Abstract
Medical abortion (MA) is recommended by the WHO as a safe and effective pregnancy termination method in the first trimester. From a feminist perspective, it is a non-medicalised, self-managed, emancipating procedure allowing persons seeking abortion to be more in control of their abortion, as opposed to surgical procedures. In European countries where MA is legal, the proportion of MA (relative to surgical abortions) varies greatly. We hypothesised that this ratio may be partly explained by country-level dimensions of gender equality. We assessed the association between MA ratios and gender equality in Europe in correlation and regression analyses, using several country-level gender equality indices. The relevance of other factors, i.e. date of introduction of MA and pregnancy week until which MA is permitted, was also investigated. MA ratios ranged from 24.4% (Italy) to 97.7% (Finland). MA was more frequent relative to surgical abortion in countries with higher levels of gender equality. All gender equality indices were associated with MA ratios (e.g. Global Gender Gap Index corr. coeff: 0.761, p < 0.0001). Specifically, markers of economic and political gender equality seemed to drive the correlations. The pregnancy week until which MA is permitted was associated with both gender equality and MA ratios. Our study suggests that women’s participation in the economic and political sphere may have repercussions on the methods offered and used through abortion services. It highlights the link between feminist perspectives, reproductive health policies and practices, and gender equality, especially in terms of access to economic resources and political representation.
Résumé
L’avortement médicamenteux est recommandé par l’OMS comme une méthode d’interruption de grossesse sûre et efficace pendant le premier trimestre. D’un point de vue féministe, c’est une procédure non médicalisée, autogérée et émancipatrice permettant aux personnes souhaitant avorter de mieux maîtriser la procédure, contrairement aux interventions chirurgicales. Dans les pays européens où l’avortement médicamenteux est légal, la proportion d’avortements médicamenteux (par rapport aux avortements chirurgicaux) varie beaucoup. Nous avons pris pour hypothèse que cette proportion pouvait être expliquée en partie par certains aspects de l’égalité entre hommes et femmes au niveau national. Nous avons évalué l’association entre la proportion d’avortements médicamenteux et l’égalité hommes/femmes en Europe dans des analyses de corrélation et de régression, en nous servant des indices d’égalité au niveau national. La pertinence d’autres facteurs, c’est-à-dire la date de l’introduction de l’avortement médicamenteux et la semaine de grossesse jusqu’à laquelle cette procédure est autorisée, a aussi été étudiée. La proportion d’avortements médicamenteux allait de 24.4% (Italie) à 97.7% (Finlande). L’avortement médicamenteux était plus fréquent que l’avortement chirurgical dans les pays connaissant des niveaux plus élevés d’égalité hommes/femmes. Tous les indices d’égalité étaient associés à des proportions d’avortements médicamenteux (par exemple, coefficient de corrélation du Global Gender Gap Index: 0.761, p < 0.0001). Précisément, les marqueurs de l’égalité politique et économique entre hommes et femmes semblaient dicter les corrélations. La semaine de grossesse jusqu’à laquelle l’avortement médicamenteux est autorisé étaient associée aussi bien avec l’indice d’égalité que la proportion d’avortements médicamenteux. Notre étude suggère que la participation des femmes dans la sphère économique et politique peut avoir des répercussions sur les méthodes offertes et utilisées par le biais des services d’avortement. Elle met en lumière le lien entre les perspectives féministes, les politiques et pratiques de santé reproductive, et l’égalité entre hommes et femmes, spécialement du point de vue de l’accès aux ressources économiques et à la représentation politique.
Resumen
El aborto con medicamentos (AM) es recomendado por la OMS como un método seguro y eficaz para la interrupción del embarazo en el primer trimestre. Desde la perspectiva feminista, es un procedimiento emancipador no medicalizado y autogestionado que les permite a las personas que buscan un aborto tener más control de su aborto, a diferencia de los procedimientos quirúrgicos. En países europeos donde el AM es legal, la proporción de AM (con respecto a abortos quirúrgicos) varía en gran medida. Hipotetizamos que esta proporción podría explicarse en parte por las dimensiones de igualdad de género en cada país. Evaluamos la asociación entre proporciones de AM e igualdad de género en Europa en análisis de correlación y regresión, utilizando varios índices de igualdad de género de cada país. Además, se investigó la pertinencia de otros factores, es decir, la fecha de introducción de AM y la semana de gestación hasta la cual se permite el AM. La proporción de AM varió de 24.4% (Italia) a 97.7% (Finlandia). El AM era más frecuente relativo al aborto quirúrgico en países con mayores niveles de igualdad de género. Todos los índices de igualdad de género estaban asociados con la proporción de AM (ej., coeficiente de correlación del Índice Mundial de Disparidad entre los Géneros: 0.761, p < 0.0001). En específico, los marcadores de igualdad de género económica y política parecían impulsar las correlaciones. La semana de gestación hasta la cual se permite el AM estaba asociada con la proporción de igualdad de género y la proporción de AM. Nuestro estudio indica que la participación de las mujeres en la esfera económica y política podría tener repercusiones en los métodos ofrecidos y utilizados por servicios de aborto. Destaca el vínculo entre las perspectivas feministas, las políticas y prácticas de salud reproductiva y la igualdad de género, en particular en lo que respecta al acceso a recursos económicos y representación política.
Introduction
Medical abortion
Since its introduction in the late 1980s, medical abortion (MA) (also known as “drug-induced abortion” or “medication abortion”), in the form of mifepristone (RU486) and misoprostol, has held out the promise of enabling better access to abortion for womenFootnote* worldwide.Citation1 In the early 2000s, the World Health Organization (WHO) added MA to the list of essential medicines.Citation2 It is now recommended as a safe and effective pregnancy termination method in the first trimester.Citation3 The preferred regimen consists of two doses: one of mifepristone, which stops the pregnancy, and one of misoprostol, which provokes the abortion (misoprostol is widely available for its use in gastroenterology for the prevention of stomach ulcers, and in some contexts in gynaecological and obstetric care to induce labour and for the management of miscarriages). The two drugs are usually taken at an interval of one to two days.Citation3 In most settings, MA requires initial consultation with a health professional during which the first dose is administered. It may be possible for women to take the second dose at home, which can be done safely.Citation4 The efficacy and acceptability of MA in the early weeks of pregnancy are comparable to those of surgical abortion.Citation5,Citation6 MA also presents several advantages from a health and healthcare perspective: it is associated with a more efficient use of resources (performed at the primary care level, outpatient delivery), a reduction in needs for surgical skills, and is a non-invasive procedure.Citation7
MA ratios in different contexts
In legally constrained contexts, where abortion legislation denies or narrowly defines the right to abortion, the practice of MA has increased over the past decades through the availability of misoprostol over the counter, on websites or on the black market. Studies conducted in Latin America,Citation8 the CaribbeanCitation9 and the Philippines,Citation10 for example, document the role of MA as a way to access safe abortion and increase women’s control over their reproductive lives. However, in countries where abortion is legal, and more specifically in Europe where this study is set, the availability of and access to MA is less studied.Citation2 In some of those countries, MA is not even an option and surgical methods dominate exclusively (e.g. Turkey).Citation11 In others, it is available in theory but, in practice, is not a common option offered to women.Citation1 In Germany, for example, the proportion of medical abortions is low (about 20%), and most abortions remain surgical.Citation12 In other countries though, MA is the most frequent type of abortion: in Sweden, over 96.4% of first-trimester abortions in 2019 were medical abortions.Citation13 In general, ratios across Europe vary widely.
Such differences in the ratio of medical to surgical abortions in the same region and in countries which tend to be considered liberal in terms of abortion legislationCitation14 are worth investigating: why is there such a variation of MA ratios across European countries?
Feminist perspective on (the availability of) medical abortion
A feminist approach to MA offers some leads for explanation. MA is seen in many contexts as an emancipating and empowering procedure that allows women to self-manage their abortion.Citation15,Citation16 Studies emphasise how women who choose MA do so to be more in control of their abortion and to avoid anaesthesia and settings where they do not feel comfortable.Citation6 As a self-managed care intervention, MA can uphold “people’s decision-making capacity, autonomy and dignity”.Citation17 Last, MA is an interesting option from a health equity point of view as it has the potential to solve access problems for those who cannot travel to abortion clinics or those living in remote areas.Citation18
As opposed to surgical procedures, where the surgery is “done” to the woman by a doctor, MA allows for more bodily autonomy. It also does not require surgical nor medical skillsCitation2 and therefore does not have to involve medical professionals. As such, it can be seen as a way to challenge traditional power relations (e.g. medical hierarchy, patriarchy) in terms of timing and place of abortion and mode of administration,Citation1 and as a “de-medicalised” alternativeCitation19 to the well-documented decades-long trend of medicalisation of reproductive health (see Inhorn,Citation20 for example). Returning to the example of Germany, German feministsCitation21 have argued that in a context where abortion remains technically a crime,Citation22 where gynaecologists cannot advertise abortion services,Citation23 and where access, in general, is limited, the predominance of surgical abortion is yet another form of unnecessary medicalisation and a way to keep control over the female body.Citation24 Without saying that MA should prevail, they argue that persons seeking abortion should at least be offered a choice between different types of abortion.
The macro determinants of abortion care
Barriers to the availability and uptake of MA go beyond the law (whether abortion is legal or not) and individual choice (the “right to choose” approach). They include macro-level constraints, such as social and cultural norms, and healthcare system characteristics. They are contextualised and embedded within systemic power and gender relations,Citation25 gender norms, and the place women hold in societies. A recent conceptual review identified as macro-level determinants of abortion care the role of abortion activism in societies, social and cultural norms concerning abortion (i.e. stigma) and gender relations.Citation26 An intersectional perspective also suggests that those structural barriers are likely to disproportionately affect women from lower socio-economic backgrounds, racialised women, women with disability, or persons from sexual and gender minorities.Citation27
The feminist point of view, therefore, prompts one question: is the proportion of MA in a given country influenced by internalised gender inequalities in society? Although it remains difficult to meaningfully measure gender norms and gender equality at the country level, there are several macro-level indices which try to capture gender (in)equality in a multi-dimensional manner: for example, taking into account indicators on health, education, politics, and economics. These are produced by international organisations such as the United Nations (UN) – a pioneer in this field – and other actors such as the World Economic Forum. They are limited in their intent and scope and subject to some criticisms,Citation28,Citation29 but have been used in health research and epidemiology to highlight gender-related inequalities, for international comparisons, and for the study of the structural determinants of health.Citation30 Recent research has shown that higher gender equality at the country level is associated with a lower frequency of abortion.Citation31 Here, we propose to use macro-level indices of gender equality to expose the association (or its absence) between MA ratios and gender equality in Europe, hypothesising that more gender-equal countries will have higher MA ratios.
Methods
To explore this hypothesis, we designed an ecological correlation study. First, we collected, described, and contrasted MA and gender-relevant macro-level characteristics of European countries where MA is authorised and where data are available. Second, we quantitatively investigated the relationship between gender equality and MA ratios through descriptive statistics and regression analyses.
Variables
Outcome of interest
The outcome of interest was the share of medical abortions among all induced abortions in a given year (most recent year available: 2017, 2018, or 2019) in each country; for short, we refer to this measure as the MA ratio. Included in the calculations were all legally conducted abortions, whatever the type of provider, the reason for abortion, or the setting (e.g. hospitals, family planning centres). Illegal abortions, for which data are in any case not usually available, were excluded from the analysis. Spontaneous abortions, also known as miscarriages, were also excluded from the analysis.
Health system level variables
At the health system level, we took into account the following information:
– the date of introduction of mifepristone and approval of MA (continuous variable);
– the pregnancy week until which MA is authorised (continuous variable).
These variables frame the practice of MA in each country. The first one gives a time reference for the introduction of the practice, the latter details about the implementation of the procedure.
Gender equality indices
Commonly used national gender equality indices have been considered for this article. The selection has been guided by the coverage they offer in terms of countries, and by the relevance of their content with regard to our research.
We used the following indices in the quantitative analyses:
– GEI: Gender Equity Index (2012) calculated by Social Watch based on data from the UN.Citation32 This index is available for use as a scale from 0 to 1 (1 = total equality) and is composed of three dimensions (sub-scores): economic, political, and educational.
– GII: Gender Inequality Index (2019) calculated by the UN.Citation33 This index has a scale from 0 to 1 (1 = total inequality), calculated from five indicators (maternal mortality ratio, adolescent birth rate, female and male population with at least secondary education, female and male shares of parliamentary seats, female and male labour force participation rates).
– GGGI: Global Gender Gap Index (2018) calculated by the World Economic Forum.Citation34 This index is available for use as a scale from 0 to 1 (1 = total equality) based on gender differences in four dimensions (sub-scores): economic, political, education and health.
– Gender Equality Index (2019) calculated by the European Institute for Gender Equality of the European Union (EIGE), and therefore not available for Norway, Iceland and Switzerland.Citation35 This index has a scale from 0 to 100 (100 = total equality) based on gender differences in six dimensions (sub-scores): work, money, time, knowledge, health, and power. We also used an extra dimension sub-score available for the year 2017: violence against women. Although this index does not cover all European countries, we retained it as it was designed specifically for the European context and contains more dimensions (e.g. “time” which measures the allocation of time spent doing care and domestic work and social activities) than the others.
– SIGI: Social Institutions and Gender Index (2019) calculated by the OECD.Citation36 This index has a scale from 0 to 100 (100 = very high discrimination) based on gender differences in four dimensions (sub-scores): discrimination in the family, restricted physical integrity, restricted access to financial resources, restricted civil liberties. For Iceland, only the Families and Liberties sub-scores were available.
These indexes are similar in their intentions but vary in the dimensions that they take into account, the variables they use in each dimension, and the way they calculate scores.Citation29 Using as many as possible allowed us to see the strength of the relationship between the MA ratio and gender equality and to identify specific dimensions of gender equality that are consistently more relevant to MA.
Analyses
First, we mapped the data in scatter plots, to assess the nature of the correlation. Second, we conducted bivariate analyses, testing the correlation between the MA ratio and gender equality for each gender equality general score and each sub-score, using Pearson correlation tests. Third, for the variables which showed a statistically significant correlation with the outcome, we ran linear regression analyses. We started by calculating unadjusted regression coefficients (model 0), and then introduced a covariate – the date of introduction of mifepristone (model 1) and the pregnancy week until which MA is permitted (model 2). For both model 1 and 2, we ran two versions of the models: in version (a), the maximum number of observations is included, while in version (b), the countries where MA is not legal are excluded. These sensitivity analyses helped us to assess the robustness of the results. Last, we ran a mediation model to refine our understanding of the relation between MA ratios (outcome), pregnancy week until which MA is permitted (mediator) and gender equality (treatment). Scatterplots were created with Excel and other quantitative analyses performed with Stata/IC 16.1. The significance level was set at p < 0.05. The mediation model was implemented using the Baron and Kenny (1986) product approach.Citation37
Results
MA ratios and abortion services characteristics
We included 23 countries in the analysis. shows the MA ratio in those countries for the most recent year available, i.e. 2017, 2018, or 2019 (see ).
Figure 1. Medical abortion ratios in Europe, most recent year available (2017, 2018, or 2019). Source: Author’s own elaboration. For the data sources, see .
Notes: 1. We intended to investigate medical abortion ratios in all of EU 28 countries (when the research was conducted, the UK was still part of the EU), plus Norway, Switzerland, and Iceland. However, for a few countries, where medical abortion is legal and performed, no data are available – for the following reasons: (i) not published and statistical office and/or public health institute did not respond to the author’s data request (countries: Czech Republic, Greece, Romania, and Bulgaria), (ii) data not collected (Austria collects only data for hospital-based abortions, Luxembourg and Latvia do not collect data by method of abortion). 2. About the UK: England and Wales and Scotland are administered under different National Health Services, and data are available separately. We, therefore, decided to look at them independently. However, for the gender equality measures, there is only one figure available, at the UK level. In Northern Ireland, all types of abortion were prohibited until March 2020, therefore not allowing enough time for inclusion in the study. In Ireland, all types of abortion were prohibited until 2018, also not allowing enough time for inclusion in the study. 3. In Croatia, medical abortion was approved in 2019, therefore not allowing enough time for inclusion in the study. 4. In six countries (Cyprus, Hungary, Poland, Lithuania, Malta, Slovak Republic), medical abortion is not legally performed, and therefore the medical abortion rate is 0.
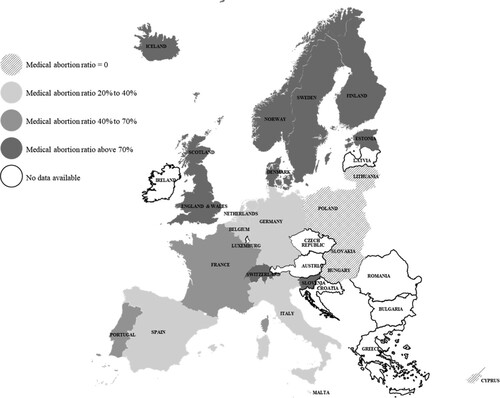
Table 1. Key characteristics of medical abortion practice in the countries where it is legal
presents descriptive statistics of key variables for comparison of MA practice between countries where it is legally performed.
MA ratios ranged from 24.4% (Italy) to 97.7% (Finland). In all countries but Portugal, surgical abortion had been available for several years, sometimes several decades, before the introduction of MA. The first country to adopt MA was France, from where the MA drug (RU486) originated. Portugal authorised abortion only in 2007, legalising both surgical and medical abortion at the same time. In most countries, MA is authorised for early abortions only, i.e. until the 7th to 9th week of pregnancy. Portugal, England, and Wales authorise MA until the 10th week and Finland, Norway and Sweden until the 12th week of pregnancy. In terms of providers, there are two main models: the one where abortions are all performed in hospitals or doctors’ practices (usually gynaecologists) and the one where family planning centres play an important role, next to the hospitals and doctors’ offices.
Association between MA ratios and gender equality
plots the MA ratios against the gender equality national indices. Values of the different gender equality indices for each country are presented in Supplementary File 1.
Figure 2 . Scatterplots of medical abortion ratios (x-axis) and gender equality indices (y-axis) with linear regression line
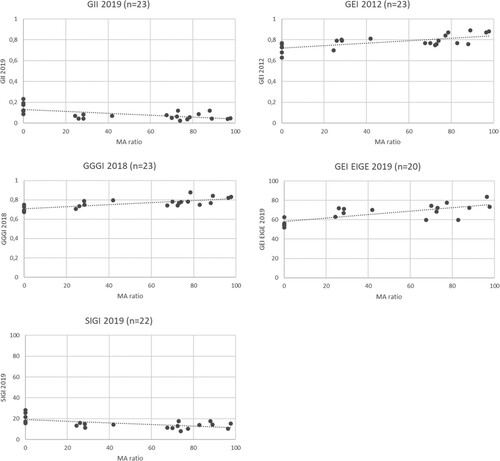
All the graphs seem to indicate the possibility of a linear association between MA ratios and gender equality. In order to explore these associations further, we computed Pearson’s correlation coefficients for all indices, as well as for all the dimension-specific sub-scores, in an attempt to explore whether a specific aspect of gender equality is driving the association ().
Table 2. Correlation coefficients between medical abortion ratio and gender equality indices
The GII (corr. coeff: −0.61, p = 0.002), the GGGI (corr. coeff: 0.761, p < 0.0001), as well as the GEI from Social Watch (corr. coeff: 0.678, p = 0.001), the GEI from EIGE (corr. coeff: 0.735, p = 0.0002), and the SIGI (corr. Coeff: −0.586, p = 0.004) were all associated with the outcome, with countries scoring better in terms of gender equality having higher MA ratios. Sub-scores within different dimensions of gender equality (namely GEI Economy and Empowerment, GGGI Economy and Politics, GEI EIGE Work, Time and Power, and SIGI Families, Finance and Liberties) were also associated with the outcome. The health sub-scores did not show an association with the MA ratio.
We then ran linear regression models for the variables which showed a statistically significant association with the outcome, controlling in turn for a key variable – the date of introduction of MA (models 1) and the number of weeks of pregnancy until which MA is permitted (models 2). In models 1(a) and 2(a), we used the maximum number of observations available, while in models 1(b) and 2(b), we removed the countries where MA is not allowed (MA ratio = 0). Overall, the date of introduction had no clear effect: although it seemed to modify the effect of the gender equality index in model 1(a), its association with the MA ratio was always not statistically significant when looking only at the sample of countries where MA is legal (model 1(b)). The number of weeks during which MA is allowed, however, showed in most cases a statistically significant correlation with MA ratios and made most of the associations between gender equality and MA ratios non-significant (). In mediation analyses, the number of weeks was strongly associated with gender equality measures and its role as a mediator between gender equality and MA ratios was made obvious: the mediated (or indirect) effect accounted for all or most of the total effect. For example, for GGGI Eco, 63% of the total effect of the gender equality sub-score on the MA ratio was mediated by the number of weeks (Supplementary material 2). In other words, this meant that rather than gender equality having a direct influence on MA ratio, gender equality was likely to have an effect on the number of pregnancy weeks until which MA is permitted, which in turn had an effect on the MA ratio.
Table 3. Regression models’ results with MA ratios as dependent variable
Discussion
We found a great diversity in MA ratios across Europe. Part of this diversity could be explained by aspects of gender equality. This is what the correlations between the gender equality indices and some of their sub-scores and MA ratios suggest: in countries where men and women are more equal in terms of economic participation and political representation (defined as “empowerment”, “politics” or “power”, depending on the indices), there are proportionately more medical abortions compared to surgical abortions. As could be expected, the health and education sub-scores tended not to be associated with MA ratios, as gender equality in terms of education and health is consistently higher than gender equality in other domains in European countries. In particular, gender equality has been reached in education in most countries under study. The relevance of the economic and political dimensions in explaining the proportion of medical relative to surgical abortions is to be interpreted in terms of gender norms and access to power. The economic and financial (in)dependence of women in their household and as a sub-group in society, as well as their representation and presence in institutions and decision-making organisations, can contribute to a more or less gender-equal, or feminist organisation of reproductive healthcare services. This emphasises the fact that availability of MA is not so much a matter of law. Indeed, MA is already a legal option in all those countries and the formal, theoretical access is not supposed to be an issue. But, in practice, in some less gender-equal contexts, health systems and practitioners may favour a more hierarchical, medicalised approach to abortion (more familiar, cleaner, quicker, more controlled, often with the patient under general anaesthesia), something that may have been challenged in countries with more progressive gender norms.
A few countries do not fit the pattern of higher gender equality coupled with a higher MA ratio. Such outliers include Germany, Belgium, and the Netherlands, which demonstrate relatively high gender equality but low MA ratios. Some explanations may be found in the fact that the three countries require a mandatory waiting (or “cooling-off”) period between a first counselling consultation and the abortion itself. Additionally, in Germany and Belgium, there is still a high level of stigma and access problems surrounding abortion in general, as well as a lack of training of the medical personnel in modern (i.e. medical) abortion techniques.Citation38 In the Netherlands, a high reliance for service delivery on specialised abortion clinics equipped for early surgical abortion may explain the persistence of the predominance of this procedure.Citation39
Another outlier is Portugal, which tends to score relatively poorly in terms of gender equality but has a relatively high MA ratio. As mentioned earlier, Portugal legalised abortion only recently compared to most countries, in 2007. At this point in time, both surgical and medical methods became available simultaneously. No period was needed for MA to “catch up” against the already established surgical abortion. This makes Portugal an ideal country to compare the use of methods. In the coming years, it will be interesting to follow the path of Ireland and Northern Ireland, which have also recently authorised both methods simultaneously, to see whether MA becomes the most used method and try to assess whether the dominance of one method over the other comes from health system or societal features.
In contrast to the Portuguese scenario, it is noteworthy to see that the year when MA became available has no obvious influence on MA ratios. The absence of clear association may be due to the small sample size. It may also suggest that higher ratios are not necessarily linked to longer availability of the method, but to some other factors, also beyond gender equality. Anecdotal evidence points to the capacity of health systems to adapt to new practices. For example, the way abortion used to be taught in medical schools when it was first legalised may have not changed over the years, and thus no younger doctors have been trained to deal with MA protocols. This may not be such a problem in countries where providers other than doctors (e.g. midwives, nurses) have long been allowed to perform abortions through a culture of task-shifting (e.g. UK, Scandinavian countries)Citation40,Citation41 or in smaller or more centralised countries where changes in practice spread more easily. Due to the quantitative nature of our analysis, it was not possible to take into account relevant features of health systems in the statistical modelling. Trying to categorise countries (e.g. those where MA is performed only by doctors vs. by midwives, or those where MA is more costly than surgical abortion vs. those where costs are similar) would have led to too much oversimplification and therefore misclassification. However, we acknowledge the importance of health systems and of different types of service provision,Citation42 and their potential role on MA ratios. We therefore encourage international comparisons through qualitative studies that would investigate the historical, health policy- and system-relevant developments that have resulted in current MA ratios.
MA ratios above 80% in Nordic and Scandinavian countries raise again the question of choice. When one technique dominates so obviously, individuals who wish to opt for a surgical abortion may have difficulties accessing it. Studies specifically looking at the choice of abortion procedure in settings that explicitly offer both medical and surgical procedures tend to show varied results but all highlight the likely heavy influence of providers’ preferences in the users’ decision-making process.Citation39,Citation43,Citation44 This is yet another reminder of how abortion practices are likely to be supply/provider-driven, rather than user-driven. Future research could also investigate the extent to which MA policies and practices allow for self-management and autonomy in various countries, considering, for example, requirements with regard to the settings for the intake of the first and second regimen dose (e.g. in medical setting? at home?), the possibility of teleconsultations, the obligation to undergo a post-abortion ultrasound, etc. There are indeed large variations in terms of MA practices across countries, from medical abortions conducted in hospitals to those conducted at home, and from medical abortions which require several in-person consultations (pre-, during, and post-abortion) to those which require only one consultation. These different forms of delivery are likely to have an influence on MA ratios.
Last, the link between gender equality and policy making in reproductive health emerges again through our mediation analyses. The upper time limit for having a (medical) abortion has always been central to political debates and influenced by many factors that go beyond the science. The Covid-19 pandemic has crystallised these tensions and reignited demands from providers, activists, and human rights organisations (see, for example, in ItalyCitation45 and FranceCitation46) to extend the time during which one can have a MA, as well as the possibility of managing the whole abortion process at home, through the mainstreaming of teleconsultations (a practice deemed safeCitation47) and supplying medication by post.Citation17 Only a few changes have happened so far and their long-term fate is uncertain.Citation48,Citation49 This points again towards a politicisation of the female body, the influence of gender norms, how decisions can be far removed from the scientific evidence, and the impact these factors have on abortion practices (including MA ratio).
This ecological study sheds new light on abortion policies and practices in Europe, going beyond what general abortion rates and categories of abortion law, from “liberal” to “restrictive” can tell us. The main finding, namely that MA ratios are higher in more gender-equal countries, provides an example of how aspects of gender equality (in particular in the economic and political sphere) are correlated with various degrees of medicalisation of the female body and translated into abortion practices. It has implications for practice, providing leads for reflection on the number of pregnancy weeks until which MA is permitted and the respective influence of health systems, providers and users in terms of choice of abortion procedure. Those considerations are even more important during the Covid-19 pandemic, which has revealed the crucial role of MA when access to regular abortion services is compromised by social distancing and “stay home” public health measures.Citation50,Citation51
In the next steps of our research, we propose to test the gender equality hypothesis in Germany, where the MA ratios are very different across the 16 states (Bundesländer). The within-country analysis will remove some of the normative and cultural effects at the country level but still allow for variation in terms of economic inequalities, political representation, religious affiliations, and local medical practices.
Strength and limitations
One of the strengths of this study is that it collected and compared data (including unpublished data) on MA across European countries. It is also innovative in that it considered the link between the MA ratio and gender equality, seeking to investigate the explanatory power of a feminist perspective on the delivery of health services.
Limitations principally lie in the measurement of the main outcome and exposure: with regard to the MA ratio, the comparability of the data may be limited by differences in how information is collected in each country. However, we excluded countries on the basis of data availability and completeness (for example, Austria, which collects data only on in-hospital abortions, was not included in the analyses) and are confident that the countries included are, at least to some extent, comparable. One can also be critical of the national gender equality indices as to what type of reality they represent and how meaningful they are.Citation52 Nevertheless, they give an indication of national-level structural constraints and social norms, and the way society is valuing women. They are not an exhaustive representation of reality but have proved to be useful tools for international comparisons and the understanding of the macro-level determinants of health. Last, the main limitation of our study is its small sample size. The fact that only 23 (22, 20, 17, or 14 depending on analyses) countries were included in the analyses limits the potential in terms of quantitative analysis and the generalisability of the results. However, we believe that the study provides leads for further exploration.
Conclusion
MA ratios are correlated with some markers of gender equality in Europe. Our results suggest that women’s participation in the economic and political sphere may have repercussions on the supply and use of abortion care, potentially influencing which methods are offered and which are used. They highlight the link between feminist perspectives, reproductive health policies and practices, and gender equality, especially in terms of access to economic resources and political representation.
Supplemental Material
Download MS Word (31 KB)Supplemental Material 1
Download MS Excel (13 KB)Acknowledgements
The author would like to acknowledge her colleagues Stephanie Batram-Zantvoort, Yudit Namer, Oliver Razum, Odile Sauzet, Charles Vial, and Lisa Wandschneider from Bielefeld University for their precious feedback on the research question, the design, and the write-up of the study. CM is responsible for the idea, design, and conduct of the research. She has drafted and finalised this article.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes
* We acknowledge that persons other than cisgender women also have abortions and we value their experiences. However, since the main outcome in this article is based on secondary data referring only to females, and since the analytical focus is on gender equality indices, which distinguish between males and females, we chose to use the term “women” throughout the text to refer to persons who have had or are planning to have an abortion.
References
- Jelinska K, Yanow S. Putting abortion pills into women's hands: realizing the full potential of medical abortion. Contraception. 2018;97(2):86–89.
- Guilaume A, Rossier C. Abortion around the world. An overview of legislation, measures, trends, and consequences. Population (Paris). 2018;73(2):217–306.
- World Health Organization. Clinical practice handbook for safe abortion. Geneva: WHO; 2014.
- Ngo TD, Park MH, Shakur H, et al. Comparative effectiveness, safety and acceptability of medical abortion at home and in a clinic: a systematic review. Bull World Health Organ. 2011;89(5):360–370.
- Ireland LD, Gatter M, Chen AY. Medical compared with surgical abortion for effective pregnancy termination in the first trimester. Obstet Gynecol. 2015;126(1):22–28.
- Swica Y, Raghavan S, Bracken H, et al. Review of the literature on patient satisfaction with early medical abortion using mifepristone and misoprostol. Expert Rev Obstet Gynecol. 2014;6(4):451–468.
- World Health Organization. Medical management of abortion. Geneva: World Health Organization; 2018.
- Lafaurie MM, Grossman D, Troncoso E, et al. Women's perspectives on medical abortion in Mexico, Colombia, Ecuador and Peru: a qualitative study. Reprod Health Matters. 2005;13(26):75–83.
- Dzuba IG, Winikoff B, Peña M. Medical abortion: a path to safe, high-quality abortion care in Latin America and the Caribbean. Eur J Contracept Reprod Health Care. 2013;18(6):441–450.
- Gipson J, Hirz A, Avila J. Perceptions and practices of illegal abortion among urban young adults in the Philippines: a qualitative study. Stud Fam Plann. 2011;42(4):261–272.
- Mihciokur S, Akin A, Dogan BG, et al. The unmet need for safe abortion in Turkey: a role for medical abortion and training of medical students. Reprod Health Matters. 2014;22(sup44):26–35.
- ProFamilia. 8 fakten zum Schwangerschaftsabbruch in deutschland. Frankfurt am Main: ProFamilia; 2018.
- Socialstyrelsen. (2018). Number of abortions, entire Sweden, age: all, 2018. [cited 2019 Oct 25]. Available from: https://sdb.socialstyrelsen.se/if_abo/resultat.aspx.
- Center for Reproductive Rights. (2019). The world's abortion laws. [cited 2019 Oct 25]. Available from: https://reproductiverights.org/worldabortionlaws.
- Ramos S, Romero M, Aizenberg L. Women’s experiences with the use of medical abortion in a legally restricted context: the case of Argentina. Reprod Health Matters. 2015;22(sup44):4–15.
- Assis MP, Larrea S. Why self-managed abortion is so much more than a provisional solution for times of pandemic. Sexual Reprod Health Matters. 2020;28(1):1779633.
- Kumar M, Daly M, De Plecker E, et al. Now is the time: a call for increased access to contraception and safe abortion care during the COVID-19 pandemic. BMJ Global Health. 2020;5(7):e003175.
- Mählck C-G, Bäckström T. Follow-up after early medical abortion: comparing clinical assessment with self-assessment in a rural hospital in northern Norway. Eur J Obstet Gynecol Reprod Biol. 2017;213:1–3.
- Iyengar SD. Introducing medical abortion within the primary health system: comparison with other health interventions and commodities. Reprod Health Matters. 2005;13(26):13–19.
- Inhorn MC. Defining women's health: a dozen messages from more than 150 ethnographies. Med Anthropol Q. 2006;20(3):345–378.
- Krolzik-Matthei K. Feministische perspektiven auf die abtreibungsdebatte in deutschland. Münster: Unrast Verlag; 2015.
- Deutscher Bundestag. Gesetzliche regelungen zum Schwangerschaftsabbruch in mitgliedstaaten der europäischen union, der türkei und kanada. sachstand WD 7-3000-156/14. Berlin: Wissenschaftliche Dienst, Deutscher Bundestag; 2014.
- Frommel M. Das verbot des »anbietens« von diensten für den Schwangerschaftsabbruch nach § 219 a Abs. 1 StGB. Juristische Rundschau. 2018;2018(5):239–241.
- Arp D. Medikamentöser schwangerschaftsabbruch: frauen sollten die wahl haben. Deutsches Ärzteblatt. 2013;110(50):A2422–A2423.
- Chiweshe M, Mavuso J, Macleod C. Reproductive justice in context: South African and Zimbabwean women’s narratives of their abortion decision. Fem Psychol. 2017;27(2):203–224.
- Coast E, Norris AH, Moore AM, et al. Trajectories of women's abortion-related care: a conceptual framework. Soc Sci Med. 2018;200:199–210.
- Marecek J, Macleod C, Hoggart L. Abortion in legal, social, and healthcare contexts. Fem Psychol. 2017;27(1):4–14.
- Permanyer I. Why call it ‘equality’ when it should be ‘achievement’? A proposal to un-correct the ‘corrected gender gaps’ in the EU gender equality index. J Eur Soc Policy. 2015;25(4):414–430.
- Gaye A, Klugman J, Kovacevic M, et al. Measuring key disparities in human development: the gender inequality index. Human Dev Res Paper. 2010;46:1–37.
- King TL, Kavanagh A, Scovelle AJ, et al. Associations between gender equality and health: a systematic review. Health Promot Int. 2020;35(1):27–41.
- Dema Moreno S, Llorente-Marrón M, Díaz-Fernández M, et al. Induced abortion and gender (in) equality in Europe: a panel analysis. Eur J Women's Studies. 2020;27(3):250–266.
- Social Watch. (2012). Measuring inequity: the 2012 gender equity index. [cited 2020 Nov 13]. Available from: https://www.socialwatch.org/node/14365.
- United Nations Development Programme (UNDP). (2018). Gender Inequality Index (GII). [cited 2021 Sep 20]. Available from: http://hdr.undp.org/en/content/gender-inequality-index-gii.
- World Economic Forum. The global gender gap report 2018. Geneva: World Economic Forum; 2018.
- European Institute for Gender Equality (EIGE). (2020). Gender Equality Index. [cited 2021 Nov 13]. Available from: https://eige.europa.eu/gender-equality-index/2020/compare-countries.
- OECD. (2019). Social Institutions and Gender Index 2019. [cited 2021 Jul 5]. https://stats.oecd.org/Index.aspx?DataSetCode=SIGI2019.
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173.
- Marques-Pereira B, Pereira S. Abortion in Belgium: a precarious right? Gender-Rivista Internazionale di Studi di Genere. 2014;3(5).
- Loeber OE. Motivation and satisfaction with early medical vs. surgical abortion in the Netherlands. Reprod Health Matters. 2010;18(35):145–153.
- Endler M, Cleeve A, Sääv I, et al. How task-sharing in abortion care became the norm in Sweden: a case study of historic and current determinants and events. Int J Gynecol Obstet. 2020;150:34–42.
- Colvin CJ, de Heer J, Winterton L, et al. A systematic review of qualitative evidence on barriers and facilitators to the implementation of task-shifting in midwifery services. Midwifery. 2013;29(10):1211–1221.
- Bracken H, Winikoff B. The state of medical abortion in Europe today. Entre Nous – Eur Mag Sex Reprod Health. 2005;59:7–9.
- Vodopivec S, Bokal EV, Pinter B. Counselling before first trimester abortion and acceptability of the procedure: results from a Slovenian cross-sectional study. Eur J Contracept Reprod Health Care. 2019;24(6):487–493.
- Moreau C, Trussell J, Desfreres J, et al. Medical vs. surgical abortion: the importance of women's choice. Contraception. 2011;84(3):224–229.
- Human Rights Watch. (2020). Italy: Covid-19 exacerbates obstacles to legal abortion-inadequate measures heighten existing risks for health, lives. [cited 2021 Mar 5]. Available from: https://www.hrw.org/news/2020/07/30/italy-covid-19-exacerbates-obstacles-legal-abortion.
- Makooi B. (2020). Coronavirus: in France, professionals look to extend legal abortion time limit. [cited 2021 Mar 5]. Available from: https://www.france24.com/en/20200402-coronavirus-in-france-professionals-look-to-extend-legal-abortion-time-limit.
- Endler M, Lavelanet A, Cleeve A, et al. Telemedicine for medical abortion: a systematic review. BJOG: Int J Obstet Gynaecol. 2019;126(9):1094–1102.
- Moreau C, Shankar M, Glasier A, et al. Abortion regulation in Europe in the era of COVID-19: a spectrum of policy responses. BMJ Sex Reprod Health. 2021;47:e14.
- Romanis EC, Parsons JA. Legal and policy responses to the delivery of abortion care during COVID-19. Int J Gynecol Obstet. 2020;151(3):479–486.
- Kirk S, Morgan L, McDermott S, et al. Introduction of the National Health Service early medical abortion service in Northern Ireland – an emergency response to the COVID-19 pandemic. BMJ Sex Reprod Health. 2021;47:293–295.
- Reynolds-Wright JJ, Johnstone A, McCabe K, et al. Telemedicine medical abortion at home under 12 weeks’ gestation: a prospective observational cohort study during the COVID-19 pandemic. BMJ Sex Reprod Health. 2021;47:246–251.
- Le Guen M, Schantz C, Pannetier J, et al. Le genre et ses indices: les normes internationales sur l’égalité femmes/hommes en question. In: Etesse M, editor. Inégalités en perspectives. Editions des archives contemporaines; 2019. p. 35–47.
- Commission Nationale d’Evaluation de la loi du 3 avril 1990 relative à l’interruption de grossesse (loi du 13 août 1990). Rapport à l'attention du Parlement 1 janvier 2016 –31 décembre 2017. Brussels: Commission Nationale d’Evaluation de la loi du 3 avril 1990 relative à l’interruption de grossesse (loi du 13 août 1990); 2020.
- Gynuity Health Projects. List of mifepristone approvals. 2017 [cited 2020 Nov 13]. Available from: https://gynuity.org/assets/resources/biblio_ref_lst_mife_en.pdf
- Moniteur Belge. Loi relative à l’interruption volontaire de grossesse. 2018 [cited 2020 Nov 18]. Available from: https://organesdeconcertation.sante.belgique.be/sites/default/files/documents/15.10.18.pdf
- Finnish Institute for Health and Welfare. [Induced abortions in the Nordic countries 2017]. [cited 2020 Nov 18]. Available from: https://www.julkari.fi/bitstream/handle/10024/137803/Tr04_19.pdf?sequence=5&isAllowed=y.
- Sundhed.dk. Medicinsk abort. 2018 [cited 2020 Nov 18]. Available from: https://www.sundhed.dk/borger/patienthaandbogen/kvindesygdomme/sygdomme/abort/medicinsk-abort/
- Department of Health and Social Care. Abortion statistics, England and Wales: 2019. Online Publication: Department of Health and Social Care; 2020. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/891405/abortion-statistics-commentary-2019.pdf
- Health Statistics and Health Research Database. RK30: abortion method by abortion type and health care provider’s county. 2020 [cited 2020 Nov 18]. Available from: https://statistika.tai.ee/pxweb/en/Andmebaas/Andmebaas__01Rahvastik__03Abordid/RK30.px/
- Medicum. Medical abortion. [cited 2020 Nov 9]. Available from: https://www.medicum.ee/en/naistenouandla/naistenouandla-teenused/medical-abortion/.
- Laanpere M, Ringmets I, Part K, et al. Abortion trends from 1996 to 2011 in Estonia: special emphasis on repeat abortion. BMC Women’s Health. 2014;14(1):81.
- Finnish Institute for Health and Welfare. Induced abortions 2019. 2020 [cited 2020 Nov 18]. Available from: https://www.julkari.fi/bitstream/handle/10024/140202/Raskaudenkeskeytykset_2019.pdf?sequence=5&isAllowed=y
- Duodecim Terveyskirjasto. Raskaudenkeskeytys. 2013 [cited 2020 Nov 18]. Available from: https://www.terveyskirjasto.fi/terveyskirjasto/tk.koti?p_artikkeli=khp00025
- Vilain A, Allain S, Dubost C-L, et al. Interruptions volontaires de grossesse: une hausse confirmée en 2019. Études et Résultats. 2019: 1163.
- Service-Public.fr. Interruption volontaire de grossesse (IVG). 2020 [cited 2020 Nov 18]. Available from: https://www.service-public.fr/particuliers/vosdroits/F1551#:~:text=l'IVG%20m%C3%A9dicamenteuse%20est%20pratiqu%C3%A9e,la%20date%20des%20derni%C3%A8res%20r%C3%A8gles)
- Statistisches Bundesamt (Destatis). Gesundheit Schwangerschaftsabbrueche 2019. [cited 2020 Nov 18]. Available from: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Schwangerschaftsabbrueche/_inhalt.html#sprg235868 2020; Fachserie 12 Reihe 3.
- Arznei-Telegramm. Jetzt auch in Deutschland: Mifepriston (RU 486; Mifegyne) für den Schwangerschaftsabbruch. 1999 [cited 2020 Nov 18]. Available from: https://www.arznei-telegramm.de/html/1999_11/9911508_01.html
- ProFamilia. Schwangerschaftabbruch. 2020. [cited 2020 Nov 18]. Available from: https://www.profamilia.de/themen/schwangerschaftsabbruch.html
- Directorate of Health. Induced abortions 1982–2018. 2020 [cited 2020 Nov 18]. Available from: https://www.landlaeknir.is/servlet/file/store93/item13095/TB1_7_2012.xls
- Landspitali. [Abortion]. [cited 2020 Nov 19]. Available from: https://www.landspitali.is/sjuklingar-adstandendur/deildir-og-thjonusta/kvenlaekningadeild-bradamottaka-og-gongudeild/.
- I.Stat. Induced abortions characteristics of the event: type of intervention, antalgic therapy and gestational age. 2020 [cited 2020 Nov 18]. Available from: http://dati.istat.it/?lang=en&SubSessionId=38ea47d7-900a-4be0-b434-fe4bcbe6abb4#
- Day M. Medical abortion becomes available in Italy. Br Med J. 2010;340:c2001.
- Ministero della Salute. Relazione del Ministro della Salute sulla attuazione della legge contenente norme per la tutela sociale della maternità e per l’interruzione volontaria di gravidanza (legge 194/78). 2018 [cited 2020 Nov 18]. Available from: http://www.salute.gov.it/imgs/C_17_pubblicazioni_2924_allegato.pdf.
- Ministerie van Volksgezondheid, Welzijn en Sport. Jaarrapportage Wet Afbreking Zwangerschap 2018. 2020 [cited 2020 Nov 18]. Available from: https://www.igj.nl/publicaties/rapporten/2020/02/06/jaarrapportage-wet-afbreking-zwangerschap-2018
- Løkeland M, Iversen OE, Engeland A, et al. Medical abortion with mifepristone and home administration of misoprostol up to 63 days’ gestation. Acta Obstet Gynecol Scand. 2014;93(7):647–653.
- Helse norge. Information for anyone considering having an abortion. 2020 [cited 2020 Nov 18]. Available from: https://www.helsenorge.no/en/sex-og-samliv/information-for-anyone-considering-having-an-abortion/
- Direção-Geral da Saúde. Relatório dos registos das interrupções da gravidez 2018. 2019 [cited 2020 Nov 18]. Available from: https://www.dgs.pt/portal-da-estatistica-da-saude/diretorio-de-informacao/diretorio-de-informacao/por-serie-1144918-pdf.aspx?v=%3d%3dDwAAAB%2bLCAAAAAAABAArySzItzVUy81MsTU1MDAFAHzFEfkPAAAA
- Public Health Scotland. Termination of pregnancy year ending December 2019. 2020 [cited 2020 Nov 18]. Available from: https://beta.isdscotland.org/find-publications-and-data/population-health/sexual-health/termination-of-pregnancy-statistics/
- Slovenia National Institute of Public Health. Fetal death monitoring information system/notification of foetal death –abortion (Form 8,171). Private correspondence dated 17.11.2020.
- Ministerio de Sanidad. Interrupcion Voluntaria del Embarazo: Datos deifinitivos correspondientes al ano 2018. 2020 [cited 2020 Nov 18]. Available from: https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/embarazo/.
- Junta de Castilla y Leon. Información previa al consentimiento de la interrupción voluntaria del embarazo. 2016 [cited 2020 Nov 18]. Available from: https://www.saludcastillayleon.es/en/salud-mujer/informacion-ive-interrupcion-voluntaria-embarazo/informacion-general.files/122083-Informaci%C3%B3n%20Previa%20al%20Consentimiento%20de%20la%20Interrupci%C3%B3n%20Voluntaria%20del%20Embarazo.pdf
- Socialstyrelsen. Bilaga – Tabeller – Statistik om aborter 2019. 2020 [cited 2020 Nov 18]. Available from: https://www.socialstyrelsen.se/en/search-results/?q=abortion+2019
- Umo. Abort. [cited 2020 Nov 18]. Available from: https://www.umo.se/kroppen/graviditet/abort/.
- Office Fédéral de la Statistique. Interruptions de grossesse. 2020 [cited 2020 Nov 18]. Available from: https://www.bfs.admin.ch/bfs/fr/home/statistiques/sante/etat-sante/reproductive/interruptions-grossesses.html.
- Office Fédéral de la Statistique. Statistique des interruptions de grossesse 2014. Neuchâtel: Office Fédéral de la Statistique; 2015.
- Santé Sexuelle Suisse. Interruption de grossesse. [cited 2020 Nov 18]. Available from: https://www.sante-sexuelle.ch/themes/grossesse-voulue-non-voulue/interrompre.
