Abstract
Background
Physical activity (PA) is impaired from the early stages of COPD, is associated with a worsening of disease prognosis, and causes COPD patients to restrict their daily activities in order to avoid breathlessness. The development of a simple tool to estimate physical activity level (PAL) could be useful for the management of COPD.
Objectives
We investigated the differences in PA according to the modified Medical Research Council (mMRC) grade in patients with COPD.
Methods
A cross-sectional study was performed on stable outpatients with COPD. PA was measured for 2 weeks using a triaxial accelerometer, and dyspnea grade was evaluated in all patients using the mMRC scale.
Results
Ninety-eight patients were recruited. Significant differences in PA duration were observed at all intensities according to the mMRC grade. Despite treatment with controller medications, 59.2% of COPD patients had low PAL, which was <1.5 metabolic equivalents multiplied by hour per day. COPD patients with an mMRC grade ≥2, which was the most balanced cutoff point in the receiver operating characteristic curve, showed a higher reduction rate of PAL (80.0% at mMRC grade 2, 71.4% at mMRC grade 3, and 100% at mMRC grade 4).
Conclusion
PA differed according to the mMRC grade, and mMRC grade ≥2 could predict a low PAL. Therefore, assessment of breathlessness by the mMRC questionnaire would be useful to stratify the risks of reduced PA in COPD.
Keywords:
Introduction
COPD is characterized by persistent airflow limitation that is associated with an enhanced chronic inflammatory response to noxious particles or gases in the airways and lungs.Citation1 It was reported that COPD was the third leading cause of death in 2012 by the World Health Organization.Citation2 Patients with COPD often have limited daily physical activity (PA). The level of PA was reported to be associated with decline of lung function and increase in hospitalizations.Citation3,Citation4 Moreover, the decline of daily PA was shown to be the strongest predictor of mortality in patients with COPD.Citation5 Recently, an accelerometer was used for evaluating PA in COPD because of its accuracy. We have validated triaxial accelerometersCitation6,Citation7 and have evaluated the features of PACitation8 and the efficacy of medication for PA in COPD.Citation9 However, equipment and several days for evaluation are required.
The modified Medical Research Council (mMRC) Questionnaire is widely used for assessing the severity of breathlessness in patients with COPD. This questionnaire was reported to be consistent with other measures of health status and to predict the decline of lung function and future mortality risk.Citation10–Citation12 Although the severity of breathlessness is assumed to be associated with PA, the differences in PA in patients with COPD according to the mMRC grade have not yet been clearly established. We hypothesized that the mMRC grade could detect low PA in patients with COPD.
The aim of this study was to investigate the differences in PA measured by a triaxial accelerometer according to the mMRC grade and also to investigate the mMRC grade that can detect low PA in patients with COPD.
Methods
Subjects
Stable COPD patients (aged ≥60 years) following treatment in accordance with the guidelines and without any other diseases that might interfere with walking were recruited from among the outpatients of Wakayama Medical University Hospital. COPD was diagnosed if the following condition existed: a postbronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity of <0.7. The patients were excluded if they had any other pulmonary diseases, such as asthma and bronchiectasis, or experienced exacerbations during the 4 weeks prior to the study.
Protocol
Patients’ age, sex, height, weight, smoking status, treatments, mMRC grade, spirometry, and PA were examined in a cross-sectional manner. Each patient wore a triaxial accelerometer, Actimarker (Panasonic, Osaka, Japan), for 2 weeks in order to measure their PAs. Written informed consent was obtained from all patients, and the study was approved by the local ethics committee (Institutional Review Board committee of Wakayama Medical University; authorization number: 968) and was registered with University Hospital Medical Information Network (UMIN) center (UMIN 000006293).
Assessment of PA
The Actimarker is a small (74.5 ×13.4 ×34.0 mm) and light-weight (36.0 g) accelerometer that is worn only at the waist and can be continuously monitored for over 1 month. The Actimarker has already been validated for evaluating PA in COPD in terms of intensity.Citation7 From the 2 weeks of monitored data, 3 consecutive nonrainy weekdays from the beginning, except the first and last days, were extracted, and the mean values of PA duration from the extracted 3 days were employed as representative values of PA for the individual according to a previous investigation.Citation7
In addition, we calculated the PA level (PAL) that was the value of metabolic equivalents multiplied by their durations (METs⋅hour). The American College of Sports Medicine and the American Heart Association recommended that older adults need moderate-intensity (between 3 METs and 6 METs) aerobic PA for a minimum of 0.5 hours for 5 days of each week.Citation13 Therefore, we regarded the patients with PAL <1.5 METs⋅hour as those with low PA.
Assessment of mMRC grade
The mMRC grade is a five-point scale based on the severity of a patient’s breathlessness related to PA. Current guidelines advocate the use of this scale to assess symptoms.Citation1 In this study, the mMRC grades were assessed by the study physicians.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 5 (GraphPad Software, Inc., La Jolla, CA, USA). Kruskal–Wallis test and post hoc Dunn’s multiple comparison test were used for comparison of PA durations and PAL among the patients of each mMRC grade. Chi-square test was used for comparison of the proportion of patients with low PAL among the mMRC grades. Using a receiver operating characteristic (ROC) curve, we determined the cutoff points for identifying the patients with low PAL. A P-value of <0.05 was considered significant.
Results
Ninety-eight patients with COPD were included in this study, and the characteristics of the included patients are shown in . Ninety-two patients (93.9%) were males, and the numbers of patients with Global Initiative for Chronic Obstructive Lung Disease (GOLD) stages I, II, III, and IV were 14 (14.3%), 50 (51%), 22 (22.4%), and 12 (12.2%), respectively.
Table 1 Characteristics of patients
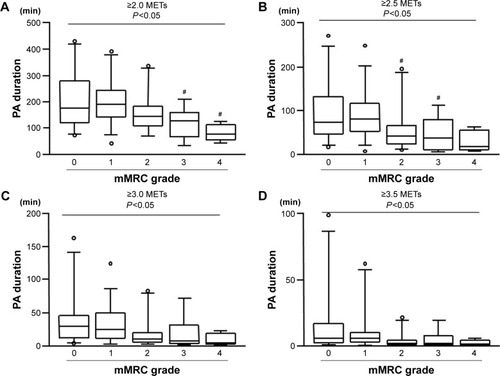
Significant differences in the PA duration according to the mMRC grade were confirmed at all intensities (≥2 METs: P=0.01, ≥2.5 METs: P=0.01, ≥3 METs: P=0.01, ≥3.5 METs: P=0.05 by Kruskal–Wallis test) (). With the post hoc analysis, the reduction of the PA duration was significant for the patients with mMRC grades 3 and 4 at ≥2.0 METs () and with mMRC grades 2 and 3 at ≥2.5 METs (), as compared to those with mMRC grade 1.
Figure 1 Differences in PA duration according to the mMRC grade.
Abbreviations: PA, physical activity; mMRC, modified Medical Research Council; METs, metabolic equivalents; min, minutes.
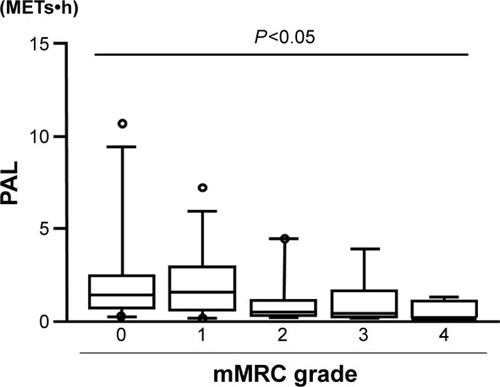
The PAL, which was calculated by METs⋅hour at ≥3 METs, was also significantly different according to the mMRC grade (P<0.005; ). However, there were no significant differences among the mMRC grades by the multiple comparison test.
Figure 2 Differences in PAL at ≥3 METs according to the mMRC grade.
Abbreviations: PAL, physical activity level; mMRC, modified Medical Research Council; PA, physical activity; METs, metabolic equivalents; h, hour.
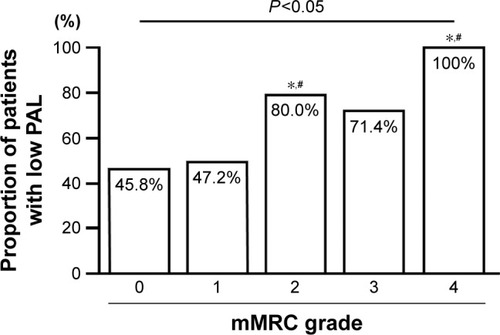
More than half of COPD patients (59.2%) had a low PAL <1.5 METs⋅hour. Even among the patients with mMRC grade 0, the proportion of those with low PAL was 45.8%. The proportion of the patients with low PAL was significantly increased as the mMRC grade increased and significantly higher in patients with mMRC grades 2 and 4 than those with mMRC grades 0 and 1 ().
Figure 3 mMRC grade and the proportion of patients with low PAL.
Abbreviations: mMRC, modified Medical Research Council; PAL, physical activity level.
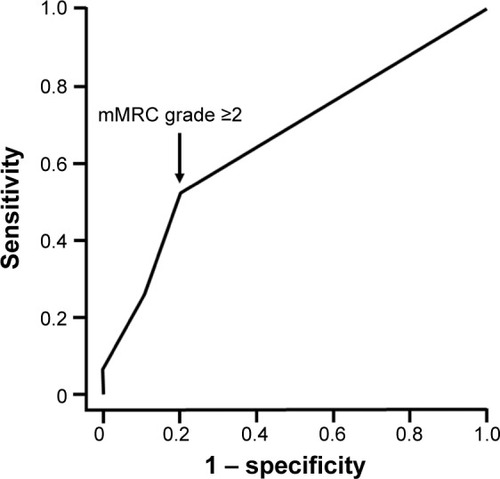
Using an ROC curve for identifying the patients with low PAL, mMRC grade ≥2 was the most balanced cutoff point and yielded 51.7% sensitivity and 80.0% specificity (area under curve =0.66) ().
Figure 4 ROC curve for identifying patients with low PAL.
Abbreviations: mMRC, modified Medical Research Council; PAL, physical activity level; ROC, receiver operating characteristic.
Discussion
We could demonstrate differences in PA duration or PAL measured by triaxial accelerometer according to the mMRC grade in patients with COPD. Among the COPD patients, 59.2% had low PAL, and even among the patients with mMRC grade 0, low PAL was observed in 45.8% of them. An mMRC grade ≥2 was the most balanced cutoff point for identifying patients with low PAL.
PA durations among the mMRC grades were significantly different at all intensities. Pitta et alCitation14 reported that patients with COPD had shorter periods of walking time per day than healthy elderly individuals (44 minutes and 81 minutes, respectively). Sakamoto et alCitation15 reported these values as 47.5 minutes in COPD and 106.5 minutes in healthy subjects. In our study, the mean PA duration at ≥3 METs, which is the intensity of a normal walking speed for a healthy adult, was about 40 minutes in COPD patients with mMRC grades 0 and 1, which is similar to previous reports. We previously reported that the reduction rate of PA in COPD patients was 50.9% at ≥3 METs.Citation8
This study showed that the PAL was significantly different according to the mMRC grade, and the proportion of the patients with low PAL was significantly increased as the mMRC grade increased. Watz et alCitation16 reported that the proportion of very inactive patients markedly increased in patients with an mMRC grade ≥2 compared with chronic bronchitis, which seems to be consistent with our results. However, this was not statistically evaluated, and the differences in PA according to the mMRC grade in patients with COPD were not clearly demonstrated.Citation16 In this study, using an ROC curve for identifying the patients with low PAL, an mMRC grade ≥2 was the most balanced cutoff point that yielded 51.7% sensitivity and 80.0% specificity. This result means that an mMRC grade ≥2 strongly suggests a marked reduction of PA. The reason for the low sensitivity may be that not only breathlessness but also sociodemographic, lifestyle, and environmental factors, as well as other clinical and functional variables, affect the PA in patients with COPD.Citation17 In GOLD,Citation1 mMRC grade ≥2 was used as a cutoff point for stratifying the impact of COPD on an individual patient, which is compatible with our results.
GOLD has recommended adjusting the therapeutics by evaluating the degree of symptoms, breathlessness, airflow obstruction, and frequency of COPD exacerbations.Citation1 In this study, the value of FEV1% predicted was correlated with the mMRC grade (r=−0.559, P<0.0001) and PAL (r=0.329, P<0.001 with linear regression analysis). We previously reported an association between the severity of airflow obstruction and breathlessness assessed by the mMRC questionnaire.Citation18 Moreover, this study showed that the mMRC questionnaire was a useful tool for estimating the level of daily PA. These results suggest that an objective evaluation of the breathlessness assessed by the mMRC questionnaire in daily practice could play an important role in improving COPD management.
However, in COPD patients, the efficacy of the pharmacological or the nonpharmacological treatments on dyspnea has been reported,Citation19–Citation22 but their efficacy in PA is still controversial.Citation23–Citation33 This discrepancy might occur because the effect of treatment on PA was modified by not only dyspnea but also other factors, including several clinical and functional variables. However, the dyspnea grade could be one of the important predictors of PA in COPD patients.
This study had several limitations. First, the number of recruited patients was small. A larger study will be required to determine the usefulness of the mMRC grade for estimating PA. Second, this study is based on a single center. Finally, potential comorbidities, including depression, osteoporosis, and muscular weakness, were not completely excluded, though the patients with diseases that might interfere with walking were excluded.
Conclusion
The PA in patients with COPD was different according to the mMRC grade. PAL was reduced compared to the American College of Sports Medicine/American Heart Association recommendation in about one half of the patients with mMRC grades 0 and 1. However, the reduction rate of PAL was much higher in those with an mMRC grade ≥2. The mMRC grade reflected the increases in the proportion of patients with low PAL. Moreover, mMRC grade ≥2 was the most balanced cutoff point for stratifying the risks of reduced PAs in COPD. The mMRC questionnaire could be a useful tool for estimating the level of PA in daily life.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
The authors thank Mr Brent Bell for reading the manuscript. This study was supported by JSPS KAKENHI grant numbers 24591136 and 15KO9187.
Disclosure
The authors report no conflicts of interest in this work.
References
- Global initiative for Chronic Obstructive Lung Disease [homepage on the Internet]Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Disease2016 Available from: http://www.goldcopd.comAccessed June 20, 2016
- World Health Organization [homepage on the Internet] Available from: http://www.who.int/en/Accessed June 20, 2016
- Garcia-AymerichJLangePBenetMSchnohrPAntóJMRegular physical activity modifies smoking-related lung function decline and reduces risk of chronic obstructive pulmonary disease: a population-based cohort studyAm J Respir Crit Care Med2007175545846317158282
- PittaFTroostersTProbstVSSpruitMADecramerMGosselinkRPhysical activity and hospitalization for exacerbation of COPDChest2006129353654416537849
- WaschkiBKirsteinAHolzOPhysical activity is the strongest predictor of all-course mortality in patients with COPD: a prospective cohort studyChest2011140233134221273294
- KandaMMinakataYMatsunagaKValidation of the triaxial accelerometer for the evaluation of physical activity in Japanese patients with COPDIntern Med201251436937522333371
- SuginoAMinakataYKandaMValidation of a compact motion sensor for the measurement of physical activity in patients with chronic obstructive pulmonary diseaseRespiration201283430030721912085
- MinakataYSuginoAKandaMReduced level of physical activity in Japanese patients with chronic obstructive pulmonary diseaseRespir Investig20145214148
- MinakataYMorishitaYIchikawaTEffects of pharmacologic treatment based on airflow limitation and breathlessness on daily physical activity in patients with chronic obstructive pulmonary diseaseInt J Chron Obstruct Pulmon Dis2015101275128226170656
- BestallJCPaulEAGarrodRGarnhamRJonesPWWedzichaJAUsefulness of the medical research council (MRC) dyspneoa scale as a measure of disability in patients with chronic obstructive pulmonary diseaseThorax199954758158610377201
- OgaTTsukinoMHajiroTIkedaANishimuraKAnalysis of longitudinal changes in dyspnea of patients with chronic obstructive pulmonary disease: an observational studyRespir Res2012138523006638
- NishimuraKIzumiTTsukinoMOgaTDyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPDChest200212151434144012006425
- HaskellWLLeeIMPateRRPhysical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart AssociationMed Sci Sports Exerc20073981423143417762377
- PittaFTroostersTSpruitMAProbstVSDecramerMGosselinkRCharacteristics of physical activities in daily life in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2005171997297715665324
- SakamotoYSakamotoKMinakataYWalking pattern in COPD patientsRehabil Nurs Epub3142015
- WatzHWaschkiBMeyerTMagnussenHPhysical activity in patients with COPDEur Respir J200933226227219010994
- Gimeno-SantosEFreiASteurer-SteyCPROactive consortium. Determinants and outcomes of physical activity in patients with COPD: a systematic reviewThorax201469873173924558112
- MatsunagaKHayataAAkamatsuKStratifying the risk of COPD exacerbation using the modified Medical Research Council scale: a multicenter cross-sectional CAP studyRespir Investig20155328285
- CasaburiRMahlarDAJonesPWA long-term evaluation of once-daily inhaled tiotropium in chronic obstructive pulmonary diseaseEur Respir J200219221722411866001
- BogdanMAAizawaHFukuchiYMishimaMNishimuraMIchinoseMEfficacy and safety of inhaled formoterol 4.5 and 9 μg twice daily in Japanese and European COPD patients: phase III study resultsBMC Pulm Med2011115122085439
- BuhlRDunnLJDisdierCINTENSITY Study InvestigatorsBlinded 12-week comparison of once-daily indacaterol and tiotropium in COPDEur Respir J201138479780321622587
- Pulmoanry rehabilitation: joint ACCP/AACVPR evidence-based guidelinesACCP/AACVPR Pulmonary Rehabilitation Guidelines Panel. American College of Chest Physicians. American Association of Cardiovascular and Pulmonary RehabilitationChest19971125136313969367481
- HatajiONaitoMItoKWatanabeFGabazzaECTaguchiOIndacaterol improves daily physical activity in patients with chronic obstructive pulmonary diseaseInt J Chron Obstruct Pulmon Dis201381523293514
- WatzHKrippnerFKirstenAMagnussenHVogelmeierCIndacaterol improves lung hyperinflation and physical activity in patients with moderate chronic obstructive pulmonary disease – a randomized, multicenter, double-blind, placebo-controlled studyBMC Pulm Med20141415825280934
- BeehKMWatzHPuente-MaestuLAclidinium improves exercise endurance, dyspnea, lung hyperinflation, and physical activity in patients with COPD: a randomized, placebo-controlled, crossover trialBMC Pulm Med20141420925539654
- MinakataYMorishitaYHiramatsuMEffect of transdermal tulobuterol patch on the physical activity in eight male subjects with chronic obstructive pulmonary diseaseClin Res Pulmonol201421010
- O’DonnellDECasaburiRVinckenWINABLE 1 study group. Effect of indacaterol on exercise endurance and hyperinflation in COPDRespir Med201110571030103621498063
- TroostersTSciurbaFCDecramerMTiotropium in patients with moderate COPD naïve to maintenance therapy: a randomized placebo-controlled trialNPJ Prim Care Respir Med2014241400324841833
- SewellLSinghSJWilliamsJECollierRMorganMDCan individualized rehabilitation improve functional independence in elderly patients with COPD?Chest200512831194120016162706
- MerckenEMHagemanGJScholsAMAkkermansMABastAWoutersEFRehabilitation decreases exercise-induced oxidative stress in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med20051728994100116040783
- PittaFTroostersTProbstVSLangerDDecramerMGosselinkRAre patients with COPD more active after pulmonary rehabilitation?Chest2008134227328018403667
- MadorMJPatelANNadlerJEffect of pulmonary rehabilitation on activity levels in patients with chronic obstructive pulmonary diseaseJ Cardiopulm Rehabil Prev2011311525920724933
- EganCDeeringBMBlakeCShort term and long term effects of pulmonary rehabilitation on physical activity in COPDRespir Med2012106121671167923063203
