Abstract
The Government of India has promoted the expansion of access to and uptake of intrauterine devices (IUDs), during both the interval (IIUD) and postpartum (PPIUD) periods, as part of its Family Planning 2020 initiative. This study, conducted by EngenderHealth as part of the Expanding Access to IUD Services in India project, examines IIUD and PPIUD continuation rates over time and investigates factors associated with IUD continuation. We recruited respondents (N = 5024) through a repeated cross-sectional household study between February and December 2019. We identified respondents using IUD client data from public health facility registers in 20 districts of Gujarat and Rajasthan. We compared continuation rates for IIUD and PPIUD adopters and used regression analyses to measure the association between continuation and demographic, quality of care, and counselling variables. IIUD continuation rates decreased from 85.6% to 78.3% and PPIUD rates decreased from 78.5% to 70.7% between month 3 and month 12. Clients experiencing side effects or other problems were 15 times more likely to discontinue IUD use than clients who did not. Clients who received IUD counselling prior to insertion were more likely to continue than those who did not. IUD continuation increased significantly in cases where both partners jointly selected the method compared to situations where women decided alone. Several sociodemographic factors were associated with continuation. Our study demonstrates the value and benefits of programmes offering IUD services emphasising quality counselling and client-centred care to increase access, uptake, and continuation.
Résumé
Dans le cadre de son initiative de planification familiale de 2020, le Gouvernement indien a encouragé l’expansion de l’accès aux dispositifs intra-utérins (DIU) et leur emploi pendant les périodes d’intervalle et du postpartum. Cette étude, réalisée par EngenderHealth, dans le cadre du projet d’élargissement de l’accès aux services de DIU en Inde, examine les taux de continuité de l’emploi du DIU dans les périodes d’intervalle et du postpartum au fil de temps et s’intéresse aux facteurs associés à la continuité de l’emploi du DIU. Nous avons recruté les répondantes (n = 5024) au moyen d’une étude transversale auprès des ménages répétée entre février et décembre 2019. Nous avons identifié les répondantes en utilisant les données sur les clientes des DIU tirées des registres des centres de santé publique de 20 districts du Gujarat et du Rajasthan. Nous avons comparé les taux de continuité de l’emploi des DIU pour les femmes ayant adopté le DIU pendant la période d’intervalle ou du postpartum et utilisé des analyses de régression pour mesurer l’association entre la continuité et les caractéristiques démographiques, la qualité des soins et les variables du conseil. Les taux de continuité de l’emploi du DIU pendant la période d’intervalle ont reculé de 85.6% à 78.3% alors que les taux pendant le postpartum passaient de 78.5% à 70.7% entre le 3e et le 12e mois. Les clientes présentant des effets secondaires ou d’autres problèmes avaient 15 fois plus de probabilités de cesser d’utiliser le DIU que les autres clientes. Les clientes qui avaient été conseillées sur le DIU avant sa pose avaient plus de chances de garder cette méthode. La continuité de l’emploi du DIU a augmenté sensiblement lorsque les deux partenaires ont sélectionné conjointement cette contraception, par comparaison aux cas où les femmes ont décidé seules. Plusieurs facteurs sociodémographiques étaient associés à la continuité de l’emploi. Notre étude démontre l’utilité et les avantages des programmes proposant des services de DIU qui mettent l’accent sur des conseils de qualité et des soins centrés sur les clientes pour augmenter l’accès, l’utilisation et la continuité de l’emploi.
Resumen
El Gobierno de India ha promovido la ampliación de la accesibilidad y aceptación de dispositivos intrauterinos (DIU), durante los períodos de intervalo (DIUI) y posparto (DIUPP), como parte de su iniciativa de Planificación Familiar 2020. Este estudio realizado por EngenderHealth, como parte del proyecto Ampliación del Acceso a Servicios de DIU en India, examina las tasas de continuación de DIUI y DIUPP con el paso del tiempo e investiga los factores asociados con la continuación del DIU. Reclutamos a informantes (N = 5024) por medio de un estudio domiciliario transversal entre febrero y diciembre de 2019. Identificamos a las informantes utilizando datos de usuarias de DIU provenientes de registros de establecimientos de salud pública en 20 distritos de Gujarat y Rajasthan. Comparamos las tasas de continuación de personas que adoptaron el DIUI y DIUPP, y utilizamos análisis de regresión para medir la asociación entre la continuación y las variables de demografía, calidad de la atención y consejería. Las tasas de continuación del DIUI disminuyeron del 85.6% al 78.3% y las tasas del DIUPP disminuyeron del 78.5% al 70.7% entre el tercer mes y el duodécimo mes. Las usuarias que presentaron efectos secundarios u otros problemas eran 15 veces más propensas a descontinuar el uso del DIU que las usuarias que no los presentaron. Las usuarias que recibieron consejería sobre el DIU antes de la colocación eran más propensas a continuar que las que no la recibieron. La continuación del DIU aumentó significativamente en casos en que ambas parejas seleccionaron el método conjuntamente, en comparación con situaciones en que las mujeres decidieron solas. Varios factores sociodemográficos estaban asociados con la continuación. Nuestro estudio demuestra el valor y los beneficios de programas que ofrecen servicios de DIU y hace hincapié en brindar consejería de calidad y atención centrada en la usuaria para ampliar el acceso, la aceptación y la continuación.
Introduction
India has seen a remarkable decline in maternal mortality over the past two decades, from 540 to 113 maternal deaths per 100,000 live births during the period 1999–2017. Evidence suggests that this decline may be due in part to improved delivery of maternal healthcare initiatives.Citation1 Despite these gains, the modern contraceptive prevalence rate over that same period witnessed a marginal decline (from 48.5% in 1999 to 47.7% in 2017) and one in eight women of reproductive age in India report an unmet need for modern contraceptive methods.Citation2 Disparities in contraceptive access and use are even greater for rural, impoverished, and uneducated populations within the country.Citation3,Citation4
Among currently married Indian women ages 15–49, female sterilisation remains the most popular modern contraceptive method (used by 36% of clients), followed by male condoms (6%), and oral contraceptives (4%). The use of long-acting reversible contraceptives remains particularly low, with only 1.5% of currently married women using an intrauterine device (IUD).Citation5 Since 2009, the national and state governments have worked continuously to increase access to high-quality IUD services in the country. IUDs provide long-term contraceptive protection and can be inserted easily at any time including during the postpartum and postabortion periods.Citation6 However, evidence from one study in India suggests that clients who choose IUDs may immediately discontinue if they experience the slightest sign of side effects, due to fears of additional discomfort or longer-term health effects.Citation7 Indeed, IUD continuation rates have varied in India, with evidence suggesting that between 15% and 25% of IUD users discontinue a method in the first 12 months of use, and that factors such as side effects, reduced need, opposition from the woman’s family, education, and/or wealth contribute to this.Citation8,Citation9 The fourth round of the National Family Health Survey estimated that 26% of IUD users discontinued use within a year of initiation.Citation5 Furthermore, additional evidence illustrates that Indian women are less aware of IUDs compared to other modern methods, and myths and misconceptions related to IUD side effects are high.Citation10,Citation11 As the country moves towards its goal of universal health care, the importance of quality sexual and reproductive health services becomes even more important.
In addition to knowledge of and personal beliefs about modern methods, access to and quality of care can influence a client’s choice of contraceptive method. Clients who receive higher quality of care are more likely to adopt and continue using modern contraception.Citation12,Citation13 The availability of contraceptive counselling, as well as the quality of that counselling, can also affect method choice and continuation. In India in particular, high-quality counselling has demonstrated a positive association with modern contraceptive use and continuation.Citation13 While this highlights the importance of high-quality counselling for acceptance of modern contraceptives, it does not differentiate between types of methods, limiting our understanding of the relationship between quality of care and IUD uptake and continuation specifically.
Traditionally, providers have offered IUDs to clients during the extended postpartum or interval period (defined by the Indian Ministry of Health guidelines as insertion occurring any time after six weeks postpartum). Since the active promotion of postpartum IUD (PPIUD) insertion, as part of the Family Planning 2020 initiative in 2010, the Government of India has advocated for the expansion of access to and uptake of IUDs during the immediate postpartum period (defined as either within 48 hours of placental delivery or during a caesarean delivery).Citation14 While IUDs were introduced in the 1970s in India, PPIUDs was not routinely implemented across the country. Scale-up was also affected by developments in contraceptive technology, changes in the national policies and World Health Organization (WHO) recommendations, and a lack of global standardised PPIUD materials. Subsequently, the PPIUD programme was only implemented at scale as of 2010.
There are several advantages associated with PPIUDs, including the reduced frequency of visits to health facilities required for clients and the cost savings for public health programmes related to service integration with maternal health care. However, the physiological status of clients during the postpartum period differs from during the interval period, and this can affect the client’s experience with the method as well as continuation rates.Citation15 There is little evidence about both the continuation patterns of interval IUD (IIUD) and PPIUD users and the demographic and health service factors that may affect IUD use.
Current evidence from India addresses determinants of general family planning uptake and continuation, with most literature focusing on sociodemographic information. There is less focus on other potential correlates, such as quality of care, side effects, experience of problems post-insertion or the importance of follow-up. Furthermore, evidence has not focused on PPIUD continuation and how the timing of the insertion procedure may affect this, as well as other elements such as PPIUD decision-making and quality of care. Although the national scale-up of PPIUD in India is relatively recent, 2.54 million women adopted IUD in the post-partum period during 2019-20, comprising approximately 45% of total IUD insertions. This paper provides novel and unique evidence that can be used nationally and beyond to understand potential factors associated with IUD voluntary uptake and continuation.
This study examined continuation rates for IIUD and PPIUD users over time and analysed the impact of contraceptive counselling and service quality on IUD continuation in India. Findings can inform improvements in providers’ clinical and counselling skills and help create other interventions to ensure high-quality services for contraceptive clients.
Methods
Intervention
EngenderHealth conducted this research study as part of the Expanding Access to IUD Services in India (EAISI) project, a technical assistance intervention operating in Gujarat and Rajasthan states. The main goal of the project was to expand access to and availability of quality IUD services by strengthening family planning counselling and clinical service provision. The project worked on strengthening services during (1) postpartum, (2) postabortion, and (3) interval. The project provided quality comprehensive training on IUD which included clinical skills in insertion and removal; infection prevention and control; counselling skills for ensuring informed voluntary decision-making; and orientation on rights and choices. This was accomplished through on-the-job training followed by intensive and regular periodic supportive supervision visits by the project’s clinical training team. There was an emphasis on building skills of providers through observed and supervised hands-on practice on clients. While the project aimed to ensure the availability of high-quality IUD services, the core principle of the intervention was to ensure informed voluntary decision-making by strengthening family planning counselling services. Specifically, these provider-training activities included: building a rapport with clients, understanding the client’s requirements and family situation, informed choice, ensuring the availability of a range of contraceptives, and helping the client implement her decision. This was complemented with the availability of job aids and separate counselling spaces in facilities with adequate privacy to improve the effectiveness of counselling. In addition to the capacity building of providers at the facility level, the project undertook health system strengthening activities such as building the capacity of health managers for supportive supervision, helping providers use data for decision-making, and ensuring availability of supplies and equipment and budgets for these activities.
The project began in 2014 and operated in 50 districts (25 districts in Gujarat and 25 districts in Rajasthan) until March 2017. In April 2017, the project expanded to cover all high caseload public health facilities in every district in both states (33 districts in Rajasthan and 33 districts in Gujarat) in order to maximise coverage. We also conducted advocacy activities in both states to create a positive enabling environment to complement the provider-focused activities.
Study population
The study population included IIUD and PPIUD clients who adopted an IUD from an EngenderHealth-supported intervention facility. Clients who received an IUD after receiving postabortion care were not included in the study because the research team did not have access to the registers for these clients.
Study design and sampling
The research team randomly selected the sample from 10 districts in Rajasthan and 10 from Gujarat. We purposively selected the 20 districts to ensure an adequate representation of regions and varying performance levels, as measured by the caseload of IUD clients. The research team also selected districts that the Government of India designated as priority areas.
The study employed a repeated cross-sectional design to obtain data from clients, using retrospective client data from registers available at all the intervention health facilities located in the selected districts. Due to the low number of eligible IUD clients available from intervention facilities, coupled with high unavailability and non-response rates of clients at the time of the survey, we collected data over two rounds (February–March and November–December 2019). In the first round, the sampling frame comprised clients who obtained an IUD in the preceding 3 or 6 months; in the second round, the sampling frame included clients who had obtained an IUD in the previous 3, 6, or 12 months. To identify potential respondents, the research team used client information from the Indian health management information system, which included registers of IIUD and PPIUD clients. The register provided key information, including client names, dates of birth, methods adopted, and village locations.
Sample size
We designed the sample size to estimate discontinuation and other client satisfaction rates with an 80% power and precision of ±5% at a 95% level of significance (deff = 2). As there was little evidence of discontinuation rates at the time of the study, the study team assumed that these rates were 50%, which requires the highest sample size. We inflated the sample size by 25% to account for non-response and non-availability, for a total sample size of 4902. To obtain this, the research team employed a quota sample to collect data from 50 women per district, per time point.
Training and fieldwork
Data collection teams, comprising 30 investigators and 10 supervisors, completed a three-day training focused on administering the questionnaire and sampling procedures. The team supervisor reviewed all questionnaires and conducted spot checks for at least 20% of all households. We retained the data collection teams for each survey wave. We used Microsoft Access software for data entry and validation.
Data collection and measures
We identified villages for data collection using the register. Trained interviewers travelled to the selected villages and contacted local community health workers to help identify households. The interviewer then contacted clients at their homes, explained the purpose of the study, and obtained verbal consent from those interested in participating. Interviewers assured clients that their responses would be confidential and explained that they had the option to end the interview at any time. Interviewers also took care to conduct interviews in private settings that ensured auditory and visual privacy for the participant. In cases where the eligible client was not at home at the time of the first visit, interviewers completed up to three additional attempts during the same day to complete the interview.
The interviewers used a structured, paper-based questionnaire to collect data during the interviews. The research team designed the survey questionnaire in English and then translated the instrument into Hindi and Gujarati. The survey instrument collected demographic and IUD continuation information. Interviewers also asked respondents to recall information related to the quality of services provided when they adopted their IUDs, including details regarding the availability and quality of provider counselling and their satisfaction with the services provided. We field-tested all data collection tools prior to launching the survey. Each interview required approximately 45 minutes to complete.
The research team completed the first round of data collection in February–March 2019 and the second round in November–December 2019.
Data analysis and variables
The research team tabulated frequencies for key variables, including demographic characteristics (age, parity, education, etc.), service quality (including counselling services), satisfaction with services (staff behaviour, timeliness, cost, etc.), follow-up visits, and decision-making. We conducted chi-square analyses for key comparisons (such as continuation rates) and determined differences to be significant at p < 0.05.
We used multivariate logistic regression to study the association of the demographic characteristics, service quality, satisfaction with services, follow-up visits, and decision-making on IUD continuation. We classified clients who still had their IUDs at the time of their interviews as “continuers”, and clients who had their IUDs removed or whose IUDs were naturally expelledFootnote* at any point prior to the interview as “discontinuers”. Given the overlapping nature of some of our independent variables, we assessed the multivariate model for multicollinearity between all independent variables in the model so that we could identify sets of variables that had linear associations. We removed variables that had a correlation coefficient with another predictor that was greater than 0.5. Association between IUD continuation and a number of other dependent variables are presented, while controlling for potential confounders, including age, educational attainment, marital status, parity, and number of living children. Adjusted odds ratios (AORs), p-values and 95% confidence intervals (CIs) from the logistic regression analyses are reported. We analysed data using SPSS version 13.
Ethical considerations
The Center for Media Studies, Institutional Review Board, New Delhi approved the project and all accompanying materials (Reference: IRB00006230; date of approval: 10 January 2019). We obtained verbal informed consent from all participants prior to enrolment; due to low literacy rates, interviewers could not obtain written consent.
Results
Demographic characteristics and IUD continuation rates
The final sample included 5024 respondents, of which 20% (N = 1012) adopted an IUD during the extended postpartum or interval period and 80% (N = 4012) adopted an IUD immediately postpartum. The mean age of the total sample was 25.6 years and 42.1% of respondents had no education or primary education only. The majority of respondents (83.4%) were homemakers. Respondents had an average of two living children. Most respondents (61.1%) received their IUD from a community health centre. Approximately half of all respondents (55.1%) had used a different family planning method before choosing an IUD.
IIUD respondents were slightly more educated than PPIUD respondents. For example, 14.9% of IIUD clients had no schooling compared to 25.4% of PPIUD respondents. IIUD clients were also more likely than PPIUD respondents to have used a contraceptive method prior to adopting an IUD (65.3% and 52.6%, respectively) ().
Table 1. Demographic characteristics and IUD behaviours of respondents
IUD continuation rates and reasons for discontinuation
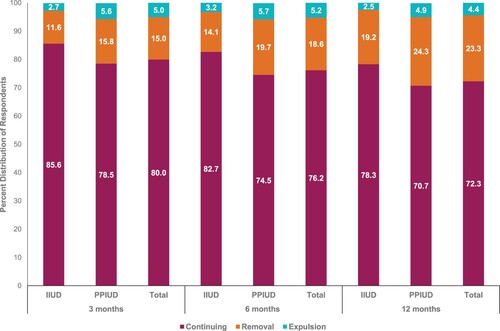
Continuation rates for both IIUD and PPIUD respondents declined steadily at 3, 6, and 12 months post-insertion (see ). Among IIUD respondents, continuation rates decreased from 85.6% at 3 months to 82.7% at 6 months and 78.3% at 12 months, and removal rates increased significantly between 3 months (11.6%) and 12 months (19.2%). Expulsion rates for IIUD clients remained fairly steady during this period (∼3%). Among PPIUD clients, continuation rates decreased from 78.5% at 3 months to 74.5% at 6 months and 70.7% at 12 months. Expulsion rates were highest at 6 months and significantly higher among PPIUD clients than IIUD clients in the same period (5.7% and 3.2%, respectively). IIUD respondents were significantly more likely to continue than PPIUD respondents (83% versus 75%, p < 0.001) (data not shown).
Among respondents who reported IUD removal, the majority (47.7%) did so within the first two months of insertion, after which the next highest rate of removal was at five months or beyond (35.9%) (see ). Side effects (including irregular periods, lower abdominal pain, excessive bleeding, vaginal discharge, and/or problems during intercourse) were the most commonly cited reason for IUD removal for both PPIUD respondents (83.3%) and IIUD respondents (87.4%). Respondents less commonly cited opposition from spouses or other family members (9.2%) or a desire to conceive (8.4%) as reasons for IUD removal. The majority of respondents who removed their IUD did so at the same facility at which they received the method (86.0% of IIUD respondents and 79.5% of PPIUD respondents).
Table 2. Timing of and reason for IUD removal
Current contraceptive use and pregnancy rates among IUD discontinuers
Among respondents who discontinued (either through removal or expulsion), 42.7% reported using another method of contraception at the time of the interview, while more than 4% were pregnant at the time of interview (see ). A larger proportion of IIUD discontinuers (48.8%) reported current method use than PPIUD discontinuers (41.7%). The most common form of new method among discontinuers was condoms (41.7%), followed by female sterilisation (38.7%), and oral contraceptives (11.5%). Older and higher parity clients were more likely to switch to female sterilisation than younger and lower parity respondents (data not shown).
Table 3. Pregnancy and contraceptive use among IUD discontinuers
Counselling and satisfaction with and quality of care
Interviewers asked respondents a series of questions related to the quality of IUD care and their satisfaction with services (see ).
Table 4. Quality of care and client satisfaction
Regarding the timing of counselling, women received counselling typically at multiple time points, such as during antenatal care (68.4%), while being admitted at the facility for delivery (43.5%), or/and after delivery (55.8%).
The majority reported receiving information about the method from their provider prior to insertion (89.5%), providers explaining what to do if side effects occurred (84.8%), and providers asking them to return for a follow-up visit (83.3%). PPIUD respondents responded less favourably than IIUD respondents across all of the quality of care indicators; this was most notable with regard to warnings about side effects (75.0% and 84.2%, respectively).
Overall satisfaction with IUD services was extremely high (96.5%), with almost all respondents reporting they would visit the same facility for other services (97.7%), recommend the facility to others (97.1%), and recommend IUDs to other women (90.2%). Interviewers asked respondents who reported satisfaction to name the aspects of services with which they were satisfied; respondents most commonly cited staff behaviour (66.8%), timeliness of services (54.3%), availability of medicines (53.1%), and counselling services provided (46.3%).Footnote† There were few differences across IIUD and PPIUD respondents for these indicators.
Logistic regression for continuation
There are a number of variables associated with IUD continuation (see ). The research team identified several quality of care variables associated with IUD continuation. Respondents who received counselling on method used prior to insertion were twice as likely to continue IUD use compared to respondents who did not receive counselling (AOR: 2.01, CI: 1.24–3.26, p < 0.001). Other quality of care indicators, like being counselled about side effects, asked to return for follow-up care and women’s perception that the conversation would remain confidential, did not have a statistically significant association with IUD continuation. We examined the overlapping relationship of these four qualities of care indicators on continuation in separate logistic regression models (tables not shown). In these analyses, the counselling about IUD still emerges as the most significant predictor of continuation. The overlap of the other three quality of care variables did not have a significant impact on continuation. However, the overlap of counselling about IUCD with the other three quality of care variables seemed to increase the effect-size on continuation marginally compared with women only being counselled about IUD and not the other three.
Table 5. Adjusted odds ratio (AOR) from multivariate logistic regression analyses
Respondents who were satisfied with services were also 2.5 times more likely to continue IUD use compared to those who were not satisfied (AOR: 2.51, CI: 1.67–3.76, p < 0.001). Respondents who experienced problems after insertion (problems defined as side effects, complications, or method dissatisfaction) were 15.77 times more likely to discontinue IUD use compared to respondents who did not experience problems (AOR: 15.77, CI:12.71–19.56, p < 0.001).
Factors related to IUD decision-making, insertion timing, and history of family planning use also correlated with continuation. Respondents who decided with their spouses to adopt an IUD were significantly more likely to continue IUD use compared to respondents who decided on their own (AOR: 1.33, CI: 1.06–1.66, p < 0.05); no other combination of decision-making was associated with continuation. IIUD respondents were significantly more likely to continue IUD use than PPIUD respondents (AOR: 1.36, CI: 1.09–1.71, p < 0.01). Respondents who obtained IUDs from community health centres were more likely to continue than respondents who obtained their IUDs from other types of facilities (AOR: 1.22, CI: 1.01–1.48, p < 0.05). Respondents who had previously used another family planning method were also significantly more likely to continue IUD use than those with no prior history of contraception (AOR: 1.32, CI: 1.11–1.56, p < 0.001).
There were no significant associations between age or occupation with IUD continuation. However, the likelihood of IUD continuation increased incrementally as a client’s educational level increased; respondents with the highest educational attainment were significantly more likely to continue IUD use than those with no education (AOR: 1.63, CI: 1.10–2.41, p < 0.01). Respondents with three, four, or more children were significantly less likely to continue IUD use than those with only one child. This decrease in continuation at higher parities is significantly associated with women switching to female sterilisation (data not shown).
Discussion
IUD uptake and continuation has been a priority of India’s Ministry of Health and Family Welfare for more than a decade; however, IUD use remains low relative to other methods, namely condoms and female sterilisation. This study revealed a number of important associations related to IUD continuation in the context of poor, rural areas of India, as represented by samples from Gujarat and Rajasthan. Key factors identified include the quality of care, problems experienced after insertion, decision-making roles, timing of insertion, and history of prior contraceptive use. We also identified several demographic characteristics associated with IUD continuation, including education and parity. We explored how these findings are associated within the context of India and are supported by other evidence.
Respondents who received IUDs from community health centres were more likely to continue IUD use. The availability of services closer to the community (in lower-level facilities) may translate to increased care-seeking behaviours for side effects, which could improve method continuation. This indicates a need to expand IUD services to lower levels of the health system, nearer to clients, in order to improve access to quality contraceptive services and enhance continuation of methods.
The most common reason for IUD removal that we found in this study was side effects, resulting in a 15-fold increased likelihood of method discontinuation. While side effects are not uncommon, clients’ inadequate knowledge of what to expect and how to manage such side effects may result in the removal of an IUD within the first few months.Citation16 Furthermore, ingrained myths related to side effects may also contribute to discontinuation. Studies on IUD acceptability in India reveal misconceptions about long-term effects, including common beliefs that side effects are signs of more grave threats such as infertility, cancer, or permanent disfiguration.Citation10 Clients experiencing side effects are more likely to seek guidance from family members or friends, who tend to propagate misconceptions that contribute to discontinuation.Citation11,Citation17 As a result, women may reflexively discontinue the method rather than seek further medical consultation.Citation18 These findings highlight the importance of follow-up care for clients, as these visits are opportunities for trained providers to address possible problems and counsel clients. The importance of counselling clients about potential side effects and approaches for managing side effects at the time of insertion is crucial. The findings also suggest that providers continue to play a crucial role. The focus of this project was to improve the quality of services, including provider counselling and attitudes, with a view to tackling the myths influencing clients. Provider training may be one important element to overcome a client’s negative attitudes and misconceptions.
IUD continuation was positively associated with quality of care, including counselling. These findings are in line with other research that demonstrates that respectful counselling and client satisfaction with services can improve family planning uptake and continuation.Citation19 Quality counselling is particularly important for preserving clients’ rights and choice of contraception and supporting method continuation. This study found that discontinuation was significantly associated with transient side effects related to the method, such as menstruation-related issues and managing the side effects. Quality counselling can help address these concerns, through the provision of correct and sufficient information, a range of contraceptive options and counselling spouses as well. Quality counselling also emphasises return to the facility at 6 weeks for the clinical examination which can address problems faced by women and allay any concerns.Citation13,Citation20
In India specifically, client-centred approaches to quality counselling have shown promise for modern method uptake and continuation.Citation21 This study found that IIUD respondents were more likely to continue IUD use than PPIUD respondents; this trend is supported by other studies.Citation22 The authors suggest that the higher continuation rates among IIUD users may be due to several reasons. They could be related to the timing of the counselling: PPFP counselling is conducted during the ANC period, when the client is in early labour or in the post-partum period within 48 hours, when the client is able to take a decision with informed choice. However, while PPIUD clients adopt their IUDs during the 48-hour period, interval clients make their decision 6 weeks after the delivery. Thus, these clients may have had more time to reflect on their method of choice or be more motivated to adopt a method since they are likely to have returned to a facility for the contraceptive. We also recognise that clients may receive counselling services at various touchpoints, including within the community or through routine facility visits prior to the delivery, and thus may be more comfortable to wait to adopt their method. Interval IUD clients may also be more motivated to continue with the method and hence able to seek care and manage the side effects better, resulting in better continuation. Further research would benefit from addressing reasons for greater continuation among IIUD clients.
Furthermore, higher expulsion rates among postpartum women may also contribute to lower continuation rates for PPIUD clients compared to IIUD clients.Citation15 Some postpartum women may fail to notice an expulsion, which can increase the chance of an unintended pregnancy; this highlights the additional importance of follow-up care for PPIUD clients. While follow-up care may improve continuation rates, particularly for women with expelled IUDs, the evidence related to the impact of follow-up visits on long-term continuation is mixed. Most studies show that follow-up visits are helpful for the overall well-being of the client and provide critical opportunities for treating complications, such as infections, and identifying involuntary removal through expulsion; however, follow-up visits have not been consistently associated with IUD continuation.Citation8,Citation23
Respondents in this study were more likely to continue IUD use if they made the decision with their partners. Furthermore, nearly 10% of discontinuers said they did so because their spouse or other family members opposed the method. This result confirms the importance of spousal support for contraceptive use, echoed by numerous studies from India and other contexts.Citation24–27 Further, clients who experience side effects may benefit from having their partners’ support and encouragement for continuation, which may lead to longer-term method use.Citation28 In India, men play a dominant role in family planning decision-making and may control women’s access to and use of methods, particularly in rural contexts;Citation29 therefore, involving men in family planning interventions could lead to improvements in method uptake and continuation.Citation30
Of all IUD discontinuers in our study, 42.7% had switched to another family planning method (40.4% adopted a modern contraceptive method). More than 50% of the discontinuers adopted a short-term method (specifically condoms or oral contraceptives). The finding that 52.9% of IUD discontinuers failed to adopt another method indicates the importance of improving counselling after discontinuation to prevent unwanted pregnancies and unsafe abortions. Around the world, unsafe abortion is the leading contributor to maternal morbidity and mortality, especially in low-resource, rural areas.Citation31 Improving uptake and continuation of long-acting reversible contraceptives among clients who wish to space births could help protect these clients from experiencing unwanted pregnancies and subsequent terminations, which, if completed unsafely, could result in morbidities and mortalities.
A number of studies undertaken in the past have recorded instances of IUDs being inserted without seeking client consent, especially in the post-partum period.Citation32 Skewed power dynamics between rural clients and providers have been described as contributing to involuntary or coercive methods for getting women to adopt family planning methods, especially IUD and female sterilisation. However, this research provides evidence to suggest that coercive practices might not be present in current public sector facility settings.
IUD clients have attributed specific advantages to having chosen IUDs. Women chose to have an IUD as it was described as a long-lasting method, reversible, easily accessible and free in government facilities, and perceived to be safe and effective. We also have data to suggest that approximately 85% of clients received information on the method, about possible side effects and the importance of follow-up visits, and clients perceived that the conversation would remain confidential. Government facilities also perform a large number of IUD removals, substantiating the adherence to client choices. Of approximately 292,000 IUD insertions done in intervention facilities over a two-year period (2018–2020), about 52,000 clients returned to the facility for follow-up, of which 11,000 clients had the IUD removed. The data from this research study shows that 61.1% of the women were counselled about IUD during the ANC period and another 40% were told about the method in the early labour period. These data seem to suggest that women have taken a conscious decision to adopt IUD after taking into consideration the pros and cons of the method. The high rates of continuation also corroborate the voluntary choice of women to adopt IUD. The conscious and informed decision of clients to adopt IUD and the subsequent satisfaction levels have also been corroborated in more recent literature.Citation33–35
These findings should be viewed in light of their limitations. As with any interviewer-administered survey, this study may be subject to social desirability or recall bias, especially among respondents who were asked to recall experiences 12 months after their initial consultations. To minimise bias, we conducted the interviews in private spaces and assured participants that their responses would remain completely confidential; however, we are unable to report that this was sufficient to prevent such bias from affecting our data. Another limitation is the generalisability of our results. We conducted our study in purposively selected districts and the experiences of respondents who received care at sites in our intervention facilities may be different from those of IUD users who receive care from other facilities, particularly those with lower client volumes, from the private sector, and in other geographical areas. In addition, we were not able to complement the quantitative results with any qualitative or observational data. This would have helped to understand more of the nuanced questions, such as the role of power dynamics and how this affects decision-making as well as addressing any questions of coercion. As we found higher discontinuation rates among PPIUD respondents compared with IIUCD clients, this might be misconstrued to indicate some element of coercion. Indeed, further research is merited.
While our study results are illuminating, future research should also explore the perspectives of providers and facility staff who may face constraints in providing high-quality services, for example, due to commodity stock-outs. Finally, our analysis represents best efforts to understand quantitative relationships between the range of factors that shape whether clients feel satisfied with their experiences obtaining IUDs and their ultimate perceptions of service quality; however, qualitative data will also offer crucial insights on this topic and are therefore highly advisable for future studies.
Conclusion
The findings from our analysis contribute to the evidence on IUD continuation rates in two states in India, and the factors that affect clients’ evaluation of quality of care. Our findings also demonstrate the likelihood of continuation as it relates to IIUD and PPIUD insertion. Quality of care entails a complete spectrum of factors, including offering a variety of methods, providing information on side effects, respecting clients’ rights and choices, supporting women’s decision to continue or discontinue and encouraging follow-up care, which can play a vital role in ensuring IUD continuation.
Amalgamation of quality family planning counselling and service provision into maternal and primary health care can both increase access and improve continuation, particularly in areas with limited family planning resources and counselling staff. By increasing awareness and support among clients’ families and communities, clients will also be better equipped to make informed contraceptive choices and manage side effects. Programmes offering IUD service provision should emphasise quality counselling as a means of improving overall access, uptake, and continuation.
Acknowledgements
The authors are grateful to Family Planning Division, Ministry of Health and Family Welfare, Government of India for providing technical leadership and oversight to the Expanding Access to IUD services in India (EAISI) project. We thank the health departments of the governments of Gujarat and Rajasthan for their active support in the implementation of the EAISI project and for granting permission and support to the project for conducting this study. The review and inputs provided by Amy Agarwal, Principal Writer and Editor at EngenderHealth is gratefully acknowledged.
Data availability
The data that support the findings in this study are available from the corresponding author upon request.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes
* Where the analysis called for “choice” in removal, we excluded clients whose IUDs were naturally expelled from the sample.
† For this question, respondents were asked to name the attribution of service with which they were satisfied and data collectors marked the corresponding responses on the questionnaire; thus, a low score on a particular attribute may not necessarily indicate dissatisfaction with a service, rather the emphasis on a particular service of satisfaction reflects what the respondent was able to recall or found most noteworthy.
References
- Agarwalla R, Panda M, Gupta E, et al. Snapshot of an improved maternal Health in India: the pillars of strength. Pan Asian J Obstet Gynecol. 2019;2(1):37–42.
- United Nations (UN). World contraceptive use 2015. New York: UN; 2015.
- Gupta RK, Singh P, Gupta R, et al. Contraceptive use: its prevalence, awareness, practices and determinants in a rural population of northern India. Int J Med Sci Public Health. 2017;6(10):1543–1548.
- Gogoi K, Hazarika PJ, Chanu NS, et al. A study on status of family planning practices and s association with socioeconomic and demographic factors in Manipur, India. Int J Stat Syst. 2017;12(3):441–455.
- International Institute for Population Sciences (IIPS) and ICF. India national Family Health Survey (NFHS-4) 2015-16. Mumbai: IIPS; 2017 : 112–115.
- Kumar A, Alwani AA, Unnikrishnan B, et al. Determinants of intrauterine device acceptance among married women in coastal Karnataka, India. J Clin Diagn Res. 2018;12(6) LC05–LC09.
- Mishra N, Panda M, Pyne S, et al. Barriers and enablers to adoption of intrauterine device as a contraceptive method: a multi-stakeholder perspective. J Family Med Prim Care. 2017;6(3):616–621.
- Sharma M, Joshi S, Nagar O, et al. Determinants of intrauterine contraceptive device discontinuation among Indian Women. J Obstet Gynecol India. 2014;64 (3):208–311.
- Agrahari K, Mohanty SK, Chauhan RK. Socio-economic differentials in contraceptive discontinuation in India. SAGE Open. 2016;6(2):2158244016646612.
- Rathi S, Jawadagi SA. A study to assess the factors affecting acceptance of intrauterine device (IUD) among rural women of Hirebagewadi, Belgaum. J Nurs Health Sci. 2014;3(2): 37–52.
- Sanogo D, RamaRao S, Jones H, et al. Improving quality of care and use of contraceptives in Senegal. Afr J Reprod Health. 2003;7(2):57–73.
- Jain AK, RamaRao S, Kim J, et al. Evaluation of an intervention to improve quality of care in family planning programme in the Philippines. J Biosoc Sci. 2012;44 (1):27–41.
- Dehingia N, Dixit A, Averbach S, et al. Family planning counseling and its associations with modern contraceptive use, initiation, and continuation in rural Uttar Pradesh, India. Reprod Health. 2019;16(1):178.
- Kamhawi S, Underwood C, Murad H, et al. Client centered counseling improves client satisfaction with family planning visits: evidence from Irbid, Jordan. Glob Health: Sci Pract. 2013;1(2):180–192.
- Neuteboom K, de Kroon CD, Dersjant-Roorda M, et al. Follow-up visits after IUD-insertion: sense or nonsense?: a technology assessment study to analyze the effectiveness of follow-up visits after IUD insertion. Contraception. 2003;68(2): 101–104.
- Gadre SS, Ahirwar R. Level of acceptance of IUD insertion in Indian women- a cross-sectional mixed research from Central India. Int J Reprod Contracept Obstet Gynecol. 2015;4(4):1079–1085.
- Hall MA, Stephenson RB, Juvekar S. Social and logistical barriers to the use of reversible contraception among women in a rural Indian village. J Health Popul Nutr. 2008;26(2):241–250.
- Shattuck D, Kerner B, Gilles K, et al. encouraging contraceptive uptake by motivating men to communicate about family planning: the Malawi Male Motivator Project. Am J Public Health. 2011;101 (6):1089–1095.
- Ali MM, Cleland JG, Shah IH. Causes and consequences of contraceptive discontinuation: evidence from 60 demographic and health surveys. Geneva: World Health Organization; 2012.
- Hardee K, Harris S, Rodriguez M, et al. Achieving the goal of the London summit on family planning by adhering to voluntary, rights-based family planning: what can we learn from past experiences with coercion? Int Perspect Sex Reprod Health. 2014;40(4):206–214.
- Chen BA, Reeves MF, Hayes JL, et al. Postplacental or delayed insertion of the Levonorgestrel intrauterine device after vaginal delivery: a randomized controlled trial. Obstet Gynecol. 2010;116(5):1079.
- Eroğlu K, Akkuzu G, Vural G, et al. Comparison of efficacy and complications of IUD insertion in immediate postplacental/early postpartum period with interval period: 1 year follow-up. Contraception. 2006;74(5):376–381.
- Steenland MW, Zapata LB, Brahmi D, et al. The effect of follow-up visits or contacts after contraceptive initiation on method continuation and correct use. Contraception. 2013;87(5):625–630.
- MacDonald L, Jones L, Thomas P, et al. Promoting male involvement in family planning in Vietnam and India: HealthBridge experience. Gend Dev. 2013;21(1):31–45.
- Lundgren R, Cachan J, Jennings V. Engaging men in family planning services delivery: experiences introducing the Standard Days Method® in four countries. World Health Popul. 2012;14(1):44–51.
- Prata N, Bell S, Fraser A, et al. Partner support for family planning and modern contraceptive use in Luanda, Angola. Afr J Reprod Health. 2017;21(2): 35–48.
- Amatya R, Akhter H, McMahan J, et al. The effect of husband counseling on NORPLANT® contraceptive acceptability in Bangladesh. Contraception. 1994;50 (3):263–273.
- Ghule M, Raj A, Palaye P, et al. Barriers to use contraceptive methods among rural young married couples in Maharashtra, India: qualitative findings. Asian J Res Soc Sci Humanit. 2015;5(6):18.
- Raj A, Ghule M, Ritter J, et al. Cluster randomized controlled trial evaluation of a gender equity and family planning intervention for married men and couples in Rural India. PLoS One. 2016;11 (5).
- Mohanty SK, Mishra S, Chatterjee S, et al. Pattern and correlates of out-of-pocket payment (OOP) on female sterilization in India, 1990-2014. BMC Womens Health. 2020;20(13).
- Ahman E, Shah IH. New estimates and trends regarding unsafe abortion mortality. International Journal of Gynecology and Obstetrics. 2011;115 (2):121–126.
- Van Hollen C. Moving targets: Routine IUD insertion in maternity wards in Tamil Nadu, India. Reprod Health Matters. 1998; 6(11):98–106
- Kumar S, Sethi R, Balasubramaniam S, et al. Women's experience with postpartum intrauterine contraceptive device use in India. Reprod Health. 2014;11:32.
- Patnaik B, Mishra K. User satisfaction and retention of Cu-T (IUD) amongst rural women in Orissa. Health Popul Perspect. 2003;26:52–58.
- The Evidence Project. Dynamics of postpartum IUD use in India: quality of care received and interim results three months after insertion. Research Brief. Washington (DC): Population Council; the Evidence Project; 2018.