Abstract
Reducing the adolescent birth rate is paramount in achieving the health-related Sustainable Development Goals, given that pregnancy and childbirth are the leading cause of mortality among young women aged 15–19. This study aimed to explore predictors of adolescent pregnancy among girls aged 13–18 years in Maharashtra, India, during the COVID-19 pandemic. Using a mixed-methods approach, primary data were gathered from two regions in Maharashtra between February and April 2022. Quantitative data from face-to-face interviews with 3049 adolescent girls assessed various household, social, and behavioural factors, as well as the socioeconomic and health impacts of COVID-19. Qualitative data from seven in-depth interviews were analysed thematically. The findings reveal that girls from low socioeconomic backgrounds face a higher likelihood of adolescent pregnancy. Multivariable analysis identified several factors associated with increased risk, including older age, being married, having more sexual partners, and experiencing COVID-19-related economic vulnerability. On the other hand, rural residence, secondary and higher secondary education of the participants, and higher maternal education were associated with a decreased likelihood of adolescent pregnancy. In the sub-sample of 565 partnered girls, partner's emotional abuse also correlated with higher rates of adolescent pregnancy. Thematic analysis of qualitative data identified four potential pathways leading to adolescent pregnancy: economic hardships and early marriage; personal safety, social norms, and early marriage; social expectations; and lack of knowledge on contraceptives. The findings underscore the significance of social position and behavioural factors and the impact of external shocks like the COVID-19 pandemic in predicting adolescent pregnancy in Maharashtra, India.
Plain Language Summary: Adolescent pregnancy is an important health issue for young girls. In South Asia, one out of every five adolescent girls becomes a mother before turning 18, and in India, around 9% of girls aged 15–19 get pregnant yearly. This study focused on understanding the factors associated with adolescent pregnancy in Maharashtra, India, especially after the COVID-19 pandemic. We collected information from both urban and rural areas in Maharashtra. A total of 3049 adolescent girls participated in a survey, and seven girls participated in detailed interviews. Our analysis showed that factors like older age, being married, having multiple sexual partners, and experiencing economic difficulties due to COVID-19 increased the chances of adolescent pregnancy. On the other hand, living in rural areas, higher education for both the girls and their mothers reduced the likelihood of adolescent pregnancy. Qualitative analysis revealed that economic challenges, concerns about safety and societal norms, early marriage, societal expectations, and lack of knowledge about contraceptives could contribute to adolescent pregnancy in Maharashtra.
Résumé
Il est capital de réduire le taux de natalité chez les adolescentes pour atteindre les objectifs de développement durable liés à la santé, puisque la grossesse et l’accouchement sont la principale cause de mortalité des jeunes femmes âgées de 15 à 19 ans. Cette étude souhaitait explorer les indicateurs de grossesse chez les adolescentes âgées de 13 à 18 ans au Maharashtra, Inde, pendant la pandémie de COVID-19. Au moyen d’une approche à méthodes mixtes, des données primaires ont été recueillis dans deux régions du Maharashtra entre février et avril 2022. Des données quantitatives obtenues au cours d’entretiens en face à face avec 3049 adolescentes ont évalué divers facteurs familiaux, sociaux et comportementaux, ainsi que les conséquences socioéconomiques et sanitaires du COVID-19. Les données qualitatives de sept entretiens approfondis ont fait l’objet d’une analyse thématique. Les résultats révèlent que les jeunes filles issues de milieux socioéconomiques défavorisés sont exposées à une probabilité accrue de grossesse à l’adolescence. Une analyse multivariée a identifié plusieurs facteurs associés à un risque supérieur, notamment l’âge plus avancé, le fait d’être mariée, d’avoir plus de partenaires sexuels et de connaître une vulnérabilité économique liée à la COVID-19. D’autre part, le lieu de résidence en milieu rural, l’éducation secondaire ou secondaire du deuxième cycle des participantes et un niveau plus élevé d’instruction des mères étaient autant de facteurs associés à une probabilité moindre de grossesse chez les adolescentes. Dans le sous-échantillon de 565 jeunes filles en couple, la violence psychologique du partenaire était également corrélée à des taux plus élevés de grossesse. L’analyse thématique des données qualitatives a identifié quatre voies potentielles aboutissant à la grossesse chez les adolescentes: les difficultés économiques et le mariage précoce; la sécurité personnelle, les normes sociales et le mariage précoce; les attentes sociales; et le manque de connaissances sur les contraceptifs. Les conclusions soulignent l’importance de la position sociale et des facteurs comportementaux ainsi que l’impact de chocs externes comme la pandémie de COVID-19 dans la prédiction de la grossesse chez les adolescentes au Maharashtra, Inde.
Resumen
Reducir la tasa de natalidad en la adolescencia es de suma importancia para lograr los Objetivos de Desarrollo Sostenible relacionados con la salud, dado que el embarazo y el parto son las principales causas de mortalidad entre mujeres jóvenes de 15 a 19 años. Este estudio pretendía explorar los predictores del embarazo en la adolescencia entre niñas de 13 a 18 años en Maharashtra, India, durante la pandemia de COVID-19. Utilizando el enfoque de métodos mixtos, se recolectaron datos primarios de dos regiones de Maharashtra entre febrero y abril de 2022. Los datos cuantitativos de entrevistas presenciales con 3049 adolescentes evaluaron diversos factores domiciliarios, sociales y conductuales, así como los impactos de COVID-19 en la socioeconomía y la salud. Se analizaron temáticamente los datos cualitativos de siete entrevistas a profundidad. Los hallazgos revelan que las niñas de bajos niveles socioeconómicos enfrentan mayor probabilidad de embarazo en la adolescencia. El análisis multivariable identificó varios factores asociados con mayor riesgo, tales como edad más avanzada, estar casada, tener más parejas sexuales y experimentar vulnerabilidad económica relacionada con COVID-19. Por otro lado, la residencia rural, la educación secundaria y secundaria superior de las participantes y la educación materna superior estaban asociadas con menor probabilidad de embarazo en la adolescencia. En la submuestra de 565 niñas con pareja, el maltrato emocional por la pareja también estaba correlacionado con mayores tasas de embarazo en la adolescencia. El análisis temático de los datos cualitativos identificó cuatro posibles rutas que conducen al embarazo en la adolescencia: dificultad económica y matrimonio precoz; seguridad personal, normas sociales y matrimonio precoz; expectativas sociales; y falta de conocimiento sobre anticonceptivos. Los hallazgos subrayan la importancia de la posición social y los factores conductuales y el impacto de shocks externos tales como la pandemia de COVID-19 para predecir el embarazo en la adolescencia en Maharashtra, India.
Introduction
Adolescent pregnancy remains a global concern, with approximately 14 million girls under 19 becoming pregnant worldwide in 2021.Citation1 Although there has been a reduction in adolescent pregnancies over time, progress has been uneven across regions. For instance, South Asia has witnessed the sharpest decline in adolescent pregnancies, yet one in five adolescent girls in the region gives birth before the age of 18.Citation2 In India, national estimates suggest that 6.8% of women aged 15–19 began childbearing between 2019 and 2021.Citation3 Adolescent pregnancies are more prevalent in rural areas and in socioeconomically disadvantaged states. For instance, as per the National Family and Health Survey, in Maharashtra, 10.6% of rural women aged 15–19 initiated childbearing, thus exceeding the state average of 7.6%. Similarly, in Tripura and West Bengal, where socioeconomic challenges persist, adolescent pregnancy rates were 22% and 16%, respectively.Citation3 These regional variations underscore the significant burden of adolescent pregnancy in India.
Adolescent pregnancy has numerous negative consequences for both young mothers and their children. It increases the risk of maternal health complications such as pre-eclampsia, eclampsia, infections, unsafe abortion, and mortality.Citation4–7 Additionally, it is associated with higher rates of neonatal deaths, preterm birth, stillbirth, small-for-gestational-age, and low birth weight.Citation8–11 Early pregnancy often leads to school dropout, limiting future educational and employment opportunities for young women.Citation12–16 Furthermore, the COVID-19 pandemic has exacerbated the issue, leading to an increase in child marriages and disruption of sexual and reproductive services, and consequently hindering efforts to reduce adolescent pregnancy.Citation17–22
The existing literature on risk factors related to adolescent pregnancy in South Asia primarily focuses on Nepal, Bangladesh, and Pakistan, with a significant dearth of empirical evidence specific to India despite the substantial population of adolescent girls residing in the country. This knowledge gap is evident from a recent systematic review on adolescent pregnancy in South Asia, which revealed a complete absence of observational studies conducted in India.Citation23 In contrast, an earlier systematic review included four studies from India; however, all were conducted before 2005.Citation24 Furthermore, limited recent empirical studies have examined the impact of the COVID-19 pandemic on adolescent pregnancy, and none of them has been conducted in India.Citation25–27
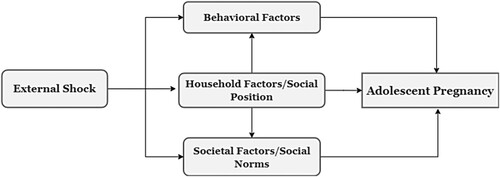
To bridge these research gaps, the present study utilises primary data to investigate household, behavioural, and societal factors associated with adolescent pregnancy during the COVID-19 pandemic in Maharashtra, India. To guide our investigation, we create a conceptual framework that draws upon the social determinants of health model proposed by the World Health Organization,Citation28 the socio-ecological model introduced by Heise,Citation29 and the conceptual framework delineating the impact of COVID-19 on the social determinants of adolescent pregnancy in sub-Saharan Africa, as outlined by Kons et al.Citation22 We adopt this approach to identify and analyse the factors influencing adolescent pregnancy within our context ().
Conceptual framework on adolescent pregnancy
Our conceptual framework proposes that external shocks, such as those triggered by public health emergencies like the COVID-19 pandemic, have a significant influence on the factors related to social position, behaviour, and social norms, consequently impacting the occurrence of adolescent pregnancy (). This framework extends Heise'sCitation29 socio-ecological model by highlighting the role of public health emergencies as catalysts for changes in these factors. For instance, a public health emergency may exacerbate a family's economic hardship, leading them to arrange an early marriage for their adolescent daughter as a means of alleviating financial burdens, thereby increasing the risk of adolescent pregnancy.Citation30,Citation31 Moreover, during public health emergencies, the lack of resources and economic constraints experienced by families may drive adolescent girls to engage in transactional sex to meet basic needs such as food or healthcare expenses, thereby heightening the likelihood of unintended pregnancies.Citation32 Additionally, pervasive gender-inequitable social norms that devalue girls’ education, encourage early marriage, restrict decision-making autonomy, and limit control over fertility choices, contribute to the disempowerment of women and girls. These norms ultimately undermine the sexual and reproductive health rights of adolescents, thereby increasing their vulnerability to adolescent pregnancy.Citation33
To the best of our knowledge, this study represents the first explicit modelling of the health and socioeconomic consequences of the pandemic on adolescent pregnancy. It contributes to the literature by employing a rigorous triangulation approach, integrating data from two sources (quantitative and qualitative) and employing three analytical approaches. Through quantitative survey data, we estimate the prevalence of adolescent pregnancy in two regions of Maharashtra and identify associated factors. Qualitative interviews with adolescent mothers offer rich insights into contextual factors and pathways to adolescent pregnancy. Additionally, cluster analysis identifies distinct social groups within the sample and their varying risk profiles for adolescent pregnancy during the pandemic.
Methods
Study design and setting
The data for this study were collected as a part of the COV-CSRD (Impact of COVID-19 on the Lives of adolescent girls in India and Zambia) project between February and April 2022. This community-based mixed-methods study was conducted in two regions in the state of Maharashtra, India: in urban settlements around the cities of Pune and Pimpri-Chinchwad and in rural villages of the Sangli district.
In Maharashtra, primary education is mandatory; about 93% of children aged 6–17 years in the state are enrolled in schools.Citation3 Maharashtra is one of the most industrialised states in India, with manufacturing industry and agriculture being the primary places of occupation. Nearly 37% of the population live below the poverty line. Further, around 31.5% and 53.6% of women are main (six months or more) and marginal (less than three months) workers, respectively. Lastly, lower castes, including scheduled castes (SC), scheduled tribes (ST), and other backward classes (OBC), account for about 55.2% of the population, and Muslims account for about 11.5%.Citation34
Study population and recruitment
A mapping exercise was conducted in schools and surrounding communities within both study areas to sample eligible girls. Adolescent girls aged 13–18 were recruited in the Pune and Pimpri-Chinchwad area and in Sangli, using simple random sampling via two approaches: identification of girls within the target age range by teachers in schools, and door-to-door community visits by trained enumerators, using a pre-defined random walk procedure. Both approaches included school-going adolescents and dropouts. A total of 3049 adolescent girls were included in this study. The study was conducted with minors, so we followed a two-stage consent procedure. First, trained enumerators collected written informed consent from a parent or legal guardian before data collection, and second, verbal assent was secured from the adolescent girl before the interview. For adolescent girls who were 18 years old or married at the time of data collection, the informed consent procedure did not involve parents, guardians, in-laws, or husbands.
Data collection and measures
Quantitative data collection
Data were collected face-to-face by trained local enumerators using a structured questionnaire either at the school or in the community, lasting between 45 and 60 minutes. The survey instrument was first prepared in English, later translated into Marathi and Hindi (the local languages) by a language expert, and then translated back into English. This instrument was piloted in the community prior to commencing data collection. The final version of the questionnaire was available in three languages. It was administered on mobile tablets alongside audio- and computer-assisted self-interview (ACASI) format for sensitive questions on girls’ sexual experiences and behaviours. We applied the ACASI format to maximise confidentiality and reduce under-reporting.Citation35
Adolescent pregnancy, i.e. pregnancy at 19 or below, was our study’s primary outcome of interest.Citation4 One binary item measured the outcome (0: never pregnant; 1: currently pregnant or has been pregnant before).
Variables of interest were categorised into four groups to reflect the factors outlined in our conceptual framework (). First, factors related to household characteristics or girls’ social position included variables measuring age, residence, caste, religion, girls’ education, parents’ education, household wealth, marital status, the presence of older female siblings living with the participant, and employment of the participant (drawn from items used in the NFHS-5, 2019-21Citation3). We classify participants based on caste as an important cultural and social construct intertwined with people’s socioeconomic status in the Indian context. Further, we divide the participants into Muslim and non-Muslim groups, as Muslim minorities are often discriminated against in India. By doing so, we are not reinforcing the stigma associated with these categories but instead trying to capture their relationships with other factors influencing adolescent pregnancy, as depicted in . In addition to these factors, four measures of intimate partner violence (IPV) (i.e. emotional, physical, sexual, and control) were also included in this group for a sub-analysis with a sample of partnered girls.Citation36
A second group of variables were behavioural factors, including self-reported information on the use of condom and number of sexual partners.Citation3
Third, we collected data on societal factors, comprising an index capturing girls’ empowerment (including 11 indicators on their voice, control over life choices, and decision-making)Citation37 and an index capturing sexual norms and attitudes (including three indicators).Citation3
A fourth group of variables included factors related to external shocks. Specifically, we focused on the impact of the COVID-19 pandemic by constructing two indices, one focusing on the health impact (comprising six indicators)Citation38 and the other on the socioeconomic impact (comprising five indicators) of the pandemic.Citation39 A detailed explanation of how these variables were characterised and measured and references for validated measurements can be found in the Additional file (Table A1&A2).
Quantitative data analysis
All analyses were completed in StataMP 17 and R-studio (“ade4” package).Citation40 Data were anonymised before analysis, and the codes are accessible at the OSF repository. First, logistic regression was performed for bivariate analyses to examine the association between each predictor variable and the outcome. Second, multivariable logistic regression was performed to predict adolescent pregnancy using the four blocks of predictor variables identified by the conceptual framework: (i) household or social position-related factors, (ii) behavioural factors, (iii) societal factors, and (iv) external shock-related factors. Variables were added to the model sequentially, with factors progressing from individual-level to structural-level importance. A multicollinearity check was applied using a variance inflation factor (VIF) with a cut-off of seven.Citation41
Block 1 included only household or social position-related factors, block 2 included household or social position-related factors and behavioural factors, block 3 included household or social position-related factors, behavioural factors, and societal factors, and block 4 included all factors of the conceptual framework. Model robustness was assessed using the Wald Chi-square test, McFadden's R2, and Count R2 to compare the different models,Citation42 and goodness of fit was assessed using Hosmer and Lemeshow test.
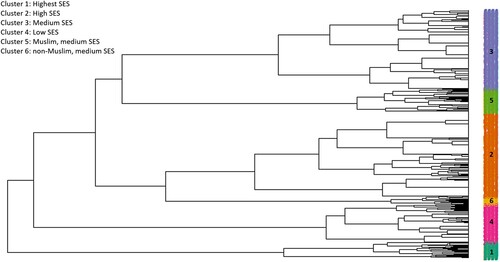
Finally, cluster analysis was performed to investigate how social position-related factors cluster among adolescent girls. This analysis did not include other factors, as social position influences behavioural and societal characteristics in the larger population.Citation29 This paper applies cluster analysis to integrate adolescent girls into similar groupings and identify which social groups are most vulnerable to adolescent pregnancy. Categorical factors, including caste, religion, girl’s education, mother’s education, father’s education, employment, and household wealth, were included in the cluster analysis for the 3049 adolescent girls. First, multiple correspondence analysis (MCA) was applied to represent data as points in a low-dimensional Euclidean space. The MCA summarises categorical variables into hierarchical orthogonal axes.Citation43 We then selected the first five axes for more than 50% of the sample variance. The Ward method was then used to perform hierarchical clustering, presented with a dendrogram. The Ward method minimises within-cluster variance by grouping observations (i.e. adolescent girls) with similar values in the MCA axes. A dendrogram visualises the dissimilarity between different clusters, and observations are allocated to clusters by drawing a horizontal line through the dendrogram. Next, the K-means algorithm was implemented to partition the data into distinct cluster solutions.Citation44 Logistic binomial regression was used to estimate the crude odds ratio (OR) comparing adolescent pregnancy between each cluster with cluster 1 as the reference. A p-value of <0.05 was set as significant.
Qualitative data and analysis
Qualitative data on sexual and reproductive health were gathered through seven in-depth interviews (IDIs) with adolescent girls who were part of the quantitative data collection and were flagged for teenage pregnancy or child marriage. Thematic saturation was achieved within these interviews, leading to no further interviews (Additional file: Table A3).
Participants were recruited purposively for IDIs if they disclosed being married underage and/or they reported a current pregnancy, past pregnancy, or abortion during the quantitative interviews. The semi-structured topic guide was developed based on the quantitative results to elicit the channels related to adolescent pregnancy and was piloted in the community before actual data collection. Trained local female interviewers, along with the primary author (SS) and RVS, a freelance researcher based in Maharashtra, conducted the interviews. The face-to-face interviews were held at private locations chosen by the participants and typically lasted between 30 and 45 minutes. The primary author (SS), originally from Madhya Pradesh, India, brought valuable insights from her decade-long experience of living in different areas of Maharashtra. She assumed the role of the note-taker during the interviews and provided a clear explanation of the study's objectives and background before proceeding with data collection. The interviews were audio recorded and transcribed verbatim in Hindi or Marathi (the participant's preferred language) and later translated into English for analysis. Thematic coding was applied to analyse the data by two authors independently, and disagreements were resolved through discussion. Ten themes relating to the causes of marriage and pregnancy were identified. ATLAS.ti was used for coding and qualitative analysis.
Ethical considerations
Ethical approval was obtained from the Institutional Review Board (IRB) at the Indian Institute of Technology Gandhinagar (IITG) on 26 November 2021 and at the Technical University of Munich (TUM) on 29 December 2021. We obtained authorisation to collect data in the schools of Pune, Pimpri-Chinchwad, and Sangli from their respective education departments at the local municipal corporation. Participants and their legal guardians were informed before data collection at the community level. Enumerators explained the participant's rights to confidentiality and anonymity and the study’s objectives before collecting the informed consent. Group or individual counselling was provided when necessary to ensure the mental health and wellbeing of enumerators and respondents.Citation45
Results
Respondent characteristics
As shown in , out of the 3049 participants, 146 (4.8%) became pregnant before the age of 19. Of these, 26 adolescent pregnancies occurred in the urban settlements of Pune/Pimpri-Chinchwad (17.8%) and 120 in the rural villages of Sangli (82.2%). Almost all pregnancies (99%) were reported by girls aged between 16 and 18 years, and only one was reported for a 13–15-year-old (see Additional file Table A4). The average age of participants was 15.5 years (SD = 1.48), 303 (9.9%) participants were Muslim and 2040 (67%) participants belonged to a lower caste (i.e. ST, SC, or OBC). Regarding relationship status, 277 (9.1%) girls were married, and 280 (9.2%) reported having a boyfriend. Furthermore, 311 (10.2%) adolescent girls reported having any sexual experience, and 55 (17.7%) girls indicated that they used a condom the last time they had sex. Most of the girls were educated until secondary level (grade 10) (73.8%), and very few received higher secondary education (grade 12) (3.9%). 5.1% of the girls’ fathers and 2.2% of their mothers had attained a post-secondary level of education. 502 (16.5%) girls had some form of informal or formal employment at the time of the interview, and 2335 (76.6%) went back to school after the COVID-19 lockdown. Please refer to Table A4 in the additional file for characteristics disaggregated by pregnancy status.
Table 1: Descriptive characteristics of study respondents (N = 3049) in Maharashtra, India
In the sub-sample of 565 partnered girls, 277 (49%) were married, and 288 (51%) were widowed, divorced, or had a boyfriend. Only three non-partnered girls and two unmarried girls with boyfriends were pregnant in our sample. In the Indian context, pregnancy outside of marriage is stigmatised, and as a result, families tend to marry their daughters if they fall pregnant. Out of the partnered girls, 155 (27.2%) girls had been exposed to sexual violence, 238 (42.1%) had experienced physical violence, and 319 (56.7%) had faced emotional violence by their partners. Furthermore, 347 (61.5%) girls reported being in a relationship with a controlling partner.
Multivariable analysis
Significant factors associated with adolescent pregnancy were identified through independent bivariate logistic regressions prior to multivariable analysis. Positive associations (p < 0.05) were found for variables including age, rural residence, low caste, marital status, employment, condom use, multiple sexual partners, harmful sexual norms, and COVID-19-related economic and health vulnerability. Conversely, negative associations (p < 0.05) were observed for variables including Muslim religion, wealth, participants’ secondary education, mother’s secondary education, father’s secondary and post-secondary education, older female sibling, and empowerment. Notably, the respondent's higher secondary education and the mother's post-secondary education did not significantly correlate with adolescent pregnancy (Additional file Table A5a&b).
We checked for multicollinearity between predictors before the regression analysis (Additional file Table A6). Results from the multivariable logistic regression analyses are presented in . After adjusting for all other social position factors in Model 1, the likelihood of adolescent pregnancy is higher for older and married girls. In contrast, participants’ education and mothers’ secondary education decreases the likelihood of adolescent pregnancy. Model 2 shows that these factors remain significantly associated with adolescent pregnancy even after including behavioural factors. After adjusting for social factors, Model 3 shows that older age, being married, the number of sexual partners, and harmful sexual norms increase the likelihood of adolescent pregnancy. In the final Model 4, including all the predictors, older age (AOR: 1.952, p < 0.01), being married (AOR: 131.482, p < 0.01), number of sexual partners (AOR: 1.523, p < 0.1), and COVID-19-related economic vulnerability (AOR: 3.241, p < 0.05) are associated with a higher likelihood of adolescent pregnancy. Residence in a rural location (AOR: 0.408, p < 0.05), participant’s secondary education (AOR: 0.425, p < 0.01) and higher secondary education (AOR: 0.247, p < 0.05), and mother’s education (AOR: 0.522, p < 0.1) are associated with a lower likelihood of adolescent pregnancy. It is important to note that the AOR of marital status is extremely high. It may be an artefact of the Indian context, where pregnancy outside of marriage is rare in this age group, and families typically expect childbearing immediately after marriage.Citation46,Citation47 The high regression coefficient is thus explained by the small number of unmarried girls (n = 5) who had children (see Additional File Figure 1). Furthermore, marital status and variables such as the place of residence and parents’ education are correlated (Additional Table A6). Therefore, the multivariable analysis may mask their association with the outcome variable.
Table 2: Associations between adolescent pregnancy and household/social position, behavioural, societal and external shock-related factors (N = 3049)
In a further analysis for the sub-sample of partnered girls (Additional Table A7), factors were added block-wise, with four additional variables capturing IPV in the household or social position block. The final model, including all predictors, shows that age (AOR: 1.691, p < 0.01), being married (AOR: 103.412, p < 0.01), suffering from emotional IPV (AOR: 2.590, p < 0.05), and COVID-19 related economic vulnerability (AOR: 2.803, p < 0.1) increase the likelihood of adolescent pregnancy among partnered girls. Other forms of IPV, namely sexual and physical abuse and partners’ controlling behaviour, are not significantly associated with adolescent pregnancy. Similar to the whole sample, residence at a rural location (AOR: 0.29, p < 0.05), participant’s secondary education (AOR: 0.496, p < 0.05), and higher secondary education (AOR: 0.345, p < 0.1), and mother’s education (AOR: 0.475, p < 0.1) decrease the likelihood of adolescent pregnancy.
Cluster analysis
We identified two possible models of social positions, with five and six clusters. The six-cluster solution was selected because it identified the various categories of girls with more nuances than the five-cluster solution. Higher-order solutions were less parsimonious and did not offer relevant insights. The first two branches of the dendrogram represent a significant social cleavage, where girls with the highest socioeconomic status (SES) are segregated from girls with medium or low SES early on in life ().
The first branch is also our first cluster (Highest SES, n = 187) which comprises mainly unemployed non-Muslim girls with secondary level of education, primarily living in families with high wealth and parents with secondary to post-secondary education. The girls in this cluster have relatively higher socioeconomic capital than the rest of the sample (second branch), accounting for a small fraction of the pregnancies in the sample, namely, 0.5%. The second cluster (High SES, n = 1043) comprises both low (63%) and general caste girls (37%), mainly non-Muslim, unemployed, having secondary level of education, with parents educated till secondary level and having high wealth. This cluster is close to Cluster 1 in terms of socioeconomic capital and accounts for about 5.4% of pregnancies.
The third cluster (Medium SES, n = 961) represents non-Muslim girls who belong to a lower caste, have secondary education and are unemployed, have parents with a primary to secondary level of education, and have medium wealth. It accounts for about 9.7% of pregnancies. The fourth cluster (Low SES, n = 472) represents a composite measure of girls with relatively low socioeconomic status. Many of these girls belong to a lower caste, are non-Muslim, are educated till primary or secondary level, are employed, have parents with primary education, and live in families with lower wealth. This cluster has the highest proportion of pregnancies, with about 20.2%.
The fifth cluster (Muslim, medium SES, n = 284) mainly represents Muslim girls with secondary level of education, living in families with medium to high wealth and having parents educated till primary or secondary level. It accounts for 5.7% of pregnancies. In the last cluster (non-Muslim medium SES, n = 102), all girls belong to non-Muslim households with medium to high wealth. They are all educated till higher secondary level and have parents educated till primary or secondary level. The proportion of pregnancies in this cluster is close to 15.1%. The membership details and the proportion of pregnancies are listed in Additional Tables A8a&b.
These clusters show how socioeconomic conditions, educational opportunities, and religious affiliation jointly shape the realities of adolescents in Maharashtra. Contexts with poor socioeconomic and educational conditions strongly determine adolescent girls’ health outcomes, including their propensity to marry and become adolescent mothers. The highest percentage of adolescent pregnancy (20%) is found in Cluster 4, with almost four times higher adolescent pregnancy than in the entire sample followed by Cluster 6 (15%) and Cluster 3 (9.7%). Belonging to Cluster 3 (OR: 2.462, p < 0.05), Cluster 4 (OR: 3.082, p < 0.01), or Cluster 6 (OR: 2.559, p < 0.05) translates into a significantly higher likelihood of adolescent pregnancy compared with Cluster 1, the cluster with highest SES (). Here, characteristics like non-Muslim, lower caste, low education levels of parents, and low to medium wealth cluster together. This means a higher risk of pregnancy among girls living in a configuration of socioeconomic disadvantage and reduced educational opportunities. We compared the goodness of fit of this model with a complete model, including the seven social position-related factors (Additional Table A9). We find that the cluster model fits the prediction of adolescent pregnancy better than the full model (BIC = 1,123 vs BIC = 1,139), suggesting that adolescent pregnancy is intersectional, i.e. the confluence of disadvantaged social circumstances in adolescents’ lives increases their vulnerability towards adolescent pregnancy in a synergistic manner rather than additive.
Table 3: Association between adolescent pregnancy and various social position clusters
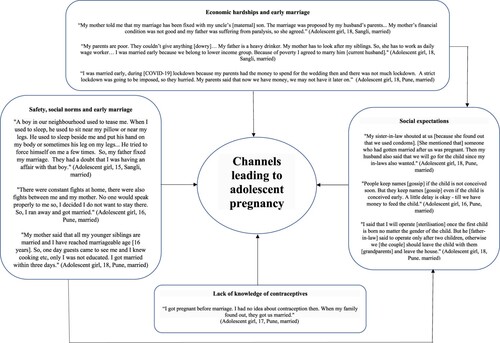
Qualitative analysis
The seven girls selected for IDIs were married before the age of 16 and had dropped out of school before or after marriage. Two were pregnant at the time of the interview, and five had one or more children (for more information on the participants’ profiles, please see Additional file: Table A3).
The qualitative data shed light on some of the associations revealed in the quantitative analyses. First, participants highlighted that their families were economically disadvantaged even prior to the pandemic. In most families included in this study, the girls’ parents were involved in daily wage or domestic work, which was severely impacted by the lockdown measures. These existing economic hardships were exacerbated by the COVID-19 pandemic and were linked to the girls being married early. The reasons cited for early marriage were to save wedding costs during the lockdown or to avoid paying a dowry in cases where the parents had a family relationship with the in-laws, and there were no demands for gifts.
Second, girls discussed concerns about their safety at home given the increased stress during the pandemic and restrictive social norms like the expectation of getting married young, girls being a burden on their family, controlled interaction with boys, limited movement outside the house before marriage or maintaining the family’s honour being imposed on them, thus leading them and/or their families to favour early marriage.
While marriage usually precedes pregnancy in the Indian context, a third channel links the abovementioned channels with adolescent pregnancy. Soon after marriage, social expectations around childbearing from in-laws and relatives were cited as the intermediary channel leading to adolescent pregnancy. Three participants discussed using condoms to delay pregnancy but eventually stopped as the social pressure to have a child increased. On the other hand, three girls (all married at 14 and aged between 16 and 18 at the time of the interview) mentioned that it was their choice to become pregnant as they wanted children and a family of their own, and therefore decided against contraception.
Fourth, one participant mentioned that the lack of knowledge of contraceptives led to her pregnancy at the young age of 11, subsequently leading to her marriage as soon as the family discovered this. She further discussed using condoms as a contraceptive method to space her two children. Selected quotes from the interviews are presented in .
Discussion
The present study examined the prevalence and determinants of adolescent pregnancy among 3049 adolescent girls in Maharashtra, India, during the COVID-19 pandemic. The findings were obtained through a mixed-methods approach, combining quantitative survey data with qualitative interviews in two regions – the urban slums of Pune and Pimpri-Chinchwad and the rural villages of Sangli. The findings reveal that approximately 5% of the sampled adolescent girls became pregnant before age 19. Several factors, including age, rural residence, secondary and higher secondary education of the participants, being married, number of sexual partners, maternal secondary education, and economic vulnerability related to the COVID-19 pandemic, consistently emerged as predictors of adolescent pregnancy. Among partnered girls, emotional abuse was also associated with adolescent pregnancy.
To comprehensively understand the complex phenomenon of adolescent pregnancy within the Indian context, we employed a rigorous analytical framework of three distinct approaches. We aimed to complement the strength of probabilistic interpretation via regression analysis with cluster analysis, which helped us identify social segregation patterns between low and high-SES girls from an intersectional perspective. Further, the thematic analysis of IDIs enabled us to gain valuable insights into the lived realities and social dynamics contributing to adolescent girls’ pregnancies in the Indian context. Together, these approaches highlight that adolescent girls living in families with limited financial resources, belonging to lower castes, experiencing educational discontinuity at the primary or secondary level, and having parents with limited education (primary or secondary level) face a heightened risk of early pregnancy.
In the quantitative analysis, we reported that married adolescent girls were more likely to be pregnant. These findings are consistent with previous studies conducted in India, Nepal, and Bangladesh.Citation9,Citation48–51 Most adolescent girls start menstruating by age 14,Citation52 translating into marriage eligibility in many societies. Early or child marriage is a common practice in South Asian countries, including India, and is also associated with multiple unwanted pregnancies.Citation48 In this context, the qualitative findings highlight that social expectations and social norms concerning marriage were important channels linked with adolescent pregnancy. Previous qualitative studies from India agree with this finding.Citation46,Citation47,Citation53 Decision on contraceptive use is usually made by husbands and in-laws,Citation53 and married adolescent girls are under immense pressure from them to conceive a child immediately after marriage.Citation46,Citation47 Girls often comply with these demands due to fear of domestic violence, being labelled barren, or losing their social position.Citation47,Citation53 These reasons may also relate to the significant association between emotional IPV and adolescent pregnancy observed in our sample.
Similar to other studies from South Asia, we also found that participants’ higher education decreased the likelihood of adolescent pregnancyCitation50,Citation54–57 and lower maternal education increased it.Citation58 Our cluster analysis confirmed similar associations with adolescents’ and parents’ poor educational attainment. We report that low and medium SES groups with lower wealth, poor educational attainment among participants and their parents, lower caste, and non-Muslim affiliation were associated with a higher likelihood of adolescent pregnancy. While comparing the BIC of the cluster model with the BIC of the seven individual social position variables model, we found that the cluster model fits better. This suggests that adolescent pregnancy can be understood as the result of the confluence of circumstances in adolescents’ lives. That is, the social position-related factors function synergistically to predict the likelihood of adolescent pregnancy rather than affecting it in an additive fashion. Our qualitative findings also support these associations. All pregnant adolescent girls interviewed in our sample dropped out of school either at the primary or secondary school level. They all belonged to working-class, non-Muslim, low-caste families and often mentioned the negative impact of economic hardships on their lives, including early marriage and subsequent pregnancy.
Furthermore, our study reported a positive association between the number of sexual partners and adolescent pregnancy. These results concur with previous studies in LMICs.Citation41,Citation59 In addition, girls showcased limited awareness of contraceptive methods beyond condoms and birth control pills in the qualitative interviews.Citation60,Citation61 Lastly, we reported a positive association between COVID-19 pandemic-related socioeconomic vulnerability and adolescent pregnancy. While there is little research on this association, one empirical study in Kenya concluded that girls experiencing COVID-19 lockdown measures had twice the risk of adolescent pregnancy before completing secondary school.Citation25 Informing this association, the IDIs highlight that the COVID-19 pandemic worsened the existing economic conditions of the families, subsequently leading to early marriages and related pregnancies. Building on this, we can hypothesise that health emergencies can exacerbate the existing social inequalities and further segregate adolescent girls into vulnerable groups characterised by limited opportunities to return to school, inadequate economic resources, and increased risk of social harm.Citation62,Citation63
This study has several limitations. First, the cross-sectional nature of the data do not allow us to establish a causal link between the predictors and adolescent pregnancy or to investigate mediation pathways. To mitigate this, we conducted qualitative interviews with pregnant girls to unpack the channels associated with the predictors. The qualitative data suggest that marriage often precedes conception and is one of the most important predictors of adolescent pregnancy in this context. However, we did not interview adolescent girls from high SES families as the cluster methodology was applied after data collection. We cannot, therefore, comment on additional channels that might work for girls in high SES families. Second, we could not compare our results with estimates on pre-pandemic adolescent pregnancy rates collected in the same sample of girls and households. Future studies could collect longitudinal data on predictors of adolescent pregnancy to compare how the associations evolve over time. Third, marriage before the age of 18 is illegal in India and, therefore, prone to non-disclosure. Consequently, some girls could not be recruited into the study either because their parents were unwilling to consent or they were afraid of their in-laws or husbands. Nevertheless, we tried to minimise possible repercussions by utilising self-interview techniques and extensively training enumerators to use non-judgemental communication. Fourth, we collected data at only two locations in Maharashtra. The generalisability of our findings beyond these regions in Maharashtra requires additional research with samples from other states in India.
Despite these shortcomings, this is the first mixed-methods study to examine the predictors of adolescent pregnancy during the COVID-19 pandemic in India. The timely context of this study sheds light on how pandemics may exacerbate the existing vulnerabilities of adolescent girls and help policymakers prioritise their efforts. One way to do this could be integrating efforts to delay child marriage under the Protection of Children from Sexual Offences (POCSO) Act to include girls up to 18 years. Another way could be to strengthen comprehensive sexuality education in schools and youth-friendly centres where adolescents can seek information and services without fear or stigma. Apart from this, our study employs cluster analysis to identify social segregation patterns between low and high-SES girls. By exploring the differences between these groups, the study goes beyond individual-level factors and highlights the importance of considering broader social contexts and structural inequalities in understanding adolescent pregnancy. As India continues to have one of the youngest populations in the world, interventions must support measures like continued education after marriage, parenting programmes, and skill development activities to address the unique circumstances faced by adolescent girls. A combination of empowerment strategies and policies, such as contraceptive availability and increasing the legal age of marriage, could be beneficial in reducing adolescent pregnancies in the long run.
Author contributions
JIS secured funding for the project. SS and JIS conceptualised the study. Data collection was overseen by SS and RVS. AFCT and SS conducted and interpreted the cluster analysis. SS led the analysis of quantitative and qualitative data and drafted the manuscript. All authors provided significant revisions and approved the final version, taking accountability for all aspects of the work's accuracy and integrity.
Supplemental Material
Download MS Word (155.3 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplemental data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/26410397.2023.2249284.
Additional information
Funding
References
- UNICEF. Early childbearing and teenage pregnancy rates by country; 2022 [cited 2023 Feb 2]. Available from: https://data.unicef.org/topic/child-health/adolescent-health/#:~:text = Globally%20in%202021%2C%20an%20estimated,their%20education%2C%20livelihoods%20and%20health.
- UNICEF South Asia. Adolescents in South Asia. 2016 [cited 2023 Jan 5]. Available from: https://www.unicef.org/rosa/what-we-do/adolescents.
- International institute for population sciences (IIPS) and ICF. National family health survey (NFHS-5), 2019-21: India: volume 1. Mumbai: IIPS; 2021.
- Ganchimeg T, Ota E, Morisaki N, et al. Pregnancy and childbirth outcomes among adolescent mothers: a world health organization multicountry study. BJOG: An Int J Obstet Gynaecol. 2014;121:40–48. doi:10.1111/1471-0528.12630
- Althabe F, Moore JL, Gibbons L, et al. Adverse maternal and perinatal outcomes in adolescent pregnancies: the global network's maternal newborn health registry study. Reprod Health. 2015;12(Suppl 2):S8. doi:10.1186/1742-4755-12-S2-S8
- Darroch JE, Woog V, Bankole A, et al. Adding it up: costs and benefits of meeting the contraceptive needs of adolescents; 2016.
- Maheshwari MV, Khalid N, Patel PD, et al. Maternal and neonatal outcomes of adolescent pregnancy: a narrative review. Cureus. 2022;14(6):e25921. doi:10.7759/cureus.25921
- Neal S, Matthews Z, Frost M, et al. Childbearing in adolescents aged 12–15 years in low resource countries: a neglected issue. New estimates from demographic and household surveys in 42 countries. Acta Obstet Gynecol Scand. 2012;91(9):1114–1118. doi:10.1111/j.1600-0412.2012.01467.x
- Patra S. Motherhood in childhood: addressing reproductive health hazards among adolescent married women in India. Rep Health. 2016;13(1):1–9. doi:10.1186/s12978-016-0171-7
- Noori N, Proctor JL, Efevbera Y, et al. The effect of adolescent pregnancy on child mortality in 46 low-and middle-income countries. medRxiv. 2021;2021-06.
- Akseer N, Keats EC, Thurairajah P, et al. Characteristics and birth outcomes of pregnant adolescents compared to older women: an analysis of individual level data from 140,000 mothers from 20 RCTs. EClinic Med. 2022;45:101309. doi:10.1016/j.eclinm.2022.101309
- World Health Organization. Global standards for quality health-care services for adolescents: a guide to implement a standards-driven approach to improve the quality of health care services for adolescents; 2015.
- UNESCO. Early and unintended pregnancy & the education sector: evidence review and recommendations. Paris: 2017.
- Birchall J. Early marriage, pregnancy and girl child school dropout. K4D helpdesk report. Brighton: Institute of Development Studies; 2018.
- Cruz E, Cozman FG, Souza W, et al. The impact of teenage pregnancy on school dropout in Brazil: a Bayesian network approach. BMC Public Health. 2021;21(1):1–8. doi:10.1186/s12889-021-11878-3
- Tsague-Agnoux M, Fezeu LK, Ndonko F. Teenage childbearing and school dropout in a sample of 18,791 single mothers in Cameroon. Reprod Health. 2022;19(1): 10. doi:10.1186/s12978-021-01323-4
- Shukla S, Ezebuihe JA, Steinert JI. Association between public health emergencies and sexual and reproductive health, gender-based violence, and early marriage among adolescent girls: a rapid review. BMC Public Health. 2023;23(1):1–14. doi:10.1186/s12889-023-15054-7
- Meherali S, Adewale B, Ali S, et al. Impact of the COVID-19 pandemic on adolescents’ sexual and reproductive health in Low- and middle-income countries. Int J Env Res Publ Health. 2021;18(24):13221. doi:10.3390/ijerph182413221
- UNICEF. COVID-19: a threat to progress against child marriage. UNICEF; 2021.
- Yukich J, Worges M, Gage AJ, et al. Projecting the impact of the COVID-19 pandemic on child marriage. J Adoles Health. 2021;69(6):S23–S30. doi:10.1016/j.jadohealth.2021.07.037
- Okeke SR, Idriss-Wheeler D, Yaya S. Adolescent pregnancy in the time of COVID-19: what are the implications for sexual and reproductive health and rights globally? Reprod Health. 2022;19(1):1–5. doi:10.1186/s12978-022-01505-8
- Kons K, Biney AA, Sznajder K. Factors associated with adolescent pregnancy in Sub-Saharan Africa during the COVID-19 pandemic: a review of socioeconomic influences and essential interventions. Int J Sex Health. 2022;34(3):386–396. doi:10.1080/19317611.2022.2084199.
- Poudel S, Razee H, Dobbins T, et al. Adolescent pregnancy in south Asia: a systematic review of observational studies. Int J Environ Res Public Health. 2022;19(22):15004. doi:10.3390/ijerph192215004
- Acharya DR, Bhattaria R, Poobalan AS, et al. Factors associated with teenage pregnancy in south Asia: a systematic review. Health Sci J. 2010;4(1):3–14.
- Zulaika G, Bulbarelli M, Nyothach E, et al. Impact of COVID-19 lockdowns on adolescent pregnancy and school dropout among secondary schoolgirls in Kenya. BMJ Glob Healt. 2022;7(1):e007666. doi:10.1136/bmjgh-2021-007666
- Karp C, Moreau C, Sheehy G, et al. Youth relationships in the era of COVID-19: a mixed-methods study among adolescent girls and young women in Kenya. J Adoles Healt. 2021;69(5):754–761. doi:10.1016/j.jadohealth.2021.07.017
- Rahiem MD. COVID-19 and the surge of child marriages: a phenomenon in Nusa Tenggara Barat, Indonesia. Child Abuse Negl. 2021;118:105168. doi:10.1016/j.chiabu.2021.105168
- World Health Organization. A conceptual framework for action on the social determinants of health; 2010.
- Heise LL. Violence against women. Viol Again Women. 1998;4(3):262–290. doi:10.1177/1077801298004003002
- Asadullah MN, Islam KMM, Wahhaj Z. Child marriage, climate vulnerability and natural disasters in coastal Bangladesh. J Biosoc Sci. 2021;53(6):948–967. doi:10.1017/S0021932020000644
- Psaki SR, Melnikas AJ, Haque E, et al. What are the drivers of child marriage? A conceptual framework to guide policies and programs. J Adoles Heal. 2021;69(6):S13–S22. doi:10.1016/j.jadohealth.2021.09.001
- Jacobson L, Regan A, Heidari S, et al. Transactional sex in the wake of COVID-19: sexual and reproductive health and rights of the forcibly displaced. Sex Reprod Healt Matter. 2020;28(1):1822493. doi:10.1080/26410397.2020.1822493
- Azcona G, Bhatt A, Davies SE, et al. Spotlight on gender, COVID-19 and the SDGs: will the pandemic derail hard-won progress on gender equality?; 2020.
- Economic Survey of Maharashtra. Directorate of economics and statistics, planning department. Mumbai: Government of Maharashtra; 2021-22. Available from: http://mls.org.in/pdf2022/budget/ESM_2021_22/Economic%20Survey%20of%20%20Maharashtra%202021-22.pdf.
- Falb K, Tanner S, Asghar K, et al. Implementation of Audio-Computer Assisted Self-Interview (ACASI) among adolescent girls in humanitarian settings: feasibility, acceptability, and lessons learned. Confl Health. 2016;10(1):1–8. doi:10.1186/s13031-016-0098-1
- Zolotor AJ, Runyan DK, Dunne MP, et al. ISPCAN child abuse screening tool children's version (ICAST-C): instrument development and multi-national pilot testing. Child Abuse Negl. 2009;33(11):833–841. doi:10.1016/j.chiabu.2009.09.004
- Dhar D, Jain T, Jayachandran S. Reshaping adolescents’ gender attitudes: evidence from a school-based experiment in India. NBER Work Paper, 25331; 2018.
- Grasso DJ, Briggs-Gowan MJ, Ford JD, et al. The epidemic–pandemic impacts inventory (EPII). University of Connecticut School of Medicine; 2020.
- Petrosyan S, Theys N, Chien S, et al. Real time insights (RTI): COVID-India: rounds 1-9, 2020-2022 data collection]. Version A; 2022. doi:10.25549/cgvw-zm73
- Dray S, Dufour AB. Theade4package: implementing the duality diagram for ecologists. J Stat Softw. 2007;22:1–20. doi:10.18637/jss.v022.i04
- Ochen AM, Chi PC, Lawoko S. Predictors of teenage pregnancy among girls aged 13–19 years in Uganda: a community based case-control study. BMC Pregn Child. 2019;19(1). doi:10.1186/s12884-019-2347-y
- Allison P. What’s the best R-squared for logistic regression. Stati Horiz. 2013;13. Accessed 6 Feb 2023. https://statisticalhorizons.com/r2logistic/.
- Husson F, Josse J, Pages J. Principal component methods-hierarchical clustering-partitional clustering: why would we need to choose for visualizing data. Agrocampus Ouest Applied Mathematics Department. 2010;17. http://www.sthda.com/english/upload/hcpc_husson_josse.pdf
- Kaufman L, Rousseeuw PJ. Finding groups in data: an introduction to cluster analysis. John Wiley & Sons; 2009.
- Steinert JI, Nyarige DA, Jacobi M, et al. A systematic review on ethical challenges of ‘field’ research in low-income and middle-income countries: respect, justice and beneficence for research staff? BMJ Global Health. 2021;6(7):e005380. doi:10.1136/bmjgh-2021-005380
- Barua A, Kurz K. Reproductive health-seeking by married adolescent girls in Maharashtra, India. Reprod Health Matter. 2001;9(17):53–62. doi:10.1016/S0968-8080(01)90008-4
- Dixit A, Bhan N, Benmarhnia T, et al. “It is painful and unpleasant”: experiences of sexual violence among married adolescent girls in Shinyanga, Tanzania. Rep Health. 2021;18:1–9. doi:10.1186/s12978-020-01058-8
- Raj A, Saggurti N, Balaiah D, et al. Prevalence of child marriage and its effect on fertility and fertility-control outcomes of young women in India: a cross-sectional, observational study. Lancet. 2009;373(9678):1883–1889. doi:10.1016/S0140-6736(09)60246-4
- Devkota HR, Clarke A, Shrish S, et al. Does women’s caste make a significant contribution to adolescent pregnancy in Nepal? A study of Dalit and non-Dalit adolescents and young adults in Rupandehi district. BMC Womens Health. 2018;18:1–11. doi:10.1186/s12905-018-0513-4
- Alam MR, Khan MN, Islam MZ, et al. Determinants of adolescent childbearing in Bangladesh: a multilevel logistic regression analysis. J. Child Adolesc. Behav. 2018;6(2).
- Ali M, Alauddin S, Khatun MF, et al. Determinants of early age of mother at first birth in Bangladesh: a statistical analysis using a two-level multiple logistic regression model. J Publ Healt (Bangkok). 2021;29:1081–1087. doi:10.1007/s10389-020-01228-9
- Deligeoroglou E, Tsimaris P. Menstrual disturbances in puberty. Best Pract Res Clin Obstet Gynaecol. 2010;24(2):157–171. doi:10.1016/j.bpobgyn.2009.11.001
- McClendon KA, McDougal L, Ayyaluru S, et al. Intersections of girl child marriage and family planning beliefs and use: qualitative findings from Ethiopia and India. Cult Health Sex. 2018;20(7):799–814. doi:10.1080/13691058.2017.1383513
- Poudel S, Upadhaya N, Khatri RB, et al. Trends and factors associated with pregnancies among adolescent women in Nepal: pooled analysis of Nepal Demographic and Health Surveys (2006, 2011 and 2016). PloS One. 2018;13(8):e0202107. doi:10.1371/journal.pone.0202107
- Ali A, Khaliq A, Lokeesan L, et al. Prevalence and predictors of teenage pregnancy in Pakistan: a trend analysis from Pakistan Demographic and Health Survey datasets from 1990 to 2018. Int Health. 2022;14(2):176–182. doi:10.1093/inthealth/ihab025
- Islam MM, Islam MK, Hasan MS, et al. Adolescent motherhood in Bangladesh: trends and determinants. PloS One. 2017;12(11):e0188294.
- Pradhan R, Wynter K, Fisher J. Factors associated with pregnancy among married adolescents in Nepal: secondary analysis of the National Demographic and Health Surveys from 2001 to 2011. Int J Environ Res Public Health. 2018;15(2):229, doi:10.3390/ijerph15020229
- Agampodi TC, Wickramasinghe ND, Jayakodi HG, et al. The hidden burden of adolescent pregnancies in rural Sri Lanka; findings of the Rajarata Pregnancy Cohort. BMC Pregnancy Childbirth. 2021;21(1):1–10. doi:10.1186/s12884-021-03977-1
- Baumgartner, J. N., Geary, C. W., Tucker, H., et al. The influence of early sexual debut and sexual violence on adolescent pregnancy: a matched case-control study in Jamaica. In International perspectives on sexual and reproductive health;35(1): 21–28. https://doi.org/10.1363/ifpp.35.021.09
- Frost JJ, Lindberg LD, Finer LB. Young adults’ contraceptive knowledge, norms and attitudes: associations with risk of unintended pregnancy. Persp Sex Repr Heal. 2012;44(2):107–116. doi:10.1363/4410712
- Vundule C, Maforah F, Jewkes R, et al. Risk factors for teenage pregnancy among sexually active black adolescents in Cape Town. S Afr Med J. 2001;91(1):73–80.
- Epstein A, Bendavid E, Nash D, et al. Drought and intimate partner violence towards women in 19 countries in sub-Saharan Africa during 2011-2018: A population-based study. PLoS Med 2020;17(3):e1003064. doi:10.1371/journal.pmed.1003064
- Smith WC. Consequences of school closure on access to education: lessons from the 2013–2016 Ebola pandemic. Int Rev Educat. 2021;67(1-2):53–78. doi:10.1007/s11159-021-09900-2