Abstract
The prevalence of type 2 diabetes mellitus (T2DM) is increasing in the elderly. Because of the unique characteristics of elderly people with T2DM, therapeutic strategy and focus should be tailored to suit this population. This article reviews the guidelines and studies related to older people with T2DM worldwide. A few important themes are generalized: 1) the functional and cognitive status is critical for older people with T2DM considering their life expectancy compared to younger counterparts; 2) both severe hypoglycemia and persistent hyperglycemia are deleterious to older adults with T2DM, and both conditions should be avoided when determining therapeutic goals; 3) recently developed guidelines emphasize the avoidance of hypoglycemic episodes in older people, even in the absence of symptoms. In addition, we raise the concern of glycemic variability, and discuss the rationale for the selection of current options in managing this patient population.
Introduction
Diabetes prevalence in older people increases with advancing age. The global prevalence of diabetes in people between the ages of 60 and 79 is 18.6%, which is more than 134.6 million people, and accounts for 35% of all cases of diabetes in adults.Citation1 Peripheral neuropathy, which is highly prevalent in older people with diabetes, increases the risk of falls and fractures, and consequently, of functional impairment.Citation2 Diabetes in older people is also associated with dementia and depression.Citation3,Citation4 Diabetic patients with depressive symptoms may need more attention in treating their condition,Citation5 particularly women.Citation6 Age-associated alteration in metabolism and excretion of medication is also a concern in the selection of antidiabetic treatment.Citation7 Older people are also at increased risk of undernutrition and skeletal muscle loss, which is generally even more evident with the presence of diabetes.Citation8,Citation9 Older people with diabetes are considered at high cardiovascular risk.Citation10 Risk of hypoglycemia is also increased due to impaired counterregulatory mechanisms.Citation11 These biopsychosocial changes increase the complexity in managing diabetes in older adults. Importantly, much attention has been paid to optimal glycemic control in the elderly in the past few years. Guidelines focusing on the elderly with diabetes were developed all over the world in the past decade with increasing focus on cognition and functional capacity.Citation10,Citation12–Citation18 This review of the literature, in addition to summarizing opinions from recently published guidelines and studies, elucidates the pathophysiological characteristics of elderly patients with type 2 diabetes mellitus (T2DM), and discusses the rationale for selection of current options in managing this patient population.
Clinical studies included in this article define elderly subgroups chronologically as aged 65 years or more to facilitate the analysis of the data.
Rationale in determining therapeutic goals for older patients
Heterogeneity of older adults cannot be overemphasized in diabetes care. Some adults were diagnosed with T2DM after age 65 with initial presentation of hyperglycemia crisis and established chronic complications; some were diagnosed from health screening without any complications, and others were diagnosed as young adults or during middle age and sustained till old age with or without microvascular complications.Citation14 Guidelines developed in recent years all highlight the need to customize therapeutic goals for various older adults with T2DM ().Citation10,Citation12,Citation14,Citation19–Citation21 Generally, appropriate therapeutic goals for older patients with T2DM should be determined based on comprehensive evaluation of cognition, functional status, comorbidities including cardiovascular risk, and geriatric syndromes.Citation22
Table 1 Categories of older people with type 2 diabetes in different guidelines
In the past decade, glycemic control was focused on glycated hemoglobin (A1C) level and postprandial glucose. Strict glycemic level is aimed at the prevention of development and progression of chronic complications of diabetes, such as nephropathy, retinopathy, and neuropathy. However, to achieve cardiovascular benefits, a prolonged period of around 10 years is needed after intensive control for 6–12 years, as revealed in the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications study and the United Kingdom Prospective Diabetes Study (UKPDS).Citation23,Citation24 These cardiovascular benefits were not observed after intensive glycemic control in long-established T2DM patients in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation trial, and the Veterans Affairs Diabetes Trial.Citation25–Citation27 For diabetic patients with limited life expectancy, maintaining independent function, preventing frailty, and preserving cognition integrity are far more important than targeting A1C alone.Citation17,Citation28 Therefore, it is important to avoid hypoglycemia events and consequent adverse outcomes, such as falls, cognitive decline, autonomic dysfunction, depression, recurrent hypoglycemia, poor compliance, and possible cardiac ischemia or arrhythmia, which may contribute to poor function and poor prognosis.Citation29–Citation31 Despite the inconsistent relationship between hypoglycemia and falls or fractures, it is still a concern that recurrent hypoglycemia may put elderly people at higher risk for falls.Citation32–Citation35 Further, this risk may be even more detrimental if the elderly patients live alone. Elders residing in long-term care facilities are at significant risk of poor functional status, frailty, and malnutrition. These frail elders may be vulnerable to hypoglycemia and its serious morbid outcomes.Citation36 On the other hand, older diabetic patients with low A1C levels may be indicative of reduced food intake and malnutrition rather than good glycemic control.Citation37 The ACCORD trial is well known for its premature termination after a median duration of 3.5 years because of higher mortality in the intensive group, targeting A1C <6% (42 mmol/mol). Based on these findings, recommendations from some guidelines propose that higher A1C goals be set for older adults.Citation10,Citation12,Citation14,Citation16,Citation19–Citation21,Citation36,Citation38 presents the glycemic targets according to different categories indicated by guidelines worldwide.
Table 2 Glycemic targets according to different categories indicated by guidelines worldwide
For reasons mentioned previously, less stringent glycemic targets have been suggested from recently developed guidelines.Citation10,Citation12,Citation14,Citation38 However, when the emphasis is made on less stringent glycemic control, it is likely to exacerbate clinical inertia, promote physician’s attempts to withdraw antidiabetic agents, and, in turn, put elderly patients at high risk for sustained hyperglycemia and associated complications, such as incontinence, dehydration, hyperglycemic crisis, cognitive decline, visual disturbances, zinc loss, poor lower extremity performance, reductions in muscle mass, falls, and consequences of dependence.Citation22,Citation39–Citation42 Physicians should keep in mind that older adults are at higher risk of hyperglycemic hyperosmolar syndrome than younger adults because of the altered perception of thirst that precludes their water intake when dehydrated, impaired functional status that limits their ability to access water, and impaired cognition that restricts their expression of thirst.Citation43 Preventing incidence of diabetes-related comorbidities is also important in reducing the deterioration in physical disability.Citation44 Thus, efforts to prevent physical disability should start from early stages, immediately after the diagnosis of diabetes.Citation45
Higher glycemic variability, independent of traditional markers for glycemic control, such as A1C, fasting plasma glucose, and postprandial glucose, was associated with increased oxidative stress, increased inflammatory markers, and impaired cognitive function.Citation46,Citation47 To prevent frailty and cognitive decline and to prevent sustained hyperglycemia and consequent microvascular complications, minimizing glycemic variability may be equally important as preventing hypoglycemia in elderly diabetic patients.Citation48
Is lower A1C really detrimental to the older patients? The ACCORD trial revealed a lesser known aspect that hypoglycemia is found more in individuals with higher A1C levels rather than those with lower A1C levels. Also, it was found that mortality was associated with higher A1Cs and nonimproved patients in the intensive group but not associated with hypoglycemia.Citation49 Evidence revealed that hypoglycemic episodes are common in older patients with A1C 8.0% (63.9 mmol/mol) or greater. Thus, raising the A1C targets may not prevent hypoglycemia in this population.Citation50 There is no strong evidence that higher A1C levels were beneficial for older adults. Thus, to achieve benefit from good glycemic control without increasing the risk of hypoglycemia in older adults, it would be better for physicians to follow a safe intensification process with appropriate selection of drugs with low glycemic variability, rather than raising A1C goals.Citation49,Citation51 If it can be achieved safely without an increase of hypoglycemia or other adverse events, A1C should be as normal as possible. Finally, all biopsychosocial aspects of older patients should be comprehensively evaluated, rather than treating the A1C alone.Citation52
How to select antidiabetic therapies considering the characteristics of older adults
Aging is characterized by a progressive impairment in carbohydrate tolerance, possibly related to disorderly insulin release, reduced insulin production and reduced glucagon-like peptide 1 (GLP-1) secretion, increased adiposity, sarcopenia, and physical inactivity.Citation14,Citation53,Citation54 Relative contribution of postprandial glucose is higher than that of fasting glucose in older people.Citation55 These important features provide clues in selecting antidiabetic therapies that are more efficacious in postprandial glucose control for older adults.
Both morbidity and mortality in the elderly are independently predicted by the duration of diabetes and advancing age. Coronary artery disease and hypoglycemia were the most common complications in the elderly, both in short- and long-lasting diabetes.Citation56 Elderly patients are more vulnerable to hypoglycemia due to age-related impairment of liver and renal function, leading to slightly decreased gluconeogenesis,Citation18 altered drug elimination, and influence of drug interaction from polypharmacy.Citation57 The hypoglycemia counterregulartory mechanism is defective in older people. Compared to those of healthy young adults, the responses of glucagon to hypoglycemia are lower in healthy elderly individuals and to a greater degree in older adults with diabetes.Citation11 However, the response of glucagon to hypoglycemia is similar in middle-aged patients and older patients with diabetes.Citation58 Older people are aware of hypoglycemia at a variable threshold between 5 mmol/L and 9 mmol/L, which is higher than the usually defined <4 mmol/L. However, the symptoms they present are nonspecific rather than typical autonomic symptoms, and are generally presented as an unwell feeling.Citation58,Citation59 These nonspecific symptoms may be misinterpreted in older patients as presentation of coexisting illnesses.Citation60
Uncontrolled hyperglycemia, repetitive hypoglycemia, and greater glucose variability are associated with worse cognition.Citation46 Therefore, choosing effective antidiabetic therapies with relatively low risk for hypoglycemia and low glucose variability is very important in older adults.Citation15 The principles of medication choice for older patients with T2DM are primarily the same as for younger adults, with special considerations in frailty, sarcopenia, cognition, and functional status. For the diabetic elders with unintentional body weight (BW) loss, sarcopenia, or sarcopenic obesity, the focus should be on avoiding medications with overt gastrointestinal side effects, which may aggravate the condition of malnutrition, worsening the frailty status. For those with cognition problems, efforts should be made to reduce regimen complexity and to avoid overt hyperglycemia and hypoglycemia. For those in end-of-life care, antidiabetic medications are aimed at avoiding symptomatic hyperglycemia with higher tolerable glycemic levels. After risk and benefit evaluations, some experts suggest metformin or dipeptidyl peptidase-4 (DPP4) inhibitors as drugs of choice for the elderly.Citation12,Citation41 In , we summarize the antidiabetic drugs with the considerations we mentioned above. Applications of antidiabetic therapies in different categories are summarized in . Interaction of oral antidiabetic drugs (OADs) and drugs used in common comorbidities are summarized in for prescribing reference.Citation61,Citation62
Table 3 Comparisons of current options in glycemic control
Table 4 Comparisons of current options in glycemic control based on different categories
Table 5 Drug interactions between antidiabetic agents and drugs used for the most common comorbidities in the elderly
Options of therapy in elderly patients
First line: lifestyle interventions and metformin
Lifestyle interventions
The importance of lifestyle interventions cannot be overemphasized. An increase of one healthy behavior was associated with a decrease in A1C level of >1.0 percentage point in older adults with diabetes.Citation63 Diet and exercise remain the cornerstones of diabetes management. While decreasing the amount of carbohydrates, diet should be designed with adequate calories to maintain ideal BW and lean muscle mass and to prevent sarcopenia or sarcopenic obesity and consequent frailty in the elderly patients. Optimizing weight in adults with diabetes is an important factor in predicting better glycemia.Citation63 Functionally independent obese elderly patients should be encouraged to maintain a healthy BW. However, compared to those who are overweight or obese, the impact of weight change in those with relatively normal weight may be complicated.Citation64 Most of the studies reviewed suggest that poor glucose regulation is associated with weight loss.Citation65 Restricted diet should be avoided in malnourished elderly patients.Citation13 Nutrition status should be thoroughly evaluated in elderly diabetic patients, with individualized nutritional planning, focusing on adequate hydration, optimal calories, and protein intake to maintain nutrition and functional status and prevent muscle loss.Citation8,Citation10,Citation22,Citation36,Citation37 Complex carbohydrates and fiber are good for decreasing glycemic excursions after meals.Citation39 The average daily protein intake should reach 1.0–1.2 g/kg BW/day to maintain and regain lean body mass and function and to prevent sarcopenia and frailty in older people.Citation66 Protein-enriched diet with concomitant muscle training may preserve or even enhance muscle mass and strength.Citation67 This may also improve functional status and muscular glucose uptake.Citation68
Physical activity is also encouraged in all adults, but should be individualized to fit individual’s medical and physical status with special considerations of degenerated joints, diabetic neuropathy, and retinopathy. Both endurance- and resistance-type exercises are recommended as they are safe and tolerable.Citation66 Cardiovascular risks should be evaluated before introducing an exercise program.Citation39 Exercise-induced hypoglycemia should be carefully assessed in older diabetic patients who are prescribed a medication regimen with higher risk of hypoglycemia.Citation39
Biguanides (metformin)
Metformin has gained increasing acceptance as first-line therapy along with lifestyle modification to achieve optimal glycemic goals. It improves insulin resistance, decreases hepatic gluconeogenesis, and induces some BW loss, with low potential for hypoglycemia.Citation39 A longitudinal cohort study showed that older men with diabetes using metformin or thiazolidinediones (TZDs) lost less lean body mass compared with those with untreated diabetes or treated with other antidiabetic agents.Citation69 This result is potentially beneficial for older adults, even in the frail elderly patients, whose muscle mass is lost with aging and accelerated with impaired fasting glucose and diabetes.Citation69
However, there are still some special considerations that preclude older adults from using metformin as a first-line therapy. The well-known side effects of metformin, namely, gastrointestinal discomfort such as anorexia, nausea, vomiting, diarrhea, and constipation, are a main concern in older adults who are frail, underweight, anorexic, and malnourished.Citation10,Citation70,Citation71 Another general concern with metformin is its risk for lactic acidosis, which is still put on the “black-box” warning regarding its use in advanced renal insufficiency (serum creatinine ≥132.6 μmol/L in men or ≥123.7 μmol/L in women or estimated glomerular filtration rate <30 mL/min), hepatic disease, congestive heart failure, and advanced age (>80 years old). It is also suggested in the package insert that metformin should be withdrawn in critical illness, persistent diarrhea, hypotension, and two days prior to contrast-enhanced imaging studies for fear of acute kidney injury and consequent accumulation of metformin in these conditions. In clinical practice, controversy exists about the association between lactic acidosis and the use of metformin.Citation72–Citation76 A Cochrane review of 347 studies in T2DM patients concluded that metformin is not associated with an increased risk of lactic acidosis, or increased levels of lactate, compared to the non-metformin group.Citation77 The causal relationship of serum concentration of metformin and lactate level is not well established.Citation78 A prospective, randomized observational study demonstrated that metformin could be safely continued even in patients with creatinine levels up to 221 μmol/L without increasing the incidence of lactic acidosis.Citation73 A retrospective cross-sectional study also showed that age per se was not associated with increase of lactate level in metformin users.Citation79 Based on existing evidence, the benefits of metformin therapy outweigh the potential risks.Citation74 It is suggested to start metformin from lower doses and reduce the maximum dose by about 50% in patients with eGFR<60 mL/min, rather than strictly avoid the drug, even in oldest-old adults.Citation80
Patients taking metformin had lower vitamin B12 (vitB12) levels than those not taking metformin.Citation81 In a multicenter, randomized, placebo-controlled trial, metformin treatment for 4.3 years was associated with decrease in vitB12 concentration of 19% and decrease in folate concentration of 5%.Citation82 Regular measurement of vitB12 and folate level might be necessary in elderly diabetic patients who received long-term metformin therapy. Early recognition of the issue with appropriate supplementation may prevent development of the consequence of vitB12 deficiency, such as macrocytic anemia and neuropathies.
Second-line or alternative first-line therapy
In patients contraindicated or intolerable to metformin therapies, all antidiabetic drugs could be used as an alternative first-line therapy, judging by the characteristics of each individual, the regulation of national health insurance, and the specific action of each drug as described below.Citation83
Thiazolidinediones
The TZDs, which are insulin sensitizers and which act through activation of peroxisome proliferator-activated receptors gamma, are effective in lowering fasting glucose level through increased peripheral insulin sensitivity, especially of muscle and adipocytes. Pioglitazone, when prescribed in patients older than 65 years, had similar effectiveness and safety as in younger adults.Citation84 It was also suggested that a combination of pioglitazone and sitagliptin improved α-cell and β-cell functions, thus reducing postprandial glucose excursions more than by either treatment alone.Citation85 Considering the low incidence of hypoglycemia of each class of the drugs, this combination seemed promising in glycemic control for older adults. However, safety profiles of TZDs are still a concern.Citation86,Citation87 It should not be used in patients with active liver disease. Increased rates of bone fractures was observed in elderly women taking rosiglitazone but not in men from the A Diabetes Outcome Progression Trial (ADOPT).Citation88,Citation89 However, increased fractures were observed at the humerus, hand, and foot, rather than the typical osteoporotic sites. A similar finding was also found in the PROactive trial.Citation90 To date, the mechanism explaining these results is still unclear. The effect of pioglitazone on bone mineral density is reported as a trend of decrease in proximal femur, hip, and lumbar spine in diabetic women, but no effect in prediabetic women. There were no changes in biochemical markers of bone turnover.Citation91,Citation92 As the clinical and pathophysiological evidence still advises the association between TZDs and fractures, its application in older adults should be made with caution.Citation93,Citation94
Another concern is its effect on cognition. As reported in the ACCORD-MIND cohort, exposure to rosiglitazone is associated with greater decline in cognitive performance compared with insulin therapy.Citation95 Despite the current evidence against the use of rosiglitazone in Alzheimer’s disease (AD), pioglitazone exhibited cognitive and functional improvement in mild AD.Citation96–Citation98 More evidence is needed to make recommendations about the use of pioglitazone in AD.
TZDs are also related to fluid retention. When used in patients with diabetic macular edema, worsening of the condition was reported.Citation99 Current evidence suggests that TZDs could still be safely continued in patients without macular edema.Citation100 However, this feature limits its application in patients with class III or IV congestive heart failure.Citation101–Citation103 The risk of ischemic stroke, myocardial ischemia, and heart failure is still inconclusive in rosiglitazone and pioglitazone.Citation101,Citation104–Citation108 Prescription of rosiglitazone in some areas is highly restricted now.
Despite the positive effect of TZDs on glycemic control, lean body mass, cognition, and low risk of hypoglycemia, drawbacks such as increased risk of fractures, probable macular edema, heart failure, and fluid retention exist. Application of TZDs in older diabetic adults needs to be carefully evaluated for its risk/benefit ratio. Newer generation TZDs, termed as selective peroxisome proliferator-activated receptors gamma modulators, which may minimize the unwanted effects of current TZDs, are being developed and may be promising in the future.Citation86
Sulfonylureas
Insulin secretagogues, which stimulate insulin release from pancreatic β-cells, have been popular for a long time because of their good efficacy and relatively low cost. As pancreatic β-cell function decreases with aging, insulin secretagogues are theoretically a good choice to enhance insulin secretion in older adults.Citation54 Risk of hypoglycemia among elderly patients treated with sulfonylureas (SU), especially glyburide (glibenclamide) and chlorpropamide, is higher than among younger adults, which is associated with more hypoglycemia-related hospitalizations.Citation109,Citation110 Higher risk of hypoglycemia related to SU use is associated with impaired renal function, impaired hepatic function, recent hospitalization, polypharmacy, alcohol use, and caloric restriction in older adults.Citation111 Sensitivity to SU may increase, especially in those aged over 80, which makes the oldest-old more vulnerable to hypoglycemia.Citation36 Despite these drawbacks, there is no need to abruptly withdraw SU from all older adults. Its once-daily dosage form is potentially good for improving compliance of older adults and for minimizing dosing errors.Citation71 Guidelines developed all over the world suggest avoidance of only glyburide in older adults, which was associated with the most long-lasting, life-threatening hypoglycemic events.Citation10 The most important thing in prescribing SU in older adults is to follow the principle of starting SU from lowest dose, to slowly titrate to the individualized target, and to closely monitor any hypoglycemia symptoms, especially in elderly patients whose pancreatic β-cell function is only mildly impaired. SUs may still fail to be effective in some patients, as they develop pancreatic β-cell failure, especially in elderly patients with long-lasting diabetes, which makes it an appropriate substitute for insulin in patients whose glycemic targets are not stringent.Citation18,Citation36
Meglitinides (repaglinide and nateglinide)
The meglitinides are rapid-acting insulin secretagogues with a short duration of action, and are aimed at increasing prandial insulin secretion.Citation112 Nateglinide should not be used with SU because of competitive binding of SU receptors. A randomized, open-label, crossover trial suggested that repaglinide is safe and effective with lower risk of hypoglycemia compared with SU in older patients with borderline poor glycemic control.Citation113 Hypoglycemia is related to missed meals, so meglitinides should be taken within 30 minutes before meals. Therefore, meglitinides should be prescribed with caution in the elderly patients with cognitive impairment and erratic eating habits.Citation10 Hepatic and renal insufficiency may prolong the action of repaglinide, resulting in higher risk of hypoglycemia in these conditions.Citation70 Disadvantages include relatively high cost, frequency of administration, and strict regulation of time of taking medicine, which contribute to the complexity of polypharmacy in older adults.Citation39,Citation71
Alpha-glucosidase inhibitors
Alpha-glucosidase inhibitors (AGIs) delay absorption of carbohydrates and result in decreased postprandial glucose excursions, improvement of glycemic variability without increased oxidative stress, and possible improvement of β-cell response.Citation112,Citation114,Citation115 Maximal antihyperglycemia is achieved with lower doses (25 mg before meals) in elderly patients than their younger counterparts.Citation116 Moreover, AGIs may increase insulin sensitivity in diabetic elderly patients.Citation117 They are effective in elderly overweight type 2 diabetic patients.Citation118 They are well tolerated in older adults even with multiple comorbidities with a low incidence of hypoglycemia as monotherapy. AGIs also reduced the risk of postprandial hypoglycemia and late hypoglycemia in older adults with T2DM who eat rice porridge as main meal, due to impaired chewing function.Citation119 When hypoglycemia occurs in regimens combined with AGIs, it should be treated with oral glucose because other complex carbohydrates will not relieve the event.Citation39 Special education should be imparted to the elderly patients and their family members to manage such hypoglycemic conditions. Further, if AGIs are prescribed with prandial insulin, mismatch between peak serum glucose levels and peak prandial insulin levels may occur, placing patients at increased risk for hypoglycemia.Citation71 The most common adverse events are gastrointestinal disturbances, especially flatulence, abdominal distension, diarrhea, abdominal pain, and abdominal discomfort, which preclude AGIs application in the elderly patients.Citation118,Citation120–Citation123 The clinical response of AGIs depends on preserved β-cell function. That is, AGIs are more effective in newly diagnosed diabetes and less effective in long-standing diabetes with severely impaired insulin secretion.Citation112 This feature is important in determining whether AGIs should be prescribed in older adults. Another concern is that AGIs should be taken with meals, which increases the complexity of the medication regimen and may lead to nonadherence.Citation124
Incretin-based therapies
Incretin-based therapies have drawn increasing attention in recent years because of their properties of enhancing glucose-dependent insulin secretion after ingestion of food.Citation22 Both GLP-1 and glucose-dependent insulinotropic peptide are degraded rapidly by DPP4, resulting in short plasma half-lives. GLP-1 suppresses glucagon secretion, delays gastric emptying, increases satiety, and decreases food intake.Citation22 There are two classes of drugs focusing on incretin effect, namely, DPP4 inhibitors and GLP-1 receptor agonists.
DPP4 inhibitors
This drug class inhibits DPP4, and thus prolongs the action of GLP-1 and glucose-dependent insulinotropic peptide in diabetic patients whose incretin response is impaired.Citation71 Among the currently available DPP4 inhibitors, sitagliptin, vildagliptin, saxagliptin, linagliptin, and alogliptin have been confirmed to be well tolerated in older adults with few gastrointestinal side effects and little effect on BW, with similar efficacy as younger adults, and can be safely used in renal insufficiency with labeled dose adjustment for each drug.Citation125–Citation131 DPP4 inhibitors resulted in reductions in A1C for patients whose baseline A1C levels were higher.Citation130 These excellent tolerability profiles, low risk of hypoglycemia, and once-daily dosing make this drug class suitable for frail and debilitated elderly patients.Citation7,Citation12,Citation22
DPP4 inhibitors enhance the effect of insulin secretion stimulated by SU, and thus increase the risk of hypoglycemia when used in combinations with SU.Citation129 This characteristic also indicates that DPP4 inhibitors are efficacious with preserved β-cell insulin secretion, and may be primarily effective early in the course of diabetes with mild hyperglycemia.Citation132,Citation133 Conversely, DPP4 inhibitors might be ineffective in elderly patients with long-lasting T2DM and poorly preserved β-cell insulin secretion. Another concern is their high expense, which may make them unavailable in some countries.Citation10
GLP-1 receptor agonists
This drug class acts on the GLP-1 receptor directly with long duration due to its resistance to degradation by DPP. GLP-1 receptor agonists are effective in glycemic control and are well tolerated without increasing the risk of hypoglycemia in older patients.Citation134–Citation136 In addition to their glucose-lowering effects, GLP-1 receptor agonists delay gastric emptying and increase satiety, resulting in weight loss, in particular reductions in subcutaneous fat mass.Citation137 Liraglutide also resulted in slight reductions of visceral fat mass in pioglitazone users.Citation137 Both liraglutide and exenatide ameliorate concomitant nonalcoholic fatty liver disease.Citation137,Citation138 The evidence of their impact on muscle mass is still lacking. However, just as the concern in DPP4 inhibitors, the effect of GLP-1 receptor agonists on A1C reductions was also inversely related to diabetes duration, ie, to the preservation of β-cell function.Citation139 Thus, the characteristics of GLP-1 receptor agonists might be beneficial to obese diabetic elders if used early in the course of diabetes.Citation12,Citation140 However, their weight-reducing effect and gastrointestinal side effects may be detrimental for the frail elderly patients with poor caloric intake and poor nutrition status.Citation10,Citation70,Citation71 These drugs should be used with caution in diabetic elders who are undergoing unintentional weight loss, and who are malnourished or at high risk for malnutrition. Metabolism and excretion of liraglutide is not affected by renal impairment, even in patients with end-stage renal disease.Citation141,Citation142 Recommendations for use of liraglutide in patients with more advanced renal impairment are limited.Citation143 Exenatide is excreted through the kidney, and is not recommended for use in severe renal impairment or end-stage renal disease.Citation131
Bile acid sequestrants
Colesevelam hydrochloride was originally approved for treatment of hyperlipidemia;Citation144 however, subsequent clinical trials demonstrated an improvement in glycemia for patients with T2DM.Citation145–Citation147 Colesevelam is a bile acid sequestrant designed to have a high affinity and capacity for binding to bile acids.Citation148 Colesevelam is nonabsorbable by the body, and its distribution is confined to the digestive tract. Its hydrophilic and water-insoluble nature facilitates binding of bile acids in the intestine and excretion of these complexes in the feces.Citation149 As a result, the body increases the conversion of cholesterol to bile acids, resulting in an uptake of low-density lipoprotein cholesterol (LDL-C) by the liver to the blood, thereby lowering serum LDL-C. Colesevelam as a monotherapy or add-on therapy for the treatment of T2DM can reduce A1C and LDL-C levels.Citation150 Further, in T2DM patients aged 65 years and older, colesevelam treatment as an add-on therapy results in similar A1C reductions.Citation151 Colesevelam is safe and well-tolerated in older adults, with certain mild to moderate gastrointestinal side effects including constipation and dyspepsia.Citation151 An advantage of prescribing colesevelam to older diabetic patients is the low risk for hypoglycemic events.Citation150
Sodium glucose cotransporter 2 inhibitors
The newest drug class for oral diabetic agents is the sodium glucose cotransporter 2 (SGLT2) inhibitors.Citation152 SGLT2 inhibitors prevent the reabsorption of renal-filtered glucose levels, resulting in decreased blood glucose levels.Citation153 SGLT2 inhibitors can be used as a monotherapy or dual and triple therapy for T2DM patients to moderately lower A1C levels (0.5%–1.0%).Citation154 Further, SGLT2 inhibitors have the added benefits of weight loss and improved blood pressure and lipid parameters.Citation154–Citation157 SGLT2 inhibitors are generally well tolerated among diabetic patients.Citation158–Citation161 Common adverse events include urinary tract infections, genital mycotic infections, hypotension/volume depletion, lipid alterations, hypoglycemia, and renal insufficiency.Citation156,Citation161–Citation165 The efficacy and safety of SGLT2 inhibitors in elderly patients is consistent with younger patients;Citation166 however, additional long-term studies are needed. Thus, the risks and benefits of SGLT2 inhibitors should be assessed in older patients on a case-by-case basis given the newness of the drug class.Citation166
Insulin
Insulin therapy is inevitable when β-cell preservation is severely impaired due to advanced age or long-lasting T2DM.Citation39 Early use of insulin may reduce glucotoxicity and restore function of β-cells.Citation39 However, insulin is often underutilized in elderly patients due to concerns about hypoglycemia, misconceptions about insulin, social stigma, needle phobia, complexity of injection skills, low adaptation capacity, and, moreover, clinical inertia.Citation70,Citation167 Before initiating insulin therapy, comprehensive evaluation of psychosocial barriers, functional status (ie, visual acuity and manual dexterity), cognitive status, and financial ability to afford insulin and insulin-delivery supplies should be made to ensure safety, compliance, and effectiveness of insulin use.Citation70
Conventional neutral protamine Hagedorn (NPH) insulin and regular insulin were not recommended due to variable bioavailability and nonphysiological pharmacokinetics that put patients in higher risk of hypoglycemia.Citation70 Long-acting insulins degludec, glargine, and detemir are safer choices than NPH in older adults because of their lower risk of hypoglycemia, especially nocturnal hypoglycemia, which may contribute to cardiovascular morbidity and falls.Citation168–Citation172 Insulin degludec resulted in less hypoglycemia than insulin glargine even in long-duration diabetic patients, whose counterregulatory hormone responses were presumed to be weaker.Citation169 Besides, insulin analogs are mostly delivered through insulin pens, which leads to improved adherence, accuracy of injection, quality of life, and decreased admissions for hypoglycemia.Citation12,Citation15,Citation173,Citation174
For elderly diabetic patients with inadequately controlled hyperglycemia, patients with early combinations of basal insulin had better glycemic control and less hypoglycemia than titration of oral antidiabetic drugs.Citation175 In diabetic elders with poorly controlled glycemia, insulin therapy did not result in higher hypoglycemia events if glycemic targets were less stringent.Citation176 A once-daily insulin regimen was also more preferred by an older population than more frequent dosing.Citation177 Prandial insulin supplement in basal bolus regimen or premixed insulin may be appropriate in highly selected elderly patients with good functional reserve.Citation70 Judicious use of insulin as an add-on therapy may improve mental health, quality of life, social functioning, treatment satisfaction, and caregiver strain in elderly diabetic patients with poor glycemic control.Citation178
Combinations of antidiabetic agents
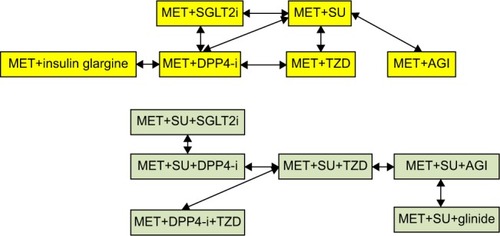
Considering the importance of avoiding hypoglycemia and managing postprandial hyperglycemia in elderly patients, some combinations may provide these desirable outcomes better than commonly used metformin plus SU in clinical practice. We summarize the results of randomized controlled trials comparing glycemic effect, hypoglycemia risk, and influence on BW among strategies of each combination in and . Current trials regarding drugs combination were not planned for the elderly patients except for a few studies including the elderly patients as a subgroup for further analysis.Citation179–Citation184 As the risk of hypoglycemia is higher in older adults, combination strategies with less hypoglycemia risk in middle-aged adults may be more appropriate for older adults.
Table 6 Comparisons of combination strategies in glycemic control
Figure 1 Comparison of combination therapies, studies including two drugs combination, and three drugs combination.
Metformin plus DPP4 inhibitors
When metformin monotherapy could not achieve glycemic target, DPP4 inhibitor was suggested as first add-on drug compared with SU, TZD, or insulin glargine in the elderly patients. Though not as effective as insulin glargine, combination of metformin with DPP4 inhibitors provided the favorable result of less hypoglycemia incidence.Citation185 Compared with SU, DPP4 inhibitor results in similar improvement of A1C, but less hypoglycemia incidence and no weight gain.Citation180–Citation184,Citation186–Citation188 This combination also showed better glycemic variability,Citation189,Citation190 decrease of glucagon production,Citation187 better β-cell function,Citation188 better insulin resistance,Citation187 and better cost-effectiveness than a combination of metformin with SU.Citation179,Citation191,Citation192 Compared with TZD, combination with DPP4 inhibitors revealed similar glycemic control and hypoglycemia risk, but less weight gain.Citation193–Citation195 Compared with metformin plus SU, metformin plus TZD was the more tolerable combination due to less hypoglycemia incidence with similar glycemic control and BW gain.Citation196–Citation198
Metformin plus SGLT2 inhibitors
SGLT2 inhibitors are newly approved drugs without experience on long-term effect and safety. Randomized controlled studies demonstrated that combination with canaglifozin is at least not inferior to combination with glimepiride or sitagliptin in glycemic control, but with less hypoglycemia incidence than glimepirideCitation199 and more BW reduction than sitagliptin.Citation200 This combination may provide favorable effects for elderly groups, but at the cost of more genitourinary tract infection. This risk should be balanced with other benefits during clinical practice.
Metformin plus acarbose
Effective on reduction of postprandial glucose excursion with low hypoglycemia risk makes AGIs an attractive second-line therapy in elderly patients, at least theoretically. However, there was only one study with a small sample size comparing acarbose and glibenclamide as second-line combination therapy. Though not significant, AGIs seemed less effective than SU in glycemic control but had a favorable effect on BW.Citation114 Evidence was not adequate to make a suggestion due to limited studies.
Triple combinations
Studies on triple combinations were limited. Most of the dual combinations in clinical practice are metformin plus SU. Some randomized controlled trials enrolled patients in poor control with metformin plus SU and compared the effect of the third drug. Combination with canaglifozin 300 mg/day was superior to sitagliptin in glycemic control and BW reduction without increased incidence of hypoglycemia.Citation201 Acarbose had similar effects as repaglinideCitation202 but was less effective than pioglitazone added on, despite favorable effect on BW control.Citation203
Metformin and pioglitazone plus DPP4 inhibitors
If metformin and pioglitazone combinations were used as the first two OADs, DPP4 inhibitors and SU decreased A1C to a similar degree. DPP4 inhibitors had a neutral effect on BW compared with BW gain in SU group. This combination was more tolerable than combination with SU, such that no patients withdrew from the study due to hypoglycemia as compared with eleven patients in the SU arm. This combination also demonstrated better protection of β-cell secretion.Citation204 These features were desirable for elderly patients.
Metformin and acarbose plus DPP4 inhibitors or mitiglinide
Despite the theoretical concern of the mismatch between peak glucose absorption and peak prandial insulin secretion in combination of acarbose with mitiglinides, a prospective randomized study revealed that daily blood glucose fluctuations were significantly improved without increase in incidence of hypoglycemia.Citation205 For elderly patients poorly controlled with metformin monotherapy, a combination of AGIs plus DPP4 inhibitors or AGIs plus mitiglinide may be an attractive add-on choice.
Conclusion
The target of glycemic management in elderly patients with T2DM has been focused on preventing frailty and preserving functional independence. Recommendations from guidelines worldwide suggest higher A1C targets than younger adults. However, evidence suggests that better glycemic control in older adults is equally important in maintaining functional independence and cognition in order to prevent hypoglycemia in such populations. Thus, a safe intensification process and selection of antidiabetic drugs with lower glycemic variability may achieve this goal. Recent developments in incretin-based therapies and long-acting insulin analogs follow this principle, and demonstrate lower hypoglycemia risk than traditional therapies such as SU and human insulin. Some combination therapies have demonstrated desirable effects in middle-aged adults and thus may be appropriate for older patients. Future research is needed to explore the best combination of antidiabetic therapies for achieving glycemic control in elderly patients safely and effectively.
Disclosure
The authors report no conflicts of interest in this work.
References
- International Diabetes FederationIDF Diabetes Atlas6th edBrussels, BelgiumInternational Diabetes Federation2013
- MenzHBLordSRSt GeorgeRFitzpatrickRCWalking stability and sensorimotor function in older people with diabetic peripheral neuropathyArch Phys Med Rehabil200485224525214966709
- RobertsROKnopmanDSPrzybelskiSAAssociation of type 2 diabetes with brain atrophy and cognitive impairmentNeurology201482131132114124647028
- HasanSSMamunAAClavarinoAMKairuzTIncidence and risk of depression associated with diabetes in adults: evidence from longitudinal studiesCommunity Ment Health J2014
- ChiuCJWrayLABeverlyEADominicOGThe role of health behaviors in mediating the relationship between depressive symptoms and glycemic control in type 2 diabetes: a structural equation modeling approachSoc Psychiatry Psychiatr Epidemiol2010451677619343264
- ChiuCJWrayLAGender differences in functional limitations in adults living with type 2 diabetes: biobehavioral and psychosocial mediatorsAnn Behav Med2011411718220827519
- MoghissiEManagement of type 2 diabetes mellitus in older patients: current and emerging treatment optionsDiabetes Ther20134223925624096685
- ParkSWGoodpasterBHLeeJSHealth, Aging, and Body Composition StudyExcessive loss of skeletal muscle mass in older adults with type 2 diabetesDiabetes Care200932111993199719549734
- KimKSParkKSKimMJKimSKChoYWParkSWType 2 diabetes is associated with low muscle mass in older adultsGeriatr Gerontol Int201414suppl 111512124450569
- International Diabetes FederationManaging Older People with Type 2 DiabetesBrusselsIDF Global Guideline2013
- Ortiz-AlonsoFJGaleckiAHermanWHSmithMJJacquezJAHalterJBHypoglycemia counterregulation in elderly humans: relationship to glucose levelsAm J Physiol19942674 pt 1E497E5067943297
- SinclairAJPaolissoGCastroMEuropean Diabetes Working Party for Older PeopleEuropean diabetes working party for older people 2011 clinical guidelines for type 2 diabetes mellitus. Executive summaryDiabetes Metab201137suppl 3S27S3822183418
- SinclairAMorleyJERodriguez-MañasLDiabetes mellitus in older people: position statement on behalf of the International Association of Gerontology and Geriatrics (IAGG), the European Diabetes Working Party for Older People (EDWPOP), and the International Task Force of Experts in DiabetesJ Am Med Dir Assoc201213649750222748719
- Sue KirkmanMBriscoeVJClarkNDiabetes in older adults: a consensus reportJ Am Geriatr Soc201260122342235623106132
- Canadian Diabetes Association Clinical Practice Guidelines Expert CommitteeMeneillyGSKnipATessierDDiabetes in the elderlyCan J Diabetes201337suppl 1S184S19024070944
- MalleryLHRansomTSteevesBCookBDunbarPMoorhousePEvidence-informed guidelines for treating frail older adults with type 2 diabetes: from the Diabetes Care Program of Nova Scotia (DCPNS) and the Palliative and Therapeutic Harmonization (PATH) programJ Am Med Dir Assoc2013141180180824074961
- ChenLKChenYMLinMHPengLNHwangSJCare of elderly patients with diabetes mellitus: a focus on frailtyAgeing Res Rev20109suppl 1S18S2220849981
- LaubscherTRegierLBarehamJDiabetes in the frail elderly: individualization of glycemic managementCan Fam Physician201258554354622586198
- BrownAFMangioneCMSalibaDSarkisianCACalifornia Healthcare Foundation/American Geriatrics Society Panel on Improving Care for Elders with DiabetesGuidelines for improving the care of the older person with diabetes mellitusJ Am Geriatr Soc2003515 suppl GuidelinesS265S28012694461
- PogachLMBrietzkeSACowanCLJrVA/DoD Diabetes Guideline Development GroupDevelopment of evidence-based clinical practice guidelines for diabetes: the Department of Veterans Affairs/Department of Defense guidelines initiativeDiabetes Care200427suppl 2B82B8915113788
- VA/DoD Clinical Practice Guideline for the Management of Diabetes Mellitus2010 Available from: http://www.guideline.gov/content.aspx?id=24192Accessed May 17, 2014
- AbbatecolaAMMaggiSPaolissoGNew approaches to treating type 2 diabetes mellitus in the elderly: role of incretin therapiesDrugs Aging2008251191392518947259
- LachinJMOrchardTJNathanDMGroupDERUpdate on cardiovascular outcomes at 30 years of the diabetes control and complications trial/epidemiology of diabetes interventions and complications studyDiabetes Care2014371394324356596
- HolmanRRPaulSKBethelMAMatthewsDRNeilHA10-year follow-up of intensive glucose control in type 2 diabetesN Engl J Med2008359151577158918784090
- DuckworthWAbrairaCMoritzTGlucose control and vascular complications in veterans with type 2 diabetesN Engl J Med2009360212913919092145
- ADVANCE Collaborative GroupPatelAMacMahonSChalmersJIntensive blood glucose control and vascular outcomes in patients with type 2 diabetesN Engl J Med2008358242560257218539916
- Action to Control Cardiovascular Risk in Diabetes Study GroupGersteinHCMillerMEByingtonRPEffects of intensive glucose lowering in type 2 diabetesN Engl J Med2008358242545255918539917
- KimJHLimSChoiSHSarcopenia: an independent predictor of mortality in community-dwelling older Korean menJ Gerontol A Biol Sci Med Sci201469101244125224721723
- CryerPEMechanisms of hypoglycemia-associated autonomic failure in diabetesN Engl J Med2013369436237223883381
- BordierLDoucetJBoudetJBauduceauBUpdate on cognitive decline and dementia in elderly patients with diabetesDiabetes Metab2014
- FrierBMSchernthanerGHellerSRHypoglycemia and cardiovascular risksDiabetes Care201134suppl 2S132S13721525444
- SchwartzAVMargolisKLSellmeyerDEIntensive glycemic control is not associated with fractures or falls in the ACCORD randomized trialDiabetes Care20123571525153122723583
- PuarTHKhooJJChoLWAssociation between glycemic control and hip fractureJ Am Geriatr Soc20126081493149722862735
- SchwartzAVVittinghoffESellmeyerDEHealth, Aging, and Body Composition StudyDiabetes-related complications, glycemic control, and falls in older adultsDiabetes Care200831339139618056893
- NelsonJMDufrauxKCookPFThe relationship between glycemic control and falls in older adultsJ Am Geriatr Soc200755122041204417971138
- SinclairAJTask, Finish Group of Diabetes UKGood clinical practice guidelines for care home residents with diabetes: an executive summaryDiabet Med201128777277721672001
- VischerUMPerrenoudLGenetCArdigoSRegiste-RameauYHerrmannFRThe high prevalence of malnutrition in elderly diabetic patients: implications for anti-diabetic drug treatmentsDiabet Med201027891892420653750
- Canadian Diabetes Association Clinical Practice Guidelines Expert CommitteeImranSARabasa-LhoretRRossSTargets for glycemic controlCan J Diabetes201337suppl 1S31S3424070959
- RosenstockJManagement of type 2 diabetes mellitus in the elderly: special considerationsDrugs Aging2001181314411232737
- YaffeKFalveyCHamiltonNDiabetes, glucose control, and 9-year cognitive decline among older adults without dementiaArch Neurol20126991170117522710333
- SinclairAMorleyJEHow to manage diabetes mellitus in older persons in the 21st century: applying these principles to long term diabetes careJ Am Med Dir Assoc2013141177778024176597
- MooradianADMorleyJEMicronutrient status in diabetes mellitusAm J Clin Nutr19874558778953554960
- GagliaJLWyckoffJAbrahamsonMJAcute hyperglycemic crisis in the elderlyMed Clin North Am200488410631084 xii15308390
- ChiuCJWrayLAOfstedalMBDiabetes-related change in physical disability from midlife to older adulthood: evidence from 1996–2003 Survey of Health and Living Status of the Elderly in TaiwanDiabetes Res Clin Pract201191341342321193244
- ChiuCJWrayLAPhysical disability trajectories in older Americans with and without diabetes: the role of age, gender, race or ethnicity, and educationGerontologist2011511516320713455
- RizzoMRMarfellaRBarbieriMRelationships between daily acute glucose fluctuations and cognitive performance among aged type 2 diabetic patientsDiabetes Care201033102169217420573753
- RizzoMRBarbieriMMarfellaRPaolissoGReduction of oxidative stress and inflammation by blunting daily acute glucose fluctuations in patients with type 2 diabetes: role of dipeptidyl peptidase-IV inhibitionDiabetes Care201235102076208222688551
- WangCPHazudaHPBetter glycemic control is associated with maintenance of lower-extremity function over time in Mexican American and European American older adults with diabetesDiabetes Care201134226827321216857
- TeohHHomePLeiterLAShould A1C targets be individualized for all people with diabetes? Arguments for and againstDiabetes Care201134suppl 2S191S19621525454
- MunshiMNSegalARSuhlEFrequent hypoglycemia among elderly patients with poor glycemic controlArch Intern Med2011171436236421357814
- MoriYExploring an optimal approach to the use of oral hypoglycemic agents based on CGM results: implications for combination therapy with oral hypoglycemic agentsNihon Rinsho20116981505151421838054
- McLarenLAQuinnTJMcKayGADiabetes control in older peopleBMJ2013346f262523615598
- MeneillyGSRyanASVeldhuisJDElahiDIncreased disorderliness of basal insulin release, attenuated insulin secretory burst mass, and reduced ultradian rhythmicity of insulin secretion in older individualsJ Clin Endocrinol Metab19978212408840939398719
- GelonezeBde OliveiraMDVasquesACNovaesFSParejaJCTambasciaMAImpaired incretin secretion and pancreatic dysfunction with older age and diabetesMetabolism201463792292924854384
- MunshiMNPandyaNUmpierrezGEDiGenioAZhouRRiddleMCContributions of basal and prandial hyperglycemia to total hyperglycemia in older and younger adults with type 2 diabetes mellitusJ Am Geriatr Soc201361453554123581911
- HuangESLaiteerapongNLiuJYJohnPMMoffetHHKarterAJRates of complications and mortality in older patients with diabetes mellitus: the diabetes and aging studyJAMA Intern Med2014174225125824322595
- ShorrRIRayWADaughertyJRGriffinMRIncidence and risk factors for serious hypoglycemia in older persons using insulin or sulfonylureasArch Intern Med199715715168116869250229
- BremerJPJauch-CharaKHallschmidMSchmidSSchultesBHypoglycemia unawareness in older compared with middle-aged patients with type 2 diabetesDiabetes Care20093281513151719487634
- AbdelhafizAHBaileyCEng LooBSinclairAHypoglycaemic symptoms and hypoglycaemia threshold in older people with diabetes – a patient perspectiveJ Nutr Health Aging2013171089990224257574
- MeneillyGSCheungETuokkoHAltered responses to hypoglycemia of healthy elderly peopleJ Clin Endocrinol Metab1994786134113488200936
- DRUGDEX® SystemGreenwood Village, COThomson Healthcare2011 Updated periodically
- Lexi-Drugs OnlineHudson, OHLexi-Comp, Inc [Updated September 13, 2014]
- ChiuCJWrayLAFactors predicting glycemic control in middle-aged and older adults with type 2 diabetesPrev Chronic Dis201071A0820040223
- ChiuCJWrayLALuFHBeverlyEABMI change patterns and disability development of middle-aged adults with diabetes: a dual trajectory modeling approachJ Gen Intern Med20132891150115623463456
- ChiuCJWrayLABeverlyEARelationship of glucose regulation to changes in weight: a systematic review and guide to future researchDiabetes Metab Res Rev201026532333520578206
- BauerJBioloGCederholmTEvidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study GroupJ Am Med Dir Assoc201314854255923867520
- DalyRMO’ConnellSLMundellNLGrimesCADunstanDWNowsonCAProtein-enriched diet, with the use of lean red meat, combined with progressive resistance training enhances lean tissue mass and muscle strength and reduces circulating IL-6 concentrations in elderly women: a cluster randomized controlled trialAm J Clin Nutr201499489991024477043
- MorrisonSColbergSRParsonHKVinikAIExercise improves gait, reaction time and postural stability in older adults with type 2 diabetes and neuropathyJ Diabetes Complications201428571572224929798
- LeeCGBoykoEJBarrett-ConnorEOsteoporotic Fractures in Men (MrOS) Study Research GroupInsulin sensitizers may attenuate lean mass loss in older men with diabetesDiabetes Care201134112381238621926282
- SoeKSacerdoteAKaramJBahtiyarGManagement of type 2 diabetes mellitus in the elderlyMaturitas201170215115921890292
- NeumillerJJSetterSMPharmacologic management of the older patient with type 2 diabetes mellitusAm J Geriatr Pharmacother20097632434220129254
- AlmirallJBriculleMGonzalez-ClementeJMMetformin-associated lactic acidosis in type 2 diabetes mellitus: incidence and presentation in common clinical practiceNephrol Dial Transplant20082372436243818388117
- RachmaniRSlavachevskiILeviZZadokBKedarYRavidMMetformin in patients with type 2 diabetes mellitus: reconsideration of traditional contraindicationsEur J Intern Med200213742812384131
- TahraniAAVarugheseGIScarpelloJHHannaFWMetformin, heart failure, and lactic acidosis: is metformin absolutely contraindicated?BMJ2007335761850851217823192
- EppengaWLLalmohamedAGeertsAFRisk of lactic acidosis or elevated lactate concentrations in metformin users with renal impairment: a population-based cohort studyDiabetes Care20143782218222424842984
- ZhangXHarmsenWSMettlerTAContinuation of metformin use after a diagnosis of cirrhosis significantly improves survival of patients with diabetesHepatology2014
- SalpeterSRGreyberEPasternakGASalpeterEERisk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitusCochrane Database Syst Rev20104CD002967
- HolsteinAStumvollMContraindications can damage your health – is metformin a case in point?Diabetologia200548122454245916283245
- LinYCLinLYWangHFLinHDFasting plasma lactate concentrations in ambulatory elderly patients with type 2 diabetes receiving metformin therapy: a retrospective cross-sectional studyJ Chin Med Assoc2010731261762221145508
- McCormackJJohnsKTildesleyHMetformin’s contraindications should be contraindicatedCan Med Assoc J2005173550250416129871
- KosELiszekMJEmanueleMADurazo-ArvizuRCamachoPEffect of metformin therapy on vitamin D and vitamin B(1)(2) levels in patients with type 2 diabetes mellitusEndocr Pract201218217918421940283
- de JagerJKooyALehertPLong term treatment with metformin in patients with type 2 diabetes and risk of vitamin B-12 deficiency: randomised placebo controlled trialBMJ2010340c218120488910
- InzucchiSEBergenstalRMBuseJBManagement of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD)Diabetes Care20123561364137922517736
- RajagopalanRPerezAYeZKhanMMurrayFTPioglitazone is effective therapy for elderly patients with type 2 diabetes mellitusDrugs Aging200421425927115012171
- AlbaMAhrénBInzucchiSESitagliptin and pioglitazone provide complementary effects on postprandial gPioglitazone is effective therapy for elderly patients with type 2 diabetes mellituslucose and pancreatic islet cell functionDiabetes Obes Metab201315121101111023782502
- KungJHenryRRThiazolidinedione safetyExpert Opin Drug Saf201211456557922616948
- RajagopalanRXuYAbbadessaMQuartet StudyGThe effect of pioglitazone on glycemic and lipid parameters and adverse events in elderly patients with type 2 diabetes mellitus: a post hoc analysis of four randomized trialsAm J Geriatr Pharmacother20064212313316860259
- KahnSEHaffnerSMHeiseMAADOPT Study GroupGlycemic durability of rosiglitazone, metformin, or glyburide monotherapyN Engl J Med2006355232427244317145742
- KahnSEZinmanBLachinJMDiabetes Outcome Progression Trial (ADOPT) Study GroupRosiglitazone-associated fractures in type 2 diabetes: an Analysis from A Diabetes Outcome Progression Trial (ADOPT)Diabetes Care200831584585118223031
- DormandyJBhattacharyaMvan Troostenburg de BruynARPROactive InvestigatorsSafety and tolerability of pioglitazone in high-risk patients with type 2 diabetes: an overview of data from PROactiveDrug Saf200932318720219338377
- GreyABollandMFenwickSThe skeletal effects of pioglitazone in type 2 diabetes or impaired glucose tolerance: a randomized controlled trialEur J Endocrinol2014170225526224217934
- BoneHGLindsayRMcClungMRPerezATRaananMGSpanheimerRGEffects of pioglitazone on bone in postmenopausal women with impaired fasting glucose or impaired glucose tolerance: a randomized, double-blind, placebo-controlled studyJ Clin Endocrinol Metab201398124691470124057294
- HabibZAHavstadSLWellsKDivineGPladevallMWilliamsLKThiazolidinedione use and the longitudinal risk of fractures in patients with type 2 diabetes mellitusJ Clin Endocrinol Metab201095259260020061432
- GreyAThiazolidinedione-induced skeletal fragility – mechanisms and implicationsDiabetes Obes Metab200911427528418671797
- SeaquistERMillerMEFonsecaVEffect of thiazolidinediones and insulin on cognitive outcomes in ACCORD-MINDJ Diabetes Complications201327548549123680059
- MillerBWWillettKCDesiletsARRosiglitazone and pioglitazone for the treatment of Alzheimer’s diseaseAnn Pharmacother201145111416142422028424
- SatoTHanyuHHiraoKKanetakaHSakuraiHIwamotoTEfficacy of PPAR-gamma agonist pioglitazone in mild Alzheimer diseaseNeurobiol Aging20113291626163319923038
- ReadSWuPBiscowMSustained 4-year cognitive and functional response in early Alzheimer’s disease with pioglitazoneJ Am Geriatr Soc201462358458624628640
- HoshikawaYOhkoshiKAssociation between pioglitazone and diabetic macular edemaNippon Ganka Gakkai zasshi2013117435736323767192
- AzarSEl-MollayessGMAl ShaarLSaltiHIBashshurZFImpact of thiazolidinediones on macular thickness and volume in diabetic eyesCan J Ophthalmol201348431231623931472
- HomePDPocockSJBeck-NielsenHRECORD Study TeamRosiglitazone evaluated for cardiovascular outcomes in oral agent combination therapy for type 2 diabetes (RECORD): a multicentre, randomised, open-label trialLancet200937396812125213519501900
- HernandezAVUsmaniARajamanickamAMoheetAThiazolidinediones and risk of heart failure in patients with or at high risk of type 2 diabetes mellitus: a meta-analysis and meta-regression analysis of placebo-controlled randomized clinical trialsAm J Cardiovasc Drugs201111211512821294599
- ViswanathanVMohanVSubramaniPEffect of spironolactone and amiloride on thiazolidinedione-induced fluid retention in South Indian patients with type 2 diabetesClin J Am Soc Nephrol20138222523223184569
- NissenSEWolskiKEffect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causesN Engl J Med2007356242457247117517853
- DormandyJACharbonnelBEcklandDJSecondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trialLancet200536694931279128916214598
- LuCJSunYMuoCHChenRCChenPCHsuCYRisk of stroke with thiazolidinediones: a ten-year nationwide population-based cohort studyCerebrovasc Dis201336214515124029780
- VallarinoCPerezAFuscoGComparing pioglitazone to insulin with respect to cancer, cardiovascular and bone fracture endpoints, using propensity score weightsClin Drug Investig2013339621631
- MahaffeyKWHafleyGDickersonSResults of a reevaluation of cardiovascular outcomes in the RECORD trialAm Heart J20131662240249e24123895806
- FuHXieWCurtisBSchusterDIdentifying factors associated with hypoglycemia-related hospitalizations among elderly patients with T2DM in the US: a novel approach using influential variable analysisCurr Med Res Opin2014291725329826
- van StaaTAbenhaimLMonetteJRates of hypoglycemia in users of sulfonylureasJ Clin Epidemiol19975067357419250272
- ChelliahABurgeMRHypoglycaemia in elderly patients with diabetes mellitus: causes and strategies for preventionDrugs Aging200421851153015182216
- KimMKSukJHKwonMJNateglinide and acarbose for postprandial glucose control after optimizing fasting glucose with insulin glargine in patients with type 2 diabetesDiabetes Res Clin Pract201192332232821376417
- PapaGFedeleVRizzoMRSafety of type 2 diabetes treatment with repaglinide compared with glibenclamide in elderly people: a randomized, open-label, two-period, cross-over trialDiabetes Care20062981918192016873803
- WangJSLinSDLeeWJEffects of acarbose versus glibenclamide on glycemic excursion and oxidative stress in type 2 diabetic patients inadequately controlled by metformin: a 24-week, randomized, open-label, parallel-group comparisonClin Ther201133121932194222078152
- EnçFYImeryüzNAkinLInhibition of gastric emptying by acarbose is correlated with GLP-1 response and accompanied by CCK releaseAm J Physiol Gastrointest Liver Physiol20012813G752G76311518688
- DeLeonMJChandurkarVAlbertSGMooradianADGlucagon-like peptide-1 response to acarbose in elderly type 2 diabetic subjectsDiabetes Res Clin Pract200256210110611891017
- MeneillyGSRyanEARadziukJEffect of acarbose on insulin sensitivity in elderly patients with diabetesDiabetes Care20002381162116710937515
- SangiorgioLAttardoTCondorelliLLunettaMEffects of the treatment with acarbose in elderly overweight type 2 diabetic patients in poor glycemic control with oral hypoglycemic agents or insulinArch Gerontol Geriatr2000311273410989161
- HsiehCJAcarbose reduces the risk of pre-lunch hypoglycemia in elderly people with diabetes eating rice porridge for breakfastDiabetes Res Clin Pract2010893e66e6820619914
- LiCHungYJQamruddinKAzizMFSteinHSchmidtBInternational noninterventional study of acarbose treatment in patients with type 2 diabetes mellitusDiabetes Res Clin Pract2011921576421251726
- SpenglerMSchmitzHLandenHEvaluation of the efficacy and tolerability of acarbose in patients with diabetes mellitus: a postmarketing surveillance studyClin Drug Investig20052510651659
- MertesGSafety and efficacy of acarbose in the treatment of type 2 diabetes: data from a 5-year surveillance studyDiabetes Res Clin Pract200152319320411323089
- BuseJHartKMinasiLThe PROTECT Study: final results of a large multicenter postmarketing study in patients with type 2 diabetes. Precose Resolution of Optimal Titration to Enhance Current TherapiesClin Ther19982022572699589817
- GerminoFWNoninsulin treatment of type 2 diabetes mellitus in geriatric patients: a reviewClin Ther201133121868188222136979
- KaryekarCSRavichandranSAllenEFlemingDFrederichRTolerability and efficacy of glycemic control with saxagliptin in older patients (aged ≥65 years) with inadequately controlled type 2 diabetes mellitusClin Interv Aging2013841943023626461
- StrainWDLukashevichVKothnyWHoellingerMJPaldaniusPMIndividualised treatment targets for elderly patients with type 2 diabetes using vildagliptin add-on or lone therapy (INTERVAL): a 24 week, randomised, double-blind, placebo-controlled studyLancet2013382989040941623706759
- SchweizerADejagerSBosiEComparison of vildagliptin and metformin monotherapy in elderly patients with type 2 diabetes: a 24-week, double-blind, randomized trialDiabetes Obes Metab200911880481219476473
- SchweizerADejagerSFoleyJEShaoQKothnyWClinical experience with vildagliptin in the management of type 2 diabetes in a patient population ≥75 years: a pooled analysis from a database of clinical trialsDiabetes Obes Metab2011131556421114604
- BarnettAHHuismanHJonesRvon EynattenMPatelSWoerleHJLinagliptin for patients aged 70 years or older with type 2 diabetes inadequately controlled with common antidiabetes treatments: a randomised, double-blind, placebo-controlled trialLancet201338299021413142323948125
- BarzilaiNGuoHMahoneyEMEfficacy and tolerability of sitagliptin monotherapy in elderly patients with type 2 diabetes: a randomized, double-blind, placebo-controlled trialCurr Med Res Opin20112751049105821428727
- GiordaCBNadaETartaglinoBPharmacokinetics, safety, and efficacy of DPP-4 inhibitors and GLP-1 receptor agonists in patients with type 2 diabetes mellitus and renal or hepatic impairment. A systematic review of the literatureEndocrine201446340641924510630
- DruckerDJNauckMAThe incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetesLancet200636895481696170517098089
- RosenstockJWilsonCFleckPAlogliptin versus glipizide monotherapy in elderly type 2 diabetes mellitus patients with mild hyperglycaemia: a prospective, double-blind, randomized, 1-year studyDiabetes Obes Metab2013151090691423531118
- AndoYTreatment strategy for elderly diabetic patient with insulin or GLP-1 receptor agonistNihon Rinsho201371111993199824397172
- BodeBWBrettJFalahatiAPratleyREComparison of the efficacy and tolerability profile of liraglutide, a once-daily human GLP-1 analog, in patients with type 2 diabetes ≥65 and <65 years of age: a pooled analysis from phase III studiesAm J Geriatr Pharmacother20119642343322055210
- LinnebjergHKotharePASegerMWolkaAMMitchellMIExenatide – pharmacokinetics, pharmacodynamics, safety and tolerability in patients ≥75 years of age with type 2 diabetesInt J Clin Pharmacol Ther20114929910821255526
- SuzukiDToyodaMKimuraMEffects of liraglutide, a human glucagon-like peptide-1 analogue, on body weight, body fat area and body fat-related markers in patients with type 2 diabetes mellitusIntern Med201352101029103423676586
- FanHPanQXuYYangXExenatide improves type 2 diabetes concomitant with non-alcoholic fatty liver diseaseArq Bras Endocrinol Metabol201357970270824402015
- PonzaniPLong-term effectiveness and safety of liraglutide in clinical practiceMinerva Endocrinol201338110311223435446
- PawaskarMLiQReynoldsMWMetabolic outcomes of elderly patient populations initiating exenatide BID versus insulin glargine in an ambulatory care settingCurr Med Res Opin201228699199722519390
- JacobsenLVHindsbergerCRobsonRZdravkovicMEffect of renal impairment on the pharmacokinetics of the GLP-1 analogue liraglutideBr J Clin Pharmacol200968689890520002084
- Malm-ErjefältMBjørnsdottirIVanggaardJMetabolism and excretion of the once-daily human glucagon-like peptide-1 analog liraglutide in healthy male subjects and its in vitro degradation by dipeptidyl peptidase IV and neutral endopeptidaseDrug Metab Dispos201038111944195320709939
- DavidsonJABrettJFalahatiAScottDMild renal impairment and the efficacy and safety of liraglutideEndocr Pract201117334535521700561
- National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final reportCirculation2002106253143342112485966
- BaysHEGoldbergRBTruittKEJonesMRColesevelam hydrochloride therapy in patients with type 2 diabetes mellitus treated with metformin: glucose and lipid effectsArch Intern Med2008168181975198318852398
- FonsecaVARosenstockJWangACTruittKEJonesMRColesevelam HCl improves glycemic control and reduces LDL cholesterol in patients with inadequately controlled type 2 diabetes on sulfonylurea-based therapyDiabetes Care20083181479148418458145
- GoldbergRBFonsecaVATruittKEJonesMREfficacy and safety of colesevelam in patients with type 2 diabetes mellitus and inadequate glycemic control receiving insulin-based therapyArch Intern Med2008168141531154018663165
- BaysHDujovneCColesevelam HCl: a non-systemic lipid-altering drugExpert Opin Pharmacother20034577979012740000
- RosenbaumDPPetersenJSDucharmeSMarkhamPGoldbergDIAbsorption, distribution and excretion of GT31-104, a novel bile acid sequestrant, in rats and dogs after acute and subchronic administrationJ Pharm Sci19978655915959145384
- OoiCPLokeSCColesevelam for type 2 diabetes mellitusCochrane Database Syst Rev201212CD00936123235674
- GavinJR3rdJonesMRFordDMTruittKESafety and efficacy of Colesevelam HCl in the treatment of elderly patientsDrugs Aging201431646147024777691
- GarberAJAbrahamsonMJBarzilayJIAACE comprehensive diabetes management algorithm 2013Endocr Pract201319232733623598536
- ClarCGillJACourtRWaughNSystematic review of SGLT2 receptor inhibitors in dual or triple therapy in type 2 diabetesBMJ Open201225ii:e001007
- DavisCSFlemingJWWarringtonLESodium glucose co-transporter 2 inhibitors: a novel approach to the management of type 2 diabetes mellitusJ Am Assoc Nurse Pract201426735636324895099
- BolinderJLjunggrenÖKullbergJEffects of dapagliflozin on body weight, total fat mass, and regional adipose tissue distribution in patients with type 2 diabetes mellitus with inadequate glycemic control on metforminJ Clin Endocrinol Metab20129731020103122238392
- BaileyCJGrossJLPietersABastienAListJFEffect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with metformin: a randomised, double-blind, placebo-controlled trialLancet201037597332223223320609968
- Riser TaylorSHarrisKBThe clinical efficacy and safety of sodium glucose cotransporter-2 inhibitors in adults with type 2 diabetes mellitusPharmacotherapy201333998499923744749
- KasichayanulaSChangMHasegawaMPharmacokinetics and pharmacodynamics of dapagliflozin, a novel selective inhibitor of sodium-glucose co-transporter type 2, in Japanese subjects without and with type 2 diabetes mellitusDiabetes Obes Metab201113435736521226818
- KasichayanulaSLiuXShyuWCLack of pharmacokinetic interaction between dapagliflozin, a novel sodium-glucose transporter 2 inhibitor, and metformin, pioglitazone, glimepiride or sitagliptin in healthy subjectsDiabetes Obes Metab2011131475421114603
- KomoroskiBVachharajaniNFengYLiLKornhauserDPfisterMDapagliflozin, a novel, selective SGLT2 inhibitor, improved glycemic control over 2 weeks in patients with type 2 diabetes mellitusClin Pharmacol Ther200985551351919129749
- StenlöfKCefaluWTKimKAEfficacy and safety of canagliflozin monotherapy in subjects with type 2 diabetes mellitus inadequately controlled with diet and exerciseDiabetes Obes Metab201315437238223279307
- FerranniniERamosSJSalsaliATangWListJFDapagliflozin monotherapy in type 2 diabetic patients with inadequate glycemic control by diet and exercise: a randomized, double-blind, placebo-controlled, phase 3 trialDiabetes Care201033102217222420566676
- StrojekKYoonKHHrubaVElzeMLangkildeAMParikhSEffect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with glimepiride: a randomized, 24-week, double-blind, placebo-controlled trialDiabetes Obes Metab2011131092893821672123
- WildingJPWooVSolerNGDapagliflozin 006 Study GroupLong-term efficacy of dapagliflozin in patients with type 2 diabetes mellitus receiving high doses of insulin: a randomized trialAnn Intern Med2012156640541522431673
- BaileyCJGrossJLHennickenDIqbalNMansfieldTAListJFDapagliflozin add-on to metformin in type 2 diabetes inadequately controlled with metformin: a randomized, double-blind, placebo-controlled 102-week trialBMC Med2013114323425012
- ElmoreLKBaggettSKyleJASkelleyJWA review of the efficacy and safety of canagliflozin in elderly patients with type 2 diabetesConsult Pharm201429533534624849690
- ChenK-WTsengH-MHuangY-YChuangY-JThe barriers to initiating insulin therapy among people with type 2 diabetes in Taiwan – a qualitative studyJ Diabetes Metab201235194
- RosenstockJSchwartzSLClarkCMJrParkGDDonleyDWEdwardsMBBasal insulin therapy in type 2 diabetes: 28-week comparison of insulin glargine (HOE 901) and NPH insulinDiabetes Care200124463163611315821
- SorliCWarrenMOyerDMersebachHJohansenTGoughSCElderly patients with diabetes experience a lower rate of nocturnal hypoglycaemia with insulin degludec than with insulin glargine: a meta-analysis of phase IIIa trialsDrugs Aging201330121009101824170235
- LeePChangABlaumCVlajnicAGaoLHalterJComparison of safety and efficacy of insulin glargine and neutral protamine hagedorn insulin in older adults with type 2 diabetes mellitus: results from a pooled analysisJ Am Geriatr Soc2012601515922239291
- Philis-TsimikasACharpentierGClausonPRavnGMRobertsVLThorsteinssonBComparison of once-daily insulin detemir with NPH insulin added to a regimen of oral antidiabetic drugs in poorly controlled type 2 diabetesClin Ther200628101569158117157113
- HorvathKJeitlerKBergholdALong-acting insulin analogues versus NPH insulin (human isophane insulin) for type 2 diabetes mellitusCochrane Database Syst Rev20072CD00561317443605
- BruntonSInitiating insulin therapy in type 2 diabetes: benefits of insulin analogs and insulin pensDiabetes Technol Ther200810424725618715198
- CoscelliCLostiaSLunettaMNosariICoronelGASafety, efficacy, acceptability of a pre-filled insulin pen in diabetic patients over 60 years oldDiabetes Res Clin Pract19952831731778529495
- PapaGFedeleVChiavettaATherapeutic options for elderly diabetic subjects: open label, randomized clinical trial of insulin glargine added to oral antidiabetic drugs versus increased dosage of oral antidiabetic drugsActa Diabetol2008451535918180864
- MooradianADOsterweilDPetrasekDMorleyJEDiabetes mellitus in elderly nursing home patients. A survey of clinical characteristics and managementJ Am Geriatr Soc19883653913963283197
- Gomez-PeraltaFCarraminana-BarreraFFelix-RedondoFJFraile-GomezJExtreme Rescue Study GroupGlycaemic control in patients with type 2 diabetes switching from premixed insulin to long-acting basal insulin analogue plus oral antidiabetic drugs: an observational studyInt J Clin Pract2012661095996822994330
- RezaMTaylorCDTowseKWardJDHendraTJInsulin improves well-being for selected elderly type 2 diabetic subjectsDiabetes Res Clin Pract200255320120711850096
- Sicras-MainarANavarro-ArtiedaRUse of metformin and vildagliptin for treatment of type 2 diabetes in the elderlyDrug Des Devel Ther20148811818
- FerranniniEFonsecaVZinmanBFifty-two-week efficacy and safety of vildagliptin vs glimepiride in patients with type 2 diabetes mellitus inadequately controlled on metformin monotherapyDiabetes Obes Metab200911215716619125777
- MatthewsDRDejagerSAhrenBVildagliptin add-on to metformin produces similar efficacy and reduced hypoglycaemic risk compared with glimepiride, with no weight gain: results from a 2-year studyDiabetes Obes Metab201012978078920649630
- FilozofCGautierJFA comparison of efficacy and safety of vildagliptin and gliclazide in combination with metformin in patients with Type 2 diabetes inadequately controlled with metformin alone: a 52-week, randomized studyDiabet Med201027331832620536495
- GökeBGallwitzBErikssonJHellqvistAGause-Nilsson I; D1680C00001 InvestigatorsSaxagliptin is non-inferior to glipizide in patients with type 2 diabetes mellitus inadequately controlled on metformin alone: a 52-week randomised controlled trialInt J Clin Pract201064121619163120846286
- GallwitzBRosenstockJRauchT2-year efficacy and safety of linagliptin compared with glimepiride in patients with type 2 diabetes inadequately controlled on metformin: a randomised, double-blind, non-inferiority trialLancet2012380984047548322748821
- AschnerPChanJOwensDREASIE InvestigatorsInsulin glargine versus sitagliptin in insulin-naive patients with type 2 diabetes mellitus uncontrolled on metformin (EASIE): a multicentre, randomised open-label trialLancet201237998332262226922683131
- NauckMAMeiningerGShengDTerranellaLSteinPPSitagliptin StudyGEfficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, compared with the sulfonylurea, glipizide, in patients with type 2 diabetes inadequately controlled on metformin alone: a randomized, double-blind, non-inferiority trialDiabetes Obes Metab20079219420517300595
- AhrénBFoleyJEFerranniniEChanges in prandial glucagon levels after a 2-year treatment with vildagliptin or glimepiride in patients with type 2 diabetes inadequately controlled with metformin monotherapyDiabetes Care201033473073220067974
- ForstTDworakMBerndt-ZipfelCEffect of vildagliptin compared to glimepiride on postprandial proinsulin processing in the beta cell of patients with type 2 diabetes mellitusDiabetes Obes Metab201315657657923384119
- HeYLFoteinosGNeelakanthamSDifferential effects of vildagliptin and glimepiride on glucose fluctuations in patients with type 2 diabetes mellitus assessed using continuous glucose monitoringDiabetes Obes Metab201315121111111923782529
- GuerciBMonnierLSerusclatPContinuous glucose profiles with vildagliptin versus sitagliptin in add-on to metformin: results from the randomized Optima studyDiabetes Metab201238435936622809630
- ViriatoDCaladoFGruenbergerJBCost-effectiveness of metformin plus vildagliptin compared with metformin plus sulphonylurea for the treatment of patients with type 2 diabetes mellitus: a Portuguese healthcare system perspectiveJ Med Econ201417749950724708176
- GranstromOBergenheimKMcEwanPSennfaltKHenrikssonMCost-effectiveness of saxagliptin (Onglyza(R)) in type 2 diabetes in SwedenPrim Care Diabetes20126212713622001114
- TakihataMNakamuraATajimaKComparative study of sitagliptin with pioglitazone in Japanese type 2 diabetic patients: the COMPASS randomized controlled trialDiabetes Obes Metab201315545546223279373
- BolliGDottaFRochotteECohenSEEfficacy and tolerability of vildagliptin vs pioglitazone when added to metformin: a 24-week, randomized, double-blind studyDiabetes Obes Metab2008101829018034842
- BolliGDottaFColinLMinicBGoodmanMComparison of vildagliptin and pioglitazone in patients with type 2 diabetes inadequately controlled with metforminDiabetes Obes Metab200911658959519515179
- UmpierrezGIssaMVlajnicAGlimepiride versus pioglitazone combination therapy in subjects with type 2 diabetes inadequately controlled on metformin monotherapy: results of a randomized clinical trialCurr Med Res Opin200622475175916684436
- MatthewsDRCharbonnelBHHanefeldMBrunettiPSchernthanerGLong-term therapy with addition of pioglitazone to metformin compared with the addition of gliclazide to metformin in patients with type 2 diabetes: a randomized, comparative studyDiabetes Metab Res Rev200521216717415386821
- CharbonnelBSchernthanerGBrunettiPLong-term efficacy and tolerability of add-on pioglitazone therapy to failing monotherapy compared with addition of gliclazide or metformin in patients with type 2 diabetesDiabetologia20054861093110415889234
- CefaluWTLeiterLAYoonKHEfficacy and safety of canagliflozin versus glimepiride in patients with type 2 diabetes inadequately controlled with metformin (CANTATA-SU): 52 week results from a randomised, double-blind, phase 3 non-inferiority trialLancet2013382989694195023850055
- Lavalle-GonzálezFJJanuszewiczADavidsonJEfficacy and safety of canagliflozin compared with placebo and sitagliptin in patients with type 2 diabetes on background metformin monotherapy: a randomised trialDiabetologia201356122582259224026211
- SchernthanerGGrossJLRosenstockJCanagliflozin compared with sitagliptin for patients with type 2 diabetes who do not have adequate glycemic control with metformin plus sulfonylurea: a 52-week randomized trialDiabetes Care20133692508251523564919
- DerosaGSalvadeoSAD’AngeloAMetabolic effect of repaglinide or acarbose when added to a double oral antidiabetic treatment with sulphonylureas and metformin: a double-blind, cross-over, clinical trialCurr Med Res Opin200925360761519232035
- DerosaGMereuRD’AngeloAEffect of pioglitazone and acarbose on endothelial inflammation biomarkers during oral glucose tolerance test in diabetic patients treated with sulphonylureas and metforminJ Clin Pharm Ther201035556557920831680
- DerosaGCiceroAFFranzettiIGA comparison between sitagliptin or glibenclamide in addition to metformin + pioglitazone on glycaemic control and beta-cell function: the triple oral therapyDiabet Med201330784685423413771
- OsonoiTSaitoMTamasawaAIshidaHOsonoiYEffects of sitagliptin or mitiglinide as an add-on to acarbose on daily blood glucose fluctuations measured by 72 h subcutaneous continuous glucose monitoring in Japanese patients with type 2 diabetes: a prospective randomized studyExpert Opin Pharmacother201415101325133524866329
- ArechavaletaRSeckTChenYEfficacy and safety of treatment with sitagliptin or glimepiride in patients with type 2 diabetes inadequately controlled on metformin monotherapy: a randomized, double-blind, non-inferiority trialDiabetes Obes Metab201113216016821199268
- CerielloAJohnsDWidelMEcklandDJGilmoreKJTanMHComparison of effect of pioglitazone with metformin or sulfonylurea (monotherapy and combination therapy) on postload glycemia and composite insulin sensitivity index during an oral glucose tolerance test in patients with type 2 diabetesDiabetes Care200528226627215677777
- PfütznerASchöndorfTTschöpeDPIOfix-study: effects of pioglitazone/metformin fixed combination in comparison with a combination of metformin with glimepiride on diabetic dyslipidemiaDiabetes Technol Ther201113663764321457065
- CharbonnelBSteinbergHEymardEEfficacy and safety over 26 weeks of an oral treatment strategy including sitagliptin compared with an injectable treatment strategy with liraglutide in patients with type 2 diabetes mellitus inadequately controlled on metformin: a randomised clinical trialDiabetologia20135671503151123604551
