Abstract
Purpose
With the limited reach of pulmonary rehabilitation (PR) and low levels of daily physical activity in chronic obstructive pulmonary disease (COPD), a need exists to increase daily exercise. This study evaluated telephone health-mentoring targeting home-based walking (tele-rehab) compared to usual waiting time (usual care) followed by group PR.
Patients and methods
People with COPD were randomized to tele-rehab (intervention) or usual care (controls). Tele-rehab delivered by trained nurse health-mentors supported participants’ home-based walking over 8–12 weeks. PR, delivered to both groups simultaneously, included 8 weeks of once-weekly education and self-management skills, with separate supervised exercise. Data were collected at three time-points: baseline (TP1), before (TP2), and after (TP3) PR. The primary outcome was change in physical capacity measured by 6-minute walk distance (6MWD) with two tests performed at each time-point. Secondary outcomes included changes in self-reported home-based walking, health-related quality of life, and health behaviors.
Results
Of 65 recruits, 25 withdrew before completing PR. Forty attended a median of 6 (4) education sessions. Seventeen attended supervised exercise (5±2 sessions). Between TP1 and TP2, there was a statistically significant increase in the median 6MWD of 12 (39.1) m in controls, but no change in the tele-rehab group. There were no significant changes in 6MWD between other time-points or groups, or significant change in any secondary outcomes. Participants attending supervised exercise showed a nonsignificant improvement in 6MWD, 12.3 (71) m, while others showed no change, 0 (33) m. The mean 6MWD was significantly greater, but not clinically meaningful, for the second test compared to the first at all time-points.
Conclusion
Telephone-mentoring for home-based walking demonstrated no benefit to exercise capacity. Two 6-minute walking tests at each time-point may not be necessary. Supervised exercise seems essential in PR. The challenge of incorporating exercise into daily life in COPD is substantial.
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive respiratory condition with systemic effect,Citation1 exacting a substantial burden of increasing breathlessness and physical restrictions on individuals.Citation2 This is of concern, as more physically active people with COPD have a lower risk of hospitalization and all-cause mortalityCitation3 and these individuals experience better physiologic function.Citation4
Pulmonary rehabilitation (PR) is an intervention shown to help people with COPD improve their physical and psychosocial health, and is advocated as an integral component of COPD management.Citation5,Citation6 Supervised exercise is regarded as a key component of PR. Those who participate in conventional PR can expect an improvement in their physical capacity, health-related quality of life, breathlessness, and fatigue.Citation7 However, the effect on daily physical activity levels in the community has only recently been investigated and appears to be minimal.Citation8
The Australian Government defines “physical activity” as skeletal bodily movement resulting in ongoing health benefits, and “exercise” as a subset of physical activity, purposefully planned to maintain or improve physical health.Citation9 “Physical capacity” refers to a person’s overall ability to function and “undertake the physically demanding activities of daily living”.Citation10 These distinctions are important. One major outcome of PR is an improvement in physical capacity. While this may correlate with daily physical activity,Citation11 formal physical capacity measures alone cannot reveal whether an individual is meeting recommended physical activity guidelines for health. Indeed, the literature indicates that people with COPD are predominantly sedentary,Citation12 with exercise guidelines not being met.Citation11
Despite the benefits of PR, its reach is limited. Internationally ~1% of people with COPD have access to PR.Citation13 Australian data reflect this, with 200 programs available nationwide, predominantly based in health care facilities and accessed by only 1% of those who might benefit.Citation14 Others have sought to increase the reach of interventions for people with COPD with promising technologies, such as brief telephone support,Citation15 mobile telephone programs,Citation16 or the computer-based Nintendo Wii Fit.Citation17 Similarly, weekly reported diary-recorded home-walking has increased physical capacity compared to usual care.Citation18
Strategies that foster self-management for sustained behavior change via telephone health-mentoring have been investigated.Citation19,Citation20 Self-management is
a process that facilitates an individual’s confidence and capability to engage in health-promoting behaviors in order to deal with the impact of their condition on all aspects of their health-namely, a sense of self, physical, emotional, social and medical domains so as to maximize function and quality of life.Citation21
Working with people to develop self-management skills is recognized as integral to PRCitation6 and could even be an alternative to formal supervised exercise sessions.
Telephone health-mentoring trials to improve self-management in COPD using community nurses improved health-related quality of lifeCitation20 and self-management capacity.Citation19 However, the effect on physical capacity or physical activity was not examined, which is important given the increasing focus on physical activity in COPD.Citation22,Citation23
One self-management approach that has reported improvements in self-reported physical activity is the group-based Stanford Chronic Disease Self-Management Program (CDSMP).Citation24 We recently investigated the addition of an hour of supervised exercise to the CDSMP for people with COPD in a randomized controlled clinical trial, finding a small statistically significant increase in physical capacity.Citation21 However, the increase of 20 m was less than half that reported in a review of traditional PRCitation7 and less than the accepted minimal clinical important difference reported by others.Citation25,Citation26 We found no difference between the intervention and control groups for self-reported physical activity.
To better meet clinical demand for PR, augmenting the gains we observed in the CDSMPCitation21 and with telephone-based self-management support in COPDCitation19,Citation20 hold promise. In this study, we investigated the effects of telephone-based health-mentoring (tele-rehab) targeting home-based walking on physical capacity and self-reported physical activity.
Materials and methods
Study design
This parallel-group randomized clinical trial in COPD aimed to evaluate the effectiveness of tele-rehab followed by PR versus usual care, that is, a waiting period followed by the same PR. The primary outcome was physical capacity measured by the 6-minute walk distance (6MWD).Citation27
The minimally important clinical difference (MICD) for the 6MWD at the time of our study was 35 m (95% confidence interval 30–42 m).Citation28 In a recent study, we found the standard deviation of the change in distance walked was 46.2 m21 and the attrition rate in our rehabilitation program was 33%. Using these data, we calculated that the study would need to recruit 37 participants in each arm (power =0.8, significance =0.05) to demonstrate potential superiority of the intervention.
Participants were assigned a unique identification number and randomized to the tele-rehab (intervention) or to usual care (control) group using computer-generated random numbers by a research assistant not associated with the study, ensuring neutral allocation after baseline data collection. The trial was registered with the Australian and New Zealand Clinical Trials Registry (ACTRN12611001034921).
Study subjects
Following a hospital admission or clinic visit, adults with COPD, who were referred for PR at the Royal Hobart Hospital, a tertiary, university-affiliated public hospital, were screened and recruited. Referring staff were aware that this study was taking place.
Individuals were included in the study if they were over 18 years of age, had spirometry-diagnosed COPD, and were at least 2 months post an exacerbation prior to data collection. They were excluded if they experienced cognitive impairment, were unable to provide informed consent, could not complete questionnaires independently, did not meet safety to exercise criteria,Citation29 or had attended some form of PR in the previous 2 years. For those people not wishing to participate in the project or who did not meet the inclusion criteria, follow-up management, including referral to a physiotherapist or PR, was offered in the course of usual care.
Detail of interventions
Screening of initial referrals confirming general study suitability (age, diagnosis, comorbidities) was followed by a telephone invitation to attend an appointment. Following informed consent, inclusion criteria were confirmed, and baseline data collected (time-point 1, TP1). The next data collection was at 8 to 12 weeks, after either tele-rehab or the usual waiting time (time-point 2, TP2), and the final data collection was after 8 weeks of PR (time-point 3, TP3).
Tele-rehab aimed to specifically support participants in undertaking exercise as well as address other mutually identified health behaviors from smoking, nutrition, alcohol consumption, physical activity, psychosocial well-being, and symptom management (“SNAPPS”).Citation30,Citation31 Following randomization, participants in the intervention group completed a summary of their SNAPPS health behaviors with the research officer and established a home-based walking plan, aiming to meet Australian guidelines at the time of the study: to walk at a moderate intensity (ie, to breathe more heavily but not to “huff and puff”) to accumulate 30 minutes daily on several and preferably all days of the week.Citation32 They received a copy of their written personal walking action plan, their personal SNAPPS summary, plus information concerning health behaviors (Supplementary material). Participants were contacted via telephone by specifically trained community nursesCitation19,Citation20,Citation33 who acted as nurse health-mentors over the next 8–12 weeks, to support the home-walking action plan and any other health behavior plans. A schedule of two calls weekly was suggested, with a minimum of four calls mutually agreed with each participant, based on findings in a previous study that indicated participants preferred a flexible schedule for health-mentoring contacts.Citation20
Participants in usual care waited for 8 to 12 weeks prior to their scheduled PR appointment without any additional contact, reflecting the Australian context of PR.Citation34 At the time of this study, the local Tasmanian waiting time was >3 months.
PR followed the format of our previous study, consisting of 1 hour, once-weekly of 8 weeks of structured group education with self-management skills development (the CDSMP) and 1 hour of gym-based weekly supervised exercise.Citation21 Supervised exercise was delivered in the same week but on a subsequent day to the education sessions. Individualized programs of aerobic exercise (aiming for at least 30 minutes of bicycle or treadmill exercise) with strengthening and stretching at a moderate to strong intensity determined and monitored by self-reported perception of exertion were developed. A discussion session targeting exercise and physical activity was offered with the education sessions. Participants reported back at the commencement of each session on their diary-recorded home-walking plans set the previous week.
Participants and community nurses gave written, informed consent. The Tasmanian Human Research Ethics Committee granted ethical approval (H0011764).
Outcome measures and data analyses
Outcome measurements were blinded. The primary outcome was change in physical capacity, measured by the 6MWD,Citation27 conducted according to standard Australian protocols. Two tests were performed at each time-point, with the longest distance of the two being recorded.Citation35 Secondary outcomes are described in . Data pertaining to self-reported physical activity are presented as: 1) data from the SNAPPS snapshot questionnaire, that is, a retrospective report of habitual moderate intensity walking (how many days per week and minutes per day performed on average over the previous 4 weeks) and 2) data from the walking diary-recorded in real time during PR. The first measure reflects the usual enquiry about physical activity in our clinical practice.
Table 1 Outcomes and measures
Analysis was by intention-to-treat, missing data handled by last case carried forward, and comparisons made using Mann–Whitney U-tests, Student’s t-tests, or chi-squared analyses. Correlations were investigated using Pearson’s correlation coefficient. Significance was set at a P-value of <0.05. Blinding with respect to participant allocation was maintained until data analyses were complete.
Results
Participants
Recruiting took place over 15 months from February 2012 (). Of the 362 individuals referred, most (73%) were inpatients referred by the respiratory nurse specialist or physiotherapists, with 23% referred directly by respiratory physicians, 4% by general practitioners and community nurses, and 3% by other hospital ward-based doctors. Of the 297 not included in the study, nearly two-thirds declined an appointment, citing health or travel issues as the main barrier to attendance (). Although we had planned to recruit 74 individuals, we made a decision to cease recruiting in order to complete the follow-up TP3 assessments as scheduled. Thus, 65 participants were randomized, 35 to the intervention and 30 to the control groups, respectively. No participant changed groups during follow-up.
Figure 1 Flowchart depicting flow of participants through the study.
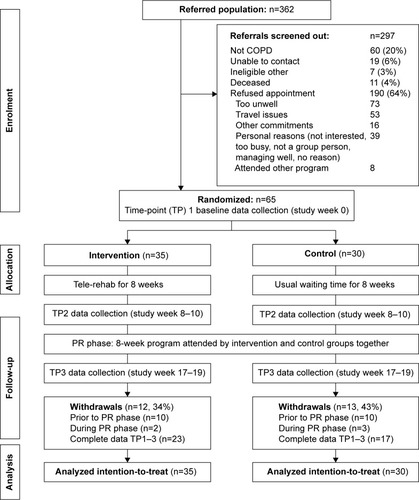
Of those 65 individuals randomized, 25 (38%) withdrew (12 interventions and 13 controls) during the study, with males (n=17, 68%) being more likely to withdraw than females (P=0.005). The majority withdrew prior to PR commencing (ten in intervention and ten controls). “Ill health” was named by nearly half as the reason for withdrawing, time constraints by a quarter, with the remainder citing travel issues, giving no reason, or just failure to keep appointments.
Eighteen trained nurses delivered the mentoring for tele-rehab. There were a total of 231 telephone contacts, with a mean of 7±3 calls per individual, each lasting a duration of 17±9 minutes per call and 7±6 days between calls. Contact with tele-rehab participants could not be made on 38 occasions and data were not recorded for 18 calls. Of 287 walking action plans set, 48% were completed, 27% not completed, and 25% not recorded. The principle reasons for not completing the walking program were being unwell or time constraints.
At the first PR session, only 31 (74%) of the 42 participants remaining by this stage expressed intention to attend the supervised exercise sessions, despite all having consented to do so at recruitment. However, only 16 (38%) actually commenced supervised exercise (ten in intervention and six controls), attending only a mean of 5±2 sessions of a possible eight. A preference to exercise at home was stated as the main reason for not commencing supervised exercise, followed by travel issues. Of those who commenced supervised exercise, a greater proportion was female (75%), did not have a partner (63%), had moderate or severe COPD (82%), and were in the intervention group (63%). A median of 6 (4) sessions were attended, with ill health cited as the predominant reason for nonattendance.
At baseline, there were no statistically significant differences between the intervention and control group subjects for demographic () or outcome () measures, or between those who withdrew and those who completed all data collections.
Table 2 Participant characteristics
Table 3 Baseline outcomes: intervention versus control group
Primary outcome at different time-points
There was a significant difference between groups for the change in the 6MWD over the first time period between TP1 and TP2, that is the effect of Tele-Rehab or usual waiting time (median 0 versus 12 meters, P=0.01). Counterintuitively, while there was no change in the active intervention group, there was an increase in the distance walked by controls (). There was no difference for the PR phase (). The 16 who attended supervised exercise did demonstrate a median increase of 12.3 m from PR but this was not statistically significant or clinically meaningful. Those not attending supervised exercise showed no change at all.
Table 4 Changes in outcomes between groups: intervention group versus control group
A statistically significant difference between the two walking tests was apparent at each time-point (). Approximately two-thirds of the group walked a small distance further on the second walking test.
Table 5 Comparison of two 6-minute walk test distances conducted 30 minutes apart at different time-points
Secondary outcomes
There were no statistically significant differences between the groups in any of the secondary outcomes ().
Walking diary data revealed no differences between groups in real-time reported walking (), although only 24 walking diaries were returned from a possible 40. Similarly, the average days walked per week and the average minutes per day during the PR phase were much the same for the two groups. Only nine participants recorded barriers to home-walking (being unwell or inclement weather), and seven cited facilitators (walking with another or incorporating exercise into daily activities).
Table 6 Walking diary data: intervention versus controls; exercise attendees versus nonattendees
Retrospectively reported walking (physical activity 1) showed a strong association with real-time recorded walking diary data (physical activity 2), with Pearson’s correlation coefficients (r) being 0.7 for days walked per week and 0.6 for minutes walked per day (P=0.001 and 0.002, respectively).
Discussion
Summary of results
This study investigated extending the reach of PR by using tele-rehab to increase home-based walking for exercise.
We found no obvious objective improvement in the 6MWD for tele-rehab, or PR, with only controls demonstrating a very small and clinically nonmeaningful increase in 6MWD during the waiting period prior to PR. This is not easily explicable, and more likely represents measurement error, rather than a true effect. There were no changes in secondary outcomes.
Although walking diaries correlated well with self-reported exercise, no differences between the intervention or control groups or those who commenced supervised exercise and those who did not were found.
Analyses of the 6MWD data from the two tests conducted at the three time-points revealed a statistically significant but not clinically meaningful increase in distance walked during the second test.
6MWD and physical activity
We found limited evidence for the effectiveness of self-management support via telephone health-mentoring on physical capacity or self-directed exercise at home. Others have similarly concluded that self-management focusing on educationCitation36 or self-management per se has minimal effect on physical capacity.Citation37 Our data support the conclusions of the latter authors that this is due to participants not exercising at sufficient intensity and, as our results indicate, not walking at a sufficient frequency. In contrast, in a recent cohort study of home-based PR with once weekly supervision, participants exercised for at least 5 days per week, for 30 to 45 minutes, and at a higher intensity than our participants did, resulting in a statistically and clinically significant increase in physical capacity.Citation38 Thus, a more demanding program, if enforceable, could have produced better outcomes.
It is possible that our tele-rehab intervention was not of sufficient duration or number of calls. A systematic review of telephone interventions for physical activity in adults, many with chronic conditions although not COPD, suggested that 12 or more calls over a 6–12-month period was effective in improving physical activity and dietary behavior.Citation39 Our study fell short of this demanding schedule, being of only 2 months’ duration with an average of seven calls per individual. Additionally, many of our participants did not complete their walking plans (27%) because they were unwell. It may be that this strategy is just not feasible for those with moderate to severe COPD because of the degree of illness these people experience. Our data revealed a strong correlation between self-reported walking and diary-recorded walking, pointing to the validity of these questions routinely used in Australian physiotherapy clinical practice.
This study has also reinforced the conclusions drawn from our previous study: a mere hour of supervised exercise added to the CDSMP (the structured education component of our PR approach) does not result in clinically important changes in physical capacity or self-reported physical activity.Citation21 This was exacerbated by the low attendance rate at supervised exercise offered separately to the education component in the clinical facility where the study took place. Despite emphasizing the importance of the supervised exercise sessions, compliance even with commencing was low (38%), suggesting that participants may have perceived this to be an “optional extra”. Attendance at exercise sessions may have been improved if this was seen to be a priority and if the importance of supervised exercise was reinforced by peers.Citation40 It is obviously necessary that participants understand that attending higher intensity supervised exercise is paramountCitation5,Citation6 and without this they cannot expect to experience the benefits of PR. Our study supports the wider literature that supervised exercise is an essential component of PR, and it is likely that exercise sessions of substantial intensity, occurring at least twice per week, are needed to improve physical capacity.Citation5,Citation6
This study lends support to the presence of a learning effect for the 6MWD.Citation41 The proportion of people walking further in our study was approximately two-thirds at each of the three time-points, in contrast to the variability of 50%–87% reported in the Field Walking Tests Technical Standards.Citation41 However, the increment was half that reported by othersCitation42 and while statistically significant, it is less than half the MICD.Citation28 Nevertheless, this small change may be important, for example, in a situation where reaching a threshold distance for 6MWD determines suitability for interventions. We would then concur with Holland et alCitation41 that conducting two walking tests and recording the longest distance is recommended. However, if the MICD is to be the benchmark by which efficacy is measured and not 6MWD per se, our results suggest that a second test is not really required.
Study limitations and implications for future practice and research
There were some limitations to our study. First, despite community nurses being trained in core self-management support skills (motivational interviewing,Citation43 problem-solving,Citation44 action planning,Citation45 and communication skills), we do not know the extent of fidelity to the intervention. Recording of telephone calls was an intent but proved to be logistically difficult in practice and was discontinued. If this is to happen in trials set in clinical practice, the equipment must be simple and quickly performed. Second, the tele-rehab intervention may have been better delivered by health professionals, such as physiotherapists who are skilled in the management of exercise, movement, and function for people with COPD. Additionally, individuals may require prior experience of structured exercise as well as integrating this into daily activities.Citation38 Future research may indicate how many supervised sessions are initially required. Third, walking plans may need to be a combination of health professional prescription and self-set criteria, rather than wholly self-set as in the CDSMP paradigm that this study followed; “tough love” may be required. Fourth, while we did address barriers to exercise and physical activity as they arose, we did not investigate illness or exercise perceptions, that is, how people with COPD perceive their condition and their ability to exercise. Perceptions about exercise have been positively correlated with physical capacityCitation46 and the same may hold true for illness perceptions and response to PR. This should be addressed prior to PR commencing, as should issues, such as anxiety and depression, which have now been shown to influence physical activity.Citation47 Furthermore, it was not possible to recruit the number of individuals suggested by the a priori power analyses during the duration of the study. Therefore, nonparametric tests were used where possible. However, due to small cell sizes, results of chi-square tests may not be accurate. Future studies may want to replicate results with larger sample sizes.
Conclusion
In this small but insightful study, there was no benefit to a tele-rehab phase prior to group-based PR. Structured education with self-management skills development (the CDSMP), diary-recorded walking plans, and 1 hour of weekly supervised exercise added little. Two 6MWD tests may not always be necessary, despite a small learning effect. Supervised exercise is a mandatory component of PR. However, ongoing incorporation of exercise into daily life is also essential and there is a huge challenge to achieving this in people with COPD.
Acknowledgments
This work was supported in part by the Royal Hobart Hospital Research Foundation Grant, Hobart, Tasmania, Australia; a Department of Health and Human Services Grant, Hobart, Tasmania, Australia; and a University of Tasmania Research Enhancement Grant, Hobart, Tasmania, Australia. The authors would like to thank Physiotherapy Services, Royal Hobart Hospital, the Menzies Research Institute, Hobart, Tasmania, Australia, where this research took place and the research assistants Roxanne Maher, Carol Phillips, Helen de Hoog, Sharon Rees, and Emmie Bostock for their unfailing assistance. Finally, we are indebted to the community nurses and the people with COPD who willingly gave of their time and of themselves to participate in our research. An abstract pertaining to this paper was presented at the Thoracic Society of Australia and New Zealand Scientific Meeting, Adelaide, Australia, as a poster presentation with interim findings. The poster’s abstract was published in “Poster Abstracts” (TP010, page 59) in (2014), Combined COPD/Cell Biology & Immunology Sig Poster Presentation. Respirology, 19: 58–64. doi: 10.1111/resp.12263_2: http://onlinelibrary.wiley.com/doi/10.1111/resp.12263_2/epdf
Disclosure
The authors report no conflicts of interest in this work.
References
- Global Strategy for the Diagnosis Management and Prevention of COPDGlobal Initiative for Chronic Obstructive Lung Disease (GOLD)2013 Available from: http://www.goldcopdAccessed June 21, 2013
- WilliamsVBrutonAEllis-HillCMcPhersonKWhat really matters to patients living with chronic obstructive pulmonary disease? An exploratory studyChron Respir Dis200742778517621574
- Garcia-AymerichJLangePBenetMSchnohrPAntóJMRegular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort studyThorax200661977277816738033
- Garcia-AymerichJSerraIGómezFPPhysical activity and clinical and functional status in COPDChest20091361627019255291
- BoltonCEBevan-SmithEFBlakeyJDBritish Thoracic Society guideline on pulmonary rehabilitation in adultsThorax201368Suppl 2ii1ii3023880483
- SpruitMASinghSJGarveyCAn official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitationAm J Respir Crit Care Med20131888e13e6424127811
- LacasseYGoldsteinRLassersonTJMartinSPulmonary rehabilitation for chronic obstructive pulmonary diseaseCochrane Database Syst Rev2006184CD003793 Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003793.pub2/abstract17054186
- NgCWhyeLMackneyJJenkinsSHillKDoes exercise training change physical activity in people with COPD? A systematic review and meta-analysisChron Respir Dis201291172622194629
- SimsJHillKHaralambousBNational Physical Activity Recommendations for Older Australians: Discussion DocumentCanberraAustralian Government Department of Health and Ageing2006
- GuyattGThompsonPJBermanBMHow should we measure function in patients with chronic heart and lung disease?J Chron Dis1985385175244008592
- PittaFTroostersTSpruitMAProbstVSDecramerMGosselinkRCharacteristics of physical activities in daily life in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2005171997297715665324
- ParkSKRichardsonCRHollemanRGLarsonJLPhysical activity in people with COPD, using the National Health and Nutrition Evaluation Survey dataset (2003–2006)Heart Lung201342423524023726356
- DesveauxLIJanaudis-FerreiraTGoldsteinRBrooksDAn international comparison of pulmonary rehabilitation: a systematic reviewCOPD201512214415324984085
- Australian Lung FoundationA submission to The Health & Hospital Reform Commission. Improving access to proven self-management therapies for effective chronic disease managementPulmonary Rehabilitation: An IllustrationLutwyche QLD 40302008 Available from: http://www.health.gov.au/internet/nhhrc/publishing.nsf/Content/039-alf/$FILE/039%20-%20SUBMISSION%20-%20Australian%20Lung%20Foundation.pdfAccessed August 11, 2014
- WewelARGellermannISchwertfegerIMorfeldMMagnussenHJörresRAIntervention by phone calls raises domiciliary activity and exercise capacity in patients with severe COPDRespir Med20081021202617920825
- LiuWTWangCHLinHCEfficacy of a cell phone-based exercise programme for COPDEur Respir J200832365165918508824
- AlboresJMaroldaCHaggertyMGerstenhaberBZuWallackRThe use of a home exercise program based on a computer system in patients with chronic obstructive pulmonary diseaseJ Cardiopulm Rehabil Prev2013331475223235321
- SinghVKhandelwalDCKhandelwalRAbusariaSPulmonary rehabilitation in patients with chronic obstructive pulmonary diseaseIndian J Chest Dis Allied Sci2003451131712683707
- WaltersJCameron-TuckerHWillsKEffects of telephone health mentoring in community-recruited chronic obstructive pulmonary disease on self-management capacity, quality of life and psychological morbidity: a randomised controlled trialBMJ Open201339E003097
- Wood-BakerRRobinsonAReidDWaltersEHClinical trial of community nurse mentoring to improve self-management in patients with chronic obstructive pulmonary diseaseInt J COPD20127407413
- Cameron-TuckerHLWood-BakerROwenCJosephLWaltersEHChronic disease self-management and exercise in COPD as pulmonary rehabilitation: a randomized controlled trialInt J COPD20149513523
- HartmanJEBoezenHMDe GreefMHGConsequences of physical inactivity in chronic obstructive pulmonary diseaseExpert Rev Respir Med20104673574521128749
- TroostersTPhysical inactivity in patients with COPD: the next step is … actionPrim Care Respir J201322439139224270366
- LorigKRSobelDSStewartALEvidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trialMed Care199937151410413387
- HollandAHillCRasekabaTLeeANaughtoMMcDonaldCUpdating the minimal important difference for six-minute walk distance in patients with chronic obstructive pulmonary diseaseArch Phys Med Rehabil201091222122520159125
- PuhanMAChandraDMosenifarZThe minimal important difference of exercise tests in severe COPDEur Respir J201137478479020693247
- GuyattGHSullivanMJThompsonPJThe 6-minute walk: a new measure of exercise capacity in patients with chronic heart failureCan Med Assoc J198513289199233978515
- PuhanMMadorMHeldUGoldsteinRGuyattGSchunemannHInterpretation of treatment changes in 6-minute walk distance in patients with COPDEur Respir J20083263764318550610
- BaladyGJAmerican College of Sports Medicine ACSM’s Guidelines for Exercise Testing and Prescription6th edPhiladelphia, LondonLippincott Williams and Wilkins2000
- Department of Health and Human ServicesStrengthening the Prevention and Management of Chronic ConditionsPolicy FrameworkHobart2005
- Royal Australian College of General PractitionersSNAP: a population health guide to behavioural risk factors in general practice2004 Available from: http://www.racgp.org.au/guidelines/greenbookAccessed April 21, 2008
- Australian Government DoHaAAn Active Way to Better Health. National Physical Activity GuidelinesCanberraAustralian Government1999–2005
- Cameron-TuckerHJosephLWaltersJHealth self-management support training positively changes practice for nurses in primary care. Oral Session: O 002Respirology201318Suppl 2103724188199
- Australian Lung FoundationMarket Research ReportPulmonary Rehabilitation Survey2007 Available from: http://www.lungnet.com.au/copd/pr_pulmon_survey.htmlAccessed September 29, 2007
- AlisonJeaThe Pulmonary Rehabilitation Toolkit on behalf of The Australian Lung Foundation (2009)2009 Available from: http://lungfoundation.com.au/health-professionals/clinical-resources/copd/pulmonary-rehabilitation-toolkitAccessed October 17, 2014
- BlackstockFCWebsterKEMcDonaldCFHillCJComparable improvements achieved in chronic obstructive pulmonary disease through pulmonary rehabilitation with and without a structured educational intervention: a randomized controlled trialRespirology201319219320224261584
- ZwerinkMBrusse-KeizerMvan der Valk PaulDSelf management for patients with chronic obstructive pulmonary diseaseCochrane Database Syst Rev2014;19(3CD002990 Available from: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD002990.pub3/abstract24665053
- GrosboisJMGicquelloALangloisCLong-term evaluation of home-based pulmonary rehabilitation in patients with COPDInt J Chron Obstruct Pulmon Dis2015102037204426445534
- EakinEGLawlerSPVandelanotteCOwenNTelephone interventions for physical activity and dietary behavior change: a systematic reviewAm J Prev Med200732541943417478269
- MooreLHoggLWhitePAcceptability and feasibility of pulmonary rehabilitation for COPD: a community qualitative studyPrim Care Respir J201221441942423135218
- HollandAESpruitMATroostersTAn official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory diseaseEur Respir J20144461428144625359355
- HernandesNAWoutersEFMMeijerKAnnegarnJPittaFSpruitMAReproducibility of 6-minute walking test in patients with COPDEur Respir J201138226126721177838
- MillerWRollnickSMotivational InterviewingNew YorkGuildford Press1991
- WarmerdamLvan StratenACuijpersPInternet-based treatment for adults with depressive symptoms: the protocol of a randomized controlled trialBMC Psychiatry20077727818093331
- LeventhalHSingerRJoneSEffects of fear and specificity of recommendation upon attitudes and behaviorJ Pers Soc Psychol196521202914313839
- FischerMJScharlooMAbbinkJConcerns about exercise are related to walk test results in pulmonary rehabilitation for patients with COPDInt J Behav Med2012191394721080250
- SchüzNWaltersJCameron-TuckerHScottJWood-BakerRWaltersHPatient anxiety and depression moderate the effects of increased self-management knowledge on physical activity: a secondary analysis of a randomised controlled trial on health-mentoring in COPDCOPD20151250250925774660
- JonesPWHardingGBerryPWiklundIChenWHKline LeidyNDevelopment and first validation of the COPD Assessment TestEur Respir J200934364865419720809
