Abstract
Background
Turkey currently has the highest obesity prevalence among its European counterparts. 32% and 61% of the population live with obesity and overweight, respectively. Overweight and obesity are linked to non-communicable diseases that incur incremental health and economic costs. The significant public health concern warrants an assessment of the cost of obesity.
Methods
A micro-costing approach from the public payer perspective was conducted to estimate direct healthcare costs associated with ten obesity-related comorbidities (ORCs) in Turkey. Clinical practice guidelines and a systematic literature review informed ORCs and the respective cost categories. This was subsequently validated by a steering committee comprising seven experts. Seventy public sector physicians were surveyed to estimate healthcare resource use. Unit costs were derived from Social Security Institute’s Healthcare Implementation Communique. Cost items were summed to determine the annual cost per patient per ORC, which was validated by the steering committee. Medical inflation was considered in a scenario analysis that varied resource unit costs.
Results
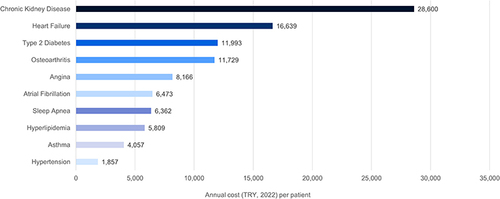
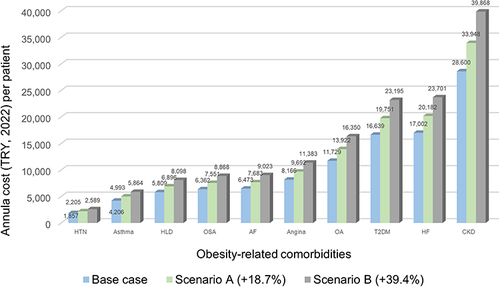
Chronic kidney disease, heart failure and type 2 diabetes are the costliest ORCs, incurring an annual cost of 28,600 TRY, 16,639 TRY and 11,993 TRY, respectively. Individuals in Turkey with any ORC triggered direct healthcare costs ranging 1857–28,600 TRY annually. Costs were driven by tertiary care resources arising from treatment-related adverse events, disease complications and inpatient procedures. In the scenario analysis, medical resource unit costs were inflated by 18.7% and 39.4%, triggering an average increase in cost across all ORCs of 1998 TRY and 4210 TRY, respectively.
Conclusion
Our findings confirm that obesity and its complications result in significant financial burden to the public healthcare system. By quantifying the burden of obesity across a comprehensive spectrum of ORCs, our study aims to support the economic case for investing in appropriate obesity interventions.
Introduction
Obesity is one of the leading risk factors that contribute to the burden of non-communicable diseases (NCD) plaguing health systems globally.Citation1,Citation2 The 2022 World Health Organisation (WHO) European Regional Obesity Report places overweight and obesity as the fourth most common risk factor for NCDs in continent.Citation3 It is also a prominent risk factor for disability and mortality, causing 7% of total years lived with disability and over 2.8 million deaths annually.Citation4,Citation5 The magnitude of the obesity problem transcends human health consequences. People who live with overweight require healthcare services more frequently and for more complicated issues. Its ramifications are also felt in the labour market where workforce participation is reduced, and on the economy where rising health expenditure on chronic conditions increases fiscal pressure.Citation6,Citation7
In Turkey, national epidemiological surveys signal a growing prevalence of obesity which has surpassed its European neighbours and rival that of the United States of America (USA).Citation4,Citation8,Citation9 61% of the Turkish population are living with overweight, and approximately one in three (32.1%) are living with obesity.Citation3,Citation8 The prevalence burgeoned alarmingly over the last few decades from 18.8% in 1990,Citation9 signalling a pressing need for measures to address obesity and its associated complications.
Obesity is a systemic disease with significant cardiometabolic effects that affect multiple organ systems. In patients with obesity, insulin resistance precedes the development of Type 2 Diabetes Mellitus (T2DM). It is a well-established association and around 80% of patients with T2DM are living with obesity.Citation10 In Turkey, a multicentre study conducted in Marmara reported that the prevalence of prediabetes was 15.2% in obese adolescents.Citation11 Obesity has also been directly correlated with non-alcoholic fatty liver disease, congestive heart failure,Citation12 poor respiratory function and airway hyperresponsiveness,Citation13 hypertension,Citation14 and vascular disease.Citation15 A study evaluating Turkish adults diagnosed with coronary heart disease, found that the prevalence of diabetes among obese women is almost three times that of non-obese women.Citation16 The same study also determined that a higher body-mass index (BMI) was significantly related to increases in plasma cholesterol and hypertension.Citation16 The burden of obesity and the chronic diseases it causes are significant. In 2012, NCDs accounted for 87.5% of all deaths among people aged 30–70 years in Turkey – of these, 36.6% were due to cardiovascular diseases (CVD), 7% to chronic respiratory diseases and 5.8% to diabetes.Citation17 In 2011, per capita healthcare expenditure in Turkey was US$1160, and 70% of the government’s total health expenditure was funnelled to addressing NCDs alone.Citation18 Turkish researchers also estimated that obesity-related comorbidities (ORCs) accounted for 7.4% of total disability-adjusted life years (DALYs), translating to an obesity-related economic burden of over US$17 million in 2015, which constituted 2.45% of the nation’s gross domestic product.Citation19
In response to the escalating public health problem, precautions for preventing obesity have been included in the Ministry of Health’s strategies for the 11th Development Plan of the Presidency (2019–2023).Citation20,Citation21 As healthcare authorities in Turkey work to develop policies that address the burgeoning obesity epidemic, timely information about the health and economic effects at the population level is needed. To date, there is a critical lack of recent and comprehensive economic evidence on this topic to guide decisions about resource allocation and appropriate interventions.Citation19 This study aims to assess the burden of obesity across a full spectrum of ORCs and deliver health system insights for policy and decision-makers in Turkey.
Methods
In this study, we sought to evaluate all fixed and variable annual costs incurred by the average patient living with obesity in Turkey across the care continuum of ten ORCs. The ten ORCs encompass an extensive range of organ systems (metabolic, cardiovascular, respiratory, musculoskeletal, and renal), and provide comprehensive quantification of the burden of obesity for our study. These comorbidities were also aligned with those examined in a UK study assessing the effect of weight loss on obesity-related outcomes.Citation22 Epidemiologic studies confirm that high BMI is a risk factor for specific diseases. This includes T2DM,Citation23–25 cardiovascular disease, which include heart failure, hypertension, angina, atrial fibrillation and hyperlipidemia,Citation23–27 sleep apnea,Citation23,Citation25,Citation28 osteoarthritis,Citation25,Citation29,Citation30 asthma,Citation23,Citation25 and chronic kidney disease (CKD).Citation23,Citation25
To overcome limited real-world data, a survey-based micro-costing analysis was considered the most detailed and feasible approach for estimating the cost of ORCs in Turkey. The methodology utilizes healthcare resource use (HCRU) information provided by public sector physicians and unit cost data of every resource consumed in the treatment of a particular patient with any ORC to generate detailed estimates of overall costs.Citation31,Citation32 The principles of conducting micro-costing studies are well established in literature despite the lack of a defined consensus standard. To date, published micro-costing analyses have utilized a wide range of resource use and price data collection methods with varying degrees of precision – data can be collected manually or electronically, prospectively or retrospectively, from a variety of sources that include surveys, patient records, billing systems, or trial data.Citation31–35
Our study considered costs from the public payer’s perspective across a full spectrum of primary, secondary and tertiary care settings. In the absence of a real-world data source for reliably extracting cost and resource use across all care settings in the Turkish public health sector,Citation36,Citation37 we conducted a micro-costing assessment using a retrospective four-tiered approach.Citation38,Citation39
First, ‘cost categories’ were identified for each ORC (ie, HCRU categories and respective itemized resources).
Second, as described by Drummond et al,Citation39 HCRU categories were quantified by assigned a cost value to each itemized resource. This was done by weighting utilization against the corresponding unit prices or relevant quantities Seventy public sector clinicians in Turkey were surveyed to provide HCRU estimates.
Third, the overall annual cost incurred by an average obese patient with an ORC was estimated by aggregating all cost categories.
Finally, aggregated costs were subject to external validation by comparisons against published estimates in literature. The aggregated costs were also reviewed by a steering committee comprising a local academic physician and a panel of six independent industry experts. A scenario analysis was also conducted to estimate known uncertainties around Turkey’s medical cost inflationary pressures.
Identification of Cost Categories
The cost categories evaluated in our micro-costing study were informed by a systematic process described in a recently published study conducted in Saudi Arabia examining the national clinical and economic burden of obesity.Citation35 Treatment pathways, which include screening, diagnosis, treatment, adverse events and complications, were triangulated via a systematic literature review.Citation35 To determine the types of healthcare cost parameters relevant to each ORC, search terms related to the ORCs as well as ‘systematic review or ‘clinical guidelines’ were used to extract references in Google Scholar and PubMed.Citation35 A steering committee comprising a panel of six industry experts and a Turkish academic physician provided additional external validation. Cost categories included in the final analysis received were unanimously agreed upon by the steering committee.
The following cost categories were considered in the micro-costing analysis for each ORC: diagnostic tests conducted per patient, scheduled outpatient visits per patient per year, pharmaceutical treatments prescribed (plus frequency, dose and duration), devices and/or consumables required for disease management per patient per year, monitoring tests required per patient per year, treatment-related adverse events (TRAE) and disease complications per patient per year. TRAE and disease complication costs considered the following care resources: outpatient visits, emergency room (ER) visits, inpatient hospitalisation, intensive care unit (ICU) care, and inpatient procedures required per patient per year.
Quantification of Cost Categories
Cost categories were compiled in a standard Excel-based template and administered via interviewer-assisted online surveys to clinical specialists between April and July 2022. Seventy specialists practicing at the consultant level in Turkey’s public health sector were surveyed to provide HCRU estimates (). The surveys were internally validated and conducted in line with ESOMAR and vendor quality guidelines. Clinician respondents were recruited by third-party agents. All respondents were screened for at least three years of specialist experience and had to have been responsible for the care of at least ten relevant patients each month. Respondents were also asked to provide informed consent for anonymized data to be included in publications and were counselled that any adverse events or product complaints reports would be raised to the relevant company. All survey participants were screened to ensure fulfillment of inclusion criteria. All survey respondents worked at a public hospital located in one of the following 19 Turkish cities – Istanbul, Adana, Gaziantep, Izmir, Konya, Malatya, Mersin, Samsun, Batman, Sanliurfa, Tekirdağ, Tokat, Ankara, Antalya, Bursa, Denizli, Edirne, Erzurum and Eskisehir.
Table 1 Specialist Clinicians Who Contributed HCRU Estimates to the Micro-Costing Analysis
Unit costs for each cost item were derived from the most updated Healthcare Implementation Communique (Sağlık Uygulama Tebliği) at the time of data collection.Citation40 The legislation is promulgated by Turkey’s Social Security Institute and details the pricing regulations, fees and payment terms for all health services provided in Turkey’s health sector. These include pharmaceuticals, medical devices, as well as outpatient and inpatient services. Data were extracted from the latest Communique at the time of study implementation, dated 28 April 2021,Citation40 and all relevant costs incurred by the public payer were included in the analysis. In keeping with the study’s public payer perspective, private sector and out-of-pocket costs were excluded from the calculations. Targeted secondary research was also conducted to validate the cost data, where required.
Cost Calculations
Costs were assessed in 2022 Turkish Lira (TRY) and a foreign exchange rate of 1 TRY = 0.057 USD was used when cost estimates were compared across countries. Each cost item within the respective cost categories was calculated separately. For all items except pharmaceutical treatments, the annual cost per patient per cost item was calculated as:
Annual cost per cost item = Unit cost x Number of healthcare resource units utilized per year x Percentage (%) of patients utilizing the healthcare resource
The annual cost for each pharmaceutical treatment per patient was calculated as:
The annual cost for each pharmaceutical treatment = Percentage (%) of patients receiving treatment x Unit cost of treatment x Average consumption per day x 30 days x 12 months
The total annual cost per patient per cost category was then calculated by summing all cost items. Finally, the total cost per patient per ORC per year was determined by summing all cost categories. Cost data are presented as mean values in TRY, or a percentage of total costs.
Data Validation
Annual cost estimates were presented to the expert steering committee for final validation. All data included in the analysis had to be unanimously agreed upon by the steering committee. The expert steering committee comprised of a senior public sector physician academic and an independent panel of 6 industry experts. The steering committee also validated unit cost estimates and assessed cost drivers. Targeted literature review was additionally conducted, to corroborate cost data, where required.
Scenario Analysis
A scenario analysis was conducted to account for the global inflationary pressures that have increased overall costs in the Turkish health sector. Rising medical care costs have presented as a major challenge to efforts by the Turkish government to ensure fiscal sustainability of the health system. In 2022, the health inflation rate soared to 122.2%,Citation41 driven by several underlying issues: Population birth rates, per-capita income, currency fluctuations, rising pharmaceutical and medical technology costs as a result of advances, and increased patient demand for services.
Prices of medicinal products in Turkey are regulated by provisions of the Decision on Pricing of Medicinal Products for Human Use (Decision).Citation42 The provisions stipulate pricing regulations that include external reference prices, public price limits, the Euro-Turkish Lira drug price exchange rate and pharmacy profit rates.Citation42,Citation43 Despite numerous cost containment strategies however, public drug spending continues to rise, with nominal spending reportedly increasing by 10% annually from 2012 to 2014.Citation44 Reasons include the expansion of Turkey’s universal health coverage to improve patient access, the penetration of high-cost drugs into the market, and changes to the Euro-Turkish lira drug exchange rate in response to fluctuating market exchange rates.Citation44
As our survey findings provided cost inputs accurate to a single time point in 2022, we accounted for the uncertainties associated with rising health care costs by varying all resource unit costs by +18.7% (the average inflation rate between 2018 and 2021;Citation41 scenario A) and +39.4% (the average inflation rate between 2018 and 2022;Citation41 scenario B). This was done to reflect the realities of rapidly rising medical service, pharmaceutical and medical material fees incurred by the public payer.
Results
Total Annual Costs for Obesity-Related Complications
Individuals in Turkey with any single ORC incurred average annual healthcare costs ranging from 1857 TRY for hypertension to 28,600 TRY for CKD per patient (). CKD, heart failure and T2DM were the top 3 most costly complications, incurring an annual cost of 28,600 TRY, 16,639 TRY and 11,993 TRY, respectively. Hypertension, asthma, and hyperlipidaemia were the least costly ORCs, incurring one-tenth to one-fifth of the cost of the most expensive complications ().
Cost Drivers
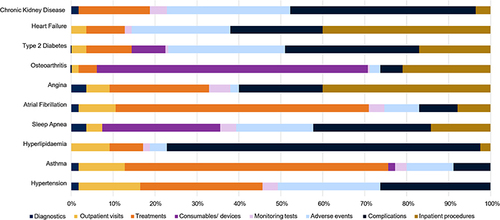
To understand variations in costs and cost drivers across the various ORCs, we explored how each HCRU cost category contributed to the total annual healthcare costs for each ORC ( and ).
Table 2 Cost Categories and Costs per Patient per Year (TRY, 2022) Associated with Each Obesity-Related Comorbidity
Across all ORCs, the proportion and absolute cost of each cost category was heterogenous. Key cost drivers for the top 3 most costly ORCs (CKD, heart failure, T2DM) were treatment-related adverse events, complications, and inpatient procedures where there was relatively higher utilization of tertiary care resources (ie, emergency department, inpatient and ICU services). Costs associated with complications was the most significant contributor to CKD costs (44.2% of total cost or 12,642 TRY). This was primarily driven by the demand on ICU resources, which contributed to 81.6% of the total cost of CKD-related complications. Similarly, the cost incurred from complications (32.0%) was the main driver of annual T2DM costs. The annual cost burden of heart failure, however, was primarily due to the cost and HCRU demands of costly inpatient procedures, including coronary artery bypass surgery and heart valve repair or replacement.
Scenario Analysis
We explored the impact of medical inflation in scenario analyses by varying unit costs of all medical resources. Costs were varied by +18.7% (scenario A) and +39.4% (scenario B) to reflect the impact of rapidly rising medical service, pharmaceutical and medical material fees incurred by the public payer. The average increase in cost across all ORCs was 1998 TRY and 4210 TRY in scenario A and scenario B, respectively ().
Discussion
Turkey’s healthcare system has been a primary focus of its economic and social reforms in the past two decades. As societies age and lifestyles evolve, the emergence of new care concerns create competition amongst healthcare priorities while fiscal constraints limit the resources available to address these challenges equally. Turkey currently has the highest obesity prevalence among its European counterpartsCitation4 and studies have estimated that obesity and its related comorbidities account for approximately half of total government spending on healthcare.Citation19,Citation45 Our results confirm and quantify the burden of obesity on health and the Turkish economy, further highlighting areas of prominent spend across the obesity care continuum.
The annual economic burden of ORCs was primarily driven by costs associated with complications, treatment-related adverse events, inpatient procedures, and pharmaceutical treatments. This pattern of cost contribution was consistently observed for 8 ORCs – asthma, hypertension, hyperlipidemia, CKD, T2DM, heart failure, angina, and atrial fibrillation. The management of disease complications and treatment-related adverse events, which involve inpatient, ICU and ER services, place substantial demands on hospital resources. In 2020, the Turkish Statistical Institute reported that 49.4% of total public health expenditure arose from care service provision and consumable spend by hospitals, which constituted the largest share amongst all health service providers.Citation45 The association of obesity with specific diseases is well establishedCitation11–13,Citation15,Citation16,Citation18,Citation19,Citation28 and its impact on increased advanced care resource utilization as a result of progressive disability, morbidity and mortality is prominent.
Our results also demonstrate the impact of rising medical inflation on the public payer’s fiscal burden. Turkey’s universal health insurance (Social Security Insurance (SSI)) is the single public payer of pharmaceuticals, medical materials, and health services in Turkey. In 2013, it financed nearly 74% of total drug spending.Citation44 Despite concerted price control strategies and currency control measures, nominal public drug spending continued to rise by 10% annually from 2012 to 2014,Citation44 with overall health inflation reaching a significant peak in 2022. The burden of ORCs is significant and rendered more substantive in the face of surging medical inflation.
Overall, healthcare cost estimates derived from our study were similar to published estimates from other countries with a similar GDP per capita and healthcare expenditure. The annual per-person healthcare cost for CKD was estimated to be 28,600 TRY (1630 USD); costs equivalent to 2535 USD was reported in a study in Spain in 2019.Citation46 The Spanish study was similarly conducted from the public health system perspective and representative of the average annual cost of CKD, across all severity stages.Citation46 Our annual cost estimates for T2DM were 12,098 TRY (690 USD), which is in in line with a local study published earlier in 2015.Citation47 The 2015 Turkish publication utilized HCRU data from the International Diabetes Management Practice Study,Citation48 and authors estimated an annual cost of T2DM per patient of 13,048 TRY (2015 TRY adjusted to 2022 TRY; 744 USD). The cost for heart failure (16,639 TRY; 948 USD) was also observed to be similar to costs previously observed in PolandCitation49 (815 EUR in 2012; 994 EUR/ 1035 USD in 2022) and Portugal (1159 EUR in 2014; 1389 EUR/ 1447 USD in 2022).Citation50 Both Polish and Portuguese studies were similarly undertaken from the public health system perspective and representative of chronic heart failure patients resource demands across the full spectrum of class I–IV. The Portuguese study also considered indirect costs associated early exit from the workforce and absenteeism as a result of heart failure.
Policies that address underlying risk factors such as obesity can help prevent the occurrence of chronic diseases, while reducing healthcare costs in the long-term.Citation51 However, the high upfront costs of preventative health interventions and the intangibility of future outcomes often mean that these considerations do not receive adequate attention in many countries. Currently, less than 3% of health spending in Organisation for Economic Co-operation and Development (OECD) countries is allocated to public health prevention activities.Citation52 By quantifying the burden of obesity, we hope to strengthen the economic argument for investing in obesity-related prevention and interventions.
Limitations
The micro-costing methodology and data sources used in this study to determine detailed healthcare costs for the various ORCs have been described as a reasonable approach for settings where direct HCRU or cost data are not available.Citation34,Citation53 However, while micro-costing in this study was based on an extensive data collection exercise, comprising a nationwide survey with exacting inclusion criteria for participating physician respondents, it should be noted that the costs derived remain estimates. In the absence of publicly available and comprehensive real-world data sources in Turkey, these findings overcome a key evidence gap, and demonstrate the burden of obesity and its complications.
Second, this study provides an understanding of the healthcare burden of obesity in Turkey but at an individual ORC level, which may suggest that an obese patient will only experience one ORC. In reality however, an obese patient is likely to experience at least two ORCs on average in their lifetime,Citation54,Citation55 where additional costs or care synergies may need to be considered to accurately reflect actual burden. Notwithstanding, findings at an individual ORC level provides key insights to understanding the variations in cost burden across the various comorbidities.
Finally, it should be acknowledged that the study provides a conservative estimate, wherein only direct costs are considered and indirect costs that arise from productivity loss and/or early labour force exit have not been included in the analysis.
Conclusion
The economic burden of ORCs on Turkish health system is substantial and our estimates suggest that significant cost savings may be realised by delaying or preventing the occurrence of ORCs.
Further, our study’s bottom-up micro-costing analysis addresses an evidence gap in Turkey and should be leveraged to drive efforts to optimise existing technologies and health information platforms that overcome current limitations around real-world patient data. A robust and reliable patient registry will facilitate data-driven decisions and enable better integrated care plans for the disease and its complications.
Our results prompt an urgent call to action for health authorities and organizations operating in the health sector to consider how investments can be optimized to prevent or delay obesity and its associated complications, thereby reducing costs to the public health system.
Ethics Declarations
The study was conducted according to ESOMAR guidelines, and informed consent was required for participation in surveys. Before commencement of the survey, participants were asked to provide consent for anonymized data to be included in publications and were advised that any adverse events or product complaints raised would be reported to the relevant company. In addition, given that no subject-identifiable data were generated, and the surveillance activities implied no risk or burden for any individuals, the study authors judged that no additional ethical review board permission was required. The study was performed in accordance with the Declaration of Helsinki (1964).
Disclosure
DGY declares receiving support from Novo Nordisk, Sanofi, Boehringer Ingelheim and Amgen to speak at scientific events, and honoraria from Novo Nordisk and Sanofi for attending advisory boards. BG, ESY and AB are employed by Novo Nordisk. OA reports consultant for Novo Nordisk, during the conduct of the study. KL and AG report Ipsos project fees from Novo Nordisk, during the conduct of the study. The authors report no other conflicts of interest in this work.
Acknowledgments
The authors would like to thank all physicians who have provided data for the study. The study team would also like to thank Sharanya J Jois and Malvin Kang for their assistance with data cleaning for the analyses.
Data Sharing Statement
All supporting data for the analysis are presented in this manuscript. The survey template is available from the corresponding author upon reasonable request.
Additional information
Funding
References
- Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9(1):88. doi:10.1186/1471-2458-9-88
- Poirier P, Giles TD, Bray GA, et al. Obesity and Cardiovascular Disease: pathophysiology, Evaluation, and Effect of Weight Loss. Circulation. 2006;113(6):898–918. doi:10.1161/CIRCULATIONAHA.106.171016
- Organization WH. Regional Office for Europe. WHO European Regional Obesity Report 2022. World Health Organization. Regional Office for Europe. 2022; Available from: https://apps.who.int/iris/handle/10665/353747. Accessed February 29, 2024.
- World Health Organisation. WHO European Regional Obesity Report 2022; 2022. Available from: https://apps.who.int/iris/handle/10665/353747. Accessed February 29, 2024.
- World Health Organisation. Obesity. World Health Organisation; 2021. Available from: https://www.who.int/features/factfiles/obesity/en/. Accessed February 29, 2024.
- Klarenbach S, Padwal R, Chuck A, Jacobs P. Population-based analysis of obesity and workforce participation. Obesity. 2006;14(5):920–927. doi:10.1038/oby.2006.106
- Michele C, Sabine V. The Heavy Burden of Obesity: the Economics of Prevention. OECD Library. 2019. doi:10.1787/67450d67-en
- Işeri A, Arslan N. Obesity in adults in Turkey: age and regional effects. European Journal of Public Health. 2009;19(1):91–94. doi:10.1093/eurpub/ckn107
- Erem C. Prevalence of Overweight and Obesity in Turkey. IJC Metabolic & Endocrine. 2015;8:38–41. doi:10.1016/j.ijcme.2015.07.002
- Bloomgarden ZT. American Diabetes Association Annual Meeting, 1999: diabetes and obesity. Diabetes Care. 2000;23(1):118–124. doi:10.2337/diacare.23.1.118
- Babaoğlu K, Hatun S, Arslanoğlu I. Evaluation of glucose intolerance in adolescents relative to adults with type 2 diabetes mellitus. J Pediatr Endocrinol Metab. 2006;19(11):1319–1326. doi:10.1515/JPEM.2006.19.11.1319
- Ozkol M, Ersoy B, Kasirga E, Taneli F, Bostanci IE, Ozhan B. Metabolic predictors for early identification of fatty liver using Doppler and B-mode ultrasonography in overweight and obese adolescents. Eur J Pediatr. 2010;169(11):1345–1352. doi:10.1007/s00431-010-1227-2
- Ulger Z, Demir E, Tanaç R. The effect of childhood obesity on respiratory function tests and airway hyperresponsiveness. Turk J Pediatr. 2006;48(1):43–50.
- Hall JE, Do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-Induced Hypertension. Circulation Research. 2015;116(6):991–1006. doi:10.1161/CIRCRESAHA.116.305697
- Yilmazer MM, Tavli V, Carti OU. Cardiovascular risk factors and noninvasive assessment of arterial structure and function in obese Turkish children. Eur J Pediatr. 2010;169(10):1241–1248. doi:10.1007/s00431-010-1216-5
- Onat A, Şenocak M. Obesity in Turkish adults: prevalence, validity as coronary risk factor, and interrelation with other risk factors. International Journal of Angiology. 1995;4(2):94–98. doi:10.1007/BF02043625
- Turkish Statistical Institute. Causes of Death Statistics, 2010, 2011 and 2012. 2013 Available from: https://data.tuik.gov.tr/Bulten/Index?p=Causes-of-Death-Statistics-2010,-2011-and-2012-15847. Accessed February 29, 2024.
- Yuksel H. Social Determinants of Obesity: the Example of Turkey. SDU Faculty of Arts and Sciences Journal of Social Sciences. 2019;48:15–33.
- Yigit A, Yigit V. Economic Burden of Obesity-Related Comorbidities in Turkey. Gumushane universitesi Saglık Bilimleri Dergisi. 2019;8(3):223–230.
- Fahrettin KOCA. 2019-2023 dönemi Sağlık Bakanlığı Stratejik planı. Statejik Yönetim. Available from: http://www.sp.gov.tr/tr/stratejik-plan/s/1652/Saglik+Bakanligi+2019-2023. Accessed February 29, 2024.
- Official Gazette. On Birinci Kalkınma Planı 2019-2023; 2019. Available from: https://www.resmigazete.gov.tr/eskiler/2019/07/20190723M1-1-1.pdf. Accessed February 29, 2024.
- Haase CL, Lopes S, Olsen AH, Satylganova A, Schnecke V, McEwan P. Weight loss and risk reduction of obesity-related outcomes in 0.5 million people: evidence from a UK primary care database. Int J Obes. 2021;45(6):1249–1258. doi:10.1038/s41366-021-00788-4
- Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–1529. doi:10.1001/jama.282.16.1523
- Singh GM, Danaei G, Farzadfar F, et al. The Age-Specific Quantitative Effects of Metabolic Risk Factors on Cardiovascular Diseases and Diabetes: a Pooled Analysis. PLoS One. 2013;8(7):e65174. doi:10.1371/journal.pone.0065174
- GBD 2015 Obesity Collaborators. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Eng J Med. 2017;377(1):13–27. doi:10.1056/NEJMoa1614362
- Collaboration TERF. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. The Lancet. 2011;377(9771):1085–1095. doi:10.1016/S0140-6736(11)60105-0
- Khan SS, Ning H, Wilkins JT, et al. Association of Body Mass Index With Lifetime Risk of Cardiovascular Disease and Compression of Morbidity. JAMA Cardiol. 2018;3(4):280–287. doi:10.1001/jamacardio.2018.0022
- Li C, Ford ES, Zhao G, Croft JB, Balluz LS, Mokdad AH. Prevalence of self-reported clinically diagnosed sleep apnea according to obesity status in men and women: national Health and Nutrition Examination Survey, 2005-2006. Prev Med. 2010;51(1):18–23. doi:10.1016/j.ypmed.2010.03.016
- Jiang L, Tian W, Wang Y, et al. Body mass index and susceptibility to knee osteoarthritis: a systematic review and meta-analysis. Joint Bone Spine. 2012;79(3):291–297. doi:10.1016/j.jbspin.2011.05.015
- Jiang L, Rong J, Wang Y, et al. The relationship between body mass index and Hip osteoarthritis: a systematic review and meta-analysis. Joint Bone Spine. 2011;78(2):150–155. doi:10.1016/j.jbspin.2010.04.011
- Chapel JM, Wang G. Understanding cost data collection tools to improve economic evaluations of health interventions. Stroke and Vascular Neurology. 2019;4(4):214–222. doi:10.1136/svn-2019-000301
- Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-Effectiveness in Health and Medicine. Oxford University Press; 1996.
- Frick KD. Micro-Costing Quantity Data Collection Methods. Med Care. 2009;47(7 Suppl 1):S76–S81. doi:10.1097/MLR.0b013e31819bc064
- Micro-costing in health and medicine: a critical appraisal | Health Economics Review | Full Text. Available from: https://healtheconomicsreview.biomedcentral.com/articles/10.1186/s13561-020-00298-5. Accessed February 29, 2024.
- Alqahtani SA, Al-Omar HA, Alshehri A, et al. Obesity Burden and Impact of Weight Loss in Saudi Arabia: a Modelling Study. Adv Ther. 2023;40(3):1114–1128. doi:10.1007/s12325-022-02415-8
- Dogac A, Yuksel M, Avcl A, et al. Electronic Health Record Interoperability as Realized in the Turkish Health Information System. Methods Inf Med. 2011;50(02):140–149. doi:10.3414/ME10-01-0022
- Kose I, Rayner J, Birinci S, et al. Adoption rates of electronic health records in Turkish Hospitals and the relation with hospital sizes. BMC Health Services Research. 2020;20(1):967. doi:10.1186/s12913-020-05767-5
- Špacírová Z, Epstein D, García-Mochón L, Rovira J, Labry lima A, Espín J. A general framework for classifying costing methods for economic evaluation of health care. Eur J Health Econ. 2020;21(4):529–542. doi:10.1007/s10198-019-01157-9
- Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes. Oxford University Press; 2015.
- Executive and Administrative Division. T.C. Resmî Gazete. Presidency of the Republic of Turkey Official Gazette; 2021. Available from: https://www.resmigazete.gov.tr/eskiler/2021/04/20210428M1.pdf. Accessed February 29, 2024.
- Türkiye’nin sağlık enflasyonu hesaplandı; yüzde 122,17 arttı. DHA | demirören Haber Ajansı; 2023. Available from: https://www.dha.com.tr/ekonomi/turkiyenin-saglik-enflasyonu-hesaplandi-yuzde-122-17-artti-2209673. Accessed February 29, 2024.
- Cumhurbaşkani Karari. Vol. 38. p. 20221012–6. Available from: https://www.resmigazete.gov.tr/eskiler/2022/10/20221012-6.pdf. Accessed February 29, 2024.
- 25 Ağustos 2022 Tarihli ve 31934 Sayılı Resmî Gazete. Available from: https://www.resmigazete.gov.tr/fihrist?tarih=2022-08-25&mukerrer=1). Accessed February 29, 2024.
- Gürsoy K. An Analysis of Public Pharmaceutical Policy, Pricing and Spending in Turkey. Journal of Social Security. 2016;6(1):225–243.
- Turkish Statistical Institute. Health Expenditure Statistics, 2020. Turkish Statistical Institute; 2023. Available from: https://data.tuik.gov.tr/Bulten/Index?p=37192&dil=2. Accessed February 29, 2024.
- Escobar C, Palacios B, Aranda U, et al. Costs and healthcare utilisation of patients with chronic kidney disease in Spain. BMC Health Services Research. 2021;21(1):536. doi:10.1186/s12913-021-06566-2
- Malhan S, Schwarzbard J, Sahin T, et al. Type 2 Diabetes in Turkey – a Cost of Illness Study. Value in Health. 2016;19(7):A669. doi:10.1016/j.jval.2016.09.1857
- Chan JCN, Gagliardino JJ, Baik SH, et al. Multifaceted determinants for achieving glycemic control: the International Diabetes Management Practice Study (IDMPS). Diabetes Care. 2009;32(2):227–233. doi:10.2337/dc08-0435
- Czech M, Opolski G, Zdrojewski T, et al. The costs of heart failure in Poland from the public payer’s perspective: polish programme assessing diagnostic procedures, treatment and costs in patients with heart failure in randomly selected outpatient clinics and hospitals at different levels of care. POLKARD. 2013;71(3):224–232.
- Fiorentino F, Ascenção R, Gouveia M, et al. The Cost Of Illness Of Heart Failure In Portugal. Value in Health. 2017;20(9):A610. doi:10.1016/j.jval.2017.08.1203
- Sassi F, Hurst J. The Prevention of Lifestyle-Related Chronic Diseases: an Economic Framework. OECD Health Working Papers. 2008. doi:10.1787/243180781313
- Gmeinder M, Morgan D, Mueller M How Much Do OECD Countries Spend on Prevention? Paris: OECD Publishing; Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/how-much-do-oecd-countries-spend-on-prevention_f19e803c-en. Accessed February 29, 2024.
- OECD. Estimating expenditure by disease, age and gender under the system of health accounts (SHA) framework. 2008. Available from: https://www.oecd.org/els/health-systems/EstimatingExpenditurebyDiseaseAgeandGender_FinalReport.pdf. Accessed February 29, 2024.
- Lim Y, Boster J. Obesity and Comorbid Conditions. Treasure Island (FL): StatPearls Publishing; 2022. Available from: http://www.ncbi.nlm.nih.gov/books/NBK574535/. Accessed February 29, 2024.
- Pi-Sunyer FX. Comorbidities of overweight and obesity: current evidence and research issues. Med Sci Sports Exerc. 1999;31(11 Suppl):S602–608. doi:10.1097/00005768-199911001-00019