Abstract
Objective
To describe and appraise the latest simulation models for direct and indirect ophthalmoscopy as a learning tool in the medical field.
Methods
The present review was conducted using four national and international databases – PubMed, Scielo, Medline and Cochrane. Initial set of articles was screened based on title and abstracts, followed by full text analysis. It comprises of articles that were published in the past fifteen years (2002–2017).
Results
Eighty-three articles concerning simulation models for medical education were found in national and international databases, with only a few describing important aspects of ophthalmoscopy training and current application of simulation in medical education. After secondary analysis, 38 articles were included.
Conclusion
Different ophthalmoscopy simulation models have been described, but only very few studies appraise the effectiveness of each individual model. Comparison studies are still required to determine best approaches for medical education and skill enhancement through simulation models, applied to both medical students as well as young ophthalmologists in training.
Introduction
The ophthalmoscopy exam is an important medical skill that allows ophthalmologists, neurologists and emergency room physicians to diagnose many sight and life-threatening conditions, although its skills have never been fully mastered by the medical community,Citation1,Citation2 mainly due to lack of physician’s confidence,Citation3,Citation4 interestCitation5 or regular practice.Citation6,Citation7 This leads to loss of a major diagnostic assistance that relies in a “small, portable and simple to comprehend” tool.Citation8
Practical skills begin with regular training, thus, simulation models have been implemented in a range of procedures in the medical field. Simulation creates opportunitiesCitation9,Citation10 and allows repetitive practice without affecting patient’s care.Citation11 Several models have been adapted to ophthalmoscopy, like computer simulation,Citation12 mannequins,Citation13 photographs and, most recently, virtual reality.Citation14,Citation15
The purpose of this article is to describe the most common devices used in simulation ophthalmoscopy training and to review the latest results of articles that evaluate each model individually.
Methods
A retrospective, descriptive review of current simulation models applied to ophthalmoscopy examination was conducted, based on the past fifteen years of research (2002–2017). Four national and international databases were consulted (PubMed, Scielo, Medline and Cochrane). An initial screen yielded a total of eighty-three articles, each meeting at least one of the following criteria:
ophthalmoscopy models in ophthalmology training,
simulation models in medical education and
experimental research using simulation models in ophthalmology.
Results and discussion
Teaching ophthalmoscopy may vary from rudimentary techniques to high-technology programs. Although certain difficulty in skill assessment has always been associated, no effective model to evaluate physician’s or students’ angle of view has been developed. Here, we describe two techniques – direct and indirect – with a mention on famous equipment and latest evaluating reports.
Direct ophthalmoscopy
Models and devices
The oldest approach of teaching ophthalmoscopy relies on a simple image-quiz model, where examiners learn normal parameters through real retinal images, and try to apply this on real patients, completing standardized questionnaires. Although limited, this approach is simple and non-expensive in ophthalmology training.
In 2004, Chung and WatzkeCitation16 described a simple model for direct exam with a handheld ophthalmoscope. It consists of a plastic closed chamber, where a 37-mm photograph of a normal retina is internally allocated, so that a physician can assess it through an 8-mm hole, which is supposed to simulate a mydriatic pupil. Common problems with this device include low photograph quality, intense light reflection and loss of space perception by examiners.
At the end of 2007, Pao et alCitation17 presented a new model called THELMA (The Human Eye Learning Model Assistant), which consists of a Styrofoam mannequin head that uses retinal images in a similar fashion as the aforementioned device. Advantages of this model include better physician–patient relationship simulation and sense of adequate position, although intense light reflection was still a problem, especially due to paper quality of printed photographs.
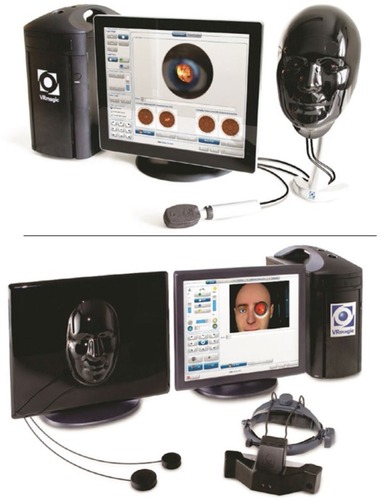
Later on, newer models have been created. The EYE Exam Simulator (developed by Kyoto Kagaku Co., Kyoto, Japan) and Eye Retinopathy Trainer® (developed by Adam, Rouilly Co., Sittingbourne, UK) are real-size mannequin heads, with an adjustable pupil that allows access to a wider, 35 mm designed, high-quality retina, through a handheld ophthalmoscope (). Due to higher complexity, young examiners may experience technical problems if there are no experienced staffs to aid initial simulation training.Citation18
In 2014, SchulzCitation19 presented a semi-reflective device where the reflected light beam from the retina splits into different pathways, where one beam of light is redirected to a video camera and projected into a laptop computer, allowing assessment by an outsider. This was developed in an attempt to create a device where instructors were able to appreciate the same field of view as the examiner’s, improving skill evaluation. Problems with this model include loss of synchrony between image projection and actual examination.
Borgersen et alCitation20 described the possible use of YouTube video lessons along with traditional theoretical lessons, since different instructional videos have been widely used in the past to aid in the guidance of general physical examination and basic medical skills. Problems with this method included lack of sufficient video lessons, low-quality videos and absence of long-term comparison studies.
Virtual reality seems to be the latest tendency nowadays for skill training. The most recent, designed by the company VRmagic, is the EYEsi Direct Ophthalmoscope Simulator,Citation18,Citation21 and it is considered to be a highly complex and humanized equipment. It consists of a touch screen device connected to an artificial human face model, where the examiner can perform an exam using the device’s own simulated handheld ophthalmoscope. This device presents unique advantages, like mapping visualized retinal regions, ability to control physiologic and pathologic functions and variants, and immediate feedback with detailed explanations. Problems with this device include expensive cost and the need of a trained staff.Citation11 Currently, there are no comparative studies regarding this model.
Studies in the literature
depicts the latest reports on models and devices described earlier.
Table 1 Direct ophthalmoscopy
Eleven studies including the first- to fourth-year medical students were reviewed. Results showed the following: 1) improved confidence by examiner, 2) improved interest in ophthalmoscopy, 3) skill enhancement and 4) better identification of anatomic structures. One study reported no self-confidence or skill improvement, although no evaluation test was applied.Citation24 Furthermore, simulation quality must be adapted to each person, since the excess of realism and complexity can confuse examiners when learning basic skills, especially medical students.Citation25
Indirect ophthalmoscopy
Models and devices
In 2006, LewallenCitation33 presented a simple model for indirect ophthalmoscopy training. It consists of a round glass sphere allocated in a Styrofoam surface. Inside, package inserts from prescription medications are inserted and positioned according to the internal diameter of the sphere. The examiner’s goal is to read the reflected words, in order to understand basic principles of indirect ophthalmoscopy exam. This is one of the simplest methods of training, although no comparative studies have been conducted with this model.
In 2009, LantzCitation34 adapted the device created by Chung and Watzke to an indirect approach. Here, the artificial pupil was designed to measure 9 mm and it was originally developed to train pathologists for autopsies. With a light-attached helmet, the purpose of this model was to estimate postmortem period, although there is no reason this could not be adapted to general ophthalmoscopy training.
Similar to the direct simulator, VRmagic also developed the EYEsi Indirect Ophthalmoscope Simulator,Citation18,Citation35 which presents the same features described earlier. Further, it also displays functions on light and lens position, although cases and images are not different from those included in the direct simulator. Both devices are presented in .
Studies in the literature
depicts the latest reports on models and devices described earlier.
Table 2 Indirect ophthalmoscopy
Only two articles describing indirect ophthalmoscopy training were considered. Both studies employed the same simulator and showed higher performance in the group that used the device (p<003; p<0.0001).
Conclusion
Simulation is a helpful tool in ophthalmoscopy training, once it can provide better understanding of skill management. Constant training is a well-known strategy for skill enhancement, although it may initially induce physicians and students to forget protocols developed to guarantee comfort and patient’s safety.
Although recent models are promising, there is still lack of studies to verify their actual efficiency and to compare recent models to traditional and rudimentary techniques. However, preliminary results presented in this review seem to be satisfactory. Further comparison studies are required for better characterization of newer simulation models.
Disclosure
The authors report no conflict of interest in this work.
References
- WuEHFaganMJReinertSEDiazJASelf-confidence in and perceived utility of the physical examination: a comparison of medical students, residents, and faculty internistsJ Gen Intern Med200722121725173017922165
- HolmboeESFaculty and the observation of trainees’ clinical skills: problems and opportunitiesAcad Med2004791162214690992
- GuptaRRLamWCMedical students’ self-confidence in performing direct ophthalmoscopy in clinical trainingCan J Ophthalmol20064121697416767203
- ShuttleworthGNMarshGWHow effective is undergraduate and postgraduate teaching in ophthalmology?Eye (Lond)199711Pt 57447509474330
- Lopes FilhoJBLeiteRALeiteDAde CastroARAndradeLSAvaliação dos conhecimentos oftalmológicos básicos em estudantes de Medicina da Universidade Federal do PiauíRev Bras Oftalmol20117012731 Portuguese
- MoradYBarkanaYAvniIKozerEFundus anomalies: what the pediatrician’s eye can’t seeInt J Qual Health Care200416536336515375096
- LippaLMOphthalmology in the medical school curriculum: reestablishing our value and effecting changeOphthalmology200911671235123619576494
- SitMLevinAVDirect ophthalmoscopy in pediatric emergency carePediatr Emerg Care200117319920411437148
- WellerJMNestelDMarshallSDBrooksPMConnJJSimulation in clinical teaching and learningMed J Aust2012196959422621154
- BenbassatJPolakBCJavittJCObjectives of teaching direct ophthalmoscopy to medical studentsActa Ophthalmol201290650350722040169
- GrodinMHJohnsonTMAcreeJLGlaserBMOphthalmic surgical training: a curriculum to enhance surgical simulationRetina200828101509151418695630
- LabuschagneMJThe role of simulation training in ophthalmologyCont Med Educ2013314157159
- XiePHuZZhangXApplication of 3-dimensional printing technology to construct an eye model for fundus viewing studyPLoS One2014911e10937325393277
- SikderSTuwairqiKAl-KahtaniEMyersWGBanerjeePSurgical simulators in cataract surgery trainingBr J Ophthalmol201498215415824158838
- TingDSWSimSSKPYauCWLRosmanMAwATYeoIYSOphthalmology simulation for undergraduate and postgraduate clinical educationInt J Ophthalmol2016189692092427366698
- ChungKDWatzkeRCA simple device for teaching direct ophthalmoscopy to primary care practitionersAm J Ophthalmol2004138350150215364247
- PaoKYUhlerTAJaegerEACreating THELMA – The Human Eye Learning Model AssistantJ Acad Ophthalmol200812529
- RicciLHFerrazCASimulation models applied to practical learning and skill enhancement in direct and indirect ophthalmoscopy: a reviewArq Bras Oftalmol201477533433825494384
- SchulzCA novel device for teaching fundoscopyMed Educ201448552452524712941
- BorgersenNJHenriksenMJKongeLSørensenTLThomsenASSubhiYDirect ophthalmoscopy on YouTube: analysis of instructional YouTube videos’ content and approach to visualizationClin Ophthalmol2016101535154127574393
- VRmagic CoDirect Ophthalmoscope Simulator Available from: http://www.vrmagic.com/fileadmin/downloads/simulator_brochures/Eyesi_Direct_Brochure_131029_EN_WEB_DP.pdfAccessed April 20, 2016
- HoegTBShethBPBraggDSKivlinJDEvaluation of a tool to teach medical students direct ophthalmoscopyWMJ20091081242619326631
- SwansonSKuTChouCAssessment of direct ophthalmoscopy teaching using plastic canistersMed Educ2011455520521
- McCarthyDMLeonardHRVozenilekJAA new tool for testing and training ophthalmoscopic skillsJ Grad Med Educ201241929623451315
- LarsenPStoddartHGriessMOphthalmoscopy using an eye simulator modelClin Teach20141129910324629245
- KellyLPGarzaPSBruceBBGraubartEBNewmanNJBiousseVTeaching ophthalmoscopy to medical students (the TOTeMS study)Am J Ophthalmol201315651056106124041982
- AndrowikiJEScravoniIARicciLHFagundesDJFerrazCAEvaluation of a simulation tool in ophthalmology: application in teaching fundoscopyArq Bras Oftalmol2015781363925714536
- SchulzCMooreJHassanDTamsettESmithCFAddressing the ‘forgotten art of fundoscopy’: evaluation of a novel teaching ophthalmoscopeEye (Lond)201630337538426563657
- ChenMSwinneyCChenMBalMNakatsukaAComparing the utility of the non-mydriatic fundus camera to the direct ophthalmoscope for medical educationHawaii J Med Public Health2015743939525821651
- MilaniBYMajdiMGreenWThe use of peer optic nerve photographs for teaching direct ophthalmoscopyOphthalmology2013120476176523246117
- GilmourGMcKiviganJEvaluating medical students’ proficiency with a handheld ophthalmoscope: a pilot studyAdv Med Educ Pract20168333628096708
- ByrdJMLongmireMRSymeNPMurray-KrezanCRoseLA pilot study on providing ophthalmic training to medical students while initiating a sustainable eye care effort for the underservedJAMA Ophthalmol2014132330430924384560
- LewallenSA simple model for teaching indirect ophthalmoscopyBr J Ophthalmol2006901013281329
- LantzPEA simple model for teaching postmortem monocular indirect ophthalmoscopyJ Forensic Sci200954367667719432744
- VRmagic CoIndirect Ophthalmoscope Simulator Available from: https://www.vrmagic.com/fileadmin/downloads/simulator_brochures/Eyesi_Indirect_Brosch%C3%BCre_160510_EN_WEB.pdfAccessed April 21, 2016
- LeitritzMAZiemssenFSuesskindDCritical evaluation of the usability of augmented reality ophthalmoscopy for the training of inexperienced examinersRetina201434478579124670999
- ChouJKosowskyTPayalARGonzalez GonzalezLADalyMKConstruct and face validity of the Eyesi indirect ophthalmoscope simulatorRetina Epub20161229