Abstract
The COVID-19 pandemic has disproportionate effects on people living in low- and middle-income countries (LMICs), exacerbating weak health systems. We conducted a scoping review to identify, map, and synthesise studies in LMICs that measured the impact of COVID-19 on demand for, provision of, and access to contraceptive and abortion-related services, and reproductive outcomes of these impacts. Using a pre-established protocol, we searched bibliographic databases (December 2019–February 2021) and key grey literature sources (December 2019–April 2021). Of 71 studies included, the majority (61%) were not peer-reviewed, and 42% were based in Africa, 35% in Asia, 17% were multi-region, and 6% were in Latin America and the Caribbean. Most studies were based on data through June 2020. The magnitude of contraceptive service-related impacts varied widely across 55 studies (24 of which also included information on abortion). Nearly all studies assessing changes over time to contraceptive service provision noted declines of varying magnitude, but severe disruptions were relatively uncommon or of limited duration. Twenty-six studies addressed the impacts of COVID-19 on abortion and postabortion care (PAC). Overall, studies found increases in demand, reductions in provision and increases in barriers to accessing these services. The use of abortion services declined, but the use of PAC was more mixed with some studies finding increases compared to pre-COVID-19 levels. The impacts of COVID-19 varied substantially, including the country context, health service, and population studied. Continued monitoring is needed to assess impacts on these key health services, as the COVID-19 pandemic evolves.
Résumé
La pandémie de COVID-19 a des conséquences anormalement importantes sur les personnes vivant dans des pays à revenu faible ou intermédiaire, ce qui aggrave encore la faiblesse des systèmes de santé. Nous avons mené un examen de la portée dans le but d’identifier, de recenser et de synthétiser les études dans les pays à revenu faible ou intermédiaire qui ont mesuré l’impact de la COVID-19 sur la demande et la prestation de services contraceptifs et relatifs à l’avortement, ainsi que l’accès à ceux-ci, et les résultats reproductifs de ces impacts. À l’aide d’un protocole préétabli, nous avons fait une recherche dans les bases de données bibliographiques (décembre 2019–février 2021) et les principales sources de littérature grise (décembre 2019–avril 2021). Sur les 71 études incluses, la majorité (61%) ne provenaient pas de revues à comité de lecture; 42% étaient basées en Afrique, 35% en Asie, 17% portaient sur plusieurs régions, alors que 6% concernaient l’Amérique latine et la Caraïbe. La plupart des études étaient fondées sur des données antérieures à juin 2020. L’ampleur des impacts relatifs aux services contraceptifs variait largement entre les 55 études (dont 24 incluaient aussi des informations sur l’avortement). Presque toutes les études ayant évalué au fil du temps les changements dans la prestation des services contraceptifs ont noté des reculs de différentes importances, mais les graves perturbations étaient relativement peu fréquentes et d’une durée limitée. Vingt-six études abordaient les conséquences de la COVID-19 sur l’avortement et les soins post-avortement. Dans l’ensemble, les études ont observé une hausse de la demande, des réductions de la prestation des services et une multiplication des obstacles à l’accès à ces services. L’utilisation des services d’avortement a reculé, mais le recours à l’avortement et aux soins post-avortement ne faisait pas apparaître de tendance très nette, certaines études ayant constaté des augmentations par rapport aux niveaux d’avant la COVID-19. Les répercussions de la COVID-19 étaient nettement variables, en particulier selon le contexte du pays, les services de santé et la population étudiée. Une surveillance continue est nécessaire pour évaluer les conséquences sur ces services de santé essentiels, au moment où la pandémie de COVID-19 évolue.
Resumen
La pandemia de COVID-19 tiene efectos desproporcionados en las personas que viven en países de bajos y medianos ingresos (PBMI), lo que debilita los sistemas de salud. Realizamos una revisión de alcance para identificar, mapear y sintetizar estudios en PBMI que midieron el impacto de COVID-19 en la demanda, el suministro y la accesibilidad de servicios de aborto y de anticoncepción, así como los resultados reproductivos de esos impactos. Utilizando un protocolo preestablecido, realizamos una búsqueda en bases de datos bibliográficas (entre diciembre de 2019 y febrero de 2021) y fuentes de literatura gris clave (entre diciembre de 2019 y abril de 2021). De 71 estudios incluidos, la mayoría (el 61%) no fueron revisados por pares, y el 42% de ellos fueron realizados en África; el 35%, en Asia; el 17%, en múltiples regiones; y el 6%, en América Latina y el Caribe. La mayoría de los estudios estaban basados en datos recolectados hasta junio de 2020, inclusive. La magnitud de los impactos relacionados con los servicios de anticoncepción varió mucho entre los 55 estudios (24 de los cuales también contenían información sobre aborto). Casi todos los estudios que evaluaron los cambios a lo largo del tiempo en la prestación de servicios de anticoncepción observaron disminuciones de diversas magnitudes, pero las interrupciones graves fueron relativamente poco comunes o de duración limitada. Veintiséis estudios abordaron los impactos de COVID-19 en los servicios de aborto y de atención postaborto (APA). En general, los estudios encontraron aumentos en la demanda, reducciones en la prestación de servicios y aumentos en las barreras para acceder a esos servicios. El uso de servicios de aborto disminuyó, pero el uso de APA era más variado: algunos estudios encontraron aumentos, en comparación con los niveles pre-COVID-19. Los impactos de COVID-19 variaron considerablemente, por contexto del país, servicio de salud y población estudiada. A medida que evolucione la pandemia de COVID-19, será necesario continuar monitoreando para evaluar los impactos en estos importantes servicios de salud.
Introduction
Since 31 December 2019, when news of a coronavirus outbreak (later named COVID-19) was reported in China, millions of cases, resulting in mild, moderate, severe, and fatal outcomes have been recorded worldwide. The pressure exerted on healthcare systems by the pandemic has disproportionate effects on people living in low- and middle-income countries (LMICs), where it exacerbates already weak health systems.Citation1 Shortages of services and healthcare providers were magnified by diversion to contain the spread, treat COVID-19 patients and provide appropriate personal protective equipment.Citation1–3 Governmental and social responses, including lockdowns, social distancing, health facility closures, reduced transport availability, and restrictions on travel have also impacted the use of healthcare services.Citation1,Citation4 A World Health Organization (WHO) survey of Ministries of Health officials in five WHO regions found that nearly all countries reported disruptions of essential health services, with more disruptions in lower-income countries.Citation5,Citation6 In a positive direction, the pandemic prompted advancements, including greater expansion of telehealth to support continuity of care. In LMICs, such developments appear to be promising, but feasibility on a broad scale and sustainability is uncertain.Citation7,Citation8 COVID-19-related disruptions in access or use of reproductive health services also intensify existing reproductive health needs in LMICs, as pandemics typically exacerbate existing inequalities (including gender inequalities).Citation9,Citation10
Prior infectious disease outbreaks have impacted the demand for, provision of, and access to reproductive health services.Citation11 Social disturbances, lost income, changes in in-person attendance at school or work, modifications to home living arrangements or travel patterns, and increasing rates of sexual and gender-based violence Citation12 could result in changes to patterns of sexual activity or fertility desires.Citation13,Citation14 For example, at the peak of the Ebola epidemic, moderate declines (6%) in the use of family planning occurred in Sierra Leone,Citation15 while dramatic declines occurred in Liberia (65%) and Guinea (51%).Citation16,Citation17 Family planning service utilisation eventually recovered in both Liberia and Guinea.Citation16,Citation17 Other research noted that, other than condoms, contraception was not systematically offered to Ebola survivors in the Democratic Republic of Congo (DRC) and there were no improvements in contraceptive access for all women of reproductive age, despite recognition of the importance of avoiding unintended pregnancy during an outbreak.Citation18 During the 2016 Zika outbreak (a virus that directly impacted fetal development), health facilities in many affected regions were incapable of responding to increases in the demand for contraception.Citation19 While a programme implemented in Puerto Rico to increase access to contraception during Zika successfully facilitated substantial uptake of long-acting reversible contraceptive methods (LARCs),Citation20 policy-level barriers in some parts of Latin America and the Caribbean impeded access to these highly effective methods.Citation21 National policies did not change to improve access to abortion services during the Zika outbreak, and women in Brazil, Colombia, and El Salvador described resorting to unsafe abortions to meet their reproductive needs.Citation10 Despite prior examples of the impact of infectious disease outbreaks on reproductive health, these services were insufficiently prioritised in initial responses to the COVID-19 pandemic.Citation22
Rationale and objectives
The context described above indicates a need to assess the consequences of changes in access to reproductive health services during the COVID-19 pandemic.Citation10, Citation23 A synthesis of empirical evidence would be useful for policy-makers, donors, and advocates in responding to the COVID-19 pandemic and strengthening health systems. As countries seek to regain lost ground and meet all people’s needs for these services, this synthesis can also call attention to relevant empirical evidence (e.g. from nationally representative surveys or health system data) for informing model-based estimates and scenarios of the magnitude of impact of COVID-19 on sexual and reproductive health (SRH) in LMICs.
Our objectives were to identify, map, and synthesise studies in LMICs that have collected data and provided empirical (non-modelled) results on a range of outcomes related to the impact of the COVID-19 pandemic on demand for, provision of, and access to contraceptive and abortion services, as well as reproductive outcomes of these impacts.
Methods
Protocol and registration
We crafted our protocol following scoping review methodology as described in the Joanna Briggs Institute (JBI) Manual for Evidence Synthesis, Chapter 11,Citation24 which builds upon the original framework proposed by Arksey and O’Malley,Citation25 extended by Levac et al.,Citation26 and further refined over time by JBI and the JBI Collaboration.Citation27,Citation28 This approach is also consistent with the Preferred Reporting Items for Systematic Reviews statement for scoping reviews (PRISMA-ScR).Citation29 Prior to beginning our review, we searched the literature to identify whether similar scoping reviews had already been completed or were under way; our findings (supplementary material A) confirmed that our scoping review could provide a unique contribution to the literature.
On 5 February 2021, we registered our a priori protocol on the Open Science Framework,Citation30 available at: https://osf.io/jqhec. Explanations for deviations from this protocol are provided in supplementary material B. Our protocol also summarises model-based estimates of the COVID-19 pandemic impact on reproductive health services, and for which empirical data are valuable for further informing and updating.
Eligibility criteria
We included studies based in LMICs (or primarily based in LMICs, for some multi-country studies), as defined by the World Bank classification of countries by Gross National Income per capita for the 2021 fiscal year.Citation31 We included studies published in English, French, Spanish, and Portuguese, the languages for which our team could translate and review. Studies could be published either in a peer-reviewed journal (identified via an electronic bibliographic database search strategy, and published between December 2019 and February 2021) or in the grey literature (identified via searching organisational websites or pre-print servers, and published between December 2019 and April 2021). We required that studies contained empirical information on the impacts of COVID-19 on the demand for, access to, or provision of contraception and/or abortion services, or the reproductive outcomes thereof.
Information sources
We included primary empirical research publications or reports of any study design (qualitative or quantitative), and systematic reviews or meta-analyses if they included novel findings (i.e. beyond findings from individual studies otherwise eligible for primary inclusion in our review). We excluded studies based entirely or primarily on modelling, reports focused on policy changes, and letters, guidelines, blogs, op-eds, conference abstracts, and dissertations, as we considered these unlikely to contain relevant information to address our objectives. We identified relevant studies using a five-pronged approach, as detailed in .
Table 1. Five-pronged approach to identifying relevant studies
Search
Following JBI methodology,Citation24 we conducted our electronic bibliographic database search in three phases. First, we conducted an initial limited search of PubMed, and then assessed text words in the title and abstract of retrieved papers, and the index terms used. Second, we reran the search, incorporating newly identified keywords and index terms. Third, we reviewed reference lists of all included studies for additional relevant sources.
A public health informationist (LR) led the development of our electronic bibliographic databases search strategies (supplementary material C), in collaboration with the lead author (CP), and with input from all co-authors and the expert advisory group. These search strategies were peer-reviewed by another public health informationist (Claire Twose). Four co-authors (CP, AB, SS, AS) conducted searches of the grey literature, pre-print servers, and reference lists, as detailed in supplementary material D. Our expert advisory group members provided suggestions for additional relevant resources.
Selection of evidence sources
We uploaded unique references into Covidence.Citation32 Two authors independently screened titles/abstracts of each record retrieved via our electronic bibliographic database search, to determine if they merited full-text review based on our inclusion/exclusion criteria (supplementary material E). Title and abstract review for all references obtained via the grey literature search was necessarily performed by a single author (i.e. searching for and simultaneously screening titles (and where available, abstracts) of identified documents). All references that two co-authors agreed had passed title/abstract screening were moved to the full-text review stage. Full-text review was also conducted independently by two authors. We resolved all screening discrepancies via discussion or, where necessary, by eliciting the opinion of additional authors.
Data charting
We created a standardised data charting form (supplementary material F) and iteratively refined it by having five co-authors (CP, AB, SS, BAU, AS) pilot-test it using three relevant studies and discussing feedback and recommendations for improvement. After finalising the charting form, we transferred it into Covidence. Two co-authors independently charted data for each included study. Finally, any discrepancies between the two completed forms were reviewed, discussed where necessary, and finalised. For any major questions, we contacted the primary authors of included studies to request additional clarity. We did not conduct a formal critical appraisal of the studies or risk of bias assessment, as these steps are not recommended for scoping reviews. We did not collect information on sources of funding for included studies; this information was not frequently provided.
Synthesis of results
After charting the data, we conducted descriptive analysis with frequency counts to summarise data availability by geographic distribution, peer-review status, topical concepts addressed, and time of most recent data collected. We produced summaries synthesising available data pertaining to the key themes from our study objectives (impacts of COVID-19 on demand, provision, access, or reproductive outcomes pertaining to contraception, abortion, and PAC).
Expert advisory group
We assembled an advisory group (individually named in acknowledgements) with expertise on the impact of outbreaks on reproductive health or provision of reproductive health services in crises and included individuals from major SRH service delivery organisations in LMICs and international bodies engaged in reproductive health monitoring and guidance. This group provided feedback on our draft protocol (prior to registration), reviewed our list of included studies to advise if we had missed key sources, reviewed and commented on our manuscript draft prior to submission, and recommended opportunities for dissemination of our findings.
Results
Selection of sources of evidence
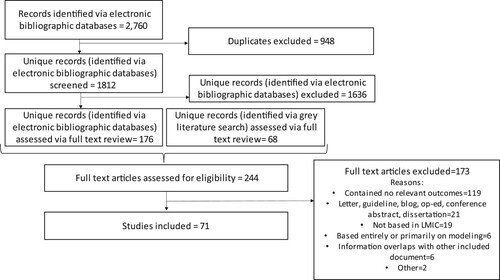
Of 1812 unique references identified via our electronic bibliographic databases, in addition to 68 unique full-text documents identified via our grey literature search, we ultimately included 71 studies ().
Figure 1. Study flow diagram
Note: It is not possible to calculate a denominator for the number of title/abstracts screened during a grey literature search, so documents deemed relevant during the grey literature search are denoted as entering the flow diagram at the full-text review stage. In addition, some full-text articles had multiple factors that made them ineligible; reasons for exclusion should be interpreted accordingly
Characteristics of sources of evidence
Of the 71 included documents, 28 were peer-reviewed and 43 were not peer-reviewed. Authors of included studies identified five studies as being conducted within humanitarian settings; however, three of these studiesCitation33–35 covered humanitarian populations as part of broader studies and did not provide findings specific for these populations, while two did so.Citation36,Citation37 A full list of the 71 included studies and key identifying information and evidence categories are in supplementary material G.
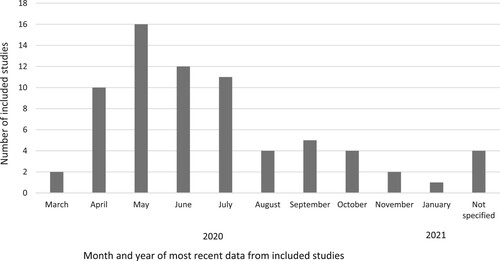
summarises the geographical distribution of included studies by region(s), subregion(s), and countries. We identified 30 studies based in Africa (over half from Eastern Africa, and primarily from Kenya), 25 from Asia (over half from Southern Asia), 12 multi-region studies (containing information from five or more countries in different regions of the world), and four studies from Latin America and the Caribbean. Forty of the 67 studies with known dates of data collection were based on data from June 2020 or earlier (); thus, our findings largely reflect evidence from the start of the COVID-19 pandemic in LMICs.
Table 2. Geographic representation of included studies
Contraception
Fifty-five studies addressed the impacts of COVID-19 on contraception, focusing on demand (n = 9), provision (n = 20), access (n = 16), or reproductive outcomes (n = 14);Citation5,Citation33–86 only 31% were peer-reviewed. Most (38 studies, 69%) involved cross-sectional or longitudinal surveys, and due to pandemic conditions, many were conducted online or by phone. Nineteen studies used administrative data (e.g. health information systems (HIS), medical records, or facilities’ service provision data). Related evidence from included studies on sexual behaviour and fertility preferences, which often undergird demand for contraceptive services, are summarised in supplementary material H.
Demand for contraceptive services
Only one of nine studiesCitation36,Citation38–40,Citation56–60 on demand for contraception had data (though retrospective) on change over time during the pandemic: an online survey using a non-probabilistic sample in Colombia showed an increase in need among adults for contraceptive supplies and visits.Citation56 Five studies highlighted levels of need during the pandemic for contraceptive information, supplies, or appointments in Colombia, Ghana, India, Kenya, Nepal, Uganda, and Zimbabwe.Citation38,Citation39,Citation56–58 The magnitude of the need for contraceptive services varied widely by study setting and population represented.
Reasons for potential change in contraceptive demand due to COVID-19 include a lack of awareness that contraceptives were being provided during the pandemic,Citation59 preferences for methods accessible with no or fewer visits to health facilities,Citation38 use of condoms to attempt prevention of coronavirus transmission,Citation60 and stigma that respondents perceived or experienced at health facilities.Citation40 Nearly all 29 key informants (in a study with organisations supporting or delivering contraceptive services in humanitarian crisis settings) said that communities were afraid to seek services due to COVID-19 risk, and demand decreased due to fear and mistrust of health authorities and systems (including in settings that had experienced Ebola outbreaks) and myths and misinformation about COVID-19.Citation36
Provision of contraceptive services
Twenty studies assessed COVID-19’s impact on contraceptive service provision.Citation5,Citation36,Citation38–55 Half (10) reported on changes in service provision, and nearly all noted declines of varying magnitude by setting.Citation5,Citation41–49 Sixty-eight percent of 105 Ministries of Health in a WHO survey (May–July 2020) reported declines of between 5% to 50% in clients receiving family planning services.Citation5 Nearly one in ten reported client declines of 50% or greater. In contrast, in a separate report on the Southeast Asia region, a WHO survey of MOH representatives reported that family planning services continued according to earlier routine schedules in seven of ten countries.Citation41 Studies using administrative data or health provider reports also showed that severe disruptions were relatively uncommon or of limited duration.Citation42–44 For example, in a study in Uganda of a representative sample of facilities that provide family planning services, just 5% suspended services during COVID-19 restrictions.Citation44
Three studies noted improvements after initial declines.Citation42,Citation43,Citation45 By November 2020, contraceptive services were scaled up compared to June 2020 or back to pre-COVID-19 levels for about half of IPPF (a global service provision organisation) Member Associations (MAs) (54 out of 105) providing SRH services, while 29 MAs reported that contraceptive services continued to be scaled down (a decrease from 39 MAs reporting this in June 2020).Citation45 Studies based on reports from contraceptive service providers in PakistanCitation42 and MozambiqueCitation43 also showed rebounds from earlier COVID-19-related declines in contraceptive service provision.
Sixteen studies described specific disruptions in or modifications to the provision of contraceptive services during the pandemic, including reduced availability or stockouts of commodities,Citation38,Citation40,Citation42,Citation44,Citation45,Citation48,Citation50–53 not being able to offer provider-administered methods (e.g. IUDs or implants),Citation36,Citation44,Citation54 health providers advising family planning clients not to seek services at health facilities,Citation55 fewer clients permitted in clinics due to social distancing measures,Citation40 and service disruptions across multiple humanitarian contexts due to mandatory restrictions, lockdowns, and curfews.Citation36 In contrast, one report of programme services across multiple countries noted a continued range of contraceptive methods available and adopted.Citation39
Access to contraceptive services
The level of perceived or experienced challenges to accessing contraceptive services varied widely across contexts, indicators, and populations, and was addressed in 16 studies.Citation33,Citation38,Citation44,Citation48,Citation52–54,Citation58,Citation61–68 For example, an online survey found that over one in three women aged 18–30 in Ghana, Kenya, Uganda, and Zimbabwe who needed family planning reported that COVID-19 affected their access to these services (34% in Ghana, 41% in Kenya, 46% in Uganda, and 38% in Zimbabwe) while this level was only 17% in Nepal.Citation38 Difficulty accessing contraception during the pandemic was common for young contraceptive users in Nairobi, Kenya (35% of adolescent girls and young women and 40% of adolescent boys and young men), and counselling on the side effects of contraceptive methods was also limited.Citation48 In two states of India, 21% of young adult women surveyed (comprising 84% of those with a family planning need) needed family planning but could not access those services.Citation58 Other studies highlighted the level of access to obtaining specific contraceptive methods, such as condoms, injectables, pills, emergency contraception, or IUDs,Citation61,Citation63,Citation64,Citation68 and only one of these showed declines over the pandemic.Citation63
Key barriers to accessing contraceptive services during the pandemic included fear of infection in generalCitation39,Citation40 and in health facilities,Citation34,Citation38,Citation44,Citation48,Citation65,Citation69 lack of transportCitation38,Citation44,Citation62 or travel-related restrictions,Citation55 cost,Citation40,Citation53 increased waiting times,Citation40 limited home visits by health workers who would normally provide contraceptive services,Citation42 lack of suppliesCitation38,Citation62 and, for adolescents in humanitarian settings, the compounding effect of other pandemic challenges, such as being out of school and isolated from peers.Citation36
Four studies described the level of contraceptive service coverage or client utilisation at a point in time during the pandemic, such as the number of clients reached.Citation35,Citation37,Citation53,Citation70 Fifteen studies based on health facility or programme data noted declines – sometimes only initially, sometimes sustained – in the number of family planning clientsCitation43,Citation44,Citation46,Citation55,Citation69,Citation71–77 or by the number of users of specific contraceptive methods over time.Citation55,Citation62,Citation69,Citation71,Citation72,Citation74–76,Citation78,Citation79 For example, in Uganda, 16% of facilities reported a large reduction in clients, 24% a moderate reduction, and 26% a small reduction during COVID-19 restrictions.Citation44 In Bangladesh, monthly service statistics showed that the use of all contraceptive methods except pills decreased by 30%–100% immediately after the national lockdown, with improvements towards pre-lockdown levels in subsequent months.Citation79 Facility data in Kenya showed significant increases in use of injectables and pills and significant decreases in the use of IUDs, implants, and emergency contraception.Citation76
Ten studies compared trends before and during the pandemic to address, in part, seasonal variation and other time-related trends in service utilisation.Citation71–80 All but one studyCitation80 documented declines during COVID-19 in at least some indicators of access to services, including the number of contraceptive method acceptors (total or by specific method), client visits, or consultations. For example, health administrative data for five countries in South Asia (Bangladesh, India, Nepal, Pakistan, and Sri Lanka) showed declines in family planning service coverage during months with the most stringent COVID-19 restrictions compared to the same period in 2019.Citation77 Monthly data from public health facilities in sub-Saharan Africa found significant monthly reductions in family planning consultations in four of seven countries studied (comparing March-July 2020 to expected levels based on HMIS data from January 2018 to February 2020),Citation75 with Mali experiencing the largest and most persistent disruptions (consultations reduced by 11-26% each month between March and July and a cumulative reduction of 17% in the five months). Other cumulative declines were 17% in Cameroon (in number of new contraceptive acceptors) and 9% in Malawi (in number of oral contraceptive users).Citation75
Reproductive outcomes of contraceptive services
Evidence on contraceptive use, specific methods used, and changes in use over time were included in 14 studies.Citation42,Citation52,Citation53,Citation56,Citation57,Citation61,Citation65,Citation67,Citation81–86 Over time, overall levels of contraceptive use as reported in population-based surveys increased to some degree,Citation57,Citation81,Citation82 remained relatively stableCitation42,Citation83 or declined slightly.Citation86 Two small-scale studies in Turkey of healthcare workersCitation84 and of female patientsCitation85 and one small-scale study in Jordan of married women recruited through social mediaCitation61 observed significant decreases in reported contraceptive use.
Five studies showed the degree of method-specific change in contraceptive use.Citation42,Citation52,Citation53,Citation67,Citation84 Two different subnational studies in Kenya found continued use of the same method among approximately nine out of ten contraceptive users.Citation53,Citation67 Three small-scale studies showed contrasting patterns in method-specific use,Citation42,Citation52,Citation84 with a slight shift from modern to less reliable contraceptive methods in Pakistan,Citation42 an increase in condom use in Turkey,Citation84 and no change in condom use in China.Citation52
Eight studies examined longitudinal contraceptive use dynamics, assessing contraceptive discontinuation or method switching during the pandemic.Citation53,Citation56,Citation57,Citation65,Citation81–83,Citation86 In general, most of these studies found that people sustained their contraceptive behaviours.Citation53,Citation57,Citation65,Citation81–83,Citation86 Variable proportions of contraceptive users across studies stopped using methods altogether, but this was in general relatively uncommon.Citation56,Citation81–83,Citation86 For example, 8% of women stopped using methods in a study in Burkina FasoCitation81 and KenyaCitation57 and 14% did so in Kinshasa, DRCCitation83, and Lagos, Nigeria.Citation86 Contraceptive method switching was also uncommon, with less than one in five respondents switching methods over the study period in five studies.Citation57,Citation81–83,Citation86 A study based on prospective, probability sample surveys in Burkina Faso and Kenya showed that most women at risk of an unintended pregnancy did not change their contraceptive status during COVID-19 (69% in Burkina Faso and 82% in Kenya).Citation65 Those who changed were more likely to initiate use (25% and 13%, respectively) rather than discontinue (6% and 5%, respectively), and those who switched transitioned to equally or more effective methods relative to their pre-COVID-19 method.
Abortion and postabortion care
Twenty-six studies addressed impacts of COVID-19 on abortion and/or PAC in terms of demand, provision, access, or outcomes;Citation34,Citation38–41,Citation45–47,Citation51,Citation52,Citation54,Citation55,Citation62,Citation63,Citation66,Citation69,Citation71–74,Citation76–78,Citation87–89 46% were peer-reviewed. The studies ranged widely in geographic coverage from a single town or facility to a multi-regional study covering 118 countries. Most used only quantitative data, two used mixed methods, and one was qualitative. More than half (54%) used administrative data primarily from HIS and facility-based data; 34% used online surveys of key informants (19%) or of individuals (15%) that were often selective of more highly educated, urban people.
Demand for abortion and PAC services
Six studies addressed the demand for abortion.Citation38,Citation39,Citation54,Citation55,Citation62,Citation63 An online survey in six countries (three in sub-Saharan Africa and three in Asia), found that 26% of young women and 30% of young men under 30 wanted information on abortion or PAC.Citation38 This study also reported that since the onset of the pandemic, 7% of young women in Zimbabwe needed PAC services. Two studies in India reported that 7% of 203 pregnant women ages 18 or older considered having an abortion (Facebook users surveyed in April 2020) and 13% of 1000 women ages 16–50 (surveyed online in July-August 2020) needed an abortion.Citation39,Citation54
In an online survey of 51 key informants in 29 countries (some of which were high-income countries) 60% reported that fear of COVID-19 was a major barrier to seeking abortion and 42% reported that women were much less likely to seek abortions during the pandemic.Citation63 Fear of infection was also reported as an important barrier to seeking abortion in other studies.Citation38,Citation54,Citation55,Citation62
Provision of abortion and PAC services
Eleven studies covered the provision of abortion-related services: 10 reported on COVID-19’s impact on provision of abortion servicesCitation38,Citation40,Citation41,Citation45,Citation51,Citation52,Citation54,Citation55,Citation63,Citation69 and two on PAC.Citation41,Citation47 Three studies reported on shortages of supplies: 12% of 121 IPPF MAs reported a shortage of safe abortion supplies in an online survey fielded 27 March—1 April 2020;Citation51 the India Family Planning Association reported on breaks in the supply chain (e.g. moving stocks from a central warehouse to branches in different states), resulting in shortages of supplies;Citation54 and a study of 117 female sex workers and 15 providers in Nairobi, Kenya reported that supplies of pregnancy test kits were inadequate, and delayed programme clients from identifying pregnancies, affecting their likelihood of seeking abortion.Citation40 Another study in India found that some providers required a COVID-19 test before surgical abortions, increasing the financial burden on the patient and leading to delays in obtaining abortions.Citation69
Some respondents in a qualitative study of people under age 30 in six countries in Asia and sub-Saharan Africa noted that private providers continued to offer abortion services during COVID-19, and that this was extremely helpful.Citation38 A FIGO survey of 51 key informants in 29 countries reported that 69% of countries with mildly restrictive abortion policies had made changes to facilitate access to abortion; in contrast, no country with highly restrictive abortion policies had made such adaptations.Citation63 A study of women obtaining reproductive health care from public facilities in Northeast Ethiopia found that more than half of women who obtained abortion did not go to facilities because of the perception that these services will not be available at facilities due to the COVID-19 crisis.Citation55
Four studies reported on broader impacts on abortion or PAC service provision.Citation41,Citation45,Citation47,Citation52 An online survey in November 2020 found that only 28% of 105 responding IPPF MAs reported that services met or exceeded pre-COVID-19 levels and 72% were below pre-COVID-19 levels.Citation45 An online survey of 1076 young people aged 15–35 years in China reported interruptions in reproductive health services (including abortion) due to COVID-19.Citation52 In contrast, a WHO survey of Ministries of Health representatives from the Southeast Asia Regional Office reported that abortion and PAC services continued to be offered at pre-COVID-19 routine schedules in facilities in seven of ten countries (excepting Indonesia, Maldives, and Sri Lanka).Citation41 The first two studies may capture on-the-ground conditions more accurately, since they surveyed providers and individuals, while the third study surveyed high-level key informants who may be reporting on the policy, and potentially less aware of actual service provision. In Pakistan, 7% of 118 providers in a May 2020 online survey reported that PAC services were disrupted at a moderate to high level.Citation47
Access to abortion and PAC services
Eight studies covered access to abortion careCitation38,Citation39,Citation46,Citation52,Citation54,Citation55,Citation62,Citation63 and one also covered access to PAC.Citation38 Two studies reported on perceptions of the decline in access to abortion services. A study of 51 key informants from 29 countries reported that 31% of respondents perceived that access to surgical abortion was much less than before COVID-19, as did 28% with respect to medication abortion.Citation63 Based on online surveys of 1000 women, a much lower proportion perceived that abortion services were available from private clinics during the pandemic versus prior: 43% versus 76% in South Africa, and 44% versus 61% in India.Citation39
A few studies assessed the actual or potential impact of COVID-19 on abortion safety. A qualitative study of young women under age 30 in six countries reported that among women who needed but could not obtain abortion/PAC services due to COVID-19, some used medication abortion (in some cases obtained from pharmacies), self-managed the abortion at home, and lacked follow up care. Others resorted to abortions using local products or went to informal providers, had unsafe abortions, and experienced delays in getting help.Citation38 Two small-scale studies in Ethiopia support these findings. In one study more than half of the small number of women who had abortions used herbs and traditional abortion providers.Citation55 The second study showed a 33% decline in average weekly gynaecological emergency visits (which include abortion) following lockdown, and authors suggested that COVID-19 preventive measures may have caused more patients to seek care from traditional healers, potentially leading to abortion complications.Citation46
Six studies provided evidence on barriers experienced in accessing abortion or PAC as a result of COVID-19.Citation38,Citation39,Citation52,Citation54,Citation62,Citation63 Two studies provided a summary indicator: 33% of women who obtained a recent abortion in China had difficulties accessing abortion care;Citation52 and in India, 72% of women who considered obtaining an abortion faced barriers to accessing the service.Citation54 The main barriers were closures of facilities and/or pharmacies or other service constraints (e.g. longer waiting times), inadequate transportation, fear of leaving home because of lockdowns or curfews, and increased cost.Citation38,Citation39,Citation54,Citation62,Citation63 One study in Nepal noted that some participants felt that appropriate safety measures were taken and did not have any hesitation in seeking abortion services;Citation62 19% of key informants in a multi-country study said that there were no barriers.Citation63
Reproductive outcomes of abortion and PAC services
Sixteen studies reported on abortion-related outcomes,Citation34,Citation38,Citation55,Citation62,Citation66,Citation69,Citation71–74,Citation76–78,Citation87–89 seven of which covered PAC.Citation34,Citation66,Citation72,Citation74,Citation76,Citation77,Citation88 Several representative or large-scale studies reported decreases in safe abortion services during COVID-19. Three studies using representative HIS data that mainly capture public sector services (in Nepal, India, and Mexico City) reported decreases of 20–40% in the number of abortions.Citation62,Citation69,Citation89 A fourth study using South African HIS data reported that abortions were dramatically lower during COVID-19 (Q2–Q3, 2020) compared to the same time period in 2019.Citation73 Another study of HIS data from one province in South Africa found a 5% decline in abortion services, with a sharper drop in second-trimester abortions.Citation71 Population Services International reported decreases in its global abortion services (covering 50 LMICs) of 20–26% for misoprostol and combined medication abortion; however, they also found an increase of 57% in manual vacuum aspirations (MVAs) services, and data are not available on the overall trend.Citation74 A UNICEF study using HIS data for India reported declines of 6% and 43% in safe abortion services in Q1 and Q2 of 2020, respectively.Citation77
Other evidence provides support for decreases in abortion services. A study of one tertiary hospital in Ethiopia reported a decrease of 16% pre- and post-COVID-19.Citation72 The number of abortion-related calls made to a public call centre service in Mexico City declined in the first week after restrictions in mobility were enacted but returned to baseline levels in week seven.Citation87 Although two studies in Nepal found an increase in the number of abortions provided, these were each of a single hospital, suggesting a shift to larger facilities, even with an overall decrease.Citation78,Citation88
Seven studies reported on the impact of COVID-19 on postabortion outcomes.Citation34,Citation66,Citation72,Citation74,Citation76,Citation77,Citation88 There are no systematic patterns in the direction of the impact, likely because of differences in contexts, including the extent to which the pandemic impacted the provision of safe abortion and PAC services, the demand for abortion, and the quality of data. Using national HIS data for Kenya, one study found no significant changes in PAC caseload, pre- and post-COVID-19 (March–June 2019 versus March–June 2020).Citation76 A UNICEF study using HIS data reported a large increase in PAC treatment in Q1 of 2020 in India (120%) and a large decline in Pakistan in Q2 of 2020 (55%).Citation77 A large-scale international provider reported a 4% increase in its PAC services in 50 LMICs worldwide (comparison of January–June 2019 versus January–June 2020).Citation74 Two small-scale studies reported increases in PAC: the caseload nearly doubled (from 4.3/month to 8.4/month) in a single-hospital study in Nepal;Citation88 and a qualitative study in Kinshasa reported increased use of PAC services from April-May to October 2020.Citation34 A study of one hospital in Ethiopia reported a 20% decrease in PAC services during the first three months of the pandemic (comparing service data for 2019 and 2020).Citation72 A non-representative, small-scale study of young people in Uganda found that 21% of the 24 women who had an abortion were unable to access PAC services.Citation66
Three studies provide evidence of the impact of COVID-19 on unwanted pregnancy. One study mentioned that half of young women surveyed in Kenya and Uganda said they would continue their pregnancy when they could not obtain abortion services due to COVID-19.Citation38 A study of women seeking care in public health facilities in a town in Ethiopia found that 15% (11 out of 72 women) reported having an unwanted pregnancy.Citation55 Of the 19% (136) of respondents who reported having any problems related to SRH, one-third had an unwanted pregnancy, in a study of young people in four regions of Uganda.Citation66
Other SRH services and outcomes
Twenty-five studies provided findings on how COVID-19 impacted SRH generally, including one or more of the three services covered in this paper (contraception, abortion, and PAC) and some other SRH interventions without disaggregation by type of service.Citation5,Citation33,Citation35–41,Citation44,Citation45,Citation47,Citation50,Citation51,Citation56,Citation62,Citation66,Citation69,Citation70,Citation81,Citation82,Citation86,Citation90–92 Several of these studies considered access to any health care, including SRH. Three of the 25 were peer-reviewed publications. Eight were multi-country studies of national-level key informants; seven were population-based (national or subnational) studies; four were qualitative or mixed methods studies; four were online, non-representative studies; and two used administrative data.
Demand for SRH services
Six studies covered the impact of the pandemic on demand for SRH services writ large.Citation5,Citation44,Citation56,Citation62,Citation66,Citation90 A study in Nigeria found an increase in demand for information on pregnancy and abortion in the first phase of lockdown and a return to pre-COVID-19 levels by June 2020, based on an analysis of Google search terms.Citation90 An online survey in Uganda reported that 23% of young people (18-30 years of age) reported fear of negative provider attitudes, and 5% reported lack of information about where to obtain SRH services.Citation66 In a WHO study, representatives from Ministries of Health in 76% of 105 responding countries reported that patients were not coming in for outpatient care due to the pandemic,Citation5 reinforced by studies in NepalCitation62 and Uganda.Citation44 A representative population-based study in Colombia reported that the proportion of respondents in need of SRH care increased from 23% in April 2020 to 40% in September 2020, reflecting barriers to obtaining care in the intervening months, including unwillingness to leave home during the quarantine (which itself increased from 12% to 32% during the same period).Citation56
Provision of SRH services
A total of 15 studies assessed provision of SRH services.Citation5,Citation33,Citation35–38,Citation41,Citation44,Citation45,Citation47,Citation50,Citation51,Citation56,Citation62,Citation69 Reductions and disruptions (of varying length and magnitude) in SRH service provision were noted by 13 of these studies.Citation5,Citation35,Citation37,Citation38,Citation41,Citation44,Citation45,Citation47,Citation50,Citation51,Citation56,Citation62,Citation69 MOH key informants in 30% of 105 countries reported at least partial disruption of SRH services; key reasons were deployment of clinical staff to COVID-19 relief (49%), insufficient personal protective equipment (PPE) (44%), closure of outpatient services (33%) and lack of supplies and commodities (30%).Citation5 Other studies suggest substantial reductions in SRH services including: a study of the 10 countries of WHO’s Southeast Asia region mentioned diversion of funding and staff allocated to SRH and adolescent and child health due to COVID-19 response efforts, as well as stockouts of some essential SRH and child health medicines, in several of these countries;Citation41 a study in Nepal reported 40-50% reduction in SRH services during the national lockdown;Citation62 in Uganda 27% of 15–49 year-olds reported reductions in clinic hours and increased absenteeism as barriers to accessing health care; Citation44 in India, distribution of supplies for social marketing organisations was disrupted and there were shortages in health workers and PPE;Citation69 and in Colombia the percent of providers discontinuing service provision increased from 5% in April to 30% in September 2020.Citation56 More moderate impacts were reported in Pakistan by May 2020 (8% of health providers in an online survey perceived a moderate to high level of disruption in contraceptive and PAC services).Citation47
A subset of the 15 studies, a series of three surveys of all national MAs and an additional Sprint survey of a subset of MAs conducted by IPPF provide valuable data to monitor change over the first nine months of the pandemic. The first survey (late March 2020) found that 11% of all service delivery points operating in 2019 had closed; 88% of 104 responding MAs had scaled down at least one service category and 36 MAs had scaled down all SRH services. The second survey (mid-late May 2020) found partial recovery in service provision (e.g. 847 clinics were closed compared to 1247 in the prior survey) and digital services were expanded (comprehensive sexuality education, counselling and information on SRH, and telemedicine) as was home delivery of SRH commodities.Citation50 However, shortfalls in SRH service provision continued to be significant.Citation35,Citation50 The third survey (November 2020) showed large improvements in the African region; 33 MAs offered self-care services for medication abortion, contraception, and HIV testing and 53 MAs offered home-based care or home delivery of SRH commodities.Citation45 However, upstream disruptions in supplies, especially contraceptives, had begun to impact availability with 78 MAs reporting procurement challenges and with the Americas region being the most impacted. A separate survey of 49 IPPF MAs that provide SRH services in humanitarian contexts reported that 61% of MAs had reduced the number of service delivery points and 73% experienced stockouts.Citation37 Two studies commented on cutbacks in the provision of SRH information and counselling for adolescents.Citation38,Citation62
Two of the 15 studies reported steps taken in humanitarian settings to mitigate COVID-19’s impact on service provision.Citation33,Citation36,Citation37 Key informants reported steps like preparedness planning, coordination, and prioritisation of SRH services including contraception.Citation36 Another study (which included participants from refugee camps) highlighted the continuation of telehealth services and providing three-month supplies of medication to cover patients during lockdown.Citation33
Access to SRH services
Thirteen studies reported on the impact of the pandemic on accessing SRH services in general.Citation5,Citation37,Citation39,Citation40,Citation44,Citation56,Citation66,Citation70,Citation81,Citation82,Citation86,Citation91,Citation92 The most frequent barriers to obtaining medical care from facilities in an online survey of young people in Uganda were lack of transportation (43%), distance from home (35%), cost (26%), and curfew (24%).Citation66 High proportions of MOH key informants in a multi-country study also identified these as key barriers to accessing facilities – 48% reported the lack of public transportation under lockdown and 33% reported financial constraints.Citation5 In Colombia, the proportion in a population-based survey reporting cost as a barrier increased from 3% in April 2020 to 26% in September 2020.Citation56 A qualitative study of sex workers in Nairobi also reported restrictions on movement as a key barrier to accessing any health services, including SRH.Citation40 A nationally representative study in Uganda fielded in September–October 2020 found that 23% of women aged 15–49 were unable to access health services (including family planning); lack of transportation was mentioned by 40% and government restrictions by 19%.Citation44
Longitudinal surveys in five slum settlements in Nairobi found that between May and June 2020, the proportion saying they were not accessing medical care increased from 9% to 12%; the main reason (47%) for not getting healthcare services is unaffordability.Citation70 The second round of this survey fielded in April found that a higher proportion of women than men (11% versus 5%) reported forgoing essential healthcare services, including family planning.Citation91
Three representative studies in Lagos State, Nigeria; Kano State, Nigeria; and Burkina Faso (national) found that substantial proportions of women aged 15–49 needed to make medical visits (20%, 33%, and 43%, respectively); and of these women, a large proportion reported experiencing some difficulties or barriers (45%, 42%, and 57%, respectively).Citation81,Citation82,Citation86 However, 88–90% in all three studies were able to access services at a facility.
Two studies reported findings based on administrative data about the impact of the pandemic on numbers served. A study on MSI Reproductive Choice’s programmes found 1.9 million fewer women served globally (versus original forecasts) due to COVID-19-related disruptions.Citation39 A study in Kwa-Zulu Natal, South Africa analysed routine health systems data on service usage and found that the average number of visits (family planning and prenatal visits combined) per clinic per day increased significantly from 7.3 pre-lockdown to 11.0 by June 2020, a change that correlates with reductions in movement restrictions and improvements in transportation that came into effect by June.Citation92 One study reported that a hotline service started during COVID-19 in a fragile context, Sudan, handled 3000 clients in its first month, providing information on a range of SRH services including contraception and abortion-related questions.Citation37
Discussion
Of 71 studies included in this scoping review, the majority (61%) were not peer-reviewed, indicating the predominant role of grey literature and pre-prints as a source for early empirical data on COVID-19 impacts on SRH services. Study evidence was primarily situated in Africa (30 studies), particularly Eastern Africa, and Asia (25 studies), particularly Southern Asia. Most studies included data from no later than June 2020.
Regarding contraceptive services, most studies (38 of 55) involved cross-sectional or longitudinal surveys and many were conducted online or by phone due to pandemic conditions. Nineteen studies used administrative data. The magnitude of the need for and access to contraceptive services varied widely by study setting and population represented. Nearly all of the ten studies on changes over time in contraceptive service provision noted declines of varying magnitude, but severe disruptions were relatively uncommon or of limited duration. Most relevant studies found declines in at least some indicators of access to contraceptive services during COVID-19. Among 17 studies with population-based data on contraceptive use and change (method starting, stopping, and switching) over time during COVID-19, results were mixed by setting.
Twenty-six studies included empirical data on abortion and PAC services, with the majority using administrative data (54%) and smaller proportions using online surveys of key informants (19%) or individuals (15%). Only six studies addressed the demand for abortion or PAC services, including major barriers to seeking abortion. Eleven studies showed evidence of the impact of the COVID-19 pandemic on the provision of abortion-related services (ten on abortion and two on PAC), including the level of and disruptions in service provision, the degree to which programmes adapted provision to facilitate client access, and the level of shortages in safe abortion supplies. Among the eight studies with data on access to abortion services (including one that also had data on PAC), two had evidence on perceived declines in access to surgical and medication abortion compared to pre-COVID-19 levels, three were about the potential or actual impact on abortion safety, and six studies addressed barriers in accessing abortion or PAC. There was more empirical evidence on the use of abortion services (16 studies, seven of which covered PAC), and most studies showed declines in abortions during the COVID-19 pandemic, with variations by geography, source of data, gestational age, and type of abortion (e.g. medication abortion). There was no systematic pattern in the direction of impact on postabortion outcomes among the seven relevant studies, possibly due to two opposing factors at play – an increase in barriers to accessing PAC and an increase in numbers of people seeking PAC because of an increase in unsafe abortion.
It is important to bear in mind that large gaps existed in meeting SRH service needs prior to the pandemic. In 2019, before the COVID-19 pandemic, approximately 218 million women of reproductive age in LMICs wanted to avoid a pregnancy but were not using a modern contraceptive method.Citation93 Unintended pregnancy rates were higher in low- and middle-income countries (respectively, 93 and 66 unintended pregnancies per 1000 reproductive-aged women per year) compared with high-income countries (34 per 1000).Citation94 Women in poorer countries were also less likely to have a safe and legal abortion or to receive high-quality postabortion care (PAC) when needed.Citation95 COVID-19-related disruptions in access to and/or use of reproductive health services increased the overall magnitude of pre-existing gaps in LMICs at least in the short term, and may have exacerbated existing inequalities (including gender inequalities) given what we know from past pandemics.Citation9,Citation10
Evidence gaps
A key gap in the existing evidence base is the dearth of data on the pandemic’s impact on the full range of sources for contraceptive, abortion, and PAC services over time, including public and private sectors. Study data tend to represent part of, not the complete picture of a country, such as data from a single health facility, from the public sector only or focused on a particular programme provider, or data at one point in time. Consequently, it is difficult to interpret reported changes during the COVID-19 pandemic as information is missing on the degree to which people may be obtaining services from other sources (e.g. pharmacies), including new or adapted sources to improve access during the pandemic (e.g. telehealth, self-care). For example, despite misoprostol and medication abortion being included in the search terms, we found no evidence regarding impacts of the pandemic on access to these effective medications from other sources such as pharmacies or informal drug sellers. With data mainly from health facilities (rather than population-based data) or from part of the health system, we have a limited understanding of what role pharmacies or self-managed abortion using misoprostol (or combined medication abortion) obtained from informal sources might have had in substituting for surgical procedures provided in clinics by medical personnel.
Similarly, another gap is nationally-representative, population-based data, and of sufficient sample size to speak to the situation of particularly vulnerable groups of people (e.g. adolescents, people living in poverty, or people with disabilities) as well as data that speak to the situation of people living in humanitarian crisis settings. While the impetus to collect data quickly and in the context of a pandemic likely led to the preponderance of studies based on convenience samples, online or mobile phone surveys, or interviews with key informants, these approaches can result in relatively selective representations of the impact of the COVID-19 pandemic.
Implications for improved data collection during a pandemic
Studies that collect data from multiple sources (for example, health administration systems, private and public sector service providers, and population-based surveys) are needed to be able to comprehensively assess the direction and magnitude of the impact of a pandemic or other major systemic shock on the provision of, demand for, and access to essential SRH services. Health systems data are likely to be continuously collected and will therefore enable the measurement of change during a pandemic; other data collection approaches such as surveys of providers or the general population would need to be repeated periodically to measure change over time. Data from multiple sources would also provide the basis for concluding if impacts on SRH need, access, use, and outcomes are in a uniform direction across sectors and whether these impacts are cumulative, or whether declines in one sector are compensated for by substitutions in another sector. Studies that are representative of the cross-section of a population, and thus generalisable, are critical. In the context of a pandemic or other major systemic shock, speed and cost are also essential elements in designing studies: for example, mobile phone surveys may satisfy these criteria in some contexts with careful attention to building in mechanisms to allow adjustment for selection bias in study samples.
Strengths and limitations
The main strength of this scoping review is that we applied guidelines for best practices in conducting scoping reviews, including working with public health informationists to develop a peer-reviewed search strategy for electronic bibliographic databases and employing a comprehensive search strategy that included multiple (four) languages and an intensive grey literature search. While we included pre-prints and other grey literature to be able to identify and potentially include more recent data in the scoping review, this also raised some limitations (described below). Other strengths of this review include the pre-registration of our study protocol, dyadic screening and extraction procedures, and feedback at critical stages of the review from an expert advisory group.
Our review has several important limitations. First, the timelines of the first COVID-19 case in a country and government responses vary by country, as does the timing of data collection across studies in this review. As a result, such variations in timelines across study contexts may have impacted the existence or magnitude of findings. Second, our search strategy necessarily ended by a certain cut-off date, so we were unable to include some relevant studies not yet released by that time.Citation6,Citation96 Findings from pre-prints and grey literature (43 of the 71 included studies) should be interpreted cautiously as they are not (or not yet) peer-reviewed. Furthermore, as is standard for scoping reviews, we did not conduct formal critical appraisals or risk of bias in included studies. Finally, we identified few studies in Latin America and the Caribbean compared with studies from Africa and Asia, leading to geographical imbalances in the current body of evidence.
We also imposed several limitations on the scope of our review. We determined that it was out of scope for us to be able to include information on modifications to contraceptive, abortion, or PAC service delivery in response to the COVID-19 pandemic (supplementary material B). Thus, we do not capture the many innovations and adaptations that facilitated the provision of and access to these essential services, such as telehealth options, self-managed abortion, or advance provision of certain contraceptive methods. In addition, we were not able to address the rights-based dimensions of COVID-19’s impact on access to these critical SRH services, and this is another limitation of the review. Examples of such dimensions include government accountability for ensuring access to care (e.g. whether abortion care is determined to be an essential service), equitable access to care (e.g. whether outreach programmes to meet the needs of marginalised communities are part of pandemic responses), and health care that respects individual autonomy (e.g. the degree to which care approaches support self-managed abortion).Citation97,Citation98 We also did not include terms related to “miscarriage” in our search strategy as it was neither feasible nor within the scope to distinguish which abortions were spontaneous versus induced. Finally, our review focuses specifically on contraceptive, abortion, and PAC services, important components of the essential package of SRH services, but which do not cover other equally important components such as services for infertility or sexually transmitted infections. However, reviews of a few other components of SRH services are available (supplementary material A).
Conclusion
Findings indicate that in the short term, the COVID-19 pandemic has had some impact on demand for, provision of, and access to contraceptive, abortion, and postabortion services in LMICs, and on related reproductive outcomes. The impact varied substantially depending on several factors, including the context of the pandemic in the study countries, the specific service, and the type of population studied. The fact that many studies had to rely on convenience samples and online data collection, given the constraints that pandemic conditions placed on the implementation of fieldwork, is an important limitation of the existing body of data; however, many studies used representative data from health or other data systems, some surveyed representative samples and several were able to compare pre- and post-pandemic conditions.
Future studies are needed to monitor demand, provision, and access to these key SRH services, as the impact of the pandemic will likely evolve in LMICs and have different and possibly greater impacts over the longer term. Empirical studies on the pandemic’s longer-term impact on access to these SRH services that are representative of the populations being studied, and that assess trends in provision, access, or outcomes related to these services are greatly needed. Such studies would measure and draw attention to existing and possibly widening gaps (whether for entire populations or for particularly vulnerable groups) and can help to inform policies and programmes to address gaps in these essential services.
Supplemental Material A-H
Download PDF (1.1 MB)Acknowledgements
We are grateful to the members of our expert advisory group, who generously donated their time, expertise, and advice to help us improve this review. They include Moazzam Ali (Epidemiologist, World Health Organization), Roopan Gill (Women’s Health Advisor, Obstetrics and Gynecology, Médecins Sans Frontieres, Sydney Medical Unit – Operational Centre Paris (OCP)), Gillian McKay (Global Health Researcher, London School of Hygiene and Tropical Medicine), and Rodolfo Gomez Ponce de Leon (Reproductive Health Regional Advisor, Pan American Health Organization).
We are also grateful to Sarah Keogh for insightful inputs on available evidence sources and on an early draft of the manuscript, Claire Twose for expert review of the electronic bibliographic search strategy, and the comments of two anonymous reviewers.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplemental data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/26410397.2022.2098557.
Additional information
Funding
References
- Okereke M, Ukor NA, Adebisi YA, et al. Impact of COVID-19 on access to healthcare in low- and middle-income countries: current evidence and future recommendations. Int J Health Plann Manage. 2020;36 (1):13–17. doi:10.1002/hpm.3067
- Bong C-L, Brasher C, Chikumba E, et al. The COVID-19 pandemic: effects on low- and middle-income countries. Anesth Analg. 2020;131 (1):86–92. doi:10.1213/ANE.0000000000004846
- Oyadiran OT, Agaga LA, Adebayo Adebisi Y, et al. Nigeria, COVID-19 and the dearth of health workers. J Glob Health. 2020;10 (2):020379. doi:10.7189/jogh.10.020379
- Purdy C. Opinion: How will COVID-19 affect global access to contraceptives – and what can we do about it? Devex. 2020. [cited 21 Apr 2020]. Available from: https://www.devex.com/news/sponsored/opinion-how-will-covid-19-affect-global-access-to-contraceptives-and-what-can-we-do-about-it-96745
- World Health Organization. Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report. Geneva: World Health Organization; 2020. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1
- World Health Organization. Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic: January-March 2021. Geneva: World Health Organization; 2021; Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS-continuity-survey-2021.1
- Doraiswamy S, Abraham A, Mamtani R, et al. Use of telehealth during the COVID-19 pandemic: scoping review. J Med Internet Res. 2020;22 (12):e24087. doi:10.2196/24087
- Bhaskar S, Bradley S, Chattu VK, et al. Telemedicine across the globe- position paper from the COVID-19 pandemic health system resilience program (REPROGRAM) international consortium (Part 1). Front Public Health. 2020;8:556720. doi:10.3389/fpubh.2020.556720
- Chattu VK, Yaya S. Emerging infectious diseases and outbreaks: implications for women’s reproductive health and rights in resource-poor settings. Reprod Health. 2020;17 (1); doi:10.1186/s12978-020-0899-y
- Wenham C, Smith J, Davies SE, et al. Women are most affected by pandemics- lessons from past outbreaks. Nature. 2020;583 (7815):194–198. doi:10.1038/d41586-020-02006-z
- Azmat SK, Ali M, Siddiqui FJ, et al. Scoping review on the impact of outbreaks on sexual and reproductive health services: proposed frameworks for pre-, intra-, and postoutbreak situations. BioMed Res Int 2021. 2021; 1–21. doi:10.1155/2021/9989478
- Roesch E, Amin A, Gupta J, et al. Violence against women during covid-19 pandemic restrictions. Br Med J. 2020;369:m1712. doi:10.1136/bmj.m1712
- Black B, McKay G. Covid-19 and reproductive health: what can we learn from previous epidemics? BMJ Opin. 2020. [accessed 22 Dec 2020]. Available from: https://blogs.bmj.com/bmj/2020/03/19/covid-19-and-reproductive-health-what-can-we-learn-from-previous-epidemics/
- Aassve A, Cavalli N, Mencarini L, et al. The COVID-19 pandemic and human fertility. Science. 2020;369 (6502):370–371. doi:10.1126/science.abc9520
- Sochas L, Channon AA, Nam S. Counting indirect crisis-related deaths in the context of a low-resilience health system: the case of maternal and neonatal health during the Ebola epidemic in Sierra Leone. Health Policy Plan. 2017;32 (suppl_3):iii32–iii39. doi:10.1093/heapol/czx108
- Bietsch K, Williamson J, Reeves M. Family planning during and after the west African Ebola crisis. Stud Fam Plann. 2020;51 (1):71–86. doi:10.1111/sifp.12110
- Camara BS, Delamou A, Diro E, et al. Effect of the 2014/2015 Ebola outbreak on reproductive health services in a rural district of Guinea: an ecological study. Trans R Soc Trop Med Hyg. 2017;111 (1):22–29. doi:10.1093/trstmh/trx009
- McKay G, Black B, Mbabmu Kahamba S, et al. Not all that bleeds is Ebola: how has the DRC Ebola outbreak impacted sexual and reproductive health in North-Kivu? New York: The International Rescue Committee; 2019. Available from: https://www.rescue.org/report/not-all-bleeds-ebola-how-drc-outbreak-impacts-reproductive-health
- Belizan M, Maradiaga E, Roberti J, et al. Contraception and post abortion services: qualitative analysis of users’ perspectives and experiences following Zika epidemic in Honduras. BMC Womens Health. 2020;20 (1):199. doi:10.1186/s12905-020-01066-7
- Lathrop E, Hurst S, Mendoza Z, et al. Final program data and factors associated with long-acting reversible contraception removal: the Zika contraception access network. Obstet Gynecol. 2020;135 (5):1095–1103. doi:10.1097/AOG.0000000000003835
- Ali M, Miller K, Gómez Ponce de Leon RF. Family planning and Zika virus: need for renewed and cohesive efforts to ensure availability of intrauterine contraception in Latin America and the Caribbean. Eur J Contracept Reprod Health Care. 2017;22 (2):102–106. doi:10.1080/13625187.2017.1288902
- Janvrin A, McKay G. Maternal, newborn, and reproductive health and COVID-19: adaptations, successes, challenges, and next steps: an expert consultation. Washington, DC: READY Initiative, Save the Children 2020. Available from: https://www.ready-initiative.org/wp-content/uploads/2020/12/MNRH-and-COVID-19-Consultation-Report-2020.pdf
- Pfitzer A, Lathrop E, Bodenheimer A, et al. Opportunities and challenges of delivering postabortion care and postpartum family planning during the COVID-19 pandemic. Glob Health Sci Pract. 2020;8 (3):335–343. doi:10.9745/GHSP-D-20-00263
- Aromataris E, Munn Z. JBI manual for evidence synthesis. JBI 2020. Available from: https://synthesismanual.jbi.global
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8 (1):19–32. doi:10.1080/1364557032000119616
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5 (1):69, doi:10.1186/1748-5908-5-69
- Peters MDJ, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13 (3):141–146. doi:10.1097/XEB.0000000000000050
- Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18 (10):2119–2126. doi:10.11124/JBIES-20-00167
- Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169 (7):467–473. doi:10.7326/M18-0850
- Polis CB, Biddlecom A, Singh S, et al. 2021. Impacts of COVID-19 on contraceptive and abortion services in low- and middle-income countries: protocol for a scoping review. 2021. osf.io/jqhec
- World Bank country and lending groups. 2020. World Bank Data Help Desk. [cited 23 Dec 2020]. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
- Covidence Systematic Review Software. 2021. Melbourne, Australia: Veritas Health Innovation 2021. Available from: www.covidence.org
- Anderson K. Plan International. Daring to ask, listen, and act: a snapshot of the impacts of COVID-19 on women and girls’ rights and sexual and reproductive health. UNFPA Jordan and Plan International; 2020. Available from: https://data2.unhcr.org/en/documents/details/77499
- Social Sciences Analytics Cell (CASS). The impacts of the COVID-19 outbreak response on women and girls in the Democratic Republic of the Congo. Kinshasa, DRC: UNICEF; 2020; Available from: https://www.unicef.org/drcongo/media/5416/file/COD-CASS-impacts-COVID-response-women-girls.pdf
- IPPF. COVID-19: SPRINT response. IPPF. 2020. Available from: https://www.ippf.org/sites/default/files/COVID19%20SPRINT%20Response%20Summary%202020%20V9.pdf
- Jacobi L. Disruptions and adaptations: the effects of COVID-19 on contraceptive services across the humanitarian-development nexus. Women’s Refugee Commission; 2020. Available from: http://www.womensrefugeecommission.org/research-resources/disruptions-adaptations-effects-covid-19-contraceptive-services-across-humanitarian-development-nexus/
- IPPF. Delivering humanitarian action during COVID-19. IPPF. 2020. Available from: https://www.ippf.org/sites/default/files/2020%20%20Global%20Covid19%20and%20Humanitarian%20two%20pager%20final%20%282%29.pdf
- Both R, Castle S, Hensen B. I feel that things are out of my hands: how COVID-19 prevention measures have affected young people’s sexual and reproductive health in Ghana, Indonesia, Kenya, Nepal, Uganda and Zimbabwe. Utrecht: Rutgers; 2021. Available from: https://www.rutgers.nl/sites/rutgersnl/files/PDF-Onderzoek/Rutgers%20SRHR%20%26%20COVID%2019%20Report_International%20Study.pdf
- MSI Reproductive Choices. Resilience, adaptation and action: MSI’s response to COVID-19. London: MSI Reproductive Choices; 2020. Available from: https://www.msichoices.org/media/3849/resilience-adaptation-and-action.pdf
- Gichuna S, Hassan R, Sanders T, et al. Access to healthcare in a time of COVID-19: sex workers in crisis in Nairobi, Kenya. Glob Public Health. 2020;15 (10):1430–1442. doi:10.1080/17441692.2020.1810298
- World Health Organization. Impact of COVID-19 on SRMNCAH services, regional strategies, solutions and innovations: a comprehensive report. New Dehli: WHO, UNFPA, UNICEF; 2021; Available from: https://apps.who.int/iris/bitstream/handle/10665/338482/rapid-assessment-mar-apr-2020-eng.pdf?sequence = 1&isAllowed = y
- Kamran I, Parveen T, Niazi R, et al. Reproductive health care in the time of COVID-19: perspectives of poor women and service providers from Rahim Yar Khan, Punjab. Islamabad: Population Council; 2020. doi:10.31899/rh14.1051
- Leight J, Hensly C, Chissano M, et al. Short-term effects of the COVID-19 state of emergency on contraceptive access and utilization in Mozambique. PLoS ONE. 2021;16 (3):e0249195. doi:10.1371/journal.pone.0249195
- Makerere University, School of Public Health at the College of Health Sciences, The Bill & Melinda Gates Institute for Population and Reproductive Health at The Johns Hopkins Bloomberg School of Public Health, Jhpiego. Performance monitoring for action (PMA) Uganda: results from phase 1 survey. Uganda and Baltimore, Maryland: 2020. Available from: https://www.pmadata.org/sites/default/files/data_product_results/Uganda%20Phase%201-COVID_Results%20Brief_Final_for%20review.pdf
- IPPF. COVID-19 global impact assessment of IPPF member associations 3rd survey results & analysis. IPPF. 2020. Available from: https://ippf-covid19.org/wp-content/uploads/2021/01/Covid19-Survey_Round-3-note_26TH-NOV-2020.pdf
- Abdela SG, Berhanu AB, Ferede LM, et al. Essential healthcare services in the face of COVID-19 prevention: experiences from a referral hospital in Ethiopia. Am J Trop Med Hyg. 2020;103 (3):1198–1200. doi:10.4269/ajtmh.20-0464
- Mureed S. Web-based poll survey to assess impact of COVID-19 on RMNCAH&N servies: perceptions of key informations. Islamabad: Health Services Academy; 2020. Available from: https://www.unicef.org/pakistan/media/3186/file/Assessing%20Impact%20of%20COVID-19%20on%20RMNCAH&N%20Services.pdf
- PMA Agile/Gender & International Centre for Reproductive Health-Kenya (ICRHK). Gender & COVID-19: access to health and contraception: access to health and contraceptive services among adolescents and young adults in Nairobi during the COVID-19 pandemic. Baltimore, Maryland:: Bill & Melinda Gates Institute for Population and Reproductive Health, Johns Hopkins University Bloomberg School of Public Health 2020. Available from: https://www.pmadata.org/sites/default/files/data_product_results/PMA%20Gender%20COVID%20Access%20Health%20Contraception%202020_0.pdf
- UNFPA. Impact of COVID-19 on family planning: what we know one year into the pandemic. UNFPA. 2021. Available from: https://www.unfpa.org/sites/default/files/resource-pdf/COVID_Impact_FP_V5.pdf
- IPPF. COVID-19 global impact assessment of IPPF member associations 2nd survey results & analysis. IPPF. 2020. Available from: https://ippf-covid19.org/wp-content/uploads/2020/10/IPPFs-2nd-COVID-19-Global-Impact-Assessment.pdf
- IPPF. COVID-19 global impact assessment of IPPF member associations - preliminary analysis and results. IPPF. 2020. Available from: https://ippf-covid19.org/wp-content/uploads/2020/04/Preliminary-results-C-19-MA-Impact-survey-April-52.pdf
- Li G, Tang D, Song B, et al. Impact of the COVID-19 pandemic on partner relationships and sexual and reproductive health: cross-sectional, online survey study. J Med Internet Res. 2020;22 (8):e20961. doi:10.2196/20961
- Population Council. Kenya: gender effects of COVID-19: responses from fourth round of data collection in five Nairobi informal settlements (Kibera, Huruma, Kariobangi, Dandora, and Mathare). Nairobi: Population Council; 2020. Available from: https://www.popcouncil.org/uploads/pdfs/2020PGY_Covid_KenyaKAPSurvey_Round4-Gender.pdf
- Chandrasekaran S, Diamond-Smith N, Srinivasan K, et al. Preparing for an increased need for abortion access in India during and after COVID-19: challenges and strategies. Stud Fam Plann. 2020;51 (4):377–383. doi:10.1111/sifp.12139
- Temesgen K, Workie A, Dilnessa T. The impact of COVID-19 infection on maternal and reproductive health care services in governmental health institutions of Dessie town, North-East Ethiopia, 2020 G.C. medRxiv 2020.09.20.20198259 [Preprint]. 2020. [accessed 10 Mar 2021]. doi:10.1101/2020.09.20.20198259
- Sánchez SM, Rivera-Montero D, Murad-Rivera R, et al. Changes COVID-19 post-quarantine behaviors, hygiene and expectations in Colombia: population survey from 1st to 13th September, 2020. medRxiv 2020.11.26.20239442. 2020. [accessed 10 Mar 2021]. doi:10.1101/2020.11.26.20239442
- International Centre for Reproductive Health Kenya (ICRHK), The Bill & Melinda Gates Institute for Population and Reproductive Health at The Johns Hopkins Bloomberg School of Public Health, Jhpiego. Performance monitoring for action (PMA) Kenya: results from COVID-19 phone survey. Kenya and Baltimore, Maryland, USA: 2020. Available from: https://www.pmadata.org/sites/default/files/data_product_results/Kenya%20Phase%201-FU_Results%20Brief_draft%204_0.pdf
- Pinchoff J, Santhya K, White C, et al. Gender specific differences in COVID-19 knowledge, behavior and health effects among adolescents and young adults in Uttar Pradesh and Bihar, India. PLoS ONE. 2020;15 (12):e0244053. doi:10.1371/journal.pone.0244053
- Population Foundation of India. Impact of COVID-19 on young people: rapid assessment in three states, May 2020. New Delhi, India: Population Foundation of India 2020. Available from: https://populationfoundation.in/wp-content/uploads/2020/08/Rapid-Assessment_Report_Youth_Survey_Covid.pdf
- Karagöz MA, Gül A, Borg C, et al. Influence of COVID-19 pandemic on sexuality: a cross-sectional study among couples in Turkey. Int J Impot Res. Published Online First. 16 December 2020. doi:10.1038/s41443-020-00378-4
- Aolymat I. A cross-sectional study of the impact of COVID-19 on domestic violence, menstruation, genital tract health, and contraception use among women in Jordan. Am J Trop Med Hyg. 2021;104 (2):519–525. doi:10.4269/ajtmh.20-1269
- Dhimal M, Subedi R, Acharya A, et al. Effect of COVID-19 pandemic and lockdown on provision and utilization of Essential Sexual Reproductive Maternal Neonatal Child and Adolescent Health and Nutrition Services in Nepal. Kathmandu: Nepal Health Research Council; 2020.
- Endler M, Al-Haidari T, Benedetto C, et al. How the coronavirus disease 2019 pandemic is impacting sexual and reproductive health and rights and response: results from a global survey of providers, researchers, and policy-makers. Acta Obstet Gynecol Scand. 2021;100 (4):571–578. doi:10.1111/aogs.14043
- Karijo E, Wamugi S, Lemanyishoe S, et al. Knowledge, attitudes, practices, and the effects of COVID-19 on health seeking behaviors and social-economic status among young people in Kenya. Research Square rs-34861 (Version 2) [Preprint]. 2020. doi:10.21203/rs.3.rs-34861/v2
- Karp C, Wood SN, Guiella G, et al. Contraceptive dynamics during COVID-19 in sub-Saharan Africa: longitudinal evidence from Burkina Faso and Kenya. BMJ Sex Reprod Health. 2021;47 (4):252–260. doi:10.1136/bmjsrh-2020-200944
- Mambo SB, Sikakulya FK, Ssebuufu R, et al. Factors that influenced access and utilisation of sexual and reproductive health services among Ugandan youths during the COVID-19 pandemic lockdown: an online cross-sectional survey. Research Square rs-48529 (Version 3) [Preprint]. 2021. doi:10.21203/rs.3.rs-48529/v3
- Population Council. Kilifi, Kenya: adult COVID-19 perceptions, prevention practices and impact: responses from the first round of adult data collection in Kilifi, Kenya. Population Council; 2020. Available from: https://www.popcouncil.org/uploads/pdfs/2020PGY_Covid_KenyaAdult_Kilifi.pdf
- Bolarinwa OA. Ignoring the elephant in the room: factors contributing to inadequate access to condoms and sources of condoms during novel coronavirus diseases 2019 in South Africa. medRxiv 2020.09.11.20192849 [Preprint]. 2020. doi:10.1101/2020.09.11.20192849
- Vora KS, Saiyed S, Natesan S. Impact of COVID-19 on family planning services in India. Sex Reprod Health Matters. 2020;28 (1):57–59. doi:10.1080/26410397.2020.1785378
- Population Council. 2020. Kenya: COVID-19 perceptions, stigma and impact: responses from fourth round of data collection in five Nairobi informal settlements (Kibera, Huruma, Kariobangi, Dandora, and Mathare). Nairobi, Kenya: Population Council 2020. Available from: https://www.popcouncil.org/uploads/pdfs/2020PGY_Covid_KenyaKAPSurvey_Round4-Stigma.pdf
- Adelekan T, Mihretu B, Mapanga W, et al. Early effects of the COVID-19 pandemic on family planning utilisation and termination of pregnancy services in Gauteng, South Africa: March–April 2020. Wits J Clin Med. 2020;2 (2):91. doi:10.18772/26180197.2020.v2n2a7
- Belay L, Hurisa T, Abbas F, et al. Effect of COVID-19 pandemic on safe abortion and contraceptive services and mitigation measures: a case study from a tertiary facility in Ethiopia. Ethiop J Reprod Health. 2020;12:51–57.
- Pattinson R, Fawcus S, Gebhardt S, et al. The effect of the first wave of Covid-19 on use of maternal and reproductive health services and maternal deaths in South Africa. Obstet Gynaecol Forum. 2020;30:10. doi:10.10520/ejc-medog-v30-n4-a10
- PSI. PSI performance report- June 2020. PSI 2020. Available from: https://www.psi.org/wp-content/uploads/2020/07/Performance-Report_0620.pdf
- Shapira G, Ahmed T, Drouard SHP, et al. Disruptions in essential health services during the first five months of COVID-19: analysis of facility-reported service volumes in eight Sub-Saharan African countries. SSRN 3757414 [Preprint]. 2020. [accessed 11 Jun 2021]. doi:10.2139/ssrn.3757414
- Shikuku D, Nyaoke I, Gichuru S, et al. Early indirect impact of COVID-19 pandemic on utilization and outcomes of reproductive, maternal, newborn, child and adolescent health services in Kenya. medRxiv 2020.09.09.20191247 [Preprint]. 2020. doi:10.1101/2020.09.09.20191247
- UNICEF. 2021. Direct and indirect effects of the COVID-19 pandemic and response in South Asia. Kathmandu, Nepal: UNICEF 2021. Available from: https://www.unicef.org/rosa/media/13066/file/Main%20Report.pdf
- Ghimire R, Adhikari S. Effects of COVID-19 on non-communicable diseases and reproductive health services in a district hospital of Nepal. Arch Pulmonol Respir Care. 2020;6:065–067. doi:10.17352/aprc.000058
- Hossain M, Hossain M, Ainul S, et al. Trends in family planning services in Bangladesh before, during and after COVID-19 lockdowns: evidence from national routine service data. Dhaka: Population Council. 2020. doi:10.31899/rh14.1038
- Pires P das N, Macaringue C, Abdirazak A, et al. Covid-19 pandemic impact on maternal and child health services access in Nampula. Mozambique: a mixed methods research. Research Square rs-104405 [Preprint]. 2020. doi:10.21203/rs.3.rs-104405/v1
- Institut Supérieur des Sciences de la Population, Université Joseph Ki-Zerbo, The Bill & Melinda Gates Institute for Population and Reproductive Health at The Johns Hopkins Bloomberg School of Public Health, Jhpiego. 2020. Performance monitoring for action (PMA) Burkina Faso: results from COVID-19 phone survey. Ouagadougou, Burkina Faso and Baltimore, Maryland, USA: 2020. Available from: https://www.pmadata.org/sites/default/files/data_product_results/BF%20Phase%201-FU_Results%20Brief_English_final.pdf
- Centre for Research, Evaluation Resources and Development (CRERD), The Bill & Melinda Gates Institute for Population and Reproductive Health at The Johns Hopkins Bloomberg School of Public Health, Jhpiego. 2020. Performance monitoring for action (PMA) Nigeria (Kano): results from COVID-19 phone survey. Nigeria and Baltimore, Maryland, USA: 2020. Available from: https://www.pmadata.org/sites/default/files/data_product_results/Nigeria%20Kano%20Phase%201-FU_Results%20Brief_Final.pdf
- University of Kinshasa School of Public Health, The Bill & Melinda Gates Institute for Population and Reproductive Health at The Johns Hopkins Bloomberg School of Public Health, Jhpiego. 2020. Performance monitoring for action (PMA) République Démocratique du Congo (Kinshasa): results from the COVID-19 phone survey. Kinshasa, DRC and Baltimore, Maryland, USA: 2020. Available from: https://www.pmadata.org/sites/default/files/data_product_results/DRC%20Kinshasa%20Phase%201-FU_Results%20Brief_English_final_0.pdf
- Culha MG, Demir O, Sahin O, et al. Sexual attitudes of healthcare professionals during the COVID-19 outbreak. Int J Impot Res. 2021;33 (1):102–109. doi:10.1038/s41443-020-00381-9.
- Yuksel B, Ozgor F. Effect of the COVID-19 pandemic on female sexual behavior. Int J Gynecol Obstet. 2020;150 (1):98–102. doi:10.1002/ijgo.13193.
- Centre for Research, Evaluation Resources and Development (CRERD), The Bill & Melinda Gates Institute for Population and Reproductive Health at The Johns Hopkins Bloomberg School of Public Health, Jhpiego. 2020. Performance monitoring for action (PMA) Nigeria (Lagos): Results from COVID-19 phone survey. Nigeria and Baltimore, Maryland, USA: 2020. Available from: https://www.pmadata.org/sites/default/files/data_product_results/Nigeria%20Lagos%20Phase%201-FU_Results%20Brief_Final.pdf
- Silverio-Murillo A, Hoehn-Velasco L, Balmori de la Miyar JR, et al. COVID-19 and women’s health: examining changes in mental health and fertility. Econ Lett. 2021;199:109729. doi:10.1016/j.econlet.2021.109729
- Shah R, Basnyat S, Panta PP. Abortion services utilization at KAHS during COVID-19 lockdown. J Karnali Acad Health Sci. 2020;3:6.
- Marquez-Padilla F, Saavedra B. COVID-19 and (un)desired fertility: the effect of stay-at-home orders on abortions in Mexico City. SSRN Published Online First. 20 October 2020. doi:10.2139/ssrn.3703581
- Dey A, Dehingia N, Raj A. Using Google trends data to assess reproductive health needs in Nigeria during COVID-19. San Diego: Center on Gender Equity and Health, University of California San Diego; 2021. Available from: https://data2x.org/wp-content/uploads/2021/02/UCSD-Brief-2_ReproductiveHealthNeedsinNigeria.pdf
- Population Council. Kenya: COVID-19 knowledge, attitudes and practices: responses from second round of data collection in five Nairobi informal settlements (Kibera, Huruma, Kariobangi, Dandora, Mathare). Nairobi: Population Council; 2020. Available from: https://www.popcouncil.org/uploads/pdfs/2020PGY_CovidKenyaKAPStudyResultsBriefRound2.pdf
- Siedner MJ, Kraemer JD, Meyer MJ, et al. Access to primary healthcare during lockdown measures for COVID-19 in rural South Africa: an interrupted time series analysis. BMJ Open. 2020;10 (10):e043763. doi:10.1136/bmjopen-2020-043763
- Sully E, Biddlecom A, Darroch JE, et al. Adding it up: investing in sexual and reproductive health 2019. New York: Guttmacher Institute; 2020. Available from: https://www.guttmacher.org/report/adding-it-upinvesting-in-sexual-reproductive-health-2019
- Bearak J, Popinchalk A, Ganatra B, et al. Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990–2019. Lancet Glob Health. 2020;8 (9):e1152–e1161. doi:10.1016/S2214-109X(20)30315-6
- Remez L, Mayall K, Singh S. Global developments in laws on induced abortion: 2008–2019. Int Perspect Sex Reprod Health. 2020;46 (Supplement 1):53–65. doi:10.1363/46e0920
- Wood SN, Karp C, OlaOlorun F, et al. Need for and use of contraception by women before and during COVID-19 in four sub-Saharan African geographies: results from population-based national or regional cohort surveys. Lancet Glob Health. 2021;9 (6):e793–e801. doi:10.1016/S2214-109X(21)00105-4
- Dasgupta J, Schaaf M, Contractor SQ, et al. Axes of alienation: applying an intersectional lens on the social contract during the pandemic response to protect sexual and reproductive rights and health. Int J Equity Health. 2020;19 (1):130. doi:10.1186/s12939-020-01245-w.
- Assis MP, Larrea S. Why self-managed abortion is so much more than a provisional solution for times of pandemic. Sex Reprod Health Matters. 2020;28 (1):1779633. doi:10.1080/26410397.2020.1779633
- Toh WQ, Treibich C, Szawlowski S, et al. Impact of COVID-19 on female sex workers in Africa: evidence from a cohort study in Senegal. SSRN 3710613 [Preprint]. 2020. [accessed 25 Mar 2021]. doi:10.2139/ssrn.3710613
- Asiamah N, Opuni FF, Mends-Brew E, et al. Short-term changes in behaviors resulting from COVID-19-related social isolation and their influences on mental health in Ghana. Community Ment Health J. 2021;57 (1):79–92. doi:10.1007/s10597-020-00722-4
- Marteleto LJ, Dondero M. Navigating women’s reproductive health and childbearing during public health crises: Covid-19 and Zika in Brazil. World Dev. 2021;139:105305. doi:10.1016/j.worlddev.2020.105305
- Feng Y-J, Fan Y-J, Su Z-Z, et al. Correlation of sexual behavior change, family function, and male-female intimacy among adults aged 18-44 years during COVID-19 epidemic. Sex Med. 2021;9 (1):100301. doi:10.1016/j.esxm.2020.100301
- Li W, Li G, Xin C, et al. Challenges in the practice of sexual medicine in the time of COVID-19 in China. J Sex Med. 2020;17 (7):1225–1228. doi:10.1016/j.jsxm.2020.04.380
- Zhu C, Wu J, Liang Y, et al. Fertility intentions among couples in Shanghai under COVID-19: a cross-sectional study. Int J Gynecol Obstet. 2020;151 (3):399–406. doi:10.1002/ijgo.13366
- Fang D, Peng J, Liao S, et al. An online questionnaire survey on the sexual life and sexual function of Chinese adult men during the coronavirus disease 2019 epidemic. Sex Med. 2021;9 (1):100293. doi:10.1016/j.esxm.2020.100293
- Arafat SMY, Alradie-Mohamed A, Kar SK, et al. Does COVID-19 pandemic affect sexual behaviour? A cross-sectional, cross-national online survey. Psychiatry Res. 2020;289:113050. doi:10.1016/j.psychres.2020.113050
- Banaei M, Ghasemi V, Dordeh M, et al. The impact of coronavirus disease 2019 on sexual health. Galen Med J. 2020;9:e1928. doi:10.31661/gmj.v9i0.1928
- Baran O, Aykac A. The effect of fear of covid-19 transmission on male sexual behaviour: a cross-sectional survey study. Int J Clin Pract. 2021;75 (4):e13889. doi:10.1111/ijcp.13889
- World Health Organization. Pulse survey on continuity of essential health services during the COVID-19 pandemic. Interim report. Geneva: World Health Organization; 2020.
- Loewen S, Pinchoff J, Ngo T, et al. The impact of disasters on sexual and reproductive health service provision and outcomes in low- and middle-income countries: a systematic review of the literature (CRD42020189123). 2020. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID = CRD42020189123
- Sheng X, Zhou R, Tan Y. Sexual and reproductive health seeking behavior among women of reproductive age during major disease outbreaks: a systematic review. 2020. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID = CRD42020201046
- Sharma KA, Zangmo R, Kumari A, et al. Family planning and abortion services in COVID 19 pandemic. Taiwan J Obstet Gynecol. 2020;59 (6):808–811. doi:10.1016/j.tjog.2020.09.005
- Eghtessadi R, Mukandavire Z, Mutenherwa F, et al. Safeguarding gains in the sexual and reproductive health and AIDS response amidst COVID-19: The role of African civil society. Int J Infect Dis. 2020;100:286–291. doi:10.1016/j.ijid.2020.08.086
- Ferreira-Filho ES, de Melo NR, Sorpreso ICE, et al. Contraception and reproductive planning during the COVID-19 pandemic. Expert Rev Clin Pharmacol. 2020;13 (6):615–622. doi:10.1080/17512433.2020.1782738
- Batiha O, Al-Deeb T, Al-zoubi E, et al. Impact of COVID-19 and other viruses on reproductive health. Andrologia. 2020;52 (9):e13791. doi:10.1111/and.13791
- Kumar N, Janmohamed K, Nyhan K, et al. Sexual health and COVID-19: protocol for a living scoping review. Research Square rs-59514 (Version 1) [Preprint]. 2020. doi:10.21203/rs.3.rs-59514/v1
- Elshafeey F, Magdi R, Hindi N, et al. A systematic scoping review of COVID-19 during pregnancy and childbirth. Int J Gynecol Obstet. 2020;150 (1):47–52. doi:10.1002/ijgo.13182
- Ozgoli G. (2020). The impact of COVID-19 on sexual and reproductive health. Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID = CRD42020212621
- Alizadeh S, Ozgoli G. The impact of COVID-19 on sexual and reproductive health: a systematic review protocol. Research Square rs-93104 [Preprint]. 2020. doi:10.21203/rs.3.rs-93104/v1
- Tolu LB, Feyissa GT. Guidelines and best practice recommendations on contraception and safe abortion care service provision amid COVID-19 pandemic: scoping review. Research Square rs-25326 (Version 1) [Preprint]. 2020. doi:10.21203/rs.3.rs-25326/v1
- Baral S, Rao A, Twahirwa Rwema JO, et al. Competing health risks associated with the COVID-19 pandemic and response: a scoping review. medRxiv 2021.01.07.21249419 [Preprint]. 2021. doi:10.1101/2021.01.07.21249419
- Bolarinwa OA, Ahinkorah BO, Ameyaw EK, et al. Impact of coronavirus disease 2019 outbreak on sexual and reproductive health outcomes: scoping review protocol. OSF. 2020. Available from: https://osf.io/85fch