Abstract
Background
The aim of the study was to assess the relationship between computed tomography (CT) densitometry and routine clinical markers in patients with chronic obstructive pulmonary disease (COPD) and alpha-1 anti-trypsin deficiency (AATD).
Methods
Multiple databases were searched using a combination of pertinent terms and those articles relating quantitatively measured CT densitometry to clinical outcomes. Studies that used visual scoring only were excluded, as were those measured in expiration only. A thorough review of abstracts and full manuscripts was conducted by 2 reviewers; data extraction and assessment of bias was conducted by 1 reviewer and the 4 reviewers independently assessed for quality. Pooled correlation coefficients were calculated, and heterogeneity was explored.
Results
A total of 112 studies were identified, 82 being suitable for meta-analysis. The most commonly used density threshold was −950 HU, and a significant association between CT density and all included clinical parameters was demonstrated. There was marked heterogeneity between studies secondary to large variety of disease severity within commonly included cohorts and differences in CT acquisition parameters.
Conclusion
CT density shows a good relationship to clinically relevant parameters; however, study heterogeneity and lack of longitudinal data mean that it is difficult to compare studies or derive a minimal clinically important difference. We recommend that international consensus is reached to standardize CT conduct and analysis in future COPD and AATD studies.
Plain language summary
Computed tomography (CT) produces a digital image that is reconstructed into the recognizable picture format. CT densitometry describes the method that uses using this information to accurately quantify the severity of emphysema, and this has been validated pathologically and clinically. However, CT densitometry is yet to be standardized and its clinical utility remains unclear. This systematic review has highlighted the vast heterogeneity that exists between studies using CT density, and despite the strong relationship to clinically relevant parameters, international consensus is still required to standardize CT conduct.
Introduction
The heterogeneity of chronic obstructive pulmonary disease (COPD) and alpha-1 anti-trypsin deficiency (AATD) is well recognized, as is the need for more descriptive biomarkers beyond lung function.Citation1 Computed tomography (CT) has been used for many years to visually diagnose emphysema, providing the most direct assessment of its presence and distribution.Citation2 Software programs have since been developed, which can objectively measure the severity of emphysema.Citation3 Quantitative CT, and in particular CT densitometry, is the method of quantifying emphysema using such software; its ability to assess emphysema has been validated clinically and pathologically.Citation4–Citation6 However, CT densitometry is yet to be standardized, with numerous factors impacting on the measurement of density and affecting results.Citation7 Changes seen on CT predate those seen on spirometry, with pathological studies demonstrating that up to one-third of the lung tissues is destroyed in emphysema before spirometry becomes abnormal. This suggests that CT densitometry may be a very important technique for detection of early disease, an area which is of increasing clinical interest.Citation8 CT densitometry was the primary outcome measure for registration level randomized clinical trials (RCTs) of augmentation therapy in AATD, where signals have been seen for this measure, and only trends in the same direction for other clinical outcomes.Citation9 More recently large cross-sectional studies in COPD have been established (eg, COPDGene), which have collected data from quantitative measures on CT as well as extensive physiology.Citation10
Understanding the implications of density data is complex for both clinicians and regulatory agencies and no systematic reviews of its utility have been undertaken. The purpose of our study was to assess the validity of CT densitometry as a measure of severity and progression of lung disease in emphysema specifically seeking relationship to lung function, mortality, hospital admissions and quality of life (QOL).
Methods
This review is registered with Prospero (CRD42015024183). All papers concerning patients with clinically or spirometrically defined COPD that compared CT densitometry data with FEV1, gas transfer (diffusing capacity of the lungs for carbon monoxide [DLCO] or transfer factor divided by the alveolar volume [KCO]) and QOL, in the same study population were included. In addition, any study that described longitudinal density change, irrespective of whether there was a direct relationship to one of our pre-specified outcomes, was included. Studies in which COPD was secondary to AATD were included.
Population
The following databases were searched with no date or language restrictions: MEDLINE (Ovid), MEDLINE In Process (Ovid), EMBASE (Ovid), Cochrane Library (Wiley) Cochrane Central Register of Controlled Trials (CENTRAL), CMR, CDSR, HTA, NHS EED and DARE. In addition, Conference Proceedings Citation Index via Web of Science and British Library’s ZETOC was searched for conference proceedings and abstracts, and ClinicalTrials.gov and WHO International Clinical Trials Registry Platform were searched for ongoing trials. Search terms for COPD and AATD were combined with all search terms for CT or CT densitometry, and lung function (see Supplementary materials for full search terms).
Study selection
Titles and abstracts of search yield were screened for relevance by 2 reviewers independently. Disagreements were resolved by discussion, where required involving a third reviewer. Relevant articles were obtained and assessed against the full selection criteria in a similar manner (see Supplementary materials for full inclusion and exclusion criteria). Studies that used visual scoring only were excluded, as were those measured in expiration only.
Data extraction
Data were extracted using the Cochrane model, and included general study information, specifics of CT acquisition (ie, reconstruction algorithm, software and slice thickness), percentage low attenuation area (%LAA), whether the scan was taken in full inspiration, use of bronchodilator during spirometry and a CT phantom for quality assurance.Citation11 This process was performed by 1 reviewer (DC) and checked by the remaining authors.
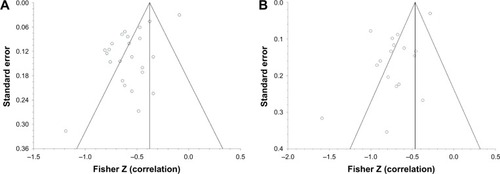
Risk of bias
Risk of bias was assessed by one reviewer (DC) and independently by AMT, MR, MK, and EL using a mixture of two recognized bias tools (Table S1). The AHRQ was used in order to accurately examine the large amount of cross sectional studies included, and QUADAS 2 where CT density is being considered as a diagnostic tool.Citation12,Citation13 Publication bias was assessed using funnel plots and Begg-Mazumdar/Egger tests, and efforts were made to reduce publication bias by using no date or language limits.
Data synthesis
Baseline characteristics are presented as mean (standard deviation) or median (interquartile range). Studies where density was taken from a single slice, where there was division into arbitrary emphysematous thresholds or that quoted mean lung density only were excluded. Studies that compared CT density with one of our chosen clinical parameters using Pearson’s correlation coefficient were meta-analyzed to estimate the Schmidt-Hunter (SH) weighted mean correlation coefficient. As SH is a random effects model, it is suitable for heterogeneous populations, with weighted means to accurately account for the variance.Citation14 I2 and chi-square analyses were performed to assess study heterogeneity. All analyses were performed using StatsDirect, and where meta-analysis was not possible, a narrative synthesis is provided.
Results
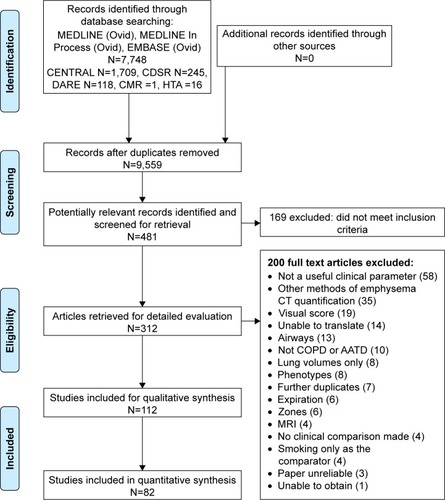
The PRISMA flow diagram () demonstrates that 112 papers were included in the overall narrative, and 82 papers could be combined in a quantitative meta-analysis. A small number of papers reported lobar densities, which were analyzed separately (Table S2). Characteristics of all included papers can be found in Table S3.
Figure 1 PRISMA flow diagram.
Cross-sectional studies of CT density
Pulmonary function tests
summarizes the baseline characteristics of studies and patients included in meta-analyses. %LAA at −950 HU was the most commonly used emphysematous threshold, with 55 individual studies reporting the association between −950 and clinical parameters, of which 23 were from larger cohort studies (eg, COPDGene, KOLD).Citation10,Citation14
Table 1 Summary of all studies included in meta-analyses
Spirometry
FEV1
A total of 36 studies compared forced expiratory volume in 1 second (FEV1) percent predicted to CT density. The forest plot in demonstrates the correlation between FEV1 percent predicted with CT density at −950 HU, and the variation between the included studies. These data are summarized in , which shows meta-analyses of the other CT parameters against FEV1 (L) or FEV1 percent predicted. The level of heterogeneity remained high in all sub-group analyses except for 900 HU and FEV1 percent predicted, which contained the smallest number of studies and thus could be less reliable.
Table 2 Summary of meta-analyses performed on all studies using Pearson’s correlation coefficient to compare FEV1 and FEV1 percent predicted with CT density
Figure 2 Forest plot of all studies included in the meta-analysis that correlated FEV1 percent predicted with −950 HU.
Abbreviation: FEV1, forced expiratory volume in 1 second.
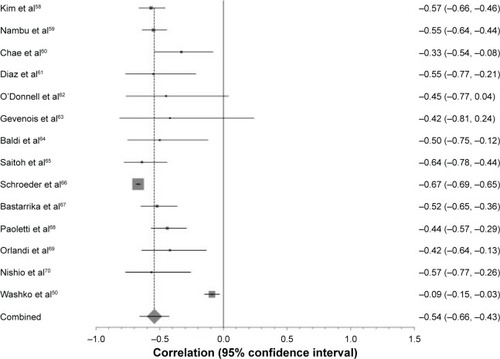
Further investigation into the cause of heterogeneity revealed major differences in the choice and combination of reconstruction algorithm, slice thickness and software program used by included studies. When meta-analysis was restricted to those studies using the same CT acquisition parameters, the forest plot became more uniform and heterogeneity reduced ().
Figure 3 The effect of CT algorithm on heterogeneity of results with respect to −950 HU and FEV1 percent predicted.
Abbreviations: CT, computed tomography; FEV1, forced expiratory volume in 1 second; SH, Schmidt-Hunter.
Seven studies performed multivariate linear regression between FEV1 and CT density (). However, for each density variable, all studies were adjusted for different variables and therefore an accurate meta-analysis could not be performed.
Table 3 Summary of studies that performed multivariate linear regression analyses to examine the relationship between FEV1 and CT density
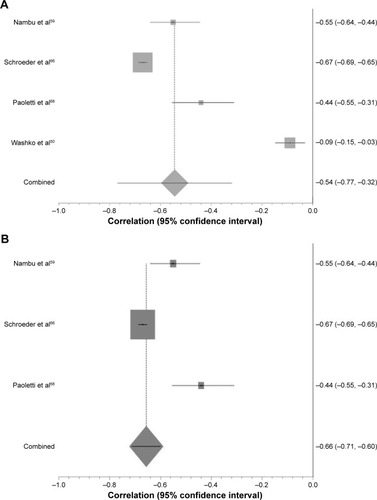
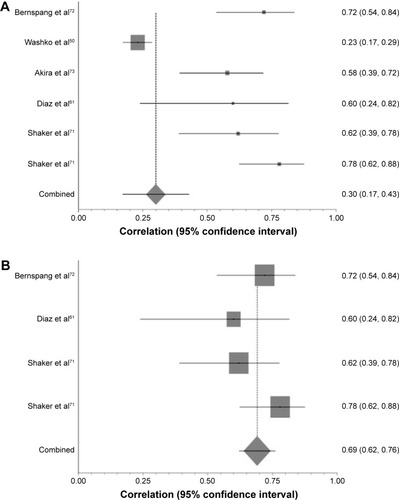
FEV1/forced vital capacity
Akin to FEV1, there was a significant correlation between each density variable and FEV1/forced vital capacity (p<0.0007; ). Again, large visual and statistical heterogeneity was improved by restricting to studies using the same CT parameters ().
Table 4 Summary of studies comparing FEV1/FVC with CT density, divided up in to the most commonly reported thresholds
Figure 4 The effect of CT algorithm on heterogeneity of results with respect to PD15 and FEV1/FVC.
Abbreviations: CT, computed tomography; PD15, 15th percentile point; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; SH, Schmidt-Hunter.
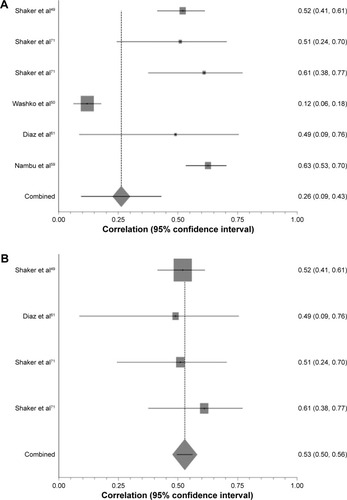
Gas transfer
A total of 23 studies compared DLCO percent predicted to CT density. The pooled correlation coefficients were universally significant across each of the density values, albeit slightly weaker than for FEV1 percent predicted and CT density (). The same pattern was seen regarding heterogeneity of results, with I2 dropping from 91.5% to 0 once CT algorithm was taken into account ().
Table 5 Studies subdivided into density parameter used, which compares gas transfer to CT measured density
Figure 5 The effect of CT algorithm on heterogeneity of results with respect to PD15 and DLCO percent predicted.
Abbreviations: CT, computed tomography; PD15, 15th percentile point; DLCO, diffusing capacity of the lungs for carbon monoxide; SH, Schmidt-Hunter.
Quality of life, symptom and composite scores
St Georges Respiratory Questionnaire (SGRQ) was the most frequently reported measure of QOL compared with CT density. A total of 2 out of 5 studies using correlation coefficients showed no relationship between the two measures, while the other 3 showed a strong association (p<0.003) (). There was variability in the density threshold and patient groups used (eg, cancer screening populations or those being considered for lung volume reduction surgery), thus precluding meta-analysis. Nevertheless studies that performed multivariate analyses consistently showed a significant association between density and SGRQ.
Table 6 Summary of studies that correlated CT density with SGRQ
Studies of BMI, airflow obstruction, dyspnea and exercise capacity and Medical Research Council (MRC) versus CT density used different density thresholds and statistical techniques but again showed strong relationships between density and the score in question in multivariate analyses ().
Table 7 Summary of studies that compare BODE and MRC with CT density, subdivided into univariate or multivariate models used
Longitudinal studies of CT density
Mortality
A total of 6 papers reported the relationship between CT density and mortality, 3 of which provided a hazard ratio for all-cause mortality () generated by multi-variable logistic regression. However, it was inappropriate to combine them statistically due to differing emphysematous thresholds and confounding variables included in their models. Emphysema as defined by CT density remained a significant independent predictor for mortality throughout.
Table 8 Studies reporting an all-cause mortality HR for emphysema as defined by CT density
Exacerbations
A total of 4 studies investigated low CT density as a risk factor for COPD exacerbations using multiple regression analyses in order to independently attribute exacerbations to density loss (). Due to different statistical methods, and the variables adjusted for, a statistical meta-analysis could not be performed. All but 1 study showed a significant relationship between CT density and exacerbations; Yoo et al found that the ability for emphysema index to predict exacerbations did not remain significant when numerous variables such as age, SGRQ and Charlson Index score were included in multiple regression analysis.Citation36 Cheng et al performed a multivariate ordinal logistic regression to demonstrate that %LAA >7.5 was associated with worse performance status and MRC grade if they presented to Accident and Emergency with an infective exacerbation of COPD.Citation37
Table 9 Summary of papers describing the association between CT density and exacerbations, subdivided into the risk of exacerbations from a low density score, and the impact exacerbations have on CT density decline
Interventional studies reporting CT density
AAT augmentation therapy
A total of 3 RCTs used CT density as an outcome measure for augmentation therapy in AATD patients;Citation9,Citation41,Citation42 change in CT density was the primary outcome in 2 studiesCitation41,Citation42 and secondary outcome in the earliest work.Citation9 A fourth paper was not included in the quantitative synthesis as it simply explored statistical approaches in data from the EXACTLE trial.Citation43 In all papers, CT density was log transformed and volume adjusted (see Table S3 for CT acquisition parameters), study duration was 2–3 years and the rate of density decline was measured in g/l−1 per year. A recent meta-analysis of these data has been reported separately, which demonstrates slower density decline in those receiving augmentation therapy than those receiving placebo (p=0.002).Citation44 The 3 papers analyzed also report overall low to moderate correlation coefficients between CT density and FEV1, KCO and exercise tolerance (0.31, 0.47 and −0.21 respectively).
All-trans retinoic acid
All-trans retinoic acid was shown to promote alveolar repair in animal models and subsequently 2 studies examined its effect in AATD as measured by CT density. However, neither showed any significant benefit on density decline nor did either comment on the observed relationship between CT density and other clinical parameters.Citation45,Citation46
Inhaled long-acting beta agonist/inhaled corticosteroid
A total of 2 studies from South Korea and the KOLD study collected longitudinal data on spirometric change over 3 months with inhaled corticosteroid/long-acting beta agonist treatment and demonstrated a significant correlation between FEV1 and baseline CT density using −950 HU as the emphysematous threshold.Citation47,Citation48 Shaker et al performed annual CT densitometry in a RCT conducted in patients with COPD, which demonstrated significantly slower decline in emphysema (using −910 HU; p=0.02) in those randomized to budesonide compared to placebo.Citation49
Standardizing studies for equal CT variables
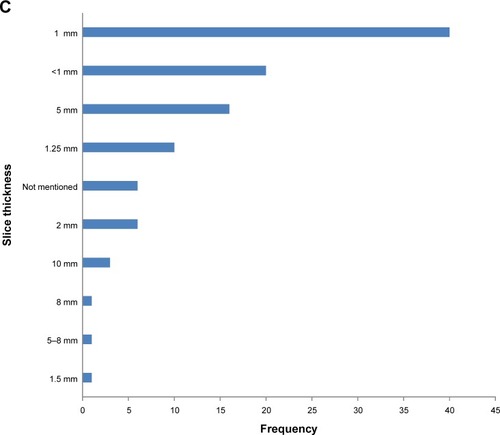
Since there were clear differences in the meta-analyses regarding the relationship between CT density and outcome when stratified by CT algorithm/statistical methods, we felt it was important to summarize the wide range of methods used in included studies ().
Figure 6 (A) Bar chart to demonstrate variety of software programs used in all studies. (B) Bar chart to demonstrate the variety of reconstruction algorithms reported. (C) Bar chart to demonstrate variety of slice thicknesses reported in all studies.
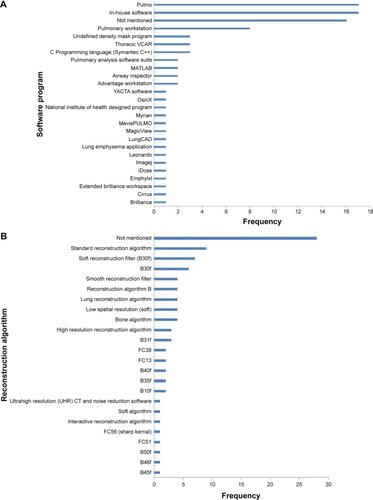
Pulmo was the most frequently used software program (used in EXACTLE and RAPID trials), followed by Pulmonary Workstation (used in COPDGene studies).
Most commonly, the reconstruction algorithm used was not mentioned, followed by “standard reconstruction algorithm”. The reconstruction algorithms are scanner specific, not always clear and therefore would be difficult to reproduce. The most frequently used slice thicknesses were 1 mm (N=40) and sub-millimeter (N=20).
Bias assessment
Risk of bias is summarized in (see Table S4 for the full risk of bias assessment). Bias introduced during patient selection was relatively low, with the patient source, selection and inclusion/exclusion criteria well described. The highest level of uncertainty that could have led to bias was within index and reference test (ie, CT and lung function). There was variability in the detail that authors gave with regards to CT acquisition, the use of a phantom and whether or not a bronchodilator was applied before spirometry was performed. Missing data and confounding variables were often not accounted for, but the statistical tests applied were considered appropriate.
Table 10 Summary of the risk of bias assessment
Publication bias
The funnel plots for −959 HU versus FEV1 percent predicted and DLCO percent predicted (analyses containing the most studies) show a significant degree of publication bias (). On further inspection of both plots, there is one study with a low standard error and large population (Washko et al) that causes the funnel plots to shift to the right.Citation50 Without this study, it stands to reason that the funnel would be more inclusive of the studies within the plot and could imply less publication bias. The risk of bias by two independent reviewers of this study was concluded as moderate, based on no mention of the time interval between the CT and pulmonary function tests. There was also no explanation of how confounding variables were assessed or controlled for, or how missing data were handled.
Discussion
The purpose of this review was to summarize all the currently available literature regarding CT density and its association with commonly used clinical parameters to develop a clear understanding of the utility of CT density measures for current and future clinical practice. This is particularly important as CT density has been used as a primary outcome in registration level clinical trials in AATD, but doubt has been cast by some authors as to its relevance as a surrogate outcome.Citation41,Citation51 Our data showed that association between CT density and other clinical parameters deemed suitable as outcomes for airways disease trials (eg, FEV1, SGRQ) were consistently significant, and furthermore there was a clear and consistent relationship to mortality. This suggests that CT density is an appropriate surrogate outcome measure in studies of emphysema, like those conducted in AATD. However, publication and other biases as well as study heterogeneity make it more difficult to draw conclusions regarding the precise strength of each relationship.
Over half of the included studies were from larger cohort studies and subsequent retrospective/cross-sectional analysis. The nature of these cohorts introduces heterogeneity in the types of patients recruited, ie, lung cancer screening studies (NELSON),Citation52 alpha one cohorts,Citation53 COPD (eg, COPDGene, KOLDCitation15,Citation54) and end-stage disease (eg, NETT).Citation55 The consistency of direction of the relationship between density and lung function across diverse patient groups is reassuring and suggests that density could be a valid surrogate outcome across the spectrum of disease severity. However, the wide range of values seen for the CT versus FEV1 correlations meant that defining the exact level of CT density that relates to, for instance, the minimal clinically important difference (MCID) for FEV1 was difficult.
The chosen CT parameter (eg, −950 HU, 15th percentile point [PD15]), software program, reconstruction algorithm and slice thickness varied grossly throughout. This level of heterogeneity was far greater than we had anticipated and made combination of all data via meta-analysis potentially less valid. The broad range of published correlation coefficients seen between −950 HU and FEV1% () (from −0.1 to −0.8) demonstrated this well, and when only studies with the same CT acquisition variables were analyzed, the level of heterogeneity fell dramatically. This implies that future CT density studies should have a standardized approach. Despite PD15 being established as the most reliable and sensitive measure, we have seen many studies that do not use this parameter, and would encourage authors to report this value so that data can be combined and our knowledge can grow.
The most appropriate CT algorithm would be a soft reconstruction algorithm (eg, B30f), slice thickness 2.5–5 mm and a software program that yields reliable and repeatable results. The algorithm and slice thickness are optimal due to minimal technical noise. Sharper algorithms and thinner slices have been demonstrated to overestimate the amount of emphysema.Citation56 Many publications used in-house software that, while producing useful data, may not be comparable to one another.Citation57 For example, Pulmo and Pulmonary Workstation are two of the most commonly used software programs (used in RAPID trial and COPDGene cohort studies, respectively), and if identical and repeatable results can be produced by both programs then cohort studies using them can then be combined and meta-analyzed to increase power. This requires direct comparison of the software on the same scans; a similar approach would be needed for slice thickness, reconstruction and so on. There are limited studies of this nature to date.Citation7
There was a paucity of longitudinal CT density data in the included studies, which precluded conclusions about the sensitivity and specificity of CT density change over time with respect to our chosen outcomes. This means that we are unable to assess the relationship between CT density and clinical parameters over time for which there was a known MCID (eg, FEV of 100 mL), and therefore a proposal of a MCID for CT density was not possible. This would be of particular use for registration level trials, which have used or intend to use this as their primary outcome.
The key strengths of this review are that it was very broad; therefore, all potential papers were captured. Rigorous checking of data extracted from the large number of included studies was done, and the statistical analyses were conducted under supervision of an experienced statistician. Limitations were largely centered on the quality and heterogeneity of the included studies. There are other CT scanner variables that we did not examine in more detail as their impact was considered less relevant, eg, scanner type and radiation dose. There were 14 papers in languages to which we did not have access to a translator such as Japanese and Korean.
Conclusion
This evidence synthesis has demonstrated that CT density relates significantly to all commonly used clinical parameters. However, the large amount of heterogeneity and lack of longitudinal data mean that how sensitive and specific CT density is to change relating to time or interventions is not clear. We recommend that international consensus be reached to standardize CT conduct and analysis in future emphysema studies.
Author contributions
AMT designed the review question; DC was the first reviewer, responsible for all data gathering, extraction and analysis. AMT was the primary independent reviewer, with bias and quality of data extraction reviewed by MR, MK and EVL. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
The authors would like to thank Peter Nightingale, the statistician responsible for reviewing the meta-analyses, and Sue Bayliss for her assistance with search terms. This study was funded by a non-commercial grant from Grifols Biotherapeutics.
Disclosure
AMT has received honoraria, research grants or educational grants from or acted as an investigator in trials for Boehringer Ingelheim, Novartis, Chiesi, GSK, AstraZeneca and Pfizer. The authors report no other conflicts of interest in this work.
References
- TurnerAMTamasiLSchleichFClinically relevant subgroups in COPD and asthmaEur Respir Rev20152413628329826028640
- HrubanRHMezianeMAZerhouniEAHigh resolution computed tomography of inflation-fixed lungs. Pathologic-radiologic correlation of centrilobular emphysemaAm Rev Respir Dis198713649359403310774
- ParrDGStoelBCStolkJStockleyRAPattern of emphysema distribution in alpha1-antitrypsin deficiency influences lung function impairmentAm J Respir Crit Care Med2004170111172117815306534
- MüllerNLStaplesCAMillerRRAbboudRT“Density Mask”. An objective method to quantitate emphysema using computed-tomographyChest19889447827873168574
- DiazAAValimCYamashiroTAirway count and emphysema assessed by chest CT imaging predicts clinical outcome in smokersChest2010138488088720558554
- CamiciottoliGBartolucciMMaluccioNMSpirometrically gated high-resolution CT findings in COPD: lung attenuation vs lung function and dyspnea severityChest2006129355856416537852
- GieradaDSBierhalsAJChoongCKEffects of CT section thickness and reconstruction kernel on emphysema quantification relationship to the magnitude of the CT emphysema indexAcad Radiol201017214615619931472
- UppaluriRMitsaTSonkaMHoffmanEAMcLennanGQuantification of pulmonary emphysema from lung computed tomography imagesAm J Respir Crit Care Med199715612482549230756
- DirksenADijkmanJHMadsenFA randomized clinical trial of alpha(1)-antitrypsin augmentation therapyAm J Respir Crit Care Med19991605 Pt 11468147210556107
- CrapoJSECOPDGene. COPD genetic epidemiology Available from: www.copdgene.org2014Accessed January 08, 2018
- HigginsJPTGreenSCochrane Handbook for Systematic Reviews of Interventions Version 5.1.0The Cochrane Collaboration2011
- WhitingPFRutjesAWWestwoodMEQUADAS-2 GroupQUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studiesAnn Intern Med2011155852953622007046
- ZengXZhangYKwongJSThe methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic reviewJ Evid Based Med20158121025594108
- FieldAPIs the meta-analysis of correlation coefficients accurate when population correlations vary?Psychol Methods200510444446716392999
- ParkTSLeeJSSeoJBKOLD Study GroupStudy design and outcomes of Korean Obstructive Lung Disease (KOLD) cohort studyTuberc Respir Dis (Seoul)201476416917424851130
- KimSSSeoJBLeeHYChronic obstructive pulmonary disease: lobe-based visual assessment of volumetric CT by using standard images-comparison with quantitative CT and pulmonary function test in the COPDGene studyRadiology2013266262663523220894
- Mohamed HoeseinFAde JongPALammersJWContribution of CT quantified emphysema, air trapping and airway wall thickness on pulmonary function in male smokers with and without COPDCOPD201411550350925093696
- HongYChaeEJSeoJBContributors of the severity of airflow limitation in COPD patientsTuberc Respir Dis2012721814
- AzizZAWellsAUDesaiSRFunctional impairment in emphysema: contribution of airway abnormalities and distribution of parenchymal diseaseAJR Am J Roentgenol200518561509151516304005
- Mohamed HoeseinFAvan RikxoortEvan GinnekenBComputed tomography-quantified emphysema distribution is associated with lung function declineEur Respir J201240484485022323577
- Mohamed HoeseinFAde HoopBZanenPCT-quantified emphysema in male heavy smokers: association with lung function declineThorax201166978278721474499
- Mohamed HoeseinFAde JongPALammersJWAirway wall thickness associated with forced expiratory volume in 1 second decline and development of airflow limitationEur Respir J201545364465125614166
- StolkJNgWHBakkerMECorrelation between annual change in health status and computer tomography derived lung density in subjects with alpha1-antitrypsin deficiencyThorax200358121027103014645966
- DowsonLJGuestPJHillSLHolderRLStockleyRAHigh-resolution computed tomography scanning in alpha1-antitrypsin deficiency: relationship to lung function and health statusEur Respir J20011761097110411491150
- BarjaktarevicISpringmeyerSGonzalezXSirokmanWCoxsonHOCooperCBDiffusing capacity for carbon monoxide correlates best with tissue volume from quantitative CT scanning analysisChest201514761485149325500912
- MotohashiNKimuraKIshiiTEmphysema on imaging is associated with quality of life in elderly patients with chronic obstructive pulmonary diseaseGeriatr Gerontol Int2010101172420102378
- de TorresJPBastarrikaGZagacetaJEmphysema presence, severity, and distribution has little impact on the clinical presentation of a cohort of patients with mild to moderate COPDChest20111391364220705800
- MartinezCHChenYHWestgatePMCOPDGene InvestigatorsRelationship between quantitative CT metrics and health status and BODE in chronic obstructive pulmonary diseaseThorax201267539940622514236
- MartinezFJCurtisJLSciurbaFNational Emphysema Treatment Trial Research GroupSex differences in severe pulmonary emphysemaAm J Respir Crit Care Med2007176324325217431226
- GietemaHAEdwardsLDCoxsonHOBakkePSECLIPSE InvestigatorsImpact of emphysema and airway wall thickness on quality of life in smoking-related COPDRespir Med201310781201120923711580
- CamiciottoliGBigazziFBartolucciMBODE-index, modified BODE-index and ADO-score in chronic obstructive pulmonary disease: relationship with COPD phenotypes and CT lung density changesCOPD20129329730422432964
- HarunaAOgaTMuroSRelationship between peripheral airway function and patient-reported outcomes in COPD: a cross-sectional studyBMC Pulm Med2010101020205936
- HarunaAMuroSNakanoYCT scan findings of emphysema predict mortality in COPDChest2010138363564020382712
- MartinezFJFosterGCurtisJLNETT Research GroupPredictors of mortality in patients with emphysema and severe airflow obstructionAm J Respir Crit Care Med2006173121326133416543549
- DawkinsPWoodANightingalePStockleyRMortality in alpha-1-antitrypsin deficiency in the United KingdomRespir Med2009103101540154719443188
- YooJWHongYSeoJBComparison of clinico-physiologic and CT imaging risk factors for COPD exacerbationJ Korean Med Sci201126121606161222147998
- ChengTWanHYChengQJObvious emphysema on computed tomography during an acute exacerbation of chronic obstructive pulmonary disease predicts a poor prognosisIntern Med J201545551752625684314
- VijayasarathaKStockleyRARelationship between frequency, length, and treatment outcome of exacerbations to baseline lung function and lung density in alpha-1 antitrypsin-deficient COPDInt J Chron Obstruct Pulmon Dis2012778979623226015
- McAllisterDAAhmedFSAustinJHEmphysema predicts hospitalisation and incident airflow obstruction among older smokers: a prospective cohort studyPLoS One201494e9322124699215
- HanMKKazerooniEALynchDACOPDGene InvestigatorsChronic obstructive pulmonary disease exacerbations in the COPDGene study: associated radiologic phenotypesRadiology2011261127428221788524
- ChapmanKRBurdonJGPiitulainenERAPID Trial Study GroupIntravenous augmentation treatment and lung density in severe α1 antitrypsin deficiency (RAPID): a randomised, double-blind, placebo-controlled trialLancet2015386999136036826026936
- DirksenAPiitulainenEParrDGExploring the role of CT densitometry: a randomised study of augmentation therapy in alpha1-antitrypsin deficiencyEur Respir J20093361345135319196813
- ParrDGDirksenAPiitulainenEDengCWenckerMStockleyRAExploring the optimum approach to the use of CT densitometry in a randomised placebo-controlled study of augmentation therapy in alpha 1-antitrypsin deficiencyRespir Res2009107519678952
- EdgarRGPatelMBaylissSCrossleyDSapeyETurnerAMTreatment of lung disease in alpha-1 antitrypsin deficiency: a systematic reviewInt J Chron Obstruct Pulmon Dis2017121295130828496314
- RothMDConnettJED’ArmientoJMFORTE Study InvestigatorsFeasibility of retinoids for the treatment of emphysema studyChest200613051334134517099008
- StolkJCooperBGStoelBRetinoid treatment of Emphysema in patients on the Alpha-1 International Registry. The REPAIR study: study design, methodology and quality control of study assessmentsTher Adv Respir Dis20104631933220926506
- LeeJHLeeYKKimEKResponses to inhaled long-acting beta-agonist and corticosteroid according to COPD subtypeRespir Med2010104454254919926461
- LeeJSHuhJWChaeEJPredictors of pulmonary function response to treatment with salmeterol/fluticasone in patients with chronic obstructive pulmonary diseaseJ Korean Med Sci201126337938521394306
- ShakerSBDirksenAUlrikCSThe effect of inhaled corticosteroids on the development of emphysema in smokers assessed by annual computed tomographyCOPD20096210411119378223
- WashkoGRCrinerGJMohsenifarZComputed tomographic-based quantification of emphysema and correlation to pulmonary function and mechanicsCOPD20085317718618568842
- GøtzschePCJohansenHKIntravenous alpha-1 antitrypsin augmentation therapy for treating patients with alpha-1 antitrypsin deficiency and lung diseaseCochrane Database Syst Rev20107CD00785120614465
- Ru ZhaoYXieXde KoningHJMaliWPVliegenthartROudkerkMNELSON lung cancer screening studyCancer Imaging201111Spec No AS79S8422185865
- ReganEAHokansonJEMurphyJRGenetic epidemiology of COPD (COPDGene) study designCOPD201071324320214461
- WiseRADrummondMBThe role of NETT in emphysema researchProc Am Thorac Soc20085438539218453344
- KemerinkGJKruizeHHLamersRJvan EngelshovenJMDensity resolution in quantitative computed tomography of foam and lungMed Phys19962310169717088946367
- KemerinkGJKruizeHHLamersRJvan EngelshovenJMDensity resolution in quantitative computed tomography of foam and lungMed Phys19962310169717088946367
- WielputzMOBardarovaDWeinheimerOVariation of densitometry on computed tomography in COPD – influence of different software toolsPLoS One2014911e11289825386874
- KimEYSeoJBLeeHJDetailed analysis of the density change on chest CT of COPD using non-rigid registration of inspiration/expiration CT scansEur Radiol201525254154925218764
- NambuAZachJSchroederJRelationships between diffusing capacity for carbon monoxide (DLCO), and quantitative computed tomography measurements and visual assessment for chronic obstructive pulmonary diseaseEur J Radiol201584598098525704753
- ChaeEJSeoJBSongJWSlope of emphysema index: an objective descriptor of regional heterogeneity of emphysema and an independent determinant of pulmonary functionAJR Am J Roentgenol20101943W248W25520173123
- DiazSCasselbrantIPiitulainenEValidity of apparent diffusion coefficient hyperpolarized 3He-MRI using MSCT and pulmonary function tests as referencesEur J Radiol200871225726318514455
- O’DonnellRAPeeblesCWardJARelationship between peripheral airway dysfunction, airway obstruction, and neutrophilic inflammation in COPDThorax2004591083784215454648
- GevenoisPADe VuystPSyMPulmonary emphysema: quantitative CT during expirationRadiology199619938258298638012
- BaldiSMiniatiMBellinaCRRelationship between extent of pulmonary emphysema by high-resolution computed tomography and lung elastic recoil in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2001164458558911520720
- SaitohTKobaHShijuboNTanakaHSugayaFLobar distribution of emphysema in computed tomographic densitometric analysisInvest Radiol200035423524310764092
- SchroederJDMcKenzieASZachJARelationships between airflow obstruction and quantitative CT measurements of emphysema, air trapping, and airways in subjects with and without chronic obstructive pulmonary diseaseAJR Am J Roentgenol20132013W460W47023971478
- BastarrikaGWisniveskyJPPueyoJCDiazLArraizaMVillanuevaALow-dose volumetric computed tomography for quantification of emphysema in asymptomatic smokers participating in an early lung cancer detection trial2009243206211
- PaolettiMCestelliLBigazziFCamiciottoliGPistolesiMChronic obstructive pulmonary disease: pulmonary function and CT lung attenuation do not show linear correlationRadiology2015276257157825848902
- OrlandiIMoroniCCamiciottoliGChronic obstructive pulmonary disease: thin-section CT measurement of airway wall thickness and lung attenuationRadiology2005234260461015671010
- NishioMMatsumotoSKoyamaHOhnoYSugimuraKAirflow limitation in chronic obstructive pulmonary disease: ratio and difference of percentage of low-attenuation lung regions in paired inspiratory/expiratory computed tomographyAcad Radiol201421101262126725086954
- ShakerSBMaltbaekNBrandPHaeussermannSDirksenAQuantitative computed tomography and aerosol morphometry in COPD and alpha1-antitrypsin deficiencyEur Respir J2005251233015640319
- BernspangEDiazSStoelBWollmerPSvegerTPiitulainenECT lung densitometry in young adults with alpha-1-antitrypsin deficiencyRespir Med20111051747920674322
- AkiraMToyokawaKInoueYAraiTQuantitative CT in chronic obstructive pulmonary disease: inspiratory and expiratory assessmentAJR Am J Roentgenol2009192126727219098209