ABSTRACT
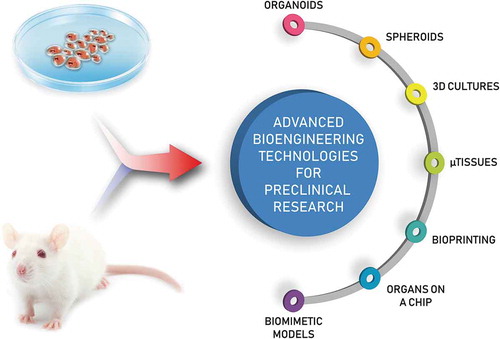
Current in vitro practices must overcome important challenges to compare favorably with human studies. The limited applicability of conventional in vitro assays and strategies can be explained by the fact that standard approaches do not enable recapitulation of the complexity of human tissues and physiological functions. To address this challenge, novel bioengineering tools, techniques and technologies are rapidly emerging to advance current fundamental knowledge and innovate in vitro practices. For example, organs-on-a-chip have recently appeared as a small-scale solution to overcome the transability, financial and ethical concerns associated with animal studies in drug discovery and development. In parallel, biomimetic interfaces are increasingly recapitulating 3D structures with tissue-like dynamic properties to allow in-depth investigation of disease mechanisms. This review aims at highlighting current bioengineering approaches poised to address the shortcomings of conventional in vitro research practices towards the generation of more effective solutions for improving human health.
Graphical Abstract
1. Introduction
Significant efforts in bioengineering research are currently focused on the development of increasingly more effective strategies to enhance the relevance and accuracy of in vitro practices. Conventional in vitro methods such as standard two-dimensional (2D) cultures rely on rigid plastic/glass culture plates and/or transwell inserts to support the adhesion and proliferation of a 2D cellular monolayer. These traditional cultures are still almost exclusively employed because of their simplicity and low cost, the abundance of comparative literature, the precise environmental control (e.g., temperature, CO2, exogenous nutrients and growth factors dissolved in the medium) and the ease of observation and analysis [Citation1,Citation2]. However, recent research has shifted toward more complex 3D systems in order to recreate a more realistic biochemical and biomechanical microenvironment that recapitulates the hierarchical architecture and dynamic nature of native tissues [Citation1]. In fact, although 2D assays have contributed to significantly advance our understanding of numerous cell-mediated processes and are still an effective approach for preliminary screening (e.g., to determine cytotoxic effects) [Citation3], conventional cell monolayer cultures are grown under simplified and physiologically unrealistic conditions, a factor that limits their translation to in vivo systems [Citation2]. In particular, in human organ systems, cells interact with a complex 3D microenvironment (i.e., the extracellular matrix, ECM), continuously supplemented by nutrients and oxygen. These physiological aspects are not recapitulated in conventional 2D systems, causing significant deviations from the in vivo reality [Citation4]. For example, in the case of cultures of central nervous system neurons, the 2D cellular microenvironment leads to aberrant cell–cell contacts and network formation, unrealistically flattens soma and growth cones and limits axon-dendrite outgrowth in all directions, ultimately causing significant deviations from the in vivo response [Citation2]. Similarly, conventional 2D models used in cancer biology modify cell morphology (e.g., forced polarity, flattened cell shape), alter the mechanical/biochemical signals and ultimately affect cell-to-cell communication [Citation5,Citation6]. Of note, such variations in cell behavior observed in conventional 2D monolayers also translate into altered sensitivity and resistance to drugs, ultimately resulting in increased rejection rates during clinical trials due to low efficacy and unacceptable toxicity in vivo [Citation7,Citation8].
To validate in vitro results and bridge them with the in vivo reality, scientists have relied on animal testing, a long-standing practice employed in many fields of biomedical research and medicine to understand a wide range of physiological/pathological phenomena and assess novel therapies prior to clinical trials with humans [Citation9,Citation10]. The main advantage of in vivo models is the use of complex living organisms that offer anatomical and physiological similarities with humans and replicate organ- and organ-system level functions, factors that have permitted to achieve important discoveries in a wide variety of research fields such as biology, physiology, endocrinology, and pharmacology (e.g., pharmacokinetics and pharmacodynamics) [Citation10]. Despite these advantages, in vivo testing has been affected by increasing costs and rising ethical issues, as well as challenges in the selection of the most informative models and in the extrapolation of data to humans due to interspecies differences [Citation9,Citation11]. In addition, animal models have shown significant differences with the human immune system in response to newly developed pharmaceutical drugs, a factor that has contributed to errant pharmacokinetic predictions in drug discovery [Citation8,Citation12]. Taken together, these limitations have spurred the search for alternative approaches to address fundamental aspects of biomedical problems.
In order to address the limitations of current in vitro practices and provide physiologically accurate alternatives to in vivo studies to lessen the current dependency on animal testing, recent efforts from the scientific community have focused on the development of in vitro systems capable of recapitulating key components of the architecture of human tissues and organ functions. In this context, bioengineering tools and methods, ranging from 3D tissue cultures (section 2.1) to biomimetic models (section 2.5), are increasingly demonstrating tremendous potential to overcome some of the limitations of conventional preclinical testing by combining the advantages of in vitro assays with the specificity of more complex in vivo models. The resulting synergy aims at replicating, in vitro, physiological processes and pathological conditions that are very challenging, and often impossible, to investigate directly in human patients, without the need of animal models. These bioengineering strategies are ultimately expected to generate accurate predictive and diagnostic data on a wide variety of biological processes, offering unique means to address specific health challenges (e.g., disease mechanisms) while developing real-world biomedical devices (e.g., drug screening assays).
This review brings attention on the latest in vitro bioengineering advances which promise to yield important long-term effects on human health. The goal of this work is not to report an exhaustive analysis of the existing literature on the subject but instead to provide the reader with a concise and critical overview of current bioengineering tools, methods and strategies for preclinical research.
2. Methods, strategies and technologies
2.1. Organoids, spheroids and 3D self-assembled tissue cultures
Pluripotent stem cells and organ-specific progenitor cells cultured as 3D entities have been shown to differentiate into a collection of cell types that self-organize spatially into structures reminiscent of aspects of a specific organ and exhibit some functionalities associated with that organ [Citation13]. The self-organization of these 3D cultures termed organoids occurs via two mechanisms: (i) cell sorting which is hypothesized to be driven by differential intercellular adhesion between cell types, and (ii) spatially restricted cell fate decision, likely influenced by local differences in the signaling environment resulting from diffusion limitations [Citation13]. Organoids provide an alternative to in vivo studies for the investigation of developmental, organ regenerative and homeostasis processes. This is because their formation implies the recapitulation of at least some of the mechanisms involved in organogenesis, organ regeneration and/or maintenance [Citation14]. The choice of cells used to generate organoids and particularly their maturation stage(s) dictate the mechanistic information that can be derived from the system. In a landmark study for the field, Sasai and coworkers produced embryonic stem cell-derived optic cup-like organoids [Citation15]. The study revealed aspects of the morphogenesis process involved in forming this complex structure, albeit painting an incomplete picture of the in vivo process owing to the absence of supporting tissues (). In another important report that helped cement the emerging field, tissue-specific adult stem cells were used to produce organoids with the crypt-villus structures of the small intestine [Citation16]. Their results highlighted expression profile similarities with native adult tissue structures. This distinction may reflect the timescale of in vitro experiments compared to the duration of human developmental and regenerative or homeostatic processes. The replication of organ structures and functionalities within micron to millimeter scale constructs also provides the opportunity to study pathological processes, as well as drug safety and efficacy. Furthermore, the use of patient-specific adult stem cells and induced pluripotent stem cells make this technology particularly suited for personalized medicine applications [Citation17].
Figure 1. Optic-cup-like organoid formed spontaneously from the 3D culture of mouse embryonic stem cell aggregates in the presence of matrigel. Reprinted from reference [Citation15] with permission. (a-l) show the temporal progression of the optic-cup-like structure formation along with the expression of key molecular markers for specific stages in the process. (m) shows the optic cup in a mouse embryo at time E11.5. (n) shows a schematic representation of key stages in the maturation of optic-cup-like. Copyright Nature Publishing Group (2011).
![Figure 1. Optic-cup-like organoid formed spontaneously from the 3D culture of mouse embryonic stem cell aggregates in the presence of matrigel. Reprinted from reference [Citation15] with permission. (a-l) show the temporal progression of the optic-cup-like structure formation along with the expression of key molecular markers for specific stages in the process. (m) shows the optic cup in a mouse embryo at time E11.5. (n) shows a schematic representation of key stages in the maturation of optic-cup-like. Copyright Nature Publishing Group (2011).](/cms/asset/2947ba1d-271c-46f3-b977-0d4f1d61833e/tapx_a_1622451_f0001_oc.jpg)
A broad range of protocols have been devised to generate organoids, reflecting in part the diversity of organ-like structures that have already been produced using this approach and the variety of cell sources, differentiation stages and relevant co-cultures that can be selected to initiate the process [Citation13]. The choice of cells also impacts the need for supplementation with exogenous factors to direct initial stem cell fate decisions. To ensure an adequate microenvironment for organoid formation, the cell masses are often encapsulated within hydrogels. Natural extracellular matrix such as Matrigel, a complex mixture of ECM molecules produced by Engelbreth-Holm-Swarm mouse sarcoma, has been broadly used for this purpose [Citation18].
While organoids exhibit organ-like structures and functionalities, they are not exact miniature recreations of the organs that they model. For example, organoids do not incorporate critical components of in vivo organ system such as vascular networks, nor are they exposed to native physical conditioning (e.g., mechanical stresses and electrical stimulation). As such, caution must be used in extrapolating information collected with this approach in vitro to in vivo processes. Lack of reproducibility, which has been identified as differences in size, shape, cellular composition and 3D architecture, between organoids produced in a same experiment has also limited the applicability [Citation19]. Decreasing organoid-to-organoid variability is particularly important for the ability to identify statistically significant effects in drug screening experiments. A number of strategies have been proposed to address these issues. These range from the development of tailored bioreactors, to the replacement of Matrigel and other ECM hydrogels with synthetic hydrogel platforms that permit increased control over the presentation of spatiotemporal biochemical and biophysical cues for the 3D cell masses [Citation13,Citation19].
While the term spheroid has often been used interchangeably with organoid, it implies a number of important distinctions. Spheroids refer to the culture of tumor cells under non-adherent conditions that have included low-adhesion plates, hanging drop culture systems and suspension cultures in convective mixing bioreactors [Citation20]. Spheroid cultures develop heterogenous structures that are reminiscent of in vivo tumors in response to biomolecular gradients across the depth of the cell masses [Citation21]. This approach has thus been broadly used as in vitro investigative tool to gain insight into tumor biology and for drug screening studies.
The potential of dissociated somatic cells to re-aggregate into tissues with anisotropic architectures resembling native organization is also well established [Citation22]. This self-organization capacity of somatic cells can also be exploited for improved in vitro culture models. For example, chondrocytes cultured at high densities form 3D cartilage tissue [Citation23], where the use of a subpopulation of these cells found in the deeper aspect of cartilage allows the formation of tissues that can be induced to form stratified cartilage that incorporates a zone of calcified cartilage, thereby recreating the cartilage-subchondral bone interface [Citation24,Citation25]. These tissue models have proved useful to investigate the response of articular cartilage to bioactive molecules [Citation26], study the cellular responses to physiological mechanical signals, which cannot be replicated with traditional 2D in vitro culture systems and for therapeutic applications [Citation27,Citation28].
2.2. Microtissues
Microengineered tissues, also termed microtissues, represent a new paradigm in the field of cell-based assays. They combine microfabrication and tissue-engineering, to provide in vitro models with tissue-like characteristics such as three-dimensional (3D) architecture, multicellularity, cell-matrix interactions, and close-to-in vivo functionality. As minimal units representing the physiological behavior of tissues, microtissues are usually cultured on conventional well plates or trans-wells relying on nutrient passive diffusion to support cell growth. As a result, they can be used in applications requiring high-throughput analysis such as drug development or toxicological assays.
Microtissues have been typically produced by adapting microfabrication technologies used in microelectronics to create miniaturized engineered constructs with precisely defined geometries. The main challenge has been, and still is, to successfully apply these engineering technologies, conventionally used in hard materials, to soft materials and cells [Citation29]. Microfabrication techniques such as replica molding, direct printing or photopatterning are used to precisely engineer hydrogels having tunable cell response, mechanical properties and microarchitecture [Citation30]. Hydrogels are the preferred choice as engineered extracellular matrices, as they possess high-water content, mechanical properties similar to the soft native ECM and allow diffusion-driven solute transport [Citation31,Citation32]. The benefits in providing more physiologically-resembling, and thus predictive data of cell behavior are vastly reported and are related to the employment of microenvironments mimicking in vivo conditions. As such, microtissues represent an enormous improvement of current reductionist cell culture monolayers, and open new research avenues by providing more reliable tools for basic research, disease modeling, and drug testing.
Currently, microtissues are successfully applied to predict drug-induced liver and cardiac toxicity, which is among the main causes of drug attrition and market withdrawal [Citation33]. While animal testing has shown severe predictive limitations, in vitro testing has traditionally been hampered by the poor survival of both primary hepatocytes and cardiomyocytes as 2D monolayers. In this context, culturing cells in 3D microenvironments have proven to be beneficial to preserve the phenotype of primary cells for longer time periods and to help differentiation and maturation of cells derived from stem cells. For instance, primary hepatocytes cultured on top of micropatterned collagen islands and surrounded by fibroblasts, in a configuration known as micropatterned co-cultures (MPCC) have high viability and functionality, and have been used in drug development applications, and drug-induced liver injury predictions ()) [Citation34]. The technique can also be used with hepatocytes derived from induced-pluripotent stem cells, which show improved maturity markers [Citation35,Citation36]. In addition to liver, cardiac microtissues also constitute a prime example of the benefits of 3D cell culture in microenvironments that recapitulate the structural and electromechanical characteristics of the native myocardium [Citation37–Citation39]. Microengineered human cardiac tissues, usually fabricated using cell-laden natural-based hydrogels casted on posts [Citation40–Citation43], or around a wire template [Citation44,Citation45] are used in preclinical toxicology and drug screening assays () [Citation46,Citation47]. Together with liver and heart, skin is also a major target of pharmaceutical research and, due to ethical-related issues restricting animal experimentation, of cosmetic research [Citation48]. As a common approach in the field, human dermal fibroblasts are first mixed with collagen type I until contraction is observed. Then, keratinocytes are added and let proliferate. In a final step, the engineered tissue is cultured in air-liquid interface conditions to promote tissue maturation ()) [Citation49]. While the use of liver and heart microtissues in routine cell-based assays is limited, several human epidermis tissue models have been approved by the Organization for Economic Cooperation and Development (OECD) and validated by the European Center for the Validation of Alternatives to animal testing (ECVAM) for regulatory safety purposes [Citation50]. Validated models to measure skin corrosion are EpiDermTM (MatTek Corporation), EpiSkinTM (Episkin S.A.), SkinEthicTM RHE (Episkin S.A.) and epiCS® (CellSystems) models [OECD, July 2016. Test No. 431: In vitro skin corrosion: reconstructed human epidermis (RHE) test method. OECD Publishing]. Regarding skin irritation, the following models are validated: EpidermTM SIT, EpiSkinTM, SkinEthicTM RHE and LabCyte EPI-MODEL (Japan Tissue Engineering Co) [OECD, July 2015. Test No. 431: In vitro skin irritation: reconstructed human epidermis (RHE) test method. OECD Publishing].
Figure 2. (a) Micropatterned co-cultures (MPCC) with fibroblasts are employed to enhance the maturity of human hepatocytes derived from iPSCs. Reprinted from reference [Citation36] with permission. (b) Cardiac microtissues casted on silicone posts: fabrication process and generation of large microtissue arrays. Cross-sectional view of a single microtissue (scale bars: 800 μm (array), 100 μm (cross section). Reprinted from reference [Citation41] with permission. (c) Biowire fabrication set-up: a suspension of cardiomyocytes in collagen type I gel is seeded in a PDMS channel around a suture wire. The wires can be easily incorporate in an electrostimulation chamber. Images of the biowire formed at low magnification and after Hematoxylin and Eosin (H&E) staining. Reprinted from reference [Citation44] with permission. (d) Schematic representation of skin reconstruction in vitro. Histological sections of normal human skin and reconstructed skin a day 7 of air exposed culture conditions. Reprinted from reference [Citation49] with permission.
![Figure 2. (a) Micropatterned co-cultures (MPCC) with fibroblasts are employed to enhance the maturity of human hepatocytes derived from iPSCs. Reprinted from reference [Citation36] with permission. (b) Cardiac microtissues casted on silicone posts: fabrication process and generation of large microtissue arrays. Cross-sectional view of a single microtissue (scale bars: 800 μm (array), 100 μm (cross section). Reprinted from reference [Citation41] with permission. (c) Biowire fabrication set-up: a suspension of cardiomyocytes in collagen type I gel is seeded in a PDMS channel around a suture wire. The wires can be easily incorporate in an electrostimulation chamber. Images of the biowire formed at low magnification and after Hematoxylin and Eosin (H&E) staining. Reprinted from reference [Citation44] with permission. (d) Schematic representation of skin reconstruction in vitro. Histological sections of normal human skin and reconstructed skin a day 7 of air exposed culture conditions. Reprinted from reference [Citation49] with permission.](/cms/asset/a22d4a5f-a934-4c2b-a40a-d792438c24ff/tapx_a_1622451_f0002_oc.jpg)
Engineered microtissues also find relevant applications in modeling human diseases. As an example, fibrosis, which is characterized by the progressive stiffening of tissues limiting organ functionality and even producing its failure, lacks proper in vitro models that recapitulate the changes in the mechanical properties of the affected tissues [Citation51]. This is a major drawback in the development of new therapies. Recently, arrays of lung microtissues suspended over multiple flexible micropillars that recapitulate the mechanical stiffening and contraction of alveolar tissue has been reported ()). The predictive capabilities of the model have been addressed by analyzing the antifibrosis efficacy of two Food and Drug Administration (FDA) approved drugs [Citation52]. Also, lately, engineered cardiac tissues fabricated on filamentous polymer matrices using two-photon polymerization have been used to reproduce the deficient contraction produced by cells deficient in the expression of sarcomere protein cardiac myosin-binding protein C (MYBPC3) ()) [Citation53]. By employing human induced pluripotent stem cells (iPSCs) bearing MYBPC3 mutation, this model aims to help in investigating the molecular mechanisms linking genetic alterations to the cardiomyopathy pathogenesis. Along the same line, human iPSC cells have also been successfully used to model skeletal muscle dystrophies such as Duchenne dystrophy [Citation54]. Muscle microtissues faithfully reproducing skeletal muscle laminopathies are produced by differentiating cells within hydrogel matrices under tension to provide myofiber alignment. Complex multicellular microtissues including skeletal muscle, vascular endothelial cells, pericytes, and motor neurons are also proposed. Finally, microtissues of epithelial barriers are believed to be key in the study of host–pathogen interactions and the global fight against antibacterial resistance. By using replica molding, bioengineered intestinal tissues were produced on 3D porous silk scaffolds. These models mimicked the oxygen gradients existing in vivo in the gut lumen and allowed for the selective survival of bacteria in aerobic, microaerobic and anaerobic conditions [Citation55]. In a follow-up study, this model was used to study the effects of long-term intestinal infection of Cryptosporidium parvum parasite [Citation56]. Three-dimensional microtissues of lung mucosa bearing epithelial and stromal cellular components (fibroblasts) were produced on collagen gels and employed to investigate the role of Staphylococcus aureus exotoxins in tissue pathology associated with pneumonia ()) [Citation57,Citation58].
Figure 3. (a) Recapitulation of tissue fibrogenesis in lung microtissues. TGF-β1 treatment induced strong expressions fibrosis biomarkers (α-SMA stress fibers, cytosolic pro-collagen, and EDA-Fibronectin (Fn)), while SEM images of a time-lapse microscopy showed elevated contraction of the fibrotic tissue (scale bar: 200 µm). Reprinted from reference [Citation52] with permission (http://creativecommons.org/licenses/by/4.0/) (b) Cardiac microtissues assembled on fiber matrices from healthy and MYBPC3 deficient cells (scale bar: 50 µm). Confocal images showed no structural disarray but calcium dynamics showed clear abnormalities. Reprinted from reference [Citation53] with permission. (c) Lung tissue models to evaluate the severity of the damaged produced by several strains of Staphylococcus aureus found in patients with pneumonia. Reprinted from reference [Citation58] with permission (http://creativecommons.org/licenses/by/4.0/).
![Figure 3. (a) Recapitulation of tissue fibrogenesis in lung microtissues. TGF-β1 treatment induced strong expressions fibrosis biomarkers (α-SMA stress fibers, cytosolic pro-collagen, and EDA-Fibronectin (Fn)), while SEM images of a time-lapse microscopy showed elevated contraction of the fibrotic tissue (scale bar: 200 µm). Reprinted from reference [Citation52] with permission (http://creativecommons.org/licenses/by/4.0/) (b) Cardiac microtissues assembled on fiber matrices from healthy and MYBPC3 deficient cells (scale bar: 50 µm). Confocal images showed no structural disarray but calcium dynamics showed clear abnormalities. Reprinted from reference [Citation53] with permission. (c) Lung tissue models to evaluate the severity of the damaged produced by several strains of Staphylococcus aureus found in patients with pneumonia. Reprinted from reference [Citation58] with permission (http://creativecommons.org/licenses/by/4.0/).](/cms/asset/db995b03-7f59-4545-8963-526e707957f8/tapx_a_1622451_f0003_oc.jpg)
These examples aim at illustrating the relevance of microtissues in disease modeling and drug development processes. However, despite their proven improved predictive capabilities, microtissues are not used in routine pre-clinical assays. The access to representative cell sources, standardization issues and lack of high-throughput capabilities are still challenging. While access to primary cells is limited and often expensive, cells derived from pluripotent stem cells are regarded as a promising alternative, especially as the differentiation process seems to be favored when cultured in 3D environments. Regarding standardization, there is still an open debate on the level of complexity required to obtain physiological representative data without compromising the reproducibility and manageability of the models. On the other hand, the reading output of a lot of the assays performed with microtissues relies on microscopy imaging. This prevents high throughput, intense labor and expensive microscopy set-ups for automation. In this sense, the use of biosensors (reviewed in section 2.6) might be key to help increasing the microtissue applications.
2.3. Tissue and organ 3D bioprinting
The promise of an eventual unlimited supply of functional engineered organs to ease the pressure on the transplant waiting lists has recently propelled 3D bioprinting into the public imagination. Three-dimensional bioprinting refers to a collection of technologies that rely on layer-by-layer assembly principles to precisely pattern mixtures of cells and biomolecules, often in combination with materials (termed bioinks) to create living anisotropic 3D structures reminiscent of our tissues and organs. These tools draw on 2D spatial data rendered by computer-aided design (CAD) software from an engineered tissue design to inform the spatial deposition of different bioinks within each layer of the structure. Despite growing research efforts towards the development of these techniques for regenerative medicine, they have primarily been used to generate complex 3D microenvironments for in vitro experimentation. Indeed, these methods afford a level of spatial reproducibility that is essential to the generation of reliable and meaningful in vitro data, whether it pertains to gaining insight into physiological processes, understanding pathophysiological responses, or evaluating tissue responses to drugs. This feature combined with the ability to construct relatively large engineered tissues offer a unique opportunity for in vitro preclinical studies that is not available with the other technologies and methodologies discussed in this review.
While methods of bioprinting share similarities with those of conventional additive manufacturing (AM) techniques used in rapid prototyping, they also have fundamental differences, made necessary by the incorporation of cells and biomolecules [Citation59]. Indeed, the need to ensure that cell viability is maintained during the process and that biomolecule denaturation is avoided imposes important constraints on printer design. For example, shear force generated during bioink delivery through capillaries can cause cell damage, while bioinks must avoid the use of cytotoxic compounds such that suitable biomaterials for 3D bioprinting remain limited. The most commonly used bioprinter technologies are based on continuous extrusion of a bioink filament through a nozzle [Citation60,Citation61], or the delivery of discrete bioink droplets from an inkjet printer head onto a collector [Citation62,Citation63]. Laser-assisted bioprinting, which relies on the application of laser pulse onto the top face of a metallic ribbon to propel a bioink droplet from the layer bound to the opposite face of the ribbon onto a collector [Citation64], and another technique that uses light to cross-link the bioinks have also been employed [Citation65]. These nozzle-free techniques help address complications with orifice clogging of the first two techniques. Each of these approaches offer advantages and limitations, notably pertaining to spatial resolution, printing speed and cell viability, such that the choice of bioprinting device should be made with the intended application and the associated importance of each of these factors in mind [Citation59].
Bioprinting has already been used to build a broad range of different 3D tissue models that incorporate aspects of the native spatial anisotropy. For example, a stratified pigmented skin model was developed that includes the dermal and epidermal layers, the latter of which is produced by the careful placement of keratinocytes and melanocytes [Citation66]. This in vitro tissue model matured into a construct that more closely resembles native tissue structures than those produced by the traditional manual casting of the different cell types. Another study saw Ma et al. develop an in vitro liver model that recapitulates the spatial organization of hepatic progenitor cells (HPC) and support cells into hexagonal lobules that exhibit improved in vitro functionality compared to 2D cultures and 3D constructs consisting of a single cell type, HPC [Citation67].
The unique ability to precisely pattern cells and biomolecules in 3D structures has also provided an opportunity to tackle a paramount challenge in regenerative medicine and with in vitro cultures, the incorporation of functional vascular networks within tissue constructs. With few exceptions, cells typically exist in the body within 100–200 μm of blood vessels, beyond which nutrient and metabolite diffusion constraints can cause cell necrosis [Citation68]. Most approaches to produce 3D tissues models for in vitro studies or in vivo implantation do not provide a direct route to the incorporation of such vascular networks. This has limited the size of 3D engineered tissues that can be studied for long periods in vitro. Perfusion and convective flow bioreactors have been used to help address this limitation, but these systems expose engineered tissues to non-physiological mechanical environments due to the stresses applied to cells from fluid flow [Citation69]. Similarly, engineered tissues intended for transplantation have often relied on the design of scaffolds with sufficiently large pores and interconnected porosity to accommodate new vascularization in vivo. This approach, even when complemented with the controlled release of proangiogenic factors, remains a slow process measured on the scale of days to weeks and can lead to substantial loss of viable resident cells [Citation70]. Bioprinting has become an essential tool in the development of strategies to integrate functional vascular networks within engineered tissues. For example, a number of groups have used coaxial extrusion processes to produce tubular structures that can serve as vascular networks ()) [Citation71,Citation72]. In this design, endothelial cells have been incorporated with the bioink used to form the tubular structure of vessels [Citation72]. While this direct extrusion-based approach enables the formation of conduits with appropriate lengths for clinically relevant constructs, it is also not easily amenable to the fabrication of branched networks [Citation73]. An alternative approach that does support the incorporation of bifurcation relies on the deposition of sacrificial ink characterized by reversible physical crosslinks (e.g., alginate, agarose, gelatin) within the 3D structure during the printing process ()) [Citation74,Citation75]. The temporary or fugitive ink patterns are subsequently liquefied and removed to reveal a network of channels that can be endothelialized and perfused with culture media, or sutured to blood vessels upon implantation. This strategy has been associated with limited long-term mechanical integrity of the channels, highlighting the need for the careful design of the bioinks to avoid rapid degradation. Similarly, efforts to reconstruct the supporting structures of blood vessels may prove beneficial [Citation73]. The resolution of current bioprinting technologies also remains too low to support the fabrication of multiscale vasculature down to sub-micron capillaries [Citation76]. To address this issue, specifically developed bioinks that deliver proangiogenic factors and/or endothelial progenitors have been patterned to promote the formation of capillary networks over time.
Figure 4. (a) Schematic of the process to produce cell-laden hydrogels with perfusable vascular networks using sacrificial glass fibers. (b) Cross-section of the construct showing vascular network lined with endothelial cells, vessel sprouts and intervessel junctions. Reprinted from reference [Citation75] with permission. Copyright Nature Publishing Group (2012).
![Figure 4. (a) Schematic of the process to produce cell-laden hydrogels with perfusable vascular networks using sacrificial glass fibers. (b) Cross-section of the construct showing vascular network lined with endothelial cells, vessel sprouts and intervessel junctions. Reprinted from reference [Citation75] with permission. Copyright Nature Publishing Group (2012).](/cms/asset/1d421f10-27ed-4580-b13e-8648746bf5c3/tapx_a_1622451_f0004_oc.jpg)
Despite the portrayal of 3D bioprinting in media coverage as a mature technology, a number of technological challenges need to be resolved before it can be used to supply functional engineered organs for clinical applications. Indeed, current printing technologies and bioink platforms fall short of enabling the recreation the structural, mechanical and biochemical complexity of tissues and organs at multiple length scales. While advances have been achieved in the presentation of temporal control mechanisms within bioprinted tissues and hydrogel systems in general, this critical component in the regulation of cellular behavior has yet to match the level of complexity observed in native tissues [Citation77]. The ability of cells to self-organize into tissue-like structures in vitro may help bridge the gap between engineered and native structures; however, acceleration of the tissue maturation process will benefit from improved bioprinter hardware and increasingly modular bioinks that mimic more closely the native cell microenvironment. The current deposition speed of 3D bioprinters also remains insufficient for the fabrication of many human-scale tissues because the time required to print these structures and harsh conditions during the bioprinting process can cause substantial cell death [Citation59]. Further, while some tissue defects are amenable to in vivo tissue maturation upon implantation, the ultimate and ambitious goal of producing full-scale functional engineered organs will require simultaneous innovations in bioreactor design. Such devices are essential to create a hospitable in vitro environment for the maturing tissues construct that includes the delivery of nutrients and other biochemical cues, the removal of metabolites and waste products and the simultaneous administration appropriate biochemical and biophysical cues, while accounting for mass transfer resistances across large engineered tissues. Nevertheless, bioprinting has already proved to be a powerful tool to support in vitro studies in disease modeling as well as drug screening [Citation78]. Bioprinting is still considered an emerging technology, especially in comparison to the broader AM field; however, it has demonstrated rapid growth in recent years. A report has predicted that the bioprinter market will reach $1.8 billion by 2027 and that it could eventually reach the tens of billions of dollars [Citation79]. Expectedly, a number of companies have proposed new products with a broad range of capabilities and price points ranging from $5,000 to $250,000, making this technology affordable for most academic labs [Citation80].
2.4. Organs-on-a-chip
The fundamental design philosophy behind the organs-on-a-chip (OOC) technology is the reduction of whole human organs and/or organ systems to minimal functional units capable of maintaining key aspects of the native tissue architecture and of the in vivo physiology. In brief, OOC platforms consist of microchannels lined by multiple cell types spatially assembled in ways to replicate organ-specific interfaces (e.g., the fetal-maternal interface in the placenta [Citation81], )). The resulting microengineered systems through a system of pumps, valves and filters, allow to precisely control the perfusion of microliter amounts of fluids through the microchannel network in a regime of laminar flow (i.e., microfluidics). Together, these features ultimately permit to mimic specific aspects of the whole-organ response, replicate the in vivo connections between different organs, investigate pharmacokinetic mechanisms and drug toxicity, among others [Citation82].
Figure 5. (a) Placenta-on-a-chip, consisting of two microchannels separated by a semipermeable membrane sandwiched between a trophoblast and an endothelial cell monolayer, mimicking the maternal-fetal interface. (b) Three-dimensional rendering (top) and cross-sectional view (bottom) of the bioengineered placental barrier consisting of trophoblast cells cultured on the apical side of the membrane and villous endothelial cells adhering on the basal side of the membrane. Scale bar: 30 μm. Reprinted from reference [Citation81] with permission. Copyright Royal Society of Chemistry (2017). (c) Schematic of a lung-on-a-chip, consisting of an epithelial and endothelial cell monolayer separated by a porous membrane to recapitulate the alveolar-capillary barrier of human lungs. In order to include biomechanical cues, a vacuum was applied to mimic the stretching of the tissue during breathing. The lung-on-a-chip permitted to reconstitute organ-level functions such as (d) the immune response to bacteria and (e) pulmonary edema. Reprinted from reference [Citation89] with permission. Copyright Nature Publishing Group (2015).
![Figure 5. (a) Placenta-on-a-chip, consisting of two microchannels separated by a semipermeable membrane sandwiched between a trophoblast and an endothelial cell monolayer, mimicking the maternal-fetal interface. (b) Three-dimensional rendering (top) and cross-sectional view (bottom) of the bioengineered placental barrier consisting of trophoblast cells cultured on the apical side of the membrane and villous endothelial cells adhering on the basal side of the membrane. Scale bar: 30 μm. Reprinted from reference [Citation81] with permission. Copyright Royal Society of Chemistry (2017). (c) Schematic of a lung-on-a-chip, consisting of an epithelial and endothelial cell monolayer separated by a porous membrane to recapitulate the alveolar-capillary barrier of human lungs. In order to include biomechanical cues, a vacuum was applied to mimic the stretching of the tissue during breathing. The lung-on-a-chip permitted to reconstitute organ-level functions such as (d) the immune response to bacteria and (e) pulmonary edema. Reprinted from reference [Citation89] with permission. Copyright Nature Publishing Group (2015).](/cms/asset/223e7a1c-b850-4505-80f7-da2972e25d99/tapx_a_1622451_f0005_oc.jpg)
A variety of methods, ranging from etching techniques to laser photoablation, have been used to fabricate microfluidic systems [Citation83,Citation84]. Among these, the most common approach for microfabricating the channels within a solid chip relies on a combination of soft lithography and replicas, with polydimethylsiloxane (PDMS) as the material of choice because of its intrinsic advantages (i.e., low cost, ability to be poured and cross-linked into intricate features, transparency to allow microscopy observation) [Citation83,Citation84]. To achieve the sought-after physiological relevance, the resulting microfluidic platforms are successively bioengineered in ways to integrate specific features that characterize living tissues and organs, such as the presence of an ECM-like microenvironment, temporal gradients of soluble factors (e.g., cytokines, growth factors, hormones) and the presence of biophysical forces. In this context, mechanical actuators that can generate different stress states (e.g., shear, compressive, tensile) to replicate the mechanobiology of living tissues have been integrated in microfluidic devices [Citation85]. This aspect was particularly important in the development of an accurate mechanobiological environment for epithelial cells in the lung-on-a-chip device [Citation86], since during normal breathing movements, lungs undergo dynamic deformation ranging from 4% to 12% stretch distension of the basement membrane ()) [Citation87].
Aside from these distinctive characteristics, the OOC technology has made additional steps forward towards the biological fidelity required to mimic their organ-level counterparts, while maintaining the ease of traditional 2D cell cultures [Citation88]. In particular, the direct use of human cells not only promises to address the translatability challenges and ethical issues encountered with animal models [Citation89], but is also expected to accelerate the development of personalized platforms for precision medicine and advanced drug screening [Citation85], in parallel with progresses in iPSC biology [Citation90]: mature cells could be in fact harvested from individual patients, reprogrammed and finally used in OOC platforms to build personalized functional models for disease mechanisms and drug screening purposes [Citation91]. Other advantages of OOCs include [Citation89]: (i) the ease of direct real-time observation of cellular processes of interest with conventional optical microscopes; (ii) the ability of controlling environmental factors (e.g., temperature and gas concentration), precisely delivering soluble factors (e.g., nutrients, drugs, cytokines, hormones), collecting metabolites, waste and other secretory factors; (iii) the reduced cost associated with the smaller volumes of reagents required; (iv) reproducibility, integration with other technologies (e.g., sensors for electrical, optical and biochemical readouts) [Citation83] and possibility to link multiple OOCs together to investigate interactions among different organs and recreate either normal or pathological whole human physiology (i.e., body-on-a-chip) [Citation92].
To date, all major organs have been reconstituted in OOC platforms: liver, skin, lung, and placenta are just few examples of the panoply of current applications of this technology. Regardless of the specific tissue type, OOCs have been mainly employed for two principal purposes [Citation93]: (i) Disease modeling: a panoply of pathological states has been investigated with OOCs. For example, cancer and immune system related conditions have been replicated to close in on disease progression (e.g. cancer metastatic growth and intravasation) [Citation94]. In this context, a large body of work has focused on the importance of the integration of immune factors [Citation8,Citation12]. To this end, by capitalizing on the key advantages of microfluidic devices (i.e., bioengineered 3D architecture of the cell microenvironment, dynamic exchange of oxygen and nutrients, time-lapse imaging) with respect to other in vitro methods, aspects such as immune cells-tumors interactions and inflammation events could be replicated [Citation8,Citation12]. Of note, OOC systems, through the precise control of the dynamic flow, also offer the distinctive advantage of dynamically mimicking endocrine signaling and replicate hormonal variations during the menstrual cycle and pregnancy, thereby promising to become a powerful tool for both translational and fundamental research in women’s health toward novel insights into female-specific diseases and sex-dependent differences in preclinical research [Citation95]. The microfluidic nature also makes OOCs a powerful tool to better understand bacterial and viral infections [Citation96]. Bacteria and viruses can be in fact circulated to investigate their interactions with the biological membranes of interest. For example, E. coli bacteria introduced in the lung-on-a-chip device activated the transmigration of circulating neutrophils through the reconstructed endothelial layer, replicating the innate immune response to pulmonary bacterial infection ()) [Citation86]. Similarly, a liver-on-a-chip has been recently used to investigate hepatitis B viral (HBV) infection, demonstrating the ability to recapitulate all steps of the HBV life cycle as well as the innate immune and cytokine responses observed in HBV-infected patients [Citation97]. (ii) Advanced drug screening/discovery: bringing a new drug to market requires up to twelve years and more than 1.7 billion US dollars. Despite these efforts, it is estimated that only 1 out of 10,000 drug candidates gains FDA approval despite successful preclinical evaluation, and up to 20% of acute kidney injuries are linked to drug toxicity effects non predicted by preclinical models [Citation8,Citation93]. For these reasons, researchers have increasingly turned to OOCs as a potential technological alternative for faster, cheaper and more predictive preclinical screening and toxicology assessment. To date, the responsiveness and toxicity to specific drugs have been assessed with different OOC platforms (e.g., liver-, lymph node-, bone marrow-, gut- and kidney-on-a-chip, among others) [Citation8,Citation93]. In this context, of particular interest because of recent advances in drug-delivery technologies for better pharmacological efficacy and bioavailability, is the employment of OOCs to evaluate the response to nanoparticle-based therapeutics (i.e., nanotoxicology). The microfluidic technology offers in fact biologically relevant platforms which only require a fraction of samples compared to conventional in vitro systems, while permitting real-time evaluation of nanoparticle transport and cellular uptake [Citation98].
The potential of OOCs for applications in human health has been highlighted by the 2016 World Economic Forum which ranked them 6th among the top 10 emerging technologies [Citation85]. Such endorsement has been echoed by funding agencies (e.g., National Institute of Health in the USA, the European Framework Program 7 and the Japan Agency for Medical Research and Development) which invested significant resources towards the development of more robust and replicable OOC platforms for commercialization [Citation3,Citation87]. In parallel, large pharmaceutical and biotechnology companies (e.g., Pfizer, Merck, Johnson&Johnson) have intensified their involvement in collaborations with academia and companies (e.g., Emulate) to support the translation of OOC platforms from the laboratory to industrial R&D, thereby further contributing to the commercialization of the technology [Citation83].
Despite its increasing employment for real-world devices, the OOC technology still requires improvements to address specific challenges and fully maturate its potential for preclinical research and commercial applications, such as [Citation3,Citation83,Citation93,Citation99]: (i) Scalability and fabrication techniques – in order to avoid volume-dependent alterations of cellular processes within OOC compartments, these devices should be scalable to the optimal organ size to avoid over- or under-production of metabolites. The ease of scalability also poses challenging repercussions in their commercialization process, for which the fabrication methods currently employed in the laboratory (e.g., lithography) should be translated to large-scale manufacturing by ensuring rapid and highly reproductible production at low cost. In addition, the design of OOC platforms should aim at enhancing throughput and usability, facilitating handling by the end-users; (ii) Materials – although PDMS is widely used in OCCs, better performing materials are required to address its limitations, such as unwanted deformations of the chip, gas permeability, hydrophobic drugs absorption and leaching; (iii) Cell sources – since OOC platforms’ accuracy strongly depends on the cell types used, the selection of cells is critical. In this context, immortalized cell lines are widely used, but alterations in their native functional activity should be accounted for. While primary cells provide a better alternative, availability, ethical and financial issues limit their employment; (iv) Perfusion process – the ideal perfusion system should avoid bubble formation and precisely control fluid recirculation to replicate in vivo mechanisms that affect absorption, elimination and distribution of metabolites and other soluble factors; (v) Imaging and analysis – with increasingly more complex cellular models, standard fluorescence imaging techniques drastically reduce the quantity of information that can be extracted from the OOC platform. Therefore, additional techniques (e.g., transepithelial/transendothelial electrical resistance – TEER) and sensing abilities need to be synergistically integrated in order to generate accurate real-time data on cellular phenomena (section 2.6).
2.5. Biomimetic in vitro models
While most of the microtissues, tissue constructs, and organs-on-a-chip aim to reproduce the main functions of a tissue or organ, usually they do not reproduce their morphology. The avenue of organoids (section 2.1), in which cells self-organize and spatially segregate to recreate the architecture found in the native tissue has pointed out the relevance of the shape in the proper tissue functionality. Epithelial and endothelial tissues in vivo form complex 3D structures such as cysts, tubules, evaginations or invaginations. Vasculature, nephrons, mammary glands, gastrointestinal epithelium, hair-follicles, and corneal limbus are only some examples of tissue complex geometries in our body that researchers have been tried to reproduce in vitro employing a variety of biomimetic microfabrication strategies. For example, photolithography and replica molding have been used to reproduce the wavy topography of the epidermal–dermal interface ()) [Citation100]. It is accepted that epidermal stem cells lie in clusters specifically located in relation to this topography, but the relationship between their location and properties is currently unknown and can be investigated by reproducing the tissue architecture [Citation100]. Also, in skin tissue, the fabrication of 3D structures with the shape of the hair-follicle bulges has attracted a lot of attention. Micro molding has been used to accurately create microwell arrays of self-assembling hair follicle germs able to generate spatially arrange hair follicles upon transplantation [Citation101]. In another study, 3D printed molds were used to pattern collagen gels laden with dermal fibroblasts. Dermal papilla cells were then cultured on the microwells to promote the differentiation of human keratinocytes into specific hair follicle lineages and their physiological arrangement ()) [Citation48]. Corneal limbus also has specific microstructures that serve as stem cell niches. Limbal architecture has been reproduced by electrospinning polymer fibers on micromoulds produced by stereolithography [Citation102] or by replica molding on collagen gels [Citation103]. Regarding tubular structures, very recently an array of kidney tubules produced from a micro-molded platform in collagen-matrigel gels. This platform allows for the modeling of kidney diseases such as cystic kidney disease and acute kidney injury as well as drug testing purpose [Citation104]. Finally, the small intestine crypt-villus morphology has also been reproduced by either replica molding procedures [Citation29,Citation105] and, more recently, by reaction-diffusion mediated photolithography ()) [Citation106]. In all the cases, a significant improvement of the properties of the epithelial barrier on the 3D structures compared with the 2D monolayers was reported. Still, and despite the benefits reported, in vitro models bearing biomimetic microstructures are relying on relatively tedious and complex fabrication processes. It is foreseen that the wider availability and applicability of 3D bioprinting methods will have an impact in this field, extending the applications of the biomimetic approach.
Figure 6. (a) Fabrication of patterned PDMS substrates to mimic the epidermal rete ridges. Keratinocyte patterning on collage-coated PDMS substrates (involucrin stained in yellow, β1 integrin stained in red, scale bar: 200 µm). Reprinted from reference [Citation100] with permission. (b) Hair follicles formed on microwells of collagen gels laden with dermal fibroblasts (FB). First, dermal papilla cells (DPC) were seeded within the wells, and then keratinocytes (KC). Cross sections of the construct (scale bar 2 mm) and immunostaining (scale bar 100 µm) show active DPC cells at their physiological positions (black arrows). Prolonged culture period led to hair fiber formation (arrowheads, scale bar 2 mm). Reprinted from reference [Citation48] with permission (http://creativecommons.org/licenses/by/4.0/). (c) Intestinal villi-like microstructures fabricated by dynamic photopolymerization on poly(ethylene glycol) hydrogels provide the barrier formed CaCo-2 cells with improved physiological characteristics (scale bars: 150 µm; (upper row); 200 µm (lower row, left and middle); 50 µm (lower row, right)). Reprinted from reference [Citation106] with permission.
![Figure 6. (a) Fabrication of patterned PDMS substrates to mimic the epidermal rete ridges. Keratinocyte patterning on collage-coated PDMS substrates (involucrin stained in yellow, β1 integrin stained in red, scale bar: 200 µm). Reprinted from reference [Citation100] with permission. (b) Hair follicles formed on microwells of collagen gels laden with dermal fibroblasts (FB). First, dermal papilla cells (DPC) were seeded within the wells, and then keratinocytes (KC). Cross sections of the construct (scale bar 2 mm) and immunostaining (scale bar 100 µm) show active DPC cells at their physiological positions (black arrows). Prolonged culture period led to hair fiber formation (arrowheads, scale bar 2 mm). Reprinted from reference [Citation48] with permission (http://creativecommons.org/licenses/by/4.0/). (c) Intestinal villi-like microstructures fabricated by dynamic photopolymerization on poly(ethylene glycol) hydrogels provide the barrier formed CaCo-2 cells with improved physiological characteristics (scale bars: 150 µm; (upper row); 200 µm (lower row, left and middle); 50 µm (lower row, right)). Reprinted from reference [Citation106] with permission.](/cms/asset/ede634b9-287f-4069-9a57-6086b54ec729/tapx_a_1622451_f0006_oc.jpg)
2.6. Biosensors
Most of the reading outputs obtained from bioengineered in vitro models rely on imaging data. This limits the throughput, complicates and makes more expensive the set-ups, and restricts their use to highly skilled personnel. To advance these drawbacks, an excellent approach seems to integrate biosensors in the bioengineered platforms. Biosensors are analytical devices that rely on the molecular recognition capabilities of biological capture probes (antibodies, oligonucleotides, enzymes or even cells) to measure the concentration of analytes. These recognition events will be transduced to a signal that will be read-out. Transducers might be of different nature, being the electrochemical, optical, thermal and mass-change based the most popular. Biosensors can be used to continuous monitoring the critical parameters of cell microenvironment, and to study the response of the models to drugs over extended periods of time. They can be applied to static cell culture (microtissues in well plates or Transwells) or to microfluidic platforms [Citation105]. To demonstrate the power of biosensor integration approach, Zhang et al. reported a platform for the automated, on-line monitoring of a multiorgan-on-a-chip platform that include sensors to monitor pH, oxygen and temperature, electrochemical biosensors to monitor soluble protein biomarkers and miniature microscopes for the imaging of the morphology of organoids cultured within the platform [Citation107]. In a proof-of-concept application, the platform was employed to monitor drug-induced toxicity in two dual organ model systems: human liver-and-heart-on-a-chip and liver-cancer-and-heart-on-a-chip, to prove the assessment of long-term response to chronic drugs and short-term response of acute toxicity, respectively. Monitoring soluble biomarkers such as cytokines through integrated biosensors is also used as a reading output to monitor pathological processes in a non-destructive manner. As an example, real-time monitoring of TNF-α in a model of tumor intravasation that included tumor cells, endothelial cells and macrophages revealed the dynamics of the process, including the increase in endothelial permeability and tumor-endothelial interactions [Citation108]. It is accepted that an improved knowledge about the molecular dynamics in cancer metastasis can lead to propose new therapeutic strategies.
On top of soluble biomarkers, some tissues, such as skeletal, cardiac, and smooth muscle require specific sensors to evaluate their main functional response, which is the capability of contraction. Mechanical forces generated from these bioengineered tissue models are usually measured by monitoring the bending of silicon cantilevers or micropillars [Citation109]. In addition, electrical activity can also be a functional hallmark for cardiac, muscle, and nervous tissues. Electrical signal can be recorded by microelectrode arrays (MEAs), which can be easily integrated in microphysiological systems [Citation110]. On the other hand, the functionality of tissue barriers formed skin, gastrointestinal tract, and blood brain barrier is usually monitored by determining the TEER. To that end, bioengineered models of these tissues can incorporate two measurement electrodes, one at each side of the cellular barrier [Citation111].
Overall, online and/or integrated monitoring capabilities might be key in the future acceptance of bioengineered models as new valuable tools in drug development. Challenges are associated to systems complexity and cost. If they can be overcome, they promise to increase the throughput of in vitro assays, allow personalized medicine applications and significantly increase the cellular and molecular basis of complex human pathologies.
3. Conclusion and outlook
Advanced in vitro platforms are likely to foster profound changes in the ways preclinical research is conducted. The application of novel bioengineering tools, strategies and techniques to improve health is poised to continue to grow until they will reach a mature level to be routinely integrated in conventional preclinical practices, resulting in a major impact on health research and economic benefits to society. However, as outlined in the previous sections, many challenges still remain to be addressed in order to implement these new technologies in research and clinical practises. In particular, while significant efforts are being made to incorporate organ systems in many of the technologies described in this work (e.g. adding vasculature in 3D printed constructs, creating multi-organoid co-cultures), in vitro studies remain simplified models that do not comprehensively include all relevant aspects of the dynamic multifactorial in vivo environment which characterizes living organisms, such as the immune response.
Although the technologies outlined in this review have been presented individually, researchers are currently integrating different approaches within the same platform in order to achieve synergistic effects stemming from the simultaneous combination of individual advantages and mitigation of each other’s limitations. For example, synergistic engineering strategies have been proposed to integrate organoids and organs-on-a-chip towards superior in vitro platforms that conjugate the high cellular fidelity of the former with the higher throughput phenotypic readouts of the latter [Citation112]. Similarly, organoids can be integrated into 3D printing processes to reconstruct the tissue’s microarchitecture [Citation113,Citation114]. Therefore, it can be envisaged that such integrative approaches will likely become the key to propel innovation in preclinical research towards the next generation of in vitro platforms for more accurate disease modeling, mechanistic studies, and drug discovery. Of note, more effective in vitro technologies are not only expected to find increasingly more applications in preclinical research but also in other sectors, such as consumer products industry, where the transition to these novel methods may soon become a necessity. In this context, the Australian Senate has recently passed a bill to ban animal testing for cosmetic development (Industrial Chemical Charges Bill 2017), aligning to the European Union directive that ousted it since 2013 [Citation3,Citation87]. This trend will likely expand to North America and worldwide, ultimately enhancing the breadth of in vitro solutions towards faster and more cost-effective development and commercialization for the consumer goods industry (e.g. cosmetics, household products, food and dietary supplements).
Acknowledgments
EM acknowledges funding by European Union’s Horizon 2020 ERC grant agreement No 647863 (COMIET), the CERCA Programme/Generalitat de Catalunya (2017-SGR-1079), and the Spanish Ministry of Economy and Competitiveness (TEC2017-83716-C2-1-R) and the Severo Ochoa Program for Centers of Excellence in R&D 2016-2019. The results presented here reflect only the views of the authors; the European Commission is not responsible for any use that may be made of the information it contains. JPS and FV acknowledge funding from the Natural Sciences and Engineering Research Council of Canada (NSERC) through the Discovery Grant. JPS also acknowledges financial support by the University of Ottawa Seed Funding Opportunity Grant. The authors acknowledge Alexander Steeves for his help with the graphical abstract.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Duval K, Grover H, Han L-H, et al. Modeling physiological events in 2D vs. 3D cell culture. Physiology. 2017;32:423–450.
- Kacy Cullen D, Wolf JA, Vernekar VN, et al. Neural tissue engineering and biohybridized microsystems for neurobiological investigation in vitro (part 1). Crit Rev Biomed Eng. 2011;39:201–240.
- Kimura H, Sakai Y, Fujii T. Organ/body-on-a-chip based on microfluidic technology for drug discovery. Drug Metab Pharmacokinet. 2018;33:43–48.
- Lee SH, Sung JH. Organ-on-a-chip technology for reproducing multiorgan physiology. Adv Healthcare Mater. 2018;7:1700419.
- Yamada KM, Cukierman E. Modeling tissue morphogenesis and cancer in 3D. Cell. 2007;130:601–610.
- Hoarau-Véchot J, Rafii A, Touboul C, et al. Halfway between 2D and animal models: are 3D cultures the ideal tool to study cancer-microenvironment interactions? IJMS. 2018;19:181.
- Edmondson R, Broglie JJ, Adcock AF, et al. Three-dimensional cell culture systems and their applications in drug discovery and cell-based biosensors. Assay Drug Dev Technol. 2014;12:207–218.
- Shanti A, Teo J, Stefanini C. In vitro immune organs-on-chip for drug development: a review. Pharmaceutics. 2018;10:278.
- Ericsson AC, Crim MJ, Franklin CL. A brief history of animal modeling. Mo Med. 2013;110:201–205.
- Conn PM. source book of models for biomedical research. Totowa, NJ: Humana Press; 2008.
- Seok J, Warren HS, Cuenca AG, et al. Genomic responses in mouse models poorly mimic human inflammatory diseases. Natl Acad Sci. 2013;110:3507–3512.
- Polini A, Del Mercato LL, Barra A, et al. Towards the development of human immune-system-on-a-chip platforms. Drug Discov Today. 2018;24:1–9.
- Lancaster MA, Knoblich JA. Organogenesis in a dish: modeling development and disease using organoid technologies. Science. 2014;345:1247125.
- Rossi G, Manfrin A, Lutolf MP. Progress and potential in organoid research. Nat Rev Genet. 2018;19:1–17.
- Eiraku M, Takata N, Ishibashi H, et al. Self-organizing optic-cup morphogenesis in three-dimensional culture. Nature. 2011;472:51–56.
- Sato T, Vries RG, Snippert HJ, et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature. 2009;459:262–265.
- Takahashi T. Organoids for drug discovery and personalized medicine. Ann Rev Pharmacol Toxicol. 2019;59:447–462.
- Lancaster MA, Renner M, Martin C-A, et al. Cerebral organoids model human brain development and microcephaly. Nature. 2013;501:373–379.
- Huch M, Knoblich JA, Lutolf MP, et al. The hope and the hype of organoid research. Development. 2017;144:938–941.
- Fang Y, Eglen RM. Three-dimensional cell cultures in drug discovery and Development. SLAS Discov. 2017;22:456–472.
- Unger C, Kramer N, Walzl A, et al. Modeling human carcinomas: physiologically relevant 3D models to improve anti-cancer drug development. Adv Drug Deliv Rev. 2014;79:50–67.
- Paul Weiss ACT. Reconstitution of complete organs from single-cell suspensions of chick embryos in advanced stages of differentiation. Proc Natl Acad Sci USA. 1960;46:1177–1185.
- Boyle J, Luan B, Cruz TF, et al. Characterization of proteoglycan accumulation during formation of cartilagenous tissue in vitro. Osteoarthritis Cartilage. 1995;3:117–125.
- Kandel RA, Boyle J, Gibson G, et al. In vitro formation of mineralized cartilagenous tissue by articular chondrocytes. In Vitro Cell Dev Biol Anim. 1997;33:174–181.
- St-Pierre J-P, Gan L, Wang J, et al. The incorporation of a zone of calcified cartilage improves the interfacial shear strength between in vitro-formed cartilage and the underlying substrate. Acta Biomater. 2012;8:1603–1615.
- St-Pierre J-P, Wang Q, Li SQ, et al. Inorganic polyphosphate stimulates cartilage tissue formation. Tissue Eng Part A. 2012;18:1282–1292.
- De Croos JNA, Dhaliwal SS, Grynpas MD, et al. Cyclic compressive mechanical stimulation induces sequential catabolic and anabolic gene changes in chondrocytes resulting in increased extracellular matrix accumulation. Matrix Biol. 2006;25:323–331.
- Kandel RA, Grynpas M, Pilliar R, et al. Repair of osteochondral defects with biphasic cartilage-calcium polyphosphate constructs in a sheep model. Biomaterials. 2006;27:4120–4131.
- Sung JH, Yu J, Luo D, et al. Microscale 3-D hydrogel scaffold for biomimetic gastrointestinal (GI) tract model. Lab Chip. 2011;11:389–392.
- Huang G, Wang L, Wang S, et al. Engineering three-dimensional cell mechanical microenvironment with hydrogels. Biofabrication. 2012;4:042001.
- Tibbitt MW, Anseth KS. Hydrogels as extracellular matrix mimics for 3D cell culture. Biotechnol Bioeng. 2009;103:655–663.
- DeForest CA, Anseth KS. Advances in bioactive hydrogels to probe and direct cell fate. Annu Rev Chem Biomol Eng. 2012;3:421–444.
- Brown GE, Khetani SR. Microfabrication of liver and heart tissues for drug development. Philos Trans R Soc Lond B Biol Sci. 2018;373:20170225.
- Khetani SR, Bhatia SN. Microscale culture of human liver cells for drug development. Nat Biotechnol. 2007;26:120–126.
- Ware BR, Berger DR, Khetani SR. Prediction of drug-induced liver injury in micropatterned co-cultures containing iPSC-derived human hepatocytes. Toxicol Sci. 2015;145:252–262.
- Berger DR, Ware BR, Davidson MD, et al. Enhancing the functional maturity of induced pluripotent stem cell-derived human hepatocytes by controlled presentation of cell-cell interactions in vitro. Hepatology. 2015;61:1370–1381.
- Radisic M, Park H, Shing H, Consi T, Schoen F, Langer R, Freed LE, Vunjak-Novakovic G. Functional assembly of engineered myocardium by electrical stimulation of cardiac myocytes cultured on scaffolds, Proc Natl Acad Sci USA 2004;101:18129–18134.
- Tulloch NL, Muskheli V, Razumova MV, Korte FS, Regnier M, Hauch KD, Pabon L, Reinecke H, Murry CE. Growth of engineered human myocardium with mechanical loading and vascular coculture, Circ Res 2011;109:47–59.
- Zhang D, Shadrin IY, Lam J, et al. Tissue-engineered cardiac patch for advanced functional maturation of human ESC-derived cardiomyocytes. Biomaterials. 2013;34:5813–5820.
- Turnbull IC, Karakikes I, Serrao GW, et al. Advancing functional engineered cardiac tissues toward a preclinical model of human myocardium. Faseb J. 2014;28:644–654.
- Legant WR, Pathak A, Yang MT, et al. Microfabricated tissue gauges to measure and manipulate forces from 3D microtissues. Proc Natl Acad Sci USA. 2009;106:10097–10102.
- Thavandiran N, Dubois N, Mikryukov A, et al. Design and formulation of functional pluripotent stem cell-derived cardiac microtissues. Proc Natl Acad Sci USA. 2013;110:E4698–707.
- Tiburcy M, Hudson JE, Balfanz P, et al. Defined engineered human myocardium with advanced maturation for applications in heart failure modeling and repair. Circulation. 2017;135:1832–1847.
- Nunes SS, Miklas JW, Liu J, et al. Biowire: a platform for maturation of human pluripotent stem cell-derived cardiomyocytes. Nat Methods. 2013;10:781–787.
- Xiao Y, Zhang B, Liu H, et al. Microfabricated perfusable cardiac biowire: a platform that mimics native cardiac bundle. Lab Chip. 2014;14:869–882.
- Amano Y, Nishiguchi A, Matsusaki M, et al. Development of vascularized iPSC derived 3D-cardiomyocyte tissues by filtration layer-by-layer technique and their application for pharmaceutical assays. Acta Biomater. 2016;33:110–121.
- Mathur A, Loskill P, Shao K, et al. Human iPSC-based cardiac microphysiological system for drug screening applications. Sci Rep. 2015;5:8883.
- Abaci HE, Coffman A, Doucet Y, et al. Tissue engineering of human hair follicles using a biomimetic developmental approach. Nat Commun. 2018;9:5301.
- Vioux-Chagnoleau C, Lejeune F, Sok J, et al. Reconstructed human skin: from photodamage to sunscreen photoprotection and anti-aging molecules. J Dermatological Sci Suppl. 2006;2:S1–S12.
- Zhang Z, Michniak-Kohn BB. Tissue engineered human skin equivalents. Pharmaceutics. 2012;4:26–41.
- Feng Y, Mitchison TJ, Bender A, et al. Multi-parameter phenotypic profiling: using cellular effects to characterize small-molecule compounds. Nat Rev Drug Discov. 2009;8:567–578.
- Asmani M, Velumani S, Li Y, et al. Fibrotic microtissue array to predict anti-fibrosis drug efficacy. Nat Commun. 2018;9:2066.
- Ma Z, Huebsch N, Koo S, et al. Contractile deficits in engineered cardiac microtissues as a result of MYBPC3 deficiency and mechanical overload. Nat Biomed Eng. 2018;2:955–967.
- Maffioletti SM, Sarcar S, Henderson ABH, et al. Three-dimensional human iPSC-derived artificial skeletal muscles model muscular dystrophies and enable multilineage tissue engineering. Cell Rep. 2018;23:899–908.
- Chen Y, Lin Y, Davis KM, et al. Robust bioengineered 3D functional human intestinal epithelium. Sci Rep. 2015;13708.
- DeCicco RePass MA, Chen Y, Lin Y, et al. Novel Bioengineered Three-Dimensional Human Intestinal Model for Long-Term Infection of Cryptosporidium parvum. Infect Immun. 2017;85.
- Nguyen Hoang AT, Chen P, Juarez J, et al. Dendritic cell functional properties in a three-dimensional tissue model of human lung mucosa. Am J Physiol Lung Cell Mol Physiol. 2012;302:L226–37.
- Mairpady Shambat S, Chen P, Nguyen Hoang AT, et al. Modelling staphylococcal pneumonia in a human 3D lung tissue model system delineates toxin-mediated pathology. Dis Model Mech. 2015;8:1413–1425.
- Murphy SV, Atala A. 3D bioprinting of tissues and organs. Nature Biotechnology. 2014;32:773–785.
- Pfister A, Landers R, Laib A, et al. Biofunctional rapid prototyping for tissue-engineering applications: 3D bioplotting versus 3D printing. J Polym Sci Part a-Polym Chem. 2004;42:624–638.
- Ozbolat IT, Hospodiuk M. Current advances and future perspectives in extrusion-based bioprinting. Biomaterials. 2016;76:321–343.
- Klebe RJ. Cytoscribing - a method for micropositioning cells and the construction of two-dimensional and 3-dimensional synthetic tissues. Exp Cell Res. 1988;179:362–373.
- Gudapati H, Dey M, Ozbolat I. A comprehensive review on droplet-based bioprinting: past, present and future. Biomaterials. 2016;102:20–42.
- Guillotin B, Souquet A, Catros S, et al. Laser assisted bioprinting of engineered tissue with high cell density and microscale organization. Biomaterials. 2010;31:7250–7256.
- Lu Y, Mapili G, Suhali G, et al. A digital micro-mirror device-based system for the microfabrication of complex, spatially patterned tissue engineering scaffolds. J Biomed Mater Res A. 2006;77:396–405.
- Ng WL, Qi JTZ, Yeong WY, et al. Proof-of-concept: 3D bioprinting of pigmented human skin constructs. Biofabrication. 2018;10:025005.
- Ma X, Qu X, Zhu W, et al. Deterministically patterned biomimetic human iPSC-derived hepatic model via rapid 3D bioprinting. Proc Natl Acad Sci USA. 2016;113:2206–2211.
- Carmeliet P, Jain RK. Angiogenesis in cancer and other diseases. Nature. 2000;407:249–257.
- Rouwkema J, Khademhosseini A. Vascularization and angiogenesis in tissue engineering: beyond creating static networks. Trends Biotechnol. 2016;34:733–745.
- Butt OI, Carruth R, Kutala VK, et al. Stimulation of peri-implant vascularization with bone marrow-derived progenitor cells: monitoring by in VivoEPR oximetry. Tissue Eng. 2007;13:2053–2061.
- Zhang Y, Yu Y, Chen H, et al. Characterization of printable cellular micro-fluidic channels for tissue engineering. Biofabrication. 2013;5:025004.
- Attalla R, Ling C, Selvaganapathy P. Fabrication and characterization of gels with integrated channels using 3D printing with microfluidic nozzle for tissue engineering applications. Biomed Microdevices. 2016;18:1241.
- Datta P, Ayan B, Ozbolat IT. Bioprinting for vascular and vascularized tissue biofabrication. Acta Biomater. 2017;51:1–20.
- Kolesky DB, Homan KA, Skylar-Scott MA, et al. Three-dimensional bioprinting of thick vascularized tissues. Proc Natl Acad Sci USA. 2016;113:3179–3184.
- Miller JS, Stevens KR, Yang MT, et al. Rapid casting of patterned vascular networks for perfusable engineered three-dimensional tissues. Nat Mater. 2012;11:768–74.
- Miri AK, Khalilpour A, Cecen B, et al. Multiscale bioprinting of vascularized models. Biomaterials. 2019;198:204–216.
- Parak A, Pradeep P, Du Toit LC, et al. Functionalizing bioinks for 3D bioprinting applications. Drug Discov Today. 2019;24:198–205.
- Ma X, Liu J, Zhu W, et al. 3D bioprinting of functional tissue models for personalized drug screening and in vitro disease modeling. Adv Drug Deliv Rev. 2018;132:235–251.
- Combellack E, Jessop ZM, Whitaker IS. The commercial 3D bioprinting industry. New York: Elsevier Ltd; 2018.
- Datta P, Barui A, Wu Y, et al. Essential steps in bioprinting from pre- to post-bioprinting. Biotechnol Adv. 2018;36:1481–1504.
- Blundell C, Tess ER, Schanzer ASR, et al. A microphysiological model of the human placental barrier. Lab Chip. 2016;16:3065–3073.
- Jackson EL, Lu H. Three-dimensional models for studying development and disease: moving on from organisms to organs-on-a-chip and organoids. Integr Biol. 2016;8:672–683.
- Ahadian S, Civitarese R, Bannerman D, et al. Organ-on-a-chip platforms: a convergence of advanced materials, cells, and microscale technologies. Adv Healthcare Mater. 2017;7:1700506–1700553.
- Mittal R, Woo FW, Castro CS, et al. Organ-on-chip models: implications in drug discovery and clinical applications. J Cell Physiol. 2018;105:e48–29.
- Rothbauer M, Rosser JM, Zirath H, et al. ScienceDirect tomorrow today: organ-on-a-chip advances towards clinically relevant pharmaceutical and medical in vitro models. Curr Opin Biotechnol. 2018;55:81–86.
- Huh D, Matthews BD, Mammoto A, et al. Reconstituting organ-level lung functions on a chip. Science. 2010;328:1658–1662.
- Nawroth JC, Barrile R, Conegliano D, et al. Stem cell-based lung-on-chips: the best of both worlds? Adv Drug Deliv Rev. 2018;1–21.
- Ronaldson-Bouchard K, Vunjak-Novakovic G. Organs-on-a-chip: a fast track for Engineered human tissues in drug development. Stem Cell. 2018;22:310–324.
- Esch EW, Bahinski A, Huh D. Organs-on-chips at the frontiers of drug discovery. Nat Rev Drug Discov. 2015;14:248–260.
- Shi Y, Inoue H, Wu JC, et al. Induced pluripotent stem cell technology: a decade of progress. Nat Publishing Group. 2016;16:115–130.
- van Den Berg A, Mummery CL, Passier R, et al. Personalised organs-on-chips: functional testing for precision medicine. Lab Chip. 2019;19:198–205.
- Sosa-Hernández JE, Villalba-Rodríguez AM, Romero-Castillo KD, et al. Organs-on-a-chip module: a review from the development and applications perspective. Micromachines. 2018;9:536.
- Zhang B, Korolj A, Lai BFL, et al. Advances in organ-on-a-chip engineering. Nat Rev Mater. 2018;3:1–22.
- Sun W, Luo Z, Lee J, et al. Organ-on-a-chip for cancer and immune organs modeling. Adv Healthcare Mater. 2019;177:1801363.
- Nawroth J, Rogal J, Weiss M, et al. Organ-on-a-chip systems for women’s health applications. Adv Healthcare Mater. 2017;7:1700550.
- Low LA, Tagle DA. Tissue chips – innovative tools for drug development and disease modeling. Lab Chip. 2017;17:3026–3036.
- Ortega-Prieto AM, Skelton JK, Wai SN, et al. 3D microfluidic liver cultures as a physiological preclinical tool for hepatitis B virus infection. Nat Commun. 2018;9:1–15.
- Ahn J, Ko J, Lee S, et al. Microfluidics in nanoparticle drug delivery; From synthesis to pre-clinical screening. Adv Drug Deliv Rev. 2018;128:29–53.
- Aziz A, Geng C, Fu M, et al. The role of microfluidics for organ on chip simulations. Bioengineering. 2017;4:39.
- Viswanathan P, Guvendiren M, Chua W, et al. Mimicking the topography of the epidermal-dermal interface with elastomer substrates. Integr Biol. 2016;8:21–29.
- Kageyama T, Yoshimura C, Myasnikova D, et al. Spontaneous hair follicle germ (HFG) formation in vitro, enabling the large-scale production of HFGs for regenerative medicine. Biomaterials. 2018;154:291–300.
- Ortega I, Ryan AJ, Deshpande P, et al. Combined microfabrication and electrospinning to produce 3-D architectures for corneal repair. Acta Biomater. 2013;9:5511–5520.
- Levis HJ, Massie I, Dziasko MA, et al. Rapid tissue engineering of biomimetic human corneal limbal crypts with 3D niche architecture. Biomaterials. 2013;34:8860–8868.
- Subramanian B, Kaya O, Pollak MR, et al. Guided tissue organization and disease modeling in a kidney tubule array. Biomaterials. 2018;183:295–305.
- Wang YI, Carmona C, Hickman JJ, et al. Multiorgan microphysiological systems for drug development: strategies, advances, and challenges. Adv Healthcare Mater. 2018;7:1701000.
- Castaño AG, García-Díaz M, Torras N, et al. Dynamic photopolymerization produces complex microstructures on hydrogels in a moldless approach to generate a 3D intestinal tissue model. Biofabrication. 2019;11:1–16.
- Zhang YS, Aleman J, Shin SR, et al. Multisensor-integrated organs-on-chips platform for automated and continual in situ monitoring of organoid behaviors. Proc Natl Acad Sci USA. 2017;114:E2293–E2302.
- Zervantonakis IK, Hughes-Alford SK, Charest JL, et al. Three-dimensional microfluidic model for tumor cell intravasation and endothelial barrier function. Proc Natl Acad Sci USA. 2012;109:13515–13520.
- Das M, Wilson K, Molnar P, et al. Differentiation of skeletal muscle and integration of myotubes with silicon microstructures using serum-free medium and a synthetic silane substrate. Nat Protoc. 2007;2:1795–1801.
- Varghese K, Molnar P, Das M, et al. A new target for amyloid beta toxicity validated by standard and high-throughput electrophysiology. Plos One. 2010;5:e8643.
- Walter FR, Valkai S, Kincses A, et al. A versatile lab-on-a-chip tool for modeling biological barriers. Sens Actuators B Chem. 2016;222:1209–1219.
- Takebe T, Zhang B, Radisic M. Synergistic engineering: organoids meet organs-on-a-chip. Cell Stem Cell. 2017;21:297–300.
- Zhao H, Chen Y, Shao L, et al. Airflow‐assisted 3D bioprinting of human heterogeneous microspheroidal organoids with microfluidic nozzle. Small. 2018;14:1802630–1802637.
- Peng W, Datta P, Wu Y, et al. Challenges in bio-fabrication of organoid cultures. Cell Biol Transl Med. 2018;3:53–71. Advances in Experimental Medicine and Biology, vol 1107. Springer, Cham.
