ABSTRACT
Background
Orthodontic appliances act as plaque traps leading to the demineralization of teeth.
Aim
The purpose of the study was to compare Probiotics, NovaMin, and fluoride-containing dentifrices in terms of the incidence of white spot lesions in subjects undergoing treatment with fixed appliances using laser fluorescence.
Materials and Methods
In this prospective double-blinded randomized clinical trial, a total of 93 subjects were equally assigned to one of the three groups (Group A – Probiotic containing dentifrice, Group B – NovaMin containing dentifrice and group C – Fluoride containing dentifrice). Diagnodent scores were noted at T0 (just before bonding) and T1 (6 months into treatment). Statistical analyses were performed with Windows version 20.0 of IBM SPSS Statistics.
Results
Significant intergroup differences were noted in all teeth except for the lower right central incisor . Teeth with the highest incidence of WSLs were the lower right canine in group C (12.9%), and the least incidence of WSL was noted in the lower left lateral incisor (group B-0.92%). An overall higher incidence of WSLs was noted in group C (46.37%) as compared to group A (20.37%) and group B (43.05%). Males had a higher incidence of WSLs in all the three groups. The incidence of WSLs was highest in the age group of 26–35 years in all three groups.
Conclusion
WSL incidence was least in subjects on Probiotics-containing dentifrice. Adult males had a high incidence of WSLs. The lower right canine had the highest overall incidence of WSLs in all groups.
Introduction
Orthodontic appliances are associated with particular oral hygiene challenges since they act as plaque traps and make satisfactory mechanical oral hygiene difficult [Citation1]]. Demineralization is an inevitable side effect of fixed orthodontic treatment, especially when it is associated with poor oral hygiene [Citation2]. White spot lesions (WSLs) are defined as ‘subsurface enamel porosities resulting from carious demineralization of smooth enamel surfaces’. [Citation3] The time period for the formation of WSLs is 4 weeks, which falls within the time frame between subsequent orthodontic appointments, and its incidence in orthodontic patients is between 2% and 96% [Citation4,Citation5]. Various diagnostic methods to detect WSLs include visual inspection, tactile inspection, the radiographic method, fibre optic transillumination, electric conductance, and laser fluorescence [Citation6].
For the prevention of WSLs, proper oral hygiene maintenance with fluoridated dentifrices and preventive fluoride treatments are advised [Citation7]. Bioactive agents like NovaMin, which are incorporated in dental care products to remineralize teeth and help with hypersensitivity, gingivitis, and bleeding gums, have been introduced in recent years [Citation8]. NovaMin contains calcium sodium phosphosilicate, which is the active ingredient that allows adhesion to the tooth surface and initiates the remineralization of enamel upon contact with saliva or any aqueous medium [Citation9,Citation10]. Probiotics containing dentifrices, and lozenges have been reported to be effective against enamel demineralization [Citation11]. Probiotic supplements have been found to reduce the number of Streptococcus mutans in saliva and the plaques around the base of brackets [Citation12].
In vitro comparison of the effectiveness of Probiotic-containing toothpaste, Fluoride-containing toothpaste and NovaMin-containing toothpaste for reduction of WSLs around orthodontic brackets has been reported [Citation13]. Still, there is a paucity of comparative clinical trials on probiotic dentifrices. Therefore, the purpose of the current study was to compare probiotics, NovaMin containing dentifrices and fluoride dentifrices for the incidence of white spot lesions in subjects undergoing orthodontic treatment with fixed appliances.
Materials and methods
Study design and study setting
This prospective double-blinded randomized clinical trial was conducted on patients reporting to a university dental hospital. represents the demographic details of the subjects enrolled in the study.
Table 1. Demographic details of the study subjects.
Selection criteria for the trial
Subjects in the age range of 13–35 years, of both genders, with all teeth present, indicated, and willing to undergo fixed orthodontic treatment with 0.022” MBT metal brackets and an extraction or non-extraction protocol on conventional elastomeric ligation were included. Exclusion criteria were as follows: (i) subjects with extensive dental restorations, hypoplastic teeth, decayed, and periodontally compromised teeth; (ii) subjects who underwent orthognathic surgery; (iii) ligation with fluoride releasing modules; (iv) subjects who were on antimicrobial mouthwash during or up to 1 month prior to the start of trial (v) subjects with poor oral hygiene; and (vi) physically and mentally handicapped subjects who were unable to maintain oral hygiene.
Sample size calculation
Sample size calculation was done using G*Power software based on a previous trial by Hoffman et al. (2015) who evaluated the efficiency of NovaMin-containing dentifrice to prevent the occurrence of white spot lesions. With a power of 80%, an alpha error of 5% and an effect size of 0.51, a sample size of 93 subjects was obtained. This was divided equally into three groups, which were a followss: Group A (intervention): Probiotic dentifrice (OEM Probiotic Dentifrice, 100 g); Group B (intervention): NovaMin dentifrice (Sensodyne Dentifrice Powered by NovaMin, 100 g); and Group C (control): Fluoride dentifrice (Colgate Total Advanced Health Anticavity Dentifrice, 200 g).
Randomization of study subjects
Subjects were randomly allocated to the control or intervention group with the help of computer-generated sequence numbers using a research randomizer (https://www.randomizer.org/).
Allocation concealment
When a subject consented to participate in the study, the central trial coordinator, who was independent of the trial, allocated the subjects to the respective group using sealed envelopes. Prior to this, details of the subjects, including name and gender, were obtained. Informed consent in two languages (Tamil and English) was obtained from all the subjects for their participation in the study.
All the identifirices were covered with white tape to blind the operator and the subject. On the tape, the group designation was mentioned by the trial coordinator for distribution to subjects in the study groups. Similarly, the trial coordinator noted the date of dispensing the dentifrice, the weight of the dentifrice, and the occurrence of allergic reactions. Dentifrices were replenished for the study subjects as and when they reported for review appointments, and regular oral hygiene instructions were reinforced by the primary investigator (AT).
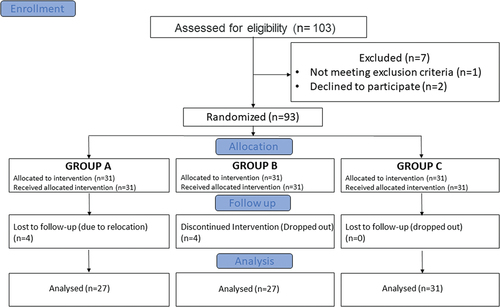
A total of 93 subjects fulfilled the selection criteria (see below) and agreed to participate. Thirty-one subjects were randomly allocated to each of the three groups, and with a dropout of eight subjects due to relocation and discontinued intervention, a total of 85 subjects were evaluated for enamel demineralization at T1. Diagnodent scores were noted at both T0 - (just before bonding) and T1 - (6 months into treatment). The identical bonding system was utilized in all three groups by the same operator, and all individuals received standard orthodontic bonding procedures, such as scaling and polishing, before the placement of brackets. At monthly intervals, instructions regarding brushing with the prescribed dentifrice twice a day were reinforced, and no other oral hygiene maintaining techniques were advised.
The demineralization of the sample teeth was measured using the technique as proposed by Stadt CB et al., in which the Diagnodent was calibrated until the result displayed on the screen matched the reference value at a 90° angle. This reference value is carved into the surface of the disc that is used to calibrate. Teeth were isolated with cotton rolls and dried in the open air for a short while. The conical tip (Tip A) of the DD-Pen (kavo, DD 2190-Pen) was placed midway along the bracket sides (gingival, incisal, mesial, and distal) and allowed to approach the enamel nearest to the bracket [Citation14]. For each of the four sides, the largest unit (with a maximum range of 0 to 99) was recorded. According to the manufacturer’s instructions, readings less than five indicate no lesions, and readings between 5 and 99 indicate lesions of increasing severity. The highest scores across all surfaces of 12, 14, 21, 23, 32, 34, 41, and 43 were identified in each subject. A mean score for each group was then determined. Any tooth surface with the highest score of more than 8 was considered to have a WSL () [Citation15]. The incidence of WSLs was higher in these selected teeth as reported by Gorelick et al.; therefore, these teeth were included.
Table 2. Diagnodent values and their interpretation [Citation16].
The principal investigator (AT) recorded the DD scores, and to verify the accuracy of the measures, the same author repeated the readings for five subjects in each group after a week.
Outcomes assessed
DD scores of various teeth across all groups were recorded during the process of bonding (T0) and 6 months into treatment (T1), and the following were reported:
Diagnodent scores at T1 in subjects using Probiotic-, NovaMin-, and Fluoride-containing dentifrices.
Comparison of the incidence percentage of WSLs in subjects using Probiotics, NovaMin, and Fluoride dentifrices.
Incidence percentage of WSLs in both genders and in different age groups.
Blinding
The primary investigator (AT) and the study participants involved in the study were blinded for the type of intervention given. A data analyst who was not a part of the study managed the data. Likewise, an independent statistician who was not involved in the study carried out the statistical analysis.
Statistical analysis
All statistical analyses were done using IBM SPSS Statistics software version 20.0 for Windows. Mean and standard deviation were calculated for the obtained data. The p-value was set at 0.05. Using a one-way ANOVA, the intergroup variation in the mean DD score was evaluated. Intraclass correlation coefficient analysis was done to analyse intraobserver reliability.
Results
The participant flow in the study is mentioned in the consort flow chart (). At T1, 35 females with a mean age of 19 ± 5.40 years and 50 male subjects with a mean age of 20.6 ± 4.11 years were involved in the study and a total of 680 teeth were studied. The intraclass correlation coefficient (ICC) for intra-rater reliability was calculated and found to be 0.824, indicating a high degree of correlation and agreement between measurements.
At T1, the total number of teeth evaluated in group A was 216 with an equal number of individual teeth. Similarly, group B also consisted of 216 teeth, with an equal number of individual teeth at T1. Group C consisted of 248 teeth with an equal distribution of individual teeth at T1 ().
represents the overall and individual percentage incidence of WSLs in different groups, genders, and age groups. An overall higher incidence of WSLs was noted in group C (46.37%) as compared to group B (43.05%) and group A (20.37%). The incidence of WSLs was higher in males than females in individual groups; that is, males in group A had a higher incidence of WSLs (35.8%) than females (23.87%). In group B, males had a higher incidence rate (32.33%) than females (14.77%), showing that males are more susceptible to developing WSLs. Additionally, males in group C appeared to have a higher incidence of WSLs (64.51%) than females (11.86%). The overall incidence of WSLs was higher in the age group of 26–35 years, followed by 19–25 years, and then 12–18 years in group C, whereas in group A and group B, it was higher in 26–35 years, followed by 12–18 years and least in 25 years.
Table 3. Overall and individual percentage incidence of WSLs in different genders and age groups at T1.
represents the incidence percentage of teeth with WSLs at T1 in individual groups based on DD scores. It indicates that the teeth with the highest incidence of WSLs were 43 in group C (12.9%), and the least incidence of WSLs was noted in 32 in group B (0.92%). represents the One-way ANOVA for the intergroup comparison of mean DD scores for individual teeth at T0 and T1. Significant intergroup differences in the mean DD scores at T1 were noted in all teeth evaluated except for 41 (p-value-0.10). Mean DD scores were higher in group C for 12, 14, 21, 34, and 43. Mean DD scores were least in group A for 14, 21, 34, and 43. The least DD scores in group B were recorded in 23 and 32.
Table 4. Percentage incidence of WSLs at T1 in individual teeth in different groups based on the mean DD scores.
Table 5. Intergroup differences in mean DD scores at T0 and T1 among different groups.
displays the post hoc analysis of intergroup differences in mean DD scores at T1 among different groups. Significant intergroup differences in the mean DD scores were observed between group A and group C for 12 and 43, with group C having higher mean DD scores for both 12 and 43. Significant intergroup differences in the mean DD scores were observed between groups A and B as well as between groups A and C, with higher mean DD scores in group C for 14, 21, 23, and 32. Significant intergroup differences in the mean DD scores were observed between groups A and C, as well as between groups B and C for 34, with group C having higher mean DD scores. However, for 41 there was no significant difference in the mean DD scores between the groups
Table 6. Intergroup differences in mean DD scores at T1 between two groups among different groups.
Discussion
Localized subsurface enamel demineralization, also known as white spot lesions, can occur around brackets as a result of orthodontic treatment, resulting in an unaesthetic appearance. There are numerous methods to diagnose these lesions, such as visual inspection and fluorescence methods; however, the Diagnodent pen is a simple and accurate method for detecting WSL [Citation17]. In the current study, an attempt was made to comparatively evaluate the effect of three different dentifrices (NovaMin, fluoride, and probiotic dentifrices) on the incidence of white spot lesions during orthodontic treatment using laser fluorescence (Diagnodent pen).
In the present study, several observations were noted. The overall incidence of WSLs was highest in group C – Fluoride-containing dentifrice (46.37%) followed by group B – NovaMin-containing dentifrice (43.05%) and least in group A- Probiotic-containing dentifrice (20.37%). On evaluating individual teeth, it was noted that the incidence of white spot lesions in the upper right lateral incisor was more in patients using fluoride dentifrice as compared to patients on Probiotic- and NovaMin-containing dentifrice.
In the upper right first premolar, enamel demineralization was higher in patients using Fluoride-containing dentifrice and least in patients on Probiotics-containing dentifrice. However, in the upper left central incisor, the incidence of WSL was highest in patients on Fluoride-containing dentifrice. Patients using a dentifrice-containing NovaMin had the lowest frequency of white spot lesions in the upper left central incisor and upper left canine. The incidence of WSL was highest in the lower left first premolar of patients using fluoride-containing dentifrice. In the lower right canine, patients on Fluoride-containing dentifrice had a higher incidence of WSLs. In the lower right central incisor, there was a higher incidence of WSL in patients on probiotics containing dentifrice.
Several authors’ studies indicated that lateral incisors and canines in the maxillary arch, followed by canines in the mandibular arch, had the highest incidence of WSLs [Citation18–20]. Similar findings were noted in the present study. In contrast to the above findings, Mizrahi et al. and Ogaard et al. reported that maxillary and mandibular first molars were commonly affected by WSLs [Citation5,Citation21]. A high incidence of WSLs in maxillary lateral incisors may be attributed to small tooth surface areas between the gingiva and bracket as well as the method of ligation which results in the retention of plaque and debris [Citation22,Citation23]. Different amounts of saliva exposure to the maxillary anterior teeth in contrast to other areas of the dentition or poor tooth brushing techniques, especially for a prolonged period of time, resulting in the ineffective cleaning of certain teeth can be attributed to the differences in WSL incidence [Citation24,Citation25].
Kau et al. conducted a similar study in which they examined the influence of Clinpro 5000 (5 mg Fluoride), Clinpro Tooth Creme (0.95 mg Fluoride), and MI-Paste plus (CPP-ACP) on the formation of WSLs over a period of 4 months and measured the enamel demineralization scores using photographs [Citation26]. Clinpro 5000 (5 mg Fluoride) was found to be more effective than MI paste and Clinpro Tooth Creme in preventing the formation of WSLs. In the present study, the intervention groups and assessment methods were different from those of Kau’s study. As compared to Kau’s work, the current investigation demonstrates that fluoride-containing dentifrices with a concentration of less than 1000 ppm F were insufficient to control WSLs.
Hoffman et al. studied the effect of NovaMin dentifrice (ReNew™) and fluoride-containing dentifrice (Crest®, 0.15% Fluoride) on the reduction of WSLs in 48 patients over a 6-month period by visual assessment of decalcification on pictures using the Gorelick Index. It was observed that there was no significant difference between the two dentifrices for the reduction of WSLs [Citation10]. In the present study, the fluoride-containing dentifrice had 1000 ppm fluoride, and enamel demineralization was assessed by laser fluorescence, as compared to Hoffman’s study. The difference in fluoride content would be a possible reason for the increase in the incidence of WSLs in the present study compared to Hoffman’s study.
Jose et al. evaluated the effect of probiotic curd and probiotic dentifrice on the count of Streptococcus mutans in plaque around orthodontic brackets using real-time polymerase chain reaction and reported that probiotic curd and probiotic dentifrice were effective in the reduction of S mutans count [Citation12]. According to the findings of the present study, probiotic dentifrice is helpful in reducing the incidence of WSLs, which may be due to the reduction of S mutans in plaque around orthodontic brackets, as demonstrated by the previous study.
In an in vitro study by Gocke et al., WSL incidence was evaluated by quantitative light-induced fluorescence in 45 freshly extracted mandibular molars treated with fluoride, NovaMin, and probiotic dentifrices. It was determined that NovaMin dentifrice was as effective as fluoride dentifrice in reducing WSL, with probiotic dentifrice exhibiting the least reduction [Citation13]. Gocke’s study was a QLF (Quantitative light-induced fluorescence) based in vitro study, and they reported the least reduction of WSLs with probiotics. QLF measures the percentage of fluorescence change of demineralized enamel with respect to surrounding sound enamel. The findings reported by Gocke et al. are not in line with the present study as in vitro studies cannot simulate the clinical scenarios. Evidence suggests that one of the disadvantages of an in vitro study is that it fails to replicate the conditions and environment of cells in an organism, thereby limiting the value of in vitro data to anticipate in vivo behaviour [Citation27]. Hibst et al. conducted a study on the detection of smooth surface caries by laser fluorescence and reported that the DIAGNOdent™ system was significantly more sensitive than conventional methods [Citation28]. Baeshen et al. evaluated the impact of fluoridated miswaks on the incidence of WSLs using a Diagnodent pen. It was concluded that the diagnodent pen was a useful tool for diagnosing and monitoring changes in WSLs over a relatively short period of time [Citation29].
Aljehani et al. evaluated the use of a Diagnodent pen and QLF for the quantification of white spot lesions adjacent to orthodontic brackets in vitro. It was concluded that although QLF was better at diagnosing incipient enamel lesions for deeper lesions, the Diagnodent pen was able to quantify the lesion. Also, it was an easier technique to be used in a clinical setup [Citation30].
Julien et al. and Akin et al. evaluated the incidence of white spot lesion formation during orthodontic treatment among genders using photographs and reported no significant differences, which are not in consensus with the results of the present study [Citation30,Citation31]. Tufecki et al. observed that 76% of male subjects and 24% of females had at least one WSL. Similarly, Boersma et al. reported an incidence of 40% in males and 22% in female patients, indicating that males have a greater chance of developing WSL. These findings are similar to those of the present study [Citation32,Citation33]. However, findings by Eltayeb et al. who evaluated the distribution of white spot lesions among orthodontic patients in different age groups through photographic assessment concluded that the development of WSL was higher in females (46.6%) and lesser in males (14.8%) [Citation18].
Limitations of the current study were that the evaluation of WSLs was only done over a period of 6 months. Plaque scores were not evaluated in the current study and may correlate with the incidence of WSLs. Also, the patient’s compliance with dentifrice use both in terms of frequency and quantity could not be monitored. Few patients dropped out of this study due to relocation and white spot lesions could not be evaluated.
Conclusion
WSL incidence was least in subjects on Probiotics-containing dentifrice. Adult males indicated a high incidence of WSLs. The lower right canine had the highest overall incidence of WSLs in all groups.
Authors’ contribution
Author A contributed to the conception, design, data acquisition, and interpretation, and performed all statistical analyses. Author B contributed to the conception, design, and data acquisition, and drafted and critically revised the manuscript
Ethical approval
The present randomized controlled trial was approved by the Institutional Scientific Review Board of Saveetha University (SRB/SDMDS11/18/ORT/01).
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Heintze SD. Oral health for the orthodontic patient. Quintessence Publishing Company; 1999. p. 67–70.
- Zachrisson BU, Brobakken BO. Clinical comparison of direct versus indirect bonding with different bracket types and adhesives. Am J Orthod. 1978;74:62–78.
- Summitt JB. Fundamentals of operative dentistry: a contemporary approach. 3. Quintessence Publishing Company; 2006. 978-0-86715-528-0; 9780867155280.
- O’reilly MM, Featherstone JDB. Demineralization and remineralization around orthodontic appliances: an in vivo study. Am J Orthod Dentofacial Orthop. 1987;92:33–40. Available from. DOI:http://dx.doi.org/10.1016/0889-5406(87)90293-9.
- Mizrahi E. Enamel demineralization following orthodontic treatment. Am J Orthod. 1982;82:62–67.
- Mitchell L. Decalcification during orthodontic treatment with fixed appliances—an overview. Br J Orthod. 1992;19:199–205. Available from. DOI:10.1179/bjo.19.3.199.
- Bishara SE, Ostby AW. White spot lesions: formation, prevention, and treatment. Semin Orthod. 2008;14:174–182.
- Miglani S, Aggarwal V, Ahuja B. Dentin hypersensitivity: recent trends in management. J Conserv Dent. 2010;13:218–224.
- Vahid Golpayegani M, Sohrabi A, Biria M, et al. Remineralization effect of topical novamin versus sodium fluoride (1.1%) on caries-like lesions in permanent teeth. J Dent. 2012;9:68–75.
- Hoffman DA, Clark AE, Wj R Jr, et al. A prospective randomized clinical trial into the capacity of a toothpaste containing NovaMin to prevent white spot lesions and gingivitis during orthodontic treatment. Prog Orthod. 2015;16:25.
- Wang Y, Dong J, Wang J, et al. Assessing the drug resistance profiles of oral probiotic lozenges. J Oral Microbiol. 2022;14:2019992.
- Jose JE, Padmanabhan S, Chitharanjan AB. Systemic consumption of probiotic curd and use of probiotic toothpaste to reduce streptococcus mutans in plaque around orthodontic brackets [Internet]. Am J Orthod Dentofacial Orthop. 2013;144:67–72. Available from. DOI:10.1016/j.ajodo.2013.02.023.
- Gokce G, Savas S, Kucukyilmaz E, et al. Effects of toothpastes on white spot lesions around orthodontic brackets using quantitative light-induced fluorescence (QLF): an in vitro study. J Orofac Orthop. 2017;78:480–486.
- Staudt CB, Lussi A, Jacquet J, et al. White spot lesions around brackets: in vitro detection by laser fluorescence. Eur J Oral Sci. 2004;112:237–243.
- Sardana D, Li KY, Ekambaram M, et al. Validation of clinical photography and a laser fluorescence device for assessment of enamel demineralization during multi-bracketed fixed orthodontic treatment [Internet]. Photodiagnosis Photodyn Ther. 2022; 38: 102828. DOI: 10.1016/j.pdpdt.2022.102828.
- DIAGNOdentTM pen [Internet]. 2017 [cited 2021 Dec 21]. Available from: https://www.kavo.com/en-in/dental-xray/diagnodent-pen-diagnostic-devices.
- Aljehani A, Tranaeus S, Forsberg C-M, et al. In vitro quantification of white spot enamel lesions adjacent to fixed orthodontic appliances using quantitative light-induced fluorescence and DIAGNOdent. Acta Odontol Scand. 2004;62:313–318.
- Eltayeb MK, Ibrahim YE, El Karim IA, et al. Distribution of white spot lesions among orthodontic patients attending teaching institutes in Khartoum. BMC Oral Health. 2017;17:88.
- Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81:93–98.
- Geiger AM, Gorelick L, John Gwinnett A, et al. The effect of a fluoride program on white spot formation during orthodontic treatment [Internet]. Am J Orthod Dentofacial Orthop. 1988;117: 29–37. DOI: 10.1016/0889-5406(88)90190-4.
- Øgaard B White spot lesions during orthodontic treatment: mechanisms and fluoride preventive aspects [Internet]. Semin Orthod. 2008; 12 : 183–193. DOI: 10.1053/j.sodo.2008.03.003.
- Sundararaj D, Venkatachalapathy S, Tandon A, et al. Critical evaluation of incidence and prevalence of white spot lesions during fixed orthodontic appliance treatment: a meta-analysis. J Int Soc Prev Community Dent. 2015;5:433–439.
- Tiwari A, Jain RK Comparison of enamel demineralisation scores between passive self-ligation brackets and conventional ligation brackets in patients undergoing orthodontic treatment – a laser fluorescence study [Internet]. J Clin Diagnostic Res. 2020; 14 DOI: 10.7860/jcdr/2020/45724.14252.
- Khalaf K. Factors affecting the formation, severity and location of white spot lesions during orthodontic treatment with fixed appliances. J Oral Maxillofac Res. 2014;5:e4.
- Jain RK, Verma P Visual assessment of extent of white spot lesions in subjects treated with fixed orthodontic appliances: a retrospective study [Internet]. World J Dent. 2022; 7: 245–249. DOI: 10.5005/jp-journals-10015-2042.
- Kau CH, Wang J, Palombini A, et al. Effect of fluoride dentifrices on white spot lesions during orthodontic treatment: a randomized trial [Internet]. The Angle Orthod. 2019; 89: 365–371. DOI: 10.2319/051818-371.1.
- Graudejus O, Wong RP, Varghese N, et al. Bridging the gap between in vivo and in vitro research: reproducing in vitro the mechanical and electrical environment of cells in vivo [Internet]. Front Cell Neurosci. 2018. DOI: 10.3389/conf.fncel.2018.38.00069.
- Hibst R, Paulus R, Lussi A. Detection of occlusal caries by laser fluorescence: basic and clinical investigations [Internet]. J Laser Appl. 2001;16:205–213. Available from. DOI:10.1078/1615-1615-00024.
- Baeshen HA, Lingström P, Birkhed D. Effect of fluoridated chewing sticks (miswaks) on white spot lesions in postorthodontic patients. Am J Orthod Dentofacial Orthop. 2011;140:291–297.
- Akin M, Tazcan M, Ileri Z, et al. Incidence of white spot lesion during fixed orthodontic treatment [Internet]. Turk J Orthod. 2013;29: 98–102. DOI: 10.13076/j.tjo.2013.26.02_98.
- Julien KC, Buschang PH, Campbell PM Prevalence of white spot lesion formation during orthodontic treatment [Internet]. The Angle Orthod. 2013; 83: 641–647. DOi: 10.2319/071712-584.1.
- Tufekci E, Dixon JS, Gunsolley JC, et al. Prevalence of white spot lesions during orthodontic treatment with fixed appliances [Internet]. The Angle Orthodontist. 2011;81:206–210. Available from: 10.2319/051710-262.1.
- Boersma JG, van der Veen MH, Lagerweij MD, et al. Caries prevalence measured with QLF after treatment with fixed orthodontic appliances: influencing factors [Internet]. Caries Research. 2005;39(1):41–47. DOI:10.1159/000081655