Abstract
Massive open online courses (MOOCs) are increasingly available in the area of health and medicine. These MOOCs are offered through various commercial and noncommercial online platforms. When offered through reputable institutions, they can provide valuable access to reliable information without the constraints of time, geographical location, or level of education. Most current courses appear introductory in nature. In its drive for quality health care, the National Academy of Medicine has prioritized a focus on known chronic care conditions. Many of these conditions are shared internationally. Among its initiatives, the academy encourages consumer and professional groups, patients, clinicians, health care organizations, and universities to work together to identify evidence-based care processes consistent with best practices, organize major prevention programs to target key associated health risk behaviors, and develop systems to measure and evaluate improvements in the provision of patient- and family-centered health care. Carefully designed and collaboratively developed MOOCs would appear a valuable resource to contribute to these initiatives. Such MOOCs can, 1) increase the health literacy of the public with regard to the prevention and treatment of known chronic care conditions, 2) provide ready access to continuing professional, and interprofessional, education, and 3) explore innovative teaching models for student learning focused on patient- and family-centered care. MOOCs would also appear helpful to facilitate effective communication among international communities of patients and clinicians, including student clinicians, with shared interests. Further, the accumulation of MOOC data through large-scale measurement and analysis, obtained nationally and internationally, has the potential to assist in greater understanding of the risk for diseases and their prevention, with this translating into medical education, and authentic, patient- and family-centered methods for student learning. This paper explores these issues.
Introduction
The purpose of this narrative review is to stimulate discussion about the role of massive open online courses (MOOCs) as innovative tools in medical education and practice to ensure effective, quality, equitable, and patient- and family-centered health care. Published papers on medically-related MOOCs were identified from searches on PubMed, Google Scholar, CINAHL, and Cochrane databases. MOOCs in general have proliferated since 2012, based on the innovative work of SiemensCitation1 and DownesCitation2 who showed that a large number of participants (frequently thousands = massive) could access, network, and share information rapidly through an authentic, meaningful, and free (open) online learning environment (course). Before delving into how MOOCs may play a role in medical education and practice for health care professionals, academics, policy developers, and people in need of medical care, it is important to understand what is needed for quality health care.
Achieving quality health care
In 2001, the Institute of Medicine (IOM; now the National Academy of Medicine) in the United States published a pivotal paper, Crossing the quality chasm, focusing attention on six essential aims of health care: services provided must be safe, effective, patient-centered, timely, efficient, and equitable.Citation3 To achieve these aims and address evident gaps in health care, the IOM advocated redesigned systems to improve the quality of medical care, and thus medical education. Principles guiding system redesign focused on care that was: 1) evidence-based to translate scientific knowledge into practice, 2) able to address individual needs of patients and families, 3) transparent to enable patients and their families to make informed choices, 4) proactive rather than reactive, and 5) characterized by collaborative, interdisciplinary, integrated work, and effective communication.Citation3
The importance of ongoing communication between all health care providers and the people in need of care resulted in renewed recognition of the value of interprofessional education (IPE) for medical, paramedical, nursing, pharmacy, dental, allied and public health, and social work students in preparation for effective interprofessional practice (IPP).Citation4 Although the nuance may be subtle, the term “interprofessional” is preferred to “interdisciplinary” due to its focus on collaborative relationships that address both education and practice as preprofessional students learn with, from, and about each other.Citation5 This learning occurs through scaf-folded opportunities that expose students to IPE, engage them in integrated work, and develop their competence for IPP.Citation5–Citation7 Data show that IPE experiences increase students’ confidence and readiness for effective teamwork and shared decision-making in professional practice.Citation8 Results from eight randomized controlled trials have documented positive outcomes in varying aspects of health care, including increased practitioner competencies and patient satisfaction.Citation4
While much has been achieved to improve the quality and safety of health care since the publication of the IOM’s 2001 report, there is still work to be performed. A systematic analysis of evidence from 18 international studies, based on the IOM’s six aims, documented that care redesign has not been so systematic; more robust research designs need to be implemented, and care design focused on patient- and family-centered care needs to be strengthened.Citation9,Citation10 In a recent report developed for the National Academy of Medicine, Frampton et alCitation11 expressed concern at the ongoing difficulty in changing the culture of medical education and practice to focus on patient- and family-centered care, communication, and empathy – core competencies in modern health care.Citation12 These investigators argued that the comprehensive framework needed to ensure safe, effective, patient-centered, timely, efficient, and equitable health care must include the lived experiences of the people who are ill, or at-risk, and those who care for them. This focus on patient (or person-) centeredness will facilitate patients’ active engagement in their care, identify meaningful and functional outcomes that are not solely practitioner driven, and facilitate the development of a patient- and family-centered evidence base that is integral to effective, quality care.Citation8,Citation11–Citation14 Contrasting this approach to evidence-based care focused on more controlled experimental designs, some have termed it “practice-based evidence.”Citation15 Both approaches are important in maintaining and evaluating quality health care. To develop and establish a culture of patient-centered care, Frampton et alCitation11 stressed the need for innovative and inclusive training for patients, their families, and health care personnel. While there are valuable case-based reports of the effectiveness of patient-centered care, Singer et alCitation16 advocated continued work based on the theory of collective learning – how learning from leadership and effective communication among groups and organizations can establish a person-centered framework to promote the quality and safety of health care beyond individual or local levels.
Prioritizing chronic care conditions in facilitating quality health care
In its drive for quality health care, the National Academy of Medicine has prioritized a focus on known chronic care conditions to make the best use of available resources. The academy encourages health care organizations, consumer and professional groups, patients, clinicians, private and public payment providers, and other stakeholders to work together to: 1) identify evidence-based care processes consistent with best practices, 2) organize major prevention programs to target key associated health risk behaviors, 3) develop and provide a supportive outcomes-based information infrastructure, 4) align reimbursement policies with the goal of quality improvement, and 5) develop systems to measure and evaluate improvements in the provision of health care.Citation3
Currently in Australia, the top five causes of death are: heart disease, dementia, cerebrovascular disease (stroke), lung cancer, and chronic respiratory disease.Citation17 In America, the top five causes of death are heart disease, malignant cancers (particularly lung cancer), chronic respiratory disease, accidents (unintentional injuries), and cerebrovascular disease; dementia is sixth.Citation18 Dementia, a progressive and terminal condition, is now accepted as one of the major causes of disability and dependency among older people and a global public health issue.Citation19 There is particular concern about the increasing number of people with dementia and associated medical conditions in developing countries.Citation20 Heart disease, stroke, chronic obstructive respiratory disease, lung cancer (and related cancers of the airway), diabetes, and obesity also remain global concerns.Citation21
The characteristics and contributions of MOOCs
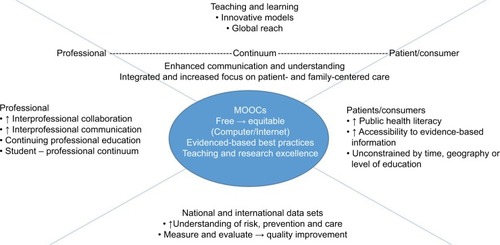
The IOM recognized the inherent potential of the Internet to transform health care, particularly in addressing known chronic care conditions, and information is now widely available to consumers, students, and health care providers through an increasing number of health- and medicine-related MOOCs. These MOOCs are offered through various commercial and noncommercial online platforms and, when offered through reputable institutions, can provide valuable access to reliable information. shows the potential contributions of health- and medicine-related MOOCs to both professional and consumer-based audiences, and these potential contributions are explored in the following section.
Figure 1 Potential contributions of health- and medicine-related MOOCs.
In a recent systematic review of health- and medicine-related MOOCs, Liyanagunawardena and WilliamsCitation22 identified 225 courses, of which 113 were listed on the MOOC aggregator site “Class Central.” They examined 98 of these MOOCs that fit the following criteria: no cost, specified start and end dates, and not related to psychology, biology, life sciences, or animal health and disease unrelated to human health. The majority of the selected MOOCs were offered in English, predominantly by universities in North America. The courses ranged in length from 3 to 20 weeks. Completion of some MOOCs provided participants with continuing professional education (medical, nursing, or dental) credit but most courses appeared introductory, as judged from their “Introduction to…” titles. A search of the Class Central site in March 2017 showed that the number of listed health- and medicine-related MOOCs had increased from 113 in 2014 to 511.
As long as one has access to a computer and the Internet, MOOCs can provide access to information compiled and presented by experts without the constraints of time, geography, or level of education.Citation23 The ability to read and write in English may be a constraint. Although some detractors fear that MOOCs may undermine current higher education models, the more common view for health and medicine is that MOOCs offered by universities appear a valuable way to address three important issues: 1) increase the health literacy of the public – and older adults can indeed benefit,Citation24,Citation25 2) provide continuing professional, and interprofessional, education for practitioners – serving as a ready resource for evidence-based care, as scientific evidence and expert consensus about best practices often take a long time to reach clinicians and patients, and 3) explore innovative teaching models for student learning, including the promotion of effective interprofessional teams, and problem-based quality improvement learning that enhances in-person traditional learning, facilitates leadership, and removes barriers frequently experienced by international students.Citation22,Citation25–Citation33 These three complementary and important components of effective medical education and practice can assist in redesigning systems of care and translating knowledge into effective care and prevention. These three components also can facilitate organizational support, efficiency modeling processes, and transparent reimbursement systems to promote effective, outcome-based care, taking advantage of collective learning and focusing on patient and family needs.
MOOCs would also appear helpful to facilitate effective communication among international communities of patients and clinicians, including student clinicians, with shared interests, strengthening the cooperative relationships essential to effective online learning.Citation34,Citation35 Further, the accumulation of MOOC data through large-scale measurement and analysis, “big data”Citation36 obtained nationally and internationally, has the potential to assist in greater understanding of the risk for diseases and their prevention, as well as increased efficiency in systematic care,Citation37 with this translating into medical and IPE, authentic, patient-centered assessment methods for student learning, and wider access for student recruitment. As universities strive to develop innovative strategies to maintain teaching and research excellence in medical education and practice in an increasingly competitive environment, participating in collaboratively developed MOOCs may prove valuable to facilitate students’ understanding of the importance of patient perspectives to drive patient-centered quality careCitation38,Citation39 ().
Table 1 Contributions of MOOCs to national and international issues in medical education and practice
MOOCs can be costly to produce, in terms of the required infrastructure and technology, including meaningful assessment methods, invited expertise, the time needed for staff to respond to participants’ discussion board posts to maintain a personal connection online, and tangible staff incentives.Citation27,Citation40 Future MOOC offerings may include a user fee, parallel to a workshop fee for face-to-face learning, or a fee for providing a certificate of completion. Some universities may feel a need to cap the number of participants, particularly if the MOOC is specific to student skill or competency development. However, collaborative work in leadership across consumer-based organizations, medical professions, universities, policy developers, and funding agencies may mitigate these challenges.
How best to measure learning through MOOCs?
In reporting data to document the success of MOOCs, investigators have focused on the types of engagement activities used to encourage social interaction and problem-solving, number of participants who engaged, the length of time spent on particular activities, and the number of participants who completed the course, with subsequent surveys and interviews of participants used as available.Citation23,Citation41–Citation43 ReichCitation44 argued that many of these measures show what participants do, but not necessarily what they learn. He stressed that ongoing MOOC design and policy development need to focus on three characteristics to document learning: 1) pretesting, then repeated testing throughout the duration of the course, 2) procedural as well as conceptual measures of learning and thinking, and 3) reliance on validated assessments to facilitate comparative cross-course analysis. In the meantime, embedded experiments, quizzes with correct answers provided, and thematic analyses of posted comments and responses on interactive discussion boards may provide valuable insights into participant learning, particularly in an interprofessional and person-centered context.
The shorter length of MOOCs may also facilitate engagement and completion, and thus learning.Citation23 To address the global public health issue of dementia, investigators at the Wicking Dementia Research and Education Centre (University of Tasmania) have developed an innovative 9-week “Understanding Dementia” MOOC (first offered in 2013)Citation23 and a 5-week “Preventing Dementia” MOOC (first offered in 2016). Both the “Understanding Dementia” and the “Preventing Dementia” MOOCs contain a pretest, the “Dementia Knowledge Assessment Scale.”Citation45 The “Preventing Dementia” MOOC also contains a validated instrument to enable participants to ascertain their risk for developing dementiaCitation46 and has been translated into Chinese. Both MOOCs include presentations from recognized national and international experts in the cause, care, and prevention of dementia, interviews with people living with dementia, and a variety of interactive activities. These activities include “thought trees” to probe participants’ understanding and experiences, and “ask an expert” discussion boards.
The “Understanding Dementia” MOOC is a pathway to the Wicking Dementia Research and Education Centre’s fully online Bachelor of Dementia Care program. MOOC participants can enroll in an elective unit (CAD110: Negotiated Study in Understanding Dementia) to receive academic credit for completing the MOOC. A similar pathway is planned to enable completers of the “Preventing Dementia” MOOC to gain academic credit through enrolling in a Bachelor of Dementia Care unit on prevention. To date, more than 83,000 participants from multiple countries and diverse educational backgrounds have participated in and completed the two MOOCs. The 34–49% completion rates are substantially more than the reported 5–15% completion rates for other medically related MOOCs.Citation23,Citation47 Further, there is no statistically significant difference in completion rates between “Understanding Dementia” MOOC participants who had previous university level experience and those who did not.Citation23 These high completion rates across a range of levels of education and occupation highlight the scale of unmet need for in-depth education about dementia prevention and care. The completion rates document the appropriateness of carefully designed MOOCs to contribute to medical education and practice, particularly for nationally and internationally known chronic care conditions. That said, a focus on chronic care conditions does not minimize the importance of MOOCs developed to address acute medical conditions, such as the Ebola crisis.Citation48
To optimize the contribution of MOOCs to the dissemination of information and learning, ReichCitation44 encouraged universities to
prioritize courses[…] designed from the outset to address fundamental questions about teaching and learning. Journal editors and conference organizers should prioritize publication of work conducted jointly across institutions, examining learning rather than engagement outcomes, and carefully designed research[…] Funding agencies should share these priorities…and support these initiatives.
Implications for research and practice
A recognized gap in health care is the lack of, or inconsistent focus on, patient- and family-centered care. Making this focus consistent can facilitate patients’ active engagement in their care, identify meaningful and functional outcomes that are not solely practitioner or policy driven, and facilitate the development of a patient- and family-centered evidence base that is integral to effective, quality care. Integrating the lived experiences of those who are ill and those who care for them into health- and medically-related MOOCs appears an important step in promoting patient- and family-centered care in medical education and practice. Integrating these lived experiences, including access and reimbursement issues, addresses important components of medical education, namely increasing health literacy, providing continuing medical education, and facilitating the development of innovative, problem-based teaching. Optimizing the advantages offered by carefully designed, well-structured, and outcomes-based MOOCs, the frequent MOOC titles of “Introduction to…” can be replaced with titles such as “Integrated perspectives on…” reflecting meaningful, authentic, evidence-based, collaborative, and integrated health and medical information to which thousands of people can have ready access.
Summary
MOOCs can provide valuable access to reliable information without the constraints of time, geographical location, or level of education. To document the effectiveness of any MOOC, its design needs to include the following features: 1) pretesting, then periodic testing of intended outcomes throughout the course, 2) procedural as well as conceptual measures of learning and thinking, including embedded interactive activities to facilitate engagement; and 3) validated assessment measures to enable comparison of learning and effectiveness across MOOCs. In this way, carefully designed and collaboratively developed MOOCs have the potential to bring together people in consumer, professional, and policy development groups, health care organizations, and universities to facilitate inclusive learning about evidence- and practice-based patient- and family-centered care. This learning can focus on prevention, intervention, and authentic, culturally appropriate, patient-centered outcomes, particularly for known chronic care conditions, many of which are global health concerns. Thus, MOOCs can play a role in increasing public health literacy, providing continuing professional education and stimulating the development of innovative teaching models for student learning focused on patient- and family-centered care.
Acknowledgments
The development of this paper was supported by funding from the JO and JR Wicking Trust (Equity Trustees). We thank Dr Susanne Becker for her assistance in the development of .
Disclosure
The authors report no conflicts of interest in this work.
References
- SiemensGConnectivism: Learning as Network-CreationELearnspace2005 Available from: http://www.elearnspace.org/blog/2005/08/11/connectivism-learning-as-network-creation/Accessed March 18, 2017
- DownesSAn introduction to connective knowledgeHugTMedia, Knowledge & Education – Exploring New Spaces, Relations and Dynamics in Digital Media Ecologies: Proceedings of the International ConferenceInnsbruck University PressInnsburck2007
- Institute of Medicine, Committee on Quality of Health Care in AmericaCrossing the Quality Chasm: A New Health System for the 21st CenturyWashington, DCNatl Acad Sci2001
- ReevesSPerrierLGoldmanJFreethDZwarensteinMInterprofessional education: effects on professional practice and healthcare outcomes (update)Cochrane Database Syst Rev20133CD002213
- World Health OrganizationFramework for Action on Interprofessional Education and Collaborative PracticeGeneva, SwitzerlandWorld Health Organization2010
- GoldbergLRScott KoontzJRogersNBrickellJConsidering accreditation in gerontology: the importance of interprofessional collaborative competencies to ensure quality health care for older adultsGerontol Geriatr Educ20123319511022289069
- WingoMTHavyerRDAComfereNINelsonDRReedDAInterprofessional collaboration milestones: advocating for common assessment criteria in graduate medical educationBMC Med Educ20151514926369325
- GoldbergLRBrownGMosackVAFletcherPAStudent reflections following exposure to a case-based interprofessional learning experience: preliminary findingsJ Interprof Care201429438038225300806
- LindenthalJJDedLisaJAHeinrichGFCalderón GersteinWSExposing medical students to expanding populationsAdv Med Educ Pract2015617718225834472
- van Leijen-ZeelenbergJEElissenAMJGrubeKThe impact of redesigning care processes on quality of care: a systematic reviewBMC Health Serv Res2016161926782132
- FramptonSBGuastelloSHoyLNaylorMSheridanSJohnston-FleeceMHarnessing evidence and experience to change culture: a guiding framework for patient and family engaged careNatl Acad Med2017
- BerghoutMvan ExelJLeensvaartLCrammJMHealthcare professionals’ views on patient-centered care in hospitalsBMC Health Serv Res20151538526373841
- NoelMAKaluzynskiTSTempletonVHQuality dementia care: integrating caregivers into a chronic disease management modelJ Appl Gerontol201736219521226081932
- ZachariaeRO’ConnorMLassesenBThe self-efficacy in patient centeredness questionnaire – a new measure of medical student and physician confidence in exhibiting patient-centered behaviorsBMC Med Educ20151515026374729
- SwisherAKPractice-based evidenceCardiopulm Phys Ther J20102124
- SingerSJBenzerJKHamdanSUImproving health care quality and safety: the role of collective learningJ Healthc Leadersh2015791107
- Australian Institute of Health and Welfare [webpage on the Internet]Leading Causes of Death2017 Available from: http://www.aihw.gov.au/deaths/leading-causes-of-death/Accessed March 20, 2017
- Centers for Disease Control and Prevention [webpage on the Internet]Chronic DiseasesAtlanta, Georgia2017 Available from: https://www.cdc.gov/chronicdisease/stats/index.htmAccessed March 20, 2017
- World Health Organization [webpage on the Internet]DementiaGeneva, Switzerland2016 Available from: http://www.who.int/mediacentre/factsheets/fs362/en/Accessed March 20, 2017
- FerriCPPrinceMBrayneCAlzheimer’s Disease InternationalGlobal prevalence of dementia: a Delphi consensus studyLancet200536695032112211716360788
- World Health Organization [webpage on the Internet]Top 10 Causes of Death WorldwideGeneva, Switzerland2015 Available from: http://www.who.int/mediacentre/factsheets/fs310/en/Accessed March 20, 2017
- LiyanagunawardenaTRWilliamsSAMassive open online courses on health and medicine: reviewJ Med Internet Res2014168e19125123952
- GoldbergLRBellEKingCRelationship between participants’ level of education and engagement in their completion of the understanding dementia massive open online courseBMC Med Educ2015156025889490
- LiyanagunawardenaTRWilliamsSAElderly learner and massive open online courses: a reviewInteract J Med Res201651e126742809
- GitlinLNHodgsonNOnline Training: Can It Prepare an Eldercare Workforce?American Society on Aging2016 Available from: http://www.asaging.org/blog/online-training-can-it-prepare-eldercare-workforceAccessed March 18, 2017
- HellerRLearning by MOOC or by crookMed J Aust2014200419219324580509
- HellerN webpage on the InternetLaptopU: Has the Future of College Moved Online?New Yorker2013 Available from: http://www.newyorker.com/magazine/2013/05/20/laptop-uAccessed March 18, 2017
- KearneyRCPremarajSSmithBMOlsonGWWilliamsonAERomanosGMassive open online courses in dental education: two viewpointsJ Dent Educ201680212112726834128
- MouradAJurjusAHusseinIHThe what or how: a review of teaching tools and methods in medical educationMed Sci Educ2016264723728
- MubuukeAGLouwAJNvan SchalkwykSUtilizing students’ experiences and opinions of feedback during problem based learning tutorials to develop a facilitator feedback guide: an exploratory qualitative studyBMC Med Educ201616626753932
- AttrillSLincolnMMcAllisterSSupervising international students in clinical placements: perceptions of experiences and factors influencing competency developmentBMC Med Educ20161618027422052
- KarpaKDHomLLHuffmanPMedication safety curriculum: enhancing skills and changing behaviorsBMC Med Educ20151523426711130
- BerghAMBacMHugoJSandarsJMaking a difference – medical students’ opportunities for transforming change in health care and learning through quality improvement projectsBMC Med Educ20161617127400963
- Scherer BassaniPBInterpersonal exchanges in discussion forums: a study of learning communities in distance learning settingsComput Educ2011564931938
- Woo NamCZellnerRDThe relative effects of positive interdependence and group processing on student achievement and attitude in online cooperative learningComput Educ2011563680688
- Hofmann-ApitiusMIs dementia research ready for big data approaches?BMC Med20151314526099627
- FrognerBKFrechHE3rdParenteSTComparing efficiency of health systems across industrialized countries: a panel analysisBMC Health Serv Res20151541526407626
- WellsJUnis struggling to define innovation: reportCampus Rev2017310
- ShweikiEMartinNDBeekleyACApplying expectancy theory to residency training: proposing opportunities to understand resident motivation and enhance residency trainingAdv Med Educ Pract2015633934625995656
- BackDABehringerFHarmsTPlenerJSostmannKPetersHSurvey of e-learning implementation and faculty support strategies in a cluster of mid-European medical schoolsBMC Med Educ20151514526337447
- DengRBenckendorffPA contemporary review of research methods adopted to understand students’ and instructors’ use of massive open online courses (MOOCs)Int J Inf Educ Technol201778601607
- SwinnertonBHotchkisstSMorrisNPComments in MOOCs: who is doing the talking and does it help?J Comput Assist Learn20173315164
- GoodingIKlaasBYagerJDKanchanaraksaSMassive open online course in public healthFront Public Health201315924350228
- ReichJRebooting MOOC research: improve assessment, data sharing, and experimental designScience20153476217343525554779
- AnnearMJToyeCMEcclestonCEDementia knowledge assessment scale: development and preliminary psychometric propertiesJ Am Geriatr Soc201563112375238126503020
- FarrowMUser perceptions of a dementia risk reduction website and its promotion of behavior changeJMIR Res Protoc201321e1523608480
- GoldbergLRKingAECookALEducation as an essential intervention in dementia literacy and careBMC Med Educ under review
- Ruiz De CastenadaRValticosAPittetDFlahaultAMOOCs (massive open online courses) as innovative tools in infections prevention and control: reflections from the first MOOC on EbolaAntimicrob Resist Infect Control20154S11625932325
