Abstract
Background
In patients with COPD, self-management skills are important to reduce the impact of exacerbations. However, both detection and adequate response to exacerbations appear to be difficult for some patients. Little is known about the underlying process of exacerbation-related self-management. Therefore, the objective of this study was to identify and explain the underlying process of exacerbation-related self-management behavior.
Methods
A qualitative study using semi-structured in-depth interviews was performed according to the grounded theory approach, following a cyclic process in which data collection and data analysis alternated. Fifteen patients (male n=8; age range 59–88 years) with mild to very severe COPD were recruited from primary and secondary care settings in the Netherlands, in 2015.
Results
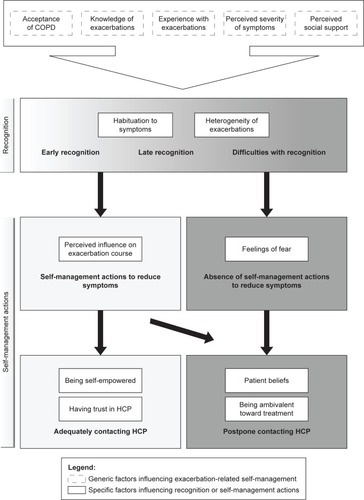
Several patterns in exacerbation-related self-management behavior were identified, and a conceptual model describing factors influencing exacerbation-related self-management was developed. Acceptance, knowledge, experiences with exacerbations, perceived severity of symptoms and social support were important factors influencing exacerbation-related self-management. Specific factors influencing recognition of exacerbations were heterogeneity of exacerbations and habituation to symptoms. Feelings of fear, perceived influence on exacerbation course, patient beliefs, ambivalence toward treatment, trust in health care providers and self-empowerment were identified as specific factors influencing self-management actions.
Conclusion
This study provided insight into factors influencing exacerbation-related self-management behavior in COPD patients. The conceptual model can be used as a framework for health care professionals providing self-management support. In the development of future self-management interventions, factors influencing the process of exacerbation-related self-management should be taken into account.
Introduction
COPD is a highly prevalent chronic disease and a major cause of mortality worldwide.Citation1 The natural course of COPD is interrupted by exacerbations characterized by a sustained worsening of patients’ respiratory symptoms, which are beyond normal day-to-day variability and may warrant medical treatment.Citation1–Citation3 These exacerbations have a serious negative impact on the quality of lifeCitation4,Citation5 and are associated with accelerated lung function decline and increased mortality.Citation6,Citation7 To address the burden of exacerbations, self-management has become increasingly important.Citation8,Citation9 Self-management skills are important to detect exacerbations early and to take prompt action to reduce the impact.Citation10 However, both detecting exacerbations and taking prompt action appear to be difficult for patients.Citation11–Citation13 Previous studies have shown that approximately 50% of exacerbations are not reported to a health care professional and subsequently do not receive adequate treatment.Citation10,Citation14,Citation15
Supporting patients in early detection of an exacerbation and teaching self-management skills using a written action plan have been shown to accelerate recovery time and decrease the acute impact of exacerbations on health status. However, no effects on the quality of life, exacerbation frequency and health care utilization have been observed.Citation16 This may be explained by the sole focus on exacerbation onset and the “one size fits all” approach regarding the design, intensity and mode of delivery in different types of patients.Citation17 Individualized and tailored strategies aimed at changing behavior across the full spectrum of exacerbation-related self-management are expected to result in a higher effect size.Citation17,Citation18 To be able to develop self-management interventions that are acceptable, valued by and effective in patients, more in-depth knowledge is needed on how patients perceive these events and behave accordingly.Citation19
Previous research has shown that patients’ perceptions toward exacerbations are complex and diverse.Citation20–Citation22 A recent meta-synthesis of qualitative studies has provided an improved understanding of patients’ responses and appraisals of exacerbations.Citation23 Furthermore, a recent study investigated patients’ assessment and management of exacerbations at home and showed that they identified exacerbations by visible and invisible symptoms and that health care contact usually occurred when patients no longer felt able to manage their symptoms by themselves.Citation24 Although considerable research has provided insight into patients’ perceptions and experiences regarding exacerbations, the underlying process of exacerbation-related self-management behavior is relatively unexplored. This lack of knowledge subsequently hampers the development of future exacerbation-related self-management interventions with higher effect sizes that fit patients’ needs and requests for care. The objective of this study was to identify and explain the underlying process of exacerbation-related self-management behavior in COPD patients necessary for the development of future targeted and tailored self-management interventions.
Methods
Study design
A qualitative study was performed according to the principles of the grounded theory approach to generate a theory to explain COPD patients’ exacerbation-related self-management behavior.Citation25,Citation26 The study was approved by the Medical Ethics Research Committee of the University Medical Center Utrecht (15-134/C).
Sample and setting
Initially, a purposive sample of Dutch patients with a clinical diagnosis of COPD, who had experienced at least one exacerbation in the past 12 months, was selected by health care providers (HCPs) from four general practices, one physiotherapy practice and one hospital in or near the city of Utrecht during the period of March–October 2015. Patients were eligible to participate if they met the inclusion and exclusion criteria described in . To increase the likelihood of reflecting different perspectives in the findings and ensuring representativeness, maximum variation sampling was used to create a large diversity in patients’ age, sex, COPD severity and time since the last exacerbation. After the initial sampling, the data collection and analysis were alternated following a cyclic process, and theoretical sampling was used to select patients who could enrich the theory as it emerged. Theoretical sampling was continued as much as possible until saturation was reached.Citation26
Table 1 Inclusion and exclusion criteria
Recruitment and informed consent
Patients were informed about the study by their HCP. If a patient was willing to participate, patient’s permission was asked to share contact details with the researcher. Subsequently, the patient received written study information and was contacted by the researcher to make an appointment for the interview. Written informed consent was obtained from all patients. Patients provided consent to consult their medical charts to obtain additional information on several predetermined characteristics. Twenty patients were approached for this study. In total, fifteen patients agreed to participate. Four patients declined to participate, and one patient could not participate due to hospitalization.
Data collection
Semi-structured in-depth individual interviews were performed to investigate patients’ perspectives toward exacerbation-related self-management. Each patient was interviewed once. A topic list was used as a framework for formulating open questions. The topics included perceived symptoms of COPD, perceptions toward exacerbations, performed actions, perceptions toward one’s own role in exacerbation management and needs regarding self-management (Table S1). To clarify the meaning of an exacerbation, patients were asked specifically if they could remember a period of symptom deterioration for which a course of prednisolone and/or antibiotics had been prescribed (Table S1). The topic list was adapted during the process based on emerging theoretical ideas. All interviews started with the same opening question: “How do you experience having a lung disease in your daily life?”.
The interviews were conducted by a nurse scientist with a nursing degree (YK) and health scientist in training (LN). An expert on qualitative research with a nursing background was involved in the process of data collection to ensure methodological quality (SV). The interviews were held in patients’ homes (n=13) or at the hospital (n=2). In three interviews, a partner was present. The duration of the interviews ranged from 45 to 90 minutes. The interview focus shifted to specific topics that were identified through the data analysis. In thirteen interviews, both researchers (YK and LN) were present, and they alternated between the interviewer and observer roles. All interviews were audiotaped. During and directly after the interviews, memos were created to describe observations, reflect on methodological issues and capture initial thoughts related to theoretical concepts.
Baseline characteristics were collected after the interviews through questionnaires. In addition, medical chart reviews were performed to obtain information on the recorded time period since the last exacerbation, lung function and comorbidities. Patient data were encoded and analyzed anonymously.
Data analysis
Data were analyzed according to the grounded theory approach by two independent researchers (YK and LN) and were discussed with a third researcher (SV). All interviews were transcribed verbatim. Data analysis was supported by NVivo 10.0 software (QSR International Pty Ltd, Version 10, 2012). The analysis took place in a cyclic process through open coding, axial coding and selective coding and was alternated with data collection.Citation26,Citation27 Using constant comparison, the identified themes were reviewed for differences and similarities in interview fragments.Citation26,Citation28 Memo writing supported the process of analysis.
First, two researchers (YK and LN) read an interview in its entirety to get an overall picture and then summarized the interview by reflecting on the interview course and information obtained related to the research objective. Second, the interview was reread in more detail, and meaningful paragraphs were open coded independently by both researchers and discussed afterward to reach consensus. Using open coding, the interview data were segmented and an initial list of codes emerged. After five interviews, the analysis shifted toward axial coding, in which codes were categorized according to similarity and organized under main themes.Citation26,Citation27 After axial coding, new data were collected to support initial ideas on connections between categories. Analytic induction was performed after the analysis of ten interviews by testing initial theoretical ideas in new cases. Finally, through selective coding, the categories were refined and connections between the categories were integrated to identify the process of exacerbation-related self-management behavior, leading to a conceptual model explaining this process. Connections between categories were confirmed with the last two interviews leading to saturation.Citation26 The third researcher’s (SV) role in this process included coding a selection of interview data and participating in discussions on the data analysis.
The credibility of the study was enhanced by emphasizing the aim to learn from patients and the researchers’ non-judgmental approach during the interviews. The potential for bias was diminished through the transcription of interviews and the use of researcher triangulation in all phases of the study.Citation29 To further enhance the credibility of the study, the process of data analysis and interpretation was systematically discussed in our research team, comprising experts in the fields of nursing science, qualitative research, self-management and COPD (MS, SV, JT).Citation29 In addition, an external expert on qualitative research performed a peer review on our methodological quality, and a clinical nurse specialist was consulted for a peer review on the interpretation of our conceptual model.
Results
Baseline characteristics of the study population are presented in . Maximum variation was achieved for disease severity (mild to very severe COPD), age (range 59–88 years), sex (almost equally distributed) and time since the last exacerbation (<1–12 months). Prescriptions for self-medication (antibiotics and/or prednisolone) were lacking in the study population, except some patients who received prescriptions during the holidays.
Table 2 Baseline characteristics of the study population (N=15)
Patient perceptions toward exacerbations
When answering our first question, almost all patients started talking about their daily symptoms and functional limitations. Most experienced symptoms were breathlessness, sputum production and fatigue. Hence, symptoms varied widely per individual. Functional limitations were mostly related to exercising, walking and talking. With the exception of two patients, all patients were familiar with the name COPD for their disease.
When asking patients about their experiences with periods of symptom deterioration for which medical treatment was indicated, two patients could not remember having such a period in the past year. Most patients had a clear memory of this period and perceived it as a very unpleasant experience sometimes invoking feelings of fear and anxiety. Only four patients were familiar with the term “exacerbation” or “lung attack” as terms to describe these periods of symptom deterioration. Other patients related these periods to pneumonia, infection or the flu. A few patients did not refer to a certain term since their HCP, in their opinion, had not explicitly mentioned a certain term. Several patients believed that some internal factors, such as emotions, stress and pushing the boundaries regarding activities, could influence exacerbation onset. Other patients attributed exacerbation onset to external factors, such as seasonal influences and air pollution.
Patterns in patients’ exacerbation-related self-management behavior
Based on patients’ stories, a conceptual model describing factors influencing exacerbation-related self-management was developed (). Our conceptual model presents the underlying process of exacerbation-related self-management behavior by explaining its influencing factors. We identified several patterns in exacerbation-related behavior based on two important self-management skills: recognition of an exacerbation and performance of self-management actions. The results are presented by first explaining these patterns in patients’ behavior followed by a description of factors that influence these patterns. The patterns in recognition serve as a starting point. With regard to recognition, three different patterns in patients were identified and detailed in our conceptual model: 1) early recognition, 2) late recognition and 3) difficulties with recognition. Subsequently, these patients showed different types of self-management actions, which were subdivided into “absence of self-management actions”, “self-management actions to reduce symptoms”, and “contacting an HCP”, as explained in .
Table 3 Operationalization types of self-management actions
Patients early recognizing exacerbations
In general, patients who recognized an exacerbation often had experienced more than one exacerbation and perceived these events as a part of their COPD. Symptoms perceived as the onset of an exacerbation were increased fatigue, increased respiratory symptoms (eg, coughing, sputum production and breathlessness), specific pain and fever.
Patients who explained that they were able to recognize an exacerbation at an early stage were generally aware of the importance of early detection and prompt action. They had a pro-active attitude. By closely monitoring symptoms, they felt able to anticipate possible problems. R12: “I try to anticipate on that moment … because I don’t want to let things get that far that I will get a pneumonia”. These patients often performed adequate self-management actions to reduce their symptoms and consulted their HCP on time. Some of these patients monitored their symptoms for 2 or 3 days when they felt able to manage the symptoms by themselves to ensure that the symptoms would not diminish on their own without prescription of medication. If their situation did not improve during this time, they contacted their HCP, or they contacted their HCP immediately in cases of sudden symptom increases. Some of these patients expressed a desire for self-treatment at home since they believed that this arrangement would allow them to take faster action. However, some patients who recognized exacerbations early postponed contacting their HCP.
Patients recognizing exacerbations late
Several patients recognized an exacerbation, but the recognition occurred late, when symptoms had already significantly increased over a number of days. These patients explained having difficulties interpreting their symptoms in a timely manner. Some of these patients realized afterward that symptoms had already been present before they recognized them. R11: “Well, afterwards you can say … oh … that was already present for a few days”. Most of these patients continued their normal daily activities and performed various actions to minimize their symptoms. Several patients adequately contacted their HCP, although most patients postponed seeking medical help until they felt a strong urgency to do so. As a result, some patients reached a point of crisis leading to hospitalization. R02: “I often kept on going way too long. And then, at a certain moment, your blood is out of oxygen. The last time in the hospital I only had 78% oxygen in my blood. So I kept on going way too long”.
Patients having difficulties recognizing exacerbations
Patients having difficulties recognizing an exacerbation did not remember having an exacerbation or remembered receiving antibiotics and/or prednisolone for a temporary increase in symptoms but associated this period with the flu or with other problems dominating during that specific period. These patients did not seem to relate their temporary illness to their COPD. R05: “… and then my husband called the doctor. I said that is not necessary. It will resolve by itself. Everyone experiences flu sometimes”. These patients generally performed little self-management actions. Their self-management actions were similar to their behavior in the stable phase, such as taking short-acting inhalation medication as they were used to doing. Overall, these patients postponed contacting an HCP and followed a wait-and-see approach. These patients expressed having little needs with regard to self-management support.
Factors influencing exacerbation-related self-management behavior
shows that we identified five generic factors influencing both recognition of exacerbations and performance of self-management actions either positively or negatively. In addition, specific factors influencing the ability to recognize an exacerbation or influencing the performance of self-management actions were identified. It is important to note that these factors mutually influenced each other as well. Details of these influencing factors are described in the following paragraphs and further illustrated by quotes in (Q references in the text refer to specific quotes in ).
Table 4 Illustrative quotes related to identified factors influencing exacerbation-related self-management
Generic factors influencing exacerbation-related self-management (both recognition and self-management actions)
Acceptance of COPD
Acceptance of COPD was identified as an important factor influencing patients’ perceptions toward COPD and exacerbations, which subsequently affected exacerbation-related self-management. A wide variety of acceptance was found ranging from difficulties with acceptance to full acceptance. Patients who accepted their COPD perceived exacerbations as events they have to deal with and were therefore more likely to recognize an exacerbation early and to adapt their behavior to their current health status by taking prompt actions (Q1 and Q2). The level of acceptance varied in patients showing late recognition. Some patients acknowledged their symptom deterioration but neglected it and were unable to anticipate on these symptoms as they solely wanted to continue on with their normal lives (Q3). Patients having difficulties with acceptance preferred to avoid confronting their disease and often tried to hide it from others; in some cases, they did so because they felt ashamed. Some of these patients did not attribute an increase in symptoms to their COPD and therefore had difficulties with recognizing an exacerbation and taking prompt actions.
Perceived severity of symptoms
The perceived severity of symptoms varied widely from hardly noticing any symptom deterioration to taking symptom deterioration seriously. Patients who were aware of the gravity of their situation, perceiving exacerbations as hazardous events, often recognized exacerbations early. Furthermore, they explained that their situation would worsen if they postponed their actions. Perceived severity of symptoms varied in patients showing late recognition or difficulties with recognition. Some of them trivialized their situation by describing their symptoms as less serious than they actually were (Q4 and Q5). These patients often recognized an increase in symptoms but took a risk in postponing adequate self-management actions. To interpret their own severity, a substantial group of patients compared themselves to other patients with more severe COPD. These comparisons could influence patients’ perceptions toward the severity of their symptoms in two different ways. On one hand, some patients trivialized their current condition by comparing themselves to others and therefore saw no reason to adapt their behaviors. On the other hand, the comparison led to patients’ recognition of the gravity of their situation and created awareness about the progressive development of COPD, resulting in stronger intentions to perform adequate exacerbation-related self-management (Q6).
Knowledge of exacerbations
Patients with adequate knowledge of exacerbations often recognized exacerbations early and took prompt actions. Patients who were aware of the importance of taking prompt action were convinced that doing so could help them reduce exacerbation severity and recovery time (Q7). However, some of these patients postponed taking action as other influencing factors overruled. Patients having difficulties with recognition had little understanding of exacerbations and explained having little insight into actions they could perform to feel better.
Experience with exacerbations
Patients explained that their former experiences with exacerbations led to their increased confidence in recognizing future exacerbations, which was initiated by having a feeling when something is wrong or by recognizing a pattern of symptoms indicating that an exacerbation is imminent (Q8). Furthermore, patients who had experienced benefits from their past actions were more likely to perform adequate self-management actions (Q9). Negative experiences contributed to the learning curve as well. For example, patients who experienced hospitalization due to postponing their actions often recognized their boundaries better. Moreover, previously experienced feelings of fear and anxiety positively influenced patients’ intentions to perform self-management actions, as they had learned to try to prevent situations that might invoke these feelings by contacting their HCP earlier (Q10).
Perceived social support
Several patients expressed the importance of social support from family and personal relationships, as well as support from HCPs, in self-managing exacerbations. The influence of social support seemed to be highest for patients having difficulties recognizing exacerbations, as they often needed support from family or personal relationships to realize that symptoms were worsening and to stimulate health care contact (Q11). Social support seemed to be less important for patients who recognized exacerbations, although these patients sometimes needed others’ support as well to take symptoms seriously and to take prompt actions. Patients who recognized exacerbations early and took prompt action often felt that they were able to manage exacerbations themselves (Q12). However, when these patients nonetheless postponed contacting an HCP, social support was an influencing factor in the decision to contact an HCP as well.
Factors influencing recognition of exacerbation
Heterogeneity of exacerbations
Heterogeneity of exacerbations was identified as a key factor in distinguishing patients showing late recognition from patients showing early recognition. Some patients felt very capable of recognizing an increase in symptoms but perceived the heterogeneity of exacerbations as a barrier. These patients found it difficult to distinguish an exacerbation from normal day-to-day symptom variations, as the onset of an exacerbation could vary from gradual to sudden, and the types and severity of symptoms were not always consistent (Q13).
Habituation to symptoms
Recognition of an exacerbation was complicated by habituation to the progression of perceived daily symptoms. Patients who experienced habituation to symptoms explained that it became more difficult to determine a significant increase in symptoms, since they had learned to cope with the severity of their symptoms (Q14 and Q15).
Factors influencing self-management actions
Perceived influence on exacerbation course
Patients’ perceived influence on the course of an exacerbation varied widely and was identified as a factor influencing self-management actions. Patients who felt able to influence the course of an exacerbation had a greater internal locus of control and were more likely to take self-management actions to reduce the severity of an exacerbation (Q16). In contrast, patients who felt that they could not influence the course of an exacerbation often postponed taking action (Q17).
Feelings of fear and anxiety
Some patients expressed feelings of fear and anxiety that limited their ability to perform adequate self-management actions to reduce symptoms. They stated that feelings of fear and anxiety were present at the time of acute symptom deterioration and included a fear of dying due to increased breathlessness and feelings of choking. These patients were often aware of strategies to reduce these perceived symptoms (such as breathing techniques and relaxation); yet, these feelings of fear and anxiety interfered with performing these strategies (Q18).
Factors influencing contacting an HCP
Being self-empowered
Being self-empowered was identified as a factor that differentiated patients who contacted their HCP early from patients who postponed contact with their HCP. Self-empowerment refers to the extent to which patients are able to take action based on their own thoughts, believing that they know what is best for themselves. Self-empowered patients in the study prioritized their own health and were able to stand up for themselves (Q19 and Q20). Patients who postponed contact with their HCP were less self-empowered and mostly influenced by a threshold that they perceived. Some of these patients experienced organizational issues as a barrier to contacting their HCP, such as not getting an opportunity to talk with their HCP. These patients were not able to stand up for themselves, resulting in a delay of action with occasionally serious consequences (Q21).
Having trust in HCP
Having trust in an HCP was identified as a factor that influenced patients contacting their HCP as patients described the importance of adequate coaching from their HCP in their self-management actions. Patients who took prompt action often had agreements with their HCP on how to act in response to exacerbations and expressed having confidence in their HCP (Q22). Some patients learned what to do in case of symptom deterioration but felt that they were not taken seriously by their HCP when they felt a need to contact their HCP, leading to postponed health care contact. In addition, some patients experienced difficulties with explaining the seriousness of their symptoms to their HCP. Patients explained that being heard by an HCP contributed to their performance of self-management actions (Q23).
Patient beliefs
For a number of patients, the threshold for contacting an HCP was influenced by their beliefs. Some patients explained that they postponed contacting an HCP out of stubbornness despite knowing better (Q24). Some patients explained having hope that their symptoms would resolve themselves and therefore postponed contacting their HCP. Other patients believed that their social responsibilities (eg, housekeeping, work) were more important than listening to their own feelings (Q25). Finally, some patients explained that they did not want to bother their HCP and therefore postponed health care contact (Q26). A few people explained that this belief was influenced by how they were raised (Q27). Patients who adequately contacted their HCP were sometimes familiar with these beliefs, but having learned from their earlier negative experiences, they were able to adapt their beliefs and consider their own health to be most important.
Being ambivalent toward treatment
Many patients were ambivalent toward taking medication, especially with regard to prednisolone, due to its negative side effects. Consequently, some of these patients postponed contacting their HCP as they preferred not to admit that they needed treatment, although they were aware of its importance. Furthermore, ambivalence toward treatment was reflected by patients who tried to avoid hospitalization and therefore postponed contacting their HCP (Q28). Conversely, patients who were convinced that they needed treatment were more likely to contact their HCP (Q29).
Discussion
This study resulted in a conceptual model explaining factors influencing exacerbation-related self-management. Based on patients’ stories, several patterns in exacerbation-related self-management were identified based on two important self-management skills: recognition of an exacerbation and performance of self-management actions. The identified patterns were dynamic in nature and could change in individual patients over time due to variability in influencing factors and disease progression. Our conceptual model shows that exacerbation-related self-management was influenced by acceptance of COPD, perceived severity of symptoms, knowledge of exacerbations, former experiences with exac-erbations and social support. In addition, specific factors influencing the ability to recognize an exacerbation or the performance of self-management actions were identified.
Several of the findings of this study were in line with other studies. Corresponding with previous research, we found that patients often had difficulties understanding the term “exacerbation”Citation22,Citation24 and that patients reported both personal and environmental factors that may cause exacerbations.Citation30 Our finding that exacerbation-related self-management behavior was determined by personal beliefs, perceptions regarding seriousness of the disease, knowledge of exacerbations and former experiences with exacerbations is consistent with the Health Belief Model.Citation31–Citation33 Furthermore, in line with previous research, acceptance was considered to be important for behavior change toward self-management,Citation34,Citation35 and the importance of social support was strengthened by previous research emphasizing the need to involve others in self-management support to change behavior.Citation36 Consistent with previous research focusing on self-management actions, our study found that feelings of fear and anxiety resulted in perceived powerlessness in response to symptomsCitation23 and perceived control on exacerbation course influenced self-management actions.Citation37–Citation40 Previous studies have also observed differences between patients who pro-actively monitored the course of an exacerbation and contacted their HCP on time and patients who postponed health care contact until feeling an urgency for medical care.Citation21,Citation24,Citation30,Citation41 Finally, regarding smoking in relation to self-management, our study concurred with earlier studies in showing that smoking was not an explanatory factor for self-management behavior.Citation42,Citation43
Our findings expand upon prior work by identifying patient beliefs, ambivalence toward treatment, self-empowerment and trust in HCPs as specific factors influencing health care contact. Patient belief was identified as a barrier for seeking medical help since various patients felt that they “bothered” their HCP. As patients explicitly mentioned their upbringing as influencing factor, this finding might be due to this older population of COPD patients being raised not to bother other people with personal problems.Citation21,Citation41 Furthermore, some patients who postponed health care contact did so because they felt that they were “not being heard” by their HCP. This finding might be explained by previous research showing that patients sometimes feel that they do not have legitimized reasons to seek help.Citation21,Citation23 The identified ambivalence toward treatment can be explained by the Health Belief Model and by previous work showing that considering the side effects of medication was related to medication adherence.Citation24,Citation31
To date, the literature has been inconclusive regarding patients’ skills toward recognition of exacerbations. Williams et alCitation24 showed that patients “just know” when they are experiencing exacerbations and that the majority of patients feel capable of distinguishing “bad days” from exacerbations, while our study identified patients showing early recognition, late recognition and patients having difficulties with recognition. These differences could be due to the recruitment strategies in the study of Williams et al. As it was part of a trial evaluating a self-management support intervention, the sample of patients may have had more engagement in self-management.Citation24 However, in line with our study, Adams et alCitation21 showed that patients did not immediately remember exacerbations and described them as “forgotten events”. Furthermore, we identified the heterogeneity of exacerbations as an important barrier that differentiated patients recognizing exacerbations late from patients early recognizing exacerbations. However, previous studies have reported that most patients had predictable symptoms and could easily identify consistent warning signs, which may have been due to the inclusion of patients with more exacerbation experiences in those studies.Citation22,Citation24 Moreover, we found that recognition was complicated by patients’ habituation to their stable symptom severity and daily fluctuations, which has not been described in previous research to our knowledge.
An important strength of this study was that data were independently analyzed by two researchers and discussed with an expert on qualitative research during the entire process. Furthermore, both credibility and confirmability were enhanced by systematically discussing the interpretation of data with experts in the field. Although the results of this study were based on fifteen patients, maximum variation sampling increased the likelihood of diversity in our data collected from a representative selection of patients, which contributed to the transferability of the study. However, this study had a few limitations. Medical chart reviews showed afterward that the inclusion and exclusion criteria were not fully met in two patients with GOLD stage 1. Their charts showed conflicting data with regard to lung function and GOLD stage, and one patient had experienced an exacerbation >12 months ago. Nonetheless, these patients were not excluded from the study since they were considered to be eligible by their HCPs and were able to share their experiences regarding exacerbations. Furthermore, the interpretation of data was based on patients’ perceptions regarding exacerbations. This might have affected the credibility of our study since previous research has shown that some patients show little understanding regarding exacerbations.Citation21,Citation22 To address this potential limitation, we clarified the term exacerbation by asking patients specifically if they could remember a period of symptom deterioration for which medical treatment was indicated.
The conceptual model provided insight into different patterns of exacerbation-related self-management and factors influencing this behavior. Since needs and requests for care flowed naturally from the problems perceived by patients,Citation19 the identified influencing factors guided our implications for practice and future research. The conceptual model provides a framework for HCPs to identify patterns in patients’ exacerbation-related self-management and stresses the need for better assessment on influencing factors to enhance self-management by eliminating identified barriers. When an HCP identifies poor exacerbation-related self-management, self-management support should be intensified, which may consist of teaching self-monitoring skills and exacerbation education supported by an action plan.Citation16,Citation44 HCPs should be aware that these patients might express limited needs regarding self-management support themselves. Patients who recognize exacerbations, and show adequate self-management skills, may benefit from continued education and decision support. HCPs should notice that patients who postpone health care contact might be experiencing barriers in the patient–HCP relationship. For this subgroup of patients, it is important that they are being heard by their HCP and that HCPs listen carefully and take their patient’ expertise seriously. Finally, patients who show adequate exacerbation-related self-management may benefit from continued self-management support and possibly self-treatment.
Moreover, the conceptual model is important for future development of self-management interventions since it shows which influencing factors should be taken into account during the development and delivery of interventions. Based on this model, special attention should be paid to the elimination of barriers in the process of self-management to be able to develop effective self-management interventions that fit patients’ perceptions, capabilities, needs and request for care. Future research should focus on the development of targeted and tailored interventions to improve the full spectrum of exacerbation-related self-management and, subsequently, reduce the impact of exacerbations.
Conclusion
This study provided in-depth insight into factors influencing exacerbation-related self-management in COPD patients. Several patterns in exacerbation-related self- management behavior were identified based on two important self-management skills: recognition of an exacerbation and performance of self-management actions. This study confirmed that recognition of exacerbations can be challenging and that self-management actions are often inadequate. The conceptual model explaining factors that influence exacerbation-related self-management can be used as a framework for health care professionals providing self-management support and as a guide for the development of future individualized and tailored exacerbation-related self-management interventions.
Acknowledgments
We thank all patients who participated in the interviews for sharing their time and experiences, and we acknowledge all health care centers for recruiting patients for this study. Furthermore, we thank Marlies Schrijvers, PhD, for her peer review of this study’s methodology and Remco Verbrugge, MSc, for his peer review of the conceptual model through his expertise as a COPD clinical nurse specialist. No funding was provided for this study.
Supplementary material
Table S1 Topic list
Disclosure
The authors report no conflicts of interest in this work.
References
- Global Initiative for Chronic Obstructive Lung Disease (GOLD)Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease [updated 2016] Available from: http://goldcopd.org/global-strategy-diagnosis-management-prevention-copd-2016/Accessed February 2, 2016
- Rodriguez-RoisinRToward a consensus definition for COPD exacerbationsChest20001175 suppl 2398S401S10843984
- BurgeSWedzichaJACOPD exacerbations: definitions and classificationsEur Respir J Suppl20034146s53s12795331
- MiravitllesMFerrerMPontAIMPAC Study GroupEffect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up studyThorax200459538739515115864
- SeemungalTADonaldsonGCPaulEABestallJCJeffriesDJWedzichaJAEffect of exacerbation on quality of life in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med19981575 pt 1141814229603117
- DonaldsonGCSeemungalTABhowmikAWedzichaJARelationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary diseaseThorax2002571084785212324669
- Soler-CatalunaJJMartinez-GarciaMARoman SanchezPSalcedoENavarroMOchandoRSevere acute exacerbations and mortality in patients with chronic obstructive pulmonary diseaseThorax2005601192593116055622
- BourbeauJvan der PalenJPromoting effective self-management programmes to improve COPDEur Respir J200933346146319251792
- EffingTWVercoulenJHBourbeauJDefinition of a COPD self-management intervention: International expert group consensusEur Respir J2016481465427076595
- WilkinsonTMDonaldsonGCHurstJRSeemungalTAWedzichaJAEarly therapy improves outcomes of exacerbations of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2004169121298130314990395
- BucknallCEMillerGLloydSMGlasgow supported self-management trial (GSuST) for patients with moderate to severe COPD: randomised controlled trialBMJ2012344e106022395923
- TrappenburgJCSchaapDMonninkhofEMHow do COPD patients respond to exacerbations?BMC Pulm Med2011114321854576
- BischoffEWHamdDHSedenoMEffects of written action plan adherence on COPD exacerbation recoveryThorax2011661263121037270
- XuWColletJPShapiroSNegative impacts of unreported COPD exacerbations on health-related quality of life at 1 yearEur Respir J20103551022103019897555
- LangsetmoLPlattRWErnstPBourbeauJUnderreporting exacerbation of chronic obstructive pulmonary disease in a longitudinal cohortAm J Respir Crit Care Med2008177439640118048806
- TrappenburgJCMonninkhofEMBourbeauJEffect of an action plan with ongoing support by a case manager on exacerbation-related outcome in patients with COPD: a multicentre randomised controlled trialThorax2011661197798421785156
- TrappenburgJJonkmanNJaarsmaTSelf-management: one size does not fit allPatient Educ Couns201392113413723499381
- SpruitMAFranssenFMRuttenEPWopereisSWoutersEFVanfleterenLEA new perspective on COPD exacerbations: Monitoring impact by measuring physical, psychological and social resilienceEur Respir J20164741024102727037307
- van MeijelBGamelCvan Swieten-DuijfjesBGrypdonckMHThe development of evidence-based nursing interventions: methodological considerationsJ Adv Nurs2004481849215347414
- BarnesNCalverleyPMKaplanARabeKFChronic obstructive pulmonary disease and exacerbations: patient insights from the global hidden depths of COPD surveyBMC Pulm Med2013135423971625
- AdamsRChavannesNJonesKOstergaardMSPriceDExacerbations of chronic obstructive pulmonary disease – a patients’ perspectivePrim Care Respir J200615210210916701769
- KesslerRStahlEVogelmeierCPatient understanding, detection, and experience of COPD exacerbations: an observational, interview-based studyChest2006130113314216840393
- HarrisonSLAppsLSinghSJSteinerMCMorganMDRobertsonN‘Consumed by breathing’ – a critical interpretive meta-synthesis of the qualitative literatureChronic Illn2014101314924227018
- WilliamsVHardingeMRyanSFarmerAPatients’ experience of identifying and managing exacerbations in COPD: a qualitative studyNPJ Prim Care Respir Med2014241406225372181
- GlaserBGStraussALThe Discovery of Grounded Theory: Strategies for Qualitative Research7th edElmer, NJAldine1967
- BoeijeHAnalysis in Qualitative Research1st edLondonSage Publications2010
- StraussALCorbinJBasics of Qualitative Research. Techniques and Procedures for Developing Grounded Theory3rd edThousand Oaks, CASage Publications2007
- WesterFStrategieën voor kwalitatief onderzoek. [Strategies for Qualitative Research]3rd edMuiderbergCoutinho1995
- LincolnYSGubaEGNaturalistic InquiryNewbury Park, CASage Publications1985
- HernandezPBalterMBourbeauJHodderRLiving with chronic obstructive pulmonary disease: a survey of patients’ knowledge and attitudesRespir Med200910371004101219269150
- RosenstockIMStrecherVJBeckerMHSocial learning theory and the health belief modelHealth Educ Q19881521751833378902
- BanduraASelf-efficacy: toward a unifying theory of behavioral changePsychol Rev1977842191215847061
- BanduraASelf-efficacyRamachaudranVSEncyclopedia of Human Behavior4New York, NYAcademic Press19947181
- VercoulenJHA simple method to enable patient-tailored treatment and to motivate the patient to change behaviourChron Respir Dis20129425926823129804
- BoerLMDaudeyLPetersJBMolemaJPrinsJBVercoulenJHAssessing the stages of the grieving process in chronic obstructive pulmonary disease (COPD): validation of the acceptance of disease and impairments questionnaire (ADIQ)Int J Behav Med201421356157023645551
- CicuttoLBrooksDHendersonKSelf-care issues from the perspective of individuals with chronic obstructive pulmonary diseasePatient Educ Couns200455216817615530751
- DislerRTGallagherRDDavidsonPMFactors influencing self-management in chronic obstructive pulmonary disease: an integrative reviewInt J Nurs Stud201249223024222154095
- DowsonCATownGIFramptonCMulderRTPsychopathology and illness beliefs influence COPD self-managementJ Psychosom Res200456333334015046971
- BourbeauJClinical decision processes and patient engagement in self-managementDis Manage Health Outcomes2008165327333
- GlanzKRimerBViswanathKTheory of reasoned action, theory of planned behaviour, and the integrated behavioral modelHealth Behaviour and Health Education. Theory, Research and Practice4th edSan Fransisco, CAYossey-Bass20086796 Available from: http://www.sanjeshp.ir/phd/phd_91/Pages/Refrences/health%20education%20and%20promotion/[Karen_Glanz,_Barbara_K._Rimer,_K._Viswanath]_Heal(BookFi.or.pdfAccessed February 2, 2016
- Gruffydd-JonesKLangley-JohnsonCDyerCBadlanKWardSWhat are the needs of patients following discharge from hospital after an acute exacerbation of chronic obstructive pulmonary disease (COPD)?Prim Care Respir J200716636336818038104
- KorpershoekYBos-TouwenIDde Man-van GinkelJMLammersJWSchuurmansMJTrappenburgJDeterminants of activation for self-management in patients with COPDInt J Chron Obstruct Pulmon Dis2016111757176627536087
- Bos-TouwenISchuurmansMMonninkhofEMPatient and disease characteristics associated with activation for self-management in patients with diabetes, chronic obstructive pulmonary disease, chronic heart failure and chronic renal disease: A cross-sectional survey studyPLoS One2015105e012640025950517
- ZwerinkMBrusse-KeizerMvan der ValkPDSelf management for patients with chronic obstructive pulmonary diseaseCochrane Database Syst Rev20143CD00299024665053