pluim BM, et al. Optimal cooling strategies for players in Australian Tennis Open conditions. J Sci Med Sport. 2018;21(3):232–237. doi: 10.1016/j.jsams.2017.05.017
- Schranner D, Scherer L, Lynch GP, et al. In-play cooling interventions for simulated match-play tennis in Hot/Humid conditions. Medicine and science In sports and exercise. 2017;49(5):991–998. doi: 10.1249/MSS.0000000000001183
- Cuddy JS, Hailes WS, Ruby BC. A reduced core to skin temperature gradient, not a critical core temperature, affects aerobic capacity in the heat. J Thermal Biol. 2014;43:7–12. doi: 10.1016/j.jtherbio.2014.04.002
- Ely BR, Ely MR, Cheuvront SN, et al. Evidence against a 40 degrees C core temperature threshold for fatigue in humans. J Appl Physiol. 2009;107(5):1519–1525. doi: 10.1152/japplphysiol.00577.2009
- DeGroot DW, Gallimore RP, Thompson SM, et al. Extremity cooling for heat stress mitigation in military and occupational settings. J Thermal Biol. 2013;38(6):305–310. doi: 10.1016/j.jtherbio.2013.03.010
- House JR. Extremity cooling as a method for reducing heat strain. J Def Sci. 1998;3(1):108–114.
- House JR, Holmes C, Allsopp AJ. Prevention of heat strain by immersing the hands and forearms in water. J R Nav Med Serv. 1997;83(1):26–30. doi: 10.1136/jrnms-83-26
- Livingstone SD, Nolan RW, Cattroll SW. Heat loss caused by immersing the hands in water. Aviat Space Environ Med. 1989;60(12):1166–1171.
- Livingstone SD, Nolan RW, Keefe AA. Heat loss caused by cooling the feet. Aviat Space Environ Med. 1995;66(3):232–237.
- Allsopp AJ, Poole KA. The effect of hand immersion on body temperature when wearing impermeable clothing. J R Nav Med Serv. 1991;77(1):41–47. doi: 10.1136/jrnms-77-41
- Giesbrecht GG, Jamieson C, Cahill F. Cooling hyperthermic firefighters by immersing forearms and hands in 10 degrees C and 20 degrees C water. Aviat Space Environ Med. 2007;78(6):561–567.
- Meade RD, Er M, Jj M, et al. Body Core Temperature After Foot Immersion and Neck Cooling in Older Adults Exposed to Extreme Heat. JAMA. 2024;331(3):253–256. doi: 10.1001/jama.2023.24417
- Sathaye JA, Dale LL, Larsen PH, et al. Estimating impacts of warming temperatures on California’s electricity system. Glob Environ Change. 2013;23(2):499–511. doi: 10.1016/j.gloenvcha.2012.12.005
- Wang Z, Hong T, Li H. Informing the planning of rotating power outages in heat waves through data analytics of connected smart thermostats for residential buildings. Environ Res Lett. 2021;16(7):074003. doi: 10.1088/1748-9326/ac092f
- Morris NB, Gruss F, Lempert S, et al. A preliminary study of the effect of dousing and Foot Immersion on Cardiovascular and thermal responses to extreme heat. JAMA. 2019;322(14):1411–1413. doi: 10.1001/jama.2019.13051
- Cramer MN, Huang M, Moralez G, et al. Keeping older individuals cool in hot and moderately humid conditions: wetted clothing with and without an electric fan. J Appl Physiol. 2020;128(3):604–611. doi: 10.1152/japplphysiol.00786.2019
- Szlyk CP, Sils FR IV, Hubbard RW, et al. Effects of water temperature and flavoring on voluntary dehydration in men. Physiol Behav. 1989;45(3):639–647. doi: 10.1016/0031-9384(89)90085-1
- Naito T, Iribe Y, Ogaki T. Ice ingestion with a long rest interval increases the endurance exercise capacity and reduces the core temperature in the heat. J Physiol Anthropo. 2017;36(1):9. doi: 10.1186/s40101-016-0122-6
- Siegel R, Maté J, Brearley MB, et al. Ice slurry ingestion increases core temperature capacity and running time in the heat. Medicine And Science In Sports And Exercise. 2010;42(4):717–725. doi: 10.1249/MSS.0b013e3181bf257a
- Moore A, Pritchett KL, Pritchett RC, et al. Effects of pre-exercise ice slurry ingestion on physiological and perceptual measures in athletes with spinal cord injuries. Int J Exerc Sci. 2021;14(2):19–32.
- Morris N, C G, O J. Ice slurry ingestion leads to a lower net heat loss during exercise in the heat. Med Sci Sports Exerc. 2016;48(1):114–122. doi: 10.1249/MSS.0000000000000746
- Lamarche DT, Meade RD, McGinn R, et al. Temperature of ingested water during exercise does not affect body heat storage. Med Sci Sports Exerc. 2015;47(6):1272–1280. doi: 10.1249/MSS.0000000000000533
- Morris NB, Bain AR, Cramer MN, et al. Evidence that transient changes in sudomotor output with cold and warm fluid ingestion are independently modulated by abdominal, but not oral thermoreceptors. J Appl Physiol. 2014;116(8):1088–1095. doi: 10.1152/japplphysiol.01059.2013
- Jay O, Morris NB. Does Cold Water or Ice Slurry Ingestion During Exercise Elicit a Net Body Cooling Effect in the Heat? Sports Med. 2018;48(Suppl 1):17–29. doi: 10.1007/s40279-017-0842-8
- Naito T, Sagayama H, Akazawa N, et al. Ice slurry ingestion during break times attenuates the increase of core temperature in a simulation of physical demand of match-play tennis in the heat. Temperature. 2018;5(4):371–379. doi: 10.1080/23328940.2018.1475989
- Thirumagal K, Gayathri R, Vishnu P. Awareness of dental pain and sensitivity among elderly women – a survey. Drug Invention Today. 2020;14(7):1027–1030.
- Chebini A, Dilli E. Cold stimulus headache. Curr Neurol Neurosci Rep. 2019;19(7):46. doi: 10.1007/s11910-019-0956-5
- Wollner L, Kollins KJ. Disorders of the autonomic nervous system. In: brocklehurst J, Tallis R Fillit H, editors. Textbook of geriatric medicine and gerontology. Edinburgh: Churchill Livingstone; 1992. p. 399–403.
- Khamnei S, Hosseinlou A, Zamanlu M. Water temperature, voluntary drinking and fluid balance in dehydrated taekwondo athletes. J Sci Med Sport. 2011;10(4):718–724.
- Rodrigues P, Orssatto LBR, Gagnon D, et al. Passive heat therapy: a promising preventive measure for people at risk of adverse health outcomes during heat extremes. J Appl Physiol. 2024;136(4):677–694. doi: 10.1152/japplphysiol.00701.2023
- Janetos K-M, O’Connor FC, Koetje NJ, et al. Heat acclimation by warm-water immersion enhances whole-body heat loss in older adults. American College of Sports Medicine Annual Meeting, Boston, Massachusetts, USA. May 28-May 31, 2024.
- Anderson BG, Bell ML. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009;20(2):205–213. doi: 10.1097/EDE.0b013e318190ee08
- Ito K, Lane K, Olson C. Equitable access to air conditioning: a city health department’s perspective on preventing heat-related Deaths. Epidemiology. 2018;29(6):749–752. doi: 10.1097/EDE.0000000000000912
- Ostro B, Rauch S, Green R, et al. The effects of temperature and use of air conditioning on hospitalizations. Am J Epidemiol. 2010;172(9):1053–1061. doi: 10.1093/aje/kwq231
- Sera F, Hashizume M, Honda Y, et al. Air Conditioning and Heat-related Mortality: A Multi-country Longitudinal Study. Epidemiology. 2020;31(6):779–787. doi: 10.1097/EDE.0000000000001241
- Statistics Canada. The Prevalence of Household Air Conditioning in Canada. 2023. https://www150.statcan.gc.ca/n1/pub/82-003-x/2023007/article/00002-eng.htm
- Randazzo T, De Cian E, Mistry MN. Air conditioning and electricity expenditure: the role of climate in temperate countries. Econ Model. 2020;90:273–287. doi: 10.1016/j.econmod.2020.05.001
- Pavanello F, De Cian E, Davide M, et al. Air-conditioning and the adaptation cooling deficit in emerging economies. Nat Commun. 2021;12(1):6460. doi: 10.1038/s41467-021-26592-2
- Notley SR, Meade RD, Akerman AP, et al. Evidence for age-related differences in heat acclimatisation responsiveness. Exp Physiol. 2020;105(9):1491–1499. doi: 10.1113/EP088728
- World Health Organization. Health impact of low indoor temperatures: Report on a WHO meeting: Copenhagen, 11-14 November 1985. World Health Organization Regional Office for Europe; 1987.
- Widerynski S, Schramm P, Conlon K, et al. The Use of Cooling Centers to Prevent Heat-Related Illness: Summary of Evidence and Strategies for Implementation. Climate and Health.Technical Report Series Climate and Health Program, Centers for Disease Control and Prevention. 2017. http://efaidnbmnnnibpcajpcglclefindmkaj/https://www.cdc.gov/climateandhealth/docs/UseOfCoolingCenters.pdf
- Bassil KL, Cole DC. Effectiveness of public health interventions in reducing morbidity and mortality during heat episodes: a structured review. Int J Environ Res And Public Health. 2010;7(3):991–1001. doi: 10.3390/ijerph7030991
- Meade RD, Notley SR, Akerman AP, et al. Efficacy of cooling centers for mitigating physiological strain in older adults during daylong heat exposure: a laboratory-based heat wave simulation. Environ Health Perspect. 2023;131(6):67003. doi: 10.1289/EHP11651
- McGarr GW, Meade RD, Kenny GP. Indoor overheating influences self-reported symptoms and mood-state in older adults during a simulated heatwave: effects of mid-day cooling centre use. Physiol Behav. 2023;271:114335. doi: 10.1016/j.physbeh.2023.114335
- Bekö G, Toftum J, Clausen G. Modeling ventilation rates in bedrooms based on building characteristics and occupant behavior. Build Environ. 2011;46(11):2230–2237. doi: 10.1016/j.buildenv.2011.05.002
- Center for Disease Control and Prevention. Heat and older adults. Natural Disasters and Severe Weather. 2024. https://www.cdc.gov/disasters/extremeheat/older-adults-heat.html
