Abstract
Oxygen is a commonly used drug in the clinical setting and like other drugs its use must be considered carefully. This is particularly true for those patients who are at risk of type II respiratory failure in whom the risk of hypercapnia is well established. In recent times, several international bodies have advocated for the prescription of oxygen therapy in an attempt to reduce this risk in vulnerable patient groups. Despite this guidance, published data have demonstrated that there has been poor uptake of these recommendations. Multiple interventions have been tested to improve concordance, and while some of these interventions show promise, the sustainability of these interventions are less convincing. In this review, we summarize data that have been published on the prevalence of oxygen prescription and the accurate and appropriate administration of this drug therapy. We also identify strategies that have shown promise in facilitating changes to oxygen prescription and delivery practice. There is a clear need to investigate the barriers, facilitators, and attitudes of clinicians in relation to the prescription of oxygen therapy in acute care. Interventions based on these findings then need to be designed and tested to facilitate the application of evidence-based guidelines to support sustained changes in practice, and ultimately improve patient care.
Introduction
Oxygen is a commonly used drug in the clinical settingCitation1–Citation4 and unquestionably saves lives. However, its use must be carefully considered. Like any drug, it may cause harm when used inappropriately.Citation4,Citation5 In practice, a common misconception that “you can’t give too much oxygen”Citation1,Citation3 or “oxygen won’t hurt”Citation4 has emerged. This has led to higher levels of oxygen therapy being delivered to patients who are critically unwell or who complain of dyspnea,Citation3 resulting in increased lengths of stay,Citation6 higher rates of admission to high dependency units,Citation6 and an increased risk of death.Citation7,Citation8 Indeed, NewCitation9 states that in the past ambulance crews regarded oxygen as a sort of “medical wet wipe […] not always therapeutic, but never harmful.”
The clinical effect supplemental oxygen can have on patients experiencing acute exacerbations of chronic obstructive pulmonary disease (COPD) is now widely known,Citation10 yet not completely understood.Citation11 Uncontrolled oxygen administration, particularly when delivered at high concentrations, can result in a worsening of hypercapnia.Citation12,Citation13 Multiple pathological mechanisms are believed to underlie this phenomenon,Citation11,Citation12,Citation14,Citation15 with the primary causes being the inhibition of pulmonary vasoconstriction. Resulting in a worse ventilation/perfusion mismatch, and a right-hand shift of the CO2 dissociation curve (Haldane effect), further increasingPaCO2.Citation13,Citation16 Other mechanisms for this phenomenon include further increases in ventilation/perfusion mismatching due to absorption atelectasis and an increased work of breathing due to the higher density of oxygen over air.Citation17 Initial beliefs that hypercapnia was primarily caused as a result of a “reduced hypoxic drive” have been largely disproved,Citation18 following the publication of results challenging these earlier hypothesis. In 1980, Aubier et alCitation18 demonstrated that while minute ventilation initially fell with the administration of high concentrations of oxygen therapy in the COPD patient cohort, this decrease was transient, with minute ventilation returning to levels only marginally lower than when breathing room air initially.
For these reasons, the use of titrated oxygen therapy in this patient group has been advocated for many years. Guidance from the British Thoracic Society (BTS),Citation17 the Global Initiative for Obstructive Lung DiseaseCitation19 and, more recently, the Thoracic Society of Australia and New ZealandCitation20 advise clinicians to administer oxygen to maintain an SpO2 between 88% and 92% in an acute hospital setting for patients with COPD and others who are vulnerable. While COPD is the most common chronic disease in clinical practice to cause hypercapnia,Citation17 other vulnerable patient groups are also at risk. These include those patients with morbid obesity, obstructive sleep apnea, cystic fibrosis, neuromuscular disorders, those with restrictive chest wall deformities, and those using respiratory depressant drugs, such as opioids and benzodiazepines.Citation17,Citation21 In patients who are not at risk of hypercapnic respiratory failure, recommendations vary between professional bodies, with the BTSCitation17,Citation21 advocating for maintenance of an SpO2 between 94% and 98% and the Thoracic Society of Australia and New ZealandCitation20 recommending maintenance of an SpO2 between 92% and 96%. Undoubtedly, the accurate delivery of oxygen therapy is important for all patients; however, the deleterious effects of poor clinical practice in this area are most significant and now well documented in those patients who are vulnerable, particularly those with COPD.Citation7,Citation22–Citation27 Austin et alCitation7 were the first to show clear evidence of the benefits of administering titrated oxygen (delivered via nasal prongs to achieve an SpO2 between 88% and 92%) to patients with acute exacerbations of COPD. Their results demonstrated that the delivery of titrated oxygen therapy reduced mortality by 58% when compared with those who received high flow oxygen therapy (delivered via a nonrebreather mask at 8–10 L/min).Citation7 A retrospective review of ambulance practice, conducted by Cameron et al,Citation28 illustrates this point. This study demonstrated that 80% of the patients with COPD brought in to the emergency department by ambulance had received high concentrations of oxygen during initial response and transfer. They reported an increased risk of serious adverse outcomes in patients who were both hypoxemic and hyperoxemic when compared to those who were normoxemic. However, hypercapnia and acidosis were more pronounced in the hyperoxemic group.
Many authorsCitation3,Citation11,Citation29–Citation33 and professional bodiesCitation17,Citation20 argue that oxygen should be treated like other drugs with orders for therapy included on a treatment (drug) chart to improve accurate administration. However, prescription of oxygen therapy has been historically poor, and compliance with or adherence to the written prescription has not been consistently demonstrated. This review examines the literature that has explored prescribing practices internationally with a variety of interventions employed in attempts to improve prescription, administration, and consequently patient outcomes.
Oxygen prescription
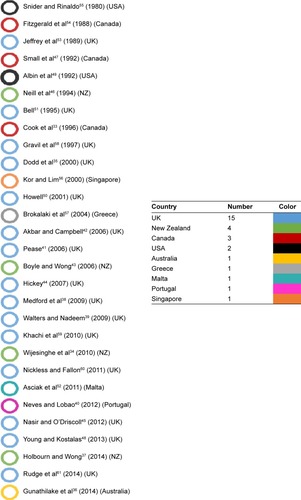
The adequacy of oxygen prescription within the acute hospital setting has been studied over many years.Citation34–Citation54 These studies have explored both the presence of a prescription and the adequacy and appropriateness of oxygen prescription in a broad range of patient groups. The literature includes studies specific to vulnerable groups, including those with chronic ventilatory failure, but is not limited to this population with evaluation being undertaken in the general clinical setting. However, since the publication of the BTS Guidelines on acute oxygen administration in 2008, there has been an increasing interest in this topic. depicts a timeline of papers (according to the geographical area that the studies were conducted) that have been published on oxygen therapy prescription and administration practices since 1980. Interestingly, over 27 years, between 1980 and 2007, 17 papersCitation33,Citation35,Citation41–Citation44,Citation46,Citation47,Citation49–Citation51,Citation53–Citation58 were found that discussed oxygen prescription rates and/or the appropriateness and accuracy of oxygen administration and subsequent monitoring of oxygen therapy. In the 6 years between 2009 and 2015, 12 papers which measured the accurate or appropriate prescription of oxygen therapy have been reported.Citation34,Citation36–Citation40,Citation45,Citation48,Citation52,Citation59–Citation61 Some of these papers also discussed various interventions that have been tested to improve prescription practices.
Figure 1 Timeline of papers published on oxygen therapy prescription and administration practices.
Overall, the literature suggests that the practice of prescribing oxygen therapy is poor.Citation34–Citation39,Citation41–Citation44,Citation46,Citation47,Citation49,Citation51,Citation52
Various reasons have been proposed for this, including:
insufficient training and education for medical and nursing staff;Citation33,Citation39,Citation41,Citation42,Citation47,Citation51,Citation54,Citation62
a lack of familiarity with oxygen delivery devices;Citation51
a lack of understanding of the effects, role and dangers of oxygen therapy;Citation35–Citation37,Citation46,Citation61
staff time constraints;Citation48
necessity to maintain SpO2 >94% due to the “between the flags” track and trigger observations charts;Citation36
practical issues related to space and place for prescribing oxygen;Citation35,Citation39,Citation61
difficulties with changing long established behavior;Citation36,Citation60
patients transferred from other wards/departments with oxygen therapy already in situ;Citation44
lack of enthusiasm by senior clinical staff;Citation44
communication difficulties between doctors and nurses;Citation36
lack of full time staff or staff turnover.Citation36,Citation38,Citation48,Citation60
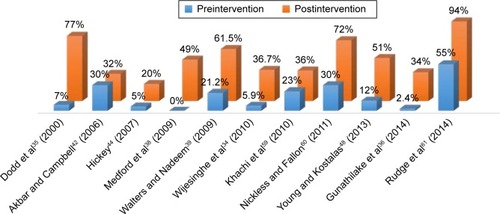
In attempts to improve overall prescription rates, different interventions have been tested in various combinations over different periods of time, with varying degrees of success. Interventions that have been employed are presented in and the degree of change achieved pre- and postintervention is presented graphically in . These interventions include:
introduction of oxygen alert stickers;Citation39,Citation59–Citation61
dedicated oxygen order chart;Citation35
clearly delineated section on the drug chart or changes to the drug chart to include space for the transcription of oxygen orders;Citation34–Citation36,Citation48,Citation60
informational posters;Citation59–Citation61
email notification/dissemination of information;Citation60,Citation61
educational session across various clinical specialties and at various key times;Citation34,Citation36,Citation39,Citation44,Citation48,Citation56,Citation59–Citation61
nurse facilitated reminder system;Citation38
development of hospital guidelines/policy to guide practice;Citation36,Citation42,Citation59,Citation60
admission bundle with electronic prescribing system;Citation45
message alerts on computer login screens.Citation60
Table 1 Interventions that have been tested in attempts to improve oxygen prescription rates
Figure 2 Accurate prescription of oxygen therapy: preintervention–postintervention study results.
One studyCitation42 demonstrated no or minimal improvement in prescribing practices after implementing an oxygen guideline to inform clinician practice. Despite no change in prescriber behavior, a large improvement was seen in the administration of oxygen according to the prescribed dose (70% vs 95%; P=0.043) and in the clinical assessment of all patients commenced on oxygen therapy, that is, increased measurement of pulse oximetry (69% vs 91%; P=0.001). The assessment of arterial blood gases for those with respiratory disease improved following the introduction of the guideline (from 65% to 87%; statistical significance was not reported) with even greater improvements seen in the reevaluation of arterial blood gases following initiation of oxygen therapy for the cohort with airways disease, increasing to 68% from 34% (P=0.037). The authorsCitation42 concluded that although little change was seen in the prescribing practices of the doctors, practice improvements were seen. Junior doctors reassessed arterial blood gases more frequently and nurses administered the prescribed dose more frequently and used pulse oximetry more often to assess patients after the introduction of the guidelines.Citation42 Similar improvements in administration and assessment have been seen in some practice areas in other studiesCitation34,Citation38 but not in othersCitation47 in which the presence of an accurate prescription did not improve oxygen administration and assessment practices in these patients.
Rudge et alCitation61 described a promising quality improvement project that occurred over three cycles which demonstrated dramatic improvements to the accurate prescription of oxygen therapy. Baseline data showed that 55% of patients using oxygen had a valid prescription; this then decreased to 54% following cycle one, but improved to 94% at the end of cycle three. They used four interventions (oxygen prescription chart, oxygen alert stickers, point of care resources, and senior led educational sessions) over a 2-year period on an Acute Medical Unit.Citation61 While these data are encouraging, there are limitations with the study design; it was a quality improvement audit conducted in one unit of a single hospital and interventions were ongoing both prior to and during the data collection phase.
Similarly, in an earlier audit undertaken by Dodd et al,Citation35 a large improvement was seen in written prescription practice (before and after implementation of a specific oxygen prescription chart, from 55% to 91%; P=<0.001) with the accuracy of these written prescriptions improving significantly (7% vs 77%; statistical significance was not reported) following the implementation of a dedicated chart on which oxygen therapy could be prescribed. The authors argued that junior doctors have inadequate levels of understanding about the effects and potential dangers of oxygen therapy; however, the improvements seen following the implementation of a dedicated oxygen prescription chart appear to indicate that junior doctors complete required documentation appropriately when it is available and the presence of a chart merely prompted this action. Importantly, this was a single-center study and no data in this study examined the adherence of other clinicians (nurses and other medical staff) to accurately deliver the actual prescription. However, the results from the study by Gunathilake et alCitation36 suggest that appropriate oxygen delivery improved as prescription rates improved. They demonstrated that the number of patients at risk of type II respiratory failure with saturation levels above 92% decreased from 47% at initial audit to 18% (P=0.04) following a multicomponent intervention and as prescribing rates increased (2.4% to 34%; P=,0.0001).Citation36 Despite these encouraging results that demonstrate improvements in practice are possible, the sustainability of this behavior has been questioned by Young and Kostalas.Citation48 They saw asignificant improvement in prescription rates (from 12% to 74%; P=<0.001) 3 months following the introduction of an oxygen prescription section on the drug chart and the delivery of an educational session, but at 12 months this had decreased to 51%.
Also of interest is a study by Medford et alCitation38 who implemented a nurse facilitated reminder system and found that there were relatively high rates of appropriate oxygen administration prior to the implementation of the reminder system, and that these did not change significantly on reaudit 4 months after implementation (70.6% and 76.5%, respectively; P=0.65). Here, nurses were empowered to remind doctors to prescribe oxygen therapy. This may indicate that in general, nurses are skilled at delivering the appropriate dose of oxygen despite the absence of a prescription as is indicated by the lack of practice change by the nurses and maintenance of a relatively high rate of appropriate administration of oxygen therapy both before and after the intervention.
Knowledge of oxygen therapy and delivery equipment
Knowledge of oxygen therapy and the equipment used to deliver oxygen may also be barriers to optimal oxygen administration. This has been highlighted in a study conducted by Ganeshan et alCitation62 who reported that commonly used oxygen delivery devices, for example, nasal cannulae, are easily recognized by doctors and nurses with less frequently used devices, such as nonrebreathing masks, being poorly recognized. In addition, when both medical and nursing clinicians were presented with sample case scenarios, a larger proportion (up 97% and 73% of doctors and nurses, respectively) were not able to accurately prescribe the correct dose of oxygen or the appropriate method for administration of oxygen for some of the scenarios described. Interestingly, this studyCitation62 demonstrated that in four out of the seven case scenarios, nurses’ knowledge of the correct delivery devices and oxygen prescription was higher than that of the doctors. Overall, however, knowledge of correct prescriptions was suboptimal.
The authors argue that even if it were compulsory for medical staff to complete written prescriptions of oxygen therapy in wards settings, it is unlikely that staff would be able to prescribe it correctly. These findings are of particular concern in light of the current guideline recommendations.Citation17,Citation20 Disturbingly, these are not stand alone results and are supported by findings from other studiesCitation63–Citation65 that show there are large gaps in the knowledge of health care staff on various aspects of respiratory therapy. Considering the frequency with which oxygen is administered in an acute hospital setting and the harm that may be caused, interventions to improve the overall knowledge and practice around oxygen therapy and therefore concordance to evidence-based guidelines are urgently required.
Auditing practice
The BTS has conducted audits of prescribing practices within the National Health Service (NHS) since the implementation of the 2008 guidelines. These audits have demonstrated slow but steady improvements in the rates of oxygen prescription. The most recently available data from the 2013 auditCitation66 demonstrated that 55% of patients who were using oxygen had some form of written order. This is an improvement from the 2008 audit which showed that only 32% of patients had a written order.Citation66 These data also demonstrate a steady decline (17.5% down to 13.8%) in the number of patients within the NHS who are using oxygen therapy,Citation66 which could result in improved patient outcomes and substantial savings for the health service. In contrast, an Australian audit demonstrated that as few as 3% of patients with COPD had an existing oxygen prescription despite 79% of patients with COPD receiving oxygen therapy at the time of audit.Citation27 This improved level of practice in the UK, where regular audits are performed, may indicate that regular auditing and review of clinical practice and practice gaps can lead to improved clinician behavior.
Current recommendations and future directions
The NHS in their latest oxygen safety reportCitation67 suggests that the main safety concerns for oxygen administration relate to the under- and overuse of oxygen, and that these are caused by the inappropriate prescription, monitoring, and administration of oxygen. Like the BTS, the NHS emphasizes the need for the accurate prescription and monitoring of patients with pulse oximetry. Similarly, the 2015 Thoracic Society of Australia and New Zealand guidelines for acute oxygen use in adults also recommend that oxygen therapy is prescribed with a specific record documented in the patient notes and drug chart, the main requirements being the documentation of a target SpO2 range.
It is clear that there is a need to improve the prescribing practices for all patients across hospital settings. Although the authors have postulated on the reasons behind why evidence-based guidelines are not adhered to, very little data exist examining why high flow oxygen continues to be given in practice (particularly in the prehospital and emergency department setting) or why the written prescription ofoxygen therapy remains low. Medford et alCitation38 and HickeyCitation44 suggest that analysis of doctors’ views on the prescription of oxygen therapy is needed and that strategies for optimizing the behavior of permanent nursing staff are necessary;Citation38 however, to date, few data have been published relating to these points. As such, little is known about the barriers or facilitators that exist to improve the implementation of these strategies in practice, yet, published literature from the past 30 years demonstrates that despite a number of interventional strategies aimed at improving practice, it continues to be a challenging practice to change.
The knowledge practice gap is a common phenomenon in health careCitation68 with some authorsCitation69 suggesting that the provision of guidelines and evidence from research, while necessary, are not sufficient in bridging the knowledge practice gap. Specifically, this has been demonstrated with the oxygen prescription data. A convincing evidence base now exists, yet the consistent application of the evidence (prescription and delivery of low flow oxygen to maintain SpO2 88%–92% in vulnerable patient groups) is not applied in daily practice. Funk et alCitation70 argue that determining the perceptions of clinicians is vital in addressing this knowledge–practice gap. Ultimately, clinicians are responsible for the delivery of care. If we are to reduce or eliminate barriers to implementing research knowledge into practice, clinicians’ opinions are vital. Tailored interventions while effective can be variable; however, a 2015 Cochrane Review concluded that “interventions tailored to address identified barriers are probably more likely to improve professional practice than no intervention or the dissemination of guidelines alone.”Citation71
Conclusion
Throughout this review, we have presented international data surrounding current practice for the prescription of oxygen therapy. These data demonstrate that the rates of concordance to recommended practice have seen a necessary change in oxygen prescription; however, there remains substantial room for improvement. This is evidenced in the large audit conducted by Roberts et alCitation26 in 2010–2011 in which 16,018 patients admitted with acute exacerbations of COPD to hospitals in 13 European countries demonstrated a high level of adherence (85%) to the Global Initiative for Obstructive Lung DiseaseCitation72 standards for the management of acute exacerbations of COPD, administering titrated oxygen therapy, to achieve PaO2 >60 mmHg or SpO2 >90%.Citation72 Despite this high level of adherence, >1,623 (10.1%) of the patients across the hospitals received either high flow oxygen or no supplemental oxygen (despite being hypoxic). Many practice gaps exist, which lead to poor patient outcomes. Pilcher and BeasleyCitation32 suggest that there is an entrenched culture of routine and indiscriminate administration of high-concentration oxygen to acutely ill patients. This culture must change and there is a clear need to examine the barriers, facilitators, and attitudes toward oxygen and its prescription in acute care if we are to improve practice and minimize harm in vulnerable patient groups. Effective interventions may assist in translating expert guidelines into clinical practice. These may facilitate the adoption of best practice guidelines and ultimately improve clinical outcomes for COPD and other vulnerable patient groups who are most impacted by poor oxygen administration practices.
Acknowledgments
VM McDonald is supported by a National Health and Medical Research Council Translating Research into Practice Fellowship.
Disclosure
The authors report no conflicts of interest in this work.
References
- MartinDSGrocottMPIIIOxygen therapy in anaesthesia: the yin and yang of O2Br J Anaesth2013111686787124233308
- Steinman KaufmanJKentBNursing management: obstructive pulmonary diseasesBrownPEdwardsHSeatonLLewis’s Medical-Surgical Nursing Assessment and Management of Clinical Problems Australia and New Zealand Edition4th edSydneyMosby Elsevier2015564614
- KaneBDecalmerSO’DriscollBREmergency oxygen therapy: from guideline to implementationBreathe201394246253
- BlakemanTCEvidence for oxygen use in the hospitalized patient: is more really the enemy of good?Respir Care201358101679169324064627
- MartinDSGrocottMPWOxygen therapy and anaesthesia: too much of a good thing?Anaesthesia201570551852225866038
- JoostenSAKohMSBuXSmallwoodDIrvingLBThe effects of oxygen therapy in patients presenting to an emergency department with exacerbation of chronic obstructive pulmonary diseaseMed J Aust2007186523523817391084
- AustinMAWillisKEBlizzardLWaltersEHWood-BakerREffect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trialBMJ2010341c5462
- WijesingheMPerrinKHealyBPre-hospital oxygen therapy in acute exacerbations of chronic obstructive pulmonary diseaseIntern Med J201141861862220214690
- NewAOxygen: kill or cure? Prehospital hyperoxia in the COPD patientEmerg Med J200623214414616439751
- McDonaldCFOxygen therapy for COPDJ Thorac Dis20146111632163925478203
- BrillSEWedzichaJAOxygen therapy in acute exacerbations of chronic obstructive pulmonary diseaseInt J Chron Obstruct Pulmon Dis201491241125225404854
- BossonNGausche-HillMKoenigWImplementation of a titrated oxygen protocol in the out-of-hospital settingPrehosp Disaster Med201429440340824983332
- AbdoWFHeunksLMAOxygen-induced hypercapnia in COPD: myths and factsCritical Care2012163234
- RocaMVerduriACorbettaLCliniEFabbriLMBeghéBMechanisms of acute exacerbation of respiratory symptoms in chronic obstructive pulmonary diseaseEur J Clin Invest201343551052123489139
- AbramsonMJCrockettAJDabscheckEThe COPDX Plan: Australian and New Zealand Guidelines for the management of Chronic Obstructive Pulmonary Disease20141111
- LittletonSWHypercapnia from hyperoxia in COPD: Another piece of the puzzle or another puzzle entirely?Respir Care201560347347525737575
- O’DriscollBRHowardLSDavisonAGBritish Thoracic SocietyBTS guideline for emergency oxygen use in adult patientsThorax200863Suppl 6vi1vi6818838559
- AubierMMurcianoDMilic-EmiliJEffects of the administration of O2 on ventilation and blood gases in patients with chronic obstructive pulmonary disease during acute respiratory failureAm Rev Respir Dis198012257477546778278
- Global Initiative for Chronic Obstructive Lung Disease (GOLD)Global Strategy for the Diagnosis, management, and Prevention of Chronic Obstructive Pulmonary Disease [updated 2016]2016i111 Available from: http://www.goldcopd.org/uploads/users/files/WatermarkedGobal%20Strategy%202016%281%29.pdfAccessed February 19, 2016
- BeasleyRChienJDouglasJThoracic Society of Australia and New Zealand oxygen guidelines for acute oxygen use in adults: ‘Swimming between the flags’Respirology20152081182119126486092
- O’DriscollBRHowardLEarisJMakVBTS Emergency Oxygen Guideline GroupBTS Guidelines for oxygen use in adults in healthcare and emergency settings [Public consultation draft]2015 Available from: https://www.brit-thoracic.org.uk/document-library/clinical-information/oxygen/emergency-oxygen-guideline-2015/bts-full-guideline-for-oxygen-use-in-adults-in-healthcare-and-emergency-settings-2015/
- ChowJWKhullarKKatechiaKKlimSKellyAMDo ambulance paramedics administer too much oxygen to patients with acute exacerbations of chronic obstructive airways disease? [Letter to the editor]Emerg Med Australas201527327527625891097
- SusantoCThomasPSAssessing the use of initial oxygen therapy in chronic obstructive pulmonary disease patients: a retrospective audit of pre-hospital and hospital emergency managementIntern Med J201545551051625682723
- GooptuBWardLAnsariSOErautCDLawDDavisonAGOxygen alert cards and controlled oxygen: preventing emergency admissions at risk of hypercapnic acidosis receiving high inspired oxygen concentrations in ambulances and A&E departmentsEmerg Med J200623863663816858099
- PilcherJCameronLBraithwaiteIComparative audit of oxygen use in the prehospital setting in acute COPD exacerbation over 5 yearsEmerg Med J201532323423824243487
- RobertsCMLopez-CamposJLPozo-RodriguezFHartlSEuropean COPD Audit teamEuropean hospital adherence to GOLD recommendations for chronic obstructive pulmonary disease (COPD) exacerbation admissionsThorax201368121169117123729193
- PrettoJJMcDonaldVMWarkPAHensleyMJMulticentre audit of inpatient management of acute exacerbations of chronic obstructive pulmonary disease: comparison with clinical guidelinesIntern Med J201242438038721395962
- CameronLPilcherJWeatherallMBeasleyRPerrinKThe risk of serious adverse outcomes associated with hypoxaemia and hyperoxaemia in acute exacerbations of COPDPostgrad Med J201288104668468922977283
- Al-ShaqsiSBrockwayBABC of oxygen therapy in acute care: Why? Who? How?N Z Med Student J20131758
- SladeSEvidence summary: oxygen therapy: hospital settingThe Joanna Briggs Institute2014
- LamontTLuettelDScarpelloJO’DriscollBRConnewSImproving the safety of oxygen therapy in hospitals: summary of a safety report from the National Patient Safety AgencyBMJ2010340313314
- PilcherJBeasleyRAcute use of oxygen therapyAust Prescr20153839810026648631
- CookDJReeveBKGriffithLEMookadamFGibsonJCMultidisciplinary education for oxygen prescription: A continuous quality improvement studyArch Intern Med199615616179718018790073
- WijesingheMShirtcliffePPerrinKAn audit of the effect of oxygen prescription charts on clinical practicePostgrad Med J2010861012899320145057
- DoddMEKelletFDavisAAudit of oxygen prescribing before and after the introduction of a prescription chartBMJ200032186486511021863
- GunathilakeRLoweDWillsJKnightABraudePImplementation of a multicomponent intervention to optimise patient safety through improved oxygen prescription in a rural hospitalAust J Rural Health201422632833325495628
- HolbournAWongJOxygen prescribing practice at Waikato Hospital does not meet guideline recommendationsIntern Med J20144412a1231123425316385
- MedfordABowenJHarveyJImproved oxygen prescribing using a nurse-facilitated reminderBr J Nurs2009181273073419543159
- WaltersGNadeemSImproving acute oxygen prescription in a respiratory care unitQual Saf Health Care200918651219955469
- NevesJTLobãoMJGrupo de trabalho EMOOxygen therapy multicentric study – a nationwide audit to oxygen therapy procedures in internal medicine wardsRev Port Pneumol2012182808522280829
- PeasePOxygen administration: is practice based on evidence?Paediatr Nurs2006188141817042302
- AkbarFACampbellIAOxygen therapy in hospitalized patients: the impact of local guidelinesJ Eval Clin Pract2006121313616422778
- BoyleMWongJPrescribing oxygen therapy. An audit of oxygen prescribing practices on medical wards at North Shore Hospital, Auckland, New ZealandN Z Med J20061191238U208016868577
- HickeySAn audit of oxygen therapy on a respiratory wardBr J Nurs200716181132113618073684
- NasirAAO’DriscollBRP45 Audit of oxygen management on nine medical wards using electronic prescribing systemsPoster presented at: British Thoracic Society Winter Meeting 2012December 5–7, 2012Westminster, London, UK
- NeillAMEptonMJMartinIRDrennanCJTownGIAn audit of the assessment and management of patients admitted to Christchurch Hospital with chronic obstructive pulmonary diseaseNZ Med J1994107986 Pt 1365367
- SmallDDuhaAWieskopfBUses and misuses of oxygen in hospitalized patientsAm J Med1992925915951605139
- YoungAFKostalasMThe acute prescription of oxygen in orthopaedic trauma patientsBr J Hosp Med20137410586589
- AlbinRJCrinerGJThomasSAbou-JaoudeSPattern of non-ICU inpatient supplemental oxygen utilization in a University HospitalChest19921026167216751446470
- HowellMAn audit of oxygen prescribing in acute general medical wardsProf Nurse200117422122412030174
- BellCIs this what the doctor ordered? Accuracy of oxygen therapy prescribed in hospitalProf Nurse1995105279300
- AsciakRFenechVAGattJMontefortSOxygen prescription and administration at the emergency department and medical wards in Mater Dei HospitalMalta Med J20112321923
- JeffreyAARaySDouglasNJAccuracy of inpatient oxygen administrationThorax198944103610372617443
- FitzgeraldJMBaynhamRPowlesACUse of oxygen therapy for adult patients outside of the critical care areas of a university hospitalLancet1988185929819832896838
- SniderGLRinaldoJEOxygen therapy in medical patients hospitalized outside of the intensive care unitAm Rev Respir Dis198012229366779679
- KorACLimTKAudit of oxygen therapy in acute general medical wards following an educational programmeAnn Acad Med Singapore20002917718110895335
- BrokalakiHMatziouVZygaSOmissions and errors during oxygen therapy of hospitalized patients in a large city of GreeceIntensive Crit Care Nurs200420635235715567676
- GravilJHO’NeillVJStevensonRDAudit of oxygen therapyInt J Clin Pract19975142172189287261
- KhachiHBurmanMWaltersLSinha-RayRAntoniouSMandalSP84 the impact of a multidisciplinary educational programme on the prescribing of oxygen in an acute trustThorax201065Suppl 4A112A113
- NicklessGFallonRImproving local compliance with standards for oxygen prescribingClin Pharm20113299 Available from: http://www.pharmaceutical-journal.com/news-and-analysis/news/improving-local-compliance-with-standards-for-oxygen-prescribing/11085599.article
- RudgeJOdedraSHarrisonDA new oxygen prescription produces real improvements in therapeutic oxygen useBMJ Qual Improv Reports20143110.1136/bmjquality.u204031.w1815
- GaneshanAHonLQSoonawallaZFOxygen: Can we prescribe it correctly?Eur J Intern Med200617535535916864012
- SmithGBPoplettNKnowledge of aspects of acute care in trainee doctorsPostgrad Med J20027892033533812151686
- EspositoSBrivioATagliabueCKnowledge of oxygen administration, aerosol medicine, and chest physiotherapy among pediatric healthcare workers in ItalyJ Aerosol Med Pulm Drug Deliv201124314915621361785
- EastwoodGMReadeMCPeckLBaldwinIConsidineJBellomoRCritical care nurses’ opinion and self-reported practice of oxygen therapy: a surveyAust Crit Care2012251233021715182
- O’DriscollBRBritish Thoracic Society Emergency Oxygen Audit 2013 (National Audit Period 15 August–1 November 2013)2014 Available from: https://www.brit-thoracic.org.uk/document-library/audit-and-quality-improvement/audit-reports/bts-emergency-oxygen-audit-report-2013/
- National Health ServiceRapid Response Report NPSA/2009/RRR006: Oxygen safety in hospitals2009 Available from: http://www.nrls.npsa.nhs.uk/resources/?entryid45=62811
- GrolRWensingWWhat drives change? Barriers to and incentives for achieving evidence-based practiceMed J Aust2004180S57S6015012583
- StrausSETetroeJGrahamIDKnowledge translation: what it is and what it isn’tStrausSETetroeJGrahamIDKnowledge Translation in Health Care. Moving from Evidence to Practice2nd edChichesterWiley2013313
- FunkSGChampagneMTWieseRATornquistEMBARRIERS: The barriers to research utilization scaleAppl Nurs Res19914139451741634
- BakerRCamosso-StefinovicJGilliesCTailored interventions to address determinants of practice. Cochrane Database of Systematic ReviewsCochrane Database Syst Rev20154i118 Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD005470.pub3/abstract ;jsessionid=1F4B90BD5BCD52658D574021CA65C97B.f03t03
- Global Initiative for Chronic Obstructive Lung Disease (GOLD)Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease [updated 2010]2010i117 Available from: http://www.goldcopd.org/uploads/users/files/GOLDReport_April112011.pdfAccessed 19th February 2016
