Abstract
Background
Physical inactivity is associated with poor outcomes in COPD, and as a result, interventions to improve physical activity (PA) are a current research focus. However, many trials have been small and inconclusive.
Objective
The aim of this systematic review and meta-analysis was to study the effects of randomized controlled trials (RCTs) targeting PA in COPD.
Methods
Databases (Physiotherapy Evidence Database [PEDro], Embase, MEDLINE, CINAHL and the Cochrane Central Register for Controlled Trials) were searched using the following keywords: “COPD”, “intervention” and “physical activity” from inception to May 20, 2016; published RCTs that aimed to increase PA in individuals with COPD were included. The PEDro scale was used to rate study quality. Standardized mean differences (effect sizes, ESs) with 95% confidence intervals (CIs) were determined. Effects of included interventions were also measured according to the minimal important difference (MID) in daily steps for COPD (599 daily steps).
Results
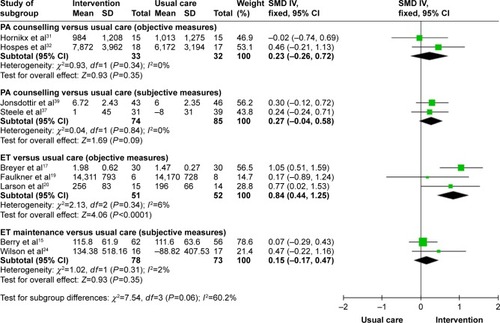
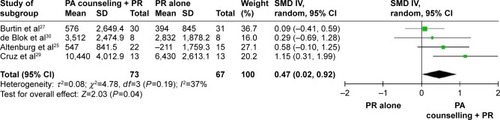
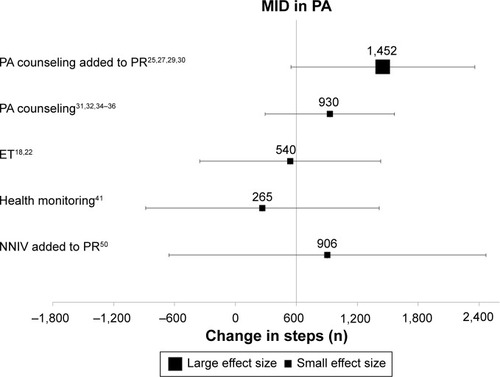
A total of 37 RCTs with 4,314 participants (mean forced expiratory volume in one second (FEV1) % predicted 50.5 [SD=10.4]) were identified. Interventions including exercise training (ET; n=3 studies, 103 participants) significantly increased PA levels in COPD compared to standard care (ES [95% CI]; 0.84 [0.44–1.25]). The addition of activity counseling to pulmonary rehabilitation (PR; n=4 studies, 140 participants) showed important effects on PA levels compared to PR alone (0.47 [0.02–0.92]), achieving significant increases that exceeded the MID for daily steps in COPD (mean difference [95% CI], 1,452 daily steps [549–2,356]). Reporting of methodological quality was poor in most included RCTs.
Conclusion
Interventions that included ET and PA counseling during PR were effective strategies to improve PA in COPD.
Introduction
Physical inactivity is a key predictor of increased hospitalization and all-cause mortality in COPD.Citation1,Citation2 A systematic review comparing activity levels in COPD patients with age-matched controls showed a marked reduction in activity duration, intensity and daily step counts, regardless of disease severity.Citation3 Physical activity (PA) levels are strongly correlated with functional exercise capacity.Citation4 In addition, a large 5-year follow-up study showed important associations between levels of PA and health-related quality of life (HRQL) in COPD.Citation5
In light of the strong relationship between PA and health outcomes in COPD, the past decade has witnessed the development of several strategies aiming to improve PA levels in COPD. The number of randomized controlled trials (RCTs) designed to test the efficacy of these interventions is growing rapidly. A recent review that studied the effects of RCTs, non-RCTs and experimental studies of PA interventions concluded that although exercise training (ET) is the most commonly used approach, its effects on PA levels are uncertain.Citation6 The inclusion of non-RCTs in this review is a potential source of bias that might overestimate the true effects of PA interventions.Citation7 To date, attempts to compare effects of interventions on PA levels using meta-analysis of published RCTs exclusively have not been reported. In this systematic review, we aimed to analyze and compare the effects of various PA interventions reported through RCTs in COPD.
Methods
The systematic review protocol is registered in PROSPERO (CRD42013004460, http://www.crd.york.ac.uk/PROSPERO).
Inclusion criteria
Studies that recruited participants diagnosed with COPD according to the Global Initiative for Chronic Obstructive Lung Diseases (GOLD) guidelines were included.Citation8 In the case of mixed populations, studies were included if 80% or more of individuals had COPD. RCTs published in peer-reviewed journals that aimed to evaluate the efficacy of interventions to improve PA levels were included. These comprised, but were not limited to, pulmonary rehabilitation (PR), ET, pharmaceutical treatment, self-management or written advice. Studies were included if PA was either a primary or a secondary outcome.
The primary outcome of the review was PA measured either objectively (eg, time spent in PA measured by activity monitors) or subjectively (eg, scores of questionnaires). Secondary outcomes of the review were functional and maximal exercise capacity, HRQL, dyspnea and lung function variables.
Search methods
Databases searched were the Cochrane library, Physiotherapy Evidence Database (PEDro), Embase, MEDLINE and CINAHL. The subject headings were “COPD”, “interventions” and “physical activities” (Supplementary materials). Databases were searched through two separate periods: from their inception to the end of January 2015 and from February 2015 to May 20, 2016. In addition, we searched major trial registries including ClinicalTrials.gov, European Union Clinical Trial Register, Australian New Zealand Clinical Trials Registry and WHO International Clinical Trials Registry Platform for relevant projects.
One author (AL) reviewed the title and abstract of trials and two authors (AL and AEH) independently assessed the full text of articles to decide on inclusion. Any disagreement was resolved by discussion. Data were extracted independently by two authors (AL and AEH) using a standardized data extraction sheet (Supplementary materials). Online software was used to extract data from plots and graphs where necessary (www.arohatgi.info/WebPlotDigitizer).
Quality assessment was performed using the PEDro quality scale, which is an 11-item scale that assesses internal and external validity of clinical trials.Citation9 The higher the given score, the better the quality. Cut points of the scale were excellent (9–10), good (6–8), fair (4–5) and poor (≤3).
Data interpretation and synthesis
Comparisons of interest were interventions aimed to improve PA versus usual care (or placebo), interventions aimed to improve PA added to PR versus PR alone, and PA intervention versus another active PA intervention. Effects of interventions on continuous outcome measures were assessed using standardized mean differences (SMDs) and 95% confidence intervals (CIs), to allow comparison of effect size (ES) across interventions. Trials reporting effects of interventions using comparable outcome measures at comparable time points were combined in a meta-analysis. Software used to conduct meta-analysis and compute ESs was Review Manager 5.3 manufactured by the Nordic Cochrane Centre. Based on Cohen’s classifications, an SMD of 0.2 is small, 0.5 is moderate and 0.8 or higher is a large effect.
Meta-analysis was conducted where trials were statistically and clinically homogeneous. Statistical homogeneity was defined as I2≤40%.Citation7 Clinical homogeneity was defined as similarity of study population, intervention components and their comparators and selected outcome measures. In the case of PA levels in an included RCT being measured using more than one variable, the variable that best reflects PA levels was selected for meta-analysis (eg, objectively measured time spent in walking was selected over self-reported PA time,Citation10 and overall PA time was selected over PA time spent in 1 day).Citation11 Objectively and subjectively measured PA variables were not pooled together in a meta-analysis. When available, change scores were extracted to measure the effects of interventions. In the case of a change score not being directly provided, baseline and final scores were used to measure mean differences, and available variables of the change (eg, correlation coefficient of the change) were used to compute standard deviation of the change.Citation7 When necessary, study investigators were contacted for additional information to compute change scores. Final scores at available time points were extracted when change score was unable to be computed.
We intended to perform sensitivity analyses to examine the effects of trial quality by excluding trials without concealed allocation and assessor blinding; however, insufficient data prevented these analyses.
In trials where PA was measured in daily steps, weighted mean differences in steps achieved by interventions were compared. Changes in the number of steps from baseline produced by different interventions were compared to the minimal important difference (MID), which has been estimated to be a change of 599 daily steps.Citation12 MID is defined as a meaningful change or effect that might be considered important to produce sizeable change in vital outcomes.Citation13
Results
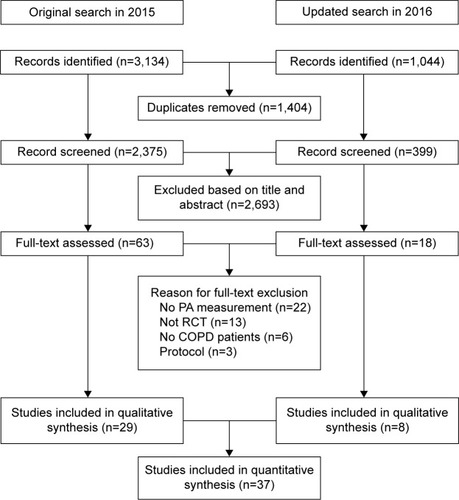
The search yielded a total of 4,178 records identified throughout the two separate periods, with 81 full texts reviewed for eligibility. A Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram () depicts the search process. A total of 37 RCTs identified in 40 separate reports met our selected criteria and were included in the systematic review.
Figure 1 PRISMA flow diagram for database search and study selection process.
Quality assessment
The quality of included studies ranged from fair to good (median PEDro score, interquartile range [IQR] =6 [5–7]; ), with only one study scoring poorly.Citation14 A total of 18 studies (48% of included RCTs) failed to conceal allocation, 27 studies (73% of included RCTs) failed to blind subjects and 23 studies (62% of included RCTs) failed to blind outcome assessors. Another common limitation was the inability to report outcomes for >85% of randomized subjects (n=20, 54%; ).
Table 1 Qualitative synthesis of included studies using PEDro scale for the quality of RCTs
Characteristics of included RCTs
Included RCTs measured the effects of ET (n=10),Citation15–Citation24 activity counseling (n=15),Citation25–Citation40 health monitoring (n=1),Citation41,Citation42 pharmacological treatment (n=3),Citation43–Citation45 nutritional interventions (n=2),Citation46–Citation48 oxygen therapy (n=4),Citation14,Citation49–Citation51 urban walking circuits (n=1)Citation52 and integrated disease management (n=1)Citation53 on PA levels in COPD. PA counseling was delivered either in a center-based setting (n=9),Citation25–Citation27,Citation29,Citation30,Citation32–Citation34,Citation39 through phone calls (n=3)Citation31,Citation36,Citation37 or by internet-mediated approaches (n=3).Citation35,Citation38,Citation40 Studies compared interventions to usual care (n=16),Citation15–Citation17,Citation19,Citation20,Citation24,Citation31,Citation32,Citation37,Citation39,Citation41,Citation42,Citation45–Citation48,Citation51,Citation53 PR programs (n=8)Citation25,Citation27–Citation30,Citation33,Citation43,Citation50,Citation52 or another active intervention (n=13).Citation14,Citation18,Citation21–Citation23,Citation26,Citation34–Citation36,Citation38,Citation40,Citation44,Citation49 Characteristics of included studies are summarized in .
Table 2 Characteristics of included studies
Characteristics of included subjects
This review included a total of 4,314 participants (males = 58%). Mean age of included participants was 66.2 (SD 4.3) years with a mean forced expiratory volume in one second (FEV1) % predicted of 50.5 (10.4). All participants had a confirmed diagnosis of COPD according to the GOLD guidelines.Citation8
Characteristics of PA measurement tools
RCTs assessed PA using several outcome measures. Objective measures included accelerometers (n=18, 50%),Citation16,Citation17,Citation20–Citation23,Citation27,Citation29,Citation33,Citation36,Citation37,Citation41,Citation44–Citation49,Citation51 pedometers (n=8, 22%)Citation18,Citation25,Citation30,Citation32,Citation34,Citation35,Citation38,Citation50 and an activity monitor (n=1).Citation31 PA was also measured subjectively using validated tools such as Seven-Day PA Recall Questionnaire (n=1),Citation19 PA Scale for the Elderly (PASE) questionnaire (n=1),Citation15 Community Healthy Activities Model Program for Seniors (CHAMPS) questionnaire (n=1)Citation26 and the International PA Questionnaire (IPAQ; n=3).Citation24,Citation39,Citation53 Nonvalidated tools to measure PA included exercise diary cards (n=1)Citation52 and trial-designed activity questionnaires (n=3).Citation14,Citation40,Citation43
Analysis of included interventions
Effects of PA interventions on PA levels
Studies comparing PA interventions versus usual care or placebo
When comparing PA counseling alone to usual care, there were small and nonsignificant effects of counseling on PA for both objective measures (n=2 studies, SMD [95% CI] 0.23 [−0.26 to 0.72], time point 1–3 months; )Citation31,Citation32 and subjective measures (n=2 studies, −0.27 [−0.04 to 0.58], 12 months; ).Citation37,Citation39 Four months of ET produced moderate to large statistically significant effects on PA (n=3 studies, 0.84 [0.44–1.25]; ),Citation17,Citation19,Citation20 whereas long-term maintenance exercise programs showed small nonsignificant effects on PA at 12 and 15 months post-intervention (n=2 studies, 0.15 [−0.17 to 0.47]; ).Citation15,Citation24 None of the studies included in the meta-analyses had blinded the assessors or the therapists from study groups. One study of essential amino acid (EAA) supplementationCitation46,Citation47 reported an increase in steps favoring the intervention arm at 3 months (577.6 steps, P=0.02); however, insufficient sample size details prevented ES calculations (Table S1). Important increases in daily steps were also reported in a crossover RCT in favor of the once-daily long-acting beta agonist, indacaterol 150 μg,Citation45 compared to placebo at 3 weeks (0.32 [0.02–0.63]; Table S1).
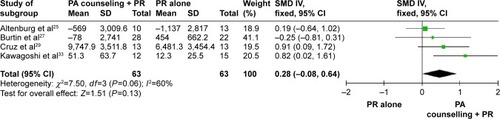
Studies comparing PA interventions added to PR versus PR alone
Adding activity counseling to PR produced short-term improvements in PA at 3 months compared to PR alone (n=4 studies, 0.47 [0.02–0.92]; and ).Citation25,Citation27–Citation30 Two of the four studies included in this meta-analysis had assessor blinding and concealed allocation.Citation27,Citation29 When analyzing sustainability of results, pooled meta-analysis showed small to moderate long-term effects of PA counseling added to PR that trended to statistical significance versus PR alone (n=4, 0.28 [−0.08 to 0.31]; I2, 60%; ).Citation25,Citation27,Citation29,Citation33 Of the included studies pooled in this analysis, the only study with assessor blinding did not report similar long-term effects on steps at 6 months post-intervention (n=1 study, 0.25 [−0.81 to 0.31]; ).Citation27 Introducing an urban walking circuit promotion program for 12 months after a 3-month course of PR improved baseline walking time when compared to usual care after PR (1.36 [0.84–1.88]; Table S2).Citation52
Studies comparing PA interventions versus another intervention
ET: Although 3 months of high-intensity ET had similar effects to light-intensity training on daily steps and walking time (−0.13 [−0.76 to 0.49] and 0.26 [−0.36 to 0.89], respectively; ), effects on time spent in moderate to vigorous physical activity (MVPA) favored the high-intensity training group at 3 months (1.16 [0.49–1.84]; ).Citation22 When comparing 6 months of home-based walking with fixed speed program to home-based walking with fixed distance,Citation21 significant increases in daily metabolic equivalent tasks (0.94 [0.25–1.63]; ) and daily MVPA time (0.72 [0.04–1.39]; ) were achieved by fixed speed walking at 12 months. Moreover, adding community-based ET to a self-management program showed moderate and significant effects on activity levels at 12 months when compared to self-management alone (0.48 [0.10–0.86]; ).Citation18
Table 3 Studies comparing PA interventions versus another active intervention
Counseling and self-management: Four months of pedometer-based counseling showed important effects on daily steps when delivered via an internet-mediated program (0.84 [0.59–1.08]; )Citation35 or through 3 months of individualized sessions (1.08 [0.65–1.15]; )Citation34 when compared to standard counseling. An internet-mediated dyspnea self-management program also showed important increases in exercise duration assessed by a nonvalidated tool compared to internet-mediated education at 12 months (0.57 [0.13–1.00]; ). None of the other interventions in this group showed important effects on PA when compared to other active interventions (eg, individualized ET versus general ETCitation23 and the once-daily long-acting muscarinic antagonist, tiotropium added to PA counseling versus placebo added to PA counseling;Citation44 Table S3).
MID of PA
Limiting the analysis to 13 trials (456 actively treated subjects) that used daily steps to measure the change in PA from baseline, only the studies that tested the addition of activity counseling to PR (n=4 studies)Citation25,Citation27,Citation29,Citation30 showed large effects that exceeded the established MID of 599 daily steps (mean difference [95% CI], 1452 [549–2,356]; ). While PA counseling aloneCitation31,Citation32,Citation34–Citation36 and the addition of nocturnal noninvasive ventilation (NNIV)Citation50 to PR achieved a mean difference in steps that exceeded MID, the ES was small and did not reach statistical significance (PA counseling [n=5 studies]: 930 [293–1,566], NNIV + PR [n=1 study]: 906 [−655 to 2,467]; ). ET (n=2 studies)Citation18,Citation22 and health monitoring via phone calls (n=1 study)Citation41 achieved differences in steps that did not exceed the MID for daily steps in COPD ().
Effects of PA interventions on functional exercise capacity
Compared to standard care, ET interventions including maintenance programCitation15 and Nordic walkingCitation17 significantly improved 6-minute walk distance (6MWD) after 6 months (0.48 [0.11–0.85] and 0.73 [0.20–1.25]; Table S4), respectively. Exercise adherence counseling also produced important effects on 6MWD at 4 months (0.44 [0.01–0.86]; Table S4).Citation37 However, these effects were not sustained at 12 months when compared to usual care (0.29 [−0.18 to 0.76]; Table S4).Citation37
Adding tiotropium to PR produced moderate effects on treadmill endurance time compared to placebo (0.67 [0.01–1.33]; Table S4).Citation43 Moderate effects on exercise capacity were also achieved after the addition of an urban walking circuit promotion program to usual care 12 months after PR (0.59 [0.12–1.07]; Table S4).Citation52
The addition of self-management to community-based ET moderately improved incremental shuttle walk distance at 12 months (0.43 [0.09–0.77]; Table S4).Citation18 Improvements in endurance shuttle walk time were present after individualized ET compared to general ET at 2 months (0.72 [0.35–1.09]; Table S4).Citation23
Effects of PA interventions on HRQL
Compared to usual care, only Nordic walking enhanced HRQL using the 36-Item Short Form Survey (SF36) physical performance domain at 3 months (1.17 [0.58–1.76]; Table S5).Citation17 Effects were sustained when reassessed 9 months post-intervention (1.61 [0.98–2.24]; Table S5).Citation17
Pedometer-based counseling produced moderate to large effects on HRQL measured using SGRQ at 3 months when compared to standard counseling in two studies (0.43 [0.03–0.83] and 1.04 [0.00–2.07]; Table S5).Citation34,Citation35 One month of activity counseling via tele-rehabilitation produced moderate effects on Clinical COPD Questionnaire when compared to ET (0.53 [1.17–0.22]; Table S5).Citation38
None of the included interventions showed important effects on dyspnea or lung function when compared to their comparators at measured time points (Tables S6 and S7).
Discussion
This systematic review found that when compared to usual care, ET including Nordic walking,Citation17 supervised exerciseCitation19 and self-efficacy enhancing exerciseCitation20 produce large effects on PA levels in COPD. These effects were not sustained after a long-term exercise maintenance program.Citation15,Citation24 While PA counseling alone failed to improve PA, the addition of counseling to PR programs succeeded in producing an important increase in activity levelsCitation25,Citation27,Citation29,Citation30,Citation33 compared to PR alone. Moreover, nutritionalCitation46,Citation47 and pharmaceuticalCitation45 interventions significantly increased PA compared to placebo; however, insufficient data and poor methodological quality restricted pooled ES calculations for these interventions. Of all included interventions, only individualized and pedometer-based counseling added to multidisciplinary PR program produced changes that exceed the newly established MID in daily steps for COPD.Citation25,Citation27,Citation29,Citation30
While PR alone achieved important increases in activity levels,Citation6 compared to usual care at 4 months, our analysis showed that providing persistent and individualized feedback on activity levels using wearable monitors in conjunction with PR achieved significant effects on activity levels that exceeded effects produced by PR alone after 3–6 months.Citation25,Citation27,Citation29,Citation30 Moreover, the addition of counseling to PR achieved significant differences in daily steps that exceeded the established MID in daily steps at 3 months while PR alone failed to produce comparable outcomes at similar time points. It is important to mention that, of the included studies that evaluated the addition of counseling to PR, three of four studies failed to blind assessors, which indicates a low methodological quality. While this report shows that effects of the combination of PR and activity counseling significantly increased PA in COPD, high-quality research, ideally using large samples followed up for long periods, would shed light on the true effects of this comprehensive strategy.
Current research concentrates on the importance of lifestyle behavioral change interventions to improve PA.Citation54 Examples of strategies that implement behavioral change are pedometer-based activity counseling, motivational interviewing and well-constructed self-management interventions.Citation55,Citation56 Failure to report robust effects of these interventions may be linked with the wide heterogeneity of self-management interventions. An international expert group has recently published a consensus definition of the construct of self-management.Citation57 Future studies should establish programs based on such robust definitions to improve the likelihood of positive outcomes and ensure that interventions are replicable.
Recommendations to improve PA in COPD inspired by other chronic health conditions stressed the importance of developing “stealth interventions”.Citation58 These interventions aimed to indirectly improve PA by reducing sedentary behavior time and, as a result, improve light-intensity PA. Reductions in sedentary time are known to reduce cardiovascular risk in other groups.Citation59 This is highly relevant to people with COPD, many of whom have cardiovascular comorbidities. Of the studies included in this systematic review, only one studied the effects of PA-focused behavioral counseling using pedometer feedback and motivational interviewing added to 8 months of PR. This study demonstrated significantly reduced sedentary time when compared to PR alone at 3 months (0.96 [0.14–1.78]).Citation29 A recent RCT compared an intervention aimed to increase the time spent in high-intensity activities versus another focused on reducing sedentary time in older adults and suggested that targeting sedentary behavior is more effective in improving physical function.Citation60 Future trials should aim to assess the impact of PA interventions on sedentary time in COPD.
While only ET including Nordic walking,Citation17 community-basedCitation18 training and individualized exerciseCitation23 programs showed large effects on exercise tolerance in people with COPD, these effects do not appear to have a direct relationship with improvements in PA or other important outcomes such as HRQL or dyspnea. However, PA counseling showed small and insignificant effects on exercise tolerance levels while achieving significant improvements in HRQL.Citation34,Citation35,Citation38 These findings suggest that the integration between ET and activity counseling interventions may be imperative in achieving important effects on patient-focused outcomes in people with COPD.
Limitations of the systematic review
Although the overall quality score of the included trials was moderate, 12 included studies demonstrated low quality as assessed by PEDro scale. Low methodological quality was mainly due to lack of concealed allocation and blinding of assessors, which might affect the strength of evidence summarized in this report. A second limitation was the inability to pool all data in a meta-analysis and compute overall effects. The wide heterogeneity of included interventions, assessment time points and frequency of treatment hindered further analysis attempts. The results reported in this systematic review should be interpreted with caution due to these limitations. It is imperative that future trials in this field select high-quality designs and methodology with long-term follow-ups to report sustainability of true effects on PA in COPD.
Much work is under way to address inactivity in COPD. Recently published protocols describe large RCTs designed to test the effects of home-based PR using motivational interviewing,Citation61 patient-centered home and community-based PA coaching program,Citation62 an integrated pharmacological, ET and self-management program (the PHYSACTO trial)Citation63 and behavioral change self-management programCitation64 on activity levels using high-quality methodology. The outcomes of these refined interventions may provide more certainty regarding the most effective interventions to improve PA in COPD.
Conclusion
This review concluded that while ET alone can improve PA in COPD, greater improvements can be made with the addition of PA counseling. Introducing an activity counseling program in conjunction with PR might be essential to enhance PA in people with COPD. Perhaps this sophisticated model will also produce positive effects on other important COPD outcomes such as exercise capacity and HRQL.
Disclosure
The authors report no conflicts of interest in this work.
References
- PittaFTroostersTProbstVSSpruitMADecramerMGosselinkRPhysical activity and hospitalization for exacerbation of COPDChest2006129353654416537849
- WaschkiBKirstenAHolzOPhysical activity is the strongest predictor of all-cause mortality in patients with COPD: a prospective cohort studyChest2011140233134221273294
- VorrinkSNKortHSTroostersTLammersJ-WJLevel of daily physical activity in individuals with COPD compared with healthy controlsRespir Res20111211821194498
- PittaFTroostersTSpruitMAProbstVSDecramerMGosselinkRCharacteristics of physical activities in daily life in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2005171997297715665324
- EstebanCQuintanaJMAburtoMImpact of changes in physical activity on health-related quality of life among patients with COPDEur Respir J201036229230020075059
- MantoaniLCRubioNMcKinstryBMacNeeWRabinovichRAInterventions to modify physical activity in patients with COPD: a systematic reviewEur Respir J2016481698127103381
- HigginsJPGreenSCochrane Handbook for Systematic Reviews of Interventions Version 5.10LondonThe Cochrane Collaboration2011
- Global Strategy for the Diagnosis, Management and Prevention of COPDGlobal Initiative for Chronic Obstructive Lung Disease (Updated 2016) Available from: http://goldcopd.org/global-strategy-diagnosis-management-prevention-copd-2016/Accessed July 18, 2016
- MaherCGSherringtonCHerbertRDMoseleyAMElkinsMReliability of the PEDro Scale for Rating Quality of Randomized Controlled TrialsPhys Ther200383871372112882612
- PrinceSAAdamoKBHamelMEHardtJGorberSCTremblayMA comparison of direct versus self-report measures for assessing physical activity in adults: a systematic reviewInt J Behav Nutr Phys Act200855618990237
- O’HalloranPDBlackstockFShieldsNMotivational interviewing to increase physical activity in people with chronic health conditions: a systematic review and meta-analysisClin Rehabil201428121159117124942478
- DemeyerHBurtinCHornikxMThe minimal important difference in physical activity in patients with COPDPLoS One2016114e015458727124297
- BrozekJLGuyattGHSchunemannHJHow a well-grounded minimal important difference can enhance transparency of labelling claims and improve interpretation of a patient reported outcome measureHealth Qual Life Outcomes200646917005037
- VergeretJBrambillaCMounierLPortable oxygen therapy: use and benefit in hypoxaemic COPD patients on long-term oxygen therapyEur Respir J19892120252707399
- BerryMJRejeskiWJAdairNEEttingerWHJrZaccaroDJSevickMAA randomized, controlled trial comparing long-term and short-term exercise in patients with chronic obstructive pulmonary diseaseJ Cardiopulm Rehabil2003231606812576914
- BorgesRCCarvalhoCRImpact of resistance training in chronic obstructive pulmonary disease patients during periods of acute exacerbationArch Phys Med Rehabil20149591638164524879965
- BreyerM-KBreyer-KohansalRFunkG-CNordic walking improves daily physical activities in COPD: a randomised controlled trialRespir Res20101111220727209
- EffingTZielhuisGKerstjensHValkPPalenJCommunity based physiotherapeutic exercise in COPD self-management: a randomised controlled trialRespir Med2011105341842620951018
- FaulknerJWalshawECampbellJThe feasibility of recruiting patients with early COPD to a pilot trial assessing the effects of a physical activity interventionPrim Care Respir J201019212413020126968
- LarsonJLCoveyMKKapellaMCAlexCGMcAuleyESelf-efficacy enhancing intervention increases light physical activity in people with chronic obstructive pulmonary diseaseInt J Chron Obstruct Pulmon Dis201491081109025336939
- PomidoriLContoliMMandolesiGCogoAA simple method for home exercise training in patients with chronic obstructive pulmonary disease: one-year studyJ Cardiopulm Rehabil Prev2012321535722193935
- ProbstVSKovelisDHernandesNACamilloCACavalheriVPittaFEffects of 2 exercise training programs on physical activity in daily life in patients with COPDRespir Care201156111799180722035826
- SewellLSinghSJWilliamsJECollierRMorganMDCan individualized rehabilitation improve functional independence in elderly patients with COPD?Chest200512831194120016162706
- WilsonAMBrownePOliveSThe effects of maintenance schedules following pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomised controlled trialBMJ Open201553e005921
- AltenburgWATen HackenNHBossenbroekLKerstjensHAde GreefMHWempeJBShort- and long-term effects of a physical activity counselling programme in COPD: a randomized controlled trialRespir Med2015109111212125499548
- BerryMJRejeskiWJMillerMEA lifestyle activity intervention in patients with chronic obstructive pulmonary diseaseRespir Med2010104682983920347286
- BurtinCLangerDVan RemoortelHPhysical activity counselling during pulmonary rehabilitation in patients with COPD: a randomised controlled trialPLoS One20151012e014498926697853
- BurtinCLangerDvan RemoortelHCorrection: physical activity counselling during pulmonary rehabilitation in patients with COPD: a randomised controlled trialPLoS One2016112e014870526829484
- CruzJBrooksDMarquesAWalk2Bactive: a randomised controlled trial of a physical activity-focused behavioural intervention beyond pulmonary rehabilitation in chronic obstructive pulmonary diseaseChron Respir Dis2016131576626703921
- de BlokBMde GreefMHten HackenNHSprengerSRPostemaKWempeJBThe effects of a lifestyle physical activity counseling program with feedback of a pedometer during pulmonary rehabilitation in patients with COPD: a pilot studyPatient Educ Couns2006611485516455222
- HornikxMDemeyerHCamilloCAJanssensWTroostersTThe effects of a physical activity counseling program after an exacerbation in patients with chronic obstructive pulmonary disease: a randomized controlled pilot studyBMC Pulm Med20151513626530543
- HospesGBossenbroekLTen HackenNHTvan HengelPde GreefMHGEnhancement of daily physical activity increases physical fitness of outclinic COPD patients: results of an exercise counseling programPatient Educ Couns200975227427819036552
- KawagoshiAKiyokawaNSugawaraKEffects of low-intensity exercise and home-based pulmonary rehabilitation with pedometer feedback on physical activity in elderly patients with chronic obstructive pulmonary diseaseRespir Med2015109336437125682543
- MendozaLHortaPEspinozaJPedometers to enhance physical activity in COPD: a randomised controlled trialEur Respir J201545234735425261324
- MoyMLCollinsRJMartinezCHAn internet-mediated pedometer-based program improves health-related quality-of-life domains and daily step counts in COPD: a randomized controlled trialChest2015148112813725811395
- NguyenHQGillDPWolpinSSteeleBGBendittJOPilot study of a cell phone-based exercise persistence intervention post-rehabilitation for COPDInt J Chron Obstruct Pulmon Dis2009430131319750190
- SteeleBGBelzaBCainKCA randomized clinical trial of an activity and exercise adherence intervention in chronic pulmonary diseaseArch Phys Med Rehabil200889340441218295615
- TabakMBrusse-KeizerMvan der ValkPHermensHVollenbroek-HuttenMA telehealth program for self-management of COPD exacerbations and promotion of an active lifestyle: a pilot randomized controlled trialInt J Chron Obstruct Pulmon Dis2014993594425246781
- JonsdottirHAmundadottirORGudmundssonGEffectiveness of a partnership-based self-management programme for patients with mild and moderate chronic obstructive pulmonary disease: a pragmatic randomized controlled trialJ Adv Nurs201571112634264926193907
- NguyenHQDoneskyDReinkeLFInternet-based dyspnea self-management support for patients with chronic obstructive pulmonary diseaseJ Pain Symptom Manage2013461435523073395
- SchuzNWaltersJAECameron-TuckerHScottJWood-BakerRWaltersEHPatient anxiety and depression moderate the effects of increased self-management knowledge on physical activity: a secondary analysis of a randomised controlled trial on health-mentoring in COPDCOPD201512550250925774660
- WaltersJCameron-TuckerHWillsKEffects of telephone health mentoring in community-recruited chronic obstructive pulmonary disease on self-management capacity, quality of life and psychological morbidity: a randomised controlled trialBMJ201339e003097
- KestenSCasaburiRKukafkaDCooperCBImprovement in self-reported exercise participation with the combination of tiotropium and rehabilitative exercise training in COPD patientsInt J Chron Obstruct Pulmon Dis20083112713618488436
- TroostersTSciurbaFCDecramerMTiotropium in patients with moderate COPD naive to maintenance therapy: a randomised placebo-controlled trialNPJ Prim Care Respir Med2014241400324841833
- WatzHKrippnerFKirstenAMagnussenHVogelmeierCIndacaterol improves lung hyperinflation and physical activity in patients with moderate chronic obstructive pulmonary disease – a randomized, multicenter, double-blind, placebo-controlled studyBMC Pulm Med20141415825280934
- Dal NegroRWAquilaniRBertaccoSBoschiFMichelettoCTognellaSComprehensive effects of supplemented essential amino acids in patients with severe COPD and sarcopeniaMonaldi Arch Chest Dis2010731253320499791
- Dal NegroRWTestaAAquilaniREssential amino acid supplementation in patients with severe COPD: a step towards home rehabilitationMonaldi Arch Chest Dis2012772677523193843
- GorisAHCVermeerenMAPWoutersEFMScholsAWesterterpKREnergy balance in depleted ambulatory patients with chronic obstructive pulmonary disease: the effect of physical activity and oral nutritional supplementationBr J Nutr200389572572912720592
- CasaburiRPJHechtATiepBInfluence of lightweight ambulatory oxygen on oxygen use and activity patterns of COPD patients receiving long-term oxygen therapyCOPD20129131122292592
- DuivermanMLWempeJBBladderGNocturnal non-invasive ventilation in addition to rehabilitation in hypercapnic patients with COPDThorax200863121052105718710905
- SandlandCJMorganMDSinghSJPatterns of domestic activity and ambulatory oxygen usage in COPDChest2008134475376018625674
- PleguezuelosEPerezMEGuiraoLImproving physical activity in patients with COPD with urban walking circuitsRespir Med2013107121948195623890958
- KruisALBolandMRAssendelftWJEffectiveness of integrated disease management for primary care chronic obstructive pulmonary disease patients: results of cluster randomised trialBMJ2014349g539225209620
- SinghSOne step at a time. lifestyle physical activity interventionsAnn Am Thorac Soc201613558658727144787
- CavalheriVStrakerLGucciardiDFGardinerPAHillKChanging physical activity and sedentary behaviour in people with COPDRespirology201621341942626560834
- LeidyNKKimelMAjagbeLKimKHamiltonABeckerKDesigning trials of behavioral interventions to increase physical activity in patients with COPD: insights from the chronic disease literatureRespir Med2014108347248124315467
- EffingTWVercoulenJHBourbeauJDefinition of a COPD self-management intervention: International Expert Group consensusEur Respir J2016481465427076595
- HillKGardinerPACavalheriVJenkinsSCHealyGNPhysical activity and sedentary behaviour: applying lessons to chronic obstructive pulmonary diseaseIntern Med J201545547444825164319
- WilmotEGEdwardsonCLAchanaFASedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysisDiabetologia201255112895290522890825
- BaroneGibbs BBrachJSByardTReducing sedentary behavior versus increasing moderate-to-vigorous intensity physical activity in older adults: a 12-week randomized, clinical trialJ Aging Health Epub201633
- HollandAEMahalAHillCJBenefits and costs of home-based pulmonary rehabilitation in chronic obstructive pulmonary disease – a multi-centre randomised controlled equivalence trialBMC Pulm Med2013135724011178
- NguyenHQBaileyAColemanKJPatient-centered physical activity coaching in COPD (Walk On!): a study protocol for a pragmatic randomized controlled trialContemp Clin Trials201646182926597414
- TroostersTBourbeauJMaltaisFEnhancing exercise tolerance and physical activity in COPD with combined pharmacological and non-pharmacological interventions: PHYSACTO randomised, placebo-controlled study designBMJ Open201664e010106
- BourbeauJLavoieKLSedenoMBehaviour-change intervention in a multicentre, randomised, placebo-controlled COPD study: methodological considerations and implementationBMJ201664e010109