Abstract
Airway mucus hypersecretion is one of the most important characteristics of chronic airway inflammatory diseases. Evaluating and managing airway mucus hypersecretion is of great importance for patients with chronic airway inflammatory diseases. This consensus statement describes the pathogenesis, clinical features, and the management of airway mucus hypersecretion in patients with chronic airway inflammatory diseases in the People’s Republic of China. The statement has been written particularly for respiratory researchers, pulmonary physicians, and patients.
Introduction
Airway mucus hypersecretion is an important pathophysiological and clinical manifestation of chronic obstructive pulmonary disease (COPD), bronchial asthma (asthma), bronchiectasis, pulmonary cystic fibrosis, and other chronic airway inflammatory diseases.Citation1 Recent studies have shown that inflammation and oxidative stress are involved in the pathogenesis of chronic airway inflammatory diseases and closely correlate with clinical outcomes and that they trigger excessive mucus production and secretion by glands and goblet cells. The American Thoracic Society, European Respiratory Society, and Chinese Thoracic Society of the Chinese Medical Association have officially recognized that airway mucus hypersecretion plays an important role in common respiratory diseases.Citation2–Citation4
Reducing the risk of mortality and other complications associated with airway mucus hypersecretion means exploring its pathogenesis in detail, as well as clarifying its relationship with chronic airway inflammatory diseases.Citation1–Citation4 To take stock of available evidence and to guide both clinical practice and research initiatives, the COPD Group and Asthma Group of the Chinese Thoracic Society of the Chinese Medical Association have developed this consensus statement about the state of knowledge and best clinical practices for managing airway mucus hypersecretion induced by chronic airway inflammatory disease.
Pathogenesis of airway mucus hypersecretion
Mucus is the normal secretory product of the lining of the epithelium, which contains secreted water, sugar, protein, lipids, minerals, and mucins. Mucins are a group of proteins and the most important components of mucus, and MUC5AC and MUC5B are the 2 main mucins in mucus; the former is the main gel-forming mucin from surface mucus or goblet cells, and the latter is a primary secretory polymeric protein from submucosal glands.Citation1,Citation2 Under normal conditions, mucus secreted into the airway protects the airway and moistens the air. Under many types of stress conditions, including smoking, infection, pathogenic factors, and oxidative stress, cells lining the airway secrete numerous prosecretory factors that lead to secretory cell hypertrophy and goblet cell hyperplasia in the airway, with concomitant overproduction of mucus.Citation1 COPD, asthma, and bronchiectasis involve airway mucus hypersecretion and ciliary dysfunction. In COPD, inflammatory responses induced by cigarette smoke and other stimulators, together with oxidative stress, injure airway epithelial cells and stimulate mucus hypersecretion. In bronchial asthma, oversecretion of mucin components MUC5AC and MUC5B in the airway, and damage to the epithelium, cause the exfoliation of ciliated cells, goblet cell hyperplasia, and submucosal gland hypertrophy, all of which ultimately lead to airway mucus hypersecretion.Citation5 In bronchiectasis, irreversible expansion of the bronchial lumen compromises mucus clearance and allows bacteria to colonize the airway. The release of toxins secreted by bacteria first causes the activation of pathogen-associated molecular patterns and danger-associated molecular patterns to increase inflammation; this inflammation in turn stimulates goblet cell hyperplasia and metaplasia, leading to airway mucus hypersecretion.Citation6–Citation9
Various types of stimulation, such as cigarette smoking, induce abundant production of reactive oxygen species and proteases, which activate epidermal growth factor receptor, Toll receptor, and other receptors, in turn triggering multiple signaling pathways such as MAPK, ERK, and NF-κB. These pathways induce goblet cell metaplasia and hyperplasia in the airway, leading to synthesis and secretion of excessive mucin and thus to airway mucus hypersecretion.Citation2–Citation4 In this way, inflammation, oxidative stress, protease imbalances, cholinergic nerve dysfunction, and other pathophysiological mechanisms can influence the risk of airway mucus hypersecretion. In addition to environmental stimulants, genetic susceptibility factors can also influence such risk.Citation10 For example, Chand et al reported that a genetic variant of p53 plays a role in determining chronic mucus hypersecretion.Citation11 Such mucus hypersecretion can affect the clinical manifestations of COPD, bronchial asthma, bronchiectasis, and other common respiratory diseases.
Airway mucus hypersecretion and chronic airway inflammatory disease
Airway mucus hypersecretion can obstruct the respiratory tract lumen, limit airflow, and accelerate decline in lung function.Citation12 At the same time, inflammatory responses compromise mucus clearance by cilia, remove alveolar surface active substances such as surfactants, and alter biophysical properties of mucus.Citation13 This can lead to recurrent airway infection, causing further airway obstruction and remodeling, thereby creating a vicious cycle. Current evidence supports the notion that chronic inflammation causes mucus hypersecretion, which then plays a role in chronic airway inflammatory diseases.
Airway mucus hypersecretion and COPD
COPD is a common disease, the main clinical feature of which is persistent, progressive airflow limitation that is associated with chronic abnormal inflammatory responses to harmful particles or gases in the respiratory tract and lungs.Citation14 COPD seriously affects patients’ ability to work and their quality of life, and it is associated with high mortality. Large epidemiological surveys in the People’s Republic of China indicate a COPD prevalence of ~8.2% in adults aged >40 years.Citation15
Airway mucus hypersecretion manifests clinically as chronic cough and expectoration. Individuals with such symptoms are nearly 3 times more likely to suffer COPD than healthy individuals, and these symptoms may be unrelated to smoking; indeed, paroxysmal cough is an independent risk factor for COPD.Citation16,Citation17 Patients with COPD have significantly more goblet cells in airway epithelium than controls, and they secrete significantly more mucoprotein;Citation18 nearly 50% of COPD patients have airway mucus hypersecretion.Citation19 Clogged airway by mucus leads to reduced airflow and then plays a role in the pathogenesis of COPD. COPD patients are at 3.5-fold greater risk of dying if they have airway mucus hypersecretion than if they do not.Citation20
In patients with airway mucus hypersecretion and COPD, accelerated decline in lung function is associated with a high rate of hospitalization and acute exacerbation of COPD. Patients with chronic cough and expectoration exhibit a significantly higher incidence of acute exacerbation, which is mostly induced by bacterial and viral infection.Citation21–Citation23 The motions involved in chronic cough and expectoration may accelerate dynamic lung hyperinflation, which may help explain why chronic cough and expectoration are independent risk factors for reduced exercise capacity in COPD patients.Citation24 In addition, among subjects with COPD, those with chronic mucus hypersecretion (chronic bronchitis phenotype) present worse quality of life symptoms and mental well-being than do those without chronic mucus hypersecretion.Citation25
The important role of airway mucus hypersecretion in COPD should be fully recognized.Citation26 Airway mucus hypersecretion, via chronic cough and expectoration, reduces airflow and exercise capacity and increases the risk of acute exacerbation, mortality, and poor prognosis in COPD patients.
Airway mucus hypersecretion and bronchial asthma
Bronchial asthma, often referred to simply as “asthma,” is a chronic airway inflammatory disease, the main clinical feature of which is reversible airflow limitation.Citation27 Those with asthma show obviously lower mucociliary clearance from airways than patients in controls.Citation28 Approximately 20%–40% of patients have increased sputum volume and symptoms of airway mucus hypersecretion, and their airway mucus is more viscous than that in patients with COPD; in addition, their airways are easily obstructed by colloidal mucus plugs.Citation29 Cough and expectoration are more obvious in moderate or severe asthma or uncontrollable asthma; these symptoms can serve as a phenotype and prognostic indicator.Citation30,Citation31 An autopsy study of 93 patients with fatal asthma found that nearly all had mucus-obstructed airways, leading investigators to conclude that asthma-related mortality, particularly among patients with severe asthma, may be due to airway mucus hypersecretion.Citation32,Citation33 The symptoms of asthma may be difficult to control because airway mucus hypersecretion facilitates bacterial colonization of airways, limits airflow, and compromises ventilation.
Airway mucus hypersecretion and bronchiectasis
Bronchiectasis is bronchial deformation and persistent bronchial expansion caused by the destruction of smooth muscles and elastic tissues on the bronchial wall due to chronic purulent inflammation and fibrosis of the bronchus and surrounding lung tissues.Citation34 Cough occurs in >90% of patients with bronchiectasis, and expectoration occurs as a complication in 75%–100% of patients with cough. Patients with bronchiectasis show reduced mucociliary activities in the airway and reduced expectoration ability, and the biophysical properties of their mucus are altered, eg, it is more viscous.Citation35 The long-term accumulation of mucus in the airway facilitates colonization by bacteria as well as recurrent cough and expectoration.Citation35 In this way, airway mucus hypersecretion is a fundamental pathophysiological and clinical feature of bronchiectasis. Linked with airway mucus hypersecretion, airway inflammation and damage occur in bronchiectasis patients, seriously affecting patients’ quality of life.Citation36
Airway mucus hypersecretion and pulmonary cystic fibrosis
Pulmonary cystic fibrosis is a congenital lung disease often associated with mutation in the cystic fibrosis transmembrane conductance regulator, responsible for producing sweat, digestive juices, and various mucus fluids.Citation37 Patients with pulmonary cystic fibrosis show severe airway mucus hypersecretion, and many suffer recurrent pulmonary infections, which can accelerate decline in the lung function. Patient sputum is characterized by obvious neutrophil infiltration, cellular DNA released from injured cells, and abundant Pseudomonas aeruginosa.Citation38 Patients also show substantial epithelial goblet cell metaplasia in the airway in contrast to healthy individuals, as well as significantly higher MUC5AC expression.Citation38 Airway mucus hypersecretion in patients with pulmonary cystic fibrosis is associated with persistent cough, expectoration, and dyspnea.
The preceding sections summarize the close relationship of airway mucus hypersecretion with incidence, progression, and prognosis of common chronic airway inflammatory diseases. Full recognition of the role of airway mucus hypersecretion in these diseases is important for guiding clinical treatment.
Evaluation of airway mucus hypersecretion
Airway mucus hypersecretion manifests mainly as chronic cough and expectoration, which are particularly obvious during stimulation, weather changes, and exacerbation of infection. The severity of cough and the volume and properties of sputum serve as an index of airway mucus hypersecretion, which can fluctuate during periods of stability or acute exacerbation of airway diseases. The cough and sputum assessment questionnaire (CASA-Q) designed by Crawford et al is one of the few tools available for assessing airway mucus hypersecretion.Citation39 The questionnaire contains 4 sections covering coughing, sputum, and their effects. Lower overall score indicates more severe airway mucus hypersecretion. CASA-Q score is closely related to the quality of life and clinical symptoms of COPD patients, and it is useful for monitoring recovery from acute COPD exacerbations.Citation39,Citation40 In addition, St George’s Respiratory Questionnaire and American Thoracic Society Questionnaire, important questionnaires that are used for many cohorts around the world and also contain questions for evaluation of cough and sputum, can also be used to evaluate airway mucus hypersecretion.Citation41,Citation42 All these questionnaires may be used to evaluate airway mucus hypersecretion and to define the questionnaire with best efficacy. No standardized methods exist for quantitating airway mucus hypersecretion in COPD patients, which requires invasive procedures and so is rarely performed in the clinic. Since cough and expectoration frequently occur in many respiratory diseases, future research should seek to clarify the differences in features of airway mucus hypersecretion caused by different diseases, in order to ensure accurate diagnosis and management.
Treatment of airway mucus hypersecretion
At present, chronic airway inflammatory diseases such as COPD and asthma are treated mainly using bronchodilators to open occluded airways or by using corticosteroid inhalation to control inflammation.Citation2–Citation4 Given the important clinical significance of airway mucus hypersecretion in chronic airway inflammatory diseases, expectorant therapy is widely used to help relieve airway stenosis, avoid recurrent infection and exacerbation, and delay decline in lung function.
Drug therapies (expectorants)
Expectorants are drugs that promote mucus activity, alter mucus viscosity, and/or promote mucus clearance.Citation43 Drugs promoting mucus activity can be classified into the following categories (): 1) expectorants that remove mucus from the respiratory tract (hypertonic normal saline and wound-healing glycerol ether); 2) mucoregulators that alter mucus secretion (carbocysteine and macrolides); 3) mucolytics that reduce mucus viscosity (N-acetylcysteine, erdosteine, and fudosteine); and 4) mucokinetic agents (bronchodilators, myrtle oil, and ambroxol). Each category is discussed in more detail below.
Table 1 Mucoactive drugs and their potential mechanism of action
Expectorants
Hypertonic saline helps clear sputum, and administering 7% hypertonic saline to patients with pulmonary cystic fibrosis accelerates mucus discharge and improves airflow and lung function.Citation44,Citation45 Aerosol inhalation of 7% hypertonic saline as an auxiliary therapy can promote mucus discharge and improve lung function and quality of life in patients with bronchiectasis.Citation46 Studies in mouse models of COPD suggest that hypertonic saline can help prevent and treat airway mucus hypersecretion, but its value in patients remains to be demonstrated.Citation47 Further study has shown that some COPD patients suffer further airway stenosis while receiving 3% hypertonic saline.Citation48 In fact, patients with different types of chronic airway inflammatory diseases respond differently to hypertonic saline, and especially some COPD patients develop dyspnea when receiving atomizing hypertonic saline.Citation48 Therefore, hypertonic saline treatment should be used in accordance with its clinical indications.
Mucoregulators
A multicenter study involving a 1-year follow-up published in 2008 reported that carbocysteine (500 mg, 3 times daily) significantly reduced the frequency of acute COPD exacerbations and that health-related quality of life was significantly higher in COPD patients than in controls.Citation49 Another study supported the idea that carbocysteine can significantly reduce the frequency of acute exacerbations, reduce the frequency of catching colds, and improve the quality of life in COPD patients.Citation50 As a result, carbocysteine is the drug recommended by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) for treating COPD. Carbocysteine (500 mg, 3 times daily) can also improve the cough threshold and relieve cough symptoms in asthma patients, and it is the recommended treatment for cough-variant asthma.Citation51
Macrolides, in addition to their antibacterial activity, show good immunomodulatory activity and can inhibit inflammation and airway mucus hypersecretion.Citation52 Long-term administration of erythromycin (250 mg, twice daily), azithromycin (250 mg, once daily), and other macrolides helps reduce the frequency of acute exacerbations in COPD patients and improves their quality of life, and evidence-based medicine has also confirmed the clinical value of macrolides for reducing the occurrence of acute COPD exacerbations.Citation53–Citation55 Although no official guidelines include macrolides among classical expectorants, the available evidence suggests that macrolides can be recommended for achieving antibiotic effects and sputum clearance in COPD patients who require antibiotics.Citation56 Evidence also suggests that macrolides have limited ability to improve lung function, but they can improve airway hyperresponsiveness in asthma patients.Citation57 In bronchiectasis patients, the macrolides erythromycin (250 mg, twice daily after conversion) and azithromycin (250 mg, once daily) can help alleviate acute exacerbations in patients with infective COPD.Citation58,Citation59 The combination of roxithromycin (150 mg, once daily) and ambroxol can improve bronchiectasis and dyspnea scores in the stable phase of the disease.Citation60 The available evidence suggests that macrolides help reverse the exacerbation of pulmonary symptoms in bronchiectasis patients.Citation61 Macrolides can be recommended for long-term use in some bronchiectasis patients with severe symptoms of airway mucus hypersecretion; these patients benefit from the compounds’ dual effects as antibiotics and immunomodulators.
Mucolytics
N-acetylcysteine is a classic antioxidant that can reduce mucus viscosity and promote mucus discharge.Citation62 In COPD patients, high-dose N-acetylcysteine (600 mg, twice daily) can significantly improve lung function, reduce the frequency of acute COPD exacerbations, delay readmission, and enhance small airway function.Citation63 A randomized controlled trial of 1,006 patients aged 40–80 years and treated at 34 Chinese hospitals for moderate or severe COPD confirmed that long-term, high-dose N-acetylcysteine (600 mg, twice daily) can effectively prevent acute COPD exacerbations.Citation64 Even patients with moderate COPD benefited significantly. GOLD indicates that N-acetylcysteine can be used to prevent acute COPD exacerbations. Little evidence exists for or against the use of N-acetylcysteine in patients with asthma, pulmonary cystic fibrosis, or bronchiectasis; large, rigorous trials are needed to examine safety and efficacy in these populations.
Erdosteine, another mucolytic, can promote mucus discharge and improve lung function in elderly patients with bronchiectasis and chronic airway mucus hypersecretion.Citation65 Fudosteine is used to treat chronic respiratory diseases, such as bronchial asthma, chronic bronchitis, pulmonary emphysema, COPD, and bronchiectasis. It works as a mucoactive agent by inhibiting MUC5AC gene expression and related signaling pathways.Citation66,Citation67 Fudosteine has been shown to inhibit peroxynitrite-induced airway nitrosative stress in lung epithelial cells by direct scavenging of peroxynitrite and plays a protective role in COPD.Citation68 These findings suggest that fudosteine may be useful for controlling oxidative/carbonyl stress-related mucus secretion in patients with asthma, bronchiectasis, or COPD.Citation69
Mucokinetic agents
The prokinetic agent most widely used in the clinic is ambroxol, which can stimulate surfactant production in the respiratory tract, regulate secretion of serous and mucus fluids, improve mucus clearance in the ciliated and non-ciliated areas of the respiratory tract, reduce phlegm and ciliary adhesion, and facilitate expectoration.Citation70 Long-term ambroxol (75 mg, twice daily) can reduce the frequency of acute exacerbations in patients with severe COPD.Citation71 It can also benefit patients who experience acute exacerbations by alleviating oxidative stress reactions.Citation72 Recent work suggests that ambroxol can work synergistically with antibiotics in a rat model of catheter-associated P. aeruginosa infection.Citation73 Oral and injected ambroxol can be used in COPD outpatients and inpatients receiving expectorant therapy, particularly those with viscous sputum and expectoration difficulties. The usual dose is 30 mg, 3 times daily; this can be adjusted based on clinical conditions. Ambroxol can improve lung function and shorten hospitalization for bronchiectasis patients with infections.Citation74 The main components of myrtle oil expectorants are eucalyptol and limonene; they also contain pinene and standard myrtle oil. Standard myrtle oil can restore mucociliary clearance in the upper and lower respiratory tracts, thereby thinning and alkalifying mucus, enhancing mucociliary movement, significantly accelerating mucus motility, and promoting sputum discharge in a rat model of COPD.Citation75 The combination of standard myrtle oil and routine treatment has been shown to accelerate mucus motility in COPD patients more than routine treatment on its own, as well as improve blood gas composition.Citation76 Myrtle oil is often used as an expectorant for COPD patients with expectoration difficulties (eucalyptol–limonene–pinene at 300 mg, 2–3 times daily; standard myrtle oil at 300 mg, 3 times daily).
Bronchodilators dilate the bronchus and reduce mucus secretion. The bronchodilator tiotropium bromide, which is an anticholinergic agent, can effectively suppress goblet cell metaplasia induced by neutrophil elastase and mucin secretion; this implies that its therapeutic effects may involve suppressing airway mucus hypersecretion in mice; thus, tiotropium bromide can also be classified as a mucus regulator.Citation77 Consistent with this idea, formoterol, one of the long-acting β2-receptor agonists, may inhibit airway goblet cell hyperplasia and MUC5AC expression and reduce airway mucus hypersecretion in asthmatic mice.Citation78 The combination of β2 agonist formoterol and tiotropium bromide can accelerate airway mucus clearance, dilate the bronchus, alleviate airway stenosis, suppress mucin synthesis, and promote ciliary motions and mucus discharge in COPD patients.Citation79 Respiratory wards in hospitals have begun routinely combining bronchodilators and expectorants to treat COPD. In the People’s Republic of China, acute COPD exacerbations are routinely treated using the combination of aerosol inhalation of isopropyl bromide and intravenous injection of ambroxol. This treatment promotes sputum discharge, alleviates symptoms of airway obstruction such as hypoxia and dyspnea, and increases clinical efficacy in patients with acute COPD exacerbation.Citation80
A systematic review of 30 clinical studies involving 7,436 subjects concluded that expectorants can reduce the frequency of acute COPD exacerbations, benefiting COPD patients with a phenotype of frequent exacerbations and patients who are repeatedly admitted to hospital.Citation81 In contrast, a large evidence base is lacking about the efficacy of expectorants in treating asthma, pulmonary cystic fibrosis, and bronchiectasis. Future studies should assess efficacy of expectorants.
Nondrug therapies
Several nondrug therapies have been described for managing patients with chronic airway inflammatory disease and associated airway mucus hypersecretion. One therapy is smoking cessation, since tobacco smoke is one of the strongest risk factors for various respiratory diseases, including COPD and asthma. Toxic ingredients in tobacco smoke may stimulate epithelial goblet cell metaplasia in the airway as well as mucin secretion, leading to airway mucus hypersecretion. Smoking cessation may therefore cut off airway mucus hypersecretion “at the source.” In the People’s Republic of China, national guidelines have been published to guide efforts by health care workers to help patients stop smoking.Citation82
Another nondrug therapy is physiotherapy, in which patients are taught about deep breathing and effective coughing, or they receive chest percussion, postural expectoration, and inhalation therapies. Inhalation therapies, which can be administered via humidified inhalation or aerosol inhalation, can moisturize the airway, dilute sputum, facilitate expectoration, and prevent sputum scab formation. Such therapies are widely used to treat common respiratory tract diseases because they provide obvious benefits with few, if any, adverse reactions.Citation83
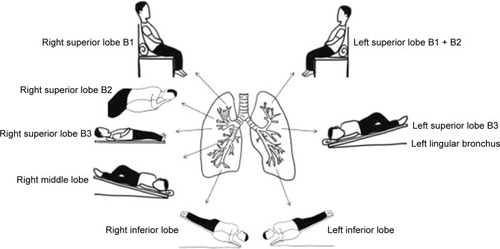
Effective mucus discharge requires different body positions depending on the site of a patient’s lesion,Citation84 and this postural drainage must be taught to patients. Appropriate body positions help the mucus flow from focus to large airway then to bronchus and help to get mucus out of the airway, and then, they play a role in mucus discharge. Patients with lesions in the right upper apical segment should expectorate while sitting in a vertical or inclined position and leaning slightly to the left. Patients with lesions in the right upper anterior segment should expectorate while supine with the right back slightly elevated. Patients with lesions in the right upper posterior segment should expectorate while in a left supine position and turning left by 45°, with a cushion placed in front to support the posture. Patients with lesions in the right middle segment should expectorate while supine with the chest and abdomen turned to the left by 45°, with a cushion placed behind to support the posture and with the right end of the bed elevated. Patients with lesions in the left upper posterior apical segment should expectorate while in the vertical sitting position or semi-supine position, with the body leaning to the right by 45° and with a cushion placed behind to support the posture. Patients with lesions in the left upper anterior segment and lingular segment should be supine, with the chest and abdomen turned to the right by 45°, with a cushion placed behind to support the posture and the left end of the bed elevated. Patients with lesions in the left lower dorsal segment should be prone, leaning slightly with the affected side upward and the head lowered. Patients with lesions in the left lower basal segment should be prone, leaning by 45° with the affected side upward, the head downward, and the chest upward; alternatively, they can adopt a contralateral supine position with the chest and abdomen turned to the right by 45°, the head lowered and facing downward and the feet pointing upward ().
Figure 1 The sketch map of body positions for postural drainage.
A third nondrug therapy is high-frequency chest wall oscillation. This is often used to enhance airway mucus clearance in patients with pulmonary cystic fibrosis and bronchiectasis, and it can significantly improve the quality of life in COPD patients and reduce sputum volume.Citation85 Intermittent positive end-expiratory pressure (PEEP) can dilate the small airway, reduce small airway obstruction, promote the sputum drainage and discharge, and accelerate mucus clearance in COPD patients. Performing PEEP twice daily for 15 minutes each time during 10 days can promote expectoration and reduce mucus density and production of purulent sputum; therefore, it may be useful for COPD patients with symptoms of airway mucus hypersecretion.Citation86
Future studies and expectations
Airway mucus hypersecretion is an important driver of airway obstruction, rapid decline in lung function, and increased frequency of acute exacerbation in patients with chronic airway inflammatory diseases; it is closely related to patient prognosis. Detailed investigation into the signaling pathways and downstream effector molecules involved in airway mucus hypersecretion will improve our understanding and the treatment of these chronic diseases. One challenge is to systematically explore how to combine traditional drugs with classic expectorants and how to combine expectorants to achieve optimal therapeutic effects. Clinicians should recognize the benefits of expectorant therapies for patients with chronic airway inflammatory diseases and should continuously seek to improve and innovate treatments for such patients.
Acknowledgments
This work was supported by National Key Research and Development Program (2016YFC0903600 and 2016YFC1304500), National Natural Science Foundation of China (81230001, 81470236 and 81670038), and the Science and Technology Pillar Program of the Department of Science and Technology of Sichuan province (2015SZ0151). The funders had no role in study design, data collection or analysis, decision to publish, and manuscript preparation. We also express our sincere thanks to the European Respiratory Society for its generosity in supplying the copyright transfer of to help spread scientific knowledge.
Disclosure
The authors report no conflicts of interest in this work.
References
- FahyJVDickeyBFAirway mucus function and dysfunctionN Engl J Med2010363232233224721121836
- CurranDRCohnLAdvances in mucous cell metaplasia: a plug for mucus as a therapeutic focus in chronic airway diseaseAm J Respir Cell Mol Biol201042326827519520914
- CerveriIBrusascoVRevisited role for mucus hypersecretion in the pathogenesis of COPDEur Respir Rev20101911610911220956178
- WenFQShenYCExpectorant therapy revisited in chronic obstructive pulmonary diseaseZhonghua Jie He He Hu Xi Za Zhi2011344243245 Chinese21609602
- RogersDFMucoactive agents for airway mucus hypersecretory diseasesRespir Care20075291176119317716385
- HensonPMDampening inflammationNat Immunol20056121179118116369556
- KorfhagenTRKitzmillerJChenGSAM-pointed domain ETS factor mediates epithelial cell-intrinsic innate immune signaling during airway mucous metaplasiaProc Natl Acad Sci U S A201210941166301663523012424
- HoltzmanMJByersDEAlexander-BrettJWangXThe role of airway epithelial cells and innate immune cells in chronic respiratory diseaseNat Rev Immunol2014141068669825234144
- TynerJWKimEYIdeKBlocking airway mucous cell metaplasia by inhibiting EGFR antiapoptosis and IL-13 transdifferentiation signalsJ Clin Invest2006116230932116453019
- DijkstraAEBoezenHMvan den BergeMDissecting the genetics of chronic mucus hypersecretion in smokers with and without COPDEur Respir J2015451607525234806
- ChandHSMontanoGHuangXA genetic variant of p53 restricts the mucous secretory phenotype by regulating SPDEF and Bcl-2 expressionNat Commun20145556725429397
- AllinsonJPHardyRDonaldsonGCShaheenSOKuhDWedzichaJAThe presence of chronic mucus hypersecretion across adult life in relation to chronic obstructive pulmonary disease developmentAm J Respir Crit Care Med2016193666267226695373
- ReidKBClarkHPalaniyarNSurfactant and lung inflammationThorax200560862062216061700
- COPD group of Chinese Thoracic SocietyGuideline for diagnosis and treatment of chronic obstructive pulmonary disease (updated 2013)Zhonghua Jie He He Hu Xi Za Zhi2013364255265 Chinese
- ZhongNWangCYaoWPrevalence of chronic obstructive pulmonary disease in China: a large, population-based surveyAm J Respir Crit Care Med2007176875376017575095
- de MarcoRAccordiniSCerveriIIncidence of chronic obstructive pulmonary disease in a cohort of young adults according to the presence of chronic cough and phlegmAm J Respir Crit Care Med20071751323917008642
- YamaneTHattoriNKitaharaYProductive cough is an independent risk factor for the development of COPD in former smokersRespirology201015231331820070589
- MaRWangYChenGZhangHZWanHYHuangSGGoblet cell hyperplasia and abnormalities in mucin expression in COPD patientsShanghai Di Er Yi Ke Da Xue Xue Bao20042412103110331044 Chinese
- MiravitllesMGuerreroTMayordomoCSánchez-AgudoLNicolauFSegúJLFactors associated with increased risk of exacerbation and hospital admission in a cohort of ambulatory COPD patients: a multiple logistic regression analysis. The EOLO Study GroupRespiration200067549550111070451
- HoggJCChuFSTanWCSurvival after lung volume reduction in chronic obstructive pulmonary disease: insights from small airway pathologyAm J Respir Crit Care Med2007176545445917556723
- BurgelPRNesme-MeyerPChanezPCough and sputum production are associated with frequent exacerbations and hospitalizations in COPD subjectsChest2009135497598219017866
- WedzichaJASinghRMackayAJAcute COPD exacerbationsClin Chest Med201435115716324507843
- WedzichaJAMechanisms of chronic obstructive pulmonary disease exacerbationsAnn Am Thorac Soc201512Suppl 2S157S159
- ZhangWLuHPengLChronic bronchitis leads to accelerated hyperinflation in COPD patients during exerciseRespirology201520461862525799924
- MeekPMPetersenHWashkoGRChronic bronchitis is associated with worse symptoms and quality of life than chronic airflow obstructionChest2015148240841625741880
- MiravitllesMCough and sputum production as risk factors for poor outcomes in patients with COPDRespir Med201110581118112821353517
- Asthma Workgroup, Chinese Thoracic Society, Chinese Society of General PractitionersChinese guideline for the prevention and management of bronchial asthma (Primary Health Care Version)J Thorac Dis20135566767724255781
- Del DonnoMBittesnichDChettaAOlivieriDLopez-VidrieroMTThe effect of inflammation on mucociliary clearance in asthma: an overviewChest200011841142114911035690
- de MarcoRMarconAJarvisDPrognostic factors of asthma severity: a 9-year international prospective cohort studyJ Allergy Clin Immunol200611761249125616750983
- ThomsonNCChaudhuriRMessowCMChronic cough and sputum production are associated with worse clinical outcomes in stable asthmaRespir Med2013107101501150823927851
- SirouxVBoudierABousquetJPhenotypic determinants of uncontrolled asthmaJ Allergy Clin Immunol20091244681687.e319665764
- KuyperLMParéPDHoggJCCharacterization of airway plugging in fatal asthmaAm J Med2003115161112867228
- AikawaTShimuraSSasakiHEbinaMTakishimaTMarked goblet cell hyperplasia with mucus accumulation in the airways of patients who died of severe acute asthma attackChest199210149169211555462
- Workgroup of bronchiectasis diagnosis and managementExpert consensus on diagnosis and management of adult bronchiectasisZhonghua Jie He He Hu Xi Za Zhi2012357485492 Chinese
- TambascioJde SouzaHCMartinezJAAfonsoJLJardimJRGastaldiACThe influence of purulence on ciliary and cough transport in bronchiectasisRespir Care201358122101210623674811
- GoeminnePCVandoorenJMoelantsEAThe Sputum Colour Chart as a predictor of lung inflammation, proteolysis and damage in non-cystic fibrosis bronchiectasis: a case-control analysisRespirology201419220321024286471
- LiuTWKangJAnalysis of clinical features of cystic fibrosis in ChineseZhong Guo Quan Ke Yi Xue152428072810 Chinese
- KredaSMDavisCWRoseMCCFTR, mucins, and mucus obstruction in cystic fibrosisCold Spring Harb Perspect Med201229a00958922951447
- CrawfordBMonzBHohlfeldJDevelopment and validation of a cough and sputum assessment questionnaireRespir Med2008102111545155518662868
- MonzBUSachsPMcDonaldJCrawfordBNivensMCTetzlaffKResponsiveness of the cough and sputum assessment questionnaire in exacerbations of COPD and chronic bronchitisRespir Med2010104453454119917525
- HardinMRennardSIWhat’s new with the St George’s Respiratory Questionnaire and why do we care?Chronic Obstr Pulm Dis201742838628848916
- CassidyRNRobertsMEColbySMValidation of a respiratory symptom questionnaire in adolescent smokersTob Regul Sci20151212112826236764
- BalsamoRLanataLEganCGMucoactive drugsEur Respir Rev20101911612713320956181
- DonaldsonSHBennettWDZemanKLKnowlesMRTarranRBoucherRCMucus clearance and lung function in cystic fibrosis with hypertonic salineN Engl J Med2006354324125016421365
- ElkinsMRRobinsonMRoseBRA controlled trial of long-term inhaled hypertonic saline in patients with cystic fibrosisN Engl J Med2006354322924016421364
- KellettFRobertNMNebulised 7% hypertonic saline improves lung function and quality of life in bronchiectasisRespir Med2011105121831183522018993
- GraeberSYZhou-SuckowZSchatternyJHirtzSBoucherRCMallMAHypertonic saline is effective in the prevention and treatment of mucus obstruction, but not airway inflammation, in mice with chronic obstructive lung diseaseAm J Respir Cell Mol Biol201349341041723590312
- TaubeCHolzOMückeMJörresRAMagnussenHAirway response to inhaled hypertonic saline in patients with moderate to severe chronic obstructive pulmonary diseaseAm J Respir Crit Care Med200116410 Pt 11810181511734428
- ZhengJPKangJHuangSGEffect of carbocisteine on acute exacerbation of chronic obstructive pulmonary disease (PEACE Study): a randomised placebo-controlled studyLancet200837196292013201818555912
- YasudaHYamayaMSasakiTCarbocisteine reduces frequency of common colds and exacerbations in patients with chronic obstructive pulmonary diseaseJ Am Geriatr Soc200654237838016460403
- IshiuraYFujimuraMYamamoriCEffect of carbocysteine on cough reflex to capsaicin in asthmatic patientsBr J Clin Pharmacol200355650451012814442
- LingLLinJTAnti-inflammatory role of macrolides on respiratory diseasesZhong Ri You Hao Yi Yuan Xue Bao2009234247253 Chinese
- SeemungalTAWilkinsonTMHurstJRPereraWRSapsfordRJWedzichaJALong-term erythromycin therapy is associated with decreased chronic obstructive pulmonary disease exacerbationsAm J Respir Crit Care Med2008178111139114718723437
- AlbertRKConnettJBaileyWCAzithromycin for prevention of exacerbations of COPDN Engl J Med2011365868969821864166
- YaoGYMaYLZhangMQGaoZCMacrolide therapy decreases chronic obstructive pulmonary disease exacerbation: a meta-analysisRespiration201386325426023817204
- SpagnoloPFabbriLMBushALong-term macrolide treatment for chronic respiratory diseaseEur Respir J201342123925123180583
- ReiterJDemirelNMendyAMacrolides for the long-term management of asthma – a meta-analysis of randomized clinical trialsAllergy20136881040104923895667
- SerisierDJMartinMLMcGuckinMAEffect of long-term, low-dose erythromycin on pulmonary exacerbations among patients with non-cystic fibrosis bronchiectasis: the BLESS randomized controlled trialJAMA2013309121260126723532242
- AltenburgJde GraaffCSStienstraYEffect of azithromycin maintenance treatment on infectious exacerbations among patients with non-cystic fibrosis bronchiectasis: the BAT randomized controlled trialJAMA2013309121251125923532241
- LiuJFZhongXNHeZYImpact of treatment with low dose roxithromycin on stable bronchiectasisZhonghua Jie He He Hu Xi Za Zhi20123511824827 Chinese23290037
- ShiZLPengHHuXWHuJGEffectiveness and safety of macrolides in bronchiectasis patients: a meta-analysis and systematic reviewPulm Pharmacol Ther201428217117824076368
- LiuSXYangLEffect of N-acetylcysteine on SOD, MDA in COPD patients with different stagesZhong Guo Lao Nian Xue Za Zhi200626810281029 Chinese
- TseHNRaiteriLWongKYHigh-dose N-acetylcysteine in stable COPD: the 1-year, double-blind, randomized, placebo-controlled HIACE studyChest2013144110611823348146
- ZhengJPWenFQBaiCXTwice daily N-acetylcysteine 600 mg for exacerbations of chronic obstructive pulmonary disease (PANTHEON): a randomised, double-blind placebo-controlled trialLancet Respir Med20142318719424621680
- ZhouBQLiXKClinic efficacy of erdosteine on elderly bronchiectasis patients with airway mucus hypersecretionShi Yong Yi Xue Za Zhi201127610661068 Chinese
- RheeCKKangCMYouMBEffect of fudosteine on mucin productionEur Respir J20083251195120218579549
- Ueno-IioTShibakuraMIioKEffect of fudosteine, a cysteine derivative, on airway hyperresponsiveness, inflammation, and remodeling in a murine model of asthmaLife Sci20139220–211015102323583570
- OsoataGOHanazawaTBrindicciCItoMPeroxynitrite elevation in exhaled breath condensate of COPD and its inhibition by fudosteineChest200913561513152019188555
- RahmanIMacNeeWAntioxidant pharmacological therapies for COPDCurr Opin Pharmacol201212325626522349417
- MalerbaMRagnoliBAmbroxol in the 21st century: pharmacological and clinical updateExpert Opin Drug Metab Toxicol2008481119112918680446
- MalerbaMPonticielloARadaeliABensiGGrassiVEffect of twelve-months therapy with oral ambroxol in preventing exacerbations in patients with COPD. Double-blind, randomized, multicenter, placebo-controlled study (the AMETHIST Trial)Pulm Pharmacol Ther2004171273414643168
- KuangSGZhangHYZhangJThe effect of ambroxol on oxidation/antioxidant imbalance in AECOPD patientsZhong Hua Nei Ke Za Zhi2001402125126 Chinese
- LuQYuJBaoLRanTZhongHEffects of combined treatment with ambroxol and ciprofloxacin on catheter-associated Pseudomonas aeruginosa biofilms in a rat modelChemotherapy2013591515623816803
- ChenCYLiuHLThe clinical efficacy of intravenous and bronchoalveolar lavage ambroxol for patients with bronchiectasis and infectionZhong Guo She Qu Yi Shi2013156128129 Chinese
- CaoLChenYZhaoYEffect of Myrtol standardized on mucus hypersecretion and clearance of Pseudomonas aeruginosa in a rat model of chronic obstructive pulmonary diseaseArzneimittelforschung2011611268569222282955
- ZhangXXShiTNieXHSystematic review of standardized myrtol in the treatment of COPDZhong Guo Yao Ye20132253639
- AraiNKondoMIzumoTTamaokiJNagaiAInhibition of neutrophil elastase-induced goblet cell metaplasia by tiotropium in miceEur Respir J20103551164117119897560
- TanYFZhangWYangLJiangSPThe effect of formoterol on airway goblet cell hyperplasia and protein Muc5ac expression in asthmatic miceEur Rev Med Pharmacol Sci201115774375021780541
- MeyerTReitmeirPBrandPEffects of formoterol and tiotropium bromide on mucus clearance in patients with COPDRespir Med2011105690090621397483
- ZhengYLZengXLTherapeutic effect analysis of Ambroxol in combination with inhaled Combivent on acute exacerbation of chronic obstructive pulmonary diseaseZhong Hua Lao Nina Yi Xue Za Zhi2014331112101211 Chinese
- PoolePBlackPNCatesCJMucolytic agents for chronic bronchitis or chronic obstructive pulmonary diseaseCochrane Database Syst Rev20128CD001287
- World Health Organization Collaborating Centre for Tobacco or Health, Tobacco Control Office of Chinese Center for Disease Control and Prevention, Chinese Association on Tobacco Control Hospital Smoking Control CommitteeChina clinical smoking cessation guidelines (2007 edition, the Tentative)Guo Ji Hu Xi Za Zhi20082816961970 Chinese
- Respiratory Care Group of Chinese Thoracic SocietyExpert consensus on aerosol treatmentZhonghua Jie He He Hu Xi Za Zhi20133711805808 Chinese
- FinkJBPositioning versus postural drainageRespir Care200247776977712088547
- ChakravortyIChahalKAustinGA pilot study of the impact of high-frequency chest wall oscillation in chronic obstructive pulmonary disease patients with mucus hypersecretionInt J Chron Obstruct Pulmon Dis2011669369922259246
- VenturelliECrisafulliEDeBiaseAEfficacy of temporary positive expiratory pressure (TPEP) in patients with lung diseases and chronic mucus hypersecretion. The UNIKO® project: a multicentre randomized controlled trialClin Rehabil201327433634622967853
