Abstract
Tobacco contains cadmium, and this metal has been attributed a causative role in pulmonary emphysema among smokers, although extracellular cadmium has not to date been quantified in the bronchoalveolar space of tobacco smokers with or without COPD. We determined whether cadmium is enhanced in the bronchoalveolar space of long-term tobacco smokers with or without COPD in vivo, its association with inflammation, and its effect on chemokine release in macrophage-like cells in vitro. Bronchoalveolar lavage (BAL), sputum, and blood samples were collected from current, long-term smokers with and without COPD and from healthy nonsmokers. Cadmium concentrations were determined in cell-free BAL fluid using inductively coupled plasma mass spectrometry. Blood monocyte-derived macrophages were exposed to cadmium chloride in vitro. Depending upon the type of sample, molecular markers of inflammation were quantified either as protein (enzyme-linked immunosorbent assay) or as mRNA (real-time polymerase chain reaction). Cadmium concentrations were markedly increased in cell-free BAL fluid of smokers compared to that of nonsmokers (n=19–29; P<0.001), irrespective of COPD. In these smokers, the measured cadmium displayed positive correlations with macrophage TNF-α mRNA in BAL, neutrophil and CD8+ cell concentrations in blood, and finally with IL-6, IL-8, and MMP-9 protein in sputum (n=10–20; P<0.05). The cadmium chloride exposure caused a concentration-dependent increase in extracellular IL-8 protein in monocyte-derived macrophages in vitro. In conclusion, extracellular cadmium is enhanced in the bronchoalveolar space of long-term smokers and displays pro-inflammatory features. Its pathogenic role in tobacco-induced disease deserves further evaluation.
Introduction
The metal cadmium is present in tobacco and therefore also in cigarettes.Citation1–Citation3 However, it is known that the content of cadmium in tobacco varies markedly depending on both brand and country of origin, even though the average cadmium content in cigarettes is always substantial (0.5–1.6 µg/g).Citation4,Citation5 Importantly, cadmium exposure is toxic to several mammalian organs and has been associated with pulmonary emphysema in tobacco smokers,Citation6 in whom elevated cadmium concentrations have been detected in body fat, blood, urine, and amniotic fluid, thereby indicating systemic absorption, presumably via the lungs.Citation7 Tentatively, cadmium is a metal that bears the potential to constitute a pathogenic factor in tobacco smokers.
There is to date limited information published on cadmium concentrations in the lungs of human tobacco smokers. Some studies on lung tissue from lung cancer patients have showed the presence of cadmium,Citation8,Citation9 and in one study, extracellular cadmium concentrations were measured in bronchoalveolar lavage (BAL) samples from patients with interstitial lung diseases.Citation10 Notably, this particular study suggested that extracellular cadmium can be detected in the bronchoalveolar space of humans. Finally, cadmium concentrations in exhaled breath condensate from smokers with or without COPD have been shown to be higher than in nonsmokers, a finding which is compatible with, although not a conclusive evidence of, increased cadmium in the bronchoalveolar space of smokers.Citation11
In terms of mechanistic actions of cadmium in animal lung models, there is limited published information as well. Inhalation of cadmium chloride (CdCl2) in dogs induced a transient neutrophil accumulation and an increased bronchial responsiveness to histamine which was reversible.Citation12 In a rat model, repeated local administration of CdCl2 induced an accumulation of both macrophages and neutrophils, as well as signs of emphysema.Citation13 Thus, cadmium is a candidate for being a pathogenic factor involved in excess mobilization of innate effector cells, tissue destruction and functional alterations, as judged from these animal models.
Until date, there is no published information on local extracellular concentrations of cadmium in the bronchoalveolar space of human tobacco smokers with and without COPD, nor in relation to markers of inflammation. Given this and what is known about the pathogenic potential and impact on innate effector cells, referred earlier, we hypothesized that extracellular cadmium concentrations are enhanced in the bronchoalveolar space of tobacco smokers and that these enhanced cadmium concentrations are associated with markers of inflammation relating to innate effector cells. The main aim of the current study was to evaluate this hypothesis and to investigate how cadmium concentrations relate to COPD. To do this, we examined BAL, blood, and sputum samples from current, long-term cigarette smokers with and without mild-to-severe COPD, and from healthy nonsmokers. We also assessed the potential of cadmium to be directly involved in the mobilization of innate effector cells by examining its effect on chemokine release in human macrophage-like cells in vitro.
Materials and methods
Study design
Ethics
The study protocol was ethically reviewed and approved by the Regional Ethics Committee in Stockholm, Sweden (Diary No 2005/733-31/1-4), and the study was conducted in accordance with the Declaration of Helsinki.
Recruitment
The study subjects were recruited through advertisement in the daily press and via the outpatient clinic at the Lung Allergy Clinic, Karolinska University Hospital. All participating subjects were recruited after oral and written informed consent, and their personal information was anonymized. This was also the case for the donors of blood leukocytes.
Study subjects
Our cohort included current smokers (n=57) as well as healthy nonsmokers (n=23).Citation14 Subjects had no asthma, allergy, or other pulmonary diseases, and denied heart diseases or other clinically significant diseases. Among the current smokers, those with a post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) <0.7 and an FEV1 39%–98% of predicted value constituted the COPD group (n=28) and smokers with a post-bronchodilator FEV1/FVC >0.7 and an FEV1 >70% of predicted value constituted the non-COPD group (n=29). Smoking was not allowed the last hour preceding the investigations.
For the measurement of extracellular cadmium concentrations in the bronchoalveolar space, we harvested and investigated BAL samples from 12 long-term smokers with COPD, 17 long-term smokers without COPD, and 19 healthy nonsmokers (clinical characteristics in ). For the evaluation of correlations between extracellular cadmium concentrations and different cellular and molecular markers of innate effector cells, the number of available samples varied, and the actual n is stated for each analysis.
Table 1 Characteristics of the groups of the study cohort
The study subjects underwent clinical examination, spirometry and bronchoscopy with the collection of BAL fluid, as previously described.Citation14–Citation16 Likewise, samples of induced sputum and blood were collected, as previously described.Citation16
Handling of BAL and sputum samples
The BAL samples were subjected to Cytospin® centrifugation, and cell differential counts were determined () from slides stained with May-Grünwald Giemsa. Cell-free BAL fluid samples were collected after centrifugation and frozen (−80°C) for subsequent analyses.Citation16 For each induced sputum sample, an equal volume of dithiothreitol (0.1%) was added to the whole-sputum sample, whereafter the sample was rocked in a water bath (15–20 minutes, at 37°C), and then filtered and centrifuged. Cell-free sputum was then collected from the supernatant and stored (−80°C) for subsequent analyses. Some of the basal results in this study have been included in previous publications;Citation14–Citation16 however, they were used in different constellations and interpreted in unique contexts.
Cadmium in cell-free BAL samples
The cadmium concentrations in cell-free BAL samples were determined utilizing an inductively coupled plasma mass spectrometry instrument (Thermo X series II; Thermo Fisher Scientific, Waltham, MA, USA) equipped with a collision/reaction cell system. This analysis of extracellular cadmium was performed according to the standard of SS-EN ISO 17294-2 (Water quality – Application of inductively coupled plasma mass spectrometry [ICP-MS] – Part 2: Determination of 62 elements) at Stockholm University, Sweden (ISO-certified laboratory).
The isotope 114Cd was utilized for the detection of cadmium concentrations in our cell-free BAL fluid samples. We chose this isotope instead of 111Cd because in samples with low cadmium concentrations, 114Cd has higher abundance compared to that of the 111Cd. Any possible interference of the 114Sn was avoided by the measurement of this particular isotope and adjusting for its presence using the instrument software.
Rhodium (103Rh) was used for recovery calculations. The limit of detection (LOD) was set to 0.01 µg/L for cadmium using 3× standard deviation (SD) in blank samples. The relative SD was consistently <20% in the samples.
In addition to the cadmium analysis described earlier, we attempted to assess background exposure to automotive particulate pollution with nanoparticles by analyzing our BAL samples for palladium.Citation17
In vitro experiments on macrophage-like cells
Cell isolation
Peripheral blood mononuclear cells (PBMCs) were isolated from the buffy coat (Karolinska University Hospital) of five healthy human donors (n=5) utilizing standard density gradient centrifugation on Ficoll-Paque™ PLUS (GE Healthcare Life Science, Little Chalfont, Buckinghamshire, UK) in accordance with the manufacturer’s instructions. Each donor yielded ~1×109 PBMCs, and we seeded these PBMCs (15 million cells/well) into six-well tissue culture plates (BD Biosciences, San Jose, CA, USA), thereby obtaining 5.76±2.4 million cells/well (mean ± SD) after exposure. To establish macrophage-like cells (ie, monocyte-derived macrophages), we first cultured PBMCs with Iscove’s modified Dulbecco’s medium (IMDM; Thermo Fisher Scientific) supplemented with 4-(2-hydroxyethyl)- 1-piperazineethanesulfonic acid (HEPES; 10 mM; Thermo Fisher Scientific) and penicillin–streptomycin antibiotics (PEST; Lonza Group, Basel, Switzerland). They were incubated (5% CO2, 2 hours at 37°C), and then the nonadhered cells were washed away using phosphate-buffered saline. The adhered cells were cultured during 7 days with supplemented IMDM (10% of heat-inactivated pooled human serum from Fisher Scientific GTF AB [Lund, Sweden] plus 10 mM of HEPES and PEST). The media were replaced every third day.
The obtained macrophage-like cells had a high purity (88%, n=5), as determined by flow cytometry (BD LSRFortessa™) targeting archetype surface antigens (CD14+, CD68+). The cell viability, as assessed using exclusion of trypan blue dye both prior to and after the in vitro experiments, was very high (99%, n=5).
Cadmium exposure
For the time-course experiments, the isolated macrophage-like cells were exposed to CdCl2 (50 µM; Sigma-Aldrich Co., St Louis, MO, USA) or control solution (vehicle) during 6, 24, and 48 hours. For the concentration–response experiments, the cells were exposed to 0, 2.5, 12.5, 25, 37.5, and 50 µM of CdCl2 during 24 hours only. All exposure experiments were performed in duplicate. After these in vitro experiments, the conditioned media were collected and frozen (−80°C) for subsequent cytokine measurements.
Molecular markers of inflammation
Protein
We quantified protein concentrations of interleukin (IL)-8/CXCL8 and IL-6 in cell-free conditioned medium, supernatant from saliva, sputum, and BAL fluid samples utilizing in-house enzyme-linked immunosorbent assay (ELISA) methods, as previously described.Citation18 Briefly, commercially available antibody pairs MAB208/MAB 206 and MAF208/MAF 206 (R&D Systems, Inc., Minneapolis, MN, USA) were used to detect IL-8 (detection range: 12.5–6,400 pg/mL) and IL-6 (detection range: 3–375 pg/mL). An intra-assay variation <10% was accepted for the duplicate samples. We also quantified protein concentrations of MMP-9 in cell-free supernatant in conditioned medium, saliva, sputum, BAL fluid, and serum samples utilizing a commercial ELISA kit (DouSet ELISA MMP-9 Kit; R&D Systems, Inc.). The analyses of MMP-9 were performed according to the manufacturer’s instructions, and an intra-assay variation <10% was accepted for the duplicate samples.
mRNA
The cells collected from the BAL fluid were resuspended in Rosewell Park Memorial Institute cell medium supplemented with 5% serum and then put into Petri dishes (2 million cells/dish). After incubation (2 hours), the nonadherent cells and supernatants were discarded, and the adhered cells (macrophages) were prepared for mRNA analysis. Total mRNA was isolated by PureLink™ Micro-to-Midi Total RNA Purification System (Thermo Fisher Scientific). DNase I amplification grade was used to remove the genomic DNA (Thermo Fisher Scientific). First-strand cDNA was synthesized (from 0.5 µg of total mRNA), using QuantiTect® Reverse Transcription Kit (Qiagen NV, Venlo, the Nether-lands). The ABI Power SYBR Green Master mix (Thermo Fisher Scientific) was used to perform the real-time polymerase chain reaction (PCR). All primers were purchased from Thermo Fisher Scientific. The widely used cDNA of glyceraldehyde-3-phosphate dehydrogenase was adopted as a house-keeping gene. One microliter of cDNA was used in each PCR volume (25 µL) to identify the products of interest. Data were analyzed using 7500 Software v.2.0.1, and the results were then calculated and expressed as 2−ΔCt.
Statistical analyses
Nonparametric statistics were applied. Results are thus presented as median with range, unless otherwise stated. Between-group comparisons were performed using the Kruskal–Wallis test followed by Mann–Whitney U-test as post hoc test when appropriate. The comparisons between different CdCl2 exposure concentrations were assessed by Friedman test and followed by Wilcoxon signed rank test as a post hoc test. Correlations were determined using Spearman rank correlation. We utilized the STATISTICA software program version 12 (StatSoft Scandinavia AB, Uppsala, Sweden), and a P-value of <0.05 was considered statistically significant. n refers to the number of independent observations.
Results
In vivo samples
Clinical characteristics
The subjects in the COPD group were somewhat older than subjects in the other two groups, but the other parameters were well matched (). The spirometry volumes FVC and FEV1 were lower in smokers with COPD compared with healthy nonsmokers, and FEV1 was lower in smokers with COPD than in those without COPD, as a consequence of the inclusion criteria.
Cadmium concentrations in cell-free BAL samples
Smokers with or without COPD had markedly higher concentrations of cadmium in cell-free BAL fluid samples than did healthy, nonsmoking controls (). However, there was no statistically significant difference between smokers with and without COPD, the two groups of long-term smokers. Cadmium concentrations below the LOD were, however, only found in healthy nonsmokers and in smokers with COPD, not in those without COPD. Palladium concentrations, which were measured in order to assess vehicle particulate pollution background, were below the LOD for all samples, thereby indicating that the background exposure from traffic was modest for all groups.
Figure 1 Concentrations (µg/L) of cadmium (Cd) in cell-free BAL fluid samples from smokers with (n=12) or without (n=17) COPD compared with healthy nonsmokers (n=19).
Abbreviation: BAL, bronchoalveolar lavage.
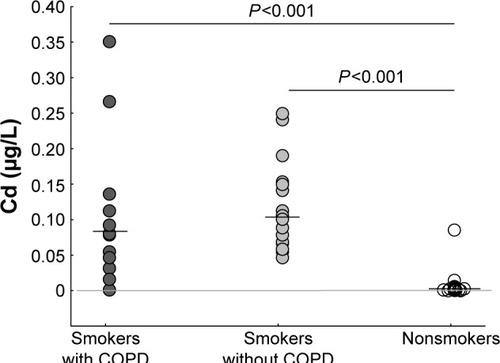
A trend toward a sex difference in cadmium concentration in cell-free BAL fluid samples was observed when pooling subjects from all study groups (females: 0.085 µg/L [0.01–0.12] and males: 0.028 µg/L [0.006–0.09]), but this trend did not prove statistically significant (P=0.09). A corresponding trend was observed when conducting the sex comparison analysis in the study groups of smokers with or without COPD separately (data not shown).
We observed no correlation between cadmium concentration in cell-free BAL fluid samples and age, smoking (pack-years and current smoking), or lung volumes (data not shown).
Cadmium and inflammatory cells
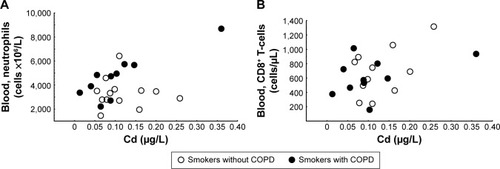
There were positive correlations between cadmium concentrations in cell-free BAL fluid samples and concentrations of neutrophils and CD8+ T-lymphocytes in blood ().
Figure 2 Relationship between cadmium (Cd) in the airways and inflammatory cells in blood.
Abbreviation: BAL, bronchoalveolar lavage.
Cadmium and molecular markers of inflammation
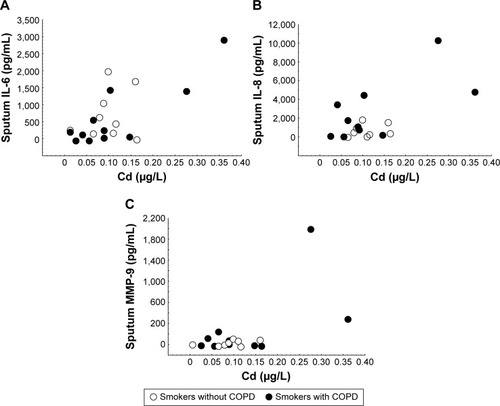
There were positive correlations between the concentrations of cadmium in cell-free BAL samples and mRNA for tumor necrosis factor (TNF)-α in BAL macrophages (). This was also true for protein concentrations of IL-6, IL-8, and MMP-9 in cell-free sputum samples (). In general, these correlation coefficients tended to become higher when calculating correlations only in smokers with COPD (correlation coefficients and P-values are given in the figure legends).
Figure 3 Relationship between cadmium (Cd) and messenger RNA for TNF-α in the airways.
Notes: Concentrations of Cd in cell-free BAL fluid and macrophage TNF-α at mRNA levels in BAL cells (all smokers: R=0.60, P=0.03, n=10; smokers with COPD only: R=0.97, P=0.002, n=6). All correlations analyzed with Spearman rank correlation test.
Abbreviations: BAL, bronchoalveolar lavage; MQ, macrophage; TNF-α, tumor necrosis factor alpha.
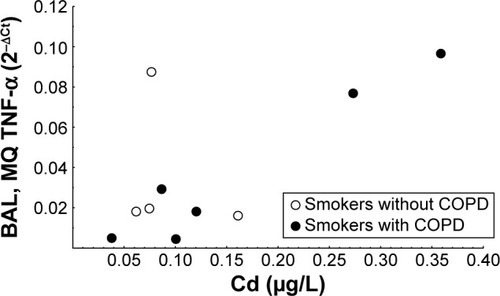
Figure 4 Relationship between cadmium (Cd) and molecular markers of inflammation in the airways.
Abbreviations: BAL, bronchoalveolar lavage; IL, interleukin.
In vitro samples
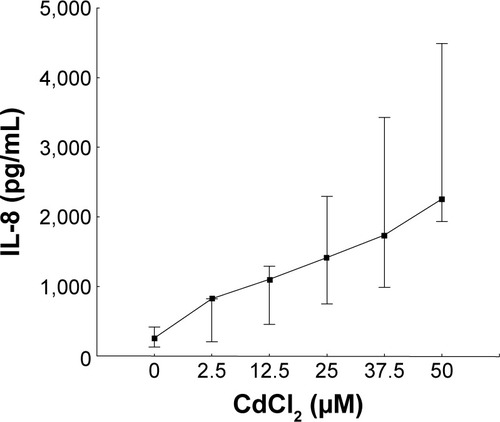
Exposure to CdCl2 caused a concentration-dependent increase of IL-8 protein concentrations in cell-free conditioned media from the macrophage-like cells cultured in vitro (). Of note, MMP-9 protein concentrations were detectable in the same conditioned media, but there was no statistically significant effect of CdCl2 on these concentrations.
Figure 5 Effect of cadmium (Cd) on the archetype chemokine IL-8 in macrophage-like cells in vitro.
Abbreviations: CdCl2, cadmium chloride; IL, interleukin.
Discussion
In this study, we demonstrate measurable cadmium concentrations in cell-free BAL fluid samples from smokers with or without COPD and show that these concentrations, in both groups, are markedly higher than those in healthy nonsmokers. We also show a positive correlation between enhanced cadmium concentrations in the cell-free BAL fluid samples from smokers regardless of COPD and several cellular or molecular markers of inflammation in the same human subjects. Finally, we demonstrate that CdCl2 stimulates the release of the archetype chemokine IL-8 in human macrophage-like cells in vitro. Taken together, our findings illustrate the pathogenic potential of extracellular cadmium in the bronchoalveolar space of tobacco smokers in terms of disease involving innate effector cells.
To the best of our knowledge, our study is the first one to characterize cadmium concentrations in the extracellular compartment of the bronchoalveolar space in smokers with and without verified COPD, compared with healthy nonsmokers. However, compatible findings have previously been obtained in one single study on exhaled breath condensate.Citation11 In that study, Mutti et al obtained evidence of higher concentrations of cadmium and other metals in the lungs of smokers with and without COPD, compared with healthy nonsmokers.Citation11 Moreover, these cadmium concentrations in exhaled breath condensate correlated with the smoking history in a positive manner, suggesting that tobacco smoke really is the origin of cadmium in the lungs. In this respect, our cohort did not have sufficient statistical power to provide supportive information.
In our study, the history of tobacco smoking (ie, tobacco load) was very similar for smokers with and without COPD, an important aspect of the careful matching of smoking subjects in our study cohort. This “similarity” makes the fact that we detected no substantial difference in local cadmium concentration for smokers with and without COPD more conclusive. However, this lack of difference in extracellular cadmium concentration questions the role of cadmium in terms of being a direct cause of the chronic airway obstruction that separated our two groups of long-term smokers. We think that this lack of difference argues in favor of cadmium bearing pathogenic potential for the development of other aspects of disease in the airways of tobacco smokers.
Specifically, the finding of positive correlations with cellular markers of inflammation related to blood neutrophils and cytotoxic T-cells known to be involved in disease related to tobacco-smoking is indeed compatible with an involvement of cadmium in the disease process.Citation11 Of note, the correlation between cadmium in BAL samples and neutrophils in blood was relatively strong, in particular for samples from smokers with COPD. Along these lines, the demonstrated correlations with molecular markers of inflammation included the archetype chemokine IL-8 as well as IL-6 and MMP-9 in sputum samples. In further support of a mechanistic link between cadmium and neutrophils, the exposure of macrophage-like cells to CdCl2 caused a clear-cut and concentration-dependent release of the archetype chemokine IL-8. Moreover, the strong correlation between extracellular cadmium concentrations in BAL samples and mRNA for TNF-α in macrophages from BAL samples adds further evidence of macrophages being targeted by cadmium from tobacco smoke. Collectively, these findings are all compatible with extracellular cadmium in the airways constituting a pathogenic factor involved in the mobilization of innate effector cells perpetuating other aspects of disease than that directly related to chronic airway obstruction.
It is difficult to judge to what extent the assessment of metals such as cadmium in a certain compartment is representative of the same metal in a different compartment. Mannino et al previously demonstrated that increased concentrations of cadmium in urine are significant predictors of impaired lung function in current and former smokers from a US normal population, but this was not the case in never-smokers from the same population.Citation19 Basically, the same findings were obtained in a study of a South Korean population, and based upon these studies, it is not possible to conclusively judge how systemic and local cadmium concentrations in the peripheral airways (using BAL samples) relate to one another.Citation20 Given that we lacked whole-blood and urine samples for the assessment of systemic cadmium concentrations in our current study cohort, this particular aspect remains of interest for future studies.
With reference to the trend toward higher cadmium concentrations in cell-free BAL fluid from female subjects in our current cohort, it is true that we were unable to prove this potential sex difference statistically significant. However, from a qualitative point of view, our results are compatible with previous publications suggesting that females have higher concentrations of cadmium in blood, urine, and kidney and that cadmium-related effects on health may be overrepresented among female subjects.Citation21,Citation22 Given that the previously postulated sex difference of cadmium in blood becomes less evident after menopause, our current results appear reasonable since smokers with COPD tend to be of higher age, as was the case of the females in our study cohort.
Interestingly, Grasseschi et al previously forwarded evidence that alveolar macrophages constitute a prominent cadmium-containing cell type in the airways.Citation23 In their study, it was revealed that smokers have a threefold increase in intracellular cadmium content in alveolar macrophages, compared with nonsmokers. However, in their study, the presence of COPD among smokers was not taken into account. Moreover, these investigators found that the cadmium content in alveolar macrophages correlated better with recent smoking history than with lifelong cumulative smoking history. Thus, either intracellular cadmium content in alveolar macrophages changes over shorter time periods or the limited life span of the macrophages sets a natural limit to the information obtained with that study approach. To us, the latter seems most feasible, given that cadmium has a very long biological half-life, ~14–24 years in urineCitation24 and 7–16 years in blood.Citation25
Finally, we think that it is important to note that the postulated involvement of alveolar macrophages and neutrophils in the local response to extracellular cadmium in the bronchoalveolar space of smokers is supported by two previous publications based on animal models in vivo.Citation12,Citation13 In essence, these previous publications illustrate cadmium-induced effects on the accumulation of innate effector cells and emphysema (in the rat model only), as well as effects on proteinase activity from MMP-2 and MMP-9, the latter likely to originate from innate effector cells.Citation12,Citation13
Conclusion
Our study on extracellular cadmium in the bronchoalveolar space of humans suggests that cadmium is markedly enhanced in the lungs of long-term smokers regardless of COPD. Moreover, our findings of several correlations with cellular and molecular markers of inflammation and, in one case, a direct effect on a key molecular marker of inflammation forward the mobilization of innate effector cells as an important action of cadmium in the airways. Clearly, this possibility deserves to be addressed in new and better-powered studies on tobacco smokers, where local cadmium concentrations can be related both to systemic cadmium and to additional parameters of specific pathology in the lungs, including the status of local host defense and the most common comorbidities among tobacco smokers.
Acknowledgments
We thank Karin Holm at Stockholm University for technical assistance with the analysis of metals in cell-free BAL fluid. We also thank Professor Carola Lidén and Doctor Hanna Karlsson, Institute of Environmental Medicine, Karolinska Institutet, for their invaluable support throughout this study. The authors gratefully acknowledge the expert technical advice from Doctor Karlhans Fru Che regarding the experiments on macrophage-like cells in vitro. Project funding was obtained from the Swedish Research Council (LP and AL), the Swedish Heart-Lung Foundation (KL, LP, and AL), the Foundation for Rehabilitation and Medical Research in Gothenburg (FRF-stiftelsen; AL), Stockholm County Council (ALF-medel; AL), King Gustav V’s and Queen Victoria’s Freemason Research Fund (AL), and federal funding from Karolinska Institutet (LP and AL). No funding was obtained from the tobacco industry.
Disclosure
The authors report no conflicts of interest in this work.
References
- O’ConnorRJLiQStephensWECigarettes sold in China: design, emissions and metalsTob Control201019Suppl 2i47i5320935196
- AjabHYaqubAMailkSAJunaidMYasmeenSAbdullaMACharacterization of toxic metals in tobacco, tobacco smoke, and cigarette ash from selected imported and local brands in PakistanScientific World Journal2014201441361424672317
- UwakweAAIbiamUALevels of cadmium in different brands of cigarettes sold in Abakaliki metropolis of NigeriaAfr J Biochem Res20093317320
- OberdorsterGAirborne cadmium and carcinogenesis of the respiratory tractScand J Work Environ Health1986125235373547632
- BernhardDRossmannAWickGMetals in cigarette smokeLife20055780580916393783
- HirstRNJrPerryHMJrCruzMGPierceJAElevated cadmium concentration in emphysematous lungsAm Rev Respir Dis197310830394715968
- PappasRSToxic elements in tobacco and in cigarette smoke: inflammation and sensitizationMetallomics201131181119821799956
- KollmeierHSeemannJWittigPRotheGMüllerKMCadmium in human lung tissueInt Arch Occup Environ Heath199062373377
- ZhangLLvJSunSElements in lung tissues of patients from a high lung cancer incidence area of ChinaBiol Trace Elem Res201214871022274755
- BargagliEMonaciFBianchiNBucciCRottoliPAnalysis of trace elements in bronchoalveolar lavage of patients with diffuse lung diseasesBiol Trace Elem Res200812422523518665336
- MuttiACorradiMGoldoniMVettoriMVBernardAApostoliPExhaled metallic elements and serum pneumoproteins in asymptomatic smokers and patients with COPD or asthmaChest20061291288129716685021
- BologninMKirschvinkNLeemansJCharacterisation of the acute and reversible airway inflammation induced by cadmium chloride inhalation in healthy dogs and evaluation of the effects of salbutamol and prednisoloneVet J200917944345018037312
- KirschvinkNVinckeGFiévezLRepeated cadmium nebulizations induce pulmonary MMP-2 and MMP-9 production and emphysema in ratsToxicology2005211364815863246
- von ScheeleILarssonKDahlénBToll-like receptor expression in smokers with and without COPDRespir Med20111051222123021439805
- BergstromJCederlundKDahlenBDental health in smokers with and without COPDPLoS One20138e5949223544074
- JiJvon SchéeleIBergströmJCompartment differences of inflammatory activity in chronic obstructive pulmonary diseaseRespir Res20141510425155252
- WilkinsonKEPalmbergLWitaspESolution-engineered palladium nanoparticles: model for health effect studies of automotive particulate pollutionACS Nano201155312532421650217
- LarssonKTornlingGGavhedDMüller-SuurCPalmbergLInhalation of cold air increases the number of inflammatory cells in the lungs in healthy subjectsEur Respir J1998128258309817153
- ManninoDMHolguinFGrevesHMSavage-BrownAStockALJonesRLUrinary cadmium levels predict lower lung function in current and former smokers: data from the Third National Health and Nutrition Examination SurveyThorax20045919419814985551
- LeemAYKimSKChangJRelationship between blood levels of heavy metals and lung function based on the Korean National Health and Nutrition Examination Survey IV-VInt J Chron Obstruct Pulmon Dis2015101559157026345298
- VahterMBerglundMAkessonALidenCMetals and women’s healthEnviron Res20028814515512051792
- VahterMAkessonALidénCCeccatelliSBerglundMGender differences in the disposition and toxicity of metalsEnviron Res2007104859516996054
- GrasseschiRMRamaswamyRBLevineDJKlaassenCDWesseliusLJCadmium accumulation and detoxification by alveolar macrophages of cigarette smokersChest20031241924192814605069
- SuwazonoYKidoTNakagawaHBiological half-life of cadmium in the urine of inhabitants after cessation of cadmium exposureBiomarkers200914778119330585
- JärupLRogenfeltAElinderCGNogawaKKjellstromTBiological half-time of cadmium in the blood of workers after cessation of exposureScand J Work Environ Health198393273316635611
