?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
COPD is concomitantly present in ~30% of patients with heart failure. Here, we investigated the pulmonary function test parameters for left ventricular (LV) diastolic dysfunction and the relationship between pulmonary function and LV diastolic function in patients with COPD.
Patients and methods
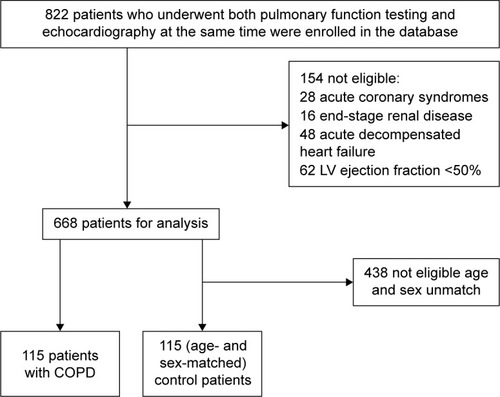
Overall, 822 patients who underwent a pulmonary function test and echocardiography simultaneously between January 2011 and December 2012 were evaluated. Finally, 115 patients with COPD and 115 age- and sex-matched control patients with an LV ejection fraction of ≥50% were enrolled.
Results
The mean age of the patients was 74.4±10.4 years, and 72.3% were men. No significant differences were found between the two groups regarding comorbidities, such as hypertension, diabetes mellitus, and anemia. The index of LV diastolic function (E/e′) and the proportion of patients with high E/e′ (defined as E/e′ ≥15) were significantly higher in patients with COPD than in control patients (10.5% vs 9.1%, P=0.009; 11.3% vs 4.3%, P=0.046). E/e′ was significantly correlated with the residual volume/total lung capacity ratio. Univariate and multivariate analyses revealed severe COPD (Global Initiative for Chronic Obstructive Lung Disease III or IV) to be a significant predictive factor for high E/e′ (odds ratio [OR] 5.81, 95% confidence interval [CI] 2.13–15.89, P=0.001 and OR 6.00, 95% CI 2.08–17.35, P=0.001, respectively).
Conclusion
Our data suggest that LV diastolic dysfunction as a complication of COPD may be associated with mechanical exclusion of the heart by pulmonary overinflation.
Introduction
COPD is a systemic inflammatory disease characterized by airflow limitation that is not fully reversible.Citation1 COPD is complicated by a high rate of cardiac diseasesCitation2 and is present in approximately one-third of patients with congestive heart failure (HF).Citation3,Citation4 Patients with HF with preserved ejection fraction (pEF) are more likely to have a history of COPD compared with patients with HF with reduced ejection fraction.Citation5 A proposed paradigm for pEF in patients with HF identifies a systemic proinflammatory state induced by comorbidities, such as COPD, diabetes mellitus (DM), hypertension (HTN), and obesity. This proinflammatory state leads to structural and functional myocardial alterations via increased oxidative stress in the vascular endothelium.Citation6 Previous studies have examined the relationship between forced expiratory volume and heart disease. Barr et alCitation7 found that an impaired endothelial function was associated with low forced expiratory volume in 1 second (FEV1) and high-resolution computed tomography percentage of emphysema in former smokers early in COPD. In a population-based study, a greater extent of emphysema on computed tomography and more severe airflow obstruction were linearly related to impaired left ventricular (LV) filling, reduced stroke volume, and lower cardiac output without changes in the ejection fraction.Citation8 Hole et alCitation9 found a significant inverse relationship between FEV1 and death due to ischemic heart disease and stroke. Previous Doppler studies have demonstrated that left ventricular diastolic dysfunction (LVDD) is frequently found in severe patients with COPD.Citation10,Citation11 However, these studies had a small sample size, excluded mild-to-moderate COPD, and did not use tissue Doppler echocardiography, which is more accurate than Doppler LV inflow study for detecting LVDD. According to the Heart Failure and Echocardiography Associations of the European Society of Cardiology, diagnostic evidence of diastolic LV dysfunction can be obtained noninvasively by tissue Doppler (E/e′ ≥15).Citation12 Thus, here, we evaluated LV diastolic function using tissue Doppler echocardiography in mild-to-moderate patients with COPD.
Our objectives were to evaluate the incidences of LVDD among the COPD and control groups with respiratory failure, determine the relationship between pulmonary function test (PFT) parameters and LVDD (E/e′), and determine the predictive factor of a high E/e′ (defined as E/e′ ≥15) as an index of severe LVDD.Citation12
Patients and methods
Study design
Overall, 822 consecutive patients who underwent both PFT and echocardiography simultaneously (within 3 months) for determining the cause of respiratory failure between January 2011 and December 2012 were evaluated (). The age criterion was ≥20 years. The exclusion criteria were presence of acute coronary syndromes (n=28), including acute myocardial infarction, end-stage renal disease requiring dialysis (n=16), past history of acute decompensated HF (n=48), or LV ejection fraction <50% (n=62). COPD was diagnosed according to the Global Initiative for Chronic Obstructive Lung Disease criteria.Citation13 Finally, 115 patients with COPD and 115 age- and sex-matched control patients with an LV ejection fraction of ≥50% were enrolled. The control group included patients with interstitial pneumonia (n=69), lung cancer (n=13), tuberculosis (n=9), and other diseases (n=24). The health statuses of patients were obtained using electronic clinical records. This retrospective study was conducted using data from a large university hospital. The protocol used complied with the Declaration of Helsinki and was approved by our institutional ethics committee of Nippon Medical School, which waived the need for patient consent owing to the retrospective nature of the study.
Relevant factors
The heart rate and systolic blood pressure were simultaneously measured at rest using electrocardiography. Height and weight were measured at the time of PFT, and the body mass index (kg/m2) was calculated as an index of obesity. HTN was defined as systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or current use of antihypertensive agents. DM was defined as fasting plasma glucose level ≥126.0 mg/dL and 2-hour plasma glucose level >200 mg/dL during an oral glucose tolerance test or current treatment with antidiabetic agents.Citation14
Anemia was defined as hemoglobin level <13 g/dL in men and <12 g/dL in women. Chronic kidney disease (CKD) was defined as glomerular filtration rate ≤60 mL/min/1.73 m2; this value was estimated using the simplified prediction equation derived from the Modification of Diet in Renal Disease study.Citation15 Clinical data were obtained from PFTs or echocardiography when the hemodynamic conditions of the patients had stabilized.
Echocardiography parameters
Transthoracic echocardiography was recorded using an iE33 system (Philips Medical Systems, Bothell, WA, USA). We conducted standard, comprehensive, motion-mode (M-mode), two-dimensional echocardiography and Doppler studies according to the American Society of Echocardiog-raphy guidelines.Citation16 The left auricle diameter, left ventricle end-systolic and end-diastolic diameters, interventricular septal thickness, and posterior wall thickness were measured using M-mode echocardiography from the left parasternal short- and long-axis views. The LV ejection fraction was calculated using the modified Simpson’s method. The tri-cuspid regurgitation velocity was obtained by continuous wave Doppler imaging from the right ventricular inflow or the apical four-chamber view position. The transtricuspid pressure gradient (TRPG) was calculated as follows:
The peak early diastolic phase (E) and late diastolic phase (A) mitral inflow velocities and the E/A ratio were measured using pulsed-wave Doppler echocardiography with the sample volume between the mitral leaflet tips. The mitral annular velocity (E′) and mean E/e′ ratio were measured at the septal and lateral annulus using tissue Doppler imaging.
PFT
Pre- and postbronchodilator PFTs were performed using CHSETAC-8900 (Nihon Kohden, Tokyo, Japan), according to the American Thoracic Society (ATS) guidelines.Citation17 We performed spirometry (forced vital capacity [FVC], FEV1, and the FEV1/FVC ratio) and plethysmography (total lung capacity [TLC], residual volume [RV], and the RV/TLC ratio). Spirometry quality was assessed according to the ATS/European Respiratory Society recommendations.Citation18 COPD and COPD severity were defined according to the ATS/European Respiratory Society COPD criteria by using postbronchodilator measures of pulmonary function.Citation19
Statistical analyses
The SPSS software package Version 20.0 (IBM Corporation, Armonk, NY, USA) was used for statistical analyses. All continuous values and categorical variables are expressed as mean ± standard deviation and the number and percentage of patients, respectively. We compared the control and COPD groups using the unpaired t-test. The relationships between PFT parameters and LVDD were tested using Pearson’s correlation. Univariate and multivariable logistic regression analyses were performed to identify potential risk factors for a high E/e′. Age, sex, obesity, anemia, HTN, DM, atrial fibrillation (AF), COPD stage, anemia, and CKD had planned inclusion in the original model. To assess the robustness of the planned model, other potential factors among the baseline characteristics were considered for inclusion in the multivariate model by stepwise selection (significance level for inclusion 0.10). A two-sided probability value of P<.05 was considered statistically significant.
Results
shows the clinical characteristics of all patients. No significant differences were found between the COPD and control groups in terms of body mass index; prevalence of HTN, DM, AF, or CKD; brain natriuretic peptide levels; hemoglobin levels; LV ejection fraction; or TRPG. However, the COPD group had a significantly higher Brinkman index for smoking compared with the control group. In the COPD group, the COPD severity according to the global initiative was COPD I in 33 (28.7%) patients, II in 42 (36.5%) patients, III in 25 (21.8%) patients, and IV in 15 (13.0%) patients.
Table 1 Clinical characteristics of the study population
Echocardiography and PFT parameters
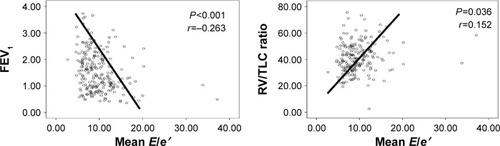
The echocardiography and PFT parameters of the two groups are shown in . E, mean E/e′ ratio, and the proportion of high E/e′ as an index of severe LVDD were significantly higher in the COPD group than in the control group. The proportion of high E/e′ was significantly higher in the severe COPD (Global Initiative for Chronic Obstructive Lung Disease III or IV) group than in the control group. However, no difference was found in the proportion of high E/e′ between the severe COPD group and mild-to-moderate COPD (Global Initiative for Chronic Obstructive Lung Disease I or II) group (17.5% vs 8.0%, P=0.320; ). No significant differences were observed between the two groups regarding standard M-mode echocardiography parameters. The COPD group had a significantly lower FEV1 and FEV1/FVC ratio and a higher RV and RV/TLC ratio compared with the control group. The mean E/e′ ratio was significantly negatively correlated with FEV1 and positively correlated with the RV/TLC ratio of PFT (). However, no significant associations were found between other PFT parameters and the mean E/e′ ratio ().
Table 2 Echocardiography and pulmonary function test parameters of the study population
Table 3 The relationship between PFT parameters and mean E/e′
Figure 2 Proportion of high E/e′ in each group.
Notes: Proportion of high E/e′ was significantly higher in the severe COPD group (Global Initiative for Chronic Obstructive Lung Disease III or IV) than in the control group (17.5% vs 4.3%, P=0.041). However, no difference was found in the proportion of high E/e′ between the severe COPD group and the mild-to-moderate COPD group (Global Initiative for Chronic Obstructive Lung Disease I or II; 17.5% vs 8.0%, P=0.320). P-value obtained using unpaired t-test.
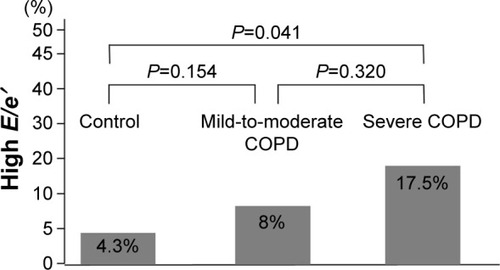
Figure 3 Correlation between mean E/e′ and FEV1 or RV/TLC ratio in all patients (n=230).
Abbreviations: FEV1, forced expiratory volume in 1 second; RV, residual volume; TLC, total lung capacity.
Univariate analysis revealed AF, severe COPD, and anemia to be significant predictive factors for high E/e′, while multivariate analysis revealed severe COPD and anemia to be significant predictive factors for high E/e′ ().
Table 4 The odds ratio of prediction for high E/e′
Discussion
This study is a complete, noninvasive hemodynamic investigation of patients with COPD by using echocardiography and PFTs. Our evaluations of mitral inflow and mitral annular velocities confirmed changes in LVDD in patients with COPD compared with the control patients. A significant increase in the E/e′ ratio was noted in the COPD group. We observed a weak but significant linear association of LVDD as measured by echocardiography, with both postbronchodilator FEV1 and the RV/TLC ratio. Univariate and multivariate analyses revealed severe COPD to be a significant predictive factor for high E/e′. Our data suggest that the cause for LVDD as a complication of COPD includes mechanical exclusion of the heart by pulmonary overinflation.
Many factors contribute to the underlying cause of LVDD in patients with COPD. First, hypoxia and a systemic proinflammatory state lead to atherosclerosis via increased oxidative stress in the vascular endothelium.Citation6,Citation7 Second, the severity of hypoxemia and pulmonary artery pressure or pulmonary vascular resistance has been reported to be closely in patients with COPD, indicating a major role in alveolar hypoxia.Citation20–Citation23 Alveolar hypoxia causes constriction of resistance pulmonary arteries, and sustained alveolar hypoxia induces pulmonary vascular remodeling.Citation24 Pulmonary HTN is observed in half of the patients with severe COPD.Citation25 Moreover, ~25% of mild-to-moderate patients with COPD without resting pulmonary HTN at onset will develop pulmonary HTN during a 6-year follow-up.Citation26 Therefore, pulmonary HTN induced by pulmonary vascular remodeling may associate with the LVDD observed in patients with COPD. Third, we demonstrated that the mean E/e′ ratio as a parameter of LVDD was significantly negatively correlated with FEV1 and positively correlated with the RV/TLC ratio of PFT. It may be explained to lead to mechanical exclusion of the heart by pulmonary overinflation. Hyperinflation in very severe patients with COPD can cause increased intrathoracic pressure and decreased venous pressure, with reductions in the blood volumes of both ventricles.Citation27 Such ventricular interdependence can impair LV filling, causing the LVDD in patients with severe COPDCitation10,Citation28 and mild-to-moderate COPD.Citation8 In this study, we demonstrated that severe COPD was a significant predictive factor for high E/e′. As a result, hyperinflation may lead to LVDD.
Study limitations
The main limitations of this study were the relatively small sample size and the retrospective design. Moreover, the control group included patients with interstitial pneumonia, lung cancer, tuberculosis, and other diseases. Therefore, the control group may need to be limited to a generally healthy cohort in future studies. Previous data suggest that patients with HF with pEF tend to be older with a female predominance.Citation5,Citation29 Age is one of the most cited factors affecting LV filling.Citation30 However, in this study, the control subjects and patients with COPD were age and sex matched. The COPD group had a significantly higher Brinkman index for smoking compared with that of the control group. Smoking itself may cause subclinical changes in the LV function.Citation31 However, the Brinkman index did not significantly correlate with E/e′ in our study. Hence, further prospective, large-scale clinical studies are needed.
Conclusion
LVDD as a complication of COPD may be associated with mechanical exclusion of the heart by pulmonary overinflation. Performing PFT for patients with HF, timely diagnosis of COPD and further intervention therapy may lead to pathological improvement and a greater understanding of COPD.
Acknowledgments
The authors thank Dr Yukichi Tokita and Dr Masatomo Yoshikawa for their help in collecting patients’ data.
Disclosure
The authors report no conflicts of interest in this work.
References
- FabbriLMLuppiFBeghéBRabeKFComplex chronic comorbidities of COPDEur Respir J20083120421218166598
- DivoMCoteCde TorresJPComorbidities and risk of mortality in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med201218615516122561964
- LainscakMClelandJGLenzenMJFollathFKomajdaMSwedbergKInternational variations in the treatment and co-morbidity of left ventricular systolic dysfunction: data from the EuroHeart Failure SurveyEur J Heart Fail2007929229917023204
- HawkinsNMPetrieMCJhundPSChalmersGWDunnFGMcMurrayJJHeart failure and chronic obstructive pulmonary disease: diagnostic pitfalls and epidemiologyEur J Heart Fail20091113013919168510
- BhatiaRSTuJVLeeDSOutcome of heart failure with preserved ejection fraction in a population-based studyN Engl J Med200635526026916855266
- PaulusWJTschöpeCA novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammationJ Am Coll Cardiol20136226327123684677
- BarrRGMesia-VelaSAustinJHImpaired flow-mediated dilation is associated with low pulmonary function and emphysema in ex-smokers: the Emphysema and Cancer Action Project (EMCAP) StudyAm J Respir Crit Care Med20071761200120717761614
- BarrRGBluemkeDAAhmedFSPercent emphysema, airflow obstruction, and impaired left ventricular fillingN Engl J Med201036221722720089972
- HoleDJWattGCDavey-SmithGHartCLGillisCRHawthorneVMImpaired lung function and mortality risk in men and women: findings from the Renfrew and Paisley prospective population studyBMJ1996313711715 discussion 715–7168819439
- BoussugesAPinetCMolenatFLeft atrial and ventricular filling in chronic obstructive pulmonary disease. An echocardiographic and Doppler studyAm J Respir Crit Care Med200016267067510934104
- WatzHWaschkiBBoehmeCClaussenMMeyerTMagnussenHExtrapulmonary effects of chronic obstructive pulmonary disease on physical activity: a cross-sectional studyAm J Respir Crit Care Med200817774375118048807
- PaulusWJTschopeCSandersonJEHow to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of CardiologyEur Heart J2007282539255017428822
- RabeKFHurdSAnzuetoAGlobal strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summaryAm J Respir Crit Care Med200717653255517507545
- Diagnosis and classification of diabetes mellitusDiabetes Care201437Suppl 1S81S9024357215
- LeveyASBoschJPLewisJBA more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study GroupAnn Intern Med199913046147010075613
- SchillerNBShahPMCrawfordMRecommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional EchocardiogramsJ Am Soc Echocardiogr198923583672698218
- Standardization of Spirometry, 1994 Update. American Thoracic SocietyAm J Respir Crit Care Med1995152110711367663792
- MillerMRCrapoRHankinsonJGeneral considerations for lung function testingEur Respir J20052615316115994402
- CelliBRMacNeeWStandards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paperEur Respir J20042393294615219010
- ChaouatANaeijeRWeitzenblumEPulmonary hypertension in COPDEur Respir J2008321371138518978137
- ChatilaWMThomashowBMMinaiOACrinerGJMakeBJComorbidities in chronic obstructive pulmonary diseaseProc Am Thorac Soc2008554955518453370
- FalkJAKadievSCrinerGJScharfSMMinaiOADiazPCardiac disease in chronic obstructive pulmonary diseaseProc Am Thorac Soc2008554354818453369
- ScharfSMIqbalMKellerCHemodynamic characterization of patients with severe emphysemaAm J Respir Crit Care Med200216631432212153963
- MinaiOAChaouatAAdnotSPulmonary hypertension in COPD: epidemiology, significance, and management: pulmonary vascular disease: the global perspectiveChest201013739S51S20522579
- ThabutGDauriatGSternJBPulmonary hemodynamics in advanced COPD candidates for lung volume reduction surgery or lung transplantationChest20051271531153615888824
- KesslerRFallerMWeitzenblumE“Natural history” of pulmonary hypertension in a series of 131 patients with chronic obstructive lung diseaseAm J Respir Crit Care Med200116421922411463591
- JörgensenKMüllerMFNelJUptonRNHoultzERickstenSEReduced intrathoracic blood volume and left and right ventricular dimensions in patients with severe emphysema: an MRI studyChest20071311050105717426209
- Vonk NoordegraafAMarcusJTRoseboomBPostmusPEFaesTJde VriesPMThe effect of right ventricular hypertrophy on left ventricular ejection fraction in pulmonary emphysemaChest19971126406459315795
- OwanTEHodgeDOHergesRMJacobsenSJRogerVLRedfieldMMTrends in prevalence and outcome of heart failure with preserved ejection fractionN Engl J Med200635525125916855265
- KleinALBurstowDJTajikAJZachariahPKBaileyKRSewardJBEffects of age on left ventricular dimensions and filling dynamics in 117 normal personsMayo Clin Proc1994692122248133658
- LichodziejewskaBKurnickaKGrudzkaKMalyszJCiurzynskiMLiszewska-PfejferDChronic and acute effects of smoking on left and right ventricular relaxation in young healthy smokersChest20071311142114817426221