Abstract
Background
Serum trace elements and oxidative stress factors are related to diabetic microvascular complications. The study was to investigate the complex relationship between trace elements, oxidative stress factors, and the severity of microvascular complications of diabetes in older adults.
Methods
The present study included patients with or without type 2 diabetes, and blood glucose, blood lipids, trace elements (iron, magnesium, zinc), oxidative stress factors (malondialdehyde (MDA), nitric oxide (NO), superoxide dismutase (SOD), and total antioxidant capacity (T-AOC)) were evaluated. Risk factors for the severity of diabetic microvascular complications in older adults with diabetes were also estimated.
Results
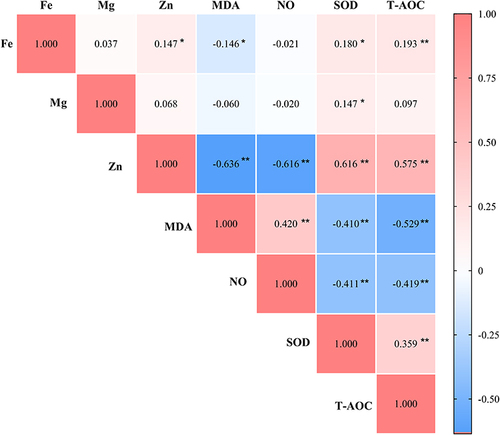
There were statistically significant differences in fasting blood glucose (FBG), triglycerides (TG), low density lipoprotein (LDL), glycated hemoglobin (HbAlc), MDA, NO, SOD, T-AOC, magnesium, and zinc between the two groups (P<0.05). Iron (rZinc = 0.147, rSOD = 0.180, rT-AOC = 0.193, P < 0.05) was positively correlated with zinc, SOD and T-AOC. Iron was negatively correlated with MDA (rMDA = −0.146, P < 0.05). Magnesium was positively correlated with SOD (rMagnesium = 0.147, P < 0.05). Zinc (rSOD = 0.616, rT-AOC = 0.575, P < 0.01) was positively correlated with SOD and T-AOC. Zinc (rMDA =−0.636, rNO=−0.616, P<0.01) was positively correlated with MDA and negatively correlated with NO. The course of disease (18.653, [5.726; 60.764], P <0.01), FBG (1.265, [1.059; 1.511], P <0.05), HbAlc (1.545, [1.431; 1.680], P <0.01), MDA (2.989, [1.900; 4.702], P <0.01) were risk factor for the severity of diabetic microvascular complications. Zinc (0.680, [0.503; 0.919], P < 0.05) and SOD (0.820, [0.698; 0.964], P < 0.05) were protective factors for the severity of diabetic microvascular complications.
Conclusion
Serum trace elements are related to oxidative stress levels in older adults with type 2 diabetes. The more stable trace element in older adults with diabetes, the lower the oxidative stress and the fewer microvascular complications of diabetes.
Introduction
Diabetes mellitus (DM) is common endocrine system chronic disease, and its microvascular complications include diabetic peripheral vascular disease (DPVD), diabetic kidney disease (DN), and diabetic peripheral neuropathy (DPN).Citation1 Diabetes and its complications can not only greatly reduce the quality of life of patients but also cause great pain to their family and an enormous burden on economy, society, and healthcare systems.Citation2 In China, the prevalence of diabetes in the elderly (≥60 years) was 20.4%, and the total number of elderly diabetes was estimated to exceed 30 million.Citation3 Diabetes in the elderly is mainly type 2 diabetes mellitus (T2DM), which has the characteristics of atypical clinical manifestations, high prevalence, hazard, and large heterogeneity. When elderly diabetes is discovered, there are already related complications, which seriously affect the prognosis.Citation4
Several studies have shown that serum trace elements are closely related to the occurrence and development of T2DM and its complications in the elderly.Citation5 Serum iron overload causes cell damage, insulin resistance and glucose and lipid metabolism disorders, and accelerates the occurrence of diabetes and its complications.Citation6 Persistent hyperglycemia in diabetes promotes oxidative stress, inhibits antioxidants, and leads to diabetic vascular damage.Citation7 Trace elements are closely related to oxidative stress. Zinc and magnesium are important antioxidants and key components of many antioxidant enzymes.Citation8 Iron induces oxidative stress and produces a large amount of oxygen free radicals.Citation9
In recent years, many studies have reported that trace elements are closely related to oxidative stress and play an important role in the occurrence and development of diabetes and its related chronic complications. However, most of these studies were small and only investigated a single microvascular complication.Citation10–13 Few studies have evaluated the correlation of serum trace elements with oxidative stress and the relationship with the severity of complications in elderly patients with type 2 diabetes, especially in Asian populations. Our study covered three diabetic microvascular complications and had a larger sample size than most previous studies. Therefore, this study intends to analyze the correlation between trace elements, oxidative stress factors, and the severity of microvascular complications of diabetes in older adults, thereby providing evidence for trace elements in the treatment of diabetes and its complications in the older adults.
Methods
Participants
We included all patients hospitalized in the Geriatrics Department of the First Hospital of Jilin University between January 2019 and September 2020. All patients were hospitalized for uncontrolled hyperglycemia or evaluated for diabetes complications. Both the T2DM group and the control group were ≥60 years old.
The diagnosis of diabetes adopts the World Health Organization’s 2006 criteria:Citation14 (1) typical symptoms, random blood glucose ≥11.1 mmol/L; (2) fasting blood glucose ≥7.0 mmol/L; (3) oral glucose tolerance test, 2-hour blood glucose ≥11.1 mmol/L. Participants without typical symptoms should repeat the blood glucose test on another day. Patients meeting any one of the above criteria were diagnosed with diabetes.
Diagnostic Criteria of Diabetic Microvascular Complications
All the participants were diagnosed at the time of hospital discharge.
Diabetic peripheral vascular disease (DPV)Citation15 was diagnosed by color Doppler ultrasonography of bilateral lower extremity vessels or neck and brain vessels. In addition, there are symptoms of lower extremity pain, cool skin, intermittent claudication, dizziness, and headache.
The diagnosis of diabetic peripheral neuropathy (DPN)Citation16 was based on the following: 1) History of diabetes. 2) For those with clinical symptoms (pain, numbness, and paresthesia), any one of the following five items (ankle reflex, acupuncture pain, vibration, pressure, and temperature) is abnormal. 3) For those without clinical symptoms, any two of the following five items (ankle reflex, pinprick pain, vibration, pressure, and temperature) are abnormal. Neuropathy caused by other factors was excluded when DPN was diagnosed.
Diabetic kidney disease (DKD)Citation17 was diagnosed by urine albumin/creatinine ratio (UACR) and serum creatinine levels. All patients were asked to provide urine samples for 3 times. DKD was diagnosed if the UACR was twice above 30 mg/g, or if an abnormally elevated serum creatinine level was detected. At the same time, CKD caused by hypertension or other diseases was excluded.
The T2DM group was divided into no complication group, one complication group, two complication group, and three complication group according to the degree of microvascular complications.
Study Design
Medical histories were obtained for all patients, including details of height, weight, and waist circumference. We also obtained iron, magnesium, zinc, malondialdehyde (MDA), nitric oxide (NO), superoxide dismutase (SOD), total antioxidant capacity (T-AOC), fasting blood glucose (FBG), glycosylated hemoglobin (HbAlc), cholesterol lipid (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL), and high-density lipoprotein cholesterol (HDL).
Iron level was assayed by the ferrozine method (BSBE, China). Magnesium was assayed by the xylene blue method (LEADMAN, China). Zinc was assayed by PAPS chromogenic reagent method (BSBE, China). FBG was assayed by glucose oxidase method (LEADMAN, China), and HbAlc was assayed by HPLC method (Bio-Rad, USA). TC and TG were assayed by CHOD-PAP method (Beckman Coulter, USA). LDL and HDL were assayed by the direct method-catalase clearance method (Beckman Coulter, USA). MDA was assayed by the thiobarbituric acid colorimetric method (TBA method) (Jiancheng Bio, China). NO was assayed by the nitrate reductase method (Jiancheng Bio, China). SOD was assayed by the nitrite formation method (WST method) (Jiancheng Bio, China). T-AOC was assayed by chemical colorimetry (Jiancheng Bio, China). Test methods for oxidative stress factors were included in the supplementary file.
We initially compared clinical characteristics, trace element, and oxidative stress levels in patients with and without diabetes. We also compared serum trace element and oxidative stress levels in patients with different numbers of microvascular complications. We also performed correlation analysis to analyze the relationship between trace elements and oxidative stress levels. We also compared the characteristics of patients with and without microvascular complications. A logistic regression analysis was further performed to analyze the role of trace elements and oxidative stress as independent risk factors for microvascular complications.
Statistical Methods
SPSS 24.0 (IBM, USA) was used to analyze the data. Normally distributed data were expressed as mean ± standard deviation (SD). Non-normally distributed data were expressed as median and interquartile range. Count data were expressed as rate or composition ratio. The t-test or rank-sum test was used to compare the biochemical levels, trace elements, and oxidative stress levels between the two groups. One-way analysis of variance (ANOVA) or Kruskal–Wallis H rank sum test was used to compare the biochemical levels, trace elements, and oxidative stress levels of complications of different severity. The chi-square test was used to compare proportions between groups. Spearman test was used to analyze the correlation between serum trace elements and oxidative stress levels in elderly diabetic patients. Univariate logistic analysis was used to analyze the correlation between biochemical levels, trace elements, oxidative stress levels, and the severity of microvascular complications. Multivariate ordinal logistic analysis was used to determine the risk factors for the severity of microvascular complications in elderly diabetic patients. The test level of α=0.05 was used, and differences with P<0.05 were considered statistically significant.
Results
The 296 patients included 192 with T2DM and 104 without T2DM. The 192 patients with T2DM included 81 (42.2%) males and 111 (57.8%) females. Forty patients (20.9%) were free of complications. One microvascular complication occurred in 74 patients (38.5%). Two different microvascular complications occurred in 63 patients (32.8%). All three complications occurred in 15 patients (7.8%) ().
Table 1 Clinical Characteristics of Patients
Comparison of Patients with and without Diabetes
Fasting blood glucose, TG, LDL, HbAlc, MDA, NO, SOD, T-AOC, magnesium, and zinc levels were significantly different between the two groups with and without T2DM. SOD, T-AOC, magnesium, and zinc in patients with DM were significantly lower than those in patients without DM. Fasting blood glucose, TG, LDL, HbAlc, MDA, and NO in patients with DM were significantly higher than those in patients without DM ().
Table 2 Clinical Characteristics of Patients with and without T2DM
Comparison of Patients with and without Diabetic Microvascular Complications
There were significant differences in the levels of fasting blood glucose, HbAlc, MDA, NO, SOD, T-AOC, magnesium, and zinc in patients with complications of different severity (P<0.05). Patients with DMC had higher fasting blood glucose, HbAlc, MDA, NO, and lower magnesium, zinc, SOD, and T-AOC ().
Table 3 Clinical Characteristics of Patients with and without Diabetic Microvascular Complications
Association Between Trace Elements and Oxidative Stress Levels in Elderly Diabetic Patients
Iron level was significantly positively correlated with zinc (Correlation Coefficient = 0.147, P < 0.05), SOD (Correlation Coefficient = 0.180, P < 0.05), and T-AOC levels (Correlation Coefficient = 0.193, P < 0.01). Iron level was significantly negatively correlated with MDA level (Correlation Coefficient = −0.146, P < 0.05). Serum magnesium level was significantly positively correlated with SOD level (Correlation Coefficient =0.147, P < 0.05). Zinc level was significantly positively correlated with SOD (Correlation Coefficient =0.616, P < 0.01) and T-AOC level (Correlation Coefficient = 0.575, P < 0.01). Zinc level was significantly negatively correlated with MDA (Correlation Coefficient =−0.636, P < 0.01) and NO level (Correlation Coefficient =−0.616, P < 0.01) ().
Figure 1 The association between trace elements and oxidative stress levels in elderly diabetic patients Matrix heatmap showed Spearman correlation coefficient values for all study parameters. Negative correlations are blue, positive correlations are red, and white indicates no association between variables. *P<0.05, **P<0.01.
Logistic Regression Analysis of the Severity of Diabetic Microvascular Complications in Elderly Patients
Age, duration of diabetes, fasting blood glucose, LDL, HbAlc, MDA, NO, SOD, T-AOC, and zinc had an impact on the severity of diabetic microvascular complications in elderly patients (P<0.05). Gender, smoking, drinking, BMI, TC, TG, HDL, iron, magnesium had no effect on the severity of microvascular complications in elderly diabetic patients ().
Table 4 Logistic Regression Analysis of the Severity of Microvascular Complications in Elderly Diabetic Patients
Risk Factors for the Severity of Microvascular Complications in Elderly Diabetic Patients
We included factors affecting the severity of microvascular complications in elderly diabetic patients: age, duration of disease, fasting blood glucose, LDL, HbAlc, MDA, NO, SOD, T-AOC, and zinc into multivariate logistic analysis. Duration of disease, fasting blood glucose, HbAlc, MDA, SOD, zinc are the influencing factors of the severity of diabetes in the elderly. Duration of disease (18.653, [5.726; 60.764], P <0.01), fasting blood glucose (1.265, [1.059; 1.511], P <0.05), HbAlc (1.545, [1.431; 1.680], P <0.01), MDA (2.989, [1.900; 4.702], P <0.01) were risk factors for diabetes severity; zinc (0.680, [0.503; 0.919], P <0.05), SOD (0.820, [0.698; 0.964], P <0.05) were protective factors ().
Table 5 Risk Factors for the Severity of Microvascular Complications in Elderly Diabetic Patients
Discussion
Microvascular complication is one of the earliest pathological changes in diabetes and is a powerful predictor of stroke and cardiovascular disease.Citation18 Long-term hyperglycemia exposure can cause changes in vascular structure and function.Citation19 Furthermore, the synergistic effects of hypertension, dyslipidemia, smoking, and duration of diabetes play an important role in the development and progression of diabetic microvascular disease.Citation20 Diabetes, hypertension, and dyslipidemia, which often coexist in older adults.Citation21 Moreover, only a small number of older adults with diabetes fully achieve the recommended goals of glycemic, blood pressure, and dyslipidemia management. To reduce the incidence of severe hypoglycemia, older adults with diabetes should be careful when setting blood glucose goals.Citation22 In addition, Northeastern China has a higher degree of aging and low awareness of diabetes, which has increased the prevalence of diabetic microvascular complications.Citation23 This study showed that the increased incidence of microvascular complications in patients with type 2 diabetes was accompanied by an increase in duration of disease, fasting blood glucose, HbAlc, and MDA and a decrease in zinc and SOD.
However, evidence supporting the role of serum trace elements and oxidative stress as an etiological factor of diabetic microvascular complications is scarce. In this study, we found that the levels of MDA and NO in elderly patients with diabetic microvascular complications were higher than those in non-DMC patients, and the levels of SOD and T-AOC were lower than those in non-DMC patients. This is consistent with previous studies suggesting that the ability to resist oxidative stress may play an important role in the development of diabetic microvascular complications.Citation24,Citation25 The levels of MDA, lipid hydrogen peroxide, and lipid peroxide in the serum of diabetic patients increased, while the antioxidant indicators such as SOD activity and T-AOC decreased.Citation26,Citation27 MDA is a product of lipid peroxidation, which can cause cross-linking and polymerization of proteins and nucleic acids, resulting in cytotoxicity.Citation28–30 NO is one of the vasodilator factors released by vascular endothelium, which maintains the integrity and balance of endothelial cells. SOD is an important antioxidant enzyme in organisms and the main substance for scavenging free radicals. T-AOC represents and reflects the body’s antioxidant enzyme system and the sum of antioxidant substances.Citation31 The research results showed that the levels of MDA, NO, SOD, and T-AOC were different among different numbers of complications in T2DM. Patients with more complications have more severe oxidative stress and weaker antioxidant capacity.
This study showed that magnesium and zinc levels of elderly diabetic patients decreased. Social and economic conditions in older adults can adversely affect dietary choices and eating patterns.Citation32 As age increases, physiological functions decline, which affects the absorption and metabolism of trace elements.Citation33 The people in the study come from the high latitudes of China, which has a cold climate, insufficient sunlight, and a temperate monsoon climate. The population in Northeast China is highly heterogeneous and consists of multiple ethnic groups. There are differences in language, socioeconomic status, eating habits, and immigration time, which affect the absorption of trace elements.Citation34 Previous studies have found that the levels of zinc and magnesium of diabetic patients decreased.Citation35 Studies have reported that copper and zinc compete for the same carrier in the intestinal absorption process, which increases the absorption of copper and decreases the absorption of zinc.Citation36 The occurrence of chronic complications of diabetes is closely related to the oxidative stress caused by metabolic disorders. Various enzymes are required to participate in the process of oxidative stress in the body, and trace elements are an important part of these enzymes.Citation37 This study found that zinc is a protective factor affecting the severity of microvascular complications in elderly diabetes.
Our study also showed that the zinc level in elderly diabetic patients is positively correlated with the levels of SOD and T-AOC, and negatively correlated with the levels of MDA and NO. Zinc is an important reducing agent, which can induce the expression of metallothionein, improves endoplasmic reticulum stress and autophagy.Citation38,Citation39 Zinc can increase nuclear factor E2-related factor 2 (Nrf2) protein expression. Nrf2 regulates the antioxidant effect in cells by regulating reactive oxygen species, superoxide dismutase, and glutathione S-transferase.Citation40,Citation41 Zinc is also a component of superoxide dismutase, which can catalyze the generation of hydrogen peroxide from peroxide anion and has the function of resisting oxygen free radicals.Citation42 A prospective cohort study found that women with low zinc intake were associated with a 17% increased risk of diabetes compared with women with adequate zinc intake.Citation43 Therefore, maintaining the level of the zinc can reduce the oxidative stress, thereby delaying the progression of diabetic microvascular complications in the older adults.
Our study also showed that magnesium level in elderly diabetic patients is positively correlated with SOD activity. Magnesium deficiency increases oxygen free radical toxicity, which may significantly contribute to an increase in oxidized lipids and the development of vascular-related diseases with age.Citation44 In the older adults, magnesium supplementation may be a new way to increase the body’s antioxidant capacity and treat type 2 diabetes.
Our study also showed that iron level in elderly diabetic patients is positively correlated with SOD and T-AOC, and negatively correlated with MDA. Iron is involved in the transport of oxygen, the synthesis of DNA and the transport of electrons.Citation9,Citation45 In addition, iron forms free radicals through the Fenton reaction leading to tissue damage.Citation46 Therefore, iron should maintain a steady state. Therefore, combining these two parameters of trace elements and oxidative stress factors has higher sensitivity and specificity in judging the risk of diabetic microvascular complications than either parameter alone.
This study has several limitations. First, the study design failed to consider the utilization of hypoglycemic drugs, thus resulting in a missed opportunity to study the effects of such drugs on trace elements and oxidative stress factors. In future studies, by improving the study design, it could be confirmed that trace elements and oxidative stress factors may be affected by hypoglycemic drugs. Second, this was a cross-sectional study. The findings only indicate an association between changes in trace elements or oxidative stress factors and diabetic microvascular complications in older adults. Third, this study failed to rule out the effect of diet, which may be an important confounding factor. In addition, there is currently a lack of research on the correlation between trace elements and diabetic retinopathy. These findings need to be validated in future prospective studies.
Conclusion
In conclusion, this study suggested that serum trace elements are associated with levels of oxidative stress in elderly diabetic patients. Duration of diabetes, FBG, HBAlc, and MDA were independent risk factors for the severity of diabetes in the older adults; zinc and SOD are independent protective factors for the severity of diabetes in the older adults. The more stable the trace element in older adults with diabetes, the lower the oxidative stress and the fewer microvascular complications of diabetes.
Abbreviations
AGE; advanced glycation end products, DN; diabetic kidney disease, DPN; diabetic peripheral neuropathy, DPVD; diabetic peripheral vascular disease, FBG; fasting blood glucose, FBG; fasting blood glucose, HbAlc; glycosylated hemoglobin, HDL; high-density lipoprotein cholesterol, LDL; low-density lipoprotein cholesterol, MDA; malondialdehyde, NO; nitric oxide, Nrf2; nuclear factor E2-related factor 2, SD; standard deviation, SOD; superoxide dismutase, T2DM; type 2 diabetes mellitus, T-AOC; total antioxidant capacity, TC; cholesterol lipid, TG; triglyceride.
Ethics Approval and Informed Consent
After approval by the Ethics Committee of the First Hospital of Jilin University (ethics number: 2016-171) and obtaining the written consent of the selected patients. This study was conducted according to the Declaration of Helsinki. All participants were informed of the purpose of the experiment. All the participants signed informed consent forms.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. Correspondence should be addressed to Yuehui Wang and Wei Sun.
Disclosure
The authors declare that they have no competing interests in this work.
Data Sharing Statement
The datasets generated and analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Khalil H. Diabetes microvascular complications—A clinical update. Diab Metab Syndr. 2017;11:S133–S139. doi:10.1016/j.dsx.2016.12.022
- Andersson E, Persson S, Hallén N, et al. Costs of diabetes complications: hospital-based care and absence from work for 392,200 people with type 2 diabetes and matched control participants in Sweden. Diabetologia. 2020;63:2582–2594. doi:10.1007/s00125-020-05277-3
- Yan Y, Wu T, Zhang M, Li C, Liu Q, Li F. Prevalence, awareness and control of type 2 diabetes mellitus and risk factors in Chinese elderly population. BMC Public Health. 2022;22:1–6. doi:10.1186/s12889-022-13759-9
- Longo M, Bellastella G, Maiorino MI, Meier JJ, Esposito K, Giugliano D. Diabetes and Aging: from Treatment Goals to Pharmacologic Therapy. Front Endocrinol. 2019;10:45. doi:10.3389/fendo.2019.00045
- Li XT, Yu PF, Yan G, et al. Association between plasma metal levels and diabetes risk: a case-control study in China. Biomed Environ Sci. 2017;30:482–491. doi:10.3967/bes2017.064
- Swaminathan S, Fonseca VA, Alam MG, Shah SV. Role of Iron in Diabetes and Its Complications. Diabetes Care. 2007;30:1926–1933. doi:10.2337/dc06-2625
- Papachristoforou E, Lambadiari V, Maratou E, Makrilakis K, Sardu C. Association of glycemic indices (hyperglycemia, glucose variability, and hypoglycemia) with oxidative stress and diabetic complications. J Diabetes Res. 2020. doi:10.1155/2020/7489795
- Krishnamurthy P, Wadhwani A. Antioxidant enzymes and human health. Antioxidant Enzyme. 2012;1:3–18.
- Galaris D, Barbouti A, Pantopoulos K. Iron homeostasis and oxidative stress: an intimate relationship. Biochimica Et Biophysica Acta (BBA) - Molecular Cell Research. 2019;118535. doi:10.1016/j.bbamcr.2019.118535
- Bigagli E, Lodovici M. Circulating oxidative stress biomarkers in clinical studies on type 2 diabetes and its complications. Oxid Med Cell Longev. 2019;2019:1–17. doi:10.1155/2019/5953685
- Ayçiçek B, Tütüncü Y, Çavdar Ü, Sennaroğlu E. Relationships between microvascular complications of diabetes mellitus and levels of macro and trace elements. Minerva Endocrino. 2020.
- Jeddi M, Torabi E. The relationship between zinc, glycemic control and microvascular complications of diabetes mellitus. Inter J Nutr Sci. 2019;4:130–136.
- Myke-Mbata BK, Meludu SC, Obochi GO, Nnodim JK. Variations in some trace elements in various degrees of Diabetes mellitus. Al Ameen J Medl Scie. 2015;8:271–275.
- Organization WH Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia: Report of a WHO/IDF consultation. 2006.
- Hinchliffe RJ, Forsythe RO, Apelqvist J, et al. Guidelines on diagnosis, prognosis, and management of peripheral artery disease in patients with foot ulcers and diabetes (IWGDF 2019 update). Diabetes/Metab Res Rev. 2020;36:e3276. doi:10.1002/dmrr.3276
- Iqbal Z, Azmi S, Yadav R, et al. Diabetic Peripheral Neuropathy: epidemiology, Diagnosis, and Pharmacotherapy. Clin Ther. 2018;40:828–849. doi:10.1016/j.clinthera.2018.04.001
- Molitch ME, Adler AI, Flyvbjerg A, et al. Diabetic kidney disease: a clinical update from kidney disease: improving global outcomes. Kidney Int. 2015;87:20–30. doi:10.1038/ki.2014.128
- Avogaro A, Fadini GP. Microvascular complications in diabetes: a growing concern for cardiologists. Int J Cardiol. 2019;291:29–35. doi:10.1016/j.ijcard.2019.02.030
- Stehouwer CD. Microvascular dysfunction and hyperglycemia: a vicious cycle with widespread consequences. Diabetes. 2018;67:1729–1741.
- Petrie JR, Guzik TJ, Touyz RM. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can J Cardiol. 2018;34:575–584. doi:10.1016/j.cjca.2017.12.005
- Iglay K, Hannachi H, Joseph Howie P, et al. Prevalence and co-prevalence of comorbidities among patients with type 2 diabetes mellitus. Curr Med Res Opin. 2016;32:1243–1252. doi:10.1185/03007995.2016.1168291
- Association, A.D. 12. Older adults: standards of medical care in diabetes—2020. Diabetes Care. 2020;43:S152–S162. doi:10.2337/dc20-S012
- Zhou X, Guan H, Zheng L, et al. Prevalence and awareness of diabetes mellitus among a rural population in China: Results from Liaoning Province. Diabetic Med. 2015;32:332–342. doi:10.1111/dme.12599
- Bhatti JS, Sehrawat A, Mishra J, et al. Oxidative stress in the pathophysiology of type 2 diabetes and related complications: current therapeutics strategies and future perspectives. Free Radical Bio Med. 2022;184:114–134.
- Domingueti CP, Dusse LMS, Carvalho MDG, de Sousa LP, Gomes KB, Fernandes AP. Diabetes mellitus: the linkage between oxidative stress, inflammation, hypercoagulability and vascular complications. J Diabetes Complicat. 2016;30:738–745. doi:10.1016/j.jdiacomp.2015.12.018
- Ahmed FN, Naqvi FN, Shafiq F. Lipid peroxidation and serum antioxidant enzymes in patients with type 2 diabetes mellitus. Ann Ny Acad Sci. 2006;1084:481–489. doi:10.1196/annals.1372.022
- Pasaoglu H, Sancak B, Bukan N. Lipid Peroxidation and Resistance to Oxidation in Patients with Type 2 Diabetes Mellitus. Tohoku J Exp Med. 2004;203:211–218. doi:10.1620/tjem.203.211
- Gęgotek A, Skrzydlewska E. Biological effect of protein modifications by lipid peroxidation products. Chem Phys Lipids. 2019;221:46–52. doi:10.1016/j.chemphyslip.2019.03.011
- Burcham PC, Kuhan YT. Introduction of Carbonyl groups into proteins by the lipid peroxidation product, malondialdehyde. Biochem Biophys Res Commun. 1996;220:996–1001. doi:10.1006/bbrc.1996.0521
- Marnett LJ. Lipid peroxidation—DNA damage by malondialdehyde. Mutat Res. 1999;424:83–95. doi:10.1016/S0027-5107(99)00010-X
- Dimmeler S, Zeiher AM. Nitric oxide–an endothelial cell survival factor. Cell Death Differ. 1999;6:964–968. doi:10.1038/sj.cdd.4400581
- Katsas K, Mamalaki E, Kontogianni MD, et al. Malnutrition in older adults: correlations with social, diet-related, and neuropsychological factors. Nutrition. 2020;71:110640. doi:10.1016/j.nut.2019.110640
- Malavolta M, Mocchegiani E. Trace Elements and Minerals in Health and Longevity. Vol. 8. Springer; 2018.
- Liu Y, Liu S, Mao J, et al. Serum trace elements profile in graves’ disease patients with or without orbitopathy in Northeast China. Biomed Res Int. 2018.
- Sinha S, Sen S. Status of zinc and magnesium levels in type 2 diabetes mellitus and its relationship with glycemic status. Int J Diabetes Dev C. 2014;34:220–223. doi:10.1007/s13410-014-0196-9
- Hall AG, King JC. The molecular basis for zinc bioavailability. Int J Mol Sci. 2023;24:6561. doi:10.3390/ijms24076561
- Wołonciej M, Milewska E, Roszkowska-Jakimiec W. Trace elements as an activator of antioxidant enzymes. Post Higieny I Medycyny Doswiadczalnej. 2016;70:1483–1498. doi:10.5604/17322693.1229074
- Piao M, Liu Y, Yu T, Lu Y. Dietary zinc reduces endoplasmic reticulum stress and autophagy to protect against diabetic renal damage in streptozotocin-induced diabetic rats. Int J Diabetes Dev C. 2019;39:340–345. doi:10.1007/s13410-018-0681-7
- Hadj Abdallah N, Baulies A, Bouhlel A, et al. Zinc mitigates renal ischemia‐reperfusion injury in rats by modulating oxidative stress, endoplasmic reticulum stress, and autophagy. J Cell Physiol. 2018;233:8677–8690. doi:10.1002/jcp.26747
- Cortese MM, Suschek CV, Wetzel W, Kröncke K, Kolb-Bachofen V. Zinc protects endothelial cells from hydrogen peroxide via Nrf2-dependent stimulation of glutathione biosynthesis. Free Radic Biol Med. 2008;44:2002–2012. doi:10.1016/j.freeradbiomed.2008.02.013
- Li D, Tian H, Li X, et al. Zinc promotes functional recovery after spinal cord injury by activating Nrf2/HO-1 defense pathway and inhibiting inflammation of NLRP3 in nerve cells. Life Sci. 2020;245:117351. doi:10.1016/j.lfs.2020.117351
- Liochev SI, Fridovich I. Copper- and zinc-containing superoxide dismutase can act as a superoxide reductase and a superoxide oxidase*. J Biol Chem. 2000;275:38482–38485. doi:10.1074/jbc.M007891200
- Sun Q, van Dam RM, Willett WC, Hu FB. prospective study of zinc intake and risk of type 2 diabetes in women. Diabetes Care. 2009;32:629–634. doi:10.2337/dc08-1913
- Barbagallo M, Dominguez LJ. Magnesium and aging. Curr Pharm Design. 2010;16:832–839. doi:10.2174/138161210790883679
- Vogt AS, Arsiwala T, Mohsen M, Vogel M, Manolova V, Bachmann MF. On iron metabolism and its regulation. Int J Mol Sci. 2021;22:4591. doi:10.3390/ijms22094591
- Ikeda Y, Funamoto M, Tsuchiya K. The role of iron in obesity and diabetes. J Med Invest. 2022;69:1–7. doi:10.2152/jmi.69.1
