ABSTRACT
This study examines the association of decision-making with contraceptive use along with other measures of women’s empowerment and the gender context. We use data on currently married women from the Demographic and Health Survey conducted in Pakistan in 2017–2018. We contrast patterns in modern contraception with traditional contraception and examine specific modern methods. Husband’s characteristics do not factor strongly in women’s modern contraceptive use. Contraceptive decision-making is more pertinent to women’s modern contraceptive use than household decision-making and is inhibited when husbands are the primary decision-makers of contraceptive decisions. In contrast, joint decision-making facilitates overall modern contraceptive use and the use of condoms in particular. Contraceptive use is reduced when the decision is made by someone other than the woman or her husband. Economic empowerment resources are weakly and inconsistently associated with modern contraceptive use. Furthermore, modern contraceptive use (particularly condoms and female sterilisation) is reduced when women live in an extended household. Region, education, and wealth remain important correlates of modern contraceptive use, even after controlling for other factors, as does the number of living children and, for female sterilisation and IUDs only, women’s working status. This study finds support for expanding the range of available methods and combining service improvements with promoting women’s empowerment, gender equity, and social behaviour change initiatives targeted to men and other family members.
Résumé
Cette étude examine l’association entre la prise de décision et l’emploi de contraceptifs, parallèlement à d’autres mesures d’autonomisation des femmes et dans le contexte du genre. Nous utilisons des données sur des femmes actuellement mariées tirées de l’Enquête Démographique et de Santé réalisée au Pakistan en 2017-2018. Nous comparons les modèles de contraception moderne avec la contraception traditionnelle et examinons des méthodes modernes précises. Les caractéristiques de l’époux ne favorisent pas sensiblement l’emploi par les femmes de contraceptifs modernes. La prise de décision sur la contraception est plus pertinente pour l’emploi par la femme de contraceptifs modernes que la prise de décision familiale et elle est inhibée quand le mari est le principal décideur en matière de contraception. Au contraire, une prise de décision conjointe facilite l’emploi de contraceptifs modernes en général et l’utilisation de préservatifs en particulier. Le recours à la contraception est réduit quand la décision est prise par quelqu’un d’autre que la femme ou son mari. Les ressources d’autonomisation économique sont faiblement et inégalement associées à l’emploi de contraceptifs modernes. De plus, l’emploi de contraceptifs modernes (en particulier les préservatifs et la stérilisation féminine) est réduit quand les femmes vivent dans une famille élargie. La région, l’éducation et la fortune restent d’important corrélats de l’emploi de contraceptifs modernes, même en tenant compte d’autres facteurs comme le nombre d’enfants vivants et, pour la stérilisation féminine et les DIU uniquement, la situation professionnelle de la femme. Cette étude trouve des arguments en faveur de l’élargissement de l’éventail de méthodes disponibles, et d’une association d’améliorations des services avec la promotion de l’autonomisation des femmes, l’égalité entre les sexes et les initiatives de changement du comportement social ciblées sur les hommes et d’autres membres de la famille.
Resumen
Este estudio examina la asociación entre la toma de decisiones y el uso de métodos anticonceptivos, así como otras medidas de empoderamiento de las mujeres y el contexto de género. Utilizamos datos de mujeres actualmente casadas provenientes de la Encuesta Demográfica y de Salud realizada en Pakistán en 2017-18. Contrastamos patrones en anticoncepción moderna con anticoncepción tradicional y examinamos métodos modernos específicos. Las características del esposo no son un factor decisivo en el uso de anticonceptivos modernos por parte de las mujeres. La toma de decisiones sobre la anticoncepción es más pertinente al uso de anticonceptivos modernos por parte de las mujeres que la toma de decisiones en el hogar y es inhibida cuando el esposo es el principal tomador de decisiones relacionadas con la anticoncepción. En cambio, la toma de decisiones conjunta facilita el uso de anticonceptivos modernos en general y el uso de condones en particular. El uso de anticoncepción se reduce cuando la decisión es tomada por otra persona que no sea la mujer o su esposo. Los recursos de empoderamiento económico están asociados superficial e incoherentemente con el uso de anticonceptivos modernos. Más aún, el uso de anticonceptivos modernos (en particular los condones y la esterilización femenina) se reduce cuando las mujeres viven en un hogar extendido. La región, educación y riqueza continúan siendo importantes correlatos del uso de anticonceptivos modernos, aún después de controlar otros factores, al igual que el número de hijos vivos y, en el caso de esterilización femenina y DIU solamente, la condición laboral de las mujeres. Este estudio encuentra apoyo para ampliar la gama de métodos disponibles y combinar el mejoramiento de los servicios con la promoción del empoderamiento de las mujeres, la equidad de género e iniciativas de cambio de comportamientos sociales dirigidas a los hombres y otros miembros de la familia.
Introduction
The right to control one’s reproduction is a recognised human right. It is central to individual self-determination, determining one’s life course and life opportunities. This human right “to decide freely and responsibly the number, spacing and timing of their children and to have the information, education and means to do so” is recognised in the 1994 International Conference for Population and Development’s Programme of Action (ICPD PoA)Citation1 and was reaffirmed at the Fourth World Conference on Women in Beijing.Citation2 Unhindered access to contraception is vital to achieving this right. As such, the World Conference on Human Rights articulates “a woman’s right to accessible and adequate health care and the widest range of family planning services, as well as equal access to education at all levels”.Citation3
Pakistan has had an active family planning programme since the 1950s. More recent investments reflect a reorientation away from the population growth concerns that motivated the programme in its early days and towards public health delivery systems that centre responsiveness to women’s reproductive health needs, rights, and informed choice. Pakistan has made commitments to the London Summit on Family Planning in 2012 and developed Costed Implementation Plans to increase contraceptive prevalence and reduce unmet need among reproductive age women.Citation4–8 The government has committed to ensuring a range of available methods in-country and has trained mid-level service providers in the public and private sectors to provide intrauterine devices (IUDs) and implants. These plans emphasise providing newly married couples with access to family planning methods at a low and affordable cost.
Nonetheless, data from successive Demographic and Health Surveys (DHS) in Pakistan indicate that early gains in contraceptive use have stalled and unmet need for family planning has plateaued since 2012.Citation9 Seventeen percent of currently married women have an unmet need for family planning, with unmet need for spacing (10%) exceeding that for limiting (8%).Citation9
Female sterilisation and condoms (9% of currently married women) are the most common modern methods of contraception. Use of other modern methods lags, with no more than 3% of currently married women using injectables, IUDs, or the pill. This method dominance in the method mix may signal limitations on informed choice.Citation10,Citation11 Analyses conducted by Track20 indicate that contraceptive use lagging behind demand raises concerns about “a wider set of social constraints that may be influencing the motivation to use, or not use, contraception.”Citation12 The family planning programme has not yet succeeded in ensuring women in Pakistan can fully realise their right to determine whether, when, and how many children to have.
One contributing factor limiting the use of modern contraception may be the relative disempowerment of women. Pakistan, as with neighbouring South Asian countries, reflects patriarchal gender norms.Citation13–15 This includes patrilineal lines of marriage and an emphasis on fertility as a source of women’s status; the practice of purdah; distinctly gendered spheres, with men active in economic and political spheres and women active in domestic and reproductive spheres; and constraints on women’s independent decision-making.
A large literature demonstrates a positive relationship between women’s empowerment and reproductive health outcomes and the ability to articulate and achieve fertility intentions and levels of contraceptive use.Citation16,Citation17 These associations also extend specifically to contraceptive use.Citation18–21 The ICPD PoA declares the empowerment and autonomy of women to be an important end in itself, as well as critical for the right to attain the highest standard of sexual and reproductive health.Citation1,Citation2
Kabeer defines empowerment as the process by which women expand the “ability to make strategic life choices in a context where this ability was previously denied to them”.Citation22 Her conceptual framework describes an iterative cycle in which empowerment resources contribute to agency (direct empowerment), which results in empowerment achievements (outcomes). In applications of this and complementary conceptual frameworks, measures of agency are most often operationalised as decision-making power. Researchers have recently focused on developing improved measurement of women’s empowerment and most conceptual frameworks and empirical studies centre decision-making.Citation17,Citation20,Citation21,Citation23–25 Among these are efforts to understand the inner processes of decision-making within couples or households as they relate to various types of decisions.Citation19,Citation26,Citation27 Meanwhile, empowerment is multi-dimensional, encompassing socio-cultural, domestic, economic, political, legal, and other domains;Citation28 although these are linked, women can be more empowered in some areas and less empowered in others. This suggests that measures of empowerment should span various types of decisions and multiple areas of women’s lives.
In conservative settings like Pakistan, women are frequently not the only ones who influence their reproductive behaviour. Much attention is focused on the role of men, namely husbands, in making fertility-related decisions. However, other actors such as mothers-in-law also impact these decisions.Citation29 As such, factors like household structure and size, the joint family system, and husband’s characteristics may influence a woman’s use of contraception and ability to achieve their reproductive rights.
Given stagnating levels of contraceptive use and unmet need in Pakistan, it is important to understand the role of women’s empowerment in shaping patterns of contraceptive use. Therefore, this study examines the factors associated with contraceptive use, with a focus on women’s empowerment. We incorporate multiple measures of decision-making, specific to contraceptive decisions and general household decisions, as well as economic empowerment resources. We analyse the role of decision-making amidst other controls as well as additional variables that describe the gender context, such as husbands’ characteristics and household type. We analyse several contraceptive outcomes, including type of contraception and specific contraceptive method.
Methods
Data
This study uses women’s data from the 2017–18 Pakistan DHS (PDHS) survey. This is the fourth DHS survey, but the first to have complete regional coverage; its data represent the population of Pakistan including all four provinces and the regions of Azad Jammu and Kashmir (AJK), the former Federally Administrated Tribal Areas (FATA), and Gilgit Baltistan, which were not included in all prior surveys.Citation9 The 2017–18 PDHS is representative at the national level, provincial level, and of urban and rural areas. 2017–18 PDHS data are freely available at https://dhsprogram.com/Data/.
The PDHS applied a multi-stage, clustered sampling approach in which the number of clusters (with enumeration areas as the primary sampling units) per region was selected proportional to the size of the region and a predetermined number of households per cluster were randomly selected. All eligible women in selected households were selected for interview. The eligible woman response rate was 94%.
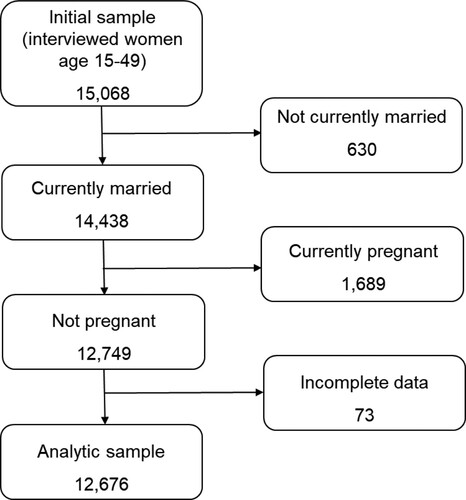
All analyses in this study use currently married women ages 15–49 as the analytic sample. Because most women eligible for interviews are currently married, the restriction to currently married women results in a small attrition of 630 women (). Analysis of determinants of modern contraceptive use is further restricted to women who are not pregnant at the time of the survey, excluding another 1,689 women. Further restriction to cases with complete data on all covariates in the model results in a final sample of 12,676 currently married, non-pregnant women.
All analyses in this study apply sampling weights that account for sampling probability and non-response. We estimate robust standard errors and use the svy suite of commands available in Stata 16 ME to adjust for the clustered sampling design.
Analytical strategy and measures
To identify factors associated with the use of contraception and specific modern methods, we estimate bivariate and multivariable multinomial logistic regression models. First, we estimate a multinomial model using a three-category outcome variable: uses any modern method of contraception, uses any traditional method, and uses no method of contraception (the reference category).
Next, a second multinomial regression is estimated to identify factors associated with specific modern methods, with “no modern method” as the reference outcome compared to the use of six specific methods of modern contraception. To ease interpretation of results for both multinomial regressions, we present relative risk ratios (RRRs), which, like odds ratios, are the exponentiated coefficient β. We present both unadjusted RRRs from separate bivariate models and adjusted RRRs from multivariable models that control for multiple factors simultaneously.
Modern methods are defined as male condoms, female sterilisation, injectables, IUDs, pills, male sterilisation, implants, lactational amenorrhoea method (LAM), emergency contraception (EC), and standard days method (SDM). Traditional methods are periodic abstinence, withdrawal, and other (unspecified) traditional methods. For the second outcome, the multinomial model distinguishes among each of the following modern methods: male condoms, female sterilisation, injectables, IUDs, pills, and “other” modern methods. “Other modern methods” combines all methods used by <1% of currently married women: male sterilisation, implants, LAM, EC, SDM, and other modern methods not identified.
In this study, we use two separate decision-making variables. The first, household decision-making, is a count variable of the number of household decisions that women participate in, either solely or jointly with their spouse. This index ranges from 0 to 4 and draws from the following four decisions: health care for oneself, making major household purchases, visits to family or relatives, and how to spend money that her husband earns. A higher value indicates participation in more household decisions. This construction as a count variable assumes that the four component decisions are of equal weight and equivalently meaningful with regard to contraceptive use. Although we conducted no formal test, each of the four decisions shows a similar-sized effect in bivariate analysis of traditional and modern contraceptive use, with unadjusted RRRs ranging from 1.3 to 1.5, suggesting that this assumption is reasonable.
The second decision-making variable is specifically related to contraceptive use. This variable is calculated for all women, regardless of current contraceptive status. Women who are currently using contraception are asked, “Would you say that using contraception is mainly your decision, mainly your husband’s decision, or did you both decide together?” while women who are not using contraception are asked an almost identically worded question, “Would you say that not using contraception is … ”. Decisions made mainly by the respondent are the reference category for this variable.
In addition to the decision-making variables, regression models include socio-economic, fertility and demographic, health service access, and family type factors. The final regression models are specified with the following covariates: woman’s age, woman’s education, woman’s work status, control over earnings, house or land ownership, household wealth quintile, residence, region, husband’s age, husband’s educational attainment, age at first marriage, number of living children, whether permission or distance is a big problem to seek medical advice/treatment, household type, and household size. Several of these variables speak to the broader empowerment or gender context. Namely, these are woman’s work status, control over earnings, and house or land ownership (indirect measures of economic empowerment),Citation24,Citation28 age at first marriage (a proxy measure of empowerment or an empowerment resource),Citation20,Citation22,Citation24 permission to seek medical advice (a proxy measure for restrictions on mobility); and household type. An alternate specification of these models that substituted spousal age and education differences for husband’s age and education yielded similar results.
Before finalising the specification of the final multinomial regression models, we first examined potential covariates for bivariate association with the outcomes and tested for collinearity. We detected several correlations among certain variables that we expected to be correlated. Namely, among education, husband’s education, wealth, and residence; among age, number of living children, and fertility desires; and among husband’s age, number of living children, and fertility desires. The degree of correlation was modest (r ≤ 0.5) and so these variables were retained. “Fertility desires”, however, was collinear with the outcome variables because all women who were sterilised wanted no more children. This variable was excluded from the final regression models.
Results
As shown in , the majority of currently married women in our sample are not using contraception, while 10% use a traditional method and 28% use a modern method. The most common modern methods are condoms (10%) and female sterilisation (9%).
Table 1. Characteristics of the analytic sample (n = 12,676)
Approximately one-third of women participate in no household decisions, while another third participate in all four household decisions. Between 9 and 12% participate in one, two, or three of these decisions, respectively. The vast majority of the sample (77%) report making decisions whether or not to use contraception jointly with their husbands. However, the proportion that reports this decision is mainly made by their husband (11%) exceeds that making the decision mainly on their own (9%). Household decision-making and contraceptive decision-making are not correlated with one another (Pearson’s r = 0.07), indicating that these are separate areas of decision-making and women who make decisions in one of these areas do not necessarily make decisions in the other.
The sample predominantly has no education (47%) or secondary education (22%), is not currently working (84%), and lives in rural areas (66%). Nearly two-thirds (65%) of the sample married by age 20. Most currently married women want no more children (47%) followed by 27% who want a child within two years. The distance to facility is a problem for seeking medical care for twice as many women (45%) as is needing permission to seek medical care (22%). The majority of the sample live in a nuclear household (61%) while 34% live in an extended household with in-laws present and most (57%) are living in a household with 5–9 household members.
Decision-making and modern and traditional contraceptive use
To explore how decision-making may be associated with contraceptive use, we estimate a multinomial regression model with these and other factors. We first estimate separate models to produce unadjusted RRRs and then a final, multivariable model with all factors combined and present adjusted RRRs in . The reference category of the outcome is “no contraceptive use” against which we compare the use of traditional and modern contraception. In separate, bivariate multinomial regression models, nearly all covariates showed an association with either traditional or modern contraceptive use or both.
Table 2. Covariates associated with the use of traditional or modern contraception: results of multinomial logistic regression (n = 12,676)
The number of household decisions in which a woman participates is unrelated to her risk of using either modern or traditional contraception, after we controlled for other factors. However, her contraceptive decision-making is compared to women who make the decision to use or not use contraception entirely on their own, women who make the decision jointly with their husband have a higher risk of using traditional contraception (RRR 5.6, p ≤ 0.001) or modern contraception (RRR = 1.8 p ≤ 0.001) rather than no contraception. In contrast, women for whom their husband mainly makes the decision whether or not to use contraception have nearly double the risk of using traditional contraception (RRR = 1.9, p < 0.05) but nearly half the risk of using modern contraception (RRR = 0.46, p ≤ 0.001) compared to women who make the decision on their own. Women for whom the decision is made by someone else (such as another family member or a medical provider) have a greatly reduced risk of using either traditional or modern contraception.
Several other variables in the model describe the gender context beyond household and contraceptive decision-making. Women who are currently working have a 58% greater relative risk of using traditional contraception and a 37% greater relative risk of using modern contraception compared to women not working (p ≤ 0.05). Neither of the two other economic empowerment variables (control over earnings and house or land ownership) are associated with modern contraceptive use. Women who have sole control over their own earnings have 50% of the relative risk of using traditional contraception (p ≤ 0.01) compared to women with no earnings and those who own a house or land have 58% greater relative risk (p ≤ 0.05) of using traditional contraception. Age at first marriage is neither associated with traditional contraceptive use nor modern contraceptive use after controlling for other factors, although there was some bivariate association with modern contraceptive use.
The positive association between husband’s age and both traditional and modern contraceptive use disappears after we control for other factors, as does the positive association with husband’s education and these two outcomes. Similarly, women who report that getting permission to go to a facility is a big problem when they are sick and want medical advice or treatment, initially appeared to have a lower risk of using either traditional or modern contraception, although this association disappears when controlling for other factors in the multivariable model.
In contrast, household variables strengthen or remain robust in the multivariable model. Women who live in an extended family household with their in-laws or other extended household have 40% and 59% reduced risk of using modern contraception (p ≤ 0.001) compared to women in nuclear households. The relationship is similar but not as large for traditional contraception. Women who live in other extended households have a reduced risk of traditional contraceptive use (RRR = 0.6, p < 0.05), but there is no statistically significant association detected for women in extended households with their in-laws.
Household size has a positive association with contraceptive use with each additional person in the household increasing the risk of modern contraception by 22% (p < 0.01) but not traditional contraception.
Among other control variables, women’s age shows no association with traditional contraceptive use, although women’s age suggests a negative association with using modern contraception at older age groups. Education is positively associated with both traditional and modern contraceptive use, although the magnitude of this relationship is stronger for modern contraceptive use.
Wealth is similarly positively associated with both traditional and modern contraceptive use, with women in the richest household wealth quintile having five times the risk of traditional use and three times the risk of modern use compared with women in the poorest quintile. Urban residence is positively associated with traditional contraceptive use but is not associated with modern contraceptive use. The association detected with modern contraceptive use in the bivariate model is eliminated when controlling for other factors.
Selected regions show a higher or lower risk of contraceptive use, although the results are not consistent across both types of contraception. Compared with FATA, Sindh and Balochistan show a lower risk of traditional contraceptive use, while Punjab, Khyber Pakhtunkhwa, and ICT Islamabad show a higher risk of modern contraceptive use.
The positive association between the number of living children and the use of traditional and modern contraception remains robust – and increases in magnitude – in the multivariable, multinomial model. For each additional living child, a woman’s risk of using traditional contraception increases 2.4 times (p ≤ 0.001), while her risk of using modern contraception increases 2.6 times (p ≤ 0.001).
Decision-making and modern methods
To provide a more detailed examination of which contraceptive method is used, shows the results from a multivariable multinomial model of factors associated with each of the five most commonly used modern methods and a combined “other modern method” category. The reference category of the outcome variable is no modern contraceptive use. All covariates were associated with at least one of the methods in a bivariate multinomial model (supplementary material) and most retain their associations in the multivariable multinomial model. Variables that are no longer associated with the use of any modern method after controlling for other factors include residence, husband’s age, and household size.
Table 3. Covariates associated with the use of selected modern methods of contraception
The number of household decisions in which a woman participates has a negative association with pill use after controlling for other factors. The adjusted relative risk falls by 21% with each additional decision in which women are involved. However, an observed positive bivariate association with the use of condoms and female sterilisation disappears in the multivariable model.
Contraceptive decision-making is variably associated with the use of modern methods. Joint decision-making has a higher adjusted risk of using condoms (RRR = 2.95, p ≤ 0.001) than do women who make the decision to use or not use contraception independently. Women for whom the decision to use contraception or not rests mainly with their husband have a lower adjusted risk of using each of the other methods: female sterilisation (42% lower, p < 0.05), injectables (88% lower, p ≤ 0.001), IUDs (84% lower, p < 0.01), pills (84% lower, p < 0.001), and other modern methods (89% lower, p ≤ 0.001).
When the decision is made by someone other than the woman or her husband, the adjusted risk is significantly and greatly reduced for each of the methods in the outcome variable. For female sterilisation, the risk is 89% lower for these women than women who make contraceptive decisions independently (p ≤ 0.001). For the other methods, it is lower by >99%.
Women who currently work have a 44–92% heightened risk of female sterilisation and IUD use (p < 0.05), even after controlling for other factors. There is no association between work status and any other modern method, nor is there any association between control over earnings and any specific modern method. However, house or land ownership is associated with a 54% increased risk of using condoms (p ≤ 0.05) and only this method.
Few associations with husband characteristics and modern methods are observed. Husbands above age 60 have a lower adjusted risk of condom and pill use compared to men aged 15–29 (p < 0.05). Husbands with higher education have a higher adjusted relative risk of using condoms and pills and lower adjusted risk of using injectables (p < 0.05).
Age at first marriage is positively associated with condom use and negatively with female sterilisation. Women who married between ages 21 and 24 (but at no other age) have a relative risk of using injectables that is more than double that for women married between ages 10 and 14 (p ≤ 0.001).
Permission to go to a health facility has a negative association with condom use (RRR = 0.7, p < 0.01). Distance to the health facility appears unrelated to the use of any particular modern method in the presence of other factors in the model.
Women in extended households (either with in-laws or other extended household forms) have a 39–60% lower adjusted risk of using condoms and female sterilisation, while women in other extended households have a 66% lower relative risk of using injectables compared to women in nuclear households. Household size shows no such association.
Among other factors, women’s age has a negative association with each modern method, with the exception of female sterilisation, for which increasing age raises the adjusted risk. Education is associated with a higher relative risk of condom and IUD use. Wealth has positive associations with modern methods, although weaker for injectables and IUDs than for condoms and female sterilisation. Meanwhile, urban residence shows no association with any method.
Regional variation in the use of modern methods is evident. Compared to the FATA region, women in every region have a higher relative risk of using “other” modern methods and, except for Balochistan, of female sterilisation. Women in Punjab, Khyber Pakhtunkhwa, Gilgit Baltistan, and ICT Islamabad have a higher relative risk of using condoms and IUDs. Women in Gilgit Baltistan also have a higher risk of using injectables while two regions – Punjab and AJK – have significantly lower adjusted risks of using pills than FATA.
The number of living children has a strong and positive association with each of the modern methods in the model, with adjusted relative risks ranging from 2.1 for female sterilisation (p ≤ 0.001) to 3.2 for “other” modern methods (p ≤ 0.001).
Discussion
This study aimed to identify how decision-making influences the use of modern contraception, among other factors related to women’s empowerment and the gender context. We find husband’s characteristics do not factor strongly in women’s modern contraceptive use after controlling for other factors, except as they relate to decision-making. Further, our study found that the form of contraceptive decision-making is more pertinent to women’s modern contraceptive use than is the number of household decisions in which women participate. Gender equality and women’s empowerment are an important end to pursue in and of itself.Citation2,Citation3 Nonetheless, this study’s findings suggest that to the extent realising reproductive rights and meeting the demand for contraception is concerned, gender-focused initiatives should carefully target contraceptive decision-making and reproductive autonomy alongside other empowerment objectives.
While other studies have found an association between household decision-making and contraceptive use,Citation18,Citation19,Citation30 these studies lacked measures specific to contraception. The absence of an association with household decision-making in the presence of contraceptive decision-making measures suggests that household decision-making may be an adequate proxy for decision-making, broadly, when more precise measures are unavailable but that we should seek to use decision-making measures closest to the domain of the outcome.
Empowerment is multi-dimensional and women may be empowered in one domain and less empowered in another.Citation28,Citation30 Consistent with this explanation, we found only a loose correlation between household and contraceptive decision-making in Pakistan. In addition to varying levels of empowerment in different domains, the association with outcomes like contraceptive use may also vary across domains, as we see in this study. Of the two forms of decision-making, contraceptive decision-making may be more proximate to our outcome of interest – contraceptive use – and this may explain why it is associated with contraceptive use whereas household decision-making is not. Further, the ability to make decisions related to contraceptive use implies some measure of reproductive autonomy and freedom from reproductive coercion. Reproductive coercion can include either pressure to become pregnant or refusal to use/allow the use of contraception. Finally, even though the domestic and reproductive spheres are generally gendered as women’s domain, the practice in Pakistan of fathers providing financial support to their children and even grandchildren at various points from childhood throughout their adult lives may give them greater licence to involve themselves in contraceptive decision-making than in household decision-making. These explanations may make contraceptive decision-making more salient than household decision-making to actual contraceptive use.
We find modern contraceptive use is inhibited when husbands are the primary decision-maker of contraceptive decisions. Husband’s decision-making is particularly inhibiting to the use of injectables, IUDs, pills, and other modern methods. These methods generally require a visit to a health provider, underlying the “gatekeeper” role men may play in health care access.
In contrast, joint decision-making facilitates traditional contraceptive use, overall modern contraceptive use, and use of condoms, in particular. This latter finding is consistent with another study in Pakistan finding an association between joint decision-making and condoms or traditional methods.Citation19 The importance of joint versus women’s independent decision-making for these methods may derive in part from their use requiring couple cooperation.
This study also finds that the use of any modern method is greatly inhibited when the decision to use or not use contraception is made by someone other than the woman or her husband. Furthermore, modern contraceptive use in general and use of the two most common methods, condoms and female sterilisation, in particular, is substantially reduced when women live in an extended household. This finding reinforces findings in other studies in South Asia that, in addition to husbands, other family members such as in-laws may exert influence over reproductive behaviours.Citation29,Citation31,Citation32
There are several reasons that mothers-in-law may be important actors in women’s reproductive decisions. This may be due to the existence of a more family or communal orientation to decision-making as opposed to an individual orientation to decision-making, particularly with regard to major life decisions. Alternatively, mothers-in-law may hold more pronatalist preferences than do younger cohorts. These women may perceive pressure to bear a child either directly from their individual mother-in-law or through the cumulative expression of these fertility preferences as descriptive and injunctive norms. Finally, in a patriarchal system, senior women’s status may be enhanced not only through proving their own fertility but through the marriage and fertility behaviour of their sons and daughters-in-law. Mothers-in-law may encourage more grandchildren and oppose contraceptive use for the younger couple, particularly in the early years of marriage, with their influence waning over time.Citation33 Communication initiatives to improve contraceptive knowledge and supportive attitudes should target not just newly married couples but their families and the broader community as well.
Our findings regarding economic empowerment resources are mixed and generally weak. Women’s working status is associated with the use of modern contraception in general and particularly with the use of female sterilisation and IUDs. House or land ownership is associated with condom use alone, while control over earnings shows no such association. While sterilisation, IUDs, pills, and injectables are free of cost at public facilities (when available), these methods incur fees from private sources. This may be one explanation for the association between working status and female sterilisation and IUDs, likely the two most costly methods. Nonetheless, any causal direction is unclear from cross-sectional data. We do not know if women choose sterilisation and IUDs because they facilitate their ability to work, or whether working provides them with the economic resources needed to secure these methods. The absence of associations with the other economic resources measures lends tentative support for the former explanation.
Our multivariable analysis confirms that region, education, and wealth remain important correlates of modern contraceptive use, even after controlling for other factors. The number of living children that women have is another important correlate whose magnitude rivals that of attaining higher education or being in the richest quintile. This finding is consistent across all methods, with the risk of contraceptive use increasing between two times (female sterilisation) to three times (other modern methods) with each additional child. Age was not associated with either traditional or modern contraceptive use until after age 40, whereas a positive association with age may have been expected. This suggests that it is not age per se, but other life course factors with which age is correlated – namely number of living children – that influences women’s contraceptive use.
The government of Pakistan has introduced an innovative pilot scheme to enable women’s sexual and reproductive rights by covering transportation costs, as well as the free provision of contraceptive methods. This approach reflects a focus on overcoming logistical barriers, such as economic and availability barriers rather than directly influencing women’s empowerment. The findings of this study suggest that such pragmatic efforts should be accompanied by initiatives to pursue gender equality generally, and women’s empowerment in contraceptive decision-making, specifically. Given the role husbands play in contraceptive decision-making currently, it would be sensible to pursue programmes to positively engage men. This may mean increasing knowledge about contraceptive methods and fostering positive attitudes toward contraceptive use. It may also mean fostering attitudes accommodating of a greater role for women in decision-making or developing communication skills necessary for successful joint decision-making. Finally, this study found that the involvement of “other” decision-makers inhibited contraceptive use. Additional investigation is warranted into who these decision-makers are and what are their motivations for discouraging contraceptive use.
Limitations
Although this study has several advantages, it has some limitations to note. First, it is based on cross-sectional data, which limits the ability to draw causal conclusions. Secondly, the use of a count variable as a measure of household decision-making rests on the assumption that the four component decisions are of equal weight and equivalently meaningful. This is a common construction for this variableCitation30,Citation34 and, although we did not explicitly test this assumption in this study, we expect that threats to inference are low. A third limitation is that the PDHS lacks measures of reproductive coercion and autonomy. Reproductive autonomy may be one pathway by which contraceptive decision-making is translated into contraceptive use. Finally, we cannot determine who the decision-maker is when women report someone other than she or her husband made the decision whether to use contraception. This “other” decision-maker may be a mother-in-law or another family member, or it may be a health provider. This is an unfortunate limitation because the implications are very different for these two options. Recommended actions may include values clarification and refresher technical training in the case of health providers or social behaviour change and communication interventions targeting senior women and community members in the case of in-laws.
Conclusion
In summary, our findings suggest that there is ample opportunity for modern contraceptive prevalence to increase, in line with women’s desire to space and limit pregnancies, under the right conditions, namely, that is an expansion of women’s decision-making ability, whether joint or independent, as it relates to contraceptive use. Our findings provide further justification for a focus on promoting women’s empowerment and gender equity as a strategy for increasing modern contraceptive prevalence and the likelihood that women’s reproductive needs are met. These findings also suggest that social behaviour change initiatives target married men in Pakistan: a combination of efforts to expand services with social behaviour change efforts directed at not only women but also men and other family members, could reduce women’s barriers to using modern contraceptive methods of their choice.
Supplemental Material
Download MS Word (67.9 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Bogale B, Wondafrash M, Tilahun T, et al. Married women’s decision making power on modern contraceptive use in urban and rural southern Ethiopia. BMC Public Health. 2011;11(342):1–7.
- Edmeades J, Hinson L, Sebany M, et al. A conceptual framework for reproductive empowerment: empowering individuals and couples to improve their health. Washington (DC): ICRW; 2018.
- Edmeades J, Pande R, MacQuarrie KLD, et al. Two sons and a daughter: sex composition and women’s reproductive behaviour in Madhya Pradesh, India. J Biosoc Sci. 2012;44(06):749–764. DOI:10.1017/S0021932012000119
- Ewerling F, Lynch JW, Victora CG, et al. The SWPER index for women’s empowerment in Africa: development and validation of an index based on survey data. Lancet Glob Health. 2017;5(9):e916–e923. DOI:10.1016/S2214-109X(17)30292-9
- Family Planning 2020. (2020). Pakistan: commitment maker since 2012. FP2020. https://www.familyplanning2020.org/pakistan.
- Balochistan Go. Costed implementation plan on family planning for Balochistan (2018-2022). Quetta: Government of Balochistan; 2018.
- Government of Khyber Pakhunkhwa. Costed implementation plan on family planning for Khyber Pakhtunkhwa (2017-21). Paeshawar: Government of Khyber Pakhunkhwa; 2017.
- Government of Punjab. Costed implementation plan on family planning for Punjab. Lahore: Government of Punjab; 2018.
- Hafeez S. Sociology of power dynamics in Pakistan. Islamabad: Book City; 1998.
- Hameed W, Azmat SK, Ali M, et al. Women’s empowerment and contraceptive use: the role of independent versus couples’ decision-making, from a lower middle income country perspective. PLoS ONE. 2014;9(8):e104633. DOI:10.1371/journal.pone.0104633
- Hamid S, Stephenson R, Rubenson B. Marriage decision making, spousal communication, and reproductive health among married youth in Pakistan. Glob Health Action. 2011;4(1):5079. DOI:10.3402/gha.v4i0.5079
- Hinson L, Edmeades J, Murithi L, et al. Developing and testing measures of reproductive decision-making agency in Nepal. SSM-Popul Health. 2019;9:100473. DOI:10.1016/j.ssmph.2019.100473
- Jejeebhoy S. Women’s education, autonomy, and reproductive behaviour: experience from developing countries, International Studies in Demography. Oxford: Clarendon Press; 1995.
- Kabeer N. Resources, agency, achievements: reflections on the measurement of women’s empowerment. In: Discussing women’s empowerment: theory and practice. Stockholm: Swedish International Development Agency; 2001, 17–54
- Khan MS, Hashmani FN, Ahmed O, et al. Quantitatively evaluating the effect of social barriers: a case–control study of family members’ opposition and women’s intention to use contraception in Pakistan. Emerg Themes Epidemiol. 2015;12(1):1–5. DOI:10.1186/s12982-014-0022-3
- Kishor S. Women’s contraceptive use in Egypt: what do direct measures of empowerment tell us?. Paper presented at the Population Association of America; Los Angeles; 2000.
- Loll D, Fleming PJ, Manu A, et al. Reproductive autonomy and modern contraceptive use at last sex among young women in Ghana. Int Perspect Sex Rep Health. 2019;45:1–12. DOI:10.1363/45e7419
- MacQuarrie KLD, Edmeades J. Whose fertility preferences matter? Women, husbands, in-laws, and abortion in Madhya Pradesh, India. Popul Res Policy Rev. 2015;34(4):615–639. DOI:10.1007/s11113-015-9364-y
- MacQuarrie KLD. Women’s empowerment and family formation across the life course in Madhya Pradesh, India: the influence of time-varying and fixed empowerment resources using structural equations MODELS. Paper presented at the XXVI IUSSP international population conference; Marrakech, Morocco; Sep 2009.
- Malhotra A, Schuler SR. Women’s empowerment as a variable in international development. In: D Narayan, editor. Measuring empowerment: cross-disciplinary perspectives. Washington (DC): World Bank; 2005. p. 71–88.
- Meinzen-Dick RS, Rubin D, Elias M, et al. Women’s empowerment in agriculture: lessons from qualitative research. Washington (DC): IFPRI; 2019.
- Mumtaz Z, Salway SM. Gender, pregnancy and the uptake of antenatal care services in Pakistan. Sociol Health Illn. 2007;29(1):1–26. DOI:10.1111/j.1467-9566.2007.00519.x
- Nadeem M, Malik MI, Anwar M, et al. Women decision making autonomy as a facilitating factor for contraceptive use for family planning in Pakistan. Soc Indic Res. 2021: 1–19.
- National Institute of Population Studies - NIPS/Pakistan, and ICF. Pakistan Demographic and Health Survey 2017-18. Islamabad: NIPS/Pakistan and ICF; 2019; http://dhsprogram.com/pubs/pdf/FR354/FR354.pdf.
- OHCHR. Vienna declaration and programme of action. World Conference on Human Rights in Vienna, 25 June 1993; Vienna, Austria. Office of the United Nations High Commissioner for Human Rights; 1993; https://www.ohchr.org/Documents/ProfessionalInterest/vienna.pdf.
- Population Welfare Department Government of Sindh. Costed implementation plan on family planning for Sindh (2015-2020). Sindh: Population welfare department, government of Sindh; 2015; https://www.familyplanning2020.org/sites/default/files/CIP-Sindh-03-15-16-final-1_0.pdf.
- Ross J, Hardee K. Access to contraceptive methods and prevalence of use. J Biosoc Sci. 2013;45(06):761–778. DOI:10.1017/S0021932012000715
- Ross J, Stover J. Use of modern contraception increases when more methods become available: analysis of evidence from 1982–2009. Global Health: Science and Practice. 2013;1(2):203–212. DOI:10.9745/GHSP-D-13-00010
- Sathar ZA, Kazi S. Women’s autonomy in the context of rural Pakistan. Pak Dev Rev. 2000;39(2):89–110. DOI:10.30541/v39i2pp.89-110
- Track20. Exploring opportunities for mCPR growth in Pakistan. Glastonbury (CT): Avenir Health and FP2020; 2018; http://www.track20.org/download/pdf/Opportunity%20Briefs/english/Pakistan%20FP%20Opportunity%20Brief.pdf.
- UNFPA. Programme of action adopted at the international conference on population and development, Cairo, 5–13 September 1994: 20th Anniversary Edition. New York (NY): United Nations; 2014; https://www.unfpa.org/sites/default/files/pub-pdf/programme_of_action_Web%20ENGLISH.pdf.
- United Nations. Beijing declaration and platform for action. Fourth World Conference on Women; Beijing, China: United Nations; 1995; https://www.un.org/womenwatch/daw/beijing/pdf/BDPfA%20E.pdf.
- Upadhyay UD, Gipson JD, Withers M, et al. Women’s empowerment and fertility: a review of the literature. Soc Sci Med. 2014;115:111–120. DOI:10.1016/j.socscimed.2014.06.014
- Yount KM, Khan Z, Miedema S, et al. The women’s agency scale 61 (WAS-61): a comprehensive measure of women’s intrinsic, instrumental, and collective agency (August 9, 2020). SSRN. 2020.