Abstract
Background
Cardiovascular diseases are the leading cause of preventable morbidity and mortality in the USA. Medical schools must prepare trainees to address prevention, including improving ability in counseling patients to modify lifestyle risk factors. Most medical students do not receive significant training or clinical experience in preventive medicine until the clinical years of medical school. To enhance student education in disease prevention and lifestyle counseling, and simultaneously target cardiovascular disease prevention in high-risk Chicago neighborhoods, the Northwestern University Feinberg School of Medicine and Chicago Department of Public Health with support from the GE Foundation, developed the Keep Your Heart Healthy program.
Methods
Medical students participated in intensive faculty-led training. They subsequently screened local residents to identify and counsel for cardiovascular disease risk factors. Fifty-one predominantly preclinical medical students screened residents of the Humboldt Park and North Lawndale neighborhoods in Chicago, IL, at 31 screening events from August to December 2013. Fifty students (98% response rate) completed a survey assessing the educational value of various program components following the pilot.
Results
Of all respondents, 92% of students reported improved knowledge of cardiovascular disease prevention and 94% reported improved knowledge of vulnerable populations and health equity. The majority (88%) reported that their participation supplemented material they learned in the classroom. Eighty-six percent of students reported that their encounters with community participants were of educational value. Integration of this program into the medical school curriculum was supported by 68% of students.
Conclusion
Keep Your Heart Healthy educates primarily preclinical medical students in cardiovascular disease prevention and prepares them to apply this knowledge for patient counseling. Results from student surveys demonstrate that this service-learning initiative enhances medical student knowledge in cardiovascular disease prevention, supplements classroom material, and provides students a valuable opportunity to apply interviewing and counseling skills in a real patient encounter.
Background
Cardiovascular diseases (CVDs) remain the leading cause of morbidity and mortality in the USA.Citation1 CVD is largely preventable with lifestyle modification and targeted drug treatments. The estimated annual direct and indirect costs of CVD were $313 billion in 2009.Citation2 In 2011, the Chicago Department of Public Health (CDPH) launched its Healthy Chicago public health agenda in order to improve the overall physical and mental health of its residents.Citation3 Healthy Chicago priorities that target CVD include heart disease and stroke prevention and obesity prevention. The Keep Your Heart Healthy (KYHH) program was developed as a partnership between CDPH, Northwestern University Feinberg School of Medicine (NUFSM), and community partners to address these citywide goals.
At the community level, KYHH aims to screen at-risk Chicago residents for CVD risk factors, counsel them on behavior and risk factor modification, and refer participants to primary care follow-up. Results from previous programs suggest that medical students’ involvement can benefit low-resource communities through health counseling and education.Citation4 This evidence indicates that medical students serve as strong advocates for patient health, which can lead to improved outcomes.
Beyond targeting community health improvement, KYHH is also an educational initiative for medical students. Student involvement in community-based programs is a successful method of experiential service-learning for education.Citation5,Citation6 Results from prior programs indicate that students participating in community volunteer work learn to interact with people of different backgrounds and improve communication skills. Students also develop new clinical skills such as taking blood pressure measurements, and gain a greater understanding of issues affecting local neighborhoods.Citation5,Citation7 Many reports have detailed the role of community health workers (CHWs)Citation8,Citation9 and lay health workersCitation10,Citation11 in community-based cardiovascular (CV) risk reduction programs. However, the available evidence for medical students is largely limited to third- and fourth-year students on their clinical rotations at community hospitals and in free clinics.Citation12–Citation15 Data are sparse regarding community-based intervention programs involving preclinical medical students outside of free clinics.
Traditionally, medical students participate in service-learning informally, such as in student-run clinics or health fairs. KYHH is unique as it is a more formal, structured community-based service-learning program that involves predominantly preclinical students in the screening and counseling for CVD risk. Participation in KYHH provides students with an opportunity to apply medical knowledge and skills in nonclinical settings. We hypothesized that student participation in KYHH would increase student knowledge of disease prevention and improve student comfort and ability in counseling and interpersonal communication. Overall, the didactic training and applied experience in which medical students participate is intended to align with NUFSM educational competencies. These competencies are based on Accreditation Council for Graduate Medical Education (ACGME) objectives for medical education. Here we detail the development, pilot implementation, and initial evaluation of KYHH as a service-learning model for medical student education at NUFSM.
Methods
Program development
In 2012, KYHH was founded through collaboration between NUFSM, CDPH, and the GE Foundation. The NUFSM principal investigator recruited eight university faculty members to serve on a KYHH Executive Committee. The Executive Committee included the Chair of the Department of Preventive Medicine, the Director of the NUFSM Institute for Public Health and Medicine, the NUFSM Vice Dean for Education, the Commissioner of CDPH, a medical student representative, and faculty experts on nutrition, motivational interviewing, community health, and CVD prevention. The Executive Committee advised the NUFSM principal investigator on project development and led medical student training sessions.
A Student Advisory Committee (SAC) was created, comprising two third-year medical student chairs, three additional third-year medical students, two second-year students, and four first-year medical students. During the development of KYHH, a senior research study coordinator was hired to organize project communication and activities. Together, the Executive Committee and SAC identified guiding objectives of KYHH, which included: 1) aligning with and strengthening the NUFSM medical student educational curriculum’s core competencies; 2) addressing a critical community and public health priority; and 3) completing a valid evaluation of the project.
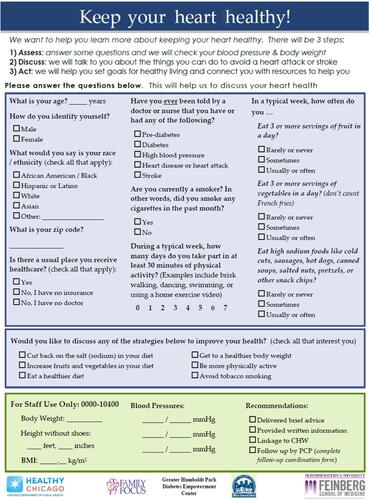
The Chicago communities of Humboldt Park and North Lawndale were selected as pilot neighborhoods since they have been previously identified as under-resourced, low-income communities with large populations of two high-risk racial minority groups (Hispanic and African-American, respectively). KYHH partnered with the Greater Humboldt Park Community Diabetes Empowerment Center and Family Focus Lawndale organizations in each respective neighborhood. Each community organization is linked with a local Federally Qualified Health Center (FQHC). CHWs from each of these organizations recruited local participants for screening. The multidisciplinary Executive Committee, which included experts in creating surveys for nutrition and physical activity, developed a screening questionnaire for students to administer at screening events (see Figure S1). A Spanish translation was created to ensure cultural sensitivity and appropriateness of the content. The Institutional Review Board at NUFSM, which reviews and approves all research projects, determined that KYHH qualified for an exemption as a research and demonstration project for public health.
Faculty and student recruitment
Prior to KYHH screening events, the study coordinator recruited NUFSM attending physicians and an Internal Medicine chief resident to supervise medical students at screening events. The SAC sent a brief survey to the NUFSM student body gauging interest for participation in KYHH. Based on positive feedback, the SAC recruited a pilot group of students to participate in the community screening events. Students were recruited via email participation surveys, interest meetings, and announcements during classes. Prior to participation, students were required to attend two, 2-hour long training sessions led by faculty experts.
Training session content
Training sessions consisted of a combination of formal didactic teaching and interactive counseling practice. Didactic lectures covered the epidemiology and prevention of CVD, the American Heart Association’s Life’s Simple 7 recommendations,Citation16 and optimal dietary modification strategies for CVD risk reduction. Interactive sessions were dedicated to motivational interviewing and counseling training in simulated patient encounters. Finally, one session was devoted to training medical students about their specific role during each screening event, including how to measure blood pressure accurately and elicit pertinent clinical and CV medical history (see Figure S1 for specific questions asked).
Students were taught to refer participants for primary care follow-up for elevated blood pressures of ≥140 mmHg systolic blood pressure and/or 90 mmHg diastolic blood pressure. In the presence of CVD warning symptoms (eg, chest pain, shortness of breath, syncope), students were trained to consult the supervising attending physician to determine the need for emergent hospital referral. Students were also advised to consult the attending physician in the event of any uncertainties in the participant encounter. At the conclusion of each training session, students were asked to complete a feedback survey evaluating each lecture for content relevance. Students were also asked to provide written feedback with suggestions to improve training sessions.
Screening event schedule and organization
Screening events were held weekly in both Humboldt Park and North Lawndale. A total of 1,161 people (877 in Humboldt Park and 284 in North Lawndale) were screened during the pilot. CHWs recruited participants for screening via handouts and poster advertisements throughout the week during various community health programs. Participants were made aware that screening sessions were hosted by NUFSM and medical students were conducting the screenings under the supervision of attending physicians. Further details on results from the community screenings have been previously published.Citation17 Additional screening events were organized for special neighborhood events (eg, festivals and food drives) at each community center. Screening and education methods were consistent for both communities. Each session was staffed by at least one supervising attending physician, the program coordinator, two to three CHWs, and up to ten students. Students with Spanish-speaking ability were encouraged to participate at the Humboldt Park events. As needed, CHWs served as translators.
Screening session content and student role
Each screening encounter began with measurement of participant height, weight, and calculation of body mass index. Each student then administered the screening questionnaire. Students sequentially asked participants each question and recorded answers on the questionnaire. Following this, students performed blood pressure measurements. Automated blood pressure cuffs (Omron BP760; Omron Corp., Kyoto, Japan) were used for this assessment, with the participant seated in a chair with both feet on the floor, the back and arm supported, for 5 minutes prior to the first measurement. Students obtained a total of three blood pressure readings, recorded each result on the questionnaire, and recorded the average of the final two readings.
Attending physicians circulated around the student– participant pairs to ensure that student counseling and risk assessment were appropriate and accurate. The attending physicians offered feedback and teaching to students when necessary, for instance looking up appropriate management guidelines to direct further care. In situations when participants reported active or recent symptoms to students or had other concerns, attending physicians joined the conversation to help determine the appropriate course of follow-up for the participant. The attending physician later taught the student about the clinical relevance and significance of the participant’s presentation.
Students were also encouraged to seek the input of the attending physician in any circumstance in which the student was unsure of further management. Participants with significantly elevated blood pressure (defined as systolic blood pressure ≥180 mmHg or diastolic blood pressure ≥120 mmHg) or symptomatic participants at the attending physician’s discretion, were urged to go immediately to a local emergency department. Asymptomatic participants with hypertension below these blood pressure levels were referred either to a FQHC or encouraged to follow-up with their primary care physician. In this case, a referral form was completed and sent to either the FQHC or the established primary care clinic.
Following blood pressure measurement, students prompted the participant to select a health behavior topic for discussion and counseling (see Figure S1). Students provided personalized counseling based on the health behavior topic preferences selected by community participants. These discussions focused on strategies participants could utilize to modify high-risk behaviors in order to reduce their personal CVD risk. Most of these counseling points were derived from the American Heart Association’s Life’s Simple 7 campaign and tailored to the cultural nuances and available local resources within the community.
After participating in at least one screening event, students were asked to complete an evaluation survey developed by the SAC. This survey was piloted to elicit students’ opinions on the educational value of KYHH (see ).
Table 1 Survey results from KYHH pilot
Results
A total of 51 students (37 first-year, four second year, two third-year, and eight fourth-year medical students) completed the two, 2-hour KYHH training sessions. The students staffed 31 screening events with each event staffed by a mean (standard deviation [SD]) of 6.8 (2.4) students. Students volunteered on average (SD) once per 7.9 (5.9) events (see for further details).
Table 2 Number of student participants and frequency of participation in KYHH pilot
All 51 students provided feedback after completing the training sessions. Seventy-one percent of participating students identified motivational interviewing as a strength of the training. CVD background data (59%) and dietary guidelines for CV health (47%) were also identified as strengths. Students indicated several areas for improvement including more practice for clinical scenarios with coaching tips (53%) and more time for role-play of communication skills (35%).
Fifty students, representing 98% of the students trained to participate, completed an evaluation of the educational value of KYHH after attending at least one screening event (see ). Ninety-two percent of respondents said their participation strengthened their knowledge base in CVD prevention. Ninety-four percent of students indicated that their participation improved their education regarding vulnerable populations and health equity.
All survey respondents (100%) reported that the opportunity to apply what they had learned in the classroom and during KYHH trainings was of educational value. Eighty-eight percent of students reported that their participation in KYHH added to the material they learned through the NUFSM curriculum. Students reported that their encounters with community participants during screening events were one of the most educational components of KYHH. Sixty-eight percent of students favored integration of KYHH into the NUFSM curriculum.
Individual student reflections on KYHH were overall positive (see ). These testimonials highlighted the unique opportunity to work in local communities, engage one-on-one with community residents, and apply in-classroom concepts in practical settings. Student comments also reflected support for integrating KYHH into the existing NUFSM curriculum.
Table 3 Student participants’ qualitative feedback for KYHH
Discussion
KYHH is a unique initiative that enables preclinical students to gain knowledge of CVD prevention, apply medical knowledge in the community setting, build interpersonal communication skills, and serve as patient educators. As shown in this report, students felt this program enriched their medical education experience. Students reported that KYHH improved their knowledge of CVD prevention, and enhanced their education surrounding vulnerable groups and health equity. The majority felt that KYHH added to the material they learned in the classroom. The majority would also support integration of KYHH into the NUFSM curriculum. Most students also felt that their encounters with community residents were of educational value. Individual student comments noted the value of practicing motivational interviewing skills in a “real patient” setting. The program also exemplifies a successful collaboration and partnership between multiple stakeholders – namely, an academic institution, public health department, and community organizations and leaders – to develop a program of mutual benefit.
Advantages of student involvement in the community
Students’ participation in community settings is increasingly recognized as an important part of medical education. The Liaison Committee on Medical Education, the primary accrediting body for schools of medicine in the USA and Canada, recommends that medical schools create sufficient opportunity for students to participate in service-learning in order to provide context to their academic coursework and emphasize future physicians’ roles as citizens and professionals.Citation18 There are limited objective outcome data which show that service learning makes a positive impact on medical student education. Prior evidence suggests that greater involvement in service-learning as a medical student may be related to above-average class rank and election to the Alpha Omega Alpha medical honor society,Citation6 although the link is not necessarily causal.
Subjective student accounts favor service-learning as an effective educational opportunity within health professions education.Citation19–Citation22 These analyses suggest that increased medical student community engagement and reciprocal knowledge transfer between students, faculty, and CHWs can help prepare medical students to practice in a health care environment that increasingly places importance on accountability to the surrounding community’s health.Citation23 Prior programs suggest that community engagement experiences support health professions student understanding of social responsibility in their future careers.Citation24 Medical students have previously indicated that engagement in service-learning supports the development of patient education skills, enhances their ability to articulate the role of physicians in the community, and promotes an understanding of how socioeconomic factors influence health care access and compliance.Citation5,Citation25,Citation26
Our results build on these findings. As a nonclinic-based service-learning opportunity, KYHH provides a venue to apply skills learned in didactic and interactive training in a community setting. This community-based, rather than classroom-based or clinically based, program enhanced students’ medical knowledge and understanding of vulnerable populations. Accordingly, students noted that their experience through KYHH supplemented the material they learned in the NUFSM curriculum.
KYHH and the NUFSM competencies
NUFSM employs a competency-based education framework for its medical students. These competencies are used to guide curricular development, define the expectations of student progress, and serve as an assessment tool for student learning and growth through medical school.Citation27 The eight competency objectives at NUFSM are: Patient-centered Medical Care, Effective Communication and Interpersonal Skills, Medical Knowledge and Scholarship, System Awareness and Team-based Care, Personal Awareness and Self-care, Community Engagement and Service, Continuous Learning and Quality Improvement, and Professional Behavior and Moral Reasoning.
These competencies, which are based on the educational competencies defined by the ACGME, serve as a launching point for all Northwestern medical school efforts. KYHH effectively addresses several of the competency points:
Patient-centered Medical Care through participant CVD risk counseling and the provision of targeted recommendations based on participant-specific risk factors and neighborhood-specific resources.
Effective Communication and Interpersonal Skills through the use of motivational interviewing for effective participant counseling, interaction with attending physicians, and encounters with community participants at screening events.
Medical Knowledge and Scholarship through didactic and applied training sessions covering CVD epidemiology, risk, prevention, and lifestyle contributions to overall health.
System Awareness and Team-based Care through involvement in high disease risk, low-resource neighborhoods promoting an understanding of barriers to health care access.
Community Engagement and Service by offering students the opportunity to interact with real patients in the community setting as a supplement to simulated interactions in the classroom setting.
Continuous Learning and Quality Improvement through participation in experiential learning and involvement in the vertical learning model (ie, attending physicians mentor senior and junior students, senior students teach and provide feedback to junior medical students).
In post-screening surveys and in-person interviews, students confirmed that KYHH helped address these competency goals. Empirical evidence demonstrates that community programs linked to course-based learning objectives, such as the one described here, have a greater impact on students than elective or voluntary experiences.Citation28 Furthermore, evidence suggests that there is an educational benefit for medical students who participate in service-learning outside of structured clinical settings in comparison to learning solely in clinical settings.Citation28 Thus, KYHH has the potential to enhance medical school education.
Limitations
Though the KYHH pilot has generated positive feedback and has been successfully implemented as a service-learning opportunity for medical students, several limitations exist. Objective outcomes data are pending for this program. We did not compare those students involved in KYHH and those uninvolved, thus we are unable to determine empirically whether participation in KYHH improves students’ performance on objective examinations, class rank, preclinical and clinical grades, or election to honor societies. Finally, KYHH students were recruited based on interest, creating a potential for volunteer bias in outcomes analysis.
Future directions
With support from students and faculty, the NUFSM Curriculum Committee approved KYHH as an elective course beginning September 2015 for the incoming class. To obtain elective credit, we will include a few changes including formalized student performance evaluations by attending physicians at community events, and a minimum attendance at ten community events. As with any curricular program, resources including staff and faculty involvement, supplies, and transportation have been required for KYHH to operate. The GE Foundation largely provided the monetary support for the pilot, and as the program has grown, additional resources have been provided by NUFSM. Furthermore, with the expansion of KYHH to up to 16 communities by 2016, NUFSM will partner with additional community-based organizations and widen the students’ ability to identify how different environmental, socioeconomic, and cultural dynamic factors affect the health of individuals and communities across Chicago.
Further analysis is needed to determine how participation in KYHH influences student education. Going forward, we plan to measure the effect of KYHH on academic outcomes such as performance on Objective Structured Clinical Examinations, clinical clerkships, and national medical licensing examinations. Preliminary results from community screenings have already been published.Citation17 We anticipate that the effect of our program on community residents’ health will continually be evaluated as the project moves forward.
Conclusion
In summary, KYHH has enhanced medical school education for participating NUFSM students by addressing several of the NUFSM and ACGME competencies. Through its novel collaboratively developed community-based screening and counseling model, KYHH may enhance medical students’ ability to emphasize and counsel for prevention in their future practice. By integrating the program into the NUFSM curriculum, we hope that KYHH will continue to strengthen the education of medical students.
Acknowledgments
The authors thank the CDPH, Greater Humboldt Park Community Diabetes Empowerment Center, Family Focus Lawndale, Omron Corporation, American Heart Association Chicago Metro Affiliate, the KYHH Executive Committee, and SAC, faculty, and student volunteers for screening events, and all community resident participants. Funding for KYHH was provided by a grant from the GE Foundation with support from NUFSM.
Supplementary material
Development and evaluation of a service-learning model for preclinical student education in cardiovascular disease prevention.
Disclosure
The authors report no conflicts of interest in this work.
References
- Centers for Disease Control and PreventionLeading Causes of DeathAtlanta, GACDC2013 Available from: http://www.cdc.gov/nchs/fastats/lcod.htmAccessed May 24, 2014
- NHLBIFact Book Fiscal Year 2012: Disease StatisticsBethesda, MDNHLBI2013
- CDPHHealthy Chicago: A Public Health AgendaChicago, ILChicago Department of Public Health2011
- GorrindoPPeltzALadnerTRMillerBMRobertFFowlerJMedical students as health educators at a student-run free clinic: improving the clinical outcomes of diabetic patientsAcad Med201489462563124556762
- BurrowsMSChauvinSLazarusCJChehardyPRequired service learning for medical students: program description and student responseTeach Learn Med1999114223231
- BrushDRMarkertRJLazarusCJThe relationship between service learning and medical student academic and professional outcomesTeach Learn Med200618191316354133
- LandyDCGorinMAO’ConnellMTStudent-led rural health fairs: attempting to improve medical education and access to health careSouth Med J2011104859860321886071
- BalcazarHAlvaradoMOrtizGSalud Para Su Corazon (health for your heart) community health worker model: community and clinical approaches for addressing cardiovascular disease risk reduction in Hispanics/LatinosJ Ambul Care Manage201134436237221914992
- BalcazarHRosenthalELBrownsteinJNRushCHMatosSHernandezLCommunity health workers can be a public health force for change in the United States: three actions for a new paradigmAm J Public Health2011101122199220322021280
- De las NuecesDHackerKDiGirolamoAHicksLSA systematic review of community-based participatory research to enhance clinical trials in racial and ethnic minority groupsHealth Serv Res2012473 Pt 21363138622353031
- DodaniSCommunity-based participatory research approaches for hypertension control and prevention in churchesInt J Hypertens2011201127312021747975
- PennantMDavenportCBaylissSGreenheldWMarshallTHydeCCommunity programs for the prevention of cardiovascular disease: a systematic reviewAm J Epidemiol2010172550151620667932
- FancherTLKeenanCMeltvedtCAn academic-community partnership to improve care for the underservedAcad Med201186225225821169777
- ChastonayPZesigerVKlohnADevelopment and evaluation of a community immersion program during preclinical medical studies: a 15-year experience at the University of Geneva Medical SchoolAdv Med Educ Pract20134697623900611
- DentMMMathisMWOutlandMThomasMIndustriousDChronic disease management: teaching medical students to incorporate communityFam Med2010421073674021061208
- AHAMy Life Check – Life’s Simple 7 Available from: http://mylifecheck.heart.org/Accessed May 21, 2014
- Ducharme-SmithAKleinDARassiwalaJThe keep your heart healthy project: engaging medical students to reduce risk of cardiovascular diseaseJacobs J Epidemiol Prev20151117
- LCMEIS-14-A: Service Learning Available from: http://www.lcme.org/connections/connections_2013-2014/IS-14-A_2013-2014.htmAccessed May 18, 2014
- MauranaCAGoldenbergKA successful academic-community partnership to improve the public’s healthAcad Med19967154254319114857
- CauleyKMauranaCAClarkMAService-learning for health professions students in the community: matching enthusiasm, talent and time with experience, real needs and schedulesTaylorBExpanding Boundaries: Serving and LearningWashington, DCCorporation for National Service199615457
- ConnorsKSeiferSDOvercoming a century of town-gown relations: redefining relationships between communities and academic health centers through community-campus partnershipsTaylorBExpanding Boundaries: Serving and LearningWashington, DCCorporation for National Service1997228
- DornanTLittlewoodSMargolisSAScherpbierASpencerJYpinazarVHow can experience in clinical and community settings contribute to early medical education? A BEME systematic reviewMed Teach200628131816627313
- HuntJBBonhamCJonesLUnderstanding the goals of service learning and community-based medical education: a systematic reviewAcad Med201186224625121169780
- FurzeJBlackLPeckKJensenGMStudent perceptions of a community engagement experience: exploration of reflections on social responsibility and professional formationPhysiother Theory Pract201127641142120946070
- AverillNJSalleeJMRobinsonJTA first-year community-based service learning elective: design, implementation, and reflectionTeach Learn Med2007191475417330999
- OlneyCALivingstonJEFischSTalamantesMABecoming better health care providers: outcomes of a primary care service-learning project in medical schoolJ Prev Interv Community2006321–213314717000606
- NUFSMCompetency Compass Available from: http://www.feinberg.northwestern.edu/Education/curriculum/principles/competencies/index.htmlAccessed October 24, 2014
- DriscollAHollandBGelmonSKerriganSA case study assessment model for evaluating the impact of service-learning on students, faculty, institutions and communitiesMich J Community Serv Learn199632231