Abstract
Aim
Medical literature revealed that there is a lack of information about the opinions of medical interns and residents about curricula provided to them during their undergraduate programs, either in a group of detached subjects or an incorporated and efficacious topic (ie, pathology).
Purpose
To assess and compare the interns’ and residents’ perspectives towards Pathology as a subject. To recognize their opinions toward the relevance and application of Pathology while practicing clinically.
Methods
This study was a cross-sectional online, self-administered questionnaire targeting interns and residents. The questionnaire consisted of 30 questions, enquiring about the demographic data, subject strength, teaching duration, interest in the subject, and usefulness of Pathology as a subject in clinical practice.
Results
Overall, 103 participants completed the survey. The female and male percentage was 59.2% and 40.8% respectively. 86.4% of participants were interns, while 13.6% were residents. 87% of participants agreed that applying pathology during clinical practice is a skill that should be strengthened in the early stages of preclinical education of Medicine. A modest percentage believed that a practitioner could efficiently treat the majority of patients with no need to know the specifics of the pathological mechanisms involved. Most of the participants believed that pathology courses helped them in making a differential diagnosis, analysis of normal and pathological constituents, and dissection and identification of structures.
Conclusion
This study highlights the positive perceptions of Jordanian interns and residents toward pathology courses. It also demonstrates that participants prefer an active and dynamic educational model with an emphasis on better integration of pathology courses and clinical experiences that fit their needs in clinical practice. Thus, we recommend future studies to compare the competencies of interns and residents enrolled in the courses with integrated medical curricula, of pathology versus those who studied the conventional medical curricula of pathology, as well as to evaluate their perceptions of medical education.
Introduction
The medical faculties in Jordan are mainly following conventional lecture-based teaching, having minimal interdisciplinary integration and lacking a problem-based learning curriculum. There is an assumption by medical educators that this module of education has resulted in a poor impact on the Sciences of Basic Medicine during clinical practice as students thought the basic medical sciences were mostly unlinked to clinical pursuit. Although many findings on perceived clinical connection and remembrance of basic medical sciences during the first years of medical education are obtainable from various resources including those from Jordan, the corresponding data about attitude, perception, and application of a specific basic medical subject such as Pathology are still scarce.
Inspection of the medical literature revealed that there is a lack of information about the opinions and responses of medical interns and residents about curricula provided to them during the study years in medical schools, either in a group of solitary subjects or an incorporated and effective theme (ie, pathology). Observation of their perspective regarding the relevance and application of pathology as a basic medical science has a key role in the reconstruction of the process of education, better achievements, and future practice of Medicine. Therefore, this study aims to explore the interns’ and residents’ perspectives of perception and the relevance and application of pathology as a preclinical basic medical science during clinical practice in Jordan. The medical education system for the basic medical sciences has been static for a long period, with slight improvement here and there. One of the most defiant questions in medical teaching is to find the proper and most applicable teaching methods and strategies to actively attract students in the learning process during medical education in the pre-clinical sciences.Citation1 Many medical schools still practice lecture-based teaching, lacking a student-oriented approach.Citation2
It has been reported that students’ opinion was, that a group discussion is helpful to better understand the subject of pathology and has contributed to effective and interactive learning in addition to better readiness for involvement and elucidation of doubts with a comprehension of diverse thoughts of their peers, which will enhance teamwork. Based on students’ thoughts, discussions within groups helped them to trigger attention to the subject that way contributing to energetic, interactive, and efficient learning, better alertness for the activity, steady involvement, better explanation of doubts, and comprehension of various opinions and thoughts of their peers which would enhance teamwork. Only a small ratio of the students Chose seminars (7%) and tutorials (6.1%) as exemplary methods of teaching.Citation3 Poor incorporation of Basic and Clinical Medical Sciences during the education of medicine may undermine the connection between these studied subjects.Citation4
Scientists are worried that recalling basic science notions weakens after the early years of medical education, with clinicians scarcely in their clinical practice using basic sciences. The reason behind this could be that ~50–60% of unrehearsed information can be lost after 2 years and over time can be further decreased when new graduates are in training for specialty and clinical pursuit.Citation5
On the other hand, expert physicians in their clinical practice have been shown to utilize the principles and mechanisms of basic science to resolve complicated and abnormal medical conditions.Citation6–8
Continuous development and update of the programs in medical education are a must to keep up-to-date with technological and scientific advances, as well as making students and graduates concoct for their future careers and clinical practice. There is continuous pressure on medical education programs to keep pace with technological and scientific advances, as well as to make graduates ready for clinical practice and various graduate careers.Citation5 A study on the clinical importance of histology carried out by Waseem et al showed that students do not realize the significance of histology in their future practice as physicians.Citation9 In contrast, Pushpa et al, found in a study conducted regarding the attitudes and perceptions of students in their first year of medical education, showed that their attitudes largely improved towards histology after the course of a year, and it changed toward clarity, interest, and self-confidence.Citation10
Continuous incorporation of the curricula of histology and pathology in the first year of medical education is very important and much endeavor is essential to enhance students’ rapprochement for microscopic anatomy. This proof can be used as an extra urge for the continuous update of the histology courses, with distinctive assertions on the application of gained information in a clinical practice-oriented environment.Citation11 Case-based learning and case discussion proved to be effective, and the preferred tool for teaching microscopic pathology remains the microscope.Citation12
In the 20th century, pathology had a core importance in medical education for future physicians, but this status has decreased in the last few decades. There are some opinions stating that courses in pathology are less significant to medical education,Citation13 but on the other hand, some believe that pathology is essential to the comprehension of diseasesCitation14 and important to the development of a well-prepared practitioner physician. There are two key factors behind the negative opinion held by some in teaching pathology; the first is the changes in the role of pathology and the second is those changes related to the nowadays medical students.Citation15
The present state of medical education is in crisis, primarily attributable to the absence of evidence-based teaching methodologies.Citation16
In Problem-Based methods of Learning, educators are required to shift their educational roles, emphasizing the elevation of students’ self-motivation through a focus on their needs in the learning process, rather than a mere accumulation of facts.Citation17 Many studies show that nowadays students are leaning towards learner-centered education with more active and dynamic models to fulfill their needs and put them at the helm of their learning process.Citation18
Pathology serves as a fundamental medical science, offering a scientific foundation for medical practice and laying the initial groundwork for learning related to human disease processes.Citation19 Pathology as a discipline previously centered on autopsies and macroscopy, has evolved throughout the years to a technically sophisticated domain encompassing histology and molecular aspects. This transformation is also reflected in the way this field is taught in medical schools.Citation15
Providing a framework for the description of the diseases and functional and structural changes in diseases to achieve a better understanding and interpretation of the clinical signs and symptoms was the main concern of teaching pathology for undergraduate students in medical schools.Citation20
Case-based learning proves more effective than instructive lectures by enhancing students’ clinical reasoning, fostering self-directed learning and communication skills, improving knowledge recall and retention, and, most crucially, motivating them to engage in the learning process.Citation21 A study by Naeem et al revealed that a majority of undergraduate students (70.8% of participants) expressed the belief that learning Pathology is beneficial for practical clinical training. They also found that integrating pathology with clinical scenarios aids in comprehending the subject.Citation19
In both medical schools and residency programs, the significance of internship experiences with clinical faculty is growing steadily. The increasing importance of apprenticeship experiences with clinical faculty in the majority of medical schools and programs of residency raises concerns about the potential detachment of clinical education from the scientific underpinnings of medical practice.Citation22
Recentering the clinical/basic medical sciences seems to be fundamental to bridging the disparity between gained information and clinical practice.Citation23 It has been noted that gaining knowledge of basic science within a clinical context provides students with a deeper understanding of these sciences and is more easily applied by the students.Citation24
The fundamental medical sciences play a crucial role in primary medical education, serving as a pivotal component in promoting cohesive and effective learning for clinical practice.Citation5
Comprehending, retaining, and applying the acquired information in the basic medical sciences, effectively integrating it into clinical practice, may depend on strategies that explicitly highlight the relevance of these foundational sciences to clinical scenarios.Citation5
Medical literature indicates that there is limited information available regarding the thoughts and perspectives of medical interns and residents on the curricula they received during their undergraduate programs. This applies to both separate subjects and integrated topics, such as pathology. So, this study sets out to dive into the thoughts of interns and residents in Jordan, aiming to understand and compare their perspectives on pathology as a subject. The goal is to recognize what they think about the importance and practical application of pathology when they are practicing medicine.
Materials and Methods
This study was conducted among postgraduates in their internship and residency programs, using a cross-sectional questionnaire.
The questionnaire consisted of 30 questions, The first part of the questions delved into participants’ demographic details, encompassing factors such as gender, and age, as well as whether the participants held positions as interns or residents. The survey questions were formulated to be responded to using a five-level Likert scale, allowing participants to express their opinions on a spectrum from strongly agree to strongly disagree, investigating the subject strength, teaching duration, interest in the subject, and usefulness of Pathology as a subject in clinical practice.
The online survey was posted on the Google Forms platform, and participants’ invitations were sent to newly graduated interns and resident physicians via the Messenger and WhatsApp messaging platforms. Each participant was provided with a full explanation of the study, which was conducted to assess and compare the interns’ and residents’ perspectives toward Pathology as a subject, and to recognize their opinions on the relevance and application of Pathology in clinical practice. All participants were informed that their responses would be confidential and were considered as consent to participate in the study. The participants were informed that their participation data would be anonymized and stored confidentially with no risks associated. The project was reviewed and approved by the Ethics Committee for Scientific Research (ECSR) at Zarqa University in accordance with the requirements for the protection of human subjects and the ethical principles related to research studies. Approval number (1/5/2023). The guidelines outlined in the Declaration of Helsinki were followed.
The collected data underwent analysis using IBM SPSS version 23 (IBM Corp., Armonk, N.Y., USA).
The attributes of the participant’s perspective of perception and their views on the information provided by the pathology course were given scores. The Likert scale granted scores from 1–5 (Strongly agree=5, agree=4, neutral=3, disagree=2, strongly disagree=1). The scores of the attributes were summed and a total score was calculated for every participant. Attributes with negative nature were assigned reverse scoring (Strongly agree=1, agree=2, neutral=3, disagree=4, strongly disagree=5). The higher the scores the higher the positive perception towards the pathology course and the higher the value of information provided in the course.
This study was undertaken to explore the interns’ and residents’ perspectives regarding the perception, relevance, and application of pathology as a basic medical science during clinical practice in Jordan.
Statistical analysis was conducted using IBM SPSS Statistics for Windows, version 23 (IBM Corp., Armonk, N.Y., USA). Frequency (%) was used to present categorical data. The relationships between categorical variables were examined through the Chi-squared test (χ2) or Fisher’s exact test. For associations between continuous variables, one-way ANOVA and independent samples t-tests were employed. Statistical significance was defined at P values ≤ 0.05.
Results
A total of 103 participants (interns and residents) responded to the questionnaire, the frequency of female respondents was higher than males, and most of the participants were young (20–25 years of age) and interns. displays the general characteristics.
Table 1 General Characteristics of the Participants, N=103
The perceptions of participants towards the pathology course were assessed by asking the participants about aspects such as clinical relevance, time frame, importance, and application in clinical practice. A large percentage of participants agreed that the microscopic and gross morphology of disease is difficult to identify and recall (85%) and that the skill of applying pathology to clinical practice should be emphasized early in medical education (87%), as indicated in .
Table 2 Perceptions of Participants Towards the Pathology Courses, N=103
Eighty-three percent of the participants agreed that the courses integrating pathology and clinical practice (case-based learning) are better than the conventional lecture-based method of teaching which emphasizes the importance of applying advanced clinically based teaching methods.
Only half of the participants thought that pathology courses improved their skills for teamwork or were interesting. Moreover, only a modest percentage believed that a physician could adequately treat most patients without a comprehensive understanding of the details of biological and pathological processes. This underscores the significance of the pathology course in enhancing the overall knowledge of physicians, as highlighted in .
Table 3 Participants´ Opinions Regarding the Information and Methods of Teaching Provided in the Pathology Courses, N=103
The scores of the different attributes of perception and information were added into a total score. Perception scores/ information and methods scores were not significantly associated with gender, age, or the position of the participants. The total average score on perception (full score=40) was 23.90 ± 3.07. The total average score on the information (full score=35) provided by the course was 23.99 ± 4.3, .
Table 4 Association Between Perception Score/ Information and Methods Score and Different Variables, N=103
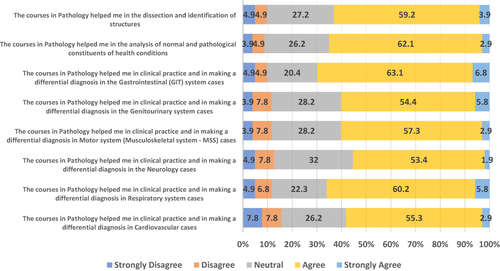
Participants’ goal is to apply education and knowledge in clinical practice. The impact of the pathology course on different aspects and medical specialties in clinical practice was evaluated. In general, over fifty percent of the participants affirmed that the pathology course was beneficial across all specialties. The impact of pathology courses varied depending on the subject and medical field. Most of the participants (interns and residents) believed that pathology courses mainly helped them in making a differential diagnosis in Gastrointestinal system (GIT) cases followed by differential diagnosis in respiratory system cases, analysis of normal and pathological constituents of health conditions, and dissection and identification of structures, .
Pathology does not seem an appealing residency choice for Participants (both interns and residents). Among the interns (n=89), a very low percentage of them (n=10, 11.2%) would consider pathology for a residency program, 37 (41.6%) would not consider it a choice, and 42 (47.2%) might consider it a choice for residency. Additionally, among the residents (n=14), almost more than two-thirds (n=10, 71.4%) did not add pathology as a choice for residency when they applied for the program. When the interns (n=89) were asked if they would consider pathology as a residency choice, pathology was more tempting to female physicians, 100% of those who would consider pathology for residency were females (n=10/10) compared to 48.6% in those who would not consider pathology, (n=18/37), and 54.8% who may consider it as a residency choice (n=23/42), Chi-Square=8.695, p=0.013. No statistically significant similar associations were found in different age groups, p value=0.362.
Discussion
Pathology has evolved into various subspecialties and has become more intricate. Nevertheless, the core focus of pathology continues to be centered on the examination of the origins and alterations induced by diseases.
The conventional educational programs of medicine have been criticized for various reasons, such as information overcrowding, emphasis on some subjects more than others, the content of pathology courses having relatively nonrelevant topics, repeated lectures, the applicability of pathology to clinical practice, and segregation between basic medical sciences and clinical sciences.
The data presented in this survey method study consists of a qualitative and quantitative part. It has been aimed to understand the participants’ preferences. Although the survey method appeared suitable for addressing the questions, there were some concerns about the methodological limitations of the study. This study showed a contradictory association between students’ perception of receiving overloaded courses, being able to recall the microscopic and gross morphological changes of diseases, and receiving information that applied to clinical practice.
The Results showed that the majority of the participants (85%) agreed that the microscopic and gross morphology of diseases is difficult to recall and identify. On the other hand, the majority of the participants (87%) emphasized the importance of reinforcing the skill of applying pathology to clinical practice early in medical education. A recent study conducted by Nabeela Naeem et al revealed a higher proportion of female participants compared to male students. A majority of the students expressed interest in the subject of pathology and agreed that knowledge about pathology is beneficial during clinical rotations.Citation25 In the same study, approximately one-third of the students (27.84%) perceived the subject of Pathology to be challenging. However, the students found the explanations, presentations, and clinical correlations utilized to simplify the subject during lectures to be satisfactory.Citation25
This data is highly aligned with the data found in the present study, where it has been found that newly graduated physicians (interns and residents) are willing to continue learning the basics of pathology, especially since more than half of them agreed that pathology courses helped them in different medical situations and approaches and helped them in making differential diagnoses in various medical conditions, in addition to analysis of normal and pathological constituents of health conditions, and dissection and identification of structures.
The majority of participants (83%) agreed that case-based learning and courses integrating pathology and clinical practice are better than the traditional lecture-based method of teaching pathology. These results align closely with those from a recent study at AlBalqa Applied University, Faculty of Medicine, Jordan. The study demonstrated the success of case Discussions and affirmed that the microscope remains a preferred and effective tool for teaching microscopic structures of tissues. Nonetheless, there is a requirement for substantial effort to enhance students’ appreciation for anatomic pathology.Citation12
It was observed that a small percentage of participants held the belief that a physician can successfully treat patients without possessing detailed knowledge of the biological and pathological processes associated with the disease condition. These results closely align with those from a study conducted by Seema Deepak et al which revealed that 70% of the participants in this study perceive subjects in preclinical years as laying a fundamental foundation for clinical procedures and skills. Moreover, 46% of the participants expressed the opinion that the curriculum lacks clinical relevance.Citation26 Comparable results were documented by Emad Aborajooh et al, indicating that around three-quarters (73.9%) of the students emphasized the importance of basic medical sciences in their development as future physicians. Furthermore, about 82% held the belief that the integration of clinical practice into basic science teaching is indispensable. Moreover, 73% of students are inclined towards integrating problem-based learning into their medical education curricula.Citation18
In our view, the objective of current pathology teaching should be to cultivate a willingness to learn the fundamentals of pathology. The manner in which this content is taught holds significance, as it shapes the perspectives of newly graduated physicians regarding the field and influences what they retain. The perception scores/information and method scores were not associated with gender, age, or whether the participants were interns or residents, and their goal was to apply education and knowledge in clinical practice. It was observed that Pathology does not emerge as an attractive choice for residency among participants, including both interns and residents. Only 11.2% of the participants considered Pathology as a career choice, a finding consistent with a study conducted by Al Khader et al.Citation12
Conclusion
The current attitudes and perceptions of new graduates (interns and residents) toward pathology courses during the years of basic medical education are interesting and warrant further consideration and analysis.
Future studies will be needed to compare the competencies of interns and residents enrolled in the courses with integrated medical curricula, of pathology versus those of interns and residents who studied the conventional medical curricula of pathology, as well as to evaluate their perceptions of medical education.
Among the targets of medical education is gaining the knowledge, attitudes, skills, and needed values required to perform medical practice professionally, competently, and safely; it is very important to have a better integration of basic sciences courses and clinical experiences to achieve these targets.
A full understanding of the pathological background of diseases and medical conditions as a basic science is a cornerstone for good medical knowledge and clinical practice, which demonstrates the importance of the contribution of the pathology course to the overall knowledge of physicians.
Better integration of pathology as a basic science with clinical practice is an important issue, with an emphasis on applying advanced clinically based teaching methods.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. All authors have reviewed and endorsed the manuscript. The criteria for authorship have been satisfied, and each author attests that the manuscript reflects honest and genuine work.
Disclosure
The authors report no conflicts of interest in this work.
References
- Koles P, Nelson S, Stolfi A, et al. Active learning in a Year 2 pathology curriculum. Med Educ. 2005;39(10):1045–1055.
- Grover S, Sood N, Chaudhary A. Reforming pathology teaching in medical college by peer-assisted learning and student-oriented interest building activities: a pilot study. Educ Health. 2017;30(2):126–132.
- Zubair AA. A survey-based analysis of students’ perspective of the current medical education system, teaching-learning methods, and their attitude towards research in a Medical College in North Karnataka with special reference to pathology as a subject. J Evid Based Med Healthc. 2019;6(15):1171–1176. doi:10.18410/jebmh/2019/244
- Ginzburg SB, Brenner J, Cassara M, Kwiatkowski T, Willey JM. Contextualizing the relevance of basic sciences: small-group simulation with debrief for first- and second-year medical students in an integrated curriculum. Adv Med Educ Pract. 2017;8:79–84. doi:10.2147/AMEP.S124851
- Malau-Aduli BS, Alele FO, Heggarty P, Teague PA, Sen Gupta T, Hays R. Perceived clinical relevance and retention of basic sciences across the medical education continuum. Adv Physiol Educ. 2019;43:293–299. doi:10.1152/advan.00012.2019
- Norman G. The basic role of basic science. Adv Health Sci Educ Theory Pract. 2012;17:453–456. doi:10.1007/s10459-012-9394-8
- Norman GR, Trott AD, Brooks LR, Smith EKM. Cognitive differences in clinical reasoning related to postgraduate training. Teach Learn Med. 1994;6:114–120. doi:10.1080/10401339409539657
- Patel VL, Groen GJ, Arocha JF. Medical expertise as a function of task difficulty. Mem Cognit. 1990;18:394–406. doi:10.3758/BF03197128
- Waseem N, Rasheed A, Gill M, Asad A, Shamim MO, Waseem F. The attitudes of medical students towards clinical relevance of histology. PAFMJ. 2021;71(1):351–356. doi:10.51253/pafmj.v71i1.3756
- Pushpa and Suruchi Histology. Perception and Attitude of First Year MBBS Students. Pushpa and Suruchi Histology; 2017:2.
- Teshome D. Attitude and perception of medical students towards histology subject at wollo university, Ethiopia. Adv Med Educ Pract. 2022;13:337–344.
- Al Khader A, Obeidat FN, Abu Shahin N, et al. Medical students’ perceptions of pathology and a proposed curricular integration with histology: a future vision of curricular change. Int J Morphol. 2020;38(1):38–42.
- Jackson M, Arnott B, Benbow EW, Marshall R, Maude P. Doctors Don’t Need to Know About the Pathological Basis of Disease. ACP News; 2003:33–39.
- Iversen OH. The teaching of pathology in undergraduate education programs in medicine in Europe. Pathol Res Pract. 1997;193(4):241–256.
- Herrmann FEM, Lenski M, Steffen J, et al. A survey study on student preferences regarding pathology teaching in Germany: a call for curricular modernization. BMC Med Educ. 2015;15(94). doi:10.1186/s12909-015-0381-7
- Nekkanti S, Manjunath S, Mahtani A, et al. A survey-based feedback analysis of the current medical teaching methodology and trends in medical research practice in a south Indian medical institute. Int J Med Students. 2018;6(1):6–14.
- Kilroy DA. Problem-based learning. Emerg Med J. 2004;21(4):411–413.
- Aborajooh E, Al-Taher R, Tarboush NA, et al. Amina Bucheeri, A cross-sectional study of basic education influence on the clinical training: attitudes and perception among Jordanian medical students. Ann Med Surg. 2020;60:456. doi:10.1016/j.amsu.2020.11.022
- Naeem N, Jamal S, Majeed S, Asghar R, Khan H. Evaluation of undergraduate medical and dental students’ perceptions and feedback of teaching-learning methodology in pathology. Prof Med J. 2022;29(3):415–419.
- Vijayan P, Ponniah A. A survey study based on undergraduate medical students’ feedback regarding pathology and the teaching-learning methodologies employed. Trop J Pathol Microbiol. 2017;3(2):149–154.
- Datta A, Ray J. Case based learning in undergraduate pathology – A study to assess its efficacy and acceptability as teaching-learning tool. IAIM. 2016;3(6):93–100.
- Brass EP. Basic biomedical sciences and the future of medical education: implications for internal medicine. J Gen Intern Med. 2009;24(11):1251–1254. doi:10.1007/s11606-009-0998-5
- Abd-Rabo M, El-Belbasy R, Abo-Elmagd EK. Medical students’ attitude and perception towards basic medical sciences in the faculty of medicine for girls, al-azhar university: a study prior to the integrated program. EJHM. 2018;70(12):2043–2050. doi:10.12816/0045026
- Torre D, Daley B, Sebastian J, Elnicki D. Overview of current learning theories for medical educators. Am j Med. 2006;119(10):903–907. doi:10.1016/j.amjmed.2006.06.037
- Naeem N, Jamal S, Majeed S, Asghar R, Khan H. Amat-ul-Naval Talha, Evaluation of undergraduate medical and dental students’ perceptions and feedback of teaching-learning methodology in pathology. Prof Med J. 2022;29(03):415–419.
- Deepak S, Dakshayani KR, Manjunatha SN. The relevance of the preclinical curriculum during clinical practice: interns’ perspective in a Government Medical College. Int J Anat Res. 2017;5(1):3379–3383.