Abstract
Uganda, hosting over 1.3 million refugees, is a salient context for exploring HIV testing with urban refugee and displaced youth. We examined associations between stigma (HIV-related and adolescent sexual and reproductive health [SRH]-related) and HIV testing services awareness and HIV testing uptake among urban refugee and displaced youth in Kampala, Uganda. We implemented a cross-sectional survey with refugee and displaced adolescent girls and young women (AGYW) and adolescent boys and young men (ABYM) aged 16-24. We conducted exploratory and confirmatory factor analysis of an adolescent SRH stigma scale and identified a two-factor structure (“Sexual activity & pregnancy stigma”,”Modern family planning & abortion stigma”). We conducted multivariable logistic regression analysis to determine the adjusted risk ratio for HIV testing services awareness and testing uptake. Among participants (n=445; mean age=19.59, SD=2.60; AGYW: n=333; 74.7%), two-thirds were aware of HIV testing services in their community and over half (56.0%) had received a lifetime HIV test. In adjusted multivariable regression analysis findings with AGYW: (a) higher sexual activity & pregnancy stigma and modern family planning & abortion stigma were associated with reduced odds of HIV testing services awareness, and (b) modern family planning & abortion stigma was associated with reduced lifetime HIV testing odds. Stigma was not associated with HIV testing awareness/uptake among ABYM. HIV testing services awareness among AGYW was lower than among ABYM, yet AGYW were more likely to have been tested and to experience adolescent SRH stigma as a testing barrier. Addressing adolescent SRH stigma may optimise AGYW's HIV testing.
Résumé
L'Ouganda, qui abrite plus de 1,3 million de réfugiés, est un contexte important pour explorer le dépistage du VIH avec les jeunes réfugiés et déplacés en milieu urbain. Nous avons examiné les associations entre la stigmatisation (relative au VIH et relative à la santé sexuelle et reproductive (SSR) des adolescents) et la connaissance des services de dépistage du VIH et le recours au dépistage du VIH chez les jeunes réfugiés et déplacés en milieu urbain à Kampala, Ouganda. Nous avons réalisé une enquête transversale auprès d'adolescents et jeunes réfugiés et déplacés des deux sexes âgés de 16 à 24 ans. Nous avons mené une analyse factorielle exploratoire et confirmatoire d'une échelle de la stigmatisation relative à la SSR des adolescents et identifié une structure à deux facteurs (« stigmatisation relative à l'activité sexuelle et la grossesse », « stigmatisation relative à la planification familiale moderne et l'avortement »). Nous avons conduit une régression logistique à variables multiples pour déterminer le rapport ajusté en fonction du risque pour la connaissance des services de dépistage du VIH et le recours au dépistage. Chez les participants (n=445 ; âge médian= 19,59, écart-type=2,60 ; adolescentes et jeunes femmes : n=333 ; 74,7%), les deux tiers connaissaient les services de dépistage du VIH dans leur communauté et plus de la moitié (56,0%) avaient déjà fait un test de dépistage. Dans les résultats de l'analyse de régression ajustée à variables multiples pour les adolescentes et les jeunes femmes : a) une plus forte stigmatisation relative à l'activité sexuelle et la grossesse, et une plus forte stigmatisation relative à la planification familiale et l'avortement étaient associées à une moindre probabilité de connaissance des services de dépistage du VIH, et b) la stigmatisation relative à la planification familiale moderne et l'avortement était associée à une probabilité réduite d'avoir déjà réalisé au moins un dépistage du VIH. Chez les adolescents et les jeunes hommes, la stigmatisation n'était pas associée à la connaissance/à l'utilisation du dépistage du VIH. La connaissance des services de dépistage du VIH chez les adolescentes et les jeunes femmes était inférieure à celle des adolescents et des jeunes hommes, pourtant les femmes avaient plus de probabilités d'avoir réalisé un test et de se heurter à la stigmatisation relative à la SSR des adolescents comme obstacle au dépistage. S'attaquer à la stigmatisation relative à la SSR des adolescents peut optimiser le dépistage du VIH chez les adolescentes et les jeunes femmes.
Resumen
Uganda, que acoge a más de 1.3 millones de refugiados, es un contexto relevante para explorar las pruebas de VIH con refugiados y jóvenes desplazados en las zonas urbanas. Examinamos las asociaciones entre el estigma (relacionado con el VIH y con la salud sexual y reproductiva [SSR] de adolescentes), el conocimiento de servicios de pruebas de VIH y la aceptación de las pruebas de VIH entre refugiados y jóvenes desplazados en las zonas urbanas de Kampala, Uganda. Aplicamos una encuesta transversal a niñas adolescentes y mujeres jóvenes (AGYW) desplazadas y a niños adolescentes y hombres jóvenes (ABYM) desplazados, de 16 a 24 años de edad. Realizamos análisis factorial exploratorio y análisis factorial confirmatorio de una escala de estigma relacionado con la SSR de adolescentes e identificamos una estructura de dos factores (‘Estigma relacionado con la actividad sexual y con el embarazo', ‘Estigma relacionado con la planificación familiar moderna y con el aborto’). Realizamos regresión logística multivariable para determinar la razón de riesgo ajustada con relación al conocimiento de servicios de pruebas de VIH y la aceptación de las pruebas. Entre las personas participantes (n=445; edad media=19.59, SD=2.60; AGYW: n=333; 74.7%), dos terceras partes tenían conocimiento de los servicios de pruebas de VIH en su comunidad y más de la mitad (56.0%) había recibido una prueba de VIH en su vida. En los hallazgos del análisis de regresión multivariable ajustada con AGYW: (a) mayor actividad sexual y estigma del embarazo y de planificación familiar moderna, y estigma del aborto estaban asociados con menor probabilidad de tener conocimiento de los servicios de pruebas de VIH, y (b) el estigma relacionado con la planificación familiar moderna y con el aborto estaba asociado con menor probabilidad de haber recibido una prueba de VIH en su vida. No se asoció estigma con el conocimiento o la aceptación de pruebas de VIH entre ABYM. El conocimiento de servicios de pruebas de VIH era menor entre AGYW que entre ABYM; sin embargo, AGYW eran más propensas a haber recibido una prueba de VIH y a haber sufrido estigma relacionado con la SSR de adolescentes, como barrera para recibir una prueba. El abordaje del estigma relacionado con la SSR de adolescentes podría optimizar las pruebas de VIH en las AGYW.
Introduction
At the end of 2017, UNAIDSCitation1 estimated that 53% of the 36.9 million people living with HIV globally were living in Eastern and Southern Africa. This region hosts 26% of the world’s 25.4 million refugees, most whom are women and children.Citation2 Eastern and Southern Africa accounts for 45% of the world’s new HIV infections, and adolescents and young people are disproportionately affected. Adolescent girls and young women (AGYW) aged 15–24 years are particularly impacted, with an HIV prevalence double that of their male counterparts.Citation1 In Uganda, home to 1.3 million refugees,Citation2 the general population of adolescent girls aged 15–19 years had an HIV prevalence three times (9.1%)Citation3 that of adolescent boys, and higher than the national prevalence of 6.2%.Citation4 The 2016 Uganda Demographic and Health Survey revealed that, although a higher proportion of AGYW (71.2%) knew their HIV status compared with adolescent boys and young men (ABYM) (56.9%),Citation5 these proportions fall far below the UNAIDS goal of 90% of persons living with HIV knowing their status by 2020Citation6 in order to achieve an AIDS-free generation. Optimising the potential of HIV testing – an essential step for accessing treatment and support – requires engagement in the HIV testing cascade, which includes both awareness of where to access HIV testing as well as regular testing uptake.
More than half of global refugees live in urban regions, where they may experience limited community support, exclusion from social and healthcare support systems, stigma, and poverty that reduces access to healthcare services. Kampala, the capital city of Uganda, reflects the global trend of refugee urbanisation, as refugees increasingly move from settlements to urban areas for employment and education opportunities.Citation7,Citation8 Kampala hosts nearly 100,000 refugees who largely live in slumsCitation9 (informal settlements) and receive limited social and economic assistance.Citation8 Uganda has among the most progressive refugee policiesCitation9 in the world, allowing refugees freedom of movement from resettlement settings on the condition that they can be self-sustaining. Many refugees in urban areas end up living in informal settlementsCitation10 that are characterised by overcrowding, violence, sex work, poverty, and high HIV prevalence.Citation11 Yet little is known about the HIV vulnerabilities and prevention and care needs of urban refugees. The living environment of informal settlements and limited government assistance likely produce different experiences of HIV vulnerabilities and prevention among urban vs rural refugees in Uganda.Citation12, Citation13
HIV testing practices among refugee and displaced adolescents and youth are shaped by a complex interplay of social and structural factors. These include elevated poverty, increased exposure to sexual and gender-based violence, and intersecting forms of stigma and discrimination (for instance, based on gender, age, and refugee status).Citation14–16 Other factors that contribute to suboptimal HIV testing uptake include limited knowledge of available health services,Citation17 language barriers in accessing sexual and reproductive health (SRH) services, and often overburdened health systems within humanitarian contexts.Citation18 For instance, in a recent cross-sectional studyCitation19 of Bhutanese refugees in eastern Nepal, a lack of knowledge about HIV testing services was one of the main reasons for not being tested.
Stigma presents formidable barriers to HIV testing uptake across global regions.Citation20 Stigma refers to social processes of devaluation that result in reduced power and opportunity, and this is experienced as awareness of negative community norms and beliefs (perceived stigma, or stigmatising lay attitudes); acts of mistreatment and discrimination, including in employment, education, and healthcare (enacted stigma); negative self-image, shame, and blame from larger contexts of mistreatment and exclusion (internalised stigma);Citation20 and fear and expectations of experiencing devaluation, exclusion, and discrimination when others learn about their stigmatised practice/identity (anticipated stigma).Citation21 Most research on barriers to HIV testing in sub-Saharan Africa focuses on the role of HIV-related stigma. For instance, a review of 13 unique samples (five studies from Uganda) of people living with HIV (n = 9088) in sub-Saharan Africa (South Africa, Lesotho, Malawi, Tanzania, Swaziland, Mozambique, Uganda, Kenya, and Burkina Faso) reported that internalised HIV-related stigma was associated with lower uptake of HIV-related services.Citation22 A systematic review of 10 studies (none from Uganda) examining the effects of HIV-related stigma on HIV testing found that participants who had higher perceived stigma had twice the odds of late diagnosis of HIV infection.Citation23
Stigma targeting adolescents who access SRH services is understudied in HIV research, yet it is particularly salient considering adolescent girls’ overrepresentation in the HIV epidemic. For instance, in a study by Nyblade et al. in Tanzania, pervasive stigma experienced by unmarried young people was a barrier to accessing SRH services.Citation24 Hall et al. developed a stigma scale that considers the effect of social, cultural, and religious norms associated with young women’s utilisation of SRH services in Ghana.Citation25 Their Adolescent SRH Stigma Scale focuses on adolescent sexual activity, pregnancy, abortion, and contraceptive use and associated negative community norms, values, and beliefs (stigmatising lay attitudes); mistreatment and discrimination (enacted stigma); and feelings of shame and blame (internalised stigma).Citation25 They found that higher adolescent SRH stigma (overall stigma scores, as well as internalised and stigmatising lay attitudes) was associated with lower lifetime contraceptive use.Citation25 To our knowledge, there is a lacuna in the literature regarding associations between adolescent SRH stigma and HIV testing.
Urban refugee and displaced youth are at the nexus of HIV disparities among youth, displaced persons, and persons living in informal settlements, yet there are knowledge gaps regarding optimal HIV prevention and testing strategies for this population.Citation13,Citation26 The objective of the present study was to (1) examine gender differences in HIV services awareness and HIV testing uptake; (2) test the reliability and factor structure of the Adolescent SRH Stigma Scale; and (3) examine associations between stigma (HIV-related, adolescent SRH-related) and HIV services awareness and HIV testing uptake among urban refugee and displaced youth in Kampala, Uganda.
Methods
Participant recruitment and data collection
We conducted this quantitative study in collaboration with refugee agencies (Interaid Uganda, Young Africans for Integral Development [YARID], Tomorrow Vijana) and government agencies (Office of the Prime Minister [OPM], Uganda AIDS Control Program, Ministry of Health) between January and March 2018. Specifically, we conducted a tablet-based cross-sectional survey with refugee and displaced adolescents and young people in five informal settlements (“slums”) across Kampala that were selected owing to a high concentration of refugee and displaced people living in each community (Kabalagala, Rubaga, Kansanga, Katwe, and Nsambya). The study team trained 12 peer research assistants (PRAs) (four ABYM [two from the Democratic Republic of the Congo (DRC), one from Burundi, and one from South Sudan] and eight AGYW [two from Burundi, four from the DRC, one from South Sudan, and one from Rwanda]) who self-identified as refugees or displaced persons aged 18–24 years, to recruit participants and to administer the tablet-based survey. The study team and co-authors also included persons with lived experiences of settling in Uganda as refugees from Rwanda, Kenya, and the DRC. The study team conducted a five-day PRA training in research methods and ethics, survey administration, and confidentiality. This training also addressed the importance of PRAs being aware of and managing personal biases. The team worked with the PRAs to discuss each survey item for clarity (data were not collected in this process) in order to refine and enhance the relevance of the survey measures for the local context and population.
Originally, this study was designed to include only AGYW owing to the threefold higher HIV infection rates among AGYW than among ABYM in Uganda. Community partners asked us to also include ABYM; thus we aimed to oversample for proportional representation to include two-thirds AGYW and one-third ABYM in order to reflect the local HIV epidemic characteristics. Power calculations conducted using G*Power 3.1 indicated that a sample size per group of 146 would be sufficient for multivariable regression analyses (effect size: 0.15; power: 0.95; number of predictors: 6; critical F: 2.1644).
We conducted convenience and peer-driven recruitment. Community partners shared study information with outreach workers and youth attending their programmes. The community partners also recommended the PRAs owing to their community involvement and wide social networks. Modified peer-driven sampling,Citation27 a technique to recruit hidden and marginalised populations, was employed for recruitment. Each participant was given study “coupons” with PRAs’ contact information and invited to recruit a maximum of five refugee and displaced youth from their social networks to participate in the study. Research ethics approval was granted by the University of Toronto, Canada, and the Uganda Ministry of Health. The study population comprised young women and men aged 16–24 years who self-identified as a refugee or displaced person, or having refugee or displaced parents; lived in one of five informal settlements (Kabalagala, Rubaga, Kansanga, Katwe, and Nsambya); and were able to provide informed consent.
We obtained written informed consent on the tablet prior to beginning the survey. The structured survey was interviewer administered by PRAs in English or Swahili (the most common spoken language for refugees from the DRC, Rwanda, and Burundi) on tablets in a location of the participant’s choice (e.g. community centre, football pitch, collaborating community agency). Participants were given the choice of completing sensitive questions (e.g. sexual practices, violence, HIV outcomes) privately, with the PRA available for support. All participants were provided with information about sexual education, HIV, and psychosocial resources. The research coordinator, a trained social worker, was available to provide support as needed. No cases of distress were reported during the survey administration. The survey duration was approximately 35–45 min and each participant received a UGX 12,500-shilling honorarium.
Measures
Main survey outcome measures: awareness of HIV services and lifetime HIV testing
Awareness of HIV services was measured with a dichotomous question: “Are you aware of where to get an HIV test near where you live?” Lifetime HIV testing was also measured as a dichotomous item: “I have had an HIV test in my lifetime.”
Exposure variables
The exposure variables examined in this study were HIV-related stigma and adolescent SRH stigma. HIV-related stigma was assessed using Steward et al.’s 10-item perceived (also referred to as felt or felt-normative) stigma subscale, with a higher score indicating higher HIV-related stigma (score range: 0–100; full-sample Cronbach α = 0.87; AGYW Cronbach α = 0.89; ABYM Cronbach α = 0.72).Citation28
We used the 19-item Adolescent SRH Stigma Scale focused on adolescent engagement in sex, pregnancy, childbearing, abortion, STI, and family planning (Cronbach α = 0.74).Citation25 This scale had three subscales: internalised stigma; enacted stigma; and stigmatising lay attitudes. Response options were on a three-point Likert scale (disagree, neutral, agree). For our analyses, we followed recommendations by Hall et al. Citation25 and coded all “agree” responses as (1), whereby higher scores reflect higher levels of stigma. Because the Adolescent SRH Stigma Scale was created for young women in Ghana, we needed to test the reliability and relevance to urban forcibly displaced AGYW and ABYM in Kampala, Uganda. The final version of the Adolescent SRH Stigma Scale used in the present Ugandan study included 14 items, as listed in .
Table 1. Ugandan adolescent sexual and reproductive health stigma scale items by gender among urban refugee and displaced adolescents and young people in Kampala, Uganda (n = 445)
Confounders
We assessed sociodemographic variables including age, education level (no education/less than secondary school, and post-secondary education), employment status (employed, unemployed, and student), and relationship status (no relationship, dating one partner/married, and casual dating/multiple partners) measured categorically. Forced sex history was measured dichotomously by asking: “Has someone sexually forced themselves on you or forced you to have sex?” An affirmative response was coded as forced sex history.
Analyses
We first conducted descriptive analyses of all variables to determine frequencies and proportions for categorical variables, and means and standard deviations (SDs) for continuous variables. Descriptive analyses included all participants with available data. We then conducted bivariate analyses (t-test and χ²) to examine sociodemographic, relationship, and outcome differences by gender (n = 445).
To assess the structure of the Adolescent SRH Stigma Scale with this population, we followed steps outlined by Bowen and GuoCitation29 to test measurement models by first creating two subsamples: calibration and validation. In step 1, we used the calibration subsample (n = 222) to conduct exploratory factor analysis (EFA) aimed at classifying individual items into adolescent SRH stigma factors. Factor loadings ≥0.30 were retained. Eigenvalues >1 (Kaiser criterion) were used to determine the number of factors to retain. Cronbach α measures were generated to examine the internal consistency of the adolescent SRH stigma subscales, with values >0.7 deemed acceptable. In step 2, confirmatory factor analysis (CFA) was conducted using the validation subsample (n = 223) to verify the factor structure from the EFA results. The three-index approachCitation30 was used to assess model fit: comparative fit index (CFI); root mean square error of approximation (RMSEA); and Tucker–Lewis Index (TLI). Good model fit is represented as CFI ≥0.95, TLI ≥0.95, and RMSEA ≤0.05. Adequate fit is represented as CFI ≥0.90, TLI ≥0.90, and RMSEA ≤0.08.Citation31
In step 3, we conducted bivariate logistic regression followed by multivariable logistic regression, controlling for factors correlated at p < .05 to identify appropriate estimates of the adjusted odds ratio (AOR) for each outcome (HIV testing services awareness, lifetime HIV testing). First, we summed items for each of the two-factor structures following the final results from the validation sample. We then used stepwise logistic regression, entering sociodemographic factors first, followed by stigma factors, to examine the independent effect of stigma factors on HIV service awareness and testing uptake. We report the unadjusted odds ratios (ORs) and AORs plus 95% confidence intervals (CIs), highlighting those significant at the 0.05 level. We stratified analysis and results by gender. Missing responses were excluded from the analyses; the number of complete responses was reported for each variable.
We conducted multivariable logistic regression analyses to examine associations between stigma scales and HIV testing uptake and awareness, controlling for potential confounders. Model fit was assessed using the omnibus χ² tests of model coefficient, the percentage of respondents correctly classified as having awareness of HIV testing services versus no awareness of HIV testing services, and ever receiving an HIV test versus never receiving an HIV test. We also considered sensitivity and specificity for each model. The Nagelkerke pseudo R2 was examined to determine the amount of variance in HIV testing services awareness and HIV testing engagement that can be explained by the set of variables included in each model. However, given that logistic regression does not have the equivalent of an R2 as found in ordinary least squares regression, interpretations of variance should be made with caution. We conducted analyses using IBM’s Statistical Package for Social Sciences 25, and CFA using Mplus 7.4.
Results
Exploratory factor analysis results
The two-factor structure of the Adolescent SRH Stigma Scale identified in the present study was further confirmed using the main correlation matrix. Kaiser–Meyer–Olkin measure of sampling adequacy was 0.80, above 0.5 and thus indicating the appropriateness of applying factor analysis. All commonalities were above 0.3, further confirming that each item shared a common variance with other items. There were two rotated components that were extracted and used as latent constructs to represent measures of adolescent SRH stigma in this study. As depicted in , the two factor loadings each included items from across the original Adolescent SRH Stigma Scale subscales (enacted, internalised, and lay attitude stigma dimensions). This suggests that the factor structure necessitated an alternative conceptualisation of elements of adolescent SRH stigma that extend beyond stigma dimensions. Examining the seven items in factor 1, three concerned stigma from being known to be sexually active, three concerned pregnancy, and one family planning. These items included three items categorised as enacted stigma in the original scale and four categorised as internalised stigma. We named this subscale “sexual activity & pregnancy stigma”. Examining the seven items in factor 2, four related to stigma regarding using modern family planning methods, two were regarding abortion stigma, and one was regarding sexual activity stigma. These included three items labelled enacted stigma in the original Adolescent SRH Stigma Scale, two categorised as stigmatising lay attitudes, and two as internalised stigma. We named this subscale “modern family planning & abortion stigma”. The overall reliability of the adapted scale was satisfactory (Cronbach α: full sample = 0.83; AGYW = 0.86; ABYM = 0.75). Reliability for the two constructs had an acceptable Cronbach α (sexual activity & pregnancy stigma subscale: full sample = 0.82; AGYW = 0.84; ABYM = 0.74; modern family planning & abortion stigma subscale: full sample = 0.68; AGYW = 0.73; ABYM = 0.51). We excluded the third factor with items 13, 14, 17, 18, and 19 because of poor internal consistency. Four of these five excluded items were categorised as stigmatising lay attitudes in the original Adolescent SRH Stigma Scale, and one as internalised stigma.
Confirmatory factor analysis results
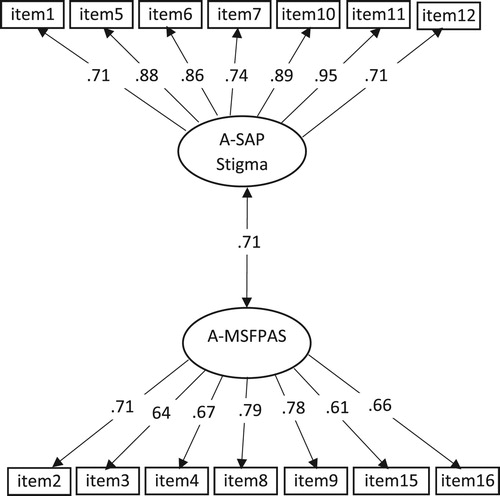
The two-factor CFA with the validation sample showed good fit: χ2 = 169.37; df = 78; p < .000; RMSEA = 0.07 (90% CI: 0.06, 0.09); CFI = 0.93; TLI = 0.92. Factor loadings ranging from 0.61 to 0.95 were higher than the recommended 0.30 cutoff. Using the validation sample, the CFA provided statistical support for the two-factor Adolescent SRH Stigma Scale. The final scales were summed and used to examine the third aim of our study ().
Figure 1. Confirmatory factor analysis results of the Ugandan Adolescent Sexual and Reproductive Health Stigma Scale among urban refugee and displaced adolescents and young people living in Kampala, Uganda
Note: Items = sexual and reproductive health stigma items that loaded onto each subscale; A-SAP = Adolescent sexual activity and pregnancy stigma; A-MFPAS = Adolescent modern family planning and abortion stigma.
Participant characteristics
presents the sociodemographic characteristics of the full sample (n = 445) as well as the gender-specific subsamples for AGYW (n = 333) and ABYM (n = 112). Of the total sample, most participants identified as AGYW and were from the DRC. Slightly over half of the participants reported a lifetime HIV test (56.0%; n = 249), with no significant gender differences. Among those who tested for HIV, more AGYW than ABYM self-reported an HIV-positive result (8/182 [4.4%] vs 1/60 [1.6%]), but this was not statistically significant.
Table 2. Characteristics of urban refugee and displaced adolescents and young people in Kampala, Uganda, by gender (n = 445)
There were gender differences across variables. Significantly more AGYW than ABYM had less than high-school education (190/333[57.1%] vs 44/112 [39.3%]; p < .001) and reported higher HIV-related stigma (M = 32.04 vs M = 29.79; p = .001). More AGYW had lived in Uganda longer than 5 years, whereas ABYM were more likely to report living in Uganda for 1–5 years (79/112 [70.5%] vs 186/333 [55.9%]; p < .001).
Differences in HIV testing awareness and uptake among urban refugee and displaced adolescent girls and young women in Kampala, Uganda
illustrates the results from χ² independent tests and t-tests examining differences associated with HIV testing services awareness and HIV testing uptake among AGYW. For instance, sociodemographic differences emerged regarding awareness of HIV testing services: older age was associated with increased awareness (M = 19.94 vs M = 18.30); persons with secondary school education were more likely to be aware than those with less than secondary school education (51% [n = 104] vs 49% [n = 100]); and those born in the DRC (62%; n = 81) reported lower awareness of HIV testing services compared with AGYW born in South Sudan (7%; n = 7), Burundi (22.5%; n = 29), Rwanda (2.3%; n = 3), and other locations (5.4%; n = 7). There were also interpersonal differences, whereby persons who were dating one partner/married reported higher HIV testing services awareness and lifetime HIV testing (45.9%; n = 85) than those with no current partners (38.4%; n = 71) or who were casual dating/had multiple partners (15.7%; n = 29). AGYW who experienced lifetime forced sex reported lower HIV testing services awareness (27.9% [n = 57] vs 72.1% [n = 147]) and lower HIV testing uptake (34.1% [n = 62] vs 65.9% [n = 120]) compared with their counterparts with no experiences of forced sex. Adolescent SRH stigma was associated with poorer HIV testing outcomes for AGYW. Those with higher sexual activity & pregnancy stigma and higher modern family planning & abortion stigma reported lower awareness of HIV testing services and lower HIV testing uptake.
Table 3. Characteristics of urban refugee and displaced adolescent girls and young women in Kampala, Uganda, by awareness of HIV testing services and lifetime HIV testing (n = 333)
Differences in HIV testing awareness and uptake among urban refugee and displaced adolescent boys and young men in Kampala, Uganda
presents the findings from χ² independent tests and t-tests examining HIV testing services awareness and HIV testing uptake among ABYM. Participants living in Uganda longer were more likely to be aware of HIV testing services (95.3%; n = 82). Participants who were older (M = 21.16 vs M = 19.34) and those with a secondary school education (70.6%; n = 48) reported higher HIV testing uptake compared with their counterparts who were younger and who had less than secondary school education (29.4%; n = 20).
Table 4. Characteristics of urban refugee and displaced adolescent boys and young men in Kampala, Uganda, by awareness of HIV testing services and lifetime HIV testing (n = 112)
Univariate and multivariate modelling of stigma and HIV testing services awareness among urban refugee and displaced adolescent girls and young women in Kampala, Uganda
shows the multivariable logistic regression results examining the independent relationship between stigma scores and awareness of HIV testing services among AGYW. In the unadjusted model, sociodemographic factors including age, education level, employment status, and relationship status emerged as being associated with awareness of HIV testing services. However, employment status was the only sociodemographic variable that remained significant in the adjusted model. In the adjusted model, the odds of HIV testing services awareness in one's community was 88% lower for respondents who were unemployed (AOR = 0.12; 95% CI = 0.03, 0.48; p < .010) and 91% lower for students (AOR = 0.09; 95% CI = 0.02, 0.35; p < .001) compared with respondents who were employed.
Table 5. Multivariable logistic regression results examining associations between stigma and HIV testing services awareness and lifetime HIV testing among urban refugee and displaced adolescent girls and young women in Kampala, Uganda (n = 333)
In unadjusted and adjusted analyses, both sexual activity & pregnancy stigma and modern family planning & abortion stigma were associated with lower odds of HIV testing awareness. Adjusting for all other factors, for each additional unit increase in sexual activity & pregnancy stigma, the odds of a respondent being aware of HIV testing services decreased by 32% (AOR = 0.68; 95% CI = 0.54, 0.87; p < .001). We also observed that a one-unit increase in modern family planning & abortion stigma was associated with a 21% decrease in HIV testing services awareness (AOR = 0.79; 95% CI = 0.64, 0.99; p < .050).
All model diagnostic statistics indicated good model fit, and both exposure and confounder factors contributed to the model. Based on the Nagelkerke pseudo R2, stigma variables and the confounders explained approximately 35% of the variance in HIV testing services awareness. In the adjusted model, approximately 67% of the respondents were correctly classified as being aware vs unaware of HIV testing services.
Univariate and multivariate modelling of HIV testing uptake among urban refugee and displaced adolescent girls and young women in Kampala, Uganda
As illustrated in , in unadjusted multivariable logistic regression analyses the sociodemographic variables associated with HIV testing uptake included older age, secondary school education (vs less than secondary school education), employment status (unemployed were more likely to test than employed, and students were less likely to test than employed), no lifetime experiences of forced sex, and relationship status (one partner vs single). In the adjusted model, older youth were 1.18 times more likely to engage in HIV testing compared with their younger counterparts (AOR = 1.18; 95% CI = 1.02, 1.38; p < .05). Respondents who were unemployed were nearly four times as likely to engage in HIV testing compared with their employed counterparts (AOR = 3.8; 95% CI = 1.43, 9.83; p < .010). Respondents who experienced lifetime forced sex had 83% lower odds of engaging in HIV testing (AOR = 0.17; 95% CI = 0.07, 0.37; p < .001) compared with respondents who did not experience lifetime forced sex. Persons dating one person or married had nearly fourfold odds of HIV testing than those who were single (AOR =3.80; 95% CI = 1.94, 7.44; p < .001).
Although sexual activity & pregnancy stigma was significantly associated with lower odds of HIV testing in the unadjusted model, it lost its significance in adjusted analyses. Modern family planning & abortion stigma was significantly associated with lower testing likelihood in both unadjusted and adjusted analyses. Each additional unit increase in modern family planning & abortion stigma was associated with a 22% decrease in HIV testing among AGYW (AOR = 0.78; 95% CI = 0.63, 0.97; p < .050).
For this model, the stigma factors and confounders contributed to the model fit. The Nagelkerke pseudo R2 revealed that stigma variables and the confounders explained approximately 44% of the variance in HIV testing uptake. In the adjusted model, 74.4% of the respondents were correctly classified as ever testing for HIV versus never testing for HIV.
Univariate and multivariate modelling of awareness of HIV testing services among urban refugee and displaced adolescent boys and young men in Kampala, Uganda
shows the multivariable logistic regression results of factors associated with the odds of HIV testing service awareness among ABYM. Only age was significant in the unadjusted model, and lost its significance in the adjusted model.
Table 6. Multivariable logistic regression results examining associations between stigma and HIV testing services awareness and lifetime HIV testing among urban refugee and displaced adolescent boys and young men in Kampala, Uganda (n = 112)
Univariate and multivariate modelling of HIV testing uptake among urban refugee and displaced adolescent boys and young men in Kampala, Uganda
shows the multivariable logistic regression results of HIV testing uptake among ABYM.
In the unadjusted model, age and education level were associated with increased likelihood of HIV testing. However, education level lost its significance in adjusted analyses. Respondents who were older were 2.8 times more likely to engage in HIV testing compared with their younger counterparts (AOR = 2.8; 95% CI = 1.06, 7.63; p < .050).
Based on the Nagelkerke pseudo R2, variables in the adjusted model were found to account for 14% of the variance in HIV testing uptake. We observed that 73.5% of the cases were correctly predicted as having engaged in HIV testing (sensitivity). With respect to specificity, 77.3% of the respondents were correctly predicted as having not engaged in HIV testing in the fully adjusted model.
Discussion
The study findings reveal that HIV testing prevalence among urban refugee young people living in informal settlements in Kampala falls far short of the UNAIDS goals of 90% of people living with HIV knowing their status.Citation6 Among this sample of urban young refugee and displaced persons, nearly two-thirds knew where to access HIV testing services in their community. While ABYM were more likely than AGYW to report knowing where these services were, there were no gender differences in lifetime HIV testing. This suggests that testing awareness does not necessarily translate into uptake, and ABYM may experience gendered testing barriers. Just over half of the participants (56.2%) had ever received an HIV test, and among those ever tested one-third reported their last test being more than one year ago. These suboptimal testing rates are alarming, as HIV testing is a central component of HIV prevention and care. These findings suggest that urban refugee adolescents and youth are a key population left behind in HIV prevention efforts in Kampala. What is particularly striking about these findings is that adolescent SRH stigma – not HIV-related stigma – was associated with HIV testing services awareness and testing uptake among urban refugee and displaced AGYW. While a rich body of research has detailed the harmful impacts of HIV-related stigma on HIV prevention and testing,Citation20,Citation22 adolescent SRH stigma is underexplored in relation to the HIV prevention cascade.
The associations between adolescent SRH stigma and the HIV testing cascade (awareness, uptake) among urban refugee and displaced AGYW signal adolescent SRH stigma as a key area for research and intervention. It is plausible that urban refugee and displaced AGYW experience negative community attitudes regarding their sexual activity and access to reproductive services that are not only a deterrent from accessing modern contraception, as reported in Ghana,Citation25 but can also curb AGYW from accessing information about other sexual health services such as HIV testing. From an intersectional stigma perspective,50 it is important to consider how these harmful norms that foster judgement towards the sexual practices of youth may intersectCitation20 with stigma targeting language barriers and immigration status.Citation32,Citation33 For instance, a mixed-methods study conducted among Congolese and Somali urban refugees in UgandaCitation33 found that more than half of participants reported experiencing discrimination and language barriers to accessing health information.Citation33 When it came to HIV testing among AGYW in the present study, those who reported lower modern family planning & abortion stigma were more likely to have been tested. This also suggests that reducing stigma around reproductive health services could encourage HIV testing uptake, aligning with findings from the Nakivale refugee settlement in UgandaCitation34 that individuals were more likely to test for HIV if the environment was less stigmatising.
There appears to be a gendered impact of adolescent SRH stigma on the HIV testing cascade. While there were no reported gender differences () in adolescent SRH stigma dimensions (sexual activity & pregnancy stigma, modern family planning & abortion stigma), it was only AGYW (not ABYM) who reported associations between adolescent SRH stigma and HIV testing awareness and uptake. This signals that adolescent SRH stigma may limit the engagement of AGYW in HIV testing services, while ABYM may not experience these same outcomes of SRH stigma. Communicating SRH information within a gender transformative approach to same-gender peer groups could help to shift gender norms and internalised dimensions of SRH stigma. An intersectional approach is needed to tackle the gender bias and inequities underpinning adolescent SRH stigma.Citation25 Future research should develop a measure of adolescent SRH stigma tailored for ABYM; the scale we used was developed and validated with AGYW in Ghana,Citation25 and our analyses failed to identify which factors were associated with HIV testing awareness and uptake with ABYM. It is plausible that, instead of being impacted by modern family planning & abortion stigma, ABYM may experience other, underexplored forms of SRH stigma. Qualitative research could also address this knowledge gap in testing barriers and facilitators for refugee and displaced ABYM.
While the original Adolescent SRH Stigma Scale developed in GhanaCitation25 included subscales of stigma dimensions (enacted, internalised, stigmatising lay attitudes), the factor structure in this Ugandan sample signalled another way to conceptualise SRH stigma experienced by adolescents. Specifically, the factor loadings suggested that stigma targeting sexual activity and pregnancy, and stigma targeting modern family planning and abortion were unique subscales. Our approach aligns with the recent Health Stigma and Discrimination Framework of Stangl et al.,Citation20 which conceptualises drivers (e.g. fear of social judgment) and facilitators (e.g. gender norms) that result in stigma marking of health conditions (e.g. HIV) and identities (e.g. age, gender) that manifest in stigma experiences (enacted, perceived, internalised) and poorer health outcomes (e.g. lower healthcare access). This Health Stigma and Discrimination FrameworkCitation20 may be applied to understand our findings: drivers (e.g. stereotypes towards sexually active AGYW) and facilitators (inequitable gender norms where it is more acceptable for ABYM than AGYW to be sexually active) result in stigma marking (e.g. sexual activity and pregnancy stigma) and subsequently stigma experiences (internalised, enacted, stigmatising lay outcomes), and ultimately poorer outcomes (lower testing awareness, lower testing uptake). By teasing apart the salient elements of SRH stigma among AGYW – stigma specifically targeting sexual activity and reproductive care engagement – findings can inform actionable stigma interventions.
Limitations, implications, and future directions
Study limitations include non-random sampling, which limits our ability to generalise study findings to all urban refugees in Uganda. Owing to the cross-sectional nature of our study, we can only infer association, not causality, between variables. The use of self-reported data might be influenced by social desirability bias, particularly regarding HIV testing results. The smaller sample of ABYM compared with AGYW limits our ability to draw comparison between factors associated with HIV testing. Qualitative research could further our understanding of social–ecological barriers to HIV testing among ABYM and the ways in which ABYM may experience adolescent SRH stigma. Future studies could use respondent-driven sampling to examine social networks and associations with stigma and related outcomes. Finally, while we followed best practicesCitation35 to build on prior research through utilising an existing scaleCitation25 vs developing a new scale for adolescent SRH stigma, factor analysis revealed different underlying latent constructs. Notably, the stigmatising lay attitudes subscale items from the original scaleCitation25 were largely excluded owing to poor fit, suggesting that lay attitude items may need to be contextually developed and evaluated with urban refugee youth in Kampala.
Notwithstanding these limitations, our study is unique in examining associations between adolescent SRH stigma and HIV testing services awareness and uptake among urban refugee and displaced youth in Kampala, Uganda – and elsewhere. We document that this is a population at risk for HIV that is falling behind the UNAIDS 90–90–90 goals.Citation6 Addressing adolescent SRH stigma is a key area for future research and can be central to advancing sexual health and rights among young refugee and displaced persons.Citation16 The study findings are also innovative in signalling the importance of considering adolescent SRH stigma that may limit testing practices among AGYW – beyond a solitary focus on HIV-related stigma. A considerable proportion of participants with secondary school education did not know where to access HIV testing, and AGYW students were less likely to be aware of testing than were employed AGYW, suggesting the need for schools to address HIV prevention and SRH stigma.
While adolescent SRH stigma interventions are required at community and healthcare levels, HIV self-testing initiativesCitation36 could also reduce testing barriers of stigma. HIV self-testing holds the potential to increase HIV testing access and uptake, particularly among youth. For instance, a study conducted in Malawi found that HIV self-testing among people aged 16–24 years was consistently higher than among older participants.Citation37 Further studies could explore values and preferences regarding HIV self-testing among young urban refugees.
Conclusions
There is a pressing need for contextually tailored HIV prevention practices and services to meet the realities of urban refugee youth living in informal settlements in Kampala. Healthcare services need to be tailored by gender and age and take into consideration the needs and realities of young forcibly displaced persons in informal settlements. Community-based approaches can work with urban refugee and displaced youth to identify and develop innovative, contextually relevant strategies for transforming inequitable gender norms and advancing SRH and rights. Addressing adolescent SRH stigma in families, communities, and healthcare settings – as well as among youth themselves – needs to be a central charge of HIV prevention strategies tailored to meet the gendered stigma experiences of AGYW. There is an urgent need for further research to conceptualise and unpack stigma experiences and HIV testing barriers and facilitators among urban refugee and displaced ABYM.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- UNAIDS. UNAIDS data 2018. Geneva; 2018. [cited 2018 Nov 24]. Available from: http://www.unaids.org/sites/default/files/media_asset/unaids-data-2018_en.pdf
- UNHCR. Global trends: forced displacement in 2017. Geneva; 2018. [cited 2018 Nov 27]. Available from: https://www.unhcr.org/5b27be547.pdf.
- Uganda AIDS Commission, United Nations Uganda. Press release on HIV situation in Uganda February 23 2017. [cited 2017 Aug 22]. Available from: http://www.un-ug.org/press-releases/press-release-hiv-situation-uganda-february-23-2017. Published 2017.
- Uganda Ministry of Health, ICAP Columbia University. Uganda population-based HIV impact assessment: 2016–2017. Kampala; 2017. [cited 2018 Jul 1]. Available from: http://www.afro.who.int/sites/default/files/2017-08/UPHIA Uganda factsheet.pdf
- Uganda Bureau of Statistics. Demographic and health survey 2016 key indicators report. Kampala; 2016. Available from: https://dhsprogram.com/pubs/pdf/PR80/PR80.pdf.
- UNAIDS. 90-90-90: an ambitious treatment target to help end the AIDS epidemic. Geneva; 2014. [cited 2017 Sep 1]. Available from: http://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf.
- Lyytinen E. Informal places of protection: Congolese refugees’ “communities of trust” in Kampala, Uganda. J Ethn Migr Stud. 2017;43(6):991–1008. DOI:10.1080/1369183X.2016.1207506.
- Omata N, Kaplan J. Refugee livelihoods in Kampala, Nakivale and Kyangwali refugee settlements. Patterns of engagement with the private sector. Oxford; 2013; [cited 2017 Sep 1]. Available from: https://www.rsc.ox.ac.uk/files/files-1/wp95-refugee-livelihoods-kampala-nakivale-kyangwali-2013.pdf.
- UNHCR. Uganda country refugee response Plan. Nairobi; 2019. [cited 2019 Feb 16]. Available from: https://data2.unhcr.org/en/documents/download/67314.
- Dahab M, Spiegel PB, Njogu PM, et al. Changes in HIV-related behaviours, knowledge and testing among refugees and surrounding national populations: a multicountry study. AIDS Care. 2013;25(8):998–1009. DOI:10.1080/09540121.2012.748165.
- Madise J, Ziraba N, Inungu AK, et al. Are slum dwellers at heightened risk of HIV infection than other urban residents? Evidence from population-based HIV prevalence surveys in Kenya. Health Place. 2012;18(5):1144–1152. DOI:10.1016/J.HEALTHPLACE.2012.04.003.
- Malamba SS, Muyinda H, Spittal PM, et al. “The Cango Lyec Project – healing the elephant”: HIV related vulnerabilities of post-conflict affected populations aged 13–49 years living in three mid-Northern Uganda districts. BMC Infect Dis. 2016;16(1):690. DOI:10.1186/s12879-016-2030-0.
- Nöstlinger C, Loos J. Migration patterns and HIV prevention in Uganda. Lancet HIV. 2018;5(4):e158–e160. DOI:10.1016/S2352-3018(18)30023-7.
- The Joint United Nations Programme on HIV/AIDS (UNAIDS). The gap report. Geneva; 2014; [cited 2017 Feb 18]. Available from: http://files.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2014/UNAIDS_Gap_report_en.pdf.
- Warren E, Post N, Hossain M, et al. Systematic review of the evidence on the effectiveness of sexual and reproductive health interventions in humanitarian crises. BMJ Open. 2015;5(12):e008226. DOI:10.1136/bmjopen-2015-008226.
- Spiegel PB, Bennedsen AR, Claass J, et al. Prevalence of HIV infection in conflict-affected and displaced people in seven sub-Saharan African countries: a systematic review. Lancet. 2007;369(9580):2187–2195. DOI:10.1016/S0140-6736(07)61015-0.
- Musheke M, Ntalasha H, Gari S, et al. A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in sub-Saharan Africa. BMC Public Health. 2013;13(1):220. DOI:10.1186/1471-2458-13-220.
- Spiegel PB. The humanitarian system is not just broke, but broken: recommendations for future humanitarian action. Lancet. 2017;6736(17):1–8. DOI:10.1016/S0140-6736(17)31278-3.
- Khatoon S, Budhathoki SS, Bam K, et al. Socio-demographic characteristics and the utilization of HIV testing and counselling services among the key populations at the Bhutanese refugees Camps in Eastern Nepal. BMC Res Notes. 2018;11(1):535. DOI:10.1186/s13104-018-3657-2.
- Stangl AL, Earnshaw VA, Logie CH, et al. The health stigma and discrimination framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019;17(1):31. DOI:10.1186/s12916-019-1271-3.
- Quinn DM, Chaudoir SR. Living with a concealable stigmatized identity: the impact of anticipated stigma, centrality, salience, and cultural stigma on psychological distress and health. J Pers Soc Psychol. 2009;97(4):634–651. DOI:10.1037/a0015815.
- Pantelic M, Shenderovich Y, Cluver L, et al. Predictors of internalised HIV-related stigma: a systematic review of studies in sub-Saharan Africa. Health Psychol Rev. 2015;9(4):469–490. DOI:10.1080/17437199.2014.996243.
- Gesesew HA, Tesfay Gebremedhin A, Demissie TD, et al. Significant association between perceived HIV related stigma and late presentation for HIV/AIDS care in low and middle-income countries: a systematic review and meta-analysis. PLoS One. 2017;12(3):e0173928. DOI:10.1371/journal.pone.0173928.
- Nyblade L, Stockton M, Nyato D, et al. Perceived, anticipated and experienced stigma: exploring manifestations and implications for young people’s sexual and reproductive health and access to care in North-Western Tanzania. Cult Health Sex. 2017;19(10):1092–1107. DOI:10.1080/13691058.2017.1293844.
- Hall KS, Manu A, Morhe E, et al. Development and validation of a scale to measure adolescent sexual and reproductive health stigma: results from young women in Ghana. J Sex Res. 2018;55(1):60–72. DOI:10.1080/00224499.2017.1292493.
- World Health Organization (WHO). Global health sector strategy on HIV, 2016–2021. Geneva: World Health Organization; 2016. [cited 2017 Feb 18]. Available from: http://apps.who.int/iris/bitstream/10665/246178/1/WHO-HIV-2016.05-eng.pdf?ua=1.
- Magnani R, Sabin K, Saidel T, et al. Review of sampling hard-to-reach and hidden populations for HIV surveillance. Aids. 2005;19(Suppl 2):S67–S72. DOI:10.1097/01.aids.0000172879.20628.e1.
- Steward WT, Herek GM, Ramakrishna J, et al. HIV-related stigma: adapting a theoretical framework for use in India. Soc Sci Med. 2008;67(8):1225–1235. DOI:10.1016/j.socscimed.2008.05.032.
- Bowen NK, Guo S. Structural equation modeling. Oxford: Oxford University Press; 2011.
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model A Multidiscip J. 1999;6(1):1–55. DOI:10.1080/10705519909540118.
- Little TD. Longitudinal structural equation modeling. New York (NY): Guilford Press; 2013.
- Shedlin MG, Decena CU, Noboa H, et al. Sending-country violence and receiving-country discrimination: effects on the health of Colombian refugees in Ecuador. J Immigr Minor Heal. 2014;16(1):119–124. DOI:10.1007/s10903-013-9777-9.
- Stark L, DeCormier Plosky W, Horn R, et al. “He always thinks he is nothing”: the psychosocial impact of discrimination on adolescent refugees in urban Uganda. Soc Sci Med. 2015;146:173–181. DOI:10.1016/J.SOCSCIMED.2015.10.045.
- O'Laughlin KN, Kasozi J, Walensky RP, et al. Clinic-based routine voluntary HIV testing in a refugee settlement in Uganda. J Acquir Immune Defic Syndr. 2014;67(4):409–413. DOI:10.1097/QAI.0000000000000317.
- Boateng GO, Neilands TB, Frongillo EA, et al. Best practices for developing and Validating scales for health, social, and behavioral research: a primer. Front Public Heal. 2018;6:149. DOI:10.3389/fpubh.2018.00149.
- Logie CH, Khoshnood K, Okumu M, et al. Self care interventions could advance sexual and reproductive health in humanitarian settings. Br Med J. 2019;365:l1083. DOI:10.1136/bmj.l1083.
- Choko AT, Kumwenda MK, Johnson CC, et al. Acceptability of woman-delivered HIV self-testing to the male partner, and additional interventions: a qualitative study of antenatal care participants in Malawi: J Int AIDS Soc. 2017;20(1):21610. DOI:10.7448/IAS.20.1.21610.
