Abstract
The majority of adolescent girls in rural India lack awareness regarding menstrual hygiene management (MHM), access to sanitary absorbents and necessary facilities in schools, homes, and workplaces. This study evaluated an intervention to strengthen a public health programme aimed to increase the use of safe, sanitary absorbents and knowledge of MHM among tribal adolescent girls. This project was implemented in 202 villages of two sub-districts of Narmada district in Gujarat, India, for one year (2018–2019). The intervention consisted of capacity building of 892 government frontline health workers and teachers, followed by supportive supervision. Convergence with concerned departments was achieved through meetings with stakeholders. “MHM-corners” and “MHM-Committees” were created at schools and Anganwadi-centres to improve access to menstrual absorbents and information. Household surveys of adolescent girls were conducted at baseline (n = 507) and end-line (n = 550) in 27 randomly selected villages to evaluate outcomes. Of 550 girls at the end-line, mean age 16.3 years, 487 (88.5%) were tribal, and 243 (44%) were out-of-school. The primary outcome of interest, the proportion of adolescent girls using safe, sanitary absorbents, increased from 69% to 90.5% (OR: 5.19, CI: 3.61–7.47). Their knowledge of the uterus as the origin of menstrual blood and hormonal changes as the cause for menstruation improved from 6.3% to 66% (p-value < 0.001) and 7.5% to 73% (p-value < 0.001), respectively. School absenteeism during menstruation reduced from 24% to 14% (p-value < 0.001). It is possible to improve MHM knowledge and practices among adolescent girls from tribal communities by utilising existing government systems. Awareness and access to safe absorbents can lead to safe and hygienic MHM practices.
Résumé
La majorité des adolescentes en Inde rurale sont mal informées de la prise en charge de l’hygiène menstruelle, de l’accès aux protections hygiéniques et aux équipements nécessaires dans les écoles, à domicile et sur le lieu de travail. Cette étude a évalué une intervention destinée à consolider un programme de santé publique visant à accroître l’utilisation de protections hygiéniques sûres et à élargir les connaissances sur la prise en charge de l’hygiène menstruelle chez les adolescentes de communautés tribales. Ce projet a été mis en œuvre dans 202 villages de deux sous-districts du district de Narmada dans l’État du Gujarat, en Inde, pendant un an (2018-2019). L’intervention consistait à renforcer les capacités de 892 enseignants et agents de santé gouvernementaux de première ligne, avec une supervision de soutien par la suite. La convergence avec les départements concernés a été obtenue grâce à des réunions avec les parties prenantes. Des « coins de prise en charge de l’hygiène menstruelle » et des « comités de prise en charge de l’hygiène menstruelle » ont été créés dans les écoles et les centres Anganwadi pour élargir l’accès aux protections sanitaires et aux informations. Des enquêtes auprès d’adolescentes ont été réalisées au début (n = 507) et à la fin (n = 550) de l’intervention dans 27 villages sélectionnés de manière aléatoire pour évaluer les résultats. Des 550 jeunes filles interrogées à la fin de l’intervention, dont l’âge moyen était de 16,3 ans, 487 (88,5%) étaient issues de communautés tribales et 243 (44%) n’étaient pas scolarisées. Principal résultat intéressant, la proportion d’adolescentes utilisant des protections hygiéniques sûres est passée de 69% à 90,5% (RC: 5,19, IC: 3,61-7,47). Elles étaient 66% à savoir que l’utérus est à l’origine du sang menstruel, contre 6,3% au début de l’intervention (valeur-p < 0,001), et 73% à comprendre que des changements hormonaux provoquent les menstruations, contre 7,5% au début de l’intervention (valeur-p < 0,001). L’absentéisme scolaire pendant les menstruations a été ramené de 24% à 14% (valeur-p < 0,001). Il est possible d’améliorer les connaissances de la prise en charge et des pratiques d’hygiène menstruelle chez les adolescentes de communautés tribales en utilisant les systèmes gouvernementaux existants. Les activités de sensibilisation et l’accès à des protections sanitaires sûres peuvent conduire à de bonnes pratiques de prise en charge de l’hygiène menstruelle.
Resumen
La mayoría de las adolescentes en las zonas rurales de India carecen de conocimientos sobre el Manejo de la Higiene Menstrual (MHM), acceso a absorbentes higiénicos e instalaciones necesarias en escuelas, hogares y lugares de trabajo. Este estudio evaluó una intervención para fortalecer un programa de salud pública cuyo objetivo era aumentar el uso de absorbentes higiénicos seguros y los conocimientos de MHM entre adolescentes tribales. Este proyecto fue ejecutado en 202 poblados de dos subdistritos del distrito de Narmada, en Gujarat, India, durante un año (2018-2019). La intervención consistió en el desarrollo de capacidad de 892 trabajadores de salud de primera línea y maestros gubernamentales, seguido de supervisión capacitante. Se logró convergencia con los departamentos involucrados por medio de reuniones con partes interesadas. Se crearon “rincones de MHM” y “Comités de MHM” en escuelas y centros Anganwadi para mejorar el acceso a información y absorbentes menstruales. Se realizaron encuestas domiciliarias de las adolescentes en la línea de base (n = 507) y en la línea final (n = 550), en 27 poblados seleccionados al azar, con el fin de evaluar los resultados. De 550 adolescentes en la línea final, con una edad media de 16.3 años, 487(88.5%) eran tribales y 243(44%) estaban fuera de la escuela. El principal resultado de interés –la proporción de adolescentes que usaban absorbentes higiénicos seguros— aumentó de 69% a 90.5% (Razón de Momios: 5.19, IC: 3.61-7.47). Su conocimiento del útero como origen de la sangre menstrual y de cambios hormonales como la causa de la menstruación mejoró de 6.3% a 66% (valor p < 0.001) y de 7.5% a 73% (valor p < 0.001), respectivamente. El ausentismo escolar durante la menstruación disminuyó de 24% a 14% (valor p < 0.001). Es posible mejorar los conocimientos y las prácticas de MHM entre las adolescentes en comunidades tribales utilizando sistemas gubernamentales ya establecidos. La conciencia y accesibilidad de absorbentes seguros puede propiciar prácticas de MHM seguras e higiénicas.
Introduction
In the context of human rights, good menstrual hygiene means the management of menstruation by women and girls safely, with privacy and dignity.Citation1 Menstrual health has been defined, in alignment with WHO’s definition of health, as a “state of complete physical, mental and social wellbeing and not merely absence of disease or information in relation to the menstrual cycle”.Citation2 Achieving menstrual health requires that girls, women and others who experience a menstrual cycle have access to accurate and age-appropriate information and are able to care for their bodies during menstruation, including access to affordable, effective menstrual absorbents.Citation2 To maintain menstrual health and hygiene, facilities should be available at all the places where women and girls spend significant periods of time: their homes, educational institutions, workplaces, health care facilities and public institutions. The inability to manage menstruation properly can adversely affect the right to education, work and health of women and girls.Citation2
Safe and effective menstrual hygiene management (MHM) has a direct impact on women’s health and development and on the achievement of the Sustainable Development Goals, 2030.Citation3 Barriers to safe and effective MHM exist in many parts of the world. For example, cultural norms enforcing untouchability of menstruating women and girls in Nepal restrict their right to food, sanitation and safety.Citation4 Even in resource-rich countries like the United States of America, low-income women suffer inequalities and deprivation related to MHM.Citation2
According to the Census of India (2011), there are 310 million women in the age group 15–49 years.Citation5 A large proportion of women and adolescent girls suffer from poor quality of life during menstruation throughout their reproductive lives due to lack of information and access to sanitary facilities and safe absorbents.Citation6,Citation7 Poor menstrual management adversely touches the lives of women from all strata of society, in rural and urban areas.Citation8 A study by Dasgupta and Sarkar in West Bengal showed that 85% of the girls were subjected to a variety of restrictions during menstruation.Citation9 Another study conducted in Maharashtra, Chhattisgarh and Tamil Nadu reported that girls in government schools dropped out of school or remained absent during their menstrual periods because of menstrual problems and inadequate facilities to manage menstruation-related basic needs like water, bathrooms, absorbents, privacy, disposal and painkillers.Citation10
Considering the low level of awareness, unhygienic practices, and silence over MHM, the Government of India has included MHM in many national policies and guidelines implemented through frontline health workers. These include the provision of subsidised sanitary pads,Citation11 the development of operational guidelines on MHM by the Ministry of Drinking Water and Sanitation,Citation12 the national Reproductive, Maternal, Neonatal, Child and Adolescent Health (RMNCH + A) strategy, the National Adolescent Health programme (Rashtriya Kishore Swasthya Karyakram or RKSK),Citation13 the “Swachh Bharat: Swachh Vidyalaya” (Clean India: Clean schools)Citation14 and a scheme for the empowerment of girls, known as Sabla.Citation15 All these schemes targeting adolescents are implemented and monitored by different government departments and different categories of frontline workers.Citation16 Moreover, the capacities of the frontline workers implementing these programmes to address MHM have been reported to be sub-optimal. Teachers hesitate to talk about reproductive health with boys and girls in school; the Accredited Social Health Activist (ASHA) and the Anganwadi Worker (AWW)Footnote† who work at the community level lack scientific knowledge regarding reproductive health and MHM.Citation17 A lack of convergence among the various government departments, each implementing their programmes, is another challenge to their ability to advance MHM among girls and women.Citation18
There is limited evidence on the outcomes of the multiple government schemes and programmes to improve adolescents’ MHM knowledge and practices. We therefore developed and implemented a scalable intervention within the government system aimed at improving MHM among adolescent girls in a rural area of Gujarat, India. This paper reports the results of the formative evaluation of this project.
Methodology
Study setting and design
The project aimed to build the capacity of frontline workers, using the existing government infrastructure, to improve MHM among adolescent girls both in and out of school. It took place from April 2018 to March 2019 in 202 villages through public schools, boarding schools, and Anganwadis of the two sub-districts of Narmada district, Gujarat, India which has a population of 188,000. Narmada is one of the aspirationalFootnote‡ districts and was selected due to its remote location and predominantly (90%) tribal population. The literacy rate was 72.3%, and the main occupation was agricultural work.Citation5
SEWA Rural, an Indian non-governmental organisation (NGO), conducted this project in collaboration with UNICEF and the Government of Gujarat. SEWA Rural is a grassroots NGO that has been providing various development and medical services in the tribal areas of Bharuch and Narmada districts of Gujarat since 1980.Citation7
Theory of change
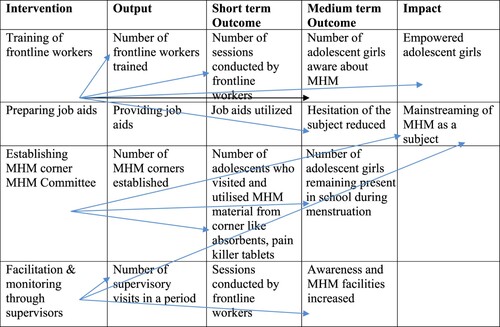
Capacity building of frontline workers and providing adolescent-friendly job aids will reduce their hesitation to talk about MHM. Awareness sessions will lead to improved knowledge among adolescents. Improved knowledge of and access to absorbents and disposal facilities would result in improved MHM practices among adolescent girls, such as hand-washing, cleaning and drying of absorbents, storage at a safe place and safe disposal of absorbents. Facilitation visits and monitoring by supervisory cadres will play an important role. Ultimately mainstreaming MHM as a subject will lead to improved and sustainable MHM ().
Interventions
Capacity building of frontline workers
We organised a one-day, module-based-training by subject experts for all the participants, in 21 groups. Two hundred and fifteen teachers, 325 AWWs, 270 ASHAs, facilitators, 82 Auxiliary Nurse Midwives (ANMs), Adolescent Health Counsellors (AHC) and supervisors participated in the training during the year 2018–2019. The topics included in the training were pubertal changes, the reproductive system, menstruation and conception, menstrual hygiene, different types of sanitary absorbents, menstrual disorders, myths related to menstruation, nutrition, early marriage, and life skills. The content of the training was the same for all, but the methodology was different as per the educational level of the participants. The training content was partly related to the school curriculum. Interactive and participatory methods were applied with all the groups. All trainees were provided with job aids such as modules, calendars, operational protocols, games, posters, and videos to facilitate sessions in their respective work areas for a duration of seven months.
Joint activities implemented by the health, education and women and child development departments
Different stakeholders, including the District Collector, District Development Officer, District Rural Development Agency, and representatives of the Departments of Health, Education and Women and Child Development, met in the convergence meetings held at regular intervals; this was facilitated by UNICEF. The “Monthly Vaccination Day” and “Adolescent Health Day” platforms organised by the health department were utilised to make adolescent girls and women at the village level aware of MHM issues. Along with adolescent girls, their mothers were involved in awareness since they are the first contact person for information and responsible for behaviour change for adolescent girls.
To create an MHM-friendly environment in schools and Anganwadis, we created a space called the “MHM corner” where access to sanitary absorbents, information on MHM, games, and painkiller tablets were made available. An “MHM Committee”, consisting of a female teacher and two girls who can be contacted for queries and are responsible for managing the MHM corner, was formed in every school.
Awareness sessions with adolescent girls
Seven sessions were planned to be conducted during the year using various media and activities, facilitated by teachers for school-going girls and by AWWs for out-of-school girls. In schools, both girls and boys were included in the sessions.
Access to absorbents and disposal facilitiesFootnote§
There was no distribution of sanitary pads as part of the project. The flannel cloth pads were available locally, and the same were made available at MHM corners by teachers and AWWs at cost.Citation7 Regarding disposal in the villages, it was routine practice to burn the used absorbents in the backyard along with the other dried waste. The school authorities have arranged for dustbins for disposal, and manual incinerators were made available by UNICEF in schools.
Supervision and monitoring
The supervisory cadres, including ANMs, ASHA facilitators, Anganwadi supervisors, and adolescent health counsellors, were trained in supportive supervision and monitoring and provided with monitoring checklists. MHM supervisors of SEWA Rural facilitated awareness sessions as well as ensuring access to sanitary absorbents. They also encouraged school authorities to create functional disposal facilities.
Participants in the intervention
Adolescent girls, frontline workers such as ASHAs, AWWs, ANMs, AHC, ASHA facilitators, teachers, their supervisors, officers of the district administration, members of state and district UNICEF teams, and members of SEWA Rural project team were participants of the study.
Definition of the primary outcome
Our primary outcome of interest was to improve the use of hygienic absorbents and to improve knowledge and menstrual hygiene practices among adolescent girls. The use of hygienic absorbents was defined as the use of disposable sanitary pads or a reusable flannel cloth pad that is washed with soap and water, sun-dried, and stored in a closed and dust-free place.Citation7 The flannel cloth pad is a menstrual absorbent that is reusable, accessible, affordable and culturally acceptable. It is red in colour and stains would not be visible, so it was culturally acceptable to dry it in sunlight. It is soft, comfortable, and has a good absorbent capacity. It is certified as safe by the laboratory.Citation7 Burning, burying, or putting in a dustbin were all considered to be safe forms of disposal.Citation11
Data collection
Recruitment of respondents and outcome measurement
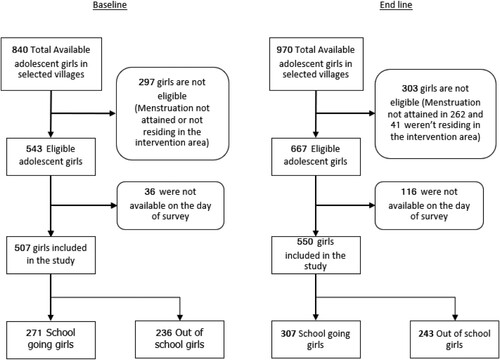
As this is an evaluation of a project that was implemented at the community level, 27 villages out of 202 villages covered by the project were randomly selected by an in-house expert not involved in project implementation. All adolescent girls in the villages were included, following the inclusion and exclusion criteria. There were 507 girls at baseline (271 and 236 school-going and out-of-school respectively) and 550 at the end-line (307 and 243 school-going and out-of-school, respectively). The same 27 villages were included in the baseline and end-line studies. All adolescent girls of these selected villages were enlisted. All menstruating girls of 10–19 years residing in the project location for a minimum of six months were eligible to participate in the study. Adolescent girls who were not menstruating and residing in non-intervention areas were excluded from the study.
Baseline and end-line data were collected individually by experienced data collectors who were not involved in the implementation of the programme. They used an open-source digital tool, “KoBo Toolbox”. Data-collectors were trained in the classroom and the field for two days. Pilot testing was done in the field, and necessary corrections were done to the tool. The data were collected individually through a survey questionnaire in the local language.
Assessment of the quality of data collection was done by an independent consultant. Five per cent of the data was collected and cross-checked in both baseline and end-line separately. For baseline data, the average concordance was found at 82% in all the critical variables and 87% for the end line.
We also used data from reports of SEWA Rural’s supervisors regarding their facilitation visits and coverage of adolescents in schools and Anganwadis.
Sample size
Based on the results of a nationally conducted survey in 2015–2016 (NFHS-4), we assumed that 48% of adolescent girls were using safe, hygienic absorbents at the baseline.Citation19 We expected that 60% of adolescent girls would use safe, sanitary absorbents at the end-line. For the power of 95% and 5% two-sided significance level, we estimated that 459 adolescent girls would need to be sampled in the baseline and end-line surveys each, to detect 12% absolute improvement in the primary outcome. The sample size was determined as 500 girls, considering a 10% sample loss.
Data analysis
Digitally collected data was available in an MS Excel sheet and analysed using SPSS23. We used the Pearson Chi-Square test for calculating the P-value. The socio-demographic characteristics of participants included at baseline and end-line were compared. The participants at baseline and end-line were similar except for age, education, mother’s education and family poverty status. Therefore, we included these four variables in logistic regression.
Ethical considerations
All personally identifiable information was removed, and unique numbers were assigned to participants, which were available only to investigators. Completed data collection forms were stored in a secured digital location. As the participants are adolescents, informed consent in the local language was sought from parents of all girls up to 18 years and self-consents for girls of age 19 years. The study protocol was approved by the institutional ethics committee (SEWA Rural IEC) on 26 June 2018.
Results
Five hundred and seven girls (271 school-going and 236 out-of-schools) who were available and eligible in the village were interviewed during the baseline survey. Similarly, 550 girls (307 school-going and 243 out-of-schools) were interviewed at the end-line ().
Most of the adolescents were from tribal communities and low-income families. Almost half of the adolescents surveyed were school dropouts and involved in agricultural work. Most of the households and schools had a water supply. Half of the respondents did not have pucca (permanent) bathrooms and functional toilets that would ensure privacy and availability of water to maintain hygiene with dignity ().
Table 1. Socio-demographic characteristics of adolescent girls in tribal areas of Gujarat (N=1057)
During the intervention, 892 (99%) frontline workers were trained in MHM. Teachers and Anganwadi workers covered 9284 (92%) school-going adolescent girls and 7200 (72%) adolescent boys; and 2647 (90%) of the out-of-school adolescent girls from all 202 villages in the awareness sessions. Over seven months, post-training MHM corners were created at almost all schools and Anganwadi Centres. Five facilitation visits by the project team were done for each frontline worker during the project period. Four convergence meetings with different departments were conducted ().
Table 2. Output indicators: adherence to intervention among adolescent girls in tribal areas of Gujarat
The job-aids helped frontline workers to explain the topic of MHM in more detail and without hesitation through the participation of adolescents in games like snakes and ladder and cards. The methods of teaching the topic were demonstrated during the training sessions, and these were adapted by the frontline workers. It was observed that more technical knowledge along with behavioural aspects was shared during sessions conducted in schools by teachers, while AWWs mainly emphasised behaviour change-related aspects. Although both male and female teachers were trained, female teachers were more comfortable in conducting sessions.
Data for school-going girls showed that the proportion of school-going girls reporting the presence of a disposal facility for menstrual absorbents in school increased from 39% to 69% (p < 0.001) between the baseline and end-line surveys. The proportion of girls reporting the availability of sanitary absorbents in their schools increased from 29% to 63% (p < 0.001), and the proportion of girls reporting MHM sessions at schools by teachers increased from 59% to 95% (p < 0.001) at the end-line ().
Table 3. School-level facilities among adolescent girls in tribal areas of Gujarat (N=578)*
The use of safe, sanitary absorbents during menstruation increased from 69% to 90% among adolescent girls (OR:5.1, 95% CI: 3.6–7.4). School-going girls were 5.9 (AOR:5.9, 95% CI: 3.4–10.2) times more likely not to use old cloth as sanitary absorbents at the end-line as compared to the baseline survey. The comparable figure for out-of-school girls was 4.8 (AOR 4.77, 95% CI: 2.87–7.91).
The proportion of school-going adolescent girls using safe, sanitary material increased from 73% at the baseline to 93% at the end-line (p < 0.001). Sixty-two per cent of the girls used flannel cloth pads, and 31% used commercially produced sanitary pads. Among out-of-school girls, the proportion using safe, sanitary absorbents improved from 64% to 88% (p < 0.001), with 72% using flannel cloth pad and 18% using commercially produced sanitary pads.
Hygienic practices like washing of menstrual absorbents with soap, drying in sunlight, and correct method of disposal have been improved significantly (p < 0.001). Drying flannel pads in sunlight during menstruation increased from 64% to 87% among school-going adolescent girls and from 62% to 87% in out-of-school adolescent girls (p < 0.001). Changing sanitary absorbents three to four times a day is considered a hygienic practice. The proportion adopting this practice increased from 11.4% to 38.4% among school-going girls and from 15.7% to 31.7% among out-of-school girls (p < 0.001).
Knowledge related to MHM also showed a statistically significant increase among both groups of adolescents. At the baseline, less than 10% of the girls knew that hormonal changes at puberty were responsible for menstruation and that the uterus was the source of menstrual blood. At the end-line, more than 75% of the school-going girls and more than 50% of out-of-school girls knew both these facts. The proportion of girls who knew about the association between menstruation and reproduction rose from less than 50% to close to 100%. More than two-thirds of the girls from both groups mentioned that their mothers were the main sources of information about MHM. Between the baseline and the end-line, the proportion of school-going adolescents reporting mothers as the main source of MHM information increased from 35% to 66.8% in school-going girls and from 28% to 72% among out-of-school girls. Teachers as a source increased from 7% to 28% in school-going girls. Friends were another major source of information. Very few mentioned healthcare workers as a source of MHM information.
Care-seeking for menstrual problems following the intervention almost doubled in both groups of girls. School absenteeism reduced significantly from 24.4% to 13.7% (p < 0.001). Severe pain and heavy bleeding were the main reasons for school absenteeism ().
Table 4. Sanitary material used, knowledge on menstruation and preparedness among adolescent girls in tribal areas of Gujarat (N = 1057)
Discussion
This is the first study showing the positive effects of implementing a model using government service delivery systems (frontline workers and existing infrastructure of schools and Anganwadi centres). This project was implemented successfully using government infrastructure and through capacity building of frontline workers in MHM. Through this project, we have tried to achieve convergence among health, nutrition, education and rural development departments to improve the menstrual hygiene practices of adolescent girls. Sharing a commitment to the cause also improved the ownership of the project. The presence of government officials in most of the training sessions showed the importance of the subject, increasing motivation among participants. Convergence played a significant role in helping to arrange the training sessions for frontline workers, monitoring, and in delivering sessions to the girls.
Use of safe, sanitary absorbents, MHM knowledge and hygienic practices improved and school absenteeism reduced.
The capacity-building activities reduced the hesitation of teachers to talk about MHM, and they could conduct the sessions confidently using job-aids provided to them. Studies by SinhaCitation3 and KamathCitation20 stated that health workers and teachers feel uncomfortable while talking about menstruation and emphasised building their capacity. Our study findings show that school and community education programmes were effective in improving behaviour. This finding is supported by Dongre et al. in a study done in Maharashtra, India, where community health education improved awareness of MHM in rural adolescent girls.Citation21 A systematic review by Sharma et al. on menstrual hygiene preparedness in schools in India also endorses the finding that schools can be a platform to disseminate information on menstrual hygiene through curricular and non-curricular activities.Citation18
There was a significant increase in knowledge regarding menstruation in the present study. This finding is similar to that of the studies by Mohammed and EmamCitation22 and Tegegne et al.,Citation23 where the knowledge that hormonal changes are responsible for menstruation and that menstrual bleeding originated in the uterus had improved through health education. The use of job-aids by teachers and AWWs facilitated their ability to talk comfortably about MHM. This may have led to improvements in knowledge of MHM in adolescent girls.Citation13,Citation16 DasguptaCitation9 and KamathCitation20 emphasised that educational programmes can be helpful to prevent the risk of reproductive tract infection and in maintaining a healthy reproductive life. In this study, there was an increase in the percentage of girls possessing information regarding menstruation before menarche.Citation24,Citation25 This is a positive outcome since preparedness for menarche makes a difference to girls’ feelings of fear and anxiety related to menstruation.Citation10,Citation26,Citation22
In the present study, the use of safe menstrual absorbents increased significantly. The increase may be due to an increase in knowledge as well as access to absorbents through the MHM corners in the schools and Anganwadi centres. MHM teams and MHM corners were established in the majority of schools and managed successfully by the teachers. Access to information, absorbents and painkillers was available through the MHM corners and teams. Similar findings regarding sanitary pad usage were found in other intervention studies done in Bangladesh by Haque et al.Citation27 and by Dongre et al.Citation21 in India. The MHM corners were accessible to boys as well, which is also important in creating an MHM-friendly environment at schools. A systematic review by Sharma et al.Citation18 on menstruation preparedness supports the fact that the sensitisation of male teachers and boys regarding MHM is equally important.
The study found that while there was a shift away from the use of old cloth, this was replaced mainly by the use of new flannel cloth. The increase in the use of flannel cloth may be due to its affordability, acceptability and availability in rural areas and non-affordability of sanitary pads among girls of low-income households.Citation7 For improving access to safe, sanitary absorbents, different sanitary absorbents should be made available with ASHAs, AWWs, village vendors and schools.
Unhygienic menstrual practices can lead to reproductive tract infections.Citation8 The study by Dasgupta et al.Citation9 adds that lack of menstrual hygiene in adolescence can have a long-term effect on women’s reproductive health. In our study, hygienic practices, like cleaning the genitalia, washing hands with soap before and after the use of absorbents, washing the absorbents with soap and water, drying in sunlight, changing absorbent material 3–4 times in a day, have improved significantly through the awareness sessions in schools and the Anganwadi. Similarly, a study from Bangladesh by Haque et al.Citation27 shows that health education programmes in schools lead to improved hygienic practices, while the study by Mohammed and EmamCitation22 shows improved knowledge as well as practices due to school health education in Egypt. The increase in hygienic behaviour in the present study is higher than in the Bangladesh study by Haquee al.Citation27 and the India study by Dasgupta and Sarkar.Citation9
Our study found that the improvement in knowledge and MHM practices was greater in school-going girls than out-of-school girls. Studies from Rajasthan, India and Ethiopia also found that school-going girls were more likely to adopt safe practices as compared to out-of-school girls.Citation23,Citation28 The greater improvement in school-going girls is likely due to exposure, peer group dynamics and available facilities for WASH.
The main source of information for girls was mothers. Girls mostly contacted their mothers when they started their first menstruation. Girls also depended on their mothers’ guidance whenever they faced any problems regarding menstruation or needed information pertaining to which absorbent to use, where to dry and store, and what to do when they have menstrual disorders. Other important sources were peers and teachers. Very few girls contacted the ASHAs and AWWs for their MHM-related queries. This shows that empowered mothers and teachers can lead to improved knowledge and practices.Citation22,Citation26 Mothers, who are the primary source of information, need to be involved during vaccination days (Mamta-day) and Adolescent Health Days.Citation9,Citation20,Citation22
Many girls suffered from menstrual disorders, and a few of them remained absent from school during menstruation. School absenteeism during menstruation was reduced from 24.4% to 13.7.% post-intervention. The reason for absenteeism was mainly pain and heavy bleeding.Citation10 The availability of WASH facilities at school is essential to reduce school absenteeism. There was a taboo against taking any tablets for treating menstrual disorders, so girls suffer and may remain absent from school, but after the intervention, the use of painkiller tablets increased from 10% to 26% and taking any treatment increased from 25% to 52%. This finding is consistent with that of the systematic review by Sivakami et al., which shows that the availability of pain medicines reduced school absenteeism.Citation10 These findings suggest that painkillers may be made available in the school medicine kits.
All the factors at schools, the workplace or in the community, including cultural norms that prevent dignified menstrual hygiene, are a barrier to human rights. Almost 90% of the girls in our study area are isolated from daily household activities like cooking food, visiting religious places or attending social events, when they are menstruating. Similar findings were present in West Bengal, as shown in the study by Dasgupta and Sarkar, where 85% of adolescent girls faced some kind of restriction due to menstruation.Citation9 Having a culturally sensitive programme that could address cultural norms about menstruation would address not only access to education but adolescent girls’ safety, which is a human right and needs to be emphasised in related programmes.Citation2,Citation29 Girls should be provided with their basic rights of sanitation, hygiene and safety.Citation30
Limitations of the study are the absence of a control group and the short duration of the intervention period. Further research will be useful to test this intervention for a longer duration using randomised control trials. Moreover, the implementers and evaluators of this project were the same, which may have created a bias. Our area is tribal and the results may not be generalisable. Further study could be done in an urban setup to generalise findings. However, many studies corroborate the findings from our study about the improvement in knowledge and menstrual hygiene practices from education interventions and these lessons can be widely applied.
Lessons learned and reflections
Looking at MHM through the human rights angle is the key to dignified menstruation management among adolescent girls. This study demonstrates that it is possible to enhance MHM among adolescents from socially marginalised groups, through interventions led by the public health system and implemented through government departments. MHM should be part of the school curriculum so that it will be sustainable and accessible to all school-going adolescents, supplemented by programmes for out-of-school girls. The technical support and handholding of frontline health workers of the government departments by an experienced local NGO was an important ingredient of the project and such collaborations between experienced NGOs and government departments can be useful. The study found that convergence among different government departments was important for satisfactory adherence to the intervention. Ensuring a shared vision among the stakeholders leads to effective implementation as well as better chances for sustainabilityCitation18 and is a critical operational requirement. Capacity building of teachers, Anganwadi workers, ASHAs and ANMs and equipping them with user-friendly job aids helps to reduce hesitation to talk about MHM. The involvement of male teachers and male adolescents helps to break the silence around menstruation. Involvement of mothers at the community level is important because mothers are often the main source of information on MHM. All the same, it is useful to have trained and experienced frontline workers as a source of information and a contact point for queries related to MHM for mothers and adolescents. Making available diverse types of absorbents gives girls a choice. At present, there is no monitoring or reporting system of MHM services in schools or Anganwadis. There is a need for efficient MIS software to monitor the availability and effectiveness of the intervention and to ensure transparency and accountability.Citation18
Acknowledgments
This was a joint study and implementation project of SEWA Rural, UNICEF, and the Government of Gujarat. The authors are very grateful for the support provided by district authorities, especially the District Collector and District Development Officer. The authors are acknowledging the support and cooperation provided by government officials of ICDS, the Health and Education department and their staff. UNICEF played a critical role in providing financial and technical support especially enabling convergence, BCC materials and training modules. The authors are thankful to our project team for their immense contribution and independent consultant for data verification. Lastly, the authors are acknowledging the adolescent girls and their parents without whom the study could not be possible.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes
† Anganwadi is the designated centre in the village where nutrition, education and health-related activities are implemented. Children of 0–6 years, out-of-school adolescent girls, pregnant and lactating mothers are enrolled in their village’s Anganwadi to get pre-school education, health awareness and supplementary nutrition. Each Anganwadi is handled by an Anganwadi worker (AWW) and a helper.
‡ The Government of India has identified 115 districts from 28 states with poor socioeconomic indicators as “aspirational districts” which are to be prioritised by development programmes.
§ However, two sanitary pad production units run by Self Help Groups were started through independent efforts by District Rural Development Authority (DRDA) in two villages that had distributed the sanitary materials in nearby villages at one time only.
References
- Human Right Watch. Understanding menstrual hygiene management and human rights. Wash United; 2017.
- Winkler IT. Human rights shine a light on unmet menstrual health needs and menstruation at the margins. Obstet Gynecol. 2019;133:235–237.
- Sinha R. Menstrual hygiene management in India: The concerns. Indian J Public Health. 2018;62:71–74.
- Amatya P, Ghimire S, Callahan KE, et al. Practice and lived experience of menstrual exiles (Chhaupadi) among adolescent girls in far-western Nepal. PLoS One. 2018;13:e0208260.
- Census of India. Sample registration system statistical report 2011; 2011. Available from: http://www.censusindia.gov.in/vital_statistics/SRS_Report/9Chap 2 - 2011.pdf .
- Dasra USAID, Kiawah T. Spot On! Improving Menstrual Health and Hygiene in India; 2015. Available from: www.dasra.org.
- Shah SP, Nair R, Shah PP, et al. Improving quality of life with new menstrual hygiene practices among adolescent tribal girls in rural Gujarat, India. Reprod Health Matters. 2013;21:205–213.
- Sumpter C, Torondel B, RezaBaradaran H. A systematic review of the health and social effects of menstrual hygiene management. PLoS One. 2013;8:1–15.
- Dasgupta A, Sarkar M. Menstrual hygiene: How hygienic is the adolescent girl? Indian J Community Med. 2008;33:77.
- Sivakami M, van Eijk AM, Harshad T et al. Effect of menstruation on girls and their schooling, and facilitators of menstrual hygiene management in schools: surveys in government schools in three states in India, 2015. J Glob Health. 2019;9:1–13.
- National Rural Health Mission. Operational guidelines-promotion of menstrual hygiene among adolescent girls (10-19 years) in rural areas. Strategy; 2010. Available from: http://www.who.int/lep/resources/SEAGLP20062.pdf.
- Ministry of Drinking Water and Sanitation. Menstrual Hygiene Management: National Guidelines. Sustainable Sanitation and Water Management; 2015. Available from: https://mdws.gov.in/sites/default/files/Menstrual Hygiene Management - Guidelines.pdf%0Ahttp://www.sswm.info.
- Ministry of Health and Famly Welfare Government of India. A strategic approach to reproductive, maternal, newborn, child and adolescent health (RMNCH + A) in India for healthy mother and child; 2013. Available from: http://nrhm.gov.in/images/pdf/programmes/rmncha-strategy.pdf.
- Ministry of Human Resource Development. SWACHH BHARAT-SWACHH VIDYALAYA CAMPAIGN. vol. September (2014).
- National institute of Public Cooperation and Child Development. Sabla Module. 2011;269.
- UNICEF India & Sarva Shiksha Abhiyan. Roadmap for Menstrual Hygiene Management; 2017.
- Geertz A, Iyer L, Kasen P, et al. Menstrual health in India | country landscape analysis. Reprod Health Matters. 2016;51:1–25.
- Sharma S, Mehra D, Brusselaers N, et al. Menstrual hygiene preparedness among schools in India: A systematic review and meta-analysis of system-and policy-level actions. Int J Environ Res Public Health. 2020;17:647.
- International Institute for Population Sciences. National Family Health Survey (NFHS-4) 2015-16 India. International Institute for Population Sciences (IIPS) and ICF. 2017. Available from: http://rchiips.org/NFHS/NFHS-4Reports/India.pdf (2017) doi:kwm120 [pii]10.1093/aje/kwm120.
- Kamath R, Ghosh D, Lena A, et al. A study on knowledge and practices regarding menstrual hygiene among rural and urban adolescent girls in Udupi Taluk, Manipal, India. Glob J Med Public Helath. 2013;2:1–9.
- Dongre AR, Deshmukh PR, Garg BS. The effect of community-based health education intervention on management of menstrual hygiene among rural Indian adolescent girls. World Health Popul. 2007;9:48–54.
- Mohammed E, Emam S. Impact of health education intervention on knowledge and practice about menstruation among female secondary school students in Zagazig City. J Am Sci. 2011;7:147–173.
- Tegegne TK, Sisay MM. Menstrual hygiene management and school absenteeism among female adolescent students in northeast Ethiopia. BMC Public Health. 2014;14:1–14.
- Van Eijk AM, Sivakami M, Thakkar MB, et al. Menstrual hygiene management among adolescent girls in India: A systematic review and meta-analysis. BMJ Open. 2016;6:e010290.
- Alam MU, Luby SP, Halder AK, et al. Menstrual hygiene management among Bangladeshi adolescent schoolgirls and risk factors affecting school absence: results from a cross-sectional survey. BMJ Open. 2017;7:e015508. doi:10.1136/bmjopen-2016-015508.
- Ali TS, Rizvi SN. Menstrual knowledge and practices of female adolescents in urban Karachi, Pakistan. J Adolesc. 2010;33:531–541.
- Haque SE, Rahman M, Itsuko K, et al. The effect of a school-based educational intervention on menstrual health: An intervention study among adolescent girls in Bangladesh. BMJ Open. 2014;4:e004607–e004607.
- Khanna A, Goyal RS, Bhawsar R. Menstrual practices and reproductive problems: A study of adolescent girls in Rajasthan. J Health Manag. 2005;7:91–107.
- Muthengi E, Austrian K. Cluster randomized evaluation of the Nia project: study protocol. Reprod Health. 2018;15:1–8.
- Chinyama J, Chipungu J, Rudd C, et al. Menstrual hygiene management in rural schools of Zambia: A descriptive study of knowledge, experiences and challenges faced by schoolgirls. BMC Public Health. 2019;19:1–10.