Abstract
Migrant women in industrialised countries experience high caesarean section (CS) rates but little is known about the effect of a previous delivery in the host country. This study set out to investigate this effect among migrant women in France, using data from the DSAFHIR study on healthcare access of migrant women living in emergency housing hotels, collected in the Paris Metropolitan area in 2017. Respondents reported life-long history of deliveries. We focused on deliveries occurring in France in 2000–2017: 370 deliveries reported by 242 respondents. We conducted chi-square tests and multivariate logistic regressions, adjusting for the clustering of deliveries among respondents by computing standard errors allowing for intragroup correlation. Mode of delivery was associated with duration of residence among multiparous women with no prior CS, with a higher CS rate with shorter duration of residence (16% vs. 7%, p = 0.04). In this group, a previous delivery in France was associated with a lower CS rate (5% vs. 16%, p = 0.008). In multivariate analysis, compared with women with previous birth in France, women giving birth in France for the first time had a higher risk of CS, regardless of duration of residence (aOR = 4.0, 95% CI = 1.3–12.1 for respondents with short duration of residence, aOR = 4.7, 95% CI = 1.2–18.0 for respondents with longer duration of residence). Efforts directed at decreasing the CS rate among migrant women should target women giving birth in the host country for the first time.
Résumé
Les migrantes dans les pays industrialisés connaissent des taux élevés de césarienne, mais on sait peu de choses sur l’incidence d’un accouchement précédent dans le pays hôte. L’étude a souhaité enquêter sur cette incidence parmi les migrantes en France, en utilisant les données de l’étude DSAFHIR sur l’accès aux soins de santé des migrantes hébergées en hôtel social, recueillies dans la zone métropolitaine de Paris en 2017. Les répondantes ont informé de leurs accouchements précédents. Nous nous sommes centrés sur les naissances s’étant déroulées en France de 2000 à 2017: 370 naissances signalées par 242 répondantes. Nous avons réalisé des tests du khi carré et des régressions logistiques multivariables, en ajustant pour le regroupement des accouchements parmi les répondantes en calculant les erreurs standard permettant une corrélation intragroupe. Le mode d’accouchement était associé à la durée du séjour chez les multipares sans césarienne préalable, avec un taux de césarienne plus élevé en cas de durée de séjour plus courte (16% contre 7%, p = 0,04). Dans ce groupe, un accouchement précédent en France était associé à un taux inférieur de césarienne (5% contre 16%, p = 0,008). Dans l’analyse multivariable, comparées aux femmes avec une naissance précédente en France, les femmes accouchant en France pour la première fois couraient un risque supérieur de césarienne, quelle que soit la durée de leur séjour (rapport de cote ajusté (Rca) = 4,0, 95% IC = 1,3–12,1 pour les répondantes avec un séjour de courte durée, Rca = 4,7, 95% IC = 1,2–18,0 pour les répondantes avec un séjour plus long). Les activités destinées à diminuer le taux de césarienne chez les migrantes devraient viser les femmes qui accouchent dans le pays hôte pour la première fois.
Resumen
Las mujeres migrantes en países industrializados presentan altas tasas de partos por cesárea, pero no se sabe mucho sobre el efecto de partos anteriores en el país anfitrión. Este estudio se propuso investigar este efecto entre mujeres migrantes en Francia, utilizando datos del estudio de DSAFHIR sobre el acceso a servicios de salud por mujeres migrantes que viven en hoteles como viviendas de emergencia, recolectados en el área metropolitana de París en 2017. Las entrevistadas informaron sus antecedentes de partos a lo largo de su vida. Nos enfocamos en los partos que ocurrieron en Francia entre los años 2000 y 2017: 370 partos informados por 242 entrevistadas. Realizamos pruebas de chi-cuadrado y regresiones logísticas multivariadas, e hicimos ajustes por el agrupamiento de partos entre entrevistadas calculando errores estándares para permitir la correlación entre grupos. La modalidad de parto estaba asociada con la duración de residencia entre mujeres multíparas sin antecedentes de cesárea; se observó una tasa más elevada de cesáreas entre mujeres cuya duración de residencia fue más corta (16% vs. 7%, p = 0.04). En este grupo, un parto anterior en Francia estaba asociado con menor tasa de cesáreas (5% vs. 16%, p = 0.008). En un análisis multivariado, comparado con mujeres con antecedentes de partos en Francia, las mujeres que dieron a luz en Francia por primera vez corrían mayor riesgo de parto por cesárea, independientemente de su duración de residencia (RMa = 4.0, IC de 95% = 1.3–12.1 para las entrevistadas con corta duración de residencia, RMa = 4.7, IC de 95% = 1.2–18.0 para las entrevistadas con mayor duración de residencia). Los esfuerzos dirigidos hacia disminuir la tasa de cesárea entre las mujeres migrantes deben dirigirse a las mujeres que dan a luz en el país anfitrión por primera vez.
Introduction
Delivery by caesarean section (CS) is an obstetrical procedure with the potential to prevent maternal and perinatal mortality and maternal morbidity in the event of childbirth complications such as prolonged or obstructed labour.Citation1 However, there is growing concern globallyCitation2,Citation3 over increased rates of caesarean section (CS) due to associated risks of maternalCitation4–6 and infant morbidity.Citation7–9
Disparities in CS rate have been reported between migrant and non-migrant women giving birth in Europe,Citation10–15 the US,Citation16–18 Canada,Citation19 AustraliaCitation20 and Israel.Citation21 Rates differ according to migrant women’s country of origin,Citation22 with higher CS rates among migrant women born in Sub-Saharan Africa consistently reported across host countriesCitation23–25 and mixed results among foreign-born Hispanic women in the US.Citation26,Citation27
Major determining factors of CS include maternal age, having had a prior CS and medical factors such as pre-eclampsia.Citation28 In migrant women, factors determining higher CS rates include poor general health,Citation29 higher body mass index (BMI)Citation30 and infectious diseases,Citation31 but also non-clinical factors such as limited access to health care,Citation29 sub-optimal care,Citation32 language barriers and lower socio-economic status.Citation11 Hypothesised reasons for the lower rates include younger maternal age and a favourable health status upon arrival in the host country. The relation between health status, migration and duration of residence has been investigated since the 1980s in terms of migrant mortality advantage,Citation33 or “healthy migrant effect”; migrants benefit from a better health status than the general population of the host country due to positive selection for migration; their health then declines over time with exposure to deleterious working and living conditions in the host country.
While health status tends to decline with longer stays in the host country, leading to increased risk of CS, other suggested determinants of CS such as language ability and access to health care improve with increased duration of residence, suggesting a decreased risk of CS with a longer duration of residence. However, studies investigating the association between caesarean delivery and duration of residence have found significantly increased risk of CS in primiparous women with longer duration of residence in SwedenCitation22 and in Norway,Citation34 while a study in the UK found this association only in multiparous women.Citation35 In the study in Norway, the increased risk of CS with duration of residence was found only in specific country-of-origin groups. A Canadian studyCitation36 found no increased risk of unplanned CS with longer duration of residence.
To our knowledge, no study has assessed the role of having had a previous birth in the host country on the risk of delivering by CS. The idea that having a previous birth in the host country could create the conditions for a less stressful pregnancy and labour and may have an influence on birth outcomeCitation37 has been discussed but never tested. We hypothesise that a previous birth in the host country generates greater familiarity with the healthcare system and leads to better communication between women and health professionals. It could modify attitudes and expectations regarding pregnancy, labour and delivery management, for women as well as for health professionals. As the probability of having delivered in the host country increases with time spent in the country, duration of residence must be taken into account to explore our hypothesis and to cast light on the associations between these two variables and caesarean delivery.
We aimed to investigate the role of duration of residence and previous birth in the host country on the risk of delivering by caesarean in a sample of migrant women in France living in emergency housing hotels.
Methods
Data
We used data from the DSAFHIR studyCitation38 (Rights and Health of Housed Migrant and Refugee Women) that investigated health and migration experiences of homeless migrant women housed in hotels as an emergency housing option in the Paris Metropolitan area in France. Since the early 2000s, the demand for emergency housing has increased in the Paris Metropolitan area, driven significantly by individuals and families migrating to France with few or no resources. Migrant families, often living in remote hotels, face obstacles accessing resources and healthcare services. As immigration policies have restricted long-term residence permits, migrant inclusion in public healthcare coverage is hampered, further challenging access to care. The DSAFHIR study was designed to investigate the health needs of women living in these circumstances and the obstacles they face in accessing healthcare services. Data was collected in 2017 and included 469 migrant women. Respondents participated in sexual and reproductive health interventions and a follow-up survey eight months after inclusion to evaluate the interventions. We use here only data collected at inclusion. A convenience sampling based on a two-stage non-random selection was used to select geographical zones and hotels where the women resided. All migrant women aged 18 years or more, housed in the selected hotels, were eligible. A multilingual team of female interviewers spent several days in each hotel and knocked on every hotel room door, inviting all migrant women residents above 18 years to participate. The questionnaire was administered in the respondents’ hotel rooms, in ten different languages.Citation38 Collected data included sociodemographic characteristics, migration trajectories, general, mental and reproductive health, access to healthcare services in France and experience of violence. Compared to migrant women in the general population in France, women in this sample had arrived in France more recently, had a high level of economic deprivation, and more often experienced language barriers and limited access to healthcare.
The outcome variable was mode of delivery, classified into two categories: vaginal delivery and caesarean delivery. Explanatory variables of interest were as follows. Respondents reported their life-long experience of pregnancies and deliveries, indicating mode of delivery, country and year of birth for each past pregnancy. Duration of residence in France at the time of delivery was calculated for each delivery, based on year of birth and year of arrival in France. Experience of a previous birth in France was computed for each delivery, using collected data on country and year of each birth. Available covariates included maternal age at delivery and maternal region of origin. Other relevant covariates (such as disposable income, marital status, medical insurance coverage, administrative status) were available only for the time of data collection and not for each delivery and therefore were not included in the analysis.
Design
In this study, we used deliveries as observations. The clustered nature of deliveries among respondents was taken into account in the analysis. Parity status was defined for each reported delivery: primiparous, multiparous without prior CS, and multiparous with prior CS. As mode of delivery is strongly determined by prior modes of delivery, with higher CS rates for multiparous women with prior CS and lower CS rates for multiparous women with no prior CS, analyses were stratified by parity status.
Population selection
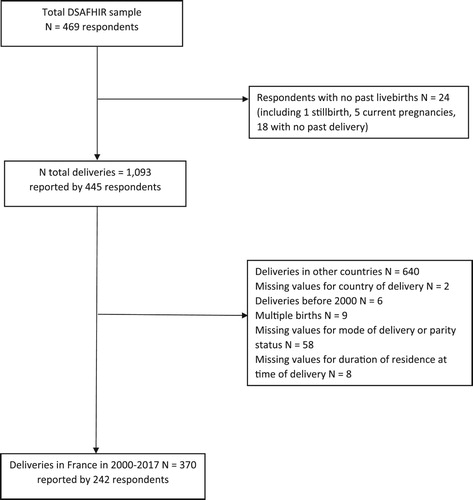
Respondents were asked to provide information about their past deliveries, from their first delivery to the time of data collection in 2017, indicating year and country, mode of delivery and birth outcome for each one. Within the total number of reported deliveries, we included in the analyses only singleton live births that took place in France from 2000 to 2017 (). Multiple births were excluded from the analyses because of their higher CS rate, but singleton births preceding or following multiple births were kept in the analyses. As our objective was to analyse delivery mode in a migration context and in the French healthcare system, deliveries in other countries were excluded from the analyses. Likewise, to limit our focus to recent practices we excluded deliveries taking place before 2000. Deliveries excluded from the analyses as index birth (or observations) were nonetheless taken into account to determine parity status and birth ranks. Due to small numbers, the group of multiparous women with prior CS was not included in the analysis.
Statistical analysis
Chi-squared tests, univariate and multivariate logistic regressions were used to assess the association between duration of residence at the time of delivery, previous delivery in France and mode of delivery, stratifying analyses on parity status. We adjusted for the clustering of deliveries among respondents by computing standard errors allowing for intragroup correlation. Collinearity between duration of residence and prior delivery in France meant that both variables could not be fitted into a single model. We therefore began by testing the association of each variable with mode of delivery separately. Then, to analyse the distinct effects of both variables on mode of delivery, we combined them, creating four categories. As there were very few cases of a prior birth in France with less than two years of residence, we grouped together all the women with a prior delivery in France, which finally resulted in three categories: no prior delivery in France and less than two years of residence, no prior delivery in France and two or more years of residence, and prior delivery in France.
Results
Analyses included 242 respondents and 370 deliveries. Two thirds of the respondents were born in Sub-Saharan Africa. Most of them (73%) migrated to France between 2010 and 2017, and 22% had been in France for less than two years. Almost half of the respondents (48%) cited security concerns for themselves or family members as the reason for migration. While 24% of respondents had no schooling or primary education, 44% completed high school or obtained higher education. Respondents had a diversity of immigration status, although 41% were undocumented (no residence permit) at the time of the survey. While 47% were covered under medical insurance for undocumented people, 7% of our analytical sample had no medical insurance coverage. One third of the sample reported no financial resources at the time of the survey. Most of the deliveries (71%) took place between 2013 and 2017. Among them, 59% of deliveries were in multiparous women with no prior CS. 42% of deliveries occurred within two years after arrival in France, while 72% occurred within four years after arrival. For 37% of deliveries, there had been a prior delivery in France. The overall CS rate was 23% ().
Table 1. Characteristics of respondents and deliveries in France, 2000–2017, DSAFHIR
Stratifying results by parity, we found no association between duration of residence and mode of delivery for the primiparous group (). Duration of residence was associated with mode of delivery only in the multiparous with no prior CS group (p = 0.04), with a CS rate of 16.1% when duration of residence was less than two years, dropping to 7.4% when duration of residence was two or more years. In multivariate analysis, controlling for maternal age and region of origin, caesarean delivery remained more likely with shorter duration of residence (aOR = 2.58; 95% CI = 1.03–6.46). Among the multiparous with no prior CS group, having had a prior delivery in France was associated with mode of delivery: the CS rate was 16.2% when there had been no prior delivery in France, while it dropped to 4.7% when there had been a prior delivery in France (p = 0.008). In multivariate analysis, controlling for maternal age and region of origin, caesarean delivery was more likely with no prior delivery in France (aOR = 4.19; 95% CI = 1.44–12.2).
Table 2. Characteristics associated with caesarean delivery in deliveries with no prior caesarean section (CS) according to parity and prior CS status, deliveries in France 2000–2017, DSAFHIR N = 329 deliveries
When combining duration of residence and prior delivery in France, CS rates were 15.8% and 17.1% when there was no prior delivery in France, regardless of duration of residence and dropped to 4.7% when there had been a prior birth in France (p = 0.03) (). Compared to deliveries with a prior birth in France, deliveries with no prior birth in France were more likely to be by CS with a shorter duration of residence (aOR = 3.99; 95% CI = 1.31–12.1) as well as with a longer duration of residence (aOR = 4.69; 95% CI = 1.23–18.0) (). We also found that a maternal age above 30 years had a higher likelihood of CS compared to maternal age under 25 years (aOR = 4.89; 95% CI = 1.02–23.5), controlling for maternal region of origin, duration of residence and prior birth in France.
Table 3. Characteristics associated with cesarean delivery among multiparous women with no prior CS deliveries in France 2000–2017, DSAFHIR N = 217 deliveries
Discussion
No association was found between duration of residence and CS delivery among the primiparous and multiparous with prior CS groups. We found that giving birth in France for the first time was associated with an increased risk of caesarean delivery among multiparous women with no prior CS, compared with women in the same group who had previously given birth in France. In this group, looking at the combined effect of both duration of residence and prior birth in France, we found that prior birth in France was the main determining factor for caesarean delivery. Indeed, the risk of CS remained high at the first birth in France, regardless of duration of residence.
Multiparous women with no prior CS are a low-risk group for CS in subsequent deliveries as they have already given birth vaginally, with consistently lower CS rates than primiparous or multiparous women with prior CS.Citation28 Our results highlight that the location of the previous birth matters in the likelihood of a subsequent CS in this group of multiparous women with no prior CS.
Contrary to previous studies,Citation22,Citation34,Citation35 we did not find higher CS rates associated with longer duration of residence, in primiparous or in multiparous deliveries. Compared with women who have already given birth vaginally, primiparous women have an overall higher risk of CS, which, in our data, is not mitigated by a shorter or longer duration of residence in France. Respondents in this population were mostly recent arrivals in France compared to migrant women in the general population and, as most deliveries occurred within four years after arrival, we were unable to evaluate the effect of longer length of residence on CS rates. Had we been able to analyse respondents’ childbirth trajectories across a longer timespan after migration, we might see an increase in CS with time (as discussed in the introductory section), accompanying worsened general health status in this vulnerable population with limited resources.
To the limited extent that women are able to opt for caesarean delivery, we could argue that migrant women’s childbirth preferences could be influenced by norms of their country of origin, all the more so if their childbirth experiences took place only before migration. In this respect, women migrating from countries where CS is valued might be more accepting of caesarean delivery.
Previous studies have investigated the effect of acculturation on perinatal outcomes, and showed more adverse birth outcomes in acculturated Hispanic migrant women in the US than in less acculturated women,Citation39,Citation40 with diverging results according to parity status.Citation41 Acculturation refers to the adoption of the cultural norms of knowledge, attitudes and behaviours of the dominant cultureCitation41 and is often defined based on country of birth, language proficiency and duration of residence. In studies in Germany, low levels of acculturation among women with an immigrant background was associated with a lower level of prenatal care utilisation but not with frequency of CS,Citation42,Citation43 decision-to-delivery interval,Citation44 or other obstetric outcomes. Our results point more specifically to a process of acculturation to giving birth in the host country, that translates into a more positive pregnancy outcome. As reported in a qualitative study of migrant women in Portugal,Citation45 having a second birth in the host country implies having previously developed knowledge about the functioning of the healthcare system, and having informed expectations about prenatal care and delivery management. To this extent, we could suggest that having had a prior birth in the host country has rendered the process of giving birth there more familiar and could allow for a less stressful or more empowered pregnancy and delivery.
The reduced likelihood of CS at a second or subsequent birth in the host country may also have to do with perceptions of migrant women by health professionals. It was shown that CS rates vary with non-clinical characteristics of women such as education,Citation35 ethnicity,Citation26 country of birth, and with the organisation of healthcare settings, as evidenced by an increased risk of CS on Fridays (the end of the working week).Citation46 As CS is a treatment decision with a certain degree of clinical discretion,Citation41 perceptions by health professionals of women’s obstetric risks are likely to influence mode of delivery. Having already given birth in the host country and being familiar with the healthcare and delivery environment might act as a signal of lower risk to health professionals.
These results cannot be generalised to all migrant women in France as respondents in this sample have a relatively short duration of residence, experience a great level of economic disadvantage and administrative difficulties, and have no stable or personal housing. Still, respondents in this sample had comparable CS rates to migrant respondents in the French National Perinatal Survey 2010,Citation47 at similar parity status and region of origin, suggesting possibly similar patterns in terms of CS risk.
Strengths and limitations
Without data on clinical factors and past medical history, we could not specify whether caesarean deliveries were planned or emergency CSs, or whether they were medically indicated. As data were self-reported, recall bias is possible but probably limited on our variable of interest, as mode of delivery is a major birth outcome. While access to medical records data would allow for relevant clinical information, it would be impractical to retrieve information from past deliveries in a variety of healthcare settings, especially in a population as mobile as the migrant women in our sample, including across borders. Self-reporting, with its limitations, is the only practical way to collect information on life-long history of pregnancies and conduct analyses on the role of birth location, birth ranks, and perinatal outcomes along the migration path.
To our knowledge, this is the first study measuring the effect of a previous birth in a host country on mode of delivery or any other birth outcomes. As a risk factor for caesarean delivery among multiparous women with no prior CS, it is easily identifiable in clinical practice, and could help draw specific attention to the increased risk of CS among multiparous women giving birth in France for the first time.
It appears particularly important for professionals to recognise the elevated risk of CS when migrant women give birth in France for the first time, even when they have given birth in the country of origin in the past. Avoiding a first CS at this delivery reduces the probability of undergoing CS in subsequent deliveries. Health professionals’ efforts directed at decreasing the CS rate among migrant women should focus on women delivering in the host country for the first time. Recognising it as a moment of increased risk for caesareans might help create the conditions to decrease the risk.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Betran AP, Torloni MR, Zhang J, et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod Health. 21 juin 2015;12:57. doi: 10.1186/s12978-015-0043-6
- WHO. Appropriate technology for birth. Lancet Lond Engl. 24 August 1985;2(8452):436–437.
- World Health Organization Human Reproduction Programme, 10 April 2015. WHO Statement on caesarean section rates. Reprod Health Matters. mai 2015;23(45):149–150. doi: 10.1016/j.rhm.2015.07.007
- Korb D, Goffinet F, Seco A, et al. Risk of severe maternal morbidity associated with cesarean delivery and the role of maternal age: a population-based propensity score analysis. CMAJ. 1 avr 2019;191(13):E352–E360. doi: 10.1503/cmaj.181067
- Deneux-Tharaux C, Carmona E, Bouvier-Colle M-H, et al. Postpartum maternal mortality and cesarean delivery. Obstet Gynecol. sept 2006;108(3 Pt 1):541–548. doi: 10.1097/01.AOG.0000233154.62729.24
- Häger RME, Daltveit AK, Hofoss D, et al. Complications of cesarean deliveries: rates and risk factors. Am J Obstet Gynecol. February 2004;190(2):428–434. doi: 10.1016/j.ajog.2003.08.037
- Chu S, Chen Q, Chen Y, et al. Cesarean section without medical indication and risk of childhood asthma, and attenuation by breastfeeding. PloS One. 2017;12(9):e0184920. doi: 10.1371/journal.pone.0184920
- Almgren M, Schlinzig T, Gomez-Cabrero D, et al. Cesarean delivery and hematopoietic stem cell epigenetics in the newborn infant: implications for future health? Am J Obstet Gynecol. nov 2014;211(5):502.e1–8. doi: 10.1016/j.ajog.2014.05.014
- Blustein J, Liu J. Time to consider the risks of caesarean delivery for long term child health. BMJ. 10 June 2015;350:h2410. doi: 10.1136/bmj.h2410
- Vangen S, Stoltenberg C, Johansen REB, et al. Perinatal complications among ethnic Somalis in Norway. Acta Obstet Gynecol Scand. avr. 2002;81(4):317–322. doi: 10.1034/j.1600-0412.2002.810407.x
- Small R, Gagnon A, Gissler M, et al. Somali women and their pregnancy outcomes postmigration: data from six receiving countries. BJOG Int J Obstet Gynaecol. déc. 2008;115(13):1630–1640. doi: 10.1111/j.1471-0528.2008.01942.x
- G.c O, M.p Z, C F, A.f C, L C, S M. Caratteristiche del puerperio e complicanze nel parto vaginale e nel taglio cesareo. Confronto fra la popolazione italiana e straniera nella casistica 2000-2004 del Policlinico. G Ital Ostet E Ginecol. 2007;12(3):75–81.
- Diani F, Zanconato G, Foschi F, et al. Management of the pregnant immigrant woman in the decade 1992–2001. J Obstet Gynaecol J Inst Obstet Gynaecol. nov 2003;23(6):615–617. doi: 10.1080/01443610310001604367
- Sauvegrain P. La santé maternelle des « Africaines » en Île-de-France : racisation des patientes et trajectoires de soins. Rev Eur Migr Int. 1 juin 2012;28(2):81–100. doi: 10.4000/remi.5902
- Linard M, Deneux-Tharaux C, Luton D, et al. Differential rates of cesarean delivery by maternal geographical origin: a cohort study in France. BMC Pregnancy Childbirth. 27 juin 2019;19(1):217. doi: 10.1186/s12884-019-2364-x
- Forna F, Jamieson DJ, Sanders D, et al. Pregnancy outcomes in foreign-born and US-born women. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. déc. 2003;83(3):257–265. doi: 10.1016/S0020-7292(03)00307-2
- Janevic T, Loftfield E, Savitz DA, et al. Disparities in cesarean delivery by ethnicity and nativity in New York city. Matern Child Health J. janv. 2014;18(1):250–257. doi: 10.1007/s10995-013-1261-6
- Johnson EB, Reed SD, Hitti J, et al. Increased risk of adverse pregnancy outcome among Somali immigrants in Washington state. Am J Obstet Gynecol. août. 2005;193(2):475–482. doi: 10.1016/j.ajog.2004.12.003
- Shah RR, Ray JG, Taback N, et al. Adverse pregnancy outcomes among foreign-born Canadians. J Obstet Gynaecol Can JOGC J Obstet Gynecol Can JOGC. mars 2011;33(3):207–215. doi: 10.1016/S1701-2163(16)34821-6
- von Katterfeld B, Li J, McNamara B, et al. Obstetric profiles of foreign-born women in Western Australia using data linkage, 1998–2006. Aust N Z J Obstet Gynaecol. juin 2011;51(3):225–232. doi: 10.1111/j.1479-828X.2010.01282.x
- Maslovitz S, Kupferminc MJ, Lessing JB, et al. Perinatal outcome among non-residents in Israel. Isr Med Assoc J IMAJ. mai. 2005;7(5):315–319.
- Juárez SP, Small R, Hjern A, et al. Length of residence and caesarean section in migrant women in Sweden: a population-based study. Eur J Public Health. 01 2018;28(6):1073–1079. doi: 10.1093/eurpub/cky074
- Minsart A-F, De Spiegelaere M, Englert Y, et al. Classification of cesarean sections among immigrants in Belgium. Acta Obstet Gynecol Scand. févr. 2013;92(2):204–209. doi: 10.1111/aogs.12003
- Bakken KS, Skjeldal OH, Stray-Pedersen B. Higher risk for adverse obstetric outcomes among immigrants of African and Asian descent: a comparison study at a low-risk maternity hospital in Norway. Birth Berkeley Calif. juin. 2015;42(2):132–140. doi: 10.1111/birt.12165
- Råssjö EB, Byrskog U, Samir R, et al. Somali women’s use of maternity health services and the outcome of their pregnancies: a descriptive study comparing Somali immigrants with native-born Swedish women. Sex Reprod Healthc Off J Swed Assoc Midwives. oct 2013;4(3):99–106. doi: 10.1016/j.srhc.2013.06.001
- Edmonds JK, Hawkins SS, Cohen BB. The influence of detailed maternal ethnicity on cesarean delivery: findings from the U. S. Birth Certificate in the State of Massachusetts. Birth. 2014;41(3):290–298. doi: 10.1111/birt.12108
- Getahun D, Strickland D, Lawrence JM, et al. Racial and ethnic disparities in the trends in primary cesarean delivery based on indications. Am J Obstet Gynecol. 1 oct 2009;201(4):422.e1–422.e7. doi: 10.1016/j.ajog.2009.07.062
- Guihard P, Blondel B. Trends in risk factors for caesarean sections in France between 1981 and 1995: lessons for reducing the rates in the future. BJOG Int J Obstet Gynaecol. janv. 2001;108(1):48–55. doi: 10.1111/j.1471-0528.2001.00009.x
- Carolan M. Pregnancy health status of sub-Saharan refugee women who have resettled in developed countries: a review of the literature. Midwifery. août. 2010;26(4):407–414. doi: 10.1016/j.midw.2008.11.002
- Merry L, Semenic S, Gyorkos TW, et al. International migration as a determinant of emergency caesarean. Women Birth J Aust Coll Midwives. oct 2016;29(5):e89–e98. doi: 10.1016/j.wombi.2016.04.001
- Gagnon AJ, Zimbeck M, Zeitlin J, et al. Migration to western industrialised countries and perinatal health: a systematic review. Soc Sci Med 1982. sept 2009;69(6):934–946.
- Essén B, Bödker B, Sjöberg NO, et al. Are some perinatal deaths in immigrant groups linked to suboptimal perinatal care services? BJOG Int J Obstet Gynaecol. juin. 2002;109(6):677–682. doi: 10.1111/j.1471-0528.2002.01077.x
- Marmot MG, Adelstein AM, Bulusu L. Lessons from the study of immigrant mortality. Lancet Lond Engl. 30 juin 1984;1(8392):1455–1457.
- Sørbye IK, Daltveit AK, Sundby J, et al. Caesarean section by immigrants’ length of residence in Norway: a population-based study. Eur J Public Health. févr. 2015;25(1):78–84. doi: 10.1093/eurpub/cku135
- Essex HN, Green J, Baston H, et al. Which women are at an increased risk of a caesarean section or an instrumental vaginal birth in the UK: an exploration within the Millennium Cohort study. BJOG Int J Obstet Gynaecol. mai. 2013;120(6):732–742 ; discussion 742–743. doi: 10.1111/1471-0528.12177
- Gagnon AJ, Van Hulst A, Merry L, et al. Cesarean section rate differences by migration indicators. Arch Gynecol Obstet. avr. 2013;287(4):633–639. doi: 10.1007/s00404-012-2609-7
- Merry L, Vangen S, Small R. Caesarean births among migrant women in high-income countries. Best Pract Res Clin Obstet Gynaecol. avr. 2016;32:88–99. doi: 10.1016/j.bpobgyn.2015.09.002
- Poncet L, Andro A, Eberhard M, et al. Investigating and improving access to reproductive healthcare for vulnerable migrant women in France. Soc Sci Protoc. 15 déc 2019;2:1–13. doi: 10.7565/ssp.2019.2672
- Singh GK, Yu SM. Adverse pregnancy outcomes: differences between US- and foreign-born women in major US racial and ethnic groups. Am J Public Health. 1 juin 1996;86(6):837–843. doi: 10.2105/AJPH.86.6.837
- Giuntella O. Assimilation and health: evidence from Linked birth records of second- and third-Generation Hispanics. Demography. 2016;53(6):1979–2004. doi: 10.1007/s13524-016-0522-6
- Zlot AI, Jackson DJ, Korenbrot C. Association of acculturation with cesarean section among Latinas. Matern Child Health J. mars. 2005;9(1):11–20. doi: 10.1007/s10995-005-2447-3
- David M, Borde T, Brenne S, et al. Caesarean section frequency among Immigrants, second- and third-Generation women, and Non-Immigrants: prospective study in Berlin/Germany. PloS One. 2015;10(5):e0127489. doi: 10.1371/journal.pone.0127489
- David M, Borde T, Brenne S, et al. Obstetric care quality indicators and outcomes based on the degree of acculturation of immigrants-results from a cross-sectional study in Berlin. Arch Gynecol Obstet. 2018;297(2):313–322. doi: 10.1007/s00404-017-4574-7
- David M, Scherer KA, Henrich W, et al. Does an immigrant background affect the indication, incidence or outcome of emergency cesarean section? Results Prospective Data Collect 111 Births. Geburtshilfe Frauenheilkd. févr 2018;78(2):167–172.
- Almeida LM, Caldas JP, Ayres-de-Campos D, et al. Assessing maternal healthcare inequities among migrants: a qualitative study. Cad Saude Publica. févr. 2014;30(2):333–340. doi: 10.1590/0102-311X00060513
- Gagnon AJ, Merry L, Haase K. Predictors of emergency cesarean delivery among international migrant women in Canada. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. juin 2013;121(3):270–274. doi: 10.1016/j.ijgo.2012.12.017
- DREES, Ministère de la Santé, ADISP. Enquête Nationale Périnatale; 2010.